Beruflich Dokumente
Kultur Dokumente
Characterization of Extended-Spectrum
Hochgeladen von
Ridho WahyutomoOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Characterization of Extended-Spectrum
Hochgeladen von
Ridho WahyutomoCopyright:
Verfügbare Formate
Journal of Medical Microbiology (2006), 55, 417421
DOI 10.1099/jmm.0.46177-0
Characterization of extended-spectrum b-lactamase (ESBL)-producing Kuwait and UK strains identied by the Vitek system, and subsequent comparison of the Vitek system with other commercial ESBL-testing systems using these strains
A. A. Dashti,1 P. West,1 R. Paton2 and S. G. B. Amyes2
Correspondence A. A. Dashti aad@hsc.edu.kw
1 2
Medