Beruflich Dokumente
Kultur Dokumente
Pulse March 2013 Cropped CMYK LR
Hochgeladen von
khamrmdOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pulse March 2013 Cropped CMYK LR
Hochgeladen von
khamrmdCopyright:
Verfügbare Formate
Supporting GPs since 1960
March 2013 | www.pulsetoday.co.uk
Plus
Key questions
on type 2 diabetes
Why has it become so
hard to recruit GPs?
Ten things you need
to do before April
Peverley on sticking
it to the malingerers
IN THIS ISSUE
2.5 CPD HOURS
DEMENTIA
SCREENING:
CRUEL
OR
KIND?
Why the planned
DES is proving so
controversial
Relax, Urgency controlled
PRESCRIBING INFORMATION
Presentation: Vesicare
film-coated tablets containing 5 mg or 10 mg solifenacin succinate.
Indication: Symptomatic treatment of urge incontinence and/or increased urinary
frequency and urgency as may occur in patients with overactive bladder syndrome. Dosage:
Adults: Recommended dose: 5 mg once daily. If needed, the dose may be increased to
10 mg once daily. Children and adolescents: Should not be used. Contraindications: Urinary
retention, severe gastrointestinal condition (including toxic megacolon), myasthenia
gravis or narrow-angle glaucoma and in patients at risk for these conditions. Patients
hypersensitive to the active substance or to any of the excipients, or undergoing
haemodialysis, or with severe hepatic impairment, or with severe renal or moderate hepatic
impairment and on treatment with a potent CYP3A4 inhibitor. Warnings and Precautions:
No clinical data are available from women who became pregnant while taking solifenacin.
Caution should be exercised when prescribing to pregnant women. The use of Vesicare
should be avoided during breast-feeding. Assess other causes of frequent urination before
prescribing. Use with caution in patients with clinically significant bladder outflow
obstruction at risk of urinary retention, gastrointestinal obstructive disorders, risk
of decreased gastrointestinal motility, severe renal or moderate hepatic impairment
(doses not to exceed 5 mg), concomitant use of a potent CYP3A4 inhibitor, hiatus
hernia/gastroesophageal reflux and/or patients currently taking medicines that can cause or
exacerbate oesophagitis, autonomic neuropathy. QT prolongation and Torsades de Pointes
have been observed in patients with risk factors, such as pre-existing long QT syndrome and
hypokalaemia. Safety and efficacy have not yet been established in patients with
a neurogenic cause for detrusor overactivity. Patients with rare hereditary problems of
galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorption
should not take this medicinal product. Angioedema with airway obstruction and
anaphylactic reaction have been reported with some patients on Vesicare
. Interactions:
Concomitant medication with other medicinal products with anticholinergic properties may
result in more pronounced therapeutic effects and undesirable effects. Allow one week
after stopping Vesicare
before commencing other anticholinergic therapy. Therapeutic
effect may be reduced by concomitant administration of cholinergic receptor agonists.
Can reduce effects of stimulators of gastrointestinal tract motility. If used concomitantly
with ketoconazole or other CYP3A4 potent inhibitor, maximum dose should be 5 mg due
to 2-3 fold increase in AUC of Vesicare
. Pharmacokinetic interactions are possible with
other CYP3A4 substrates with higher affinity and CYP3A4 inducers. Adverse Effects: Dry
mouth, blurred vision, constipation, nausea, dyspepsia, abdominal pain, urinary tract
infection, peripheral oedema, colonic obstruction, rash, urinary retention, hallucinations,
confusional state, angioedema, anaphylactic reaction, delirium, Torsade de Pointes,
electrocardiogram QT prolonged. Prescribers should consult the Summary of Product
Characteristics in relation to other side effects. Basic NHS Cost: Vesicare
5 mg blister packs
of 30 tablets 27.62; Vesicare
10 mg blister packs of 30 tablets 35.91. Legal Category:
POM. Product Licence Number: Vesicare
5 mg PL 00166/0197; Vesicare
10 mg
PL 00166/0198. Date of Revision: January 2013. Further information available from: Astellas
Pharma Ltd, 2000 Hillswood Drive, Chertsey, KT16 0RS. Vesicare
is a Registered Trademark.
For full prescribing information please refer to the Summary of Product Characteristics.
For medical information phone 0800 783 5018.
Date of preparation: February 2013
VES12484UK(1)
Adverse events should be reported. Reporting forms
and information can be found at www.mhra.gov.uk/yellowcard
Adverse events should also be reported to Astellas Pharma Ltd.
Please contact 0800 783 5018.
www.pulsetoday.co.uk Pulse March 2013 3
c
o
v
e
r
p
i
c
t
u
r
e
:
D
r
r
o
B
e
r
t
F
r
i
e
D
L
A
N
D
,
s
c
i
e
N
c
e
p
h
o
t
o
L
i
B
r
A
r
y
/
G
i
o
v
A
N
N
i
t
A
i
t
/
A
M
A
N
D
A
o
A
k
L
e
y
/
j
o
e
D
M
i
L
e
s
March 2013
How not to miss
necrotising fasciitis
Page 50
A GPs day in photos
Page 64
We are paid less than
our salaried GP
Page 22
ThIS MONTh
6 Coverstory
Willearlierdementiadiagnosisharmpatients?
Why some GPs believe the planned case-finding DES may backfire
10 Digest
Your round-up of all the key political, finance and commissioning news
12 Contractupdate
The GPC responds to the threatened imposition
16 Clinicalround-up
All the latest guidelines, papers and policy developments
18 Investigation:WhyhasrecruitingGPsbecomesohard?
How the GP vacancy rate has quadrupled in just two years
22 Investigation:PMspracticessqueezedasfundingreviewsbite
With practices facing brutal cuts, does PMS have a future?
VIEWS
29 editorial
A profession losing its appeal
30 Feedback
Highlights from your letters and online comments
32 theBigInterview:DrPaulCundy
The GPCs IT lead on telehealth, GPES and Summary Care Records
36 Debate:CanGPsmonitorhospitalcare?
Two GPs argue for and against the Francis Inquirys recommendation
37 McCartney
on how Mid Staffs shows the folly of relying on data and box-ticking
38 Copperfeld
on whether patients are getting more stupid
70 Peverley
on how he gives scroungers short shrift
cLINIcaL
42 Keyquestionsontype2diabetes1.5CPDHoUrs
Expert answers to Dr David Russells dilemmas
44 theinformation:Bellspalsy
Two specialists advise, using PUNs and DENs
47 Picturequiz:CutaneousmanifestationsofHIv
Test your diagnostic skills
48 Practicalgenetics:Cancer1CPDHoUr
Dr Judith Hayward advises on patients with a family history of bowel cancer
50 Hownottomissnecrotisingfasciitis
Dr Adrian Boyle highlights the signs and pitfalls
YOUr PracTIcE
60 tenthingstodotoprepareforApril2013
Our GP panel on getting ready for the CQC, CCGs and the contract changes
62 Financediary:Avoidbecomingadysfunctionalpractice
Accountant Bob Senior offers tips
63 Dilemma:Aconfictofinterestbetweenpartners
What to do when one partner is a provider and another is on the CCG board
64 Workinglife:DrDavidWeinstein
A GP and a photographer revisit a photo essay that followed a 1940s doctor
4 March 2013 Pulse www.pulsetoday.co.uk
GP contract latest
Follow the very latest developments in
the GP contract talks
pulsetoday.co.uk/gpcontract
How not to miss type 1 diabetes
in children
The key signs and pitfalls in diagnosing
the condition
pulsetoday.co.uk/hntm-diabetes
Paper of the day
The best of the latest research, plus its
implications for GPs
pulsetoday.co.uk/paper-of-the-day
Dr Tom Gillham
Meet Pulses brand-new blogger
pulsetoday.co.uk/blogs
Paediatric clinic:
Intussusception
A nine-month-old boy presents to his GP with a
two-day history of non-bilious vomiting and crying
pulsetoday.co.uk/paediatric-clinic
Photo essay: Dr David Weinstein
View the full gallery of images from
a day in the life of one GP
pulsetoday.co.uk/weinstein
This months most
popular modules
Key questions on gout
1.5 CPD HOURS
Excellent module, clear with good
evidence-based references
Dr Nigel Chatwin
Clinical casebook: addiction
1.5 CPD HOURS
Excellent and very relevant to practice
Dr Maajida Ahmad
Key questions on asthma
1.5 CPD HOURS
An excellent educational module with
precise guidance for GPs
Dr Bhasker Patel
Guideline debrief: ectopic
pregnancy and miscarriage
1.5 CPD HOURS
Interesting and highly applicable
Dr Kathleen Turner
The information: plantar fasciitis
0.5 CPD HOURS
Very helpful c lear and straightforward
Dr Amanda Brown
Dont miss out join now at
pulse-learning.co.uk
pulse-learning.co.uk pulsetoday.co.uk
ONLINE-ONLY HIGHLIGHTS
You can now read
Pulse on your iPad
Over the past couple of months
weve had a fantastic response
from GPs to the new-look Pulse
magazine and one repeated
question: When are you launching
an iPad app?
Im pleased to say that we have
now done just that. Our new
interactive app enables you to
read all our trademark
investigations, analyses and
clinical features as they appear
in print, but youll be able to
do much more besides
watch embedded videos,
access further information
directly online and link up
your reading with CPD on
Pulse Learning.
The app is completely free, and
as a bonus youll get each months
Pulse as soon as its published,
before your print copy arrives
by post.
To nd out more and
download the app, go to
pulsetoday.co.uk/iPad and
as with the magazine, please
do let me know what you think
and how it can be improved at
editor@pulsetoday.co.uk
Steve Nowottny
Editor
Presentation: Betmiga
prolonged-release flm-coated
tablets containing 25mg or 50mg mirabegron. Indication:
Symptomatic treatment of urgency, increased micturition
frequency and/or urgency incontinence as may occur in adult
patients with overactive bladder (OAB) syndrome. Dosage:
Adults (including the elderly): Recommended dose: 50mg once
daily. Children and adolescents: Should not be used.
Contraindications: Hypersensitivity to active substance or
any of the excipients. Warnings and Precautions: Should
not be used in patients with end stage renal disease (or patients
requiring haemodialysis), severe hepatic impairment and severe
uncontrolled hypertension. Not recommended in patients with
severe renal impairment and/or moderate hepatic impairment
concomitantly receiving strong CYP3A inhibitors. Dose
adjustment to 25mg is recommended in patients with; mild/
moderate renal and/or mild hepatic impairment receiving
strong CYP3A inhibitor concomitantly and in patients with
severe renal and/or moderate hepatic impairment. Caution in
patients with a known history of QT prolongation or in patients
taking medicines known to prolong the QT interval. Not
recommended during pregnancy and in women of childbearing
potential not using contraception. Not recommended
during breastfeeding. Interactions: Clinically relevant drug
interactions between Betmiga
and medicinal products that
inhibit, induce or are a substrate for one of the CYP isozymes
or transporters are not expected, except for inhibitory effect
on the metabolism of CYP2D6 substrates. Betmiga
is a
moderate and time-dependent inhibitor of CYP2D6 and weak
inhibitor of CYP3A. No dose adjustment needed when
administered with CYP2D6 inhibitors or CYP2D6 poor
metabolisers. Caution if co-administered with medicines with a
narrow therapeutic index and signifcantly metabolised by
CYP2D6. When initiating in combination with digoxin, the
lowest dose for digoxin should be prescribed and serum
digoxin should be monitored and used for titration of digoxin
dose. Substances that are inducers of CYP3A or P-gp decrease
the plasma concentrations of Betmiga
. No dose adjustment is
needed for Betmiga
when administered with therapeutic
doses for rifampicin or other CYP3A or P-gp inducers. The
potential for inhibition of P-gp by Betmiga
should be
considered when combined with sensitive P-gp substrates.
Increases in mirabegron exposure due to drug-drug interactions
may be associated with increases in pulse rate. Adverse
Effects: Urinary tract infection, tachycardia, vaginal infection,
cystitis, palpitation, atrial fbrillation, dyspepsia, gastritis, urticaria,
rash, rash macular, rash papular, pruritus, joint swelling,
vulvovaginal pruritus, blood pressure increase, liver enzymes
increase, eyelid oedema, lip oedema, leukocytoclastic vasculitis
and purpura. Prescribers should consult the Summary of Product
Characteristics in relation to other side effects. Pack and prices:
Betmiga
25mg and Betmiga
50mg pack of 30 tablets 29.00.
Legal Category: POM. Product Licence Number:
Betmiga
25mg EU/1/12/809/001 - 007; Betmiga
50mg
EU/1/12/809/008 - 014. Date of Preparation: January 2013.
Further information available from: Astellas Pharma Ltd,
2000 Hillswood Drive, Chertsey, Surrey, KT16 0RS, UK. Betmiga
is a Registered Trademark. For full prescribing information
please refer to the Summary of Product Characteristics.
For Medical Information phone 0800 783 5018.
Date of preparation: February 2013 BET13068UK
Prescribing information
Adverse events should be reported.
Reporting forms and information can
be found at www.mhra.gov.uk/yellowcard
Adverse events should also be reported
to Astellas Pharma Ltd.
Please contact 0800 783 5018
Reference:
1. Gras J. Drugs of Today 2012;48(1):2532.
N
E
W
Its time to think
of something else.
The rst in class
3
-adrenoceptor
agonist to treat the symptoms of
overactive bladder (OAB)
1
MUK147_Betmiga_290x230_AW.indd 1 13/02/2013 09:59
6 March 2013 Pulse www.pulsetoday.co.uk
cover story
this month
When he launched his challenge on
dementia a year ago, Prime Minister
David Cameron fired the starting gun on
a frantic stream of activity at the DH.
To the delight of dementia charities,
he said diagnosis and awareness levels
were shocking and accused the NHS of
collective denial over the true
prevalence of the disease.
He then tasked civil servants with
raising diagnosis rates for the condition
by 2015, with GPs at the forefront of the
plan. Now practices face a potential
3,600 cut in income if they do not sign
up to a new dementia case-finding DES
from April, funded by the retirement of
QOF indicators.
But GPs are questioning the basis of
the DES, and weighing up the pros and
cons of labelling thousands of patients
as having dementia when the services to
support them may not be in place and the
diagnosis could have far-reaching
consequences for their daily lives.
As controversy over the programme
grows, Pulse asks if the Governments
plans for dementia case-finding could
cause more harm than good.
Variation
The drive to increase diagnosis rates is
based on figures showing that only 42%
of people with dementia in England have
a formal diagnosis.
The Alzheimers Society estimates
were based on age-specific rates
determined in a review of evidence by
Kings College London and the London
School of Economics in 2007. They show
wide regional variation, with as few as
34% of the true number of cases
diagnosed in North Wales and as many
as 70% in Glasgow (see map, page 8).
A spokesperson for the charity says
the variation is due to a lack of joined-up
services: GPs want to know that there
are places they can refer to and that there
are services in place, so theres no reason
to have a nihilistic attitude.
But health secretary Jeremy Hunt has
gone much further, accusing GPs of
being unable or unwilling to diagnose
dementia, and showing a grim fatalism
that denies patients access to treatment.
In a recent article in the Daily Telegraph,
he claimed: Some even believe that
without an effective cure theres no point
putting people through the anxiety of a
memory test even though drugs can help
stave off the condition for several years.
In the Spectator, Conservative
commentator Richard Marsh claims this
emphasis on dementia is a sign of
a canny minister who knows it is
important to be seen to take action on
a disease of great public concern.
The move may be good politics, but is
it good medicine? The most recent NICE
appraisal of anticholinesterase inhibitors
concluded that they offer only small
clinical benefits for cognitive function
and have uncertain benefits for
behaviour, and there was little evidence
to support anecdotal claims they reduce
progression of dementia and delay time
to institutionalisation.
The drugs are now recommended by
NICE as options for managing mild as
well as moderate Alzheimers disease,
but as author and Alzheimers patient Sir
Terry Pratchett says, drugs for dementia
are like sandbags in the stream they
slow its progress but dont stop it.
DES specifcations
Since last March, targets to increase
diagnosis rates have been included in the
NHS outcomes framework, dementia
champions have been placed on hospital
wards and an audit of prescribing in
dementia has been launched.
But the biggest change will be in
Will earlier
dementia
diagnosis
harm
patients?
As practices prepare to take on the new dementia case-
fnding DES from April, Michael Woodhead investigates
claims widespread screening will do more harm than good
Read the draft
specifcations
for the DES
pulsetoday.co.uk/
dementia-spec
s
c
i
e
n
c
e
p
h
o
t
o
l
i
b
r
a
r
y
www.pulsetoday.co.uk Pulse March 2013 7
general practice, which will be tasked by
the new DES with screening all patients
aged 75 and over, those aged 60 and over
with risk factors, and all patients with
learning disabilities or long-term
neurological problems.
The DHs proposed specifications for
the DES due to be finalised in the next
few weeks by the NHS Commissioning
Board suggest patients should be
questioned to establish if they are
concerned about memory; then
a specific test, such as GPCog, should
be used to detect any early signs.
If a patient has suspected dementia,
GPs will be mandated to refer them to
specialist services, such as a memory
clinic, to confirm the diagnosis, then
provide treatment if necessary and give
advice and support to the patients carer.
The DH says the DES is designed to
promote early diagnosis, and insists it is
not a screening scheme.
We are suggesting GPs could deliver
a proactive approach to assessing
patients known to be at risk as a way of
improving diagnosis and care.
Controversy
The DES has proved controversial so far,
with a group of doctors, including former
RCGP president Dr Iona Heath, setting
up a petition opposing it.
They claim the DES case-finding
programme is being introduced without
any evidence of benefit and that it could
harm patients through misdiagnosis and
overtreatment, as well as distressing
patients and their families.
Dr Martin Brunet, a GP in Guildford,
Surrey, and one of the doctors leading the
petition which has 300 signatures
says the DES could confuse patients.
He says: Theres no consent, no prior
warning, which makes it quite unethical.
I think the Government and the people
promoting this are being paternalistic
and not respecting patient consent,
choices and autonomy.
The group has been invited by
dementia tsar Professor Alistair Burns to
propose an alternative way of boosting
diagnosis rates but has yet to agree on
the possible solution.
Dr Brunet says current services need
improvement, as waiting times at memory
clinics are too long and patients with
dementia dont receive adequate help, for
instance with advanced care planning or
power of attorney. He says: People
Were just
giving
someone
a label of
dementia
Dr Martin
Brunet
Expert view
Professor Steve Iliffe
GPs are right to be wary
I am not sure the scale of the problem
is as big as the Government thinks it is.
In our EVIDEM study of GP dementia
diagnosis, we are not fnding large
numbers of patients you have to do
anything with. The idea that there is
some massive unmet need is probably
not right.
I suspect some [prevalence] fgures
have been infated over time.
We are fnding a tendency to
under-document dementia in the QOF.
GPs are cautious over labelling
patients with dementia this is
understandable and may be right.
The patient may respond negatively
and it might be the last thing they want
on their records. It does close the door
to some things, particularly rehabilita-
tion services, for instance, post-stroke.
There is a lot of GP bashing over
dementia that is not warranted.
Professor Steve Iliffe, professor of
primary care for older people at
University College London and a GP in
Kilburn, north west London, is leading
the unpublished EVIDEM study
Who is likely to be
screened under the DES?
Patients aged 60 and over with CVD,
stroke, peripheral vascular disease
and diabetes
Patients with learning disabilities
Patients with long-term neurological
conditions, such as Parkinsons disease
All other patients aged 75 and over
Source: Department of Health
www.pulsetoday.co.uk 8 March 2013 Pulse
cover story
this month
promote early diagnosis to say we can help
patients plan for the future, but we dont
help them do that were just giving
someone a label of dementia and leaving
them to get on with it. Having a diagnostic
label of dementia without support is
probably worse than not having it at all.
Dr Eamonn Jessup is a GP in Prestatyn
in North Wales, an area often dubbed the
geriatric coast because of the number of
retired people, but which also has some
of the lowest rates of dementia diagnosis
in the country.
He has doubts about how case-finding
will work because of the grey area
between mild cognitive impairment and
Alzheimers disease.
He says: We have difficulty with
knowing the threshold for diagnosis at
the end of the day what can we actually
do for people with dementia? We can put
a good team around them to support the
family, but the medications are not great.
But not all GPs agree. Dr Ian
Greaves, a dementia GPSI in Gnosall,
Staffordshire, warns that late diagnosis
often leads to catastrophic consequences.
He says: People are admitted with an
acute presentation and diagnosis is
occurring in a hospital setting.
That leads to an extended hospital
stay and the only option then is for them
to go into a care home. It would make a
lot of sense if people got a diagnosis at
the appropriate time and had a care plan
that went in with them to the hospital.
According to Dr Greaves, there are
many positive examples of GP practices
providing better care for dementia
patients. He argues: I would like to see our
profession value [early diagnosis] because
of the value it offers patients, not just
because its put into the QOF or a DES.
Dr Nick Cartmell, a GP in Ashburton,
Devon, and clinical lead for dementia at
NHS Devon and the South West
Dementia Partnership, says: We should
not be pursuing early diagnosis purely
for the sake of increasing prevalence
figures, but rather ensuring timely
diagnosis for people who will benefit
from that diagnosis.
He suggests the DES should be
narrowed to cover screening solely of
those on QOF registers with a previous
stroke, TIA or ischaemic heart disease,
as they are more likely to have dementia.
He adds: The current emphasis on
increased prevalence should be matched
by an equal emphasis on the provision
of high-quality post-diagnosis services
across the UK, so we dont simply
diagnose more people only for them to
fall into a care vacuum.
Evidence base
The National Screening Committees
assessment for Alzheimers in June 2010
concluded there was not enough
evidence to warrant population
screening, although another review is
due to report this year.
There is also some evidence to support
the claim that patients commonly
experience anxiety and distress while
waiting for a definite diagnosis. A small
study published in the British Journal of
General Practice recently looked at the
experiences of 27 patients referred by
GPs to memory clinics in England, and
found they felt abandoned and ignored
while awaiting a diagnosis. The authors
recommended policymakers should act
cautiously before urging more rapid
diagnosis.
And Professor Steve Iliffe, professor of
primary care for older people at
University College London, says
unpublished data from his EVIDEM study
on GP dementia diagnosis suggests the
Government is exaggerating the potential
benefits of the DES (Expert view, page 7).
Memory clinics
Access to memory clinics is another
significant issue, with a report by MPs
last year finding waiting times of up to
a year.
CCGs are to be measured from April
on memory clinic waiting times, but it is
unlikely they will be given additional
funding and GPs fear these services will
be swamped.
Dr Lindsay Hadley, a GP in Bexhill on
Sea, East Sussex, has set up her own
primary care memory clinic after
becoming frustrated at delays in her area,
and says it has been overwhelmed.
She says: Where we are, about a third
have been diagnosed with dementia and
this DES is going to push it up to 70% or
80%. But there arent the services.
The answer is to develop primary care
memory services. It would be more
important to have a LES for helping with
diagnosing and looking after people with
dementia.
Recognising
dementia is a key
clinical session at
Pulse Live
Dr Patrick Brooke,
chief offcer at
Solihull Clinical
Commissioning
Group, will tell
you all you need
to know about the
new DES. Book
your place at
pulse-live.co.uk
How dementia diagnosis rates vary across the UK
45
%
40
%
Scotland
North East
North West
East Midlands
London
West Midlands
Northern
Ireland
Wales
South West
East of England
South Central
South East
Coastal
Yorkshire and
the Humber
64
%
50
%
49
%
49
%
45
%
43
%
39
%
41
%
44
%
40
%
63
%
Source: Alzheimers Society. Figures relate to
estimates of the proportion of true dementia
cases that have been diagnosed
Combined Abbreviated Prescribing Information: Asacol 400mg MR Tablet, Asacol
800mg MR Tablet, Asacol 250mg and 500mg Suppositories and Asacol Foam Enema
Presentation: Asacol 400mg MR Tablets, PL 10947/0011; each modifed release tablet contains
400mg mesalazine (5-aminosalicylic acid). Bottles of 120, 39.21. Bottles of 90, 29.41. Asacol
800mg MR Tablets, PL 10947/0012; each modifed release tablet contains 800mg mesalazine
(5-aminosalicylic acid). Bottles of 180, 117.62. Asacol 250mg Suppositories, PL 10947/0013,
each containing 250mg mesalazine. Packs of 20, 4.82. Asacol 500mg Suppositories, PL
10947/0014, each containing 500mg mesalazine. Packs of 10, 4.82. Asacol Foam Enema, PL
10947/0015, 1g mesalazine per metered dose. Carton containing can of 14 metered doses,
14 disposable applicators and 14 disposable plastic bags, 26.72 Indications: Ulcerative
colitis: Treatment of mild to moderate acute exacerbations. Maintenance of remission.
Suppositories particularly appropriate for distal disease, Foam Enema for distal colon disease
only. 400mg Tablets, 800mg Tablets, Suppositories: Maintenance of remission. 400mg
Tablets and 800mg Tablets only: Crohns ileo-colitis: Maintenance of remission. Dosage and
administration: ADULTS: 400mg Tablets: Acute disease: 6 tablets a day, in divided doses,
with concomitant corticosteroid therapy where clinically indicated. Maintenance therapy: 3 to
6 tablets a day, in divided doses. 800mg Tablets: Mild acute exacerbations: 3 tablets a day in
divided doses. Moderate acute exacerbations: 6 tablets a day in divided doses. Maintenance
of remission of ulcerative colitis and Crohns ileo-colitis: Up to 3 tablets a day, in divided doses.
Suppositories: 250mg: 3 to 6 a day, in divided doses, with the last dose at bedtime. 500mg: A
maximum of 3 a day, in divided doses, with the last dose at bedtime. Foam Enema: 1 (disease
of rectosigmoid region) or 2 (disease of descending colon) metered doses as single daily
dose for 4-6 weeks. ELDERLY: The normal adult dosage may be used unless renal function is
impaired. CHILDREN: 800mg Tablets: Not recommended. 400mg Tablets, Suppositories,
Foam Enema: No dosage recommendation. Contra-
indications: A history of sensitivity to salicylates or
renal sensitivity to sulfasalazine. Confrmed severe
renal impairment (GFR <20ml/min). 400mg Tablets,
Suppositories and Foam Enema only: Children under 2 years of age. 800mg Tablets only:
Hypersensitivity to any of the ingredients. Severe hepatic impairment. Gastric or duodenal
ulcer, haemorrhagic tendency. Precautions: Use in the elderly should be cautious and subject
to patients having a normal renal function. Asacol should be used with extreme caution in
patients with confrmed mild to moderate renal impairment. Renal function should be
monitored (with serum creatinine levels measured) prior to start of treatment, and periodically
during treatment, taking into account individual history & risk factors. Mesalazine should be
discontinued if renal function deteriorates. If dehydration develops, normal fuid & electrolyte
balance should be restored as soon as possible. Serious blood dyscrasias (some with fatal
outcome) have been very rarely reported with mesalazine. Haematological investigations
including a complete blood count may be performed prior to therapy initiation, during
therapy, and are required immediately if the patient develops unexplained bleeding, bruising,
purpura, anaemia, fever or sore throat. Stop treatment if suspicion or evidence of blood
dyscrasia. Concurrent use of other known nephrotoxic agents, e.g. NSAIDs & azathioprine,
may increase risk of renal reactions. 400mg Tablets and 800mg Tablets: Lactulose or similar
preparations which lower stool pH should not be concomitantly administered. 400mg tablets,
Suppositories, Foam Enema: Only use during pregnancy if benefts outweigh the risk. Avoid
during lactation unless essential. 800mg Tablets only: Mesalazine should be used with
caution during pregnancy and lactation when the potential beneft outweighs the possible
hazards in the opinion of the physician. If neonate develops suspected adverse reactions
consideration should be given to discontinuation of breast-feeding or discontinuation of
treatment of the mother. Discontinue treatment immediately if acute symptoms of intolerance
occur including vomiting, abdominal pain or rash. Patients with the rare hereditary problems
of galactose intolerance, the Lapp lactase defciency or glucose-galactose malabsorption
should not take this medicine because of the presence of lactose monohydrate. Standard
haematological indices (including the white cell count) should be monitored repeatedly
in patients taking azathioprine, especially at the beginning of such combination therapy,
whether or not mesalazine is prescribed. Undesirable Effects: Common: Nausea, diarrhoea,
abdominal pain, headache. Rare reports of leucopenia, neutropenia, agranulocytosis, aplastic
anaemia, thrombocytopenia, peripheral neuropathy, pancreatitis, abnormalities of hepatic
function and hepatitis, myocarditis, pericarditis, alopecia, lupus erythematosus-like reactions
and rash (inc. urticaria), drug fever, interstitial nephritis and nephrotic syndrome with oral
mesalazine treatment, usually reversible on withdrawal. Renal failure has been reported.
Suspect nephrotoxicity in patients developing renal dysfunction. Very rarely, mesalazine may
be associated with exacerbation of the symptoms of colitis, Stevens Johnson syndrome &
erythema multiforme. 400mg Tablets, Suppositories, Foam Enema: Rare reports of
allergic and fbrotic lung reactions. 800mg Tablets only: Common: vomiting, arthralgia
/ myalgia. Rare reports of vertigo, bronchospasm, eosinophilic pneumonia, bullous skin
reactions. Very rarely, interstitial pneumonitis. Suppositories, Foam Enema: Rarely, local
irritation may occur after use of rectal dosage forms of mesalazine. Legal category: POM.
Marketing Authorisation Holder: Warner Chilcott UK Ltd, Old Belfast Road, Millbrook,
Larne, County Antrim, BT40 2SH, UK. Asacol is a trademark. Refer to Summary of Product
Characteristics before prescribing. Date of preparation Feb 2012. AS8478a.
Adverse events should be reported. Reporting forms and information
can be found at www.mhra.gov.uk/yellowcard. Adverse events should also
be reported to Warner Chilcott UK Ltd on 0800 0328701
References:
1. Orchard T et al. Aliment Pharmacol Ther 2011; 33(9): 10281035.
2. Data on fle: UK/AS/0125/08-11b(1).
Date of preparation: December 2012
UK/AS/0175/12-12b
Help them back to normal, everyday life
When moderately active ulcerative colitis prevents your patients from getting on with their usual,
daily routine, give them Asacol 800mg MR tablets at 4.8g/day. With fast symptom improvement
(rectal bleeding and stool frequency) at 2 weeks
1,2
and symptom resolution (cessation of rectal
bleeding and normalisation of stool frequency) by week 6 in the majority of patients,
2
Asacol can
help you put your patients back where they belong.
Relieve, resolve and resume
(MESALAZINE)
ASA221 Pulse 290x230 AW.indd 1 19/12/2012 10:36
10 March 2013 Pulse www.pulsetoday.co.uk
This monTh
Your essential
round-up of all the
political, fnancial
and business news
relevant to your
practice. For full
stories and analysis
go to pulsetoday.co.
uk/news
Sainsburys to expand
in-store GP surgeries
Sainsburys is
planning an
expansion of the
primary care
services in its stores,
with a further seven
GP surgeries due to
open across the
country this year.
Premises will be offered rent-free and
will not be run or funded by Sainsburys.
Read the full story at pulsetoday.co.uk/
sainsburys
GPs press ministers
on health tourism
GPs should be able to charge overseas
visitors if there is any doubt over their
eligibility for healthcare in order to
prevent health tourism, LMC leaders
have urged ministers.
Bedfordshire and Hertfordshire LMC
has written to the Department of Health
and the Home Office to urge them to
tackle the difficulties faced by GP
practices, which have to treat visitors even
if think they may not be eligible for care.
In the letters, the LMC urged the
Government to ensure visitors entering
the country had their eligibility stamped
on their passport.
Read the full story at pulsetoday.co.uk/
health-tourism
DigesT
Quote of the month
This is about
the safety and
care of patients:
sort it out
Dr Paul Roblin on the lengthy and
obscure summaries used by the new
NHS 111 service
pulsetoday.co.uk/111-summaries
Doubts over online
access to records
Fewer than a third of doctors think giving
patients online access to their full
records is a good idea, a medical defence
body survey has found.
The poll of 850 members of the
Medical Protection Society and 1,766
members of the public also found 66% of
doctors and 73% of the public believe
particularly sensitive information should
never be accessible online.
A spokesperson for the MPS said the
survey showed the Governments plans to
give patients full access by 2015 should be
reconsidered, with some information
automatically redacted from records
unless patients requested it.
Read the full story at pulsetoday.co.uk/
records-access
GMC tightens rules on
self-prescribing
The number of doctors hauled in front of
the GMC for self-prescribing has trebled
in two years, according to figures
released by the regulator.
The GMC said the number of closed
fitness-to-practise cases featuring
allegations of self-prescribing, self-
treatment or informal treatment of family
and colleagues had increased from 36 in
2010 to 82 in 2011 and 98 in 2012.
The rise in cases was revealed as GMC
guidance on self-prescribing and
treatment of close family or friends was
tightened up. a
l
a
M
y
x
2
/
p
r
e
s
s
a
s
s
o
c
i
a
t
i
o
n
/
j
u
l
i
n
a
c
l
a
x
t
o
n
/
j
o
n
e
n
o
c
h
www.pulsetoday.co.uk Pulse March 2013 11
Locum cost reimbursement
Practices are set to be paid an average
of 1,500 to cover locum
superannuation costs from April,
regardless of whether they use locums
or not.
The BMA has criticised the
Governments plan for GP practices to
pay the superannuation themselves and
be reimbursed by the flat payment into
the global sum, warning GPs may find it
impossible to take on CCG work if
locum superannuation costs are not
fully covered.
GPC negotiator Dr David Bailey said:
It wont be based on use, it will be
based on patient numbers.
Read the full story at pulsetoday.co.uk/
locum-costs
Case-management DES
There is no evidence case management
can reduce unplanned hospital
admissions, casting doubt over one of
the Governments new DESs from April,
an analysis has concluded.
The meta-analysis of 11 trials
concluded case-management in older
people should not be promoted as
a mechanism for reducing unplanned
admissions.
Read the full story at pulsetoday.co.uk/
case-management
Sir David Nicholson
Campaigners have been calling for the
resignation of NHS chief executive
Sir David Nicholson in the wake of the
Mid Staffordshire scandal, because he
acted as interim chief executive of the
health authority that oversaw Stafford
hospital. But GP leaders have refused to
join the calls for him to quit. GPC chair
Dr Laurence Buckman said: I dont
think its useful to blame leaders.
Read more at pulsetoday.co.uk/leaders-
nicholson
Would-be GP troubleshooters
A CCG has asked GPs to help urgently
assess every patient on one hospitals
wards to see if they can be discharged,
in a bid to ease unusually high levels
of demand.
An email from Basildon and
Brentwood CCG interim chair Dr Anil
Chopra, sent to local GPs, said Basildon
Hospital had over the past few months
struggled to achieve even the minimum
waiting times in A&E and this has
worsened to crisis point over the past
couple of weeks.
Read the full story at pulsetoday.co.uk/
gp-troubleshooters
Home visits
Changes to dog laws will give greater
legal protection to doctors and
healthcare staff facing dangerous dogs
on private property.
Under proposals put forward by NHS
Protects legal protection unit, current
legislation on dog attacks in public
places will be extended to cover visiting
private residences.
The changes mean that dog-owning
patients will be held to account for the
behaviour of their pets if they cause
injuries on private property.
Read the full story at pulsetoday.co.uk/
dog-bites
Professor Clare Gerada
The RCGP chair has been voted one of
the 100 most powerful women in the
UK by Radio 4s Womans Hour. Other
prominent women who made the list
included Chief Medical Officer Dame
Sally Davies and the Queen.
Read the full story at pulsetoday.co.uk/
gerada-100
A bad month for... A good month for...
Digest
Talking point
of the month
What does the
Francis Inquiry
mean for GPs?
What did the Francis Inquiry fnd?
Robert Francis QCs damning report into
the failings at Mid Staffordshire NHS
Foundation Trust found appalling
standards of hospital care and made
290 recommendations for fundamental
change.
What did it recommend for GPs?
It said GPs should have an independent
monitoring role to ensure hospitals
provide high-quality care. It said the
failures in care at the hospital went
unnoticed because local GPs only
expressed substantive concern after they
were specifically asked by investigators.
What will this mean for GPs?
The Government has yet to issue
a formal response to the enquiry, but the
Prime Minister has already said GPs
must be more enquiring about hospital
care. Health secretary Jeremy Hunt has
also said he is considering plans for
a new chief inspector of primary care
to identify failing practices and
a revamp of CQC inspections.
Read the full story at pulsetoday.co.uk/
francis-inspector
Get the news
as it happens
Join the thousands
of GPs who get
all the key
developments
delivered directly
to their inbox via
the Pulse Daily
newsletter.
Register at
pulsetoday.co.uk/
emails
The latest guidance from the GMC,
Good practice in prescribing and managing
medicines and devices (2013), says GPs
must avoid prescribing for themselves
or anyone with whom they have a close
personal relationship.
Read the full story at pulsetoday.co.uk/
self-prescribing
GPs told 300k reft
needed for CQC
A GP practice has been told by NHS
managers its surgery must have
a 300,000 refurbishment in order to
prepare for CQC inspection.
The Monkspath Surgery in Solihull,
built in 1985, has been told it is non-
compliant with infection control rules
and must be completely refurbished.
The PCT said it was simply trying to
provide a safe environment for patients,
but the CQC has criticised the work as
unnecessary, and urged any practice
faced with PCT demands to refurbish
their premises to contact it.
Read the full story at pulsetoday.co.uk/
300k-refit
www.pulsetoday.co.uk 12 March 2013 Pulse
contract update
this month
When oa starts making every day a pain
BuTrans patches, for moderate OA pain, may help make everyday life more manageable again.
Prescribe your patients BuTrans patches for continuous pain relief from OA.
BuTrans patches contain an opioid analgesic.
Marketing Authorisation holder: Napp Pharmaceuticals Limited, Cambridge Science Park, Milton
Road, Cambridge, CB4 0GW, UK. Tel: 01223 424444. Member of the Napp Pharmaceuticals Group.
Prescribers should refer to the Summary of Product Characteristics before prescribing, particularly
in relation to side-effects, precautions and contra-indications. Further information is available
from Napp Pharmaceuticals Limited. For medical information enquiries, please contact
medicalinformationuk@napp.co.uk BuTrans and the NAPP device are Registered Trade Marks.
2011 - 2012 Napp Pharmaceuticals Limited. December 2012 UK/BUTR-12080 POM CD (Sch 3)
Adverse events should be reported. Reporting forms and information can be found
at www.mhra.gov.uk/yellowcard. Adverse events should also be reported to Napp
Pharmaceuticals Limited on 01223 424444.
BUTR-12080 Pulse third page ad final.indd 1 03/01/2013 15:39:12
How the changes will hit GPs
Follow all the
latest contract
developments
as they happen
pulsetoday.co.uk/
gpcontract
n
e
i
l
o
c
o
n
n
o
r
BMA fghts back on
contract imposition
The BMA has
fought back against
the Governments
planned imposition
of changes to the
GP contract in
England with a
31-page analysis
detailing how practices and patients will
be affected.
The official response to the
consultation published as Pulse went
to press included the results of a survey
of 8,000 GPs that found nearly 90%
believe they will be less able to provide
high-quality care as a result of the
Governments proposed contract deal for
2013/14. It also showed nearly two-thirds
of practices in England are planning to
make changes to current services
available to patients.
Overall, 30% said their practice would
have to reduce access for patients.
The BMAs analysis also said key
aspects of the contract proposal should
be delayed, including the plan to give
practices the job of paying locum
superannuation and the reduction in the
timeframe for QOF indicators from 15 to
12 months.
It argued the proposed changes work
against the thrust of the Francis Inquirys
recommendations by introducing
increasingly challenging targets for
box-ticking rather than core, holistic
patient care.
But the Department of Health was
quick to insist the changes would
focus time and money upon patient
care and have the potential to save
more lives.
Read the full story at pulsetoday.co.uk/
gpcontract
Main points of the
BMA submission
Changes to more equitable funding
between GMS and PMS practices should
not reduce the overall level of
investment and should be approved by
GPs through an opinion survey or
special conference
QOF exception-reporting guidance
should be revised, because rates are
likely to rise
Superannuation changes will have
a distorting effect on locums
The dementia DES is not supported by
evidence and contradicts NICE
There is great potential for unintended
negative consequences with plans for
making full patient records, including
test results, available online
The case-management DES will reduce
time available for routine patients
The changes will have a real impact
on recruitment and retention in general
practice
If the Government does impose the
proposals in their entirety with no
changes, do you expect your practice
to do anything differently?
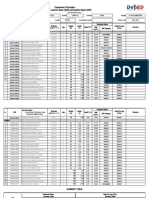
What will you do?
Source: BMA survey of 6,600 partners and salaried GPs
58%
Yes
42%
No/dont know
0 10 20 30 40 50
0 10 20 30 40 50
46% expect to make administrative staff redundant
42% do not expect their practice to do anything different
30% expect to reduce access for patients
30% will reduce the use of locums
25% will reduce CCG involvement
Where do you turn when a
sulphonylurea wont do?
ONGLYZA
TM
2.5MG & 5MG FILM-COATED TABLETS (saxagliptin)
PRESCRIBING INFORMATION. Consult Summary of Product Characteristics
before prescribing.
Presentation: 2.5mg or 5mg saxagliptin (as hydrochloride) flm-coated
tablets. Indications: Adults 18 and older: For Type 2 diabetes mellitus
patients to improve glycaemic control in combination with diet, exercise:
and metformin, when metformin alone, does not provide adequate glycaemic
control; and sulphonylurea, when sulphonylurea alone does not provide
adequate glycaemic control, where metformin is considered inappropriate;
and thiazolidinedione, when thiazolidinedione alone does not provide
adequate glycaemic control and thiazolidinedione is considered appropriate;
and in combination with insulin (with or without metformin), when this
regimen alone, with diet and exercise, does not provide adequate glycaemic
control Dosage: Adults: 5mg once daily as add-on therapy with or without
food at any time of the day. Use in combination with a sulphonylurea and
insulin, consider a lower dose of sulphonylurea or insulin to reduce the
risk of hypoglycaemia. Children and Adolescents: < 18 years old: Safety
and effcacy not yet established. Moderate Hepatic Impairment: Use with
caution. Severe Hepatic Impairment: Not recommended. Moderate & Severe
renal impairment: 2.5mg once daily, caution in patients with severe renal
impairment. Assessment of renal function is recommended prior to initiation
of Onglyza, and, in keeping with routine care, renal assessment should be
done periodically thereafter. End stage renal disease: Not recommended.
Elderly: 75 years: Use with caution. Contraindications: Hypersensitivity
to saxagliptin, any of the excipients or history of a serious hypersensitivity
reaction, including anaphylactic reaction, anaphylactic shock, and
angioedema, to any dipeptidyl peptidase 4 inhibitor. Warnings and
precautions: Not for the treatment of Type 1 diabetes mellitus or diabetic
ketoacidosis. Onglyza is not a substitute for insulin in insulin-requiring
patients. Inform patients of the characteristic symptom of acute
pancreatitis: persistent, severe abdominal pain. If suspected discontinue
use of Onglyza and other potentially suspect medicinal products. If a
serious hypersensitivity reaction to saxagliptin is suspected, discontinue
use, assess for other potential causes, and institute alternative treatment.
Not recommended in patients with rare hereditary galactose intolerance,
the Lapp lactase defciency or glucose-galactose malabsorption. Limited
experience in NYHA class I-II. No experience in cardiac failure (NYHA
class III-IV) or immunocompromised patients. In keeping with routine
care, monitoring for skin disorders is recommended. Drug interactions:
Clinical data suggest low risk for clinically meaningful interactions with
co-administered medicinal products. Caution with CYP3A4/5 inducers as
glycaemic effect may be lowered. Pregnancy and lactation: Avoid use unless
clearly necessary. Undesirable events: Common adverse reactions reported
across add-on trials: Upper respiratory infection; urinary tract infection;
gastroenteritis; sinusitis; headache; and vomiting. Add-on to metformin:
Nasopharyngitis (common) Add-on to sulphonylurea: Hypoglycaemia (very
common) Add-on to thiazolidinedione: Peripheral oedema (common).
Adverse reactions reported in at least two more patients treated with
Onglyza compared to control: Add-on to metformin: Common: Dyspepsia
and myalgia. Add-on to sulphonylurea: Uncommon: dyslipidaemia and
hypertriglyceridaemia. Adverse reactions reported in post-marketing
experience: Nausea (common); pancreatitis (uncommon); hypersensitivity
reactions (uncommon); anaphylactic reactions including anaphylactic
shock (rare); angioedema (rare) and rash (common). Key: Very common
( 1/10), common ( 1/100 to <1/10), uncommon ( 1/1,000 to <1/100)
and rare ( 1/10,000 to <1/1,000). Refer to SmPC for complete information
on side effects. Legal Category: POM. Marketing authorisation number:
EU/1/09/545/012 & EU/1/09/545/006. Presentation & basic NHS price:
Onglyza 2.5mg flm-coated tablets 28: 31.60; Onglyza 5mg flm-coated
tablets 28: 31.60. Further information is available from: Bristol-Myers
Squibb / AstraZeneca EEIG, Bristol-Myers Squibb House, Uxbridge Business
Park, Sanderson Road, Uxbridge, Middlesex, UB8 1DH, UK. [ONGLYZA] is a
trademark of the Bristol-Myers Squibb / AstraZeneca group of companies.
Date of PI preparation: 09 2012 Approval code: 422UK12PM139
CV 12 0143
References:
1. Gke B et al. Int J Clin Pract 2010; 64: 1691-1631
2. Onglyza Summary of Product Characteristics
Date of preparation: January 2013
422UK13PR00414 2348001
Adverse events should be reported. Reporting forms and
information can be found at www.mhra.gov.uk/yellowcard.
Adverse events should also be reported to Bristol-Myers
Squibb Pharmaceuticals Ltd. Medical Information on
0800 731 1736 or medical.information@bms.com
For your type 2 diabetes patients vulnerable to hypos, theres Onglyza
as an early add-on to metformin:
Less hypoglycaemia with comparable reduction
in HbA1c to a sulphonylurea at 1 year*
1
Onglyza 5 mg can be taken once a day,
at any time, with or without food. No need
for dose titration.
*Non-inferiority study comparing metformin and saxagliptin vs. metformin and glipizide
Onglyza 2.5 mg is suitable for patients with moderate or severe renal impairment. Caution in use with severe renal
impairment. Not recommended in ESRD requiring dialysis.
2
Nicorette Invisi Patch Prescribing Information:
Presentation: Transdermal delivery system available in 3 sizes (22.5, 13.5 and
9cm
2
) releasing 25mg, 15mg and 10mg of nicotine respectively over 16 hours.
Uses: Nicorette Invisi Patch relieves and/or prevents craving and nicotine
withdrawal symptoms associated with tobacco dependence. It is indicated
to aid smokers wishing to quit or reduce prior to quitting, to assist smokers
who are unwilling or unable to smoke, and as a safer alternative to smoking for
smokers and those around them. Nicorette Invisi Patch is indicated in pregnant
and lactating women making a quit attempt. If possible, Nicorette Invisi Patch
should be used in conjunction with a behavioural support programme. Dosage:
It is intended that the patch is worn through the waking hours (approximately
16 hours) being applied on waking and removed at bedtime. Smoking Cessation:
Adults (over 18 years of age): For best results, most smokers are recommended to
start on 25 mg / 16 hours patch (Step 1) and use one patch daily for 8 weeks. Gradual
weaning from the patch should then be initiated. One 15 mg/16 hours patch (Step
2) should be used daily for 2 weeks followed by one 10 mg/16 hours patch (Step 3)
daily for 2 weeks. Lighter smokers (i.e. those who smoke less than 10 cigarettes per
day) are recommended to start at Step 2 (15 mg) for 8 weeks and decrease the dose
to 10 mg for the fnal 4 weeks. Those who experience excessive side effects with the
25 mg patch (Step 1), which do not resolve within a few days, should change to a
15 mg patch (Step 2). This should be continued for the remainder of the 8 week
course, before stepping down to the 10 mg patch (Step 3) for 4 weeks. If symptoms
persist the advice of a healthcare professional should be sought. Adolescents
(12 to 18 years): Dose and method of use are as for adults however, recommended
treatment duration is 12 weeks. If longer treatment is required, advice from a
healthcare professional should be sought. Smoking Reduction/Pre-Quit: Smokers
are recommended to use the patch to prolong smoke-free intervals and with the
intention to reduce smoking as much as possible. Starting dose should follow the
smoking cessation instructions above i.e. 25mg (Step 1) is suitable for those who smoke
10 or more cigarettes per day and for lighter smokers are recommended to start at
Step 2 (15 mg). Smokers starting on 25mg patch should transfer to 15mg patch as soon
as cigarette consumption reduces to less than 10 cigarettes per day. A quit attempt
should be made as soon as the smoker feels ready. When making a quit attempt
smokers who have reduced to less than 10 cigarettes per day are recommended
to continue at Step 2 (15 mg) for 8 weeks and decrease the dose to 10 mg
(Step 3) for the fnal 4 weeks. Temporary Abstinence: Use a Nicorette Invisi Patch
in those situations when you cant or do not want to smoke for prolonged periods
(greater than 16 hours). For shorter periods then an alternative intermittent
dose form would be more suitable (e.g. Nicorette inhalator or gum). Smokers of
10 or more cigarettes per day are recommended to use 25mg patch and
lighter smokers are recommended to use 15mg patch. Contraindications:
Hypersensitivity. Precautions: Unstable cardiovascular disease, diabetes mellitus,
renal or hepatic impairment, phaeochromocytoma or uncontrolled hyperthyroidism,
generalised dermatological disorders. Angioedema and urticaria have been reported.
Erythema may occur. If severe or persistent, discontinue treatment. Stopping
smoking may alter the metabolism of certain drugs. Transferred dependence is
rare and less harmful and easier to break than smoking dependence. May enhance
the haemodynamic effects of, and pain response to, adenosine. Keep out of reach
and sight of children and dispose of with care. Pregnancy and lactation: Only
after consulting a healthcare professional. Side effects: Very common: itching.
Common: headache, dizziness, nausea, vomiting, GI discomfort; Erythema.
Uncommon: palpitations, urticaria. Very rare: reversible atrial fbrillation. See SPC
for further details. NHS Costs: 25mg packs of 7: (9.97); 25mg packs of 14:
(16.35); 15mg packs of 7: (9.97); 10mg packs of 7: (9.97). Legal category: GSL.
PL holder: McNeil Products Ltd, Roxborough Way, Maidenhead, Berkshire, SL6 3UG.
PL numbers: 15513/0161; 15513/0160; 15513/0159. Date of preparation:
Feb 2012.
10767_ocdnic_DPS_Pulse_290x460_fal1b.indd 1 15/02/2013 15:12
Discover A logical
combination to unlock
a smoke-free future
With sustained 16-hour background support
1
from NICORETTE
INVISIPATCH
and fast craving relief
2
from NICORETTE
QUICKMIST mouthspray, discover
an NRT combination that applies logic to the quitting needs of smokers.
The combination that appears to make most sense is patch plus
an acute delivery form
3
ASH Guidance
NICORETTE
INVISI 25mg PATCH
+
QuickMist Mouthspray
nicotine
Adverse events should be reported.
Reporting forms and information can be
found at www.mhra.gov.uk/yellowcard
Adverse events should also be reported to
McNeil Products Limited on 01344 864 042.
Nicorette QuickMist Prescribing Information:
Presentation: oromucosal spray containing 13.2ml solution. Each 0.07 ml
contains 1 mg nicotine, corresponding to 1 mg nicotine/spray dose. Uses: Relieves
and/or prevents craving and nicotine withdrawal symptoms associated with
tobacco dependence. It is indicated to aid smokers wishing to quit or reduce prior
to quitting, to assist smokers who are unwilling or unable to smoke, and as a safer
alternative to smoking for smokers and those around them. It is indicated in
pregnant and lactating women making a quit attempt. Dosage: Adults and
Children over 12 years of age: The patient should make every effort to stop
smoking completely during treatment with Nicorette QuickMist. One or two sprays
to be used when cigarettes normally would have been smoked or if cravings
emerge. If after the frst spray cravings are not controlled within a few minutes, a
second spray should be used. If 2 sprays are required, future doses may be
delivered as 2 consecutive sprays. Most smokers will require 1-2 sprays every
30 minutes to 1 hour. Up to 4 sprays per hour may be used; not exceeding 2 sprays
per dosing episode and 64 sprays in any 24-hour period. Nicorette QuickMist
should be used whenever the urge to smoke is felt or to prevent cravings in
situations where these are likely to occur. Smokers willing or able to stop smoking
immediately should initially replace all their cigarettes with the Nicorette QuickMist
and as soon as they are able, reduce the number of sprays used until they have
stopped completely. When making a quit attempt behavioural therapy, advice and
support will normally improve the success rate. Smokers aiming to reduce
cigarettes should use the Mouthspray, as needed, between smoking episodes to
prolong smoke-free intervals and with the intention to reduce smoking as much as
possible. Contraindications: Children under 12 years and Hypersensitivity.
Precautions: Unstable cardiovascular disease, diabetes mellitus, G.I disease,
uncontrolled hyperthyroidism, phaeochromocytoma, hepatic or renal impairment.
Stopping smoking may alter the metabolism of certain drugs. Transferred
dependence is rare and both less harmful and easier to break than smoking
dependence. May enhance the haemodynamic effects of, and pain response to,
adenosine. Keep out of reach and sight of children and dispose of with care.
Pregnancy & lactation: Only after consulting a healthcare professional. Side
effects: Very common: dysgeusia, headache, hiccups, nausea and vomiting
symptoms, dyspepsia, oral soft tissue pain and paraesthesia, stomatitis, salivary
hypersecretion, burning lips, dry mouth. Common: dizziness, paraesthesia,
palpitations, cough, aphthous stomatitis, gingival bleeding, toothache, pharyngeal
hypoaesthesia. Other: chest pain, atrial fbrillation, dyspnoea. See SPC for
further details. NHS Cost: 1 dispenser pack 11.48 2 dispenser pack 18.50.
Legal category: GSL. PL holder: McNeil Products Ltd, Roxborough Way,
Maidenhead, Berkshire, SL6 3UG. PL number: 15513/0357. Date of preparation:
Sept 2012.
References:
1. Nicorette
Invisi 25mg Patch Summary of Product Characteristics.
2. Nicorette
QuickMist Summary of Product Characteristics.
3. Guidance for health professionals on changes in the licensing
arrangements for nicotine replacement therapy. ASH, London. Dec 2005.
Date of preparation: February 2013 UK/NI/13-1241
10767_ocdnic_DPS_Pulse_290x460_fal1b.indd 2 15/02/2013 15:13
16 March 2013 Pulse www.pulsetoday.co.uk
This monTh
All the new
guidelines,
journal papers
and clinical policy
developments with
practice-changing
implications
Alert over stepping
down ICS in asthma
Patients with stable asthma who
stop taking low-dose inhaled steroids
more than double their risk of an
exacerbation over the following six
months, a meta-analysis has found.
The finding casts doubt on the BTS/
SIGN guideline recommendation to
consider a reduction in ICS dose every
three months in those with stable
asthma.
For every five patients with stable
asthma who stop taking inhaled steroids,
one will suffer an exacerbation as
a result, the study concluded. There was
also a mean decrease in FEV1 of 130ml
in those who gave up inhaled steroids.
The US researchers analysed data
from seven randomised controlled trials
involving 1,040 patients with stable
asthma. They found patients whose ICS
treatment was stopped were 2.3 times
more likely than those who continued on
ICS to suffer an exacerbation over the
following six months.
Professor Mike Thomas, chief medical
adviser for Asthma UK and a GP in
Minchinhampton, Gloucestershire, said:
Sometimes people are so well controlled,
they are tempted to stop treatment. Some
may be able to, but they need to be
informed about the risk of asthma
attacks and withdrawal of inhaled
steroids should be carefully monitored.
J Allergy Clin Immunol 2013, online 14 Jan
Measure BP in both
arms, GPs advised
Single blood pressure readings are not
accurate, a study has concluded.
Researchers who checked the BP in
both arms of 710 patients attending
a hypertension clinic at
University Hospital
Birmingham, and
then compared
the readings
with 24-hour
ambulatory
blood pressure,
found systolic
pressure in the arm
with the higher single
reading was on average 25.1 mmHg
higher than the ABPM, compared with s
c
i
e
n
c
e
p
h
o
t
o
l
i
b
r
a
r
y
/
a
l
a
n
h
a
r
r
i
s
CliniCal round-up
Guideline of the month
niCE: Fertility
Scope of the guideline
Infertility is estimated to affect one in
seven couples in the UK. The leading
causes are male factors (30%), ovulatory
disorders (25%), tubal damage (20%) and
unexplained infertility (25%). This
update of 2004 guidance covers
investigations and treatment options
once a diagnosis has been established.
Key points for GPs
A couple who have not conceived after
a year of unprotected intercourse should
be offered assessment and investigation.
Consider an early referral if the woman
is over 35 or if there is a known clinical
cause or predisposing factors.
GP initial assessment should include
semen analysis using the 2010 WHO
reference values if the first sample is
abnormal, repeat three months later.
A menstrual history should be taken
to assess ovulation possibly confirmed
with a mid-luteal progesterone.
Women with irregular cycles should
have FSH and LH measured.
Women aged under 40 should be
offered three full cycles of IVF funded by
the NHS and those aged 40-42 should be
offered one cycle.
Women with no known comorbidities
(such as pelvic inflammatory disease or
endometriosis) should be offered
hysterosalpingography (HSG) or
hysterosalpingo-contrast-sonography to
assess for tubal damage.
Expert comment
Dr Scott Wilkes, a GP in Amble,
Northumberland and associate editor of
the Journal of Family Planning and
Reproductive Health Care: The focus is
on the need to perform an initial
assessment to ensure efficient
management and appropriate referral.
But the prevalence of obesity is
increasing and with it ovulatory
dysfunction so GPs have a significant
role to play in weight reduction, which is
the first-line treatment for this cohort.
Practical issues
The recommendation to offer women
aged 4042 one cycle of IVF may be
difficult to implement in areas where
IVF is not offered to women over 40.
Open access to HSG is not widely
available.
The increased emphasis on weight loss
in both men and women to improve the
chances of ovulation and successful
treatment may prove challenging in
primary care.
The guidance excludes interventions
including ovulation prediction kits,
temperature charting and clomifene for
ovulation induction which couples
might have previously found useful.
The guideline
CG156. Fertility: assessment and
treatment for people with fertility
problems. NICE 2013.
Guideline debrief:
in our cpD module,
Guideline debrief:
fertility, Dr Wilkes
uses six case
histories to outline
the Gp implications
of the new nice
guidance.
2 CPD hourS
pulse-learning.
co.uk
For the full
guideline and GP
reaction go to
pulsetoday.co.uk/
NICE-fertility
www.pulsetoday.co.uk Pulse March 2013 17
a mean difference of 15.5mmHg between
the arm with the lower BP and the ABPM.
This reinforced the importance of NICE
advice to measure BP in both arms
and repeat this if the difference between
arms is more than 20mmHg, the
researchers said.
Dr Terry McCormack, a GP in Whitby
and member of the NICE guideline
development group for hypertension,
said: Unless you are using equipment
which simultaneously takes BP in both
arms, you need to do a series of tests to
be accurate.
BJGP 2013, online 28 Jan
New drug options for
urinary incontinence
Draft NICE guidelines for urinary
incontinence recommend a wider range
of antimuscarinic drugs for use first-line.
Women with overactive bladder
syndrome or mixed urinary incontinence
should be offered a choice of oxybutynin,
tolterodine or immediate-release
propiverine, according to the draft
released for consultation last month.
Current NICE guidance, from 2006,
recommends only oxybutynin first line,
with other antimuscarinics reserved for
women unable to tolerate oxybutynin.
Under the updated draft, extended-
release formulations of trospium,
oxybutynin and tolterodine may be
offered as second-line treatments, as well
as darifenacin.
Dr Julian Spinks, a GP in Rochester,
Kent, and member of the 2006 guideline
development group, said: The basic
outline of how to treat has not really
changed.
The overall thrust is still to start with
lifestyle modification, pelvic floor
training for urge incontinence and
management of overactive bladder with
bladder training.
pulsetoday.co.uk/urinary-incontinence
Beta-blocker benefts
reduced in AF
Patients with heart failure who also have
atrial fibrillation gain less benefit from
-blockers than those who are in sinus
rhythm, a meta-analysis has found.
The review of four trials of -blockers
in heart failure found patients with AF
had 14% lower mortality than those
taking placebo whereas -blocker use
was associated with 37% lower mortality
than placebo among patients in sinus
rhythm.
The UK and Dutch researchers
concluded that the effect of -blockers
is significantly different among heart
failure patients who also have AF.
But they did note that carvedilol had
a relatively favourable effect in the
analysis in AF patients in the one study
that examined it, although those patients
had milder disease than those in other
studies.
JACC Heart Failure 2013; 1: 21-8
GPs refer most cancer
after one or two visits
More than 80% of patients presenting to
their GP with symptomatic cancers are
referred after one or two visits, a new
study shows.
Data from more than 13,000 cancer
patients analysed by the National Audit
of Cancer Diagnosis in Primary Care
found 58% were referred on their first GP
visit and a further 25% on their second.
The researchers said encouraging GPs
to refer patients with non-specific
symptoms may improve the timeliness of
diagnosis but at the cost of more false
positives, patient anxiety and
overinvestigation.
B J Cancer 2013, online 7 Feb
Avoid injections in
tennis elbow
Corticosteroid injections should be
avoided in patients with tennis elbow as
they are associated with worse outcomes,
researchers warn.
The randomised trial compared
steroid injection, placebo injection and
either injection plus physiotherapy.
Those who received steroid injections
were 14% less likely to experience
complete recovery at a year than those
who had a placebo. Steroid injection was
also associated with a 77% higher risk of
recurrence than placebo. Physio had no
significant impact on either recovery or
recurrence rates at a year.
Dr Louise Warburton,
a musculoskeletal medicine GPSI in
Shrewsbury, said: Previous work showed
corticosteroids produce only short-term
benefits. Physio seemed better. Now with
a high recurrence rate from injections
and physio effects wearing off after
a year, we are left with a management
plan of short-term physiotherapy.
JAMA 2013, online 6 Feb
CliniCal round-up
Keep up to date
with clinical
news and CPD
Sign up for the
Pulse Daily email
newsletter to make
sure you dont miss
any of the big
developments from
the guidelines and
journals
pulsetoday.co.uk/
emails
Paper of the month
NICE traffc light system for
childhood fever misses infections
The study
In what is claimed to be the first major
validation study of the 2007 NICE
guidelines for assessing feverish illness
in children, Australian researchers
used the recommended traffic light
assessment tool in almost 16,000
children aged under five presenting to
a paediatric A&E.
The fndings
The NICE traffic light tool missed 20%
of UTIs, 14% of cases of bacteraemia
and 8% of pneumonia cases, all of
which were classified as green rather
than red or amber risk.
Combining the red and amber risk
categories, the NICE tool had
a sensitivity of 86% and a specificity of
29% for detection of serious bacterial
infection. The addition of routine
urinalysis would have improved
sensitivity to 92%.
What does it mean for GPs?
The researchers said the missed UTIs
were of greatest concern as occult
bacteraemia had become much rarer
in febrile children following the
introduction of pneumococcal
vaccination.
They suggested urine analysis should
be routinely performed in children with
fever and suspected bacterial infection,
pointing out that NICE recommended it
in children with fever without apparent
source yet did not include it in the
traffic light assessment tool.
However, they added that the low
specificity of the traffic light test meant
clinical judgment was still important to
avoid overinvestigation.
Expert comment
Dr Kathryn OBrien, clinical lecturer in
primary care at Cardiff University and
a GP in the city: Taking urine samples
from loads of children isnt really
feasible in general practice. Its difficult
to obtain urine samples from children.
Dipsticks have been found to be
unreliable for diagnosing UTI in young
children and are not recommended by
NICE for use in children under three
years old. So were not even sure that
the UTIs missed by the traffic light
system were actually UTIs.
The paper
BMJ, 2013; 346: f866
To read the full story and
Dr OBriens expert analysis, go to
pulsetoday.co.uk/NICE-traffc-lights
30 April 1 May
Birmingham
Book now for your
comprehensive
annual update on
all the latest clinical
developments
pulse-live.co.uk
www.pulsetoday.co.uk 18 March 2013 Pulse
investigation
this month
Four years ago it would have seemed
ludicrous to predict a shortage of GPs
to fill partnerships and salaried posts.
Deaneries were warning GPs to expect
unemployment after training, with
reports of 5080 applicants for every
full-time role in some areas. Pulse even
launched a One Voice campaign calling
for contractual changes and incentives to
make it easier for practices to take on
extra partners.
But fast-forward to 2013 and the
profession is facing a very different jobs
market. Many GPs are now complaining
of a dramatic reduction in the quality
and number of candidates for vacant
partnerships and of rising locum costs.
As practices struggle to cope with
rising expenses, below-inflation funding
awards and a huge shift in workload
from hospitals into primary care, they
are finding it harder to recruit GPs to
share the load.
Rising vacancies
A Pulse snapshot survey of 220 practices,
covering around 950 full-time positions,
reveals the full extent of the problem.
The results show an average vacancy
rate for all full-time-equivalent GP posts
in the practice of 7.9% in January 2013
almost double the 4.2% figure found in
a similar Pulse survey in January 2012,
which itself was twice the official figure
of 2.1% at the start of 2011.
Theres no doubt that, for practices
looking to take on GPs, the quadrupling
of the vacancy rate in just two years is
causing real problems. Dr Peter
Swinyard, chair of the Family Doctor
Association and a GP in Swindon, says:
It is immensely hard to recruit. This is
the experience of a lot of the doctors
I have talked to. We are on our second
firm of headhunters now, at significant
expense, to fill our vacancy.
Dr Anne Crampton, a GP partner in
Crowthorne, Berkshire, says there were
30 applicants when her practice
advertised a partner post three years ago,
but only five for a similar post this year.
She says: I dont know why general
practice seems to be so unpopular.
This difficulty in recruiting came as
a complete surprise.
Dr Malcolm Kendrick, a member of
the GPCs sessional executive committee
and a salaried GP in Cheshire, says there
has been an absolute turnaround from
the situation five years ago.
It is becoming more difficult to recruit
partners. There is definitely less appetite
for partner roles.
Recruitment is not such an issue in
Scotland, Dr Kendrick adds, but rural
practices in Wales are struggling to take
on partners.
GPC deputy chair Dr Richard Vautrey
says the problem has been a big concern
at the BMA contract roadshows:
Wherever we have been, GPs have been
telling us there is a recruitment and
retention crisis. It is starting to happen
now.
The recruitment crisis comes at
a particularly difficult time for practices,
with CCGs taking over commissioning
responsibilities and the new GP contract
hiking up practice workload from April.
The GPC argued in response to the
Governments contract imposition that
practices have reached a point of
workload saturation, while LMCs have
reported a shocking rise in requests for
pastoral care partly as a result of
excessive workload.
The difficulties practices are having in
Why has recruiting
gPs become so hard?
With the GP vacancy rate quadrupling in two years, practices are facing
a recruitment crisis just as they prepare to take on more work, fnds Jaimie Kaffash
General
practice is
looking less
attractive as
a career
Dr Peter
Swinyard
g
e
t
t
y
J
o
u
r
n
a
l
:
P
u
l
s
e
D
e
r
m
a
l
:
D
e
r
m
o
l
R
a
n
g
e
M
u
l
t
i
t
a
s
k
i
n
g
A
d
S
i
z
e
:
2
9
0
x
2
3
0
m
m
B
l
e
e
d
:
3
m
m
S
u
p
p
l
y
a
s
h
i
-
r
e
s
P
D
F
J
o
b
N
o
:
2
2
8
9
0
Like Jack,
Dermol can also
do two things
at once!
The Dermol family of antimicrobial
emollients - for patients of all ages who
suffer from dry and itchy skin conditions
such as atopic eczema/dermatitis.
Specially formulated to be effective and acceptable on sensitive eczema skin
Significant antimicrobial activity against MRSA and FRSA (fusidic acid-
resistant Staphylococcus aureus)
1
Over 15 million packs used by patients
2
A family of antimicrobial emollients
WASH SHOWER LOTION CREAM BATH
Dermol
Dermol
Wash, Dermol
200 Shower Emollient
and Dermol
500 Lotion Benzalkonium chloride
0.1%, chlorhexidine dihydrochloride 0.1%, liquid
paraffin 2.5%, isopropyl myristate 2.5%.
Dermol
Cream Benzalkonium chloride 0.1%,
chlorhexidine dihydrochloride 0.1%, liquid paraffin
10%, isopropyl myristate 10%.
Uses: Antimicrobial emollients for the management of dry and
pruritic skin conditions, especially eczema and dermatitis, and
for use as soap substitutes. Directions: Adults, children and the
elderly: Apply direct to the skin or use as soap substitutes.
Dermol
600 Bath Emollient Benzalkonium
chloride 0.5%, liquid paraffin 25%, isopropyl
myristate 25%.
Uses: Antimicrobial bath emollient for the management of dry,
scaly and/or pruritic skin conditions, especially eczema and
dermatitis. Directions: Adults, children and the elderly: Add to
a bath of warm water. Soak and pat dry.
Contra-indications, warnings, side-effects etc: Please refer
to SPC for full details before prescribing. Do not use if sensitive
to any of the ingredients. In the unlikely event of a reaction stop
treatment. Keep away from the eyes. Take care not to slip
in the bath or shower. Package quantities, NHS prices and
MA numbers: Dermol Wash: 200ml pump dispenser 3.55,
PL00173/0407. Dermol 200 Shower Emollient: 200ml shower
pack 3.55, PL00173/0156. Dermol 500 Lotion: 500ml pump
dispenser 6.04, PL00173/0051. Dermol Cream: 100g tube
2.86, 500g pump dispenser 6.63, PL00173/0171. Dermol
600 Bath Emollient: 600ml bottle 7.55, PL00173/0155.
Legal category: P MA holder: Dermal Laboratories, Tatmore
Place, Gosmore, Hitchin, Herts, SG4 7QR. Date of preparation:
February 2012. Dermol is a registered trademark.
Adverse events should be reported. Reporting
forms and information can be found at
www.mhra.gov.uk/yellowcard. Adverse events
should also be reported to Dermal.
References:
1. Gallagher J. et al. Poster presented at EADV Congress 2009.
2. Dermol Range Total Unit Sales since launch. Dermal
Laboratories Ltd. Data on file.
Dermol knocks out Staph
and soothes itchy eczema
www.dermal.co.uk
22890_Dermol Range Ad_Pulse_AW:1 20/12/12 09:49 Page 1
Because HPV is the last
thing on a girls mind
ABRIDGED PRESCRIBING INFORMATION
GARDASIL
(Human Papillomavirus Vaccine [Types 6, 11, 16, 18]
(Recombinant, adsorbed)).
Refer to Summary of Product Characteristics for full product information.
Presentation: Gardasil is supplied as a single dose pre-lled syringe
containing 0.5 millilitre of suspension. Each dose of the quadrivalent
vaccine contains highly puried virus-like particles (VLPs) of the major
capsid L1 protein of Human Papillomavirus (HPV). These are type 6
(20 g), type 11 (40 g), type 16 (40 g) and type 18 (20 g).
Indications: Gardasil is a vaccine for use from the age of 9 years
for the prevention of premalignant genital lesions (cervical, vulvar and
vaginal) and cervical cancer causally related to certain oncogenic Human
Papillomavirus (HPV) types and genital warts (condyloma acuminata)
causally related to specic HPV types. The indication is based on the
demonstration of efcacy of Gardasil in females 16 to 45 years of
age and in males 16 to 26 years of age and on the demonstration of
immunogenicity of Gardasil in 9- to 15-year old children and adolescents.
Dosage and administration: The primary vaccination series consists
of 3 separate 0.5 millilitre doses administered according to the following
schedule: 0, 2, 6 months. If an alternate schedule is necessary the second
dose should be administered at least one month after the rst and the
third dose at least three months after the second. All three doses should
be given within a 1 year period. The need for a booster dose has not
been established. The vaccine should be administered by intramuscular
injection. Contraindications: Hypersensitivity to any component of the
vaccine. Hypersensitivity after previous administration of Gardasil. Acute
severe febrile illness. Warnings and precautions: The decision to
vaccinate an individual should take into account the risk for previous HPV
exposure and potential benet from vaccination. As with all vaccines,
appropriate medical treatment should always be available in case of
rare anaphylactic reactions. The vaccine should be given with caution to
individuals with thrombocytopaenia or any coagulation disorder because
bleeding may occur following an intramuscular administration in these
individuals. Syncope, sometimes associated with falling, can occur before
or after vaccination with Gardasil as a psychogenic response to the needle
injection. Vaccinees should be observed for approximately 15 minutes
after vaccination; procedures should be in place to avoid injury from faints.
There is insufcient data to recommend use of Gardasil during pregnancy
therefore the vaccination should be postponed until after completion
of the pregnancy. The vaccine can be given to breastfeeding women.
Gardasil will only protect against diseases that are caused by HPV types
6, 11, 16 and 18 and to some limited extent against diseases caused
by certain related HPV types. Vaccination is not a substitute for routine
cervical screening. Individuals with impaired immune responsiveness,
due to either the use of potent immunosuppressive therapy, a genetic
defect, or other causes, may not respond to the vaccine. As with any
vaccine, vaccination with Gardasil may not result in protection in all
vaccine recipients. There are no safety, immunogenicity or efcacy
data to support interchangeability of Gardasil with other HPV vaccines.
Undesirable effects: Very common side effects include: headache
and at the injection site, erythema, pain and swelling. Common side
effects include bruising and pruritus at the injection site, pyrexia, nausea,
and pain in the extremity. Rarely urticaria and very rarely bronchospasm
has been reported. Idiopathic thrombocytopenic purpura, Guillain-Barr
Syndrome and hypersensitivity reactions including, anaphylactic/
anaphylactoid reactions have also been reported. For a complete list of
undesirable effects please refer to the Summary of Product Characteristics.
Package quantities and basic NHS cost: Single pack containing
one 0.5 millilitre dose pre-lled syringe with two separate needles.
NHS cost: 86.50 per dose. Marketing authorisation holder:
Sano Pasteur MSD SNC, 8 rue Jonas Salk, F-69007, Lyon, France
Marketing authorisation number: EU/1/06/357/007 (pre-lled
syringe with two separate needles) Legal category: POM
Registered
trademark Date of last review: Nov 2012
Adverse events should be reported. Reporting forms and information can be found at
www.mhra.gov.uk/yellowcard Adverse events should also be reported to Sano Pasteur MSD,
telephone number 01628 785291.
Reference: 1. Department of Health, Third Annual Report on HPV coverage. http://immunisation.dh.gov.uk/annual-hpv-
vaccine-coverage-in-england-in-201011-report/ Date accessed January 2013.
FIND THEM. REMIND THEM. HELP TO PROTECT THEM.
P
R
O
T
E
C
T
I
O
N
A
G
A
I
N
S
T
H
P
V
R
E
L
A
T
E
D
D
I
S
E
A
S
E
S
In 2010/11 over 10% of eligible girls did not start their course of HPV vaccination
to help protect against cervical cancer
1
Gardasil is available at no cost for GP practices through Movianto UK Ltd for
unvaccinated girls aged 1217
UK16362 a 02/13
BC_1548_SPMSD_UK16362 a_Gardasil GP ad update_Jan 2013_Pulse_V1_FINAL.indd 1 15/02/2013 14:27
www.pulsetoday.co.uk Pulse March 2013 21
investigation
this month
filling vacancies are also having
a financial impact. In the Pulse survey,
practices reported an average increase
in locum costs of 9.5% over the past
12 months, on top of the further
9% increase seen in 2011.
Portfolio careers
So why are so few GPs applying for
jobs? Official figures from the NHS
Information Centre show there was
a slight fall in the number of GP partners
in 2011 27,218 compared to 2001, when
there were 27,938. By contrast, the
number of consultants rose sharply from
27,782 in 2001 to 39,088 in 2011.
However, the total number of practising
GPs has increased by an average of 2.3%
annually since 2001, from 31,835 to
39,780. In other words, fewer GPs are
taking the route into partnership, instead
remaining salaried or locums. However,
unlike in 2009, when competition for
partnership vacancies was fierce, this
now seems to be through choice.
A shift towards portfolio careers and
a steadily rising number of women
choosing to work part time are both
having an impact, GPs say.
Dr Crampton says: Nobody wants
to work full time. Initially, we wanted
a nine-session partner.
What most GPs seem to want to do
now is part-time general practice and
part-time GPSI work clinical assistants,
out-of-hours work, that type of thing.
Dr Kendrick agrees partnerships are
widely seen as unattractive: There is
a lot of uncertainty about the contract
imposition, falling income and people
seeing partners working ridiculous
hours.
GPs doing other roles are now
saying: This does not look like such
an attractive option.
At the other end of the scale, GPs are
increasingly considering early retirement
as the demands of the job pile up. Exactly
half of the respondents to Pulses survey
said they were thinking of retiring early.
Many cited workload as a key reason for
considering early retirement.
Dr Swinyard says: Were seeing more
and more principals saying: Sod this, Im
going early. Some take roles working as
locums for the last few years of their
practice lives. Its a shame to lose the
wisdom of senior people you cannot
replace that.
Looking to the future
The Department of Health has recognised
that more GPs are needed for the NHS to
function, with former health secretary
Andrew Lansley last year setting out
a plan to boost the number of GP trainees
by 20% by 2015 in England so that GP
registrars would make up 50% of the
specialty training places (up from 41%).
But this drive is floundering. Figures
from the GP National Recruitment Office
(GPNRO) last summer showed there
were 2,693 GP training places accepted
in England in 2012, which actually
represented a net decrease of three
compared with the previous year.
This compares with a rise of almost
700 in hospital training places in
England, with 4,725 places accepted,
up from 4,034 in 2011. The proportion of
GP trainees fell from 40% in 2011 to 36%
in 2012.
A DH spokesman says: The DH and
Health Education England are currently
working with key stakeholders to support
the increase of training numbers in
general practice.
A national GP taskforce has been
established to support this work and
make recommendations for increasing
training posts to 3,250 each year.
An unattractive proposition
According to the Committee of General
Practice Education Directors, the
struggle to recruit new GPs is down to an
excess of hospital training places, rather
than a dearth of GP ones. Chair Dr Barry
Lewis, a GP in Rochdale, says: We have
expanded training steadily and have an
expansion target for the next three years
there is no shortage of training places.
We have empty slots in programmes,
except in London and the South East.
There are not enough applicants
because an excess of hospital specialty
posts is still in the system.
There is a significant imbalance in
the workforce at junior level that has
and continues to produce too many
-ologists and too few generalists,
especially GPs.
Research published last month
showed that only 28% of medical
graduates cite general practice as their
first-choice career, compared with 71%
who opt for secondary-care specialties.
Study leader Professor Michael
Goldacre, a professor of public health at
the University of Oxford, says there is
some cause for concern about this
relative lack of interest in general
practice from newly qualified doctors.
He says: A much smaller percentage
express a preference for a career in
general practice than the NHS actually
needs.
Rising medical school fees and the
proposed four-year training for GPs,
which could begin as soon as 2014, are
also likely to have an effect on the
numbers entering the profession.
The reluctance of many medical
graduates to opt for general practice is
not new. However, the Government is
doing a poor job of encouraging people
into the profession, says Dr Vautrey.
There is a feeling there are better
opportunities for them in hospital or
abroad, he says.
Dr Swinyard still looking to fill his
practices outstanding vacancy says
more must be done to encourage the next
generation into the profession.
General practice as a whole is looking
less attractive as a long-term career
option, he says. I still think this is the
best job in the world, but it is becoming
bloody hard to do it.
Editorial: A profession fast losing its
appeal, page 29
It has become an arms
race to get an applicant
I have found it diffcult to fll vacancies
recently. The quality of applicants and
the number has defnitely fallen.
It had been declining for a while but
it dropped dramatically in the past year.
It is a sellers market. There have
been instances where applicants have
been offered another job at the same
time elsewhere and it has become an
arms race to get that applicant in the
post by offering as attractive
a proposition as possible.
There are more people taking up
locum posts and working out of hours
in APMS providers than previously.
I dont think people want to be tied
into long-term contracts.
I think it will get worse if you want to
recruit a partner when no one knows
what is happening in three years time,
let alone fve.
Dr Richard van Mellaerts is a GP in
Kingston, Surrey
How GP vacancy rates have risen
GPs are in
a recruitment
crisis
Watch the Big
Interview with
Dr Bill Irish, chair
of the GP National
Recruitment Offce
pulsetoday.co.uk/
tbi-irish
Source: Pulse surveys and the NHS Information Centre
2.1%
2011
4.2%
2012
7.9%
2013
www.pulsetoday.co.uk 22 March 2013 Pulse
investigation
this month
In the waxing and waning fortunes of
PMS GPs, 2013 may come to be seen as
a watershed. Over the past two years,
a Pulse investigation reveals, half of such
practices have had their contracts
reviewed by managers, in the biggest
reappraisal of their funding since the
alternative GP contract was introduced.
Some report losing tens of thousands
of pounds in funding, sending GP
drawings plummeting and putting staff
at risk of redundancy. Others have gained
from the review. But most agree the
overarching purpose of the PMS contract
to provide local services has been
dumbed down by managers seeking
easy efficiency savings.
Some practices have reverted to the
GMS contract, a few have closed, but
many have had to come to terms with
new contract terms and the uncertainty
looks set to continue as the NHS
Commissioning Board begins a root-and-
branch overhaul of practice funding
from 2014.
Two-tier funding
Established as a pilot scheme in the 1997
Act for Primary Care, PMS was the first
opportunity for GPs in England to
negotiate their own contracts locally
with PCTs, based on the health needs of
their local population.
Over time, PMS contracts became
Dr Derek Hopper
explains how PMS
GPs in his area
secured their deal
pulsetoday.co.uk/
pms-negs
We are paid less than our salaried GP
We switched to a PMS contract in 2001
and our original objectives closely
matched Lambeths health needs at
that time. But last year, we were called
to a meeting.
We were given a presentation and at
the end of the meeting we were given
an envelope telling us how much we
were going to lose.
Ours was 179,000. It was a huge
chunk of our funding.
The funds cut were spent on clinical
staff and now we and our patient
access and services are hurting. We are
the second-largest practice in our
borough, with some of the highest
needs in the UK.
We have extremely high
consultation rates due to the high
disease prevalence rates, particularly
mental health issues.
We are still providing these services,
but we are having to fund it with
different methods. The clinical need
doesnt go away just because the
money goes away.
We [the partners] are now being
paid less than our salaried GP, and I
know that is not unusual because I am
part of a peer support group and it is
the same across the board.
We didnt cut the nurses pay. These
two outreach nurses were paid for by
the PMS funding, which then
disappeared. They were doing work
with frail, elderly people with long-
term conditions, just the services that
are needed now that more hospital
work is shifting to be carried out in the
community.
We are having another pay cut this
month it is going to be a reduction of
around 40%.
We do good things, but we now
have our arms tied behind our backs.
Dr Di Aitken is a GP in Lambeth, south
London
In a statement issued to Pulse, NHS
Lambeth said: Our review has given us
the opportunity to refocus and better
incentivise the provision of primary
care contracts to be more closely
aligned towards our priority health
goals which seek to address the
highest health needs in Lambeth, as
prioritised by local people and health
professionals.
One PMS practice in three has had
its contract changed in the past
two years and many are switching
back to GMS. Does PMS have
a future? Sofa Lind investigates
Pms
practices
squeezed
as funding
reviews
bite
j
O
e
d
M
I
L
e
S
Methylprednisolone BP 4%
50
+
years and still going strong
Prescribing Information
Depo-Medrone: Methylprednisolone acetate 40 mg/ml;
Depo-Medrone with Lidocaine: Methylprednisolone acetate
40 mg/ml, lidocaine hydrochloride 10 mg/ml. Please refer to the
SPC before prescribing Depo-Medrone or Depo-Medrone with
Lidocaine. Presentation: Injectable sterile aqueous suspension.
Indications: Depo-Medrone: Corticosteroid responsive conditions;
rheumatoid arthritis, SLE, Stevens-Johnson syndrome, asthma,
severe seasonal rhinitis, ulcerative colitis, Crohns disease,
osteoarthritis. Depo-Medrone with Lidocaine: Local anti-
infammatory or anti-rheumatic use where additional anaesthesia
is advantageous. Dosage and administration: Depo-Medrone:
Intramuscular, intralesional, intra-articular, periarticular, intrabursal
routes and into the tendon sheath. Dosage Range: 0.13 ml
(4120 mg). Dosing regimen depends on individual approved
indications. For full details on dosing and administration please
see Summary of Product Characteristics. Depo-Medrone with
Lidocaine: Intra-articular, periarticular, intrabursal routes and
into the tendon sheath. Dosage Range: 0.12 ml (480 mg).
Dosing regimen depends on individual approved indications. For
full details on dosing and administration please see Summary of
Product Characteristics. All aseptic precautions should be taken
and infected areas avoided. Elderly Patients: As adult dose.
Children: Dosage should be reduced for infants and children.
Contra-Indications, warnings, etc: Hypersensitivity to the
components and in the presence of systemic infections unless
specifc anti-infective therapy is employed. Neither product
should be given by the intrathecal or intravenous routes. For single
dose use only. Do not mix with other fuids. Rarely depigmentation
and skin depression occur at the injection site. Do not inject into
Achilles tendon. Intra-articular injection produces increased risk of
infammatory response in the joint. Systemic absorption from this
route can produce systemic and local effects. Some hypothalamic-
pituitary-adrenal axis suppression occurs, possibility of increased
suppression with multiple dosing. Patients should carry a Steroid
Treatment card, which gives clear guidance on the precautions
to be taken to minimise risk and which gives details of prescriber,
drug, dosage and the duration of treatment. For Depo-Medrone
only: Avoid superfcial or subcutaneous placement of intramuscular
injections. For Depo-Medrone with Lidocaine only: No
additional beneft derives from the intramuscular administration.
Use in pregnancy and lactation: Inadequate safety evidence,
balance clinical beneft against possible risk. Corticosteroids
are excreted in breast milk. Use in children: Corticosteroids can
cause growth retardation. Side-effects: Known corticosteroid
effects may be observed. Some of the serious side effects that
may occur include: Anaphylactic reaction, peptic ulceration with
perforation and haemorrhage, acute pancreatitis, congestive heart
failure, hypertension, psychiatric reactions (e.g. suicidal thoughts)
and psychotic reactions (e.g. mania, delusions). For full details on
all other side effects please see SPC Package quantities: 1, 2
and 3 ml vials. Depo-Medrone with Lidocaine: 1 ml and 2 ml
vials only. Basic NHS cost: Depo-Medrone Injection 1 ml 3.44.
Depo-Medrone Injection 1 ml x 10 34.04. Depo-Medrone
Injection 2 ml 6.18. Depo-Medrone Injection 2 ml x 10 61.39.
Depo-Medrone Injection 3 ml 8.96. Depo-Medrone 3 ml x 10
88.81. Depo-Medrone + Lidocaine Injection 1 ml 3.94.
Depo-Medrone + Lidocaine Injection 1 ml x 10 38.88.
Depo-Medrone + Lidocaine Injection 2 ml 7.06. Depo-Medrone +
Lidocaine Injection 2 ml x 10 70.13. Product licence numbers:
Depo-Medrone: PL 00032/5038R. Depo-Medrone with
Lidocaine: PL 00057/0964. Marketing authorization
holder: Depo-Medrone: Pharmacia Limited, Ramsgate Road,
Sandwich, Kent CT13 9NJ, UK. Depo-Medrone with
Lidocaine: Pfzer Limited, Ramsgate Road, Sandwich, Kent
CT13 9NJ, UK. Legal Category: POM. Further information
is available on request from: Medical Information at
Pfzer Limited, Walton Oaks, Dorking Road, Tadworth, Surrey,
KT20 7NS, UK. Tel: +44 (0) 1304 616161. Date of preparation:
March 2012. Ref: DM + DM+L 4_5 UK
Adverse events should be reported.
Reporting forms and information can be found at
www.mhra.gov.uk/yellowcard.
Adverse events should also be reported to
Pfzer Medical Information on 01304 616161
w
w
w
.
d
e
p
o
m
e
d
r
o
n
e
.
c
o
.
u
k
Date of preparation: April 2012 UK/MED/12/0006
www.pulsetoday.co.uk 24 March 2013 Pulse
investigation
this month
M
P
3
5
8
Still the only preservative-free single unit dose
eye drops for the relief of allergy symtoms
Available on prescription
www.moorfeldspharmaceuticals.co.uk
+44 (0)20 7684 9090 (option 1)
Adverse events should be reported. Reporting forms and
information can be found at www.yellowcard.gov.uk/
Adverse events should also be reported to Moorfelds
Pharmaceuticals on 020 7684 9090 (option 1).
CATACROM
Product Information: Catacrom
Sodi um Cromogl i cate 2% w/v
Eye Drops BP wi thout preser vati ve (uni t dose) MA Holder: Moorfi el ds Eye
Hospi tal NHS Foundati on Trust, tradi ng as Moorfi el ds Pharmaceuti cal s, 34 Ni l e
Street, London, N1 7TP. Legal Category: P. Indication: Rel i ef and treatment of
al l ergi c, red, water y, i tchy and puffy eyes caused by hayfever, house mi tes, and
other causes of al l ergy such as pet hai rs. Contra-indications: Hypersensi ti vi ty
to Sodi um Cromogl i cate. If i rri tati on or sti ngi ng persi sts or worsens, di sconti nue
treatment and consul t a physi ci an. Precautions: Cauti on i f admi ni stered to
pregnant, or anyone pl anni ng to become pregnant or breast- feedi ng pati ents.
If changes occur to your vi si on, do not dri ve or operate machi ner y unti l vi si on i s
cl ear. Side effects: Irri tati on, mi l d sti ngi ng and bl urred vi si on may occur after
i nstal l ati on. Pl ease consul t the SPC for further i nformati on.
Relief and treatment of seasonal and perennial allergic conjunctivitis
Prevents allergic symptoms such as redness, watering, itching and puff ness
Pulse Quarter page ad 145x109.5 AW.indd 1 11/02/2013 10:35
very popular with a third of GPs
practising under one by 2002 providing
a wider range of primary care services.
But the PMS revolution also drove
a wedge between GPs, with fears of
a two-tiered profession developing as
PMS practices commanded higher
funding per head than many GMS GPs
could ever have dreamt of.
Those rising earnings also caught the
eye of the national media, which decried
drawings of up to 150,000 a year.
The backlash began in 2006. The
Government sent out a notice to all PCT
chief executives in England saying they
must conduct a value for money review
of all PMS contracts, ensuring they were
equitable and fair in relation to GMS.
A further blow followed in 2010, when
the DH added a clause to PMS
regulations giving PCTs the right to
terminate contracts without grounds.
The NAPC warned that PMS GPs faced
unilateral variation to PMS contracts
rather than genuine negotiations. In
some cases, those fears have been
realised.
Hypocrisy
Six months ago Dr Tom Frewin, a
single-handed GP in Bristol, was subject
to a PCT-wide review of PMS contracts
that resulted in his practice losing about
67,000 a year. Dr Frewin has taken a big
hit to his pay rather than reduce the
services he provides, but he warns that
this is not sustainable over the long
term.
He says: For a single hander that is
a lot. It was a PCT-wide review of the
outliers only. If you just looked at
capitation, I might have been 5% over the
average. But weighted capitation changes
this. With weighted capitation it is fine if
you go across a large group, but when
you pick out individuals you get some
bizarre results.
He says redistributing funds is not
always wrong or unfair, but says he feels
he was not listened to by NHS managers.
There were no negotiations. They said
they would negotiate and there were a lot
of meetings, but what a complete waste
of time that was. It is an entire hypocrisy.
In a statement to Pulse, a spokesperson
for NHS Bristol insisted it had followed
an extremely robust process in
renegotiating PMS contracts.
But Dr Frewin is not alone in feeling
hard done by. Dr Di Aitkens practice in
Lambeth, south London, lost 179,000 of
its annual funding, leaving the partners
on lower pay than their salaried GP (case
study, page 22).
In fact, Pulse can reveal that in the past
two years, over half (55%) of PMS
contracts have been subject to review.
The data obtained under the
Freedom of Information Act covers
1,278 PMS contracts held by PCTs on
1 April 2011. More than a third of
practices (37%) have seen their contract
terms varied as a result of review, while
4% have had their contracts terminated,
resulting in practice closure, merger or
in most cases reversion to a GMS
contract. In total, 30 of the 1,278 practices
reverted to GMS.
In some areas, the changes to PMS
contracts have been dramatic. NHS
Derby City has retained just two of the 16
PMS contracts it held two years ago after
14 practices decided to revert to GMS.
A spokesperson said the reviews were an
opportunity for the PCT to standardise
and simplify primary care contracts and
that practices now had the additional
security of a GMS contract.
But such changes have led to the first
reduction in the number of PMS GPs
since the introduction of the new
contract. Figures from the NHS
Information Centre show that in 2011,
the most recent year for which figures
are available, 44.4% of GPs worked in
PMS practices the lowest proportion
since 2005.
Dumbed down
Not all reviews end in cuts, however.
Dr James Kingsland, national
clinical lead of the NHS Clinical
The rise and fall of PMS
1998 Pilots of PMS contracts begin with
83 practices in England
2003 The DH announces that it will end the
PMS pilot and give the contract
permanent status
2004 The new GMS contract comes into
force and PMS contracts are
established
2006 DH directs PCTs to carry out
value for money reviews of all
PMS contracts
2010 DH adds clause to PMS regulations
giving PCTs the right to terminate
contracts without grounds
2011 A group of 20 PMS practices lose
their High Court case against PCTs,
with the court upholding trusts
right to unilaterally cancel PMS
contracts so long as they give six
months notice
march 2012 Workforce fgures show a fall in the
number of PMS GPs after six years of
consecutive rises
october 2013 DH announces plans for more
equitable funding for all practices
For a single
hander,
67,000
is a lot
Dr Tom
Frewin
Prescribing information can be found on the adjacent page
References:
1. Reitamo S and Allsopp R. J Dermatol Treat 2010; 21: 3444.
2. Protopic 0.1% Summary of Product Characteristics, August 2012.
3. Protopic 0.03% Summary of Product Characteristics, August 2012.
Adult patients with moderate-to-severe atopic dermatitis (AD) treated proactively
twice-weekly with 0.1% Protopic were free from major fare for a median of 142 days,
compared with 15 days for those receiving Protopic fare treatment alone
1,2*
PRO12106UK December 2012
142 days
without a major eczema flare?
Thats a whole British summer.
Exposure of the skin to sunlight should be minimised and patients advised on appropriate sun protection methods, such
as minimisation of the time in the sun, use of a sunscreen product and covering of the skin with appropriate clothing
2,3
*
Protopic is for use in patients with moderate-to-severe AD who have failed to adequately respond to
2,3
or are intolerant of conventional therapies, such as topical corticosteroids
2
PRO073_Protopic_Pulse advert_236 x 296_V1.indd 1 18/12/2012 09:14
www.pulsetoday.co.uk 26 March 2013 Pulse
INVESTIGATION
THIS MONTH
Commissioning Community and a PMS
GP in Wallasey, Merseyside, says his PCT
has just topped up his practice funding
by 4,000 for carrying out additional
vaccinations. But, while he says his
contract has been managed well, he has
heard from colleagues that not all PCTs
have been as understanding.
My practice was one of the first-wave
PMS sites in the country. We were
pioneers, very enthusiastic, but over time
[PMS] has been dumbed down, without
the real flexibility it had when we first
started. It is a shame. There are PCTs that
just dont understand the nature of PMS
contracts and just look at basic
information like costs-per-patient
baseline and say: There is a difference
and therefore we want our money back
which is an incredibly rudimentary
process.
NAPC chair Dr Charles Alessi also says
many of the reviews have started with
a misconception that PMS is better
remunerated: Of course we all have to
change what we are doing. We are all in
the same situation at the moment, in
terms of the fiscal environment. But what
is important is that we do [this] in a way
that is ordered well, and that we are not
just making assumptions and proceeding
on those assumptions.
GPC deputy chair Dr Richard Vautrey
says that reviews of contracts by PCTs
over recent years have been destabilising
for PMS practices, particularly when
done for financial reasons.
He says: There have been a lot of
reviews, and quite vigorous reviews
taking place, some inappropriate.
An uncertain future
Pressure on PMS funding is not likely to
ease any time soon, although practices
may see a more consistent application of
the reviews from April.
Starting next year, PMS-funded
practices are facing a contract overhaul
that will last for seven years. The
Government claims this will result in
a more equitable funding structure for
GPs that bases GMS and PMS funding
around the same principles. The NAPC
has said a further round of changes is
causing increasing anxiety among GPs,
but Dr Alessi says he has been
encouraged by recent discussions with
the NHS Commissioning Board.
He says: As of April, renegotiations
are going to be conducted with rigour.
There is going to be a single process and
that is encouraging, because that is what
we have been asking for. We will also be
intimately involved in the detail of that
process.
The GPC has also cautiously welcomed
the move. Dr Vautrey says: I think
moving to one arrangement, one process,
led by the board should be helpful as
long as it is done in a measured and
understanding way.
[PCT] reviews are very variable,
approached in different ways. Practices
want stability. They want to be treated
fairly.
Over time, PMS has
been dumbed down,
without the real
exibility it had when
we rst started
Dr James Kingsland
As of April, PMS
renegotiations
will be conducted
with rigour
Dr Charles Alessi
J
O
N
E
N
O
C
H
/
P
A
U
L
S
T
U
A
R
T
Adverse events should be reported. Reporting forms and information can be found at
www.mhra.gov.uk/yellowcard Adverse events should also be reported to Astellas Pharma Ltd.
Please contact 0800 783 5018.
PRESCRIBING INFORMATION
PRO12106UK December 2012
PRESCRIBING INFORMATION: Protopic
0.03%
ointment (tacrolimus monohydrate) Protopic
0.1% ointment
(tacrolimus monohydrate) ACTIVE INGREDIENT Protopic
0.03% ointment (1g) contains 0.3mg of tacrolimus as
tacrolimus monohydrate (0.03%). Protopic
0.1% ointment
(1g) contains 1.0mg of tacrolimus as tacrolimus monohydrate
(0.1%). THERAPEUTIC INDICATIONS Protopic
0.03%:
- treatment of moderate to severe atopic dermatitis in children
(2 years of age and above) who failed to respond adequately
to conventional therapies such as topical corticosteroids. -
treatment of moderate to severe atopic dermatitis in adults
who are not adequately responsive to or are intolerant of
conventional therapies such as topical corticosteroids.
Protopic
0.1%: - treatment of moderate to severe atopic
dermatitis in adults who are not adequately responsive to or
are intolerant of conventional therapies such as topical
corticosteroids. Protopic
0.03%, 0.1%:- maintenance
treatment of moderate to severe atopic dermatitis for
prevention of fares and prolongation of fare-free intervals in
patients experiencing a high frequency of disease exacerbations
(i.e. occurring 4 or more times per year) who have had an
initial response to a maximum of 6 weeks treatment of twice
daily tacrolimus ointment (lesions cleared, almost cleared or
mildly affected). DOSAGE AND METHOD OF USE
Protopic
should be initiated by physicians with experience in
the diagnosis and treatment of atopic dermatitis. Protopic
can
be used for short-term and intermittent long-term treatment.
Treatment should not be continuous on a long term basis.
Protopic
should be applied as a thin layer to affected or
commonly affected areas of the skin and may be used on any
part of the body, including face, neck and fexure areas
(except eyes and mucous membranes). Protopic
should not
be applied under occlusion. Protopic
is not recommended for
use in children below the age of 2 years until further data are
available. Specifc studies have not been conducted in elderly
patients. However clinical experience has not shown the
necessity for any dosage adjustment. Treatment of fares:
Protopic
treatment should begin at the frst appearance of
signs and symptoms. Each affected region of the skin should be
treated with Protopic
until lesions are cleared, almost cleared
or mildly affected. Thereafter, patients are considered suitable
for maintenance treatment (see below). At the frst signs of
recurrence (fares) of the disease symptoms, treatment should
be re-initiated. General considerations for treatment of fares:
Use in children (2 years of age and above) Protopic
0.1% is
not indicated for use in children. Treatment with Protopic
0.03% should be started twice a day for up to three weeks.
Afterwards the frequency of application should be reduced to
once a day until clearance of the lesion. Use in adults (16 years
of age and above) Treatment should be started with Protopic
0.1% twice a day and continued until clearance of the lesion. If
symptoms recur, twice daily treatment with Protopic
0.1%
should be restarted. An attempt should be made to reduce the
frequency of application or use the lower strength if the clinical
condition allows. Generally, improvement is seen within one
week of starting treatment. If no signs of improvement are
seen after two weeks of treatment, further treatment options
should be considered. Maintenance of fare-free intervals:
Protopic
should be applied once a day twice weekly
(e.g. Monday and Thursday) to commonly affected areas to
prevent progression to fares. Between applications there
should be 2-3 days without Protopic
treatment. Adult patients
(16 years of age and above) should use Protopic
0.1%,
children (2 years of age and above) should use the lower
strength Protopic
0.03%. If signs of a fare reoccur, twice
daily treatment should be re-initiated. After 12 months, a
review of the patients condition should be conducted by the
physician and a decision taken whether to continue
maintenance treatment. In children, this review should include
suspension of treatment to assess the need to continue this
regimen and to evaluate the course of the disease.
UNDESIRABLE EFFECTS Very common: Burning sensation
(which tends to resolve within one week of starting treatment),
pruritus. Common: Sensation of warmth, erythema, pain,
irritation, paraesthesia and rash at site of application. Alcohol
intolerance (facial fushing or skin irritation after consumption
of an alcoholic beverage). Patients may be at an increased risk
of herpes viral infections (herpes simplex [cold sores], eczema
herpeticum, Kaposis varicelliform eruption) and folliculitis.
Uncommon: acne. During post-marketing experience: Rosacea
and application site oedema. Also, cases of malignancies,
including cutaneous (i.e. cutaneous T Cell lymphomas) and
other types of lymphoma, and skin cancers, have been
reported in patients using tacrolimus ointment. Application site
impetigo and application site infections occurred more
frequently in a study of maintenance treatment in adults and
children. Prescribers should consult the summary of product
characteristics in relation to other side effects.
PRECAUTIONS FOR USE Exposure of the skin to sunlight
should be minimised and the use of ultraviolet (UV) light from
a solarium, therapy with UVB or UVA in combination with
psoralens (PUVA) should be avoided during use of Protopic
.
Patients should be advised on appropriate sun protection
methods, such as minimisation of the time in the sun, use of a
sunscreen product and covering of the skin with appropriate
clothing. Protopic
should not be applied to lesions that are
considered to be potentially malignant or pre-malignant. The
development of any new change different from previous
eczema within a treated area should be reviewed by the
physician. Protopic
is not recommended in patients with skin
barrier defect, such as Nethertons syndrome, lamellar
ichthyosis, generalised erythroderma or cutaneous Graft Versus
Host Disease. Care should be exercised if applying Protopic
to
patients with extensive skin involvement over an extended
period of time, especially in children. Patients, particularly
paediatric patients should be continuously evaluated during
treatment with respect to the response to treatment and the
continuing need for treatment. After 12 months this evaluation
should include suspension of Protopic
treatment in paediatric
patients. The potential for local immunosuppression
(possibly resulting in infections or cutaneous malignancies) in
the long term (i.e. over a period of years) is unknown.
Protopic
contains the active substance tacrolimus, a
calcineurin inhibitor. In transplant patients, prolonged systemic
exposure to intense immunosuppression following systemic
administration of calcineurin inhibitors has been associated
with an increased risk of developing lymphomas and skin
malignancies. In patients using tacrolimus ointment, cases of
malignancies, including cutaneous (i.e. cutaneous T Cell
lymphomas) and other types of lymphoma, and skin cancers
have been reported. Protopic
should not be used in patients
with congential or acquired immunodefciencies or in patients
on therapy that cause immunosuppression. Patients with atopic
dermatitis treated with Protopic
have not been found to have
signifcant systemic tacrolimus levels. Lymphadenopathy was
uncommonly (0.8%) reported in clinical trials. The majority of
these cases related to infections (skin, respiratory tract, tooth)
and resolved with appropriate antibiotic therapy. Patients who
receive Protopic
and who develop lymphadenopathy should
be monitored to ensure that the lymphadenopathy resolves.
Lymphadenopathy present at initiation of therapy should be
investigated and kept under review. In case of persistent
lymphadenopathy, the aetiology of the lymphadenopathy
should be investigated. In the absence of a clear aetiology for
the lymphadenopathy or in the presence of acute infectious
mononucleosis, discontinuation of Protopic
should be
considered. The effect of treatment with Protopic
on the
developing immune system of children aged below 2 years has
not been established. Before commencing treatment with
Protopic
, clinical infections at treatment sites should be
cleared. Emollients should not be applied to the same area
within 2 hours of applying Protopic
. Concomitant use of other
topical preparations has not been assessed. There is no
experience with concomitant use of systemic steroids or
immunosuppressive agents. Protopic
should be used with
caution in patients with hepatic failure. Protopic
should not be
used during pregnancy unless clearly necessary and is not
recommended when breast-feeding. Protopic
is unlikely to
have an effect on the ability to drive or use machines.
CONTRAINDICATIONS Hypersensitivity to macrolides in
general, to tacrolimus or to any of the excipients.
INTERACTIONS Paediatric population:- An interaction study
with protein-conjugated vaccine against Neisseria menigitidis
serogroup C has been investigated in children aged 2-11 years.
No effect on immediate response to vaccination, the generation
of immune memory, or humoral and cell-mediated immunity
has been observed. Systemically available tacrolimus is
metabolised via the hepatic Cytochrome P450 3A4. The
possibility of interactions cannot be ruled out and the
concomitant systemic administration of known CYP3A4
inhibitors in patients with widespread and/or erythrodermic
disease should be done with caution. PACKAGE SIZES
Prices exclude VAT: Protopic
0.03% ointment 19.44
(30g tube), 35.46 (60g tube) Protopic
0.1% ointment
21.60 (30g tube), 39.40 (60g tube) LEGAL
CATEGORY: POM. MARKETING AUTHORISATION
NUMBERS Protopic
0.03% ointment EU/1/02/201/001-
2 Protopic
0.1% ointment EU/1/02/201/003-4.
FURTHER INFORMATION AVAILABLE FROM: Astellas
Pharma Ltd, 2000 Hillswood Drive, Chertsey, Surrey, KT16
0RS. UK. DATE OF REVISION: September 2012 FOR
FULL PRESCRIBING INFORMATION REFER TO THE
SUMMARY OF PRODUCT CHARACTERISTICS.
PRO073_Protopic_Pulse advert_PI_98 x 263.indd 1 18/12/2012 09:12
Prescribing Information
Traxam
Gel (Felbinac)
Presentation: Traxam Gel 3% w/w is a clear, non-greasy, non-staining gel
containing 30mg felbinac in each gram. Indication: Topical anti-infammatory
and analgesic for the relief of rheumatic pain, pain of non-serious arthritic
conditions and soft tissue injuries such as sprains, strains and contusions.
Dosage and Administration: Cutaneous administration. In adults and elderly:
Rub 1g Traxam Gel (approximately 1 inch/2.5cm of gel) lightly into the affected
area(s) 2 to 4 times a day. Do not exceed total daily dose of 25g regardless of
the size or number of affected areas. Children: Not recommended. Wash hands
following application unless they are the site of treatment. Contraindications:
Hypersensitivity to the ingredients. Patients in whom attacks of asthma, urticaria
or acute rhinitis are precipitated by aspirin or other non-
steroidal anti-infammatory drugs. Special Precautions
and Warnings: Use of Traxam should be limited to intact
and non diseased skin and it should not be applied with
occlusive dressings, or simultaneously to the same site
as other topical preparations. Discontinue if rash develops. Contact with mucous
membranes and the eyes should be avoided. Topical application of large amounts
may result in systemic effects, such as hypersensitivity, asthma and renal disease.
To avoid the possibility of photosensitivity, patients should be advised against
excessive exposure of treated areas to sunlight. Pregnancy and Lactation:
Not recommended. Interactions: Serum levels following topical application are
extremely low and therefore clinical drug interactions are unlikely. Concurrent use
of aspirin or other NSAIDs may result in increased incidence of adverse reactions.
Adverse Effects: The overall incidence of side effects reported with Traxam Gel
is low (less than 2%). Anaphylaxis, respiratory reactivity comprising asthma,
aggravated asthma or dyspnoea, purpura, angioedema, bullous dermatoses
(including epidermal necrolysis and erythema multiforme) and skin photosensitivity
have been reported. Local reactions such as mild erythema, irritation, dermatitis;
pruritus and paraesthesia which recover upon cessation of treatment may be
seen with Traxam Gel/Foam. Whilst systemic side effects are rare; gastrointestinal
disturbances and hypersensitivity reactions such as rashes and bronchospasm
have been reported. Please refer Summary of Product Characteristics for
detailed information. Legal Category: POM. Basic NHS Cost: 100gm gel 8.03.
Marketing Authorisation Numbers: PL 12762/0085. Marketing Authorisation
Holder: Mercury Pharmaceuticals Ltd., NLA Tower, 12-16 Addiscombe Road,
Croydon, Surrey; CR0 0XT, UK. Date of preparation: July 2012.
Adverse events should be reported to the local regulatory
authority. Reporting forms and information can be found at
http://yellowcard.mhra.gov.uk. Adverse events should also
be reported to Mercury Pharma Medical Information
at 08700 70 30 33 or via e-mail to
medicalinformation@mercurypharma.com
Visit www.managingpain.co.uk for more information.
UK/TRA/ADV/194/2012 Date of preparation: July 2012.
At their age
youd think
theyd know
better...
...fortunately
for them theres
Relieves pain and Relieves pain and
infammation infammation
G
E
L
100482 MER Pulse Traxam Ad (290x230) AW.indd 1 26/11/2012 16:32
Its time to take IBS seriously
UKLIN1616 January 2013
Irritable Bowel
Syndrome
Painful, distressing, exhausting
Irritable Bowel Syndrome is a physical disorder associated
with multiple symptoms that include chronic abdominal pain,
bloating and either constipation (IBS-C), diarrhoea (IBS-D) or
mixed symptoms of diarrhoea and constipation (IBS-M).
In other words, IBS has a much more serious effect on patients
lives than you might think.
J
o
b
N
o
:
A
L
M
0
1
J
1
2
0
0
5
_
M
a
r
k
e
t
_
S
h
a
p
i
n
g
_
P
U
L
S
E
_
2
9
0
x
2
3
0
S
i
z
e
:
2
9
0
x
2
3
0
m
m
1
A
B
P
I
:
T
Y
P
E
F
A
C
E
:
I
M
A
G
E
S
H
R
:
L
R
:
C
M
Y
K
:
S
P
O
T
:
S
c
i
e
n
c
e
w
r
i
t
e
r
:
D
e
s
i
g
n
:
A
r
t
D
i
r
:
C
r
e
a
t
.
D
i
r
:
C
o
p
y
w
r
i
t
e
r
/
P
r
o
o
f
:
S
.
M
a
n
:
A
c
c
.
M
a
n
:
A
c
c
.
D
i
r
:
ALM01J12005_Market_Shaping_PULSE_290x230.indd 1 31/01/2013 12:05
www.pulsetoday.co.uk Pulse March 2013 29
EDITORIAL
I
ts been widely accepted for some time now
that general practice needs more GPs. The
shift of work from secondary to primary care
is an ongoing trend, the retirement time
bomb seems to have been ticking for years
and the small matter of GPs taking on
commissioning responsibility, now just four
weeks away, has been on the horizon since 2010. But
our investigation this month suggests long-standing
fears of a recruitment crisis have finally been
realised, with the average vacancy rate for GP posts
at practices quadrupling in just two years.
It is important, of course, not to overstate the case.
An average vacancy rate is a crude measure which
masks regional variation, and there have always been
cyclical fluctuations in the jobs market. Just a few
years ago, we were talking about a recruitment crisis
in general practice which consisted of there being too
few jobs for GPs, rather than the other way round.
Its also worth acknowledging the shortages are
partly due to general practices rapidly changing
demographics. 2013 is supposed to be the year when
women will for the first time make up the majority of
the GP workforce, but its not just female GPs who are
increasingly keen on a better work-life balance.
Portfolio careers, meanwhile, are fast becoming the
norm. Dr David Weinstein, for instance, the Brighton
GP featured in our Working Life photo essay this
month (page 64), works every Friday in A&E and
says the variety makes him a better doctor.
Whatever the causes, both CCGs and the
Department of Health must do more to ensure
practices can plug the gaps. Adequate backfill for
partners taking on commissioning work and
including sessional GPs in CCG work will help
somewhat; asking practices to pay locums
superannuation and then reimbursing them
according to list size rather than locum use,
as is currently the plan, will probably not.
But beyond the immediate difficulties in filling
vacancies, the jobs crisis raises fundamental
questions about the future of the profession, a nd how
it can attract the new blood it desperately needs.
General practice has always been a hard sell to
medical graduates tempted by the glamour of hospital
medicine, but in the years after the introduction of the
2004 contract, healthy earnings, acceptable hours and
a degree of independence
made it an attractive
alternative. Yet, despite the
DH boldly declaring that
GP registrars should
account for 50% of
specialty training places by
2015 and opening up more
training slots as a result,
deaneries are struggling to
fill the ones they have.
If ministers are serious
about increasing the
number of GPs, they must make it an enticing
career option once again. GPs cite an unmanageable
workload and box-ticking clinical culture as
off-putting factors for would-be trainees, while
increasing bureaucracy and contractual uncertainty
are dissuading many from the financial commitment
of partnership. In the past few months alone,
ministers have brought in revalidation, ripped up
the GP contract and gone to war over pensions.
If they really do value general practice, they have
a funny way of showing it.
For an older generation general practice will
always be, as Dr Peter Swinyard puts it, the best job
in the world. But that generation is a retiring breed.
Their successors need to know it will still be the best
job in the world in 20 years time.
A profession fast
losing its appeal
Email
pulse@pulsetoday.co.uk
Address (editorial)
Pulse,
Brieng Media, 3rd Floor
Mermaid House,
2 Puddle Dock,
London
EC4V 3DB
Group editor
Jo Haynes
Editor
Steve Nowottny
Group clinical editor
Adam Legge
Deputy editor
Nigel Praities
Senior journalist
Jaimie Kaffash
Senior journalist
Soa Lind
Journalist
Madlen Davies
Digital content
manager
Jessica Baron
Online intern
Cat Atteld
Deputy clinical editor
Rhiannon Smith
Assistant clinical editor
David Swan
Assistant features
editor
Ellie Broughton
Art director
Ravi Naidoo
Art editor
James Depree
Editorial adviser
Dr Keith Hopcroft
Production controller
Justine Sumner
Classied executive
Cliff Brown
Key account manager
George Haddad
Key account manager
Richard Springham
Projects director
Paul Berressem
Commercial director
Sanjay Chudasama
CEO, Brieng Media
Neil Thackray
CMO, Brieng Media
Rory Brown
Editorial enquiries
020 7332 2904
Classied advertising
020 7332 2924
Display advertising
020 7332 2928
pulsetoday.co.uk
020 7332 2938
Delivery and
subscription
Medical Reader, c/o
BHP, 2-3 Commercial
Way, Christy Close,
Southelds, Basildon
SS15 6EF
Free circulation:
Call 0845 1369316
or email
medicalreader@
binleys.com
Paid subscription:
Call 0844 543 8022
Registered ofce
Brieng Media, 3rd
Floor Mermaid House,
2 Puddle Dock, London
EC4V 3DB
Brieng Media 2013
All rights reserved.
No part of this
publication may be
reproduced or
transmitted in any form
or by any means,
electronic or mechanical
including photocopying,
recording or any
information storage or
retrieval system without
the express prior written
consent of the publisher.
The contents of Pulse
are subject to
reproduction in
information storage and
retrieval systems.
Pulse is available on
subscription at 160 per
year (single copy 16).
Overseas subscriptions,
including Europe, $327
per year (single copy
$41). Refunds on
cancelled subscriptions
will only be provided at
the publishers
discretion, unless
specically guaranteed
within the terms of
subscription offer.
Brieng Media may pass
suitable reader
addresses to other
relevant suppliers.
If you do not wish to
receive sales
information from other
companies, please write
to Pulse, Brieng Media,
3rd Floor Mermaid
House, 2 Puddle Dock,
London EC4V 3DB.
Printed by Headley
Brothers, The Invicta
Press, Ashford, Kent
If ministers
really do value
GPs, they have
a funny way of
showing it
V
I
E
W
S
Steve Nowottny,
Pulse editor
Dovobet Gel: Topical treatment of scalp psoriasis in adults. Topical
treatment of mild-to-moderate non-scalp plaque psoriasis vulgaris in
adults. Dovobet Ointment (calcipotriol/betamethasone dipropionate):
Treatment of stable plaque psoriasis vulgaris amenable to topical therapy
in adults. Please consult the Summary of Product Characteristics before
prescribing, particularly in relation to side-effects, precautions and
contraindications. POM. Further information is available on request from
the marketing authorisation holder: LEO Pharma, Longwick Road, Princes
Risborough, Bucks HP27 9RR. LEO LEO Pharma, UK. All LEO trademarks
mentioned belong to the LEO Group. Code 1008/11053 January 2013.
Adverse events should be reported. Reporting forms and information
can be found at: www.mhra.gov.uk/yellowcard. Adverse events
should also be reported to Drug Safety at LEO Pharma by calling
01844 347333.
Compare ointment and gel for
yourself. Order vehicle samples
today www.dovobetgel.co.uk
Its about time you saw the dierence
28664 Dovobet Half Horizontal Pulse Ad v8 AW.indd 1 01/02/2013 11:50
www.pulsetoday.co.uk 30 March 2013 Pulse
GPs must consider
new ways of working
in order to survive
From Dr Malcolm Ridgway, Blackburn
I think all GPs are aware of the extra
stress on practices and the likely further
increases in demand and reductions in
income (Shocking numbers of GPs
seeking pastoral support, say LMCs,
pulsetoday.co.uk/news).
For me, we are trying to utilise
a general practice model that was
invented before the inception of the
NHS to deliver 21st-century care. Many
commentators (such as the Kings Fund)
are now calling for the cottage industry/
corner shop organisational model of
general practice to be updated. The
RCGP has talked about federation. The
Government, I think, is piling on the
pressure to enforce structural changes
voluntarily or GPs will have to
surrender and succumb to an enforced
salaried model, vertical integration or
whatever scheme seems politically
beneficial at the time.
I always feel we should be in control of
our own destiny, yet all I see from GP
colleagues is a head-in-the-sand, hope it
all goes away or I retire attitude. When
will we wake up and smell the coffee?
There are possible models that maintain
continuity of care, improve quality and
reduce variation, maintain practice
sovereignty, expand and improve
services, bring more expertise and care
out into the community and yet improve
work-life balance and maintain incomes.
Successful businesses generally expand
and diversify (like Google and Tesco) and,
at the end of the day, GP practices are
businesses at least for now. Yet the vast
majority of GPs wont even consider
alternative models of working.
I think Pulse should start a campaign
that debates innovative solutions to do
what I have said above, and at least gets
GPs thinking outside the box. I am close
to retirement, so none of this will really
affect me, but I am getting fed up with
the increasingly intense demands from
clinical work. Also, I have seen lots of
GPs of my age or younger retiring not
because they feel able to financially, but
because they can no longer cope with
how general practice has become. These
are people at the height of their
experience and knowledge and they will
be sadly missed by their patients, and
indeed the NHS.
From Dr Ivan Camphor, secretary of
Mid Mersey LMC, via pulsetoday.co.uk
General practice is going through
exceptionally challenging times. Morale
is at an all-time low, and we are all
suffering from overload. I work 12-hour
days in the week and spend all Sunday,
like colleagues, doing paperwork. Were
only human, and we need to see our
families and friends to survive
emotionally. At the moment GPs are
maxed out many of my colleagues in
their 50s are retiring simply to get away
from the workload. General practice isnt
sustainable at the moment which
makes the failure of the latest contract
negotiations all the more painful to
watch.
We must fnd
alternative
models for
general
practice
Come to Pulse
Live, your
one-stop annual
event to debate
the future of
general practice
pulse-live.co.uk
Could GPs learn business lessons from Tesco?
Letter of the month
Feedback
Views
Email: letters@pulsetoday.co.uk
Lets call ministers
bluff and resign from
CCGs en masse
From Dr Anthony OBrien, Silverton, Devon
Why is the GPC not suggesting
co-ordinated action in response to the
contract imposition? We have a powerful
negotiating weapon that we seem to be
ignoring. A co-ordinated resignation of
practices from CCGs would have no effect
on patients or doctors but would cause
apoplexy in Government and Whitehall.
It is surprising that GPs who have been
coerced into commissioning are not now
questioning whether we wish to continue
our involvement. Why should we help
the Government with its NHS rationing
difficulties? The Government cannot
allow its commissioning project to fail.
But CCGs are membership organisations.
The statutory duty to belong to a CCG
may be part of the new contract but it is
not in the old one.
If we resign from our CCGs, political
chaos will follow. The Government will
be forced back to the negotiating table.
The public will not be affected and will
have no understanding of what is
happening. We will not be seen to be
complaining about money just
reconsidering the flawed health bill
proposals. Commissioning enthusiasts
might have to twiddle their thumbs for
a bit, but we have survived without fully
functioning PCTs for many months.
A few more will not sink the NHS.
If practices want to leave CCGs, they
do not have to justify themselves. If the
Government wishes to use the courts to
impose the contract and commissioning,
we should challenge them to do so. It is
important to emphasise this is not a
debate about money or pros and cons of
commissioning. It is a point of principle.
We have negotiated in good faith and do
not wish to be treated in this way.
Shame on the GPC for being so
despondent. We should all stand up,
stop moaning and call for a boycott of
commissioning if negotiations are not
reopened.
Common sense
approach to CSA
must stay
From Dr Hamish
Duncan, Exeter, via
pulsetoday.co.uk
While it is laudable
to ensure the CSA
exam is rigorous and
non-discriminatory,
lets not create a two-tier
pass rate (Lawyers give RCGP three
weeks to sort CSA, or face legal action,
pulsetoday.co.uk/news). a
l
a
M
y
x
2
Dovobet Gel: Topical treatment of scalp psoriasis in adults. Topical
treatment of mild-to-moderate non-scalp plaque psoriasis vulgaris in
adults. Dovobet Ointment (calcipotriol/betamethasone dipropionate):
Treatment of stable plaque psoriasis vulgaris amenable to topical therapy
in adults. Please consult the Summary of Product Characteristics before
prescribing, particularly in relation to side-effects, precautions and
contraindications. POM. Further information is available on request from
the marketing authorisation holder: LEO Pharma, Longwick Road, Princes
Risborough, Bucks HP27 9RR. LEO LEO Pharma, UK. All LEO trademarks
mentioned belong to the LEO Group. Code 1008/11053 January 2013.
Adverse events should be reported. Reporting forms and information
can be found at: www.mhra.gov.uk/yellowcard. Adverse events
should also be reported to Drug Safety at LEO Pharma by calling
01844 347333.
Compare ointment and gel for
yourself. Order vehicle samples
today www.dovobetgel.co.uk
Its about time you saw the dierence
28664 Dovobet Half Horizontal Pulse Ad v8 AW.indd 1 01/02/2013 11:50
What youre saying
about the Francis
Inquiry
We do not need GPs
to be given the role
of assessing care
standards. We need
to use existing
processes properly
The concept of
a primary care-led NHS
was always just wishful
thinking easily said
but never done
And there was me
thinking the CQC
actually had a purpose
Join the debate at
pulsetoday.co.uk/your-comments
Join the debate
Have your say on
the big GP issues of
the moment at
pulsetoday.co.uk/
forum
Being a good doctor includes a certain
level of understanding of the cultural and
linguistic norms of the society you serve,
the systems to deliver the service and the
ability to work within a different cultural
context. If someone is not good enough
to do this, they should fail regardless of
background. Multiple failings should
lead to removal from training. There is
nothing politically incorrect, racially
motivated or immoral about this, its just
good common sense.
In the same vein, lets ensure this
challenge is rigorous and sensible and
the outcome does not succumb to
political correctness. If the verdict goes
against the plaintiffs, they must accept it
and move on. If it finds in favour, the
RCGP needs to answer serious questions
about its impartiality and conduct.
How many GPs does
it take to change
a lightbulb?
From Dr Gavin Jamie, Swindon,
via pulsetoday.co.uk
Your story (CCG calls GPs into crisis
point hospital to help assess every
patient for discharge, pulsetoday.co.uk/
news), reminded me of a joke on Twitter
a few weeks ago: Q: How many National
Rifle Association members does it take to
change a lightbulb? A: More guns!
It sometimes seems the reflex answer
to any issue in health is More GPs!
While this faith in our omnipotence is
touching, it may be seen by others as
arrogance or even pomposity. Hospitals
are full of excellent doctors capable of
making good assessments of their
patients. Could they benefit from more
knowledge of community care? Quite
possibly. But lets respect them, let them
do their job and fund decent and prompt
community care.
Feedback
32 March 2013 Pulse www.pulsetoday.co.uk
Views
The BiG iNTeRView
Dr Paul Cundy
its time to
pull the plug
on summary
Care Records
Does the NHS IT programme promise genuine progress
or just change for its own sake? Madlen Davies talks to the
GPCs IT lead Dr Paul Cundy
In this practice we have a disproportionate
number of nuns, begins Dr Paul Cundy,
in answer to a question about concerns
over data requests from the new General
Practice Extraction Service (GPES), the
Government-run system that is set to
make patient records more accessible to
NHS managers, researchers and private
companies.
We have concerns that some queries
might not be appropriate for those
patients.
It is a typically clear-headed response,
sensitive to the real-world concerns of
patients, to a question about the use of IT,
for which he has been a GPC
spokesperson for nearly 12 years.
Sitting in his surprisingly low-tech
practice in Wimbledon, south-west
London, Dr Cundy appears relaxed,
despite the continual stream of new-
technology projects clogging up his
in-tray as they float downstream from
the Department of Health.
A member of the GPC for 18 years and
a GP since 1982, Dr Cundy has seen his
fair share of politicians promising
whizz-bang technology solutions that
turn out to be duds.
And this Government, he says, is no
different.
Its a continuing disappointment
that successive governments have
introduced policy that is not based on
evidence, he says with an air of weariness.
Thats the political world, its not the
scientific world we live in. The GPC will
point out the evidence; its up to the
Government to decide whether to listen.
Online records
Dr Cundy is leading the GPCs IT
subcommittee at a time when historic
decisions are being made about the
future of NHS IT. Health secretary Jeremy
Hunt who has promised a paperless
NHS by 2018 has made technology a top
priority, with the Governments
information strategy aiming to enable
patients to book GP appointments, access
their records and contact their GP online
by 2015.
Dr Cundy says these proposals for GPs
are self-evidently very sensible but need
to be carefully managed: The net effect
will lower the threshold at which
patients will communicate with health
services; that will inevitably result in an
increase in workload.
If general practice suffers what has
happened in the States, where theres
a 25% across-the-board increase in work,
primary care will fall apart because it
cannot sustain that level of increase.
Summary Care Records
He is even more strident on the long-
running Summary Care Record (SCR)
Choose and Book
is an absolute
nightmare
Watch the full
interview with
Dr Paul Cundy
pulsetoday.co.uk/
tbi-cundy
CV
Chair of the GPC
IT subcommittee
since 1999 (bar
two years)
GP in
Wimbledon,
south-west
London, since
1982
Ran a GP
out-of-hours
commissioning
group for 10 years
Ran an IT
company for
15 years
Lists motor
racing, fying
planes and
anything
mechanical as his
hobbies
www.pulsetoday.co.uk Pulse March 2013 33
www.pulsetoday.co.uk 34 March 2013 Pulse
The big inTerview
views
Dr Cundy on...
...online access to GPs
If general practice suffers
what has happened in
the States, primary care
will fall apart
...Choose and Book
The patient and GP can
only choose from the
appointments offered by
the trust. Theres no
choice there you are
given what youre given
...the SCR programme
The system is a disgrace;
the plug should be pulled
as soon as possible
...the GPES
Were on the verge of
a public information
campaign saying: When
you go to see your GP,
the information thats
been taken will not be
used just for your
personal care
programme. According to the latest NHS
Connecting for Health bulletin, almost
23 million people in England more than
one in three now have an SCR, and their
records have been accessed a combined
total of 242,341 times since their creation.
But Dr Cundy is unimpressed by the
stats, and offers some calculations of his
own: If you look at that in terms of
utilisation rate, it means that each time
an SCR has been accessed for a patient,
it has cost 1,200 for that access.
The system is an absolute disgrace
and the plug should be pulled as soon as
possible, he adds, though he later
stresses that he is speaking in a personal
capacity on this issue and that official
BMA policy remains that the SCR
programme should stand on its merits.
Dr Cundy supports LMC leaders who
have called for patient information
campaigns on the SCR to be restarted, as
most patients are blissfully unaware any
record has been created in their name.
The information programme was run
several years ago, he says. These records
are now being created and patients are
not aware of whats going on.
GPES
Dr Cundy is also highly critical of the
DH programme to make data from GP
records more accessible to NHS managers
and others through the new GPES system.
The Government is keen to stamp
on any suggestion that it is creating
a super-database, but Dr Cundy says
the initiative marks a sea-change in
attitudes to the use of patient data.
He says: Theres a great move at the
moment to say that patient data in the
NHS is there for use by the NHS, but
thats not the way data has been used for
the past 60 years. Thats a fundamental
change and patients need to understand
that.
The GPES system enables data both
patient-identifiable and anonymous to
be extracted from GP systems and sent to
the Health and Social Care Information
Centre, which can send it on to
customers in the NHS and potentially
also private companies.
The GPC negotiated some important
protections, namely that GPs must agree
to the extract being taken and requests
for data must go before the GPES
Independent Advisory Group, which will
conduct an information governance
assessment.
The NHS Commissioning Board
recently announced it planned regular
extractions of anonymised data on
demographics, diseases, events and
referrals from GP systems.
Dr Cundy says: Most patients do not
understand that their information may
be used to police CCGs, trusts and GPs.
If were going to be moving to an area
where its being used to routinely manage
whats going on in the NHS which is
a legitimate aspiration then patients
need to understand that.
He advocates a public information
campaign on the GPES to inform patients
that when you go to see your GP or go to
A&E or hospital, the information thats
been taken will not be used just for your
personal care but for other things too.
Telehealth
Dr Cundy is also critical of another of the
Governments big ideas, questioning
whether GPs can cope with leading the
drive on telehealth.
Theres no doubt there are a few niche
areas where the use of telehealth can be
very valuable, he says.
But for the average patient who lives
half a mile from their practice, and who
has conditions that are not terribly
urgent and is mobile, telehealth is of no
value whatsoever.
You go from a situation where you
take someones blood pressure once
every six months to 24 every day. That
overwhelms systems.
He concludes with an observation that
might apply not just to telehealth but to
the wider NHS IT strategy: We have to be
careful not to do things just because they
can be done.
New this month
Go online to watch
our Big Interview
with Dr John
Canning on the
CQC, GP contract
and work capability
assessments
pulsetoday.co.uk/
tbi-canning
PALEXIA
SR and PALEXIA
Prescribing Information.
Refer to the Summary of Product Characteristics (SmPCs) before prescribing. Presentation:
Palexia SR: 50 mg (white), 100 mg (pale yellow), 150 mg (pale pink), 200 mg (pale orange)
and 250 mg (brownish red) prolonged-release tablets contain 50 mg, 100 mg, 150 mg,
200 mg and 250 mg of tapentadol (as hydrochloride) respectively. Palexia: 50 mg (white)
and 75 mg (pale yellow) flm-coated tablets contain 50 mg and 75 mg of tapentadol (as
hydrochloride) respectively. Indication: Palexia SR is indicated for the management of
severe chronic pain in adults, which can be adequately managed only with opioid analgesics.
Palexia is indicated for the relief of moderate to severe acute pain in adults, which can be
adequately managed only with opioid analgesics. Dosage and method of administration:
Individualise according to severity of pain, the previous treatment experience and the
ability to monitor the patient. Swallowed whole with suffcient liquid, with or without food.
Palexia SR should not be divided or chewed. Palexia SR dosage: Initial dose 50 mg twice
a day. Switching from other opioids may require higher initial doses. Titrate in increments
of 50 mg twice a day every 3 days for adequate pain control. Total daily doses greater
than 500 mg not recommended. Palexia dosage: Initial dose 50 mg every 4 to 6 hours.
On the frst day of dosing, an additional dose may be taken 1 hour after the initial dose, if
no pain control. The frst days dose should not exceed 700 mg. Maximum maintenance
daily dose of up to 600 mg. Discontinuation of treatment: Taper dose gradually to prevent
withdrawal symptoms. Renal/hepatic impairment: Not recommended in severe patients.
Caution and dose adjustments with moderate hepatic impairment. Elderly: May need
dose adjustments. Children below 18 years: Not recommended. Contraindications:
Hypersensitivity to ingredients, suspected or having paralytic ileus, acute alcohol
intoxication, hypnotics, centrally acting analgesics or psychotropics. Not for use when
mu-opioid receptor agonists are contraindicated (e.g. signifcant respiratory depression,
acute or severe bronchial asthma or hypercapnia). Special warnings and precautions:
At risk patients may require monitoring due to misuse, abuse, addiction or diversion.
At high doses or in mu-opioid receptor agonist sensitive patients, dose-related respiratory
depression may occur. Caution and monitoring required with impaired respiratory function.
Should not use in patients susceptible to intracranial effects of carbon dioxide retention (e.g.
increased intracranial pressure, impaired consciousness or coma). Use with caution with head
injury, brain tumors, history or at risk of seizures, moderate hepatic impairment, biliary tract
disease or acute pancreatitis. Not recommended with severe renal or hepatic impairment.
Avoid use in patients who have taken monoamine oxidase inhibitors (MAOIs) within the last
14 days, due to cardiovascular events. Should not use with hereditary problems of galactose
intolerance, Lapp lactase defciency or glucose-galactose malabsorption. Interactions: Use
with benzodiazepines, barbiturates and opioid analgesics, antitussive drugs and substitutive
treatments may enhance the risk of respiratory depression. Central nervous system (CNS)
depressants (e.g. benzodiazepines, antipsychotics, H1-antihistamines, opioids, alcohol) can
enhance the sedative effect and impair vigilance. Consider dose reduction with respiratory or
CNS depressant agents. In isolated cases, serotonin syndrome has been reported with Palexia
SR/Palexia in combination with serotoninergic medicinal products (e.g. serotonin
re-uptake inhibitors). Care should be taken with mixed mu-opioid agonist/antagonists
or partial mu-opioid agonists due to risk of reducing the analgesic effect. Use
with strong inhibitors of uridine diphosphate transferase isoenzymes (involved in
glucuronidation) may increase systemic exposure of Palexia SR/Palexia. Risk of
decreased effcacy or adverse events if used with strong enzyme inducing drugs
(e.g. rifampicin, phenobarbital, St Johns Wort). Pregnancy and lactation: Do not use.
Driving and using machines: May have major effect on ability to drive and use machines,
especially at the beginning or change in treatment, in connection with alcohol or tranquilisers.
Undesirable effects: Very common (1/10): dizziness, somnolence, headache, nausea.
Palexia SR only: constipation. Palexia only: vomiting. Common (1/100, <1/10):
decreased appetite, anxiety, sleep disorder, tremor, fushing, diarrhoea, dyspepsia, pruritus,
hyperhidrosis, rash, asthenia, fatigue, feeling of body temperature change. Palexia SR only:
depressed mood, nervousness, restlessness, disturbance in attention, involuntary muscle
contractions, dyspnoea, vomiting, mucosal dryness, oedema. Palexia only: confusional
state, hallucinations, dry mouth, muscle spasms, constipation, abnormal dreams. Other
important undesirable effects: Palexia SR only: drug hypersensitivity (uncommon 1/1000,
<1/100), respiratory depression (rare 1/10,000, <1/1000); Palexia only: respiratory
depression (uncommon 1/1000, <1/100), hypersensitivity (rare 1/10,000, <1/1000).
No evidence of increased risk of suicidal ideation or suicide with Palexia SR/Palexia.
Consult the SmPCs for full details. Overdose: Seek specialist treatment (see SmPCs).
Legal classifcation: POM, CD (Schedule II). Marketing Authorisation numbers,
pack sizes and basic NHS cost: Palexia SR: 50 mg: PL 21727/0041, 28 pack
(12.46) and 56 pack (24.91); 100 mg: PL 21727/0042, 56 pack (49.82); 150 mg:
PL 21727/0043, 56 pack (74.73); 200 mg: PL 21727/0044, 56 pack (99.64)
and 250 mg: PL 21727/0045, 56 pack (124.55). Palexia: 50 mg: PL 21727/0032,
28 (12.46) and 56 pack (24.91); 75 mg: PL 21727/0033, 28 (18.68) and 56
pack (37.37). Marketing Authorisation Holder: Grnenthal Ltd, Regus Lakeside
House, 1 Furzeground Way, Stockley Park East, Uxbridge, Middlesex, UB11 1BD, UK. Date of
preparation: February 2012. P12 0053a.
References
1. Tzschentke, T.M., et al. Drugs Today (Barc), 2009; 45(7): 483-96.
2. Palexia SR, Summary of Product Characteristics. February 2011.
UK/P13 0009. Date of preparation: February 2013.
visit www.palexia.co.uk for more information
Palexia SR (tapentadol prolonged release tablets) is indicated for the treatment of severe
chronic pain in adults, which can be adequately managed only with opioid analgesics
2
Tapentadol is a Controlled Drug, Schedule 2
Start to unlock severe chronic
back pain with Palexia SR
A STRONG ANALGESIC WITH TWO
MECHANISMS OF ACTION IN ONE MOLECULE
1
Adverse events should be reported. Reporting forms and information can
be found at http://www.mhra.gov.uk/yellowcard. Adverse events should
also be reported to Grnenthal Ltd (telephone 0870 351 8960).
GR0042_Palexia_Master_Ad_Pulse_Mag_290x230_AW.indd 1 15/02/2013 16:48
www.pulsetoday.co.uk 36 March 2013 Pulse
DEBATE
VIEWS
Can GPs monitor hospital care?
YES
Dr Robert Varnam
says GPs are well
placed to take on the
Francis Inquiry
recommendation to
monitor the quality
of secondary care
More opinions online
I understand where Robert Francis QC is
coming from, but I dont think it is feasible.
GPs do look at what happens to their
patients when they are admitted. I, for
example, have frequently raised issues
when things have not been done
properly, or raised complaints about
poor care where appropriate.
But he is asking us to do this in a much
more systematic way. This requires
a whole new stream of work and we dont
have any mechanisms with which to
identify these concerns.
This is another example where lots of
work is being put at the door of GPs
without any resources. At the moment
there are no such systems at all in GP
practices. We are totally dependent on,
and only see, the patients discharge letter.
I dont have a problem with rethinking
how GPs define their role maybe it is
something that we need to be concerned
about. But could GP monitoring prevent
another Mid Staffs? Thats just
conjecture, really. The point about Mid
Most of the recommendations from the
Francis Inquiry in the wake of the Mid
Staffordshire scandal were aimed at
national regulators and local hospitals.
However, there are some significant
implications for general practice,
including the proposed duty of candour
legislation and the reminder that both
CCGs and GPs share a responsibility for
improving patient safety.
GPs are well placed to pick up on
some safety issues within hospitals.
This is not about spying on our hospital
colleagues but rather being vigilant for
opportunities to improve patient care.
Two major barriers, though, are time
and confidence in the system. We need to
ensure the forms for recording safety
issues are easy to access and quick to
complete for GPs and our teams. And we
also need to be confident that our safety
reports result in improvement for
patients. Theres no point in taking time
out of a busy day to complete a form if it
doesnt end up benefiting patients.
Evidence shows that people will report
NO
Professor Aneez
Esmail says the
recommendations
are unresourced
and unrealistic
safety concerns if they receive rapid
feedback and can see that effective action
is taken.
These changes are likely to require
a massive increase in the responsiveness
of local commissioners and national
agencies. Im optimistic CCGs will create
a much more cooperative and clinically
led culture between primary and
secondary care. One challenge for many
CCGs will be breaking some of the
traditions in NHS commissioning. In
many areas, commissioning has revolved
around contracts CCGs are in a good
position to take a fresh approach, which
begins with clinical collaboration.
As far as I can see, none of the lessons
from the Mid-Staffs tragedy are new.
The challenge for CCGs and the national
regulators is to put the old lessons into
practice.
Dr Robert Varnam is a GP in Manchester
and clinical lead for primary care at the
NHS Institute for Innovation and
Improvement
Staffs is that no one questioned it, and
the issue is who is best to do that.
It is possible that CCGs should have
that responsiblity, and perhaps could set
up systems to do this. The logical thing
when you talk about monitoring patterns
is that it is going to be the commissioning
groups that need to develop that.
If patients are going to do an exit
interview, which hospitals say they will,
then you might argue that is something
commissoners need to look at when they
make decisions about the hospital.
I would not write the idea off, but
it requires a level of analysis and
sophistication that is quite complex.
We have already got enough to do with
planning and commissioning services,
let alone monitoring them.
Professor Aneez Esmail is a professor of
general practice at the University of
Manchester. His research has focused on
patient safety, including the Shipman
Inquiry
Book prescriptions wont work
without guided support from GPs
Dr Martin Brunet says many GPs are
already offering book prescriptions,
but argues that the campaign still
lacks the practical detail it needs to
take off
pulsetoday.co.uk/brunet
The profession must face up to the
reality of GP burnout
GPs must be honest about the stess
and mounting workload they face, and
should be taught coping strategies,
writes Dr Sara Khan
pulsetoday.co.uk/khan
Debate: will the dementia DES
beneft patients?
Dr Alec Turnbull says the proposed
dementia DES will improve patients
quality of life, but Dr John Cosgrove
argues that case fnding is not enough
pulsetoday.co.uk/DES-debate
CCGs will
create a more
cooperative
culture
between
primary and
secondary
care
This is
another
example of
work being
put at the
door of GPs
www.pulsetoday.co.uk Pulse March 2013 37
H
ow did it happen? The Francis
report on the Mid Staffordshire
hospital scandal is at best
uncomfortable reading,
at worst, horrendous. People
died needlessly because of
poor care. Why?
There has been debate recently about how
useful hospital standardised mortality ratios
(HSMRs) really are. But it is clear that the
rates at Mid Staffordshire were higher than
expected as far back as 2001.
There are multiple problems in pulling
reliable data from existing coding systems.
The trust spent time and money investigating
mortality statistics and wrongly identified
coding errors rather than substandard care as
responsible for the apparently high mortality
rates. Making changes to coding practice was
considered to be the best solution. It wasnt
until 2008 that the Healthcare Commission
launched a full investigation.
But look again and the warning signs were all
there. In 2001, the chief executive of South
Western Staffordshire PCT warned the hospital
leadership was not competent. In January 2002,
a clinical governance review recommended
urgent action over a range of concerns. In 2003,
another review noted inadequate medical
and nursing staffing. Junior doctors had
been removed from position because of
concerns over training. Staff were utterly
demoralised and facing a chronic lack
of manpower. The medical director told
the inquiry a quick walk around the
wards would have shown... there was
cause for concern.
Evidence-based medicine is in my blood.
I like numbers. I like robust proof. But no
matter what the HSMR had been, the
story on the ground was there to be heard. If
patients are left to soil themselves or go unfed,
if staff are demoralised and distressed, this is
what we should have been hearing. That
evidence was there. But who was listening?
People tend to go into medicine or nursing
because they have a desire to do something
useful. So what happens when the professional
culture goes sour? I was thinking about this
today when I caught myself worrying about all
the contract indicators
I was missing. I was
torn between what
would tick boxes and
what would be best for
my patients.
What would happen
if we ditched the
QOF and made
appointments 15
minutes long? What
if we collected the data
we thought clinically
useful, and peer reviewed each other,
supporting ourselves and our colleagues?
What if we asked our patients to help us do
what we said we wanted to do in our interview
at medical school deliver our work as
a vocation?
As the QOF drives its fingernails under the
skin of the consultation, we get further away
from centring what we do on patients. We
look at the computer instead. I hate it. We
have less time to listen, and less time to hear.
This was at least part of the problem in Mid
Staffordshire: numbers mattered more.
The skill of GPs is being squeezed out by the
demands of the contract. We are being pushed
harder to meet tighter targets. But what are
we doing? And who is it for?
The Mid Staffordshire scandal was an object lesson in the danger of
relying too heavily on data and box-ticking, writes Margaret
When listening
matters most
McCartney
A quick walk
around the
wards would
have shown
there was cause
for concern
Dr Margaret
McCartney
is a GP in
Glasgow
Read more of
Dr McCartneys
columns at
pulsetoday.co.uk/
mccartney
38 March 2013 Pulse www.pulsetoday.co.uk
I
ll come straight to the point. Patients:
theyre a bit stupid, arent they? Ive
spent more than 25 years in general
practice waiting for them to up their
game. But Im starting to think its
hopeless.
True, just occasionally they can be
something other than stupid. Take today,
for example. I saw one patient who was quick
and one who was honest. The quick one was
a young woman who, I pointed out, had now
attended twice claiming that her
dihydrocodeine-containing handbag had
been stolen. And yet, I said smugly, Ive never
seen you with a handbag. Thats because
theyve all been nicked, she shot back, which
is smarter and less expletive-riddled than
youd expect from a junkie.
The honest one? A middle-aged man who
phoned about his Viagra. Im afraid theres
a problem at your end, he said. No, I thought,
theres a problem at your end, thats why
youre taking a phosphodiesterase type-5
inhibitor, but carry on. It turned out wed
forgotten to tick the private prescription box
on the computer, so his last few FP10s had
been free on the NHS. Actually, he said, it
was my wife who made me phone, which
put a different slant on the situation, while
rendering him even more honest. And
a bit poorer.
So, some are quick and honest. But
mostly, as I survey the wreckage of the
day, they are stupid. There is, of course,
the low-grade stupidity of glazed-eyed
punters who need me to explain what the
combination of sore throat, runny nose
and cough might possibly add up to,
and who also presumably need
reminding not to stick their
moistened fingers in the plug socket.
And theres the acute-on-chronic stupids,
whose denseness deserves wider
dissemination for posterity. Hence:
Patient 1, a 70-year-old man whos had
a stiff and creaking neck for nine yes nine
months. No prizes for guessing he has cervical
spondylosis. But a gold medal in moronalysis
if you realised his underlying concern, as
MRCGP hopefuls call it, is no kidding
meningitis.
Patient 2, a 28-year-old bloke whos had
a clicky and painful
jaw intermittently for
a year. Self-diagnosis?
Tetanus. My
diagnosis? Slack-jaw.
Where would you
rate these examples,
stupidity-wise, on
a scale of one to
monumental? I dont
mean to be unkind.
I know they dont
have medical degrees.
But Im not a mechanic, and yet if my car
wont start in the morning, I dont
automatically assume its been written off
by a truck, do I?
Its possible, of course, that my perceptions
distorted. Maybe GP attenders are skewed
towards the stupid end of the spectrum.
Perhaps we dont see the sensible ones who
piece together their symptoms intelligently
and decide they dont need to bother a doctor.
Then again, maybe they really are all a bunch
of malingering, neurotic stupids.
And if my appraiser is reading this, a) See
you soon and b) Dont worry that Im showing
signs of burn-out. Ive always been like this.
After a quarter of a century in general practice, Copperfeld has given up
hope that patients will develop any common sense
Im with Stupid,
unfortunately
Dr Tony
Copperfeld is
a GP in Essex.
You can email
him at:
tonycopperfeld
@hotmail.com
CopperfIeld
Presumably
they also need
reminding not
to stick wet
fngers in a plug
socket
Read
Copperfelds
blog at
pulsetoday.co.uk/
copperfeld
or follow him
on Twitter
@DocCopperfeld
Calm skin.
Peaceful night.
Applied regularly, the patient friendly formula of Diprobase
will hydrate, soothe and calm eczematous skin,
1
helping to reduce night-time itching and scratching.
Diprobase Prescribing Information
Please refer to the full SPC text before prescribing this product.
Adverse events should be reported. Reporting forms and information can be found at www.mhra.gov.uk/yellowcard.
Adverse events should also be reported to MSD (tel: 01992 467272)
Code: 02/15 DERM-1069551-0002 Date of preparation: February 2013
Reference: 1. Diprobase Summaries of Product Characteristics, accessed February 2013
Merck Sharp & Dohme Limited, 2013. All rights reserved.
Uses: Diprobase Cream and Ointment are emollients, with moisturising and
protective properties, indicated for follow-up treatment with topical steroids or in
spacing such treatments. They may also be used as diluents for topical steroids.
Diprobase products are recommended for the symptomatic relief of red, inamed,
damaged, dry or chapped skin, the protection of raw skin areas and as a pre-
bathing emollient for dry/eczematous skin to alleviate drying effects. Dosage: The
cream or ointment should be thinly applied to cover the affected area completely,
massaging gently and thoroughly into the skin. Frequency of application should be
established by the physician. Generally, Diprobase Cream and Ointment can be used
as often as required. Contra-indications: Hypersensitivity to any of the ingredients.
Side-effects: Skin reactions including pruritus, rash, erythema, skin exfoliation,
burning sensation, hypersensitivity, pain, dry skin and bullous dermatitis have been
reported with product use. Package Quantities: Cream: 50g tubes, 500g pump
dispensers; Ointment: 50g tubes, 500g tubs. Basic NHS Costs: Cream: 50g tube =
1.28; 500g pump = 6.32; Ointment: 50g tube = 1.28; 500g tub = 5.99 Legal
Category: GSL. Marketing Authorisation Numbers: Cream: PL 00025/0575;
Ointment: PL 00025/0574. Marketing Authorisation Holder: Merck Sharp &
Dohme Limited, Hertford Road, Hoddesdon, Hertfordshire, EN11 9BU, UK. PI Code:
DERM-1053797-0000 Date of Revision of Text: September 2012
20624 MSD HCP Sleep_Pulse Ad_Jan 13.indd 1 19/02/2013 09:02
NEW LAMA FOR COPD
Date of preparation: January 2013
1. Jones PW et al. Aclidinium Bromide in Patients with Chronic Obstructive Pulmonary Disease: Improvement in Symptoms and Health
Status in the ATTAIN Study. Poster presented at the American College of Chest Physicians Annual Congress, Honolulu, Hawaii, USA,
October 22-26, 2011. 2. Kerwin EM et al. COPD 2012, 9(2):90101. 3. EKLIRA GENUAIR Summary of Product Characteristics 2012.
4. Beier J et al. Thorax 2012, 67: A26-A27. 5. Karabis A et al. Poster presented at ISPOR 15th Annual European Congress, Berlin,
Germany, 3-7 November 2012. 6. Chrystyn H et al. Int J Clin Pract. 2012;66(3):309-17. 7. MIMS September 2012.
Adverse events should be reported. Reporting forms and information can be found at
www.mhra.gov.uk/yellowcard. Adverse events should also be reported to Almirall Ltd.
Active Ingredient: Each delivered dose contains 375 g aclidinium
bromide equivalent to 322 g of aclidinium. Each metered dose
contains 12.6 mg lactose monohydrateIndication: As a
maintenance bronchodilator treatment to relieve symptoms in
adult patients with chronic obstructive pulmonary disease
(COPD). Dosage and Administration: The recommended
dose is one inhalation of 322 g aclidinium twice daily. Consult
SmPC and package leafet for method of administration.
Contraindications, Warnings, etc: Contraindications:
Hypersensitivity to aclidinium bromide, atropine or its
derivatives, including ipratropium, oxitropium or tiotropium,
or to the excipient lactose monohydrate. Precautions: Should
not be used to treat asthma or for relief of acute episodes of
bronchospasm, i.e. rescue therapy. May cause paradoxical
bronchospasm. Re-evaluation of the treatment regimen should be
conducted if there is a change in COPD intensity. Use with caution
in patients with a myocardial infarction during the previous 6
months, unstable angina, newly diagnosed arrhythmia within
the previous 3 months, or hospitalisation within the previous
12 months for heart failure functional classes III and IV as per the
New York Heart Association. Consistent with its anticholinergic
activity, dry mouth has been observed and may in the long term
be associated with dental caries. Also, use with caution in patients
with symptomatic prostatic hyperplasia or bladder-neck
obstruction or with narrow-angle glaucoma. Patients with rare
hereditary problems of galactose intolerance, Lapp lactase
defciency or glucose-galactose malabsorption should not
take this medicine. Interactions: Although co-administration
with other anticholinergic- containing medicinal products is
not recommended and has not been studied; no clinical
evidence of interactions when taking the therapeutic dose has
been observed. Pregnancy and lactation: Aclidinium bromide
should only be used during pregnancy if the expected benefts
outweigh the potential risks. It is unknown whether aclidinium
bromide and/or its metabolites are excreted in human milk. The
beneft forthe breast-feeding child and long-term beneft of
therapy for the mother should be considered when making a
decision whether to discontinue therapy. Ability to drive and use
machines: The effects on the ability to drive and use machines
are negligible. The occurrence of headache or blurred vision may
infuence the ability to drive or use machinery. Adverse Effects:
Common: sinusitis, nasopharyngitis, headache, cough, diarrhoea.
Consult SmPC in relation to other side-effects. Legal Category:
POM Marketing Authorisation Number(s): EU/1/12/778/002
Carton containing 1 inhaler with 60 unit doses. NHS Cost:
28.60 (excluding VAT) Marketing Authorisation Holder:
Almirall S.A. General Mitre, 151 08022 Barcelona Spain.
Further information is available from: Almirall Limited,
1 The Square, Stockley Park, Uxbridge, Middlesex UB11 1TD, UK.
Tel: (0) 207 160 2500. Fax: (0) 208 7563 888. Email: almirall@
professionalinformation.co.uk
Date of Revision: 09/2012 Item code: UKACL1352 Eklira and
Genuair are both registered trademarks.
Eklira
Genuair
t
322 micrograms inhalation powder aclidinium bromide
Comparable effcacy to traditional
LAMA treatment with twice daily dosing
3-5
Sustained bronchodilation from day 1
1
Improves patients breathlessness
and health status
**
(vs. control)
1
Simple and easy-to-use device
3,5-7
15% annual cost saving vs. tiotropium
7
* Based on the cost of 1 Spiriva
Handihaler
vs. Eklira
Genuair
initiation at month1
Network meta-analysis and phase III study evaluation of
aclidinium vs. tiotropium
** Measured by St Georges Respiratory Questionnaire
Assumes use of 1 Spiriva
HandiHaler
and 11 reflls in 1 year
or 12 EKLIRA GENUAIR packs in 1 year
UKACL1332k
Around-the-clock COPD symptom
control, making a real difference
to patients lives
1-3
1
8
%
l
e
s
s
i
n
i
t
i
a
t
i
o
n
c
o
s
t
v
s
.
t
i
o
t
r
o
p
i
u
m
H
a
n
d
i
H
a
l
e
r
7
*
12081007A_PULSE_290x230_1332k.indd 1 29/01/2013 12:43
www.pulsetoday.co.uk Pulse March 2013 41
In THIS ISSue
c
l
I
n
I
c
a
l
Key questions
Type 2 diabetes
1.5 cpd HourS
page 42
practical genetics
cancer genetics
1 cpd Hour
page 48
How not to miss
necrotising fasciitis
page 50
The information
Bells palsy
page 44
plus...
picture quiz cutaneous manifestations of HIV
page 47 s
c
i
e
n
c
e
p
h
o
t
o
l
i
b
r
a
r
y
x
2
/
j
u
l
i
a
n
c
l
a
x
t
o
n
/
a
M
a
n
d
a
o
a
k
l
e
y
42 March 2013 Pulse www.pulsetoday.co.uk
Key questions
CliniCal
q
What is the current evidence on
prescribing aspirin 75mg daily in
patients with type 2 diabetes for
primary prevention?
a
The latest evidence and guidance
does not support the use of aspirin
for primary prevention in people with
diabetes.
NICE 2008 guidelines
1
suggested that
aspirin 75mg should be offered to
patients with diabetes aged over 50 with
a blood pressure above 145/90mmHg,
and to those younger than 50 with other
significant risk factors. But the evidence
base has changed since this guidance was
published new evidence has shown the
benefits of low-dose aspirin in primary
prevention in people with diabetes do
not exceed the risks, for example
gastrointestinal bleeding.
SIGN guidance published in March
2010
2
says that aspirin should not be used
in primary prevention.
q
Which class of antihypertensive
drugs should be used frst line in
patients with type 2 diabetes aged
over 55 years ACE inhibitors or
calcium channel blockers?
a
ACE inhibitors should be used first
line in patients with type 2 diabetes
aged over 55 years. The NICE guideline
update on type 2 diabetes
3
recommends
that an ACE inhibitor (or ARB, if ACE
inhibitor is not tolerated) should be the
first-line therapy. These agents lower
blood pressure and there is evidence that
they give renal protection. Patients with
diabetes on an ACE inhibitor (or ARB)
are less likely than patients taking either
nothing, or calcium channel blockers to
develop microalbuminuria or if they
already have it, this is less likely to
progress to frank proteinuria or
end-stage renal failure.
NICE diabetes recommendations do
not make any distinction between
patients over or under the age of 55 years.
This age recommendation comes from
the general NICE hypertension guidelines
which do not specifically cover people
with diabetes.
q
NICE advocates human rather
than analogue insulins frst line in
those with poor glycaemic control on
oral drugs, but many GPs are less
comfortable with human insulin than
analogue. Also, I understand that
insulin glargine is coming off patent
soon. Could you offer any pragmatic
advice on this?
Professor Roger Gadsby answers GP Dr David Russells
questions on prescribing aspirin, metformin, and human
and analogue insulin
a
NICE
3
recommends that for most
people with type 2 diabetes who
require insulin:
insulin therapy should be initiated
from a choice of a number of insulin
types and regimens
treatment should preferably begin with
human NPH insulin taken at bed-time or
twice daily according to need.
NICE
3
also recommends that long-
acting insulin analogues can be
considered as an alternative for patients:
who require assistance from a carer or
healthcare professional to administer
their insulin injections (NPH often needs
to be administered twice daily)
whose lifestyle is significantly
restricted by recurrent symptomatic
hypoglycaemia
who would otherwise need twice daily
basal insulin injections.
So, there are circumstances where
starting with an analogue basal insulin is
recommended, although NICE must have
felt that the evidence of benefit for basal
analogue insulin over NPH did not justify
the cost difference in most patients.
Insulin glargine is due to come off
patent in the next couple of years. We
will have to wait until generic long-acting
basal analogue insulins are launched to
see if their cost becomes similar to the
current NPH insulins.
Remember that NICE guidelines are
advisory, so if an individual prescriber
feels that their experience and expertise
is in initiating one type of basal insulin,
and that that insulin is the best one for
their patient, they have a reason and
defence for that clinical action.
q
Given the rarity of lactic acidosis,
at what level of renal impairment
should metformin be withdrawn? Our
local nephrologists have suggested
rather higher levels of creatinine and
lower eGFR than usually suggested.
a
Metformin is safe down to an eGFR
of 30 ml/min/1.73m
2
, but probably
with a dose reduction when the eGFR is
below 50.
The balance has to be drawn between
not denying people with mild to
moderate renal impairment the benefits
of taking metformin, and the perceived
increased risk of lactic acidosis if
metformin accumulates in patients with
severe renal impairment.
Research Ive been involved with due
to be published soon suggests that it is
fine to use metformin at full dose with an
eGFR at or above 50. It is safe to use it
1.5 CPD
HouRs
Go online to
complete this
article as a
CPD module
This module will
be available free
to all members of
Pulse Learning
until 14 March
pulse-learning.
co.uk
New this month
Go online to see
new Key questions
CPD modules on:
Hyperhidrosis
1 CPD HOuR
Pre-travel advice
1.5 CPD HOuRs
pulse-learning.
co.uk
type 2 diabetes
www.pulsetoday.co.uk Pulse March 2013 43
References
1 NICE. Type 2 Diabetes.
2008.CG66
2 SIGN. Management of
diabetes. 2010. SIGN 116
3 NICE. Type 2 diabetes
(rapid update of
glycaemic lowering
section of CG66). 2009.
CG87
4 Thanabalasingham G
and Owen KR. Diagnosis
and management of
maturity onset diabetes
of the young (MODY).
BMJ, 2011;343:837-842
5 Holman RR, Paul SK,
Bethel MA et al. 10-year
follow up of intensive
glucose control in type 2
diabetes. N Engl J Med,
2008;359:1577-1789
down to an eGFR of 30 but with
a maximum dose of 1g daily.
Metformin should only be used where
eGFR is below 30 with the agreement of
a specialist and where the risks and
benefits have been assessed and agreed
to be in favour of its use.
Q
What factors would make you
consider that a patient may not
have type 2 diabetes but may have
type 1 diabetes or maturity onset
diabetes of the young? How can we
make these alternative diagnoses?
A
In most cases, it is possible to
distinguish between type 1 and type
2 diabetes by the age at first presentation,
the symptoms at presentation, the
presence of ketonuria and the need for
insulin to control hyperglycaemia.
It can be difficult to differentiate
between type 1 and type 2 when diabetes
presents acutely but without ketosis
in adults.
It is wise to always consider the
possibility that such an individual might
have type 1 diabetes, and to follow them
very closely until it becomes clear that
they do have type 2 diabetes.
The genetic forms of diabetes (which
include maturity onset diabetes of the
young) tend to have a very strong
multigenerational family history.
Some people with maturity onset
diabetes of the young who present in
young adulthood may be wrongly
diagnosed as having type 1 diabetes.
Others may present under the age of 45
with apparent having type 2 diabetes, but
without features of insulin resistance.
The diagnosis is made by sending
samples for molecular genetic testing.
It is important to make the diagnosis of
maturity onset diabetes of the young as
sulfonylurea therapy is the effective
treatment for the most common forms,
and if the patient is using insulin therapy
it can be stopped.
4
Q
When should bariatric surgery be
considered in patients with type
2 diabetes? Patients whove had
successful bariatric surgery
sometimes appear to have their
diabetes cured their sugars
normalise to the extent that they can
stop their treatment. Are they still
diabetic?
A
The role of bariatric surgery as
a treatment for type 2 diabetes
requires more research and no definitive
consensus about its role has yet been
reached.
Obese people with type 2 diabetes who
have undergone bariatric surgery, and
who lose a lot of weight, may be able to
stop glucose-lowering medications and
may have HbA
1c
levels in the normal
range.
This can also happen after very
significant weight loss through dieting.
Diabetes in remission is the preferred
term, rather than cured, as diabetes is
likely to recur if the person regains
enough weight.
It is important to ensure that these
patients are still offered annual screening
for diabetes macrovascular and
microvascular complications as they will
continue to be at risk from these.
Q
Should glitazones ever be
initiated now in the UK given
their withdrawal for safety reasons
in other parts of the world?
A
NICE
3
recommends that glitazones
(pioglitazone is the only one
available in the UK) be considered as
second-line agents, with a DPP4 agent
as the other possible choice, to be
added to metformin where there is
a significant risk of hypoglycaemia
or its consequences.
This guideline also recommends that
a glitazone be considered as a possible
third-line agent to be added to metformin
plus sulfonylurea.
Rosiglitazone which was the other
glitazone launched in the UK was
withdrawn worldwide in 2010 because
of an increased risk of cardiovascular
ischaemic events.
There is evidence from a randomised
controlled trial and a number of
observational studies that pioglitazone
reduces the risk of cardiovascular
ischaemic events.
Evidence has emerged that there is
an association between pioglitazone use
and increased risk of bladder cancer.
A warning to this effect has been
issued by the regulatory authorities
in Europe, but they considered that
pioglitazone still had a place in therapy
and did not order its removal from the
market. Though it has been withdrawn
in France.
Pioglitazone came off patent nearly
12 months ago and its price has dropped
significantly, helping to support
cost-effectiveness discussions.
Q
How important is it to achieve
early good glycaemic control in
diabetes?
A
It is important to achieve early good
glycaemic control in patients who
are newly diagnosed with diabetes.
The follow-up evidence from the UK
Prospective Diabetes Study
5
suggests that
getting patients to an HbA
1c
of 7% and
keeping them there for as long as
possible reduces cardiovascular disease
events in the long term.
There is no benefit in getting people
with diabetes for 10 years or more down
from an HbA
1c
of 7.5% to 6.5% and it
may cause harm.
In observational studies the best
outcomes are obtained when people have
HbA
1c
levels in the 7% to 7.5% range.
Professor Roger Gadsby is a GP and
associate clinical professor at the
University of Warwick. Professor Gadsby
is GP lead for National Diabetes Audit and
primary care lead for NHS diabetes. He
was on the guideline development group
for the 2008 NICE diabetes guideline.
Dr David Russell is a GP in Darlington
Go to the online
version of this
article to
see three extra
Q&As on:
CVD risk
reduction
self-testing
oral treatment
pulsetoday.co.uk/
kq-diabetes
www.pulsetoday.co.uk 44 March 2013 Pulse
CliniCal
THE inFORMaTiOn
Bells
palsy
Mr Christopher
Skilbeck and
Mr Rupert Obholzer
advise on a case using
PUNs and DENs
The patients unmet needs (PUNs)
A 20-year-old woman who is otherwise
well and on no medication, presents with
a two-day history of weakness on the left
side of her face. She has self-diagnosed
Bells palsy which you confirm on
examination. Her eye on the affected side
is sore, though vision is normal. She has
discovered that some doctors advise
aciclovir because the palsy may be
caused by Herpes simplex virus. She
wants to know your view and whether
she should have a course of steroids.
The doctors educational needs
(DENs)
How common is Bells palsy and what are
the current theories of causation?
Bells palsy a partial or complete
idiopathic lower motor neurone facial
paralysis has an incidence of between
11 and 40 per 100,000 per year. Around
two-thirds of cases of acute facial
weakness are truly idiopathic. The peak
incidence is between 30 and 50 years of
age, with an equal male-to-female ratio.
The aetiology is unclear, but an
infectious origin is most likely, triggering
an immunological response which leads
to neuronal injury. HSV has been
implicated, but HSV type 1 can be isolated
from 86% of human geniculate ganglion
cells with no history of facial palsy.
How can the GP confidently exclude other
causes for this type of symptom?
The classical Bells palsy history is of
a short duration. Patients report pain
on the affected side, which may be
post-auricular. Subsequently, they
develop weakness that peaks within
48 hours. Slower onset, or progressive
weakness, suggests a more sinister cause.
Clinical examination should confirm
the lower motor neurone weakness. The
ears and neck, including the parotid
gland and facial skin, should be carefully
examined. An assessment of the patients
eye closure is mandatory. Finish with
a full cranial nerve examination. If this
reveals no other abnormalities, the
diagnosis is very likely to be Bells palsy.
What treatment should be offered? How
time-sensitive are these treatments?
Patients with clear or suspected Bells
palsy should be started on oral
corticosteroids as soon as possible after
onset, ideally within 72 hours. This
treatment improves outcomes, but there
is no additional benefit from antiviral
regimens, according to a trial that
compared antivirals with corticosteriods,
and we would not recommend them
1
.
The treatment arm of the study used
prednisolone as a single 25mg tablet,
taken twice daily for 10 days. There is no
evidence of benefit of steroids initiated
later than 72 hours, but we would
consider trying them up to two weeks.
Antiviral medication is mandated in
Ramsay-Hunt syndrome suggested by
vesicles around the pinna or in the
mouth, on the tongue or on the palate.
What potential ocular complications are
there? How can GPs prevent or treat them?
Patients with severe weakness and
incomplete eye closure may experience
corneal exposure, leading to drying and
trauma, and irreversible ulceration can
occur. So, in addition to pharmacological
treatment, eye care with lubrication is
appropriate taping at night and daytime
eye protection are advised.
What is the prognosis of Bells palsy, and
do certain patient groups have a worse
outlook than others? What are the possible
long-term complications?
Most patients with Bells palsy will
recover well, but up to 30% will have
a poor outcome with persistent facial
weakness and associated psychological
distress. One study showed 72% of those
treated with prednislone returned to
normal movement at 12 months. Those
who do not receive steriods can expect
a resolution rate of less than 60%.
Sometimes reinnervation of the target
muscles occurs in a haphazard way, and
synkinesis the involuntary movement
of one part of the face while attempting
to move another, for example the mouth
moving on tight eye closure may result.
Pregnancy appears to protect women
from Bells palsy, although pregnant
women who are affected seem to have
a worse prognosis. Poor prognosis is also
associated with complete paralysis, slow
recovery and older age. Idiopathic facial
palsy is recurrent in up to 15% of cases.
Care should be taken to exclude a middle
ear or skull base cause. Referral is
recommended for any patient where
clinical examination suggests another
cause, those with incomplete recovery
and when the palsy is recurrent.
Mr Christopher Skilbeck is an ENT/skull
base fellow and Mr Rupert Obholzer is
a consultant ENT/skull base surgeon at
Guys & St Thomas Hospitals, London
This article was produced with Facial
Palsy UK a new charity dedicated to
providing information and supporting
patients and their families. For more
information visit: facialpalsy.org.uk
References
1 Sullivan FM, Swan IRC,
Donnan PT et al. Early
treatment with
prednsiolone or aciclovir
in Bells palsy. N Engl J
Med 2007; 357:1598-1607
Further reading
Davenport RJ,
McKinstry B, Morrison
JM et al. Bells palsy: new
evidence provides a
definitive drug therapy
strategy. Br J Gen Pract
2009;59:569-70
Salinas RA, Alvarez G,
Daly F and Ferreira J.
Corticosteroids for Bells
palsy (idiopathic facial
paralysis). Cochrane
Database of Systematic
Reviews. 2010
Lockhart P, Daly F,
Pitkethly M et al.
Antiviral treatment for
Bells palsy (idiopathic
facial paralysis).
Cochrane Database of
Systematic Reviews.
2009
Patients with Bells palsy should be started on oral corticosteroids as soon as possible
s
c
i
e
n
c
e
p
h
o
t
o
l
i
b
r
a
r
y
Hot topics in
headache
2 CPD HoURs
pulse-learning.
co.uk
Recurrent VTE is three times more frequent in patients
with cancer versus patients without cancer
6
VTE can complicate the management of patients with
cancer and increase morbidity
79
Extended treatment of VTE with Fragmin
halves the relative risk of recurrent
DVT/PE versus VKA* in patients with solid tumours at 6 months
10
* Warfarin was used in all but two countries in the Fragmin
CLOT study.
10
HR: 0.48; 95% CI: 0.300.77; P=0.002; ARR: 8%.
10
ARR: absolute risk reduction. LMWH: low molecular weight heparin. NSTEMI: Non-ST
elevation myocardial infarction. VKA: vitamin K antagonists. VTE: venous thromboembolism,
including deep vein thrombosis (DVT) and pulmonary embolism (PE).
Date of preparation: November 2012. UK/FRA/12/0058. Page 1 of 2
Prescribing information, adverse event reporting
information and references can be found overleaf.
In addition, Fragmin
has a broad range of indications
with approved licences for:
Treatment of VTE
2
Surgical and medical thromboprophylaxis
3
Unstable angina and NSTEMI
4
Haemodialysis and haemoltration
5
Your VTE patients might be home but they may not be dry
Fragmin
is the only LMWH licensed for extended treatment
of symptomatic VTE and prevention of its recurrence in solid
tumour patients
1
66998-4 PFI_FRA 230x290 pulse Ad 2012_R2.indd 1 22/02/2013 12:48
Fragmin
is a registered trademark of Pzer Ltd. Date of preparation: November 2012. UK/FRA/12/0058. Page 2 of 2
FRAGMIN
(dalteparin sodium) ABBREVIATED PRESCRIBING
INFORMATION ALL PRESENTATIONS AND INDICATIONS (See Fragmin
Summary of Product Characteristics for full Prescribing
Information). Treatment of VTE Fragmin 7,500 IU, 10,000 IU, 12,500
IU, 15,000 IU, 18,000 IU single-dose syringes containing dalteparin
sodium 7,500 IU in 0.3 ml; 10,000 IU in 0.4 ml; 12,500 IU in 0.5 ml;
15,000 IU in 0.6 ml; 18,000 IU in 0.72 ml. Indication: Treatment of
venous thromboembolism (VTE) presenting clinically as deep vein
thrombosis (DVT), pulmonary embolism (PE) or both. Dosage and
Administration: By subcutaneous (s.c.) injection. Normal risk of
bleeding: single daily dose to match bodyweight: <46 kg 7,500 IU;
46-56 kg 10,000 IU; 57-68 kg 12,500 IU; 69-82 kg 15,000 IU;
83 kg 18,000 IU. Single daily dose should not exceed 18,000 IU.
Fragmin 10,000 IU/1 ml Ampoules containing 10,000 IU dalteparin
sodium in 1 ml. Fragmin 100,000 IU/4 ml Multidose Vial containing
100,000 IU dalteparin sodium in 4 ml with benzyl alcohol. Indication:
Treatment of venous thromboembolism (VTE) presenting clinically
as deep vein thrombosis (DVT), pulmonary embolism (PE) or both.
Dosage and Administration: By s.c. injection. Normal risk of bleeding:
Fragmin 200 IU/kg s.c. once daily. Single daily dose should not exceed
18,000 IU. Increased risk of bleeding: Fragmin 100 IU/kg s.c. twice daily,
up to a maximum total daily dose of 18,000 IU. For VTE treatment,
anticoagulant monitoring is generally not necessary. Simultaneous
anticoagulation with oral vitamin K antagonists can start immediately.
Continue Fragmin until prothrombin complex levels have decreased to
a therapeutic level usually at least 5 days of combined treatment. Legal
Category: POM. Basic NHS Prices: 10 prelled syringes: 7,500 IU/0.3 ml
42.34; 5 prelled syringes: 10,000 IU/0.4 ml 28.23; 12,500 IU/0.5 ml
35.29; 15,000 IU/0.6 ml 42.34; 18,000 IU/0.72 ml 50.82. For
10 ampoules: 10,000 IU/1 ml 51.22. For 1 Multidose Vial: 100,000 IU/4
ml 48.66. PL Numbers: 7,500 IU/0.3 ml 00057/0985. 10,000 IU/0.4 ml
00057/0976. 12,500 IU/0.5 ml 00057/0980. 15,000 IU/0.6 ml
00057/0981. 18,000 IU/0.72 ml 00057/0982. 10,000 IU/1 ml Ampoules
00057/0977. 100,000 IU/4 ml Multidose Vial 00057/0979. Surgical
Thromboprophylaxis Fragmin 2,500 IU/0.2 ml or Fragmin 5,000 IU/
0.2 ml single-dose syringes containing dalteparin sodium. Indication:
Peri- and post-operative surgical thromboprophylaxis. Dosage and
Administration: By s.c. injection. Moderate risk of thrombosis: Fragmin
2,500 IU s.c. 1-2 hours before surgery; thereafter 2,500 IU s.c. once daily
in morning until full ambulation (usually 5-7 days). High risk of
thrombosis: Fragmin 2,500 IU s.c. 1-2 hours before surgery; then again
8-12 hours later. Thereafter, 5,000 IU s.c. once daily in morning until full
ambulation (usually 5-7 days). Alternatively, 5,000 IU Fragmin s.c. on
evening before surgery, then 5,000 IU s.c. on each subsequent evening.
Prolonged thromboprophylaxis in hip replacement surgery: 5,000 IU
Fragmin s.c. on evening before surgery, then 5,000 IU s.c. on each
subsequent evening up to 5 weeks post-operatively. If Fragmin is to be
commenced post-operatively the rst dose of Fragmin (2,500 IU) should
be administered as soon as the perceived risk of bleeding is no longer
present. Legal Category: POM. Basic NHS Prices: 10 prelled syringes:
2,500 IU/0.2 ml 18.58; 5,000 IU/0.2 ml 28.23. PL Numbers:
2,500 IU/0.2 ml 00057/0983; 5,000 IU/0.2 ml 00057/0984. Medical
Thromboprophylaxis Fragmin 5,000 IU/0.2 ml single-dose syringes
containing dalteparin sodium. Indication: The prophylaxis of proximal
DVT in patients bedridden due to a medical condition, including, but not
limited to: congestive cardiac failure (NYHA class III or IV), acute
respiratory failure or acute infection, who also have a predisposing risk
factor for venous thromboembolism such as age over 75 years, obesity,
cancer or previous history of VTE. Dosage and Administration: 5,000 IU
s.c. once daily prescribed for up to 14 days. Legal Category: POM. Basic
NHS Prices: 10 prelled syringes 5,000 IU/0.2 ml: 28.23. PL Number:
00057/0984. Haemodialysis or Haemoltration Fragmin 10,000 IU/
1 ml or Fragmin 10,000 IU/4 ml Ampoules containing dalteparin sodium
10,000 IU in 1 ml and 10,000 IU in 4 ml. Indication: Prevention of clotting
in the extracorporeal circulation during haemodialysis or haemoltration,
in patients with chronic renal insufciency or acute renal failure. Dosage
and Administration: In chronic renal insufciency with no known
additional bleeding risk: Long-term haemodialysis or haemoltration
(more than 4 hours): Fragmin intravenous (i.v.) bolus injection 30-40 IU/
kg body weight, followed by an infusion of 10-15 IU/kg body weight/hour.
Short-term haemodialysis or haemoltration (less than 4 hours): as
above, or a single i.v. bolus injection of Fragmin 5,000 IU. For both long
and short-term haemodialysis and haemoltration the plasma anti-Factor
Xa levels should be within the range 0.5-1.0 IU/ml. In acute renal failure,
or patients at high risk of bleeding: i.v. bolus injection of Fragmin 5-10 IU/
kg body weight, followed by an infusion of 4-5 IU/kg body weight/hour
and plasma anti-Factor Xa levels should be within the range 0.2-0.4 IU/
ml. Legal Category: POM. Basic NHS Prices: For 10 ampoules: 10,000
IU/1 ml 51.22. 10,000 IU/4 ml 51.22. PL Numbers: 10,000 IU/1 ml
00057/0977. 10,000 IU/4 ml 00057/0978. Unstable Angina Fragmin
Graduated Syringe 10,000 IU/ml Solution for Injection single-
dose syringe containing dalteparin sodium 10,000 IU in 1 ml. Fragmin
10,000 IU/1 ml Ampoules containing 10,000 IU dalteparin sodium in
1 ml. Fragmin 7,500 IU single-dose syringes containing 7,500 IU in
0.3 ml. Indication: Unstable angina and non Q-wave myocardial
infarction administered concurrently with aspirin. Extended Use beyond
8 days in patients awaiting angiography/revascularisation. Dosage and
Administration: Duration of therapy; acute phase: 120 IU/kg body weight
administered s.c. 12 hourly for up to 8 days. Maximum dose is 10,000
IU/12 hours. Extended phase: beyond 8 days, for those awaiting
revascularisation, treatment is recommended to be given until the day of
the invasive procedure in a xed dose of 5,000 IU (women <80 kg and
men <70 kg) or 7,500 IU (women 80 kg and men 70 kg) 12 hourly.
Treatment until the revascularisation procedure but not for more than 45
days. Maximum dose 10,000 IU/ 12 hours. Legal Category: POM. Basic
NHS Prices: For 5 single-dose graduated syringes: 10,000 IU/1 ml
28.23. For 10 ampoules: 10,000 IU/1 ml 51.22. For 10 prelled
syringes: 7,500 IU/0.3 ml 42.34. PL Numbers: Graduated Syringe
10,000 IU/ml Solution for Injection single-dose syringe 00057/0986.
10,000 IU/1 ml Ampoules 00057/0977, 7,500 IU single-dose syringes
00057/0985. Extended treatment of Symptomatic Venous
Thromboembolism in patients with Solid Tumours Fragmin 5,000
IU, 7,500 IU, 10,000 IU, 12,500 IU, 15,000 IU, 18,000 IU single-dose
syringes containing dalteparin sodium 5,000 IU in 0.2 ml; 7,500 IU in
0.3 ml; 10,000 IU in 0.4 ml; 12,500 IU in 0.5 ml; 15,000 IU in 0.6 ml;
18,000 IU in 0.72 ml. Indication: Patients with solid tumours: Extended
treatment of symptomatic VTE and prevention of its recurrence. Dosage
and Administration: Administer Fragmin 200 IU/kg total body weight s.c.
once daily for month 1 (rst 30 days of treatment), followed by a Fragmin
dose of approximately 150 IU/kg, s.c., once daily for months 2-6 using
xed-dose syringes. Maximum daily dose should not exceed 18,000 IU.
In cancer patients with body weight <40 kg at time of venous
thromboembolic event, Fragmin should not be used for extended
treatment of symptomatic VTE and prevention of its recurrences due to
lack of data (refer to SPC for dosing tables). Renal failure: In the case of
signicant renal failure, dened as a creatinine clearance <30 ml/min,
the dose of Fragmin should be adjusted based on anti-Factor Xa activity
(refer to SPC for further information). In the case of chemotherapy-
induced thrombocytopenia, the Fragmin dose should be interrupted/
reduced (refer to SPC for further information). Legal Category: POM.
Basic NHS Prices: 10 prelled syringes: 5,000 IU/0.2 ml 28.23;
7,500 IU/0.3 ml 42.34; 5 prelled syringes: 10,000 IU/0.4 ml 28.23;
12,500 IU/0.5 ml 35.29; 15,000 IU/0.6 ml 42.34; 18,000 IU/0.72 ml
50.82. PL Numbers: 5,000 IU/0.2 ml 00057/0984. 7,500 IU/0.3 ml
00057/0985. 10,000 IU/0.4 ml 00057/0976. 12,500 IU/0.5 ml
00057/0980. 15,000 IU/0.6 ml 00057/0981. 18,000 IU/0.72 ml
00057/0982. All Presentations Use in Children: Safety and efcacy not
established. Use in Elderly: No dose adjustment needed.
Contraindications: Known hypersensitivity to Fragmin or other low
molecular weight heparins and/or heparins; history of conrmed or
suspected immunologically mediated heparin induced thrombocytopenia
(Type II); acute gastroduodenal ulcer; cerebral haemorrhage; known
haemorrhagic diathesis; serious coagulation disorders, septic
endocarditis; injuries to and operations on the central nervous system,
eyes or ears. Known hypersensitivity to benzyl alcohol for Multidose Vial
presentation. In patients receiving Fragmin for treatment rather than
prophylaxis, local and/or regional anaesthesia in elective surgical
procedures is contra-indicated with the higher treatment doses of
dalteparin. Dalteparin should not be used in patients who have suffered a
recent (within 3 months) stroke unless due to systemic emboli. In cancer
patients with body weight <40 kg at time of venous thromboembolic
event, Fragmin should not be used for extended treatment of symptomatic
VTE and prevention of its recurrences due to lack of data. Warnings and
Precautions: Do not administer by intramuscular (i.m.) route. Due to risk
of haematoma, other medicines given i.m. should be avoided for 24 hours
if the dose of dalteparin exceeds 5,000 IU. Caution in conditions with
increased risk of bleeding; e.g. following surgery or trauma, haemorrhagic
stroke, severe liver or renal failure, thrombocytopenia or defective
platelet function, uncontrolled hypertension, hypertensive or diabetic
retinopathy, patients receiving concurrent anticoagulant/antiplatelet
agents and in elderly patients 80 years may be at an increased risk
of bleeding complications within therapeutic dosage ranges where
careful clinical monitoring is required. Caution should also be observed at
high dose treatment with dalteparin especially in patients treated for
acute DVT, PE or unstable coronary artery disease. Monitoring of anti-Xa
levels is not usually required but should be considered for certain special
patient populations such as paediatrics, those with renal failure, those
who are very thin or morbidly obese, pregnant or at increased risk for
bleeding or rethrombosis. Close monitoring is recommended in the case
of low and changing physiologic renal function e.g. neonates. If a
transmural myocardial infarction occurs in patients where thrombolytic
treatment might be appropriate, this does not necessitate discontinuation
of treatment with Fragmin but might increase the risk of bleeding.
Monitor plasma potassium before and during Fragmin if risk of
hyperkalaemia. Careful observation and care needed for patients having
spinal or epidural anaesthesia. Not recommended for use in the
prevention of valve thrombosis in patients with prosthetic heart valves.
Limited data are available regarding the safety and efcacy of
antithrombotic therapy in patients with primary or metastatic tumours of
the brain who develop concurrent thromboembolic events. There is a risk
of fatal intracranial bleeding with use of anticoagulation in this category
of patients. Therefore, if treatment with Fragmin is considered it should
be monitored closely with regular re-assessment of the status of tumour
involvement of the brain and other individual risks. Thrombocytopenia,
should it occur, usually appears within 3 weeks following the beginning
of therapy. It is therefore recommended that the platelet counts are
measured before starting treatment with Fragmin and monitored closely
in the rst 3 weeks and regularly thereafter during treatment (refer to SPC
for more information). Patients with severely disturbed hepatic function,
signicant renal failure or chemotherapy-induced thrombocytopenia may
need a dosage reduction and should be monitored accordingly. Dalteparin
cannot be used interchangeably (unit for unit) with unfractionated
heparin, other low molecular weight heparins, or synthetic
polysaccharides. The 100,000 IU/4 ml Multidose Vial contains benzyl
alcohol so must not be used in premature or newborn babies. Benzyl
alcohol may cause toxic reactions in infants and children up to 3 years
old. Other formulations without benzyl alcohol are available. Drug
Interactions: Care with agents affecting coagulation/platelets and
NSAIDs (refer to SPC for more information). Pregnancy and Lactation:
Dalteparin should be used during pregnancy only if clearly needed, and
caution should be exercised when prescribing to pregnant women (refer
to SPC for more information). The Multidose Vial contains benzyl alcohol
therefore should not be used in pregnancy. Epidural anaesthesia during
childbirth is absolutely contraindicated in women who are being treated
with high dose anticoagulants. Not recommended for use in pregnant
women with prosthetic heart valves. Limited data are available for
excretion of dalteparin in human milk. A risk to the suckling child cannot
be excluded. A decision on whether to continue/discontinue breast-
feeding or to continue/discontinue therapy with Fragmin should be made
taking into account the benet of breast-feeding to the child and the
benet of Fragmin therapy to the woman. Side Effects: Commonly
reported side effects include reversible non-immunologically-mediated
thrombocytopenia (Type I), haemorrhage (bleeding at any site),
subcutaneous haematoma at injection site, transient elevation of liver
transaminases (ASAT, ALAT). Other side effects include: hyperkalaemia,
allergic reactions, urticaria, pruritus, skin necrosis, transient alopecia,
pain at injection site, immunologically mediated heparin-induced
thrombocytopenia (Type II, with or without associated thrombotic
complications-arterial and/or venous thrombosis or thromboembolism).
(Refer to SPC for information on other side effects and post-marketing
experience). Marketing Authorisation Holder: Pzer Limited, Ramsgate
Road, Sandwich KENT, CT13 9NJ, United Kingdom. Further information is
available on request: Pzer Limited, Walton Oaks, Dorking Road,
Tadworth, Surrey KT20 7NS, United Kingdom. Date of preparation:
October 2012. Company Ref: FR 6_3
Adverse events should be reported.
Reporting forms and information can be found
at www.mhra.gov.uk/yellowcard.
Adverse events should also be reported
to Pzer Medical Information on 01304 616161
References: 1. Fragmin SmPC [Extended Treatment in Oncology (5000/18,000 IU syringes), October 2012]. 2. Fragmin SmPC [Treatment of VTE (7500/18,000 IU syringes, 10,000 IU/1ml ampoules, 100,000 IU/4ml Multidose
Vial), October 2012]. 3. Fragmin SmPC [Medical and Surgical Thromboprophylaxis (2500 IU and 5000 IU syringes), October 2012]. 4. Fragmin SmPC [Unstable Angina (Graduated syringe 10,000 IU/ml solution for injection,
10,000 IU/1ml ampoule, 7500 IU), October 2012]. 5. Fragmin SmPC [Haemodialysis/Haemoltration (10,000 IU/1ml & 10,000 IU/4ml ampoules), October 2012]. 6. Prandoni P et al. Blood. 2002;100:34843488. 7. Debourdeau
P et al. Support Care Cancer. 2008;16:13331341. 8. Khorana AA et al. Blood. 2008;111:49024907. 9. Levitan N et al. Medicine. 1999;78:285291. 10. Lee AY et al. N Engl J Med. 2003;349: 146153. Please refer to the
eMC website for full details of Fragmin SmPCs.
66998-4 PFI_FRA 230x290 pulse Ad 2012_R2.indd 2 22/02/2013 12:48
Answers
www.pulsetoday.co.uk Pulse March 2013 47
picture quiz
clinical
cutaneous manifestations of HiV
These four patients with HIV presented with cutaneous complaints can you make
the diagnoses from the pictures and case histories below?
1 M o l l u s c u m c o n t a g i o s u m
M o l l u s c u m c o n t a g i o s u m i s a v i r a l
i n f e c t i o n a l m o s t u n i v e r s a l l y
e n c o u n t e r e d i n s e x u a l l y a c t i v e p e o p l e
w i t h H I V . M o s t l e s i o n s a r e s e l f - l i m i t i n g
t y p i c a l l y w h i t e , p i n k , o r s k i n - c o l o u r e d
u m b i l i c a t e d , r a i s e d p a p u l e s . H I V -
p o s i t i v e p a t i e n t s m a y d e v e l o p g i a n t
l e s i o n s . M o l l u s c u m c o n t a g i o s u m i n H I V
p a t i e n t s i s h a r d t o t r e a t t h e m o s t
w i d e l y u s e d m e t h o d s a r e c u r e t t a g e
a n d c r y o s u r g e r y .
2 S e b o r r h o e i c d e r m a t i t i s
S e b o r r h o e i c d e r m a t i t i s c o n s i s t s
o f s l i g h t l y i n d u r a t e d e r y t h e m a t o u s
p a t c h e s u s u a l l y w i t h a b u n d a n t g r e a s y
s c a l e . I t u s u a l l y c a u s e s m o d e r a t e
d i s c o m f o r t , b u t i n H I V - i n f e c t e d p a t i e n t s
h a s a p r o p e n s i t y t o b e m o r e s e v e r e
w i t h t h i c k e r s c a l e . T h e r a p y c e n t r e s
a r o u n d t o p i c a l a n t i f u n g a l a n d
c o r t i c o s t e r o i d p r e p a r a t i o n s . T r e a t m e n t
o f H I V - a s s o c i a t e d s e b o r r h o e i c
d e r m a t i t i s m i r r o r s t h a t o f o r d i n a r y
s e b o r r h o e i c d e r m a t i t i s .
3 K a p o s i s s a r c o m a
K a p o s i s s a r c o m a i s t h e m o s t f r e q u e n t
n e o p l a s t i c d i s o r d e r i n H I V - i n f e c t e d
p a t i e n t s a n d i s a n A I D S - d e f n i n g
c o n d i t i o n . E a r l y l e s i o n s a p p e a r a s
v i o l a c e o u s o r y e l l o w i s h - g r e e n
e c c h y m o t i c m a c u l e s a n d p a t c h e s t h a t
m a y s i m u l a t e t r a u m a , i n s e c t b i t e
r e a c t i o n s , o r d e r m a t o f b r o m a s . I n t i m e ,
t h e s e e n l a r g e o r b e c o m e c o n f u e n t .
4 E r y t h r a s m a
E r y t h r a s m a i s a c u t a n e o u s b a c t e r i a l
i n f e c t i o n g e n e r a l l y p r e s e n t i n g a s
a r e d , s c a l y p l a q u e w i t h w e l l
d e m a r c a t e d b o r d e r s . T h e l e s i o n m a y
a d v a n c e a n d c h a n g e f r o m r e d t o
b r o w n w i t h a n a r e a o f c e n t r a l c l e a r i n g .
I t i s u s u a l l y n o t s e l f - l i m i t i n g a n d m a y
l a s t w e e k s o r m o n t h s . E r y t h r o m y c i n i s
u s u a l l y e f f e c t i v e .
This patient has noticed the gradual development
of these papular lesions on his fank over the last
few months.
This bluish-red lesion has been slowly enlarging on this
mans upper abdomen over the last month or two. A
couple of other lesions similar but smaller seem to
be developing on his back.
This man has been aware of this non-itchy unilateral
rash in his left axilla for many weeks. A combination
steroid/antifungal cream prescribed by his GP has made
no difference.
Despite using moisturisers and a mild steroid cream, this
man has been unable to cure this scaly rash on his face.
There is a similar rash on his scalp and behind his ears.
These cases are
taken from
Cutaneous
Manifestations of
HIV Disease by
Clay J Cockerell
and Antoanella
Calame. ISBN
9781840761429
(Manson
Publishing);
available
from:www.
mansonpublishing.
com/colour_
handbooksand all
good booksellers
priced 115.00
Key questions
on HIV
1.5 CPD HourS
pulsetoday.co.uk/
kq-hiv
1 2
3 4
www.pulsetoday.co.uk 48 March 2013 Pulse
Increasing public awareness of a genetic
predisposition to some cancers is leading
to family history being frequently raised
with GPs.
This article discusses two patients
with a family history of bowel and other
cancers including risk assessment and
management of those in different risk
categories.
The next article in this series will
consider family history of breast and
ovarian cancer this will be published
on pulsetoday.co.uk on 8 March.
Case one
Mrs H attends soon after her mothers
death. Her mother had been
diagnosed with bowel cancer several
years earlier at the age of 62. Mrs H is
concerned about her risk.
Most cancers are sporadic, resulting
mainly from environmental factors
such as smoking and HPV or due to
chance. Hereditary cancer syndromes,
which usually follow an autosomal
dominant inheritance pattern, only
account for around 5-10% of cancers.
Family history is the main tool in
identifying families at high risk young
age, multiple cancers of the same site,
and multiple family members affected
are suggestive of an underlying cancer
syndrome.
The British Society of
Gastroenterology (BSG) guidelines
1
outline identification and surveillance of
those at above-population risk of
colorectal cancer, and local guidelines
may also exist. Because Mrs H only has
one relative affected at over 50 years of
age, and there is no family history of
associated cancers (see table opposite,
top), then she is likely to be at normal
population risk.
Give Mrs H reassurance and
information specifically about red flag
symptoms for colorectal cancer.
If the family history alters, risk may
alter and the patient should return to
seek further advice.
Advise patients to return if they
develop red flag symptoms.
Encourage patients to take part in the
NHS Bowel Cancer Screening
Programme every two years from the
age of 60-69.
Offer lifestyle advice about weight,
smoking, alcohol intake and exercise.
Genetics GPSI Dr Judith Hayward advises on how to manage patients with a family
history of bowel and other cancers the rest of her series will follow online
Cancer genetics
s
c
i
e
n
c
e
p
h
o
t
o
l
i
b
r
a
r
y
1 CPD
HOUR
Go online to
complete this
article as a
CPD module
this module will
be available free
to all members of
pulse learning
until 14 March
pulse-learning.
co.uk
CliniCal
new seRies will continue online
PRaCtiCal genetiCs
www.pulsetoday.co.uk Pulse March 2013 49
Reducing intake of red meat
particularly processed will lower risk.
Signpost to further support and
information, for example Macmillan:
macmillan.org.uk/cancerinformation
and Cancer Research UK:
cancerresearchuk.org.uk.
Mrs H reattends a few months later
because her brother had rectal
bleeding shortly after her mother
died, and has now been diagnosed
with bowel cancer at the age of 42.
Mrs H now has two first-degree relatives
affected and is at above-population risk.
She should be referred to a regional
genetics service, local gastroenterology
unit or a community family history
clinic, depending on whats available
locally.
Surveillance would be offered with
regular colonoscopies. The age at which
they start and their frequency would
depend on risk category.
The BSG guidelines
1
suggest that
individuals at low to moderate risk are
offered a colonoscopy at age 55, or as
soon as they present after the age of 55.
Those at high to moderate risk are
usually offered colonoscopies every five
years from the age of 50-75.
Mrs H then returns again, having
found out that her mothers sister
died of endometrial cancer.
Mrs H now has three relatives affected
by colorectal and related cancers.
Any patient in this situation should be
offered referral to the regional genetics
service.
Ovarian and endometrial cancer can
occur within another cancer syndrome
hereditary non-polyposis colorectal
cancer (HNPCC). The same management
principles apply to HNPCC as to other
hereditary cancer syndromes increased
surveillance, and prophylactic
oophorectomy and hysterectomy as
HNPCC carries a 10% and 50% lifetime
risk of ovarian and endometrial cancer
respectively. The table above outlines the
risks of specific cancers and suggested
surveillance.
Diagnostic testing is often possible if
there is a living family member affected
with cancer if a mutation is found in an
HNPCC-related gene then predictive
testing can be offered to family members
who are currently unaffected.
Mrs Hs brother attends his regional
genetics service for diagnostic testing
to identify any mutation in HNPCC-
related genes. Before he is seen,
Mrs H, now aged 38, returns with
abdominal bloating and intermittent
loose stools. Although her symptoms
are clinically more suggestive of IBS,
a fast-track referral is made in view of
the family history. Colonoscopy
reveals a malignant tumour of the
ascending colon.
This case highlights that patients with
significant family histories are at
increased risk of developing cancer, even
if symptoms suggest a non-malignant
cause. It is important to ask about family
history in patients with symptoms which
arent red flags a significant family
history lowers the threshold for further
investigation.
Case two
Mr C aged 28 was referred
routinely to general surgery with
painless rectal bleeding suggestive
of haemorrhoids. His symptoms
appeared typical, but the GP was
concerned about his risk of polyps
after asking about family history.
Mr Cs mother had multiple colorectal
polyps and had a preventative
colectomy in her 40s. His
sigmoidoscopy revealed a colorectal
polyp, so a full colonoscopy is
performed. This reveals several
further colorectal polyps.
A family history of colorectal polyps may
be significant some types of polyp can
undergo malignant change. There are
several hereditary polyposes, the most
significant being familial adenomatous
polyposis. Untreated, this carries
virtually a 100% lifetime risk of colorectal
cancer. Individuals may not have a family
history of cancer, but identifying them is
crucial in view of their elevated risk, and
they should be offered referral to
regional genetics services. Annual
colonoscopy should be initiated from
puberty, with prophylactic colectomy
indicated, usually before the age of 30.
This article has summarised
management of patients with a family
history of some common cancers. But,
many other cancer types can occur
within cancer syndromes, and discussion
of these is beyond the scope of this
article. Have a high index of suspicion of
any family history where cancers occur
at a young age, or several relatives are
affected particularly with the same type
of cancer.
Dr Judith Hayward is a GPSI in genetics in
Bradford, and works with the Yorkshire
Regional Genetics Service
This article has been written with the
help of Dr Julian Adlard, consultant in
cancer genetics at Yorkshire Regional
Genetics Service.
Above-population risk of colorectal cancer
Number of Cancer type Minimum degree Average age
family members of relationship of diagnosis
affected
1 Colorectal First-degree Over 50
relative
2 Colorectal First-degree Any age
relatives (includes
both parents)
3 Colorectal First- or second Any age
(although up to degree relatives
two may be related (at least one must
cancers*) be frst-degree)
*Related cancers include endometrial, ovarian, small bowel, renal or bladder, biliary tract,
thyroid, or sebaceous adenoma or bowel polyps.
Risks and surveillance in patients with HNPCC
Cancer type Approximate Suggested surveillance
lifetime risk
Colorectal cancer 80% (men) colonoscopy every one to two years
40% (women) from age 25
Gastric cancer 10% gastroscopy every two to three years
from age 50-75
Endometrial 50% (women) none symptom awareness and
cancer vigilance
Ovarian cancer 10% (women) currently not recommended
Urinary tract 1-4% No current consensus: an example may
cancer be annual surveillance from age 40 via
renal ultrasound, intravenous urogram
+/- cystoscopy.
Reference
1 Cairns SR, Scholefield
JH, Steele RJ et al, on
behalf of the British
Society of
Gastroenterology, and
the Association of
Coloproctology for Great
Britain and Ireland.
Guidelines for colorectal
cancer screening and
surveillance in moderate
and high risk groups
(update from 2002).
Gut 2010;59:666-90
Further reading
NICE . Familial Breast
Cancer. October 2006.
CG41
Rafi I and Spicer J.
Genetics and Primary
Care. Chapter 5: Cancer
Genetics Radcliffe
Publishing, 2007
Coming up online
Each week, a new
article in the
practical genetics
series will be
published online.
Look out for:
Cancer genetics:
breast and ovarian
cancers
Ethical issues in
genetics
Antenatal
screening
Discussing
family history
pulsetoday.co.uk/
clinical
New series will continue online
practical geNetics
50 March 2013 Pulse www.pulsetoday.co.uk
how not to miss
clinical
Adverse events should be reported. Reporting forms and information can
be found at www.mhra.go.uk/yellowcard. Adverse events should also be
reported to the Sano drug safety department on 01483 505515.
GBIE.GLA.12.11.03a. Date of preparation: December 2012
Lantus
(insulin glargine) is indicated for the treatment of diabetes mellitus in adults, adolescents and
children of 2 years or above. Please consult the summary of product characteristics before prescribing,
particularly in relation to side effects, precautions and contra-indications. Legal category: POM. MA
holder: Sano Aventis Deutschland GmbH, D-65926 Frankfurt am Main, Germany. Further information
is available from: Sano, One Onslow Street, Guildford, Surrey, GU1 4YS. Tel: 01483 505515 or the
Sano Diabetes Care Line 08000 35 25 25. Information about this product, including adverse reactions,
precautions, contra-indications and method of use can be found at www.diabetesmatters.co.uk
THE YOU KNOW
101333_Lantus_The_1_You_Know_PULSE_145x230_LANDSCAPE_ad_with_bleed_v4.indd 1 21/01/2013 11:58
necrotising
fasciitis
Emergency medicine consultant Dr Adrian
Boyle discusses the signs, and pitfalls in
diagnosing necrotising fasciitis
Worst outcomes if missed
Death between 20 and 40% of people
with necrotising fasciitis die, despite
surgery.
Disfigurement early diagnosis and
treatment reduces mortality and the
disfigurement from surgery. Delays to
surgery increase the risk of amputation.
Epidemiology
There are about 500 cases of
necrotising fasciitis in the UK each year.
Necrotising fasciitis is more common
in patients with diabetes, chronic
hepatitis and malignancy particularly
leukaemia people who inject drugs and
those who are immunosuppressed.
Necrotising fasciitis can occur because
of infected pressure sores.
It is rare in childhood, but there is an
association with varicella infection.
A GP should expect to see at least one
case in their career.
Diagnosis is frequently made late, after
multiple presentations.
Symptoms and signs
The classic symptoms of necrotising
fasciitis are rarely present initially so
distinguishing necrotising fasciitis from a
M
a
n
d
a
o
a
k
l
e
y
www.pulsetoday.co.uk Pulse March 2013 51
Enjoy in-depth investigation
and analysis of the big
developments in
general practice, plus:
go direct to further
information online
link up your reading with
relevant online CPD
watch our video features
in full
beat the post and read Pulse
as soon as its published
The Pulse iPad app is here
Read Pulse magazine on your iPad
with our free interactive app
All registered members of PulseToday or Pulse Learning can use the app. Simply use your Pulse username and password to log into the app and the latest issue of Pulse will appear
in your Newsstand. If youre not already a member, its free and takes just a couple of minutes to register pulsetoday.co.uk/register
Download the app at
pulsetoday.co.uk/iPad
iPad app 199x130.indd 1 22/02/2013 11:08
cellulitis can be difficult in the early
phases of the disease. Early symptoms
are non-specific:
fever
pain out of proportion to the clinical
findings
inability to use the affected limb.
The limbs are most commonly
affected and the perineum is also
a common site, but any part of the body
can develop necrotising fasciitis.
In patients with fever, clinical
suspicion may be aroused by something
being not quite right for a diagnosis
of cellulitis. The classic cyanotic and
bullous skin changes may only appear
late in the process, but the site of
infection may appear unusual. The pain
may seem too severe for cellulitis, despite
relatively mild skin signs, or there may
be overlying sensory loss. Pain is caused
by tissue necrosis, but the nerves can also
be infarcted as perforating vessels to the
tissues are thrombosed by the necrotic
process. This can cause exquisite pain
and tenderness, but also sensory loss to
the overlying skin. The patient may seem
disproportionately unwell for the degree
of skin involvement. The progression of
the illness can suggest the diagnosis the
patient may seem relatively well initially,
but will deteriorate despite antibiotic
therapy. Crepitus and haemorrhagic
blisters are a late sign.
In patients presenting with pain alone,
the severity of pain and absence of
trauma may suggest the diagnosis.
Differential diagnosis
Symptoms of necrotising fasciitis are
initially similar to the much more
common and benign cellulitis. Patients
with severe musculoskeletal pain may
suggest that their pain is caused by an
assumed or trivial injury.
Investigations
There are no useful investigations that
can be done in primary care necrotising
fasciitis is mainly a clinical diagnosis.
Where there is doubt, prompt surgical
exploration at hospital is probably best,
though MRI or CT scans can be used.
If necrotising fasciitis is suspected,
the patient should be referred as an
emergency. Patients are usually initially
cared for by general surgeons
or plastic surgeons, depending on
local services.
Dr Adrian Boyle is a consultant in
emergency medicine at Addenbrookes
Hospital in Cambridge and an honorary
senior research fellow at Cambridge
University.
Further reading
Sultan HY, Boyle AA and Shepherd N. Necrotising
fasciitis. BMJ, 2012;345:e4274
Five key questions to ask
1 Can you walk or
use the limb?
Inability to use
the limb is
suggestive
of necrotising
fasciitis.
2 Are there any
patches of
numbness?
This would
indicate whether
any sensory
nerves have been
infarcted.
3 Where exactly
is the pain worst?
Pain which is
greatest slightly
distant to an area
of cellulitis is
suggestive
of necrotising
fasciitis.
4 Is the pain
around a wound?
Uncomplicated
wound infections
are not usually
very painful.
5 Are you
feverish and
unwell?
Patients are
usually toxic.
Five red herrings
1 Patients may
attribute limb
pain to a minor
or non-existent
injury.
2 The skin signs
may be relatively
mild at frst.
3 Patients who
inject drugs
often present
without systemic
signs.
4 Patients may
look well in the
initial stages
of the disease,
which can last
a few days.
5 Lymphangitis
is unusual in
necrotising
fasciitis this
usually suggests
a different
diagnosis.
www.pulsetoday.co.uk 52 March 2013 Pulse
s
c
i
e
n
c
e
p
h
o
t
o
l
i
b
r
a
r
y
x
4
pulse-learning.co.uk
Latest
modules
Also new
this month
Guideline debrief
Fertility
2 CPD hours
this case-based learning module uses
primary care case histories to update
you on the Gp-relevant sections of the
new nice guideline
The information
Patellofemoral pain syndrome
0.5 CPD hours
a concise, practical guide to the
pathophysiology, underlying causes,
diagnosis and management of this
catch-all label for knee pain
Key questions
Pre-travel advice
1.5 CPD hours
a travel health specialist answers a Gps
questions including advice on last-
minute vaccines, altitude sickness and
malaria prophylaxis
CKD in primary care
When renal function takes a dip
1 CPD hour
a simple and useful guide to
management of sudden deterioration
of eGFr
Dr Tarun Sharma
Key questions
Asthma
1.5 CPD hours
Very useful module with lots of
practical tips to improve asthma
management
Dr Andreas Photiou
The information
rosacea
0.5 CPD hours
Very good, practical tips useful in
primary care
Dr Krishna Jamuna
Clinical casebook
Addiction
1.5 CPD hours
crisp, clear and concise advice for
front-line use
Dr David Oram
hot topics
End-of-life care
2 CPD hours
incredibly useful round-up of the
palliative care developments relevant
to us in primary care
Dr Matthew Hughes
Practice business
Managing an online appointment
service
1 CPD hour
Very informative, its an eye opener
Dr Maurice Williams
Keep up with all the new modules and online-
only clinical articles by signing up to the weekly
Pulse Education newsletter
pulsetoday.co.uk/emails
Souvenaid
is a Food for Special Medical Purposes for the dietary management
of early Alzheimers disease and must be used under medical supervision.
*
Unique, patented combination of nutrients: Omega 3 fatty acids (DHA & EPA), Uridine
monophosphate, Choline, Phospholipids, B vitamins and other cofactors which are all required to
make neuronal membranes
3
.
1. Scheltens P, et al. J Alzheimers Dis, 2012
2. Scheltens P, et al. Alzheimers Dement. 2010 Jan;6(1):1-10.e1.
3. Kennedy EP Weiss SB (1956) J Biol Chem 222(1):193-214
Souvenaid
contains a unique, patented combination of
nutrients
*
which have been shown to improve memory
in early Alzheimers disease
1,2
. It is a well-tolerated,
1,2
convenient (125ml) once-daily drink.
Souvenaid is based on more than 10 years of research.
To find out more information go to
www.souvenaid.com
A new
approach
in early
Alzheimers
disease.
Doublebase Gel Isopropyl myristate 15% w/w, liquid paraffin 15% w/w. Uses: Highly
moisturising and protective hydrating gel for dry skin conditions. Directions: Adults, children
and the elderly: Apply direct to dry skin as required. Doublebase Dayleve Gel Isopropyl
myristate 15% w/w, liquid paraffin 15% w/w. Uses: Long lasting, highly moisturising and
protective hydrating gel for dry skin conditions. Directions: Adults, children and the elderly:
Apply direct to dry skin morning and night, or as often as necessary.
Contra-indications, warnings, side effects etc: Please refer to SPC for full details before
prescribing. Do not use if sensitive to any of the ingredients. In the unlikely event of a reaction
stop treatment. Package quantities, NHS prices and MA numbers: Doublebase Gel: 100g
tube 2.65, 500g pump dispenser 5.83, PL00173/0183. Doublebase Dayleve Gel: 100g tube
2.65, 500g pump dispenser 6.29, PL00173/0199. Legal category: P
MA holder: Dermal Laboratories, Tatmore Place, Gosmore, Hitchin, Herts, SG4 7QR. Date of
preparation: November 2012. Doublebase and Dayleve are trademarks.
R
x
by name for formulation of choice
Doublebase Dayleve
TM
Gel Doublebase
TM
Gel
Isopropyl myristate 15% w/w, liquid paraffin 15% w/w
Original emollient Gel
Emolliency like an ointment
Cosmetic acceptability like a cream
Enhanced emollient Gel
Highly emollient long lasting protection
As little as twice daily application
No other emollients perform quite like them!
Doublebase The difference is in the GELS
www.dermal.co.uk
H
ig
h
o
il c
o
n
te
n
t
+
g
ly
c
e
r
o
l
H
ig
h
o
il &
g
ly
c
e
ro
l
c
o
n
te
n
t
+
p
o
v
id
o
n
e
J
o
u
r
n
a
l
:
P
u
l
s
e
D
e
r
m
a
l
:
D
o
u
b
l
e
b
a
s
e
J
a
z
z
D
u
o
A
d
S
i
z
e
:
2
9
0
x
2
3
0
m
m
B
l
e
e
d
:
3
m
m
S
u
p
p
l
y
a
s
h
i
-
r
e
s
P
D
F
J
o
b
N
o
:
2
2
8
9
1
Adverse events should be reported. Reporting forms and information can be found at
www.mhra.gov.uk/yellowcard. Adverse events should also be reported to Dermal.
22891_DB Jazz Duo Ad_Pulse_AW:1 20/12/12 14:42 Page 1
www.pulsetoday.co.uk Pulse March 2013 55
Pulse Live is a new must-attend
event offering an annual update
for all GPs covering your
practice, your clinical work,
and your career
By attending Pulse Live you can:
Get up to speed with the clinical,
financial and policy developments
you need to know about
Share ideas and experiences with
hundreds of GP colleagues
Earn 14 CPD CREDITS for two
days attendance (or seven for
one day)
You can debate the big issues
around clinical care and the future of
your profession, put your questions
to the experts, or appear on our
soapbox to share a gripe or a success
with your peers.
Pulse Live will help you make the
most of your working hours
and cope with this years QOF
and contract challenges.
Do come and join us, wed love
to see you there. Book now
through the Pulse Live website
pulse-live.co.uk
Your one-stop annual update
Its your event
Professor David Haslam, former chair
and president of the RCGP and chair
designate of NICE, will chair both days
of Pulse Live.
He will open the conference with
a talk entitled At the heart of the NHS,
looking at where general practice fits
into the new NHS.
About Pulse Live, he says: The most
important people there will be the
delegates themselves, GPs who are
working at the coalface. The programme
has been built around their real world.
Is the NHS wasting
millions on statins?
Is the NHS wasting precious funds on
primary prevention of cardiovascular
disease or is it making good,
evidence-based use of GPs time
and taxpayers money?
Delegates will vote on
clinical evidence presented on
both sides at the Pulse Live Big
Debate.
GP debater Dr Malcolm
Kendrick, author of The
Great Cholesterol Con,
will go head to head
with Dr Terry
McCormack, a GP in Whitby with
a special interest in cardiology, who
will put the case in favour of using
statins for primary prevention.
Which way will your vote go?
A comprehensive
clinical update
Clinical sessions at Pulse Live will update
you on key areas of practice,
summarising new research, helping with
common dilemmas and giving you tips to
put into practice straight away.
On day one, the clinical stream will
include recognising dementia, reducing
gastroenterology referrals, the coil in
emergency contraception, dermatology
treatment and referral and key areas to
get right in end-of-life care.
On the second day,
clinical sessions will
include whats new in
diabetes, 10 tips on
serious mental
illness, four ways to
make a difference in
ENT, musculoskeletal
update, 10 tips for better care of
multimorbidity, and whats new in COPD.
How to cope with
2013 QOF changes
Proposed QOF changes from April 2013
mean that GP practices are going to have
to take a more selective approach.
Dr Gavin Jamie, a GP in Swindon and
founder of the QOF Database, will advise
you on the law of diminishing returns
and how to cope with the new world of
the QOF.
His session will cover new indicators
and changes to thresholds and timings.
He will also look at the business case
which targets should your practice
prioritise and which are not worth
chasing?
THE NATIONAL CONFERENCE FOR GENERAL PRACTICE | 30 APRIL 1 MAY | HILTON METROPOLE, BIRMINGHAM
56 March 2013 Pulse www.pulsetoday.co.uk
Plenary sessions
Pulse Live Big Debate Are GPs all heading for burnout?
Pulse Live Clinical Debate Is the NHS wasting millions on primary prevention?
Sessional GP stream
How to set up and survive as a locum
Chambers a real alternative to partnership
Plenary sessions
Pulse Live Big Discussion Where does general practice fit into the NHS of the future?
Pulse Live Big Interview Editor Steve Nowottny puts your questions to Professor Malcolm
Grant, chair of the NHS Commissioning Board
Plus in the Pulse Live Hub Skills workshops, Soapbox, speakers area, refreshments and exhibition
Highlights from the
Pulse Live programme
QOF How the new world of
the QOF affects you and
which targets to prioritise
Nursing homes Improving
the way that GPs and homes
work together
Practice team dilemmas
Managing human resources
effectively in straitened times
Diabetes Whats new in
screening and therapeutic
agents?
Musculoskeletal Quick
wins for common problems
and new QOF indicators
Serious mental illness
10 tips including crisis
management
ENT Four ways to make
a difference
Multimorbidity 10 tips for
better care
COPD Whats new,
including telehealth
Traditional general
practice Is the cottage
industry model fit for the
future?
Where to go next? How to
develop your career in the
new NHS
Digital health Technology
and social media tips and
pitfalls for GPs
Efficiency How to make
better use of your time
Six key threats to practices
from April 2013 and how to
avoid them
Maximising revenue
Optimising your income and
keeping an eye on your
cashflow
Reducing emergency
admissions Mission
impossible or an achievable
goal for the average practice?
Dementia Case finding and
meeting the new DES
Dermatology 10 key points
on treatment and referral
Gastroenterology Five
ways to reduce your referrals
Emergency contraception
The case for the coil
Cardiovascular Update on
key challenges
End-of-life care Three key
areas to get right
Legal panel How to avoid
a career-ending complaint
Commissioning Whats in
it for you and your practice?
Competitor or colleague?
How practices should work
together to benefit
themselves and their patients
Burnout and stress
Prevention and how to cope
Day 1
30 April
Day 2
1 May
Additional
programme
topics are
being
conrmed
all the
time see
updates at
pulse-live.
co.uk/
programme
www.pulsetoday.co.uk Pulse March 2013 57
Pulse Live key speakers
Rt Hon Stephen
Dorrell MP
Chair of the House of
Commons health select
committee
Dr Richard Vautrey
GP in Leeds and deputy chair
of the GPC
Professor
Malcolm Grant
Chair, NHS Commissioning
Board
Dr Richard
Fieldhouse
GP in Chichester and chief
executive of the National
Association of Sessional GPs
(NASGP)
Dr David Carson
Director, Primary Care
Foundation, and former
GP and DH adviser on
emergency care
Dr Stephen Brown
GP in Buckinghamshire and
GPSI in ENT
Professor
Stewart Mercer
GP and professor of primary
care research, Institute of
Health and Well-being,
University of Glasgow
Dr Elizabeth
England
GP in Birmingham with a
special interest in mental
health, and senior clinical
lecturer in primary care
mental health, University of
Birmingham
Dr Kartik Modha
GP in London and founder
of Tikos GP Group
Richard Apps
Partner, RSM Tenon
accountants
Dr Pauline
Brimblecombe
GP and GPSI in community
gynaecology, Cambridge
Dr Hilary Pinnock
Reader with the Allergy and
Respiratory Research Group,
University of Edinburgh, and
GP in Whitstable, Kent
For the
full list of
speakers
see the
Pulse Live
website
pulse-live.
co.uk
www.pulsetoday.co.uk 58 March 2013 Pulse
Pulse Live is your event
Heres how you can get involved
How to book: see the insert in this
edition of Pulse or go online to
pulse-live.co.uk
Apply for a place
on the Pulse Live
Soapbox
If theres an issue related to
your work as a GP that you
want to get off your chest, we
want to hear from you.
The issue you raise might
be a gripe about clinical
guidelines, prescribing policy,
the financial squeeze on GPs
or the future of clinical
commissioning. Or maybe
you have a nugget of advice
thats worked for you that you
want to celebrate and share
with colleagues.
The GPs who submit the
best ideas will get a slot on
the Pulse Live Soapbox, and
everyone who applies will get
a free place to attend the event.
Email your ideas to
pat.anderson@pulse
today.co.uk
Send in your
questions for the
Pulse Big Interview
Pulse editor Steve Nowottny
will put your questions to
Professor Malcolm Grant,
chair of the NHS
Commissioning Board in the
final session of Pulse Live.
Perhaps you are wondering
how much power GPs will
really have in the new world
of clinical commissioning.
You might want to quiz him
on the Francis Inquirys call
for GPs to police the quality
of hospital care. Or maybe
youre upset about the
prospect of your local CCG
constitution being imposed
on your practice.
Email your questions and
the best will be put to
Professor Grant on the
Pulse Live stage.
steve.nowottny@pulse
today.co.uk
Come and meet the
Pulse editorial team
Group editor Jo Haynes and
Pulse editor Steve Nowottny
will be at the event and ready
to chat about Pulses online,
print and live content.
We want to hear what
matters to you, so we can
ensure we meet your needs
through our websites,
magazine and events.
Dr Penny Newman will use the Soapbox
to talk about women in medicine
Professor Malcolm Grant will face
questions from GPs
Steve Nowottny, editor of Pulse, wants
to hear your ideas and opinions
MOVICOL
Liquid, Orange Flavour, concentrate for oral solution. Abbreviated Prescribing
Information. REFER TO FULL SUMMARY OF PRODUCT CHARACTERISTICS (SmPC) BEFORE
PRESCRIBING. Presentation: A clear, concentrated liquid, which is diluted in water to make an
orange avoured drink. Each 25 ml of MOVICOL Liquid is diluted in 100 ml of water before use and
contains the following active ingredients: 13.125 g macrogol (polyethylene glycol) 3350, 178.5 mg
sodium hydrogen carbonate, 350.7 mg sodium chloride and 46.6 mg potassium chloride. Dosage and
administration: Adults, adolescents and the elderly: 25 ml diluted in 100 ml of water 1-3 times daily
in divided doses, according to individual response. For extended use, the dose can be adjusted down to
1 or 2 doses per day, each consisting of 25 ml diluted in 100 ml of water. Extended use may be necessary
in patients with severe chronic or resistant constipation, secondary to multiple sclerosis or Parkinsons
Disease, or induced by regular constipating medicine, in particular opioids and antimuscarinics. A course
of MOVICOL Liquid treatment does not normally exceed 2 weeks, but can be repeated if required.
Children (below 12 years): not recommended. See MOVICOL Paediatric Plain. Contra-indications:
Intestinal perforation or obstruction due to structural or functional disorders of the gut wall, ileus
and severe inammatory conditions of the intestinal tract, such as Crohns disease, ulcerative colitis
and toxic megacolon. Hypersensitivity to the active substances or any of the excipients. Warnings
and precautions for use: If patients develop any symptoms indicating shifts of uids/electrolytes
MOVICOL Liquid should be stopped immediately. MOVICOL Liquid contains 8.125 mmol of sodium in
each diluted dose of 125 ml and should be considered when administered to patients on a controlled
sodium diet. MOVICOL Liquid contains benzyl alcohol. Do not exceed the maximum recommended daily
dose. Interactions: There is a possibility that the absorption of concomitantly administered medication
could be transiently reduced. Pregnancy and lactation: There is insufcient data on use in pregnancy
and lactation, and should only be used if considered essential. Undesirable effects: Reactions
related to the gastrointestinal tract are the most common and include: abdominal pain, abdominal
distension, nausea, dyspepsia, vomiting, diarrhoea, atulence, borborygmi and anal discomfort. Allergic
reactions, including anaphylactic reaction, angioedema, dyspnoea and skin reactions can occur. Other
effects can include electrolyte disturbances, headache and peripheral oedema. Licensing and legal
category: Legal Category: UK P, IE Prescription-only. Cost: 500 ml UK 4.45, IE 7.71. MA numbers:
PL20011/0007, PA 1336/2/4. For further information contact: Norgine Pharmaceuticals Limited,
Norgine House, Moorhall Road, Hareeld, Middlesex, UB9 6NS. Telephone: +44 1895 826606. E-mail:
medinfo@norgine.com MOVICOL
is a registered trademark of the NORGINE
group of companies.
Date of preparation/revision: MO/3141/NOV/12.
UK
Adverse events should be reported. Reporting forms and information can be
found at www.mhra.gov.uk/yellowcard. Adverse events should also be reported
to Medical Information at Norgine Pharmaceuticals Ltd on 01895 826606.
Ireland
Adverse events should be reported to Medical Information at Norgine
Pharmaceuticals on +44 1895 826606.
Reference:
1. Attar A et al. Gut 1999; 44: 226-230.
MO/3213/JAN/13
For the treatment of chronic constipation
macrogol 3350, sodium hydrogen carbonate,
sodium chloride, potassium chloride
www.MOVICOL.co.uk
Blends proven efcacy
1
with fast-mix convenience
MV631_Movicol Liquid_230x290_Pulse_3213.indd 1 03/01/2013 3 Jan 09:42
60 March 2013 Pulse www.pulsetoday.co.uk
Identify
the work
you are not
funded to
undertake
Dr Nigel
Watson
Ten Top Tips
Our expert panel of GPs advises on how to get ready for the
contract changes, CQC registration and the CCG handover
preparing for
April 2013
y
o
u
r
p
r
A
c
T
i
c
e
Identify and reduce excessive
workload
1
All NHS providers of care are
suffering from rising workload and
financial restrictions and to
manage this, many are offloading work
onto GPs. Many practices have reached
saturation point and are struggling to
meet the needs of their registered
population. With major changes to the
GMS contract planned for April, partners
need to audit their existing workload to
discover sources that they feel might be
inappropriate or excessive. Identify the
work that you are not funded to
undertake and then discuss whether this
can be stopped always remembering
your professional responsibilities to your
patients.
Dr Nigel Watson is chair of the GPCs
commissioning and service development
subcommittee, chief executive of Wessex
LMCs and a GP in the New Forest
Prepare for a tougher QOF
2
There are radical changes
proposed for the QOF in the 2013/4
contract. It will become much
more difficult to achieve QOF points and
achieving the top quartile will be very
challenging. Practices will have to
prioritise work.
We have done two things at my
practice. We took a detailed look at the
proposed changes and discussed how
best to achieve QOF points when the new
contract is finalised. We plan to aim for
a broad spread of QOF points without
aiming for the top quartile in most cases.
We also bought an automated blood-
pressure monitor for the waiting room,
which has reduced the burden on staff
time in terms of blood pressure readings
needed for the QOF. We expect it to have
paid for itself in the next year or two.
Dr Adam Jenkins is vice-chair of Ealing,
Hammersmith and Hounslow LMC and
a GP in Greenford, west London
Draw up a 12-month fnancial plan and
put a freeze on hiring new staff
3
Practices should aim to sustain
themselves financially. Before
April, partners and practice
managers should check cash-flow
arrangements. Keep cash in reserve if
you can, and anticipate any impact from
the loss of the MPIG from 2014 onwards.
Staffing is every practices major
outgoing, so dont recruit any new staff
or partners until April. Long-term
commitments leave practices lumbered
if income goes down it is better to be
short-staffed for a few months.
Dr Sella Shanmugadasan is chair of Tower
Hamlets LMC and a GP in Shoreditch,
east London
Negotiate a lease agreement to fx
your service charges
4
In north-east London, a large
number of practices operate out
of healthcare centres, dont have a
contract with the PCT and have disputed
their service charge. Many partnerships
have fallen behind on payments. Its hard
to calculate the service charge but even
harder to challenge invoices if theres no
agreement. We dont know how NHS
Property Services (PropCo) is going to
operate or calculate service charges,
but we cant wait around to find out.
Dr Sella Shanmugadasan
Review all practice policies ahead
of CQC visits
5
GPC guidance on CQC compliance,
which we have been following at
my practice, suggests you review
policies. Then make sure all GPs and staff
know the policies and use them. Our
practice manager takes the lead but
weve also appointed people as leads in
different areas for example, the nurses
lead on infection control. We have also
set up an intranet site so that the policies
and procedures are in one place. We
explained to staff that CQC inspections
are part of an ongoing process. Keep
reviewing policies regularly and give staff
the confidence theyll need when the
inspector knocks.
Dr Richard Vautrey is deputy chair of the
GPC and a GP in Leeds
Ensure compliance with
CQC standards
6
By all means take forward your
plans for the CQC by updating
policies and procedures, training
staff, setting up systems for ongoing
notifications to the CQC, and so on. But
concentrate mainly on ensuring you
meet the necessary standards. If you are
www.pulsetoday.co.uk Pulse March 2013 61
GPs should
help CCGs
to plan
resources
for new
services
Dr Deborah
Colvin
struggling with some of them, prepare
plans to tackle problem areas, with
a realistic timescale and implementation
plan. This will prove to your CQC
inspector you are taking any issues
seriously.
Dr Sobhi Sadek is a GP in Northampton
Ensure your CCG resources GPs
for key work
7
If local commissioners want to run
a new service, GPs should help
them plan resources. In our area
the CCG wanted to run a new records
service for palliative care patients, so we
suggested ways it could be run and
resourced by the CCG through general
practice. Communication and
engagement are key to the success of new
initiatives, and the capacity of partners to
commit to services outside core work.
Dr Deborah Colvin is chair of City and
Hackney LMC and a GP in Hackney,
east London
Research how your practice will be
affected by local cuts and rationing
8
General practice, as ever, will be
expected to pick up the slack and
the bill when cuts are made. We
need to learn to trust what we know and
be prepared to fight hard for it.
This means keeping in touch with
local commissioning strategies, paying
attention to CCG communications and
reading commentaries from other
agencies. We need to be able to respond
to top-down impositions through
lobbying, petitioning the public and
learning about platforms for public
communication. Developing
relationships with local, trade and
national media and employing PR
experts will be key skills. We need also to
forge alliances with local councils as
highlighted in the Lewisham hospital
campaign where the mayor waded in.
Dr Andy Field is a GP in York
Prepare for cuts to local
enhanced services
9
Keep an eye on what is happening
to local enhanced services. Most
will fall under the control of CCGs,
but some will be commissioned (or paid
for) by the local authority, with CCGs or
the NHS Commissioning Board involved
in their detail. The risk is that funding for
some LESs will be stopped. If that is the
case, stop doing the work and raise the
issue with your CCG and LMC. They may
relaunch a LES, or make interim
payments for you to continue the work
while they decide whether to sustain it.
There is a clear opportunity to
renegotiate LESs where they have been
poorly funded or run under onerous
conditions. But if practices are not robust
in their approach to delivery and pricing,
they could find themselves delivering
more and more for less and less. Do your
research and plan which services to
launch, lobby for and pitch for.
Dr John Ashcroft is a vice-chair of
Derbyshire LMC and a GP in Ilkeston
Get to grips with the Any Qualifed
Provider model
10
From April 2013 it will be
up to CCGs to decide when
and where to use AQP as
a commissioning tool. Some practices
will want to bid for new AQP contracts,
but they must be fully aware of the terms.
AQP contracts are based on
competition, not price. The award for
a successful contract is based on the
national tariff. These contracts vary
from the LESs. AQP funding is paid
retrospectively based on the number of
referrals. Even if its a good service, if its
not used there might be less return on
your investment. In that respect, theyre
unlike LESs where you can plan the
finance youll get for undertaking them.
Preparing a pitch takes 40-50 hours or
longer. You will need to invest in staff,
equipment and other resources. You may
also need to rely on co-operation with
secondary and community care. Id
recommend partners look at what AQP
contracts will be available in future, and
research the opportunities and risks.
Dr George Rae is a GPC member and a GP
in Newcastle-upon-Tyne
Go online to
complete CPD
modules on AQP
contracts,
managing your
cash fow and
revalidation
pulse-learning.
co.uk g
e
t
t
y
www.pulsetoday.co.uk 62 March 2013 Pulse
finance diary: March
your practice
As commissioning begins to take shape
ahead of the handover to CCGs in April,
there are increasing opportunities for
GPs to tender for services across a
locality and to bid to run other practices.
It is important to consider the type of
organisation you want to constitute for
the business from the outset.
Tax considerations
Where a business is run through a
limited company or community-interest
company (CIC), the companys profits are
subject to corporation tax at 20% on
profits below 300,000 and currently
24% at the full rate (although this will be
reduced to 21% from April 2014). This is
favourable compared to a partnership or
limited liability partnership (LLP), where
the income coming in as the top slice of
a GPs personal income is subject to
income tax at 45% above 150,000 and
60% on taxable income between
100,000 and 118,410 in 2013/14.
However, if the profits from a limited
company are going to be drawn out as
dividends, then higher-income tax rates
will apply to shareholders who are
higher-rate taxpayers. Income tax and
employers and employees National
Insurance contributions will apply to
directors salaries, making the total tax
charge much higher than would be paid
by a partner or self-employed individual.
Where any spouses or partners who
are basic-rate or non-taxpayers are to be
brought in as shareholders, they should
subscribe for shares from the outset.
Dividends covered by the personal
allowance or basic rate tax are then not
subject to any additional income tax.
Commercial considerations
A limited company, CIC or LLP can be
seen to be more independent than putting
the new business through the main
medical partnership and can provide
a joint venture vehicle if two partnerships
are launching a combined bid. However,
with any new entity, the pre-qualification
questionnaire will require evidence of
financial support and it may be necessary
to introduce capital, whereas an existing
partnership would already have
a financial track record and capital base.
An LLP is effectively a hybrid being,
treated for accounting purposes as an
independent entity, in the same way as
a company with accounts that have to be
on public record at Companies House.
For tax purposes, its members are taxed
as individuals on the profits earned,
regardless of whether they are
distributed or not, in the same way as
partners in a partnership. An LLP does
give limited liability, which can be
attractive in a riskier business.
A CIC is a limited company but it is
also a social enterprise with restrictions
on the profits that can be withdrawn by
the shareholders. This does not prevent
directors remuneration being fully paid
for the services provided by the directors.
Given the reinvestment in the business of
the surpluses for the benefit of patients,
this can give an advantage over
a profit-making company in a tender.
If any shareholders are not doctors,
nurses, practice managers or other
members of the NHS family, then the
company will not qualify as an employing
authority, in which case employees
income would not be superannuable.
This may be advantageous for GPs who
are concerned about the pension cap, but
could be a disincentive for staff. Similarly
an LLP cannot have NHS employing-
authority status.
Valerie Martin-Long is a partner at the
specialist medical accountants PKF, and
can be contacted on 01483 564646 or
valerie.martin-long@uk.pkf.com
Article developed
in association
with
Setting up a new business entity
Valerie Martin-Long on how GPs bidding to run services can best organise their business
Pulse retains
editorial control
of this content
how to avoid becoming
a dysfunctional practice
With tough times ahead, it is vital practices pull together and partners delegate
effectively. Bob Senior advises on the warning signs of problems in store
Tough times lie ahead and teamwork will
be essential if practices are to ride out the
storm. Dysfunctional practices, where
GPs fail to delegate effectively or where
partners fall out, will only make a bad
situation worse.
Unfortunately I have noted an
increasing number of practices where
solicitors have been called in to sort out
partnership disputes (usually at great
expense) or where profits have fallen so
much that partners are deserting the ship.
I have noticed three common signs of
trouble, so if your practice is showing
them, now is the time to change.
GPs who micromanage
Although responsibility for patient care
ultimately rests with the doctors, GPs
have to work as part of a team. Clear
expectations must be established of what
will be done by each team member,
training given, and robust processes
established to ensure work is completed.
GPs should not be permanently
checking up on staff. Nurses need to be
trusted to operate within their remit and
practice managers should be allowed to
get on with running the practice.
Partners not talking to each other
In a busy practice it is not uncommon for
partners to comment that they have no
time to talk to colleagues. This can be
overcome with effort, perhaps by moving
practice meetings occasionally from the
traditional lunchtime slot to first thing in
the morning or in the evening. Unless
partners devote time to the practice they
could find it collapses around them.
But if partners are not talking to each
other because they have fallen out, this
must be resolved. If it isnt, things go
downhill quickly and all partners feel the
effects. In my experience, if partners are
unable to patch things up, one of them
needs to leave the practice promptly.
Allowing the situation to drag on will
mean solicitors have to get involved
further down the line.
No succession planning
Many GPs are struggling to cope with
what is happening now, let alone plan for
the future. But with many now in their
50s and young doctors changing their
attitudes to partnership, practices need
to tackle succession planning now.
Bob Senior is chair of the Association of
Independent Specialist Medical
Accountants and head of medical services
at RSM Tenon
Go online to read
previous Bob
Senior columns
including advice
on managing
premises costs
and preparing for
next years tax
return
pulsetoday.co.uk/
fnancediary
www.pulsetoday.co.uk Pulse March 2013 63
Your practice
Dilemma
One of the GP partners at your
practice sits on the CCG board, while
another fronts a local GP provider
organisation that is planning to bid
for contracts. You are concerned that
the practices internal relationships
might be put under strain during the
bidding process and particularly if
the board does not award contracts
to the partners organisation. How
should you manage this?
Dr Mark Gaffney
The CCG board partner
cannot have any say in
decisions about the provider
How to deal with this will
depend on the individual
characters, but the provider
organisation partner needs
to understand the CCG
board partner cannot have any say in
board decisions in relation to the
provider. I would have an open
discussion with the provider partner and
explain my concerns and expectations.
All GPs on CCGs are potentially
conflicted, simply by their independent
contractor status and ability to develop
outside interests. It becomes more
complex when board members belong to
an external commercial enterprise. That
person may have expert knowledge,
which would be foolish to ignore, but
how do you ensure impartiality?
There are only so many GPs in the UK.
Those with the drive to be entrepreneurs
are likely to be the same people who will
make the boards a success. How do we
harness that? The Committee for
Standards in Public Life published the
seven Nolan Principles as core working
values for anyone who serves the public:
selflessness, integrity, objectivity,
accountability, openness, honesty and
leadership. I would add another
principle for conflicted CCG board
members: absence. They should be
excluded from conflicted items at board
meetings but asked for input at seminar
level where no decisions are taken.
Dr Mark Gaffney is a co-founder and joint
managing director of East Sussex Out
Patient Services and a GP in Eastbourne
Dr Ken Aswani
Recognise that GPs will be
involved in different areas
of work
The partners should have
a full discussion in the
practice to ensure any
adverse fallout is minimised.
The CCG board member
would have to declare a conflict of
interest in any procurement where their
partners organisation is bidding. This
means they are likely to be excluded from
the process.
The partner who leads the provider
organisation will need to accept the CCGs
decision without worrying it was
influenced by their partner. They should
not apply influence to the CCG board
member or other CCG board members
that may be interpreted as unfair.
The other partners will need to
understand the CCG board member must
act on behalf of all its population and
practices, and cannot favour an
individual practice. The lay member of
the CCG, on behalf of the board, will need
to have governance systems to ensure
conflicts of interest do not compromise
decision-making.
As the two partners have conflicts
of interest it is important to have
appropriate partnership agreements,
particularly if there are any financial
arrangements. This would include the
extent to which a partner can have other
provider interests and how these may
financially affect the practice. Additional
time partners spend on outside provider
interests has to be negotiated. CCG
governance and the individuals
professional duty to maintain probity
should be respected, but GPs will be
involved in different areas of work, and
this should not discourage innovation.
Dr Ken Aswani is the medical director at
Waltham Forest Federated GP Consortium
and a GP in Leytonstone
Lynne Abbess
The decision lies outside
the practice it is for the
board to take
Management of conflicts
will become an essential
part of the new NHS.
However in the present
situation, there is nothing
for the practice itself to manage.
The decision is for the CCG board to
take. If there is discussion about the
award of the contract to the GP provider
organisation of which the fellow partner
is a member, the CCG board member
should remove themselves while the
decision is taken.
It is important to distinguish the role
a partner plays outside the practice from
the partnership business. In this case,
the decision has nothing to do with the
partnership. If it is understood the CCG
board member/partner is unable to
influence the decision, that should
prevent difficulties within the practice.
It is also important that partners
appreciate their responsibility lies with
the partnership. If an external activity
presents a conflict, then they will need
to decide which way to jump. It is not
reasonable to expect the other partners
to put up with the challenges from one
GPs external interest.
Lynne Abbess is a partner at Hempsons
solicitors
Now go online to
read this months
other practice
dilemmas:
A Muslim patient
presents after her
brother threatens
her with honour-
based violence
pulsetoday.co.uk/
HBV-dilemma
Should you offer
NHS treatment to
self-funding IVF
patients?
pulsetoday.co.uk/
IVF-dilemma
a confict of interest
between partners
One GP is on the CCG board, the other runs a provider. Three experts advise on
how to avoid a damaging rift within the practice
a
l
a
M
y
64 March 2013 Pulse www.pulsetoday.co.uk
photo essay
your practice
1 Surgery
opening.
Normally
a 7.30am start,
reviewing the
morning
appointments.
2 First
vaccinations
for this baby at
eight weeks old.
3 Home visit. This
patients carer
had been worried
about a sore leg,
but the patient
just needed
reassurance.
4 Arriving for
an A&E shift.
5 The patient
on the trolley
needed a log
roll to clear her
c-spine.
6 Trying to
establish why
this patient had
collapsed at
home.
7 Having a badly
needed fve-
minute break.
View the full series
See all 32 pictures
from this photo
essay online
pulsetoday.co.uk/
weinstein
1
www.pulsetoday.co.uk Pulse March 2013 65
In the documentary photo series
Country Doctor, published in Life
magazine in 1948, photojournalist
W Eugene Smith captured the working
life of a family doctor in Colorado.
Six decades later, photographer
Giovanni Tait and Dr David Weinstein
undertook a similar exercise.
Dr Weinstein works most of the week
as a GP in Brighton, but spends Friday
afternoons as an A&E middle-grade
doctor. I was beginning to feel burnt
out in primary care, he explains.
The balance keeps me sane.
Mr Tait was struck by how his photo
essay echoed the original: Fundamentally
the job has hardly changed.
pulsetoday.co.uk/weinstein
Dr David
Weinstein
A GP and photographer explain the idea
behind their remake of an iconic photo essay
that followed a family doctor in the 1940s
2 3
4
5 6
7
www.pulsetoday.co.uk 66 February 2013 Pulse
online
your practice
Editors
choice
From the
latest
practice
business
and
working
life
articles
online
Better end-of-life care
Dr Damian Patterson on how his practice
got gold-standard accreditation
pulsetoday.co.uk/GSF-casestudy
A GP for the homeless
Dr Nigel Hewett explains why he chose
to work with this vulnerable group
pulsetoday.co.uk/nigel-hewett
Reducing workload
Dr Masood Nazir makes 10 suggestions
to save time on admin and meetings
pulsetoday.co.uk/saving-time
Online appointments
1 CPD hOuR Dr Osman Bhatti explains
how to enable online booking
pulsetoday.co.uk/onlineappointments
Last-minute QOF tips
Dr Simon Clay covers exception coding
to help practices gain maximum points
pulsetoday.co.uk/lastminute-qof
Software to cut errors
Dr Sarah Rodgers guide to a new
plug-in to cut script errors
pulsetoday.co.uk/PINCER-guide
a
l
a
M
y
x
2
/
g
e
t
t
y
/
j
u
l
i
a
N
C
l
a
x
t
O
N
x
2
Gps prefer
pulse learning
96
%
94
%
91
%
83
%
rate Pulse
Learning higher
than any other
CPD site
would
recommend
Pulse Learning
to their GP
colleagues
say Pulse
Learning has
changed their
day-to-day
practice
have already
decided to
renew their
premium
membership
Based on a survey of 732 Pulse learning members carried out in December 2012.
Dont get left behind, join now at
pulse-learning.co.uk
Premium members have exclusive access to over 400 clinical,
practice business and commissioning CPD modules
11835P Pulse 290x230 Advertorial_Mar '13.indd 1 15/02/2013 16:40
68 March 2013 Pulse www.pulsetoday.co.uk
RECRUITMENT
Do you really want to make a difference?
We are currently looking to recruit:
Salaried GP/Nurse Practitioner
Avicenna Medical Practice
Bradford, West Yorkshire.
Full time/ part time
Highly motivated GPs and/or Nurse Practitioners who are committed to
providing and developing high quality clinical services with the full support
of our extensive team of experienced GPs.
We will particularly welcome applications from GPs and/or Nurse
Practitioners with an interest in personal development/GPwSi services is
desirable though not essential.
Investors in People GOLD Standards accredited and a finalist in HSJ
Workforce Development Award 2010
Further information or to apply please contact:
Sarah Rhodes, Practice Manager Tel: 01274 664464/07837004309
sarah.rhodes@bradford.nhs.uk
Avicenna- SINGLE UNIT_Avicenna- SINGLE UNIT 15/02/2013 10:05 Page 1
Growing PMS practice in South West London
seeking for a part time 4 session initially
and likely to become
A full time salaried partner.
High QOF achievement.
Paper light EMIS Web system.
Team of 2GPS & 2 Practice nurses.
Medical student teaching
A knowledge of Tamil language would be an advantage.
Salary negotiable.
Please send or email CV with covering letter to
Tina Bowles, at tinabowles@nhs.net
Gunasuntharam- SINGLE UNIT_Gunasuntharam- SINGLE UNIT 21/02/2013 10:59
Beechfield Medical Centre
Beechfield Gardens, Spalding, Lincolnshire
Salaried GP but would consider Partnership
(6- 9 sessions)
What can we tell you about ourselves?
New purpose built premises in busy market town
Friendly and supportive working environment with excellent nursing
and admin teams
Part dispensing
List size 14,500 and growing
6 Partners
EMIS LV - moving to EMIS Web
High QOF achievement
Active involvement in Clinical Commissioning
GU and FP clinic
www.beechfieldmc.co.uk
Start date May/June but this is flexible for the right candidate. Rate of
pay dependent upon skills and experience. Informal visits and enquiries
welcome.
Apply with CV to:
Grant Scott, Practice Manager, Beechfield Medical Centre, Spalding,
Lincs. PE11 1UN or
email grant.scott@lpct.nhs.uk for more information.
Closing date: 29 March 2013
BEACHFIELD -DOUBLE UNIT_BEACHFIELD -DOUBLE UNIT 11/02/2013 16:01 Page 1
Mastercall Healthcare
Mastercall Healthcare is an established award winning provider of
urgent unscheduled and scheduled primary care services.
SESSIONAL GPs
We are looking to enhance our existing team of sessional GPs at our
Stockport and Trafford Health Centres. We are looking for patient
focused, innovative, flexible and enthusiastic GPs in both our out of
hours service and GP-led walk-in centre.
Successful GPs will enjoy integrated and flexible working patterns
developing a high quality primary care service for the people of Stockport
& Trafford.
GPs will benefit from a robust clinical governance infrastructure and a
range of professional training and development opportunities to enhance
their continued professional development in primary care and enhance
their appraisal portfolio.
Excellent benefits including competitive rates of pay plus NHS
superannuation. MRCGP is desirable. We give full training in telephone
consulting skills. A variety of shifts are available during in-hours, out of
hours and overnights on a sessional basis.
To apply please send your CV to Jenny Abbott, HR Manager at
abbottj@stockport-pct.doctorscoop.nhs.uk or telephone 0161 476 7006
for further information.
Mastercall Healthcare is an Equal Opportunities employer.
Mastercall -DOUBLE UNIT_Mastercall -DOUBLE UNIT 21/02/2013 11:23 Page 1
Partner or Salaried GP required from July 2013
Due to retirement of full-time (8.5 sessions per week) Partner,
we seek a committed, flexible GP to join our friendly,
democratic 6 partner Practice on the eastern edge of Derby.
We are happy to consider full and part-time applicants.
12,000 patients
2 sites (Spondon Village & Chaddesden)
High QOF achievement and Patient Satisfaction
TPP SystmOne, paper light
Opportunity to train medical students
CV and covering letter please by 31st March to
Wayne Pitcher, Practice Manager, Dr Gates & Partners, Chapel Street
Medical Centre, 10 Chapel Street, Spondon, Derby, DE21 7RJ
Informal enquiries and visits welcomed, Tel 01332 680521,
email wayne.pitcher@nhs.net
DR GATES- SINGLE UNIT_DR GATES- SINGLE UNIT 21/02/2013 11:04 Page 1
Full Time Slaried GP Post
Salary 90,000
Coastal Health Care Ltd
In the Fleetwood Area.
Scheduled and Unscheduled Care options available.
Do you want to be involved in a dynamic organisation delivering
a variety of healthcare across the Lancashire Coast?
Innovative and high quality GP required to work in scheduled
and unscheduled care environment.
Flexible working hours
No overnight commitments
6 weeks annual leave
For an information pack, Job Description and
Application form please phone 01253 655552
Monday - Friday 09.00 - 16.00 only.
Closing date 8th March.
COASTAL- SINGLE UNIT_COASTAL- SINGLE UNIT 18/02/2013 10:11 Page 1
www.pulsetoday.co.uk Pulse March 2013 69
HANWORTH MIDDLESEX :
SALARIED GP
up to 8 sessions pw. PARTNERSHIP PROSPECTS.
We require a Doctor who will provide high standards of care and
contribute to the development of this innovative Practice
Approx 4000 patients.
Modern purpose built Medical Centre
TPP SystemOne. High QOF Achievment.
Friendly dedicated Practice team including Nurse, HCA
Application with CV to s.winayak@nhs.net
Sheena Winayak , The Medical Centre, 192 Twickenham
Road, Hanworth, Middlesex TW13 6HD
MEDICAL- SINGLE UNIT_COASTAL- SINGLE UNIT 21/02/2013 10:51 Page 1
PERTHFECT
If there was ever an ideal destination for qualied doctors, its
Perth. Exciting opportunities, great salaries, an outdoor life-
style, warm weather, a warm welcome everything you could
wish for, youll nd here in the capital city of Western Australia.
If Perth is the place for you, we can help you make the perfect
move by sorting out all the paperwork and administration.
For more information, contact Mairead at Locumotion.
Email: mdonovan@locumotion.com Phone: 01 299 3550.
www.locumotion.com
LOCUMOTION -DOUBLE UNIT_LOCUMOTION -DOUBLE UNIT 14/01/2013 10:13 Page 1
Cappadocia, Turkey, boasts one of the most unusual
landscapes in the world with its "fairy chimneys"
arising from canyons and its underground cities. Join
Conference Plus in this unique location for a truly
stunning backdrop to Continuing Medical Education
of the highest quality.
Cappadoc|a,Istanbul & 8odrum
Seville, the capital of Moorish Spain, and even better
when combined with the magnicent Alhambra on
our Granada extension. Wonderful sights, fantastic
dining and a day trip to mediaeval Cordoba all
arranged around our academic programme of
obstetrics, orthopaedics and gastroenterology.
Sev|lle,Cordoba & Granada
Discover the breathtaking scenic beauty on this tour
of Peru, exploring the Amazon basin whilst learning of
the medicinal properties of the ora, the White City of
Arequipa, the magnicent Condors and hot springs at
Colca Canyon. At Lake Titicaca we will hold clinics for
its island communities. All tours based around a
varied and enlightening academic programme.
The Amaton, a Peruv|an adventure
Book online at: www.conferenceplus.co.uk
or email: info@conferenceplus.co.uk
Tel: 01923 859363
28th May - 1st June 2013
8th - 12th October 2013
12th -26th October 2013
Relain
Keval|dat|on
Arranging high quality education in the world's most exciting destinations it
K
in la el Re
& l u b n a t s I , a | c o d a p p a C
m e h t f o e n o s t s a o b , y e k r u T , a i c o d a p p a C
s ''s d lld rrl o wwo e h tth n iin n o iio tti a cca u ddu e y tty i lli a ua q h gg iig h g nng iin g n aa rra rrr A
d | l a v e KKe
Ke
ii in i a a l e R
t s 1 - y a M h t 8 2
t a
m u r d o 8 &
l a u s u n u t s o m
n iin tti s ees dde dde
n
g ng iin tti iit cci xxc eex t s o m s ''s
n o | t a d
3 1 0 2 e n u J t
A h T
d a n a r G & a b o d r o C , e l l | v e S
e t n e o r t s a g d n a s c i d e a p o h t r o , s c i r t e t s b o
m a r g o r p c i m e d a c a r u o d n u o r a d e g n a r r a
d r o C l a v e a i d e m o t p i r t y a d a d n a g n i n i d
h g i s l u f r e d n o W . n o i s n e t x e a d a n a r G r u o
A t n e c i n g a m e h t h t i w d e n i b m o c n e h w
n a , n i a p S h s i r o o M f o l a t i p a c e h t , e l l i v e S
. y t i l a u q t s e h g i h e h t f o
d e M g n i u n i t n o C o t p o r d k c a b g n i n n u t s
n o i t a c o l e u q i n u s i h t n i s u l P e c n e r e f n o C
u o r g r e d n u s t i d n a s n o y n a c m o r f g n i s i r a
c y r i a f " s t i h t i w d l r o w e h t n i s e p a c s d n a l
m e h t f o e n o s t s a o b , y e k r u T , a i c o d a p p a C
t c O h t 2 1 - h t 8
a d
. y g o l o r e
f o e m m
l l a a b o d
c i t s a t n a f , s t
n o a r b m a h l A
r e t t e b n e v e d
n o i t a c u d E l a c i
y l u r t a r o f
n i o J . s e i t i c d n u
" s y e n m i h
l a u s u n u t s o m
3 1 0 2 r e b o
| v u r e P a , n o t a m A e h T
g o r p c i m e d a c a g n i n e t h g i l n e d n a d e i r a v
a d e s a b s r u o t l l A . s e i t i n u m m o c d n a l s i s t i
h l l i w e w a c a c i t i T e k a L t A . n o y n a C a c l o C
d n a s r o d n o C t n e c i n g a m e h t , a p i u q e r A
h t , a r o e h t f o s e i t r e p o r p l a n i c i d e m e h t
h w n i s a b n o z a m A e h t g n i r o l p x e , u r e P f o
t u a e b c i n e c s g n i k a t h t a e r b e h t r e v o c s i D
c O h t 6 2 - h t 2 1
9 1 0 : l e TTe
c @ o f n i : l i a m e r o
w w : t a e n i l n o k o o B
e r u t n e v d a n a
. e m m a r g
a d n u o r a
r o f s c i n i l c d l o h
t a s g n i r p s t o h d
f o y t i C e t i h W e h
f o g n i n r a e l t s l i h
r u o t s i h t n o y
3 1 0 2 r e b o t
3 6 3 9 5 8 3 2 9
k u . o c . s u l p e c n e r e ffe n o c
k u . o c . s u l p e c n e r e ffe n o c . w w
CONFERENCE PLUS -DOUBLE UNIT_CONFERENCE PLUS -DOUBLE UNIT 29/01/2013 13:39 Page 1
URGENT CARE -DOUBLE UNIT_URGENT CARE -DOUBLE UNIT 07/01/2013 12:5
Book your appointment now!
enquiries@nzlocums.com | www.nzlocums.com
Positions in New Zealand...
We can provide:
FREE comprehensive recruitment service
Exciting GP opportunities
Immigration assistance
Were visiting London! Book your personal
consultation from 30-31 May at NZ High
Commission, 80 Haymarket, London.
NZLocums- SINGLE UNIT_NZLocums- SINGLE UNIT 21/02/2013 11:13 Page 1
www.pulsetoday.co.uk 70 March 2013 Pulse
Peverley
B
ack in the day, we used to be
an all-male practice, and
consequently I was as au fait
with the complexities of the
menstrual cycle as any GP in
the country. Im not saying
I enjoyed dealing with these endless problems
(who does?) but I could handle it fairly well
and even managed to look as if I cared, quite
a lot of the time.
Now the demographics of general practice
have changed for the better. Pretty much
every practice, including ours, has a couple of
Nice Lady Doctors to deal with all this tedium.
My total freedom from exposure to the
menstrual diary comes at a price, however.
The reception staff have identified another
type of patient who they think might best be
dealt with by me. Every time some swivel-eyed,
sweating sociopath with benzo-hunger in his
eyes rocks up to the front desk at ten to six,
they say: Aha! Another one for Dr Peverley.
The reason for this (apart from me being
six foot three) is that I tend to judge people,
and act on those judgments. Were not
supposed to do this; non-judgmentalism is
a touchstone of our times. But if someones
behaviour is in my opinion self-destructive,
anti-social or detrimental to other
individuals or society in general, I will
generally tell them. Of course, these days,
you cant write worthless parasite in the
medical records, so my notes are littered
with phrases such as this patient is
disabled by inherent moral perplexity.
Well, I know what it means.
One such prize specimen joined our
practice and handed in his repeat
prescription to be filled. When he came
in, it was immediately obvious that his
walking stick was more of a badge of
entitlement than a mobility aid.
My old doctor wasnt giving me what
I needed, he explained. That may or may
not have been true, but after looking at his
prescription, it was certainly the case that his
old doctor had been giving him what he didnt
need. Shampoo? I asked sweetly. Ive got
a scalp condition. I had a quick look. No you
havent, I pointed out, and the black line went
through that one.
I dont want to know
why you were getting
toothpaste on
prescription, but youre
not getting it from us.
Another black line.
Have you got gluten
intolerance? Whats
gluten intolerance?
Never mind that just
now. But youll not be
needing all this bread,
pasta and biscuits from now on.
Then we (well, I say we...) decided that the
morphine, tramadol and diazepam werent
really appropriate for a 23-year-old with a bad
back (investigations all normal) so they went
too. So did the protein drinks, because by now
I was on a roll.
I need a sick note for the disability, was his
next try. What diagnosis shall I put on it? Oh
anything, I dont mind. I think Ill wait for your
records before I issue anything of that nature.
I handed him his new repeat prescription, now
comfortably fitting on one side of paper, and he
looked at it with disbelief: Wheres all me gear?
Im gonna f*ckin complain about you!
He got up to storm out. Youve forgotten
your stick, I told him.
Every now and then a scrounger of the frst order shambles into
Phils consulting room, and hes not afraid to give them both barrels
Sticking it to the
malingerers
Dr Phil Peverley
is a GP in
Sunderland and
was PPA and
BSME columnist
of the year in
2012.
Read more
Peverley
columns at
pulsetoday.
co.uk/peverley
Of course, these
days, you cant
write worthless
parasite in
the medical
records
J
o
u
r
n
a
l
:
P
u
l
s
e
D
e
r
m
a
l
:
D
e
r
m
a
x
R
o
c
k
e
t
A
d
S
i
z
e
:
2
9
0
x
2
3
0
m
m
B
l
e
e
d
:
3
m
m
S
u
p
p
l
y
a
s
h
i
-
r
e
s
P
D
F
J
o
b
N
o
:
2
2
9
3
5
LIFT OFF
FOR SCALY SCALPS
Dermax Therapeutic Shampoo. Benzalkonium chloride 0.5% w/w.
Uses: For the topical treatment of pityriasis capitis and other
seborrhoeic scalp conditions, where there is scaling and dandruff.
Directions: Adults, children and the elderly: Wet the hair. Apply a
liberal quantity of the shampoo to the scalp and, with the tips of
the fingers, rub in thoroughly. Rinse. Repeat the application and
massage to produce a rich lather. Remove as much lather as possible
with the hands, before rinsing thoroughly under running water.
Contra-indications, warnings, side-effects etc: Please refer to
SPC for full details before prescribing. Do not use if sensitive to any
of the ingredients. Keep away from the eyes. No known side-effects.
Package quantity, NHS price and MA number: 250ml bottle 5.69,
PL 00173/0198. Legal Category: MA holder: Dermal Laboratories,
Tatmore Place, Gosmore, Hitchin, Herts, SG4 7QR. Date of
preparation: February 2012. Dermax is a registered trademark.
P
dermax.co.uk
Adverse events should be reported. Reporting
forms and information can be found at
www.mhra.gov.uk/yellowcard. Adverse events
should also be reported to Dermal.
Therapeutic Shampoo
benzalkonium chloride
Lift and clear with
22935_Dermax Rocket Ad_FULL PI_Pulse_AW:1 31/1/13 09:48 Page 1
LAMA = long-acting muscarinic antagonist.
References: 1. SPIRIVA
18 g Summary of Product Characteristics. http://medicines.org.uk/emc. Accessed August 2012. 2. Tashkin DP et al. for the UPLIFT Study
Investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 2008;359:15431554.
Prescribing Information (UK) SPIRIVA
(tiotropium)
Inhalation powder, hard capsules containing 18 microgram tiotropium (as
bromide monohydrate). Indication: Tiotropium is indicated as a maintenance
bronchodilator treatment to relieve symptoms of patients with chronic
obstructive pulmonary disease (COPD). Dose and Administration: Adults
only age 18 years or over: Inhalation of the contents of one capsule once
daily from the HandiHaler
device. Contraindications: Hypersensitivity to
tiotropium bromide, atropine or its derivatives, or to the excipient lactose
monohydrate which contains milk protein. Warnings and Precautions: Not
for the initial treatment of acute episodes of bronchospasm, i.e. rescue
therapy. Immediate hypersensitivity reactions may occur after administration
of tiotropium bromide inhalation powder. Caution in patients with narrow-
angle glaucoma, prostatic hyperplasia or bladder-neck obstruction.
Inhaled medicines may cause inhalation-induced bronchospasm. In
patients with moderate to severe renal impairment (creatinine clearance
50 ml/min) tiotropium bromide should be used only if the expected benefit
outweighs the potential risk. Patients should be cautioned to avoid getting
the drug powder into their eyes. They should be advised that this may
result in precipitation or worsening of narrow-angle glaucoma, eye pain or
discomfort, temporary blurring of vision, visual halos or coloured images in
association with red eyes from conjunctival congestion and corneal oedema.
Should any combination of these eye symptoms develop, patients should stop
using tiotropium bromide and consult a specialist immediately. Tiotropium
bromide should not be used more frequently than once a day. Spiriva capsules
contain 5.5 mg lactose monohydrate. Interactions: Although no formal drug
interaction studies have been performed, tiotropium bromide inhalation
powder has been used concomitantly with other drugs without clinical evidence
of drug interactions. These include sympathomimetic bronchodilators,
methylxanthines, oral and inhaled steroids, commonly used in the treatment of
COPD. The co-administration of tiotropium bromide with other anticholinergic-
containing drugs has not been studied and is therefore not recommended.
Fertility, Pregnancy and Lactation: No documented clinical data on exposed
pregnancies are available. The potential risk for humans is unknown. Tiotropium
bromide should therefore only be used during pregnancy when clearly indicated.
It is unknown whether tiotropium bromide is excreted in human breast milk.
Use of tiotropium bromide during breast feeding is not recommended.
A decision on whether to continue or discontinue breast feeding or therapy with
tiotropium bromide should be made taking into account the benefit of breast
feeding to the child and the benefit of tiotropium bromide therapy to the woman.
Clinical data on fertility are not available for tiotropium. Effects on ability to
drive and use machines: No studies have been performed. The occurrence of
dizziness, blurred vision, or headache may influence the ability to drive and
use machinery. Undesirable effects: Common ( 1/100 to <1/10) Dry mouth.
Uncommon ( 1/1000 to <1/100) Dizziness, headache, taste disorders, vision
blurred, atrial fibrillation, pharyngitis, dysphonia, cough, gastrooesophageal
reflux disease, constipation, oropharyngeal candidiasis, rash, dysuria, urinary
retention. Serious undesirable effects consistent with anticholinergic effects
include glaucoma, constipation and intestinal obstruction including ileus
paralytic as well as urinary retention. An increase in anticholinergic effects may
occur with increasing age. Prescribers should consult the Summary of Product
Characteristics for further information on side effects. Pack sizes and NHS price:
Combopack HandiHaler device and 30 capsules (3 blister strips) 34.87 Refill
Pack 30 capsules (3 blister strips) 33.50. Legal category: POM. MA Number:
PL 14598/0062. Marketing Authorisation Holder: Boehringer Ingelheim
International GmbH, D-55216 Ingelheim am Rhein, Germany. Prescribers should
consult the Summary of Product Characteristics for full prescribing information.
Prepared in August 2012.
Adverse events should be reported.
Reporting forms and information can be found at
www.mhra.gov.uk/yellowcard. Adverse events should
also be reported to Boehringer Ingelheim Drug
Safety on 0800 328 1627 (freephone).
With a long-term record of success in reducing symptoms, exacerbations
and hospitalisations vs placebo, SPIRIVA
is a LAMA you can count
on to help lead your COPD patients to everyday victories.
1,2
P
r
o
d
u
c
in
g
w
in
n
e
r
s
since 2002
Date of preparation: August 2012 UK/SPI-121384
Founded on a decade of proven success
5434 Spiriva 290x230 Ad.indd 1 02/01/2013 16:16
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- What Is A Heart Transplant?Dokument2 SeitenWhat Is A Heart Transplant?Michael MirasolNoch keine Bewertungen
- ODD in The Classroom - Strategies For Dealing With Behavioural IssuesDokument81 SeitenODD in The Classroom - Strategies For Dealing With Behavioural IssuesRosangela Lopez CruzNoch keine Bewertungen
- Pogona Vitticeps) Nannizziopsis GuarroiDokument8 SeitenPogona Vitticeps) Nannizziopsis GuarroiAkın SeverNoch keine Bewertungen
- Botany (Virus)Dokument48 SeitenBotany (Virus)Madhuri DeviNoch keine Bewertungen
- 3 - Lower Gastrointestinal DisorderDokument14 Seiten3 - Lower Gastrointestinal DisorderNica EnriquezNoch keine Bewertungen
- Reaserch Content On Breast Cancer and Lesson Plan 1 PDFDokument33 SeitenReaserch Content On Breast Cancer and Lesson Plan 1 PDFNabanita KunduNoch keine Bewertungen
- ANAPHY Lec Session #19 - SAS (Agdana, Nicole Ken)Dokument7 SeitenANAPHY Lec Session #19 - SAS (Agdana, Nicole Ken)Nicole Ken AgdanaNoch keine Bewertungen
- Physical Restraint Reduction For Older AdultsDokument11 SeitenPhysical Restraint Reduction For Older Adultsantariksa tedyNoch keine Bewertungen
- 7 F1 EURAMOS1 AA Protocol COSS 31072007 Gesamt PDFDokument457 Seiten7 F1 EURAMOS1 AA Protocol COSS 31072007 Gesamt PDFJemma ArakelyanNoch keine Bewertungen
- Vet Obst Lecture 1 Pregnancy in Domestic AnimalsDokument53 SeitenVet Obst Lecture 1 Pregnancy in Domestic AnimalsgnpobsNoch keine Bewertungen
- Notes On Maternal & Child Care (Pregnancy)Dokument3 SeitenNotes On Maternal & Child Care (Pregnancy)Oink TopusNoch keine Bewertungen
- Chapter 6 - Pest and Disease Management in Plant Propagation and NurseryDokument22 SeitenChapter 6 - Pest and Disease Management in Plant Propagation and NurserySheena Jane SegalesNoch keine Bewertungen
- 1 s2.0 S0040162520312774 Main PDFDokument7 Seiten1 s2.0 S0040162520312774 Main PDFCardboard GamingNoch keine Bewertungen
- 10.1136@bmjspcare 2019 002120Dokument11 Seiten10.1136@bmjspcare 2019 002120Ambulatório Dieta Cetogênica HUBNoch keine Bewertungen
- Sf8 Nutritional-Stat-Baseline 6 Pearl 2022Dokument8 SeitenSf8 Nutritional-Stat-Baseline 6 Pearl 2022Dante Maligsa BautistaNoch keine Bewertungen
- CDI Consumer Factsheet BrochureDokument2 SeitenCDI Consumer Factsheet BrochurebejarhasanNoch keine Bewertungen
- Procedure of Hot Stone MassageDokument18 SeitenProcedure of Hot Stone Massagealejandro9yahoo.com100% (1)
- SHO Paper 2Dokument9 SeitenSHO Paper 2Kenny Low100% (1)
- Visual Diagnosis and Traditional Chinese Medicine: Face Reading - What Your Face SaysDokument8 SeitenVisual Diagnosis and Traditional Chinese Medicine: Face Reading - What Your Face SaysTaniaNoch keine Bewertungen
- Sweet DeathDokument5 SeitenSweet DeathJBNoch keine Bewertungen
- Biology I Lecture Outline 7 Viruses: (Textbook Pages 273-2Dokument12 SeitenBiology I Lecture Outline 7 Viruses: (Textbook Pages 273-2Rukhsana HabibNoch keine Bewertungen
- Early Intervention Support and Inclusion For Children With Disability - ADHCDokument4 SeitenEarly Intervention Support and Inclusion For Children With Disability - ADHCMirolz PomenNoch keine Bewertungen
- FdarDokument2 SeitenFdarkasandra dawn Beriso67% (3)
- 5. Chronic pancreatitis. СholelithiasisDokument58 Seiten5. Chronic pancreatitis. Сholelithiasischai rinNoch keine Bewertungen
- Of Of: National HeadquartersDokument5 SeitenOf Of: National Headquarterschitobarba19726762Noch keine Bewertungen
- The Final FRCR Self-AssessmentDokument244 SeitenThe Final FRCR Self-AssessmentAman KumarNoch keine Bewertungen
- Advantages and Disadvantages of Aphakics Correction, Types of Aphakic Correction, Problems of Newly Corrected AphakicsDokument78 SeitenAdvantages and Disadvantages of Aphakics Correction, Types of Aphakic Correction, Problems of Newly Corrected AphakicsTika100% (1)
- Pedia 102 MIDTERM EXAMSDokument15 SeitenPedia 102 MIDTERM EXAMSquidditch07Noch keine Bewertungen
- Nursing Care Plan HyperthyroidismDokument2 SeitenNursing Care Plan Hyperthyroidismderic76% (17)
- What Is The Difference Between Perception and PerspectiveDokument4 SeitenWhat Is The Difference Between Perception and Perspectivebday23100% (1)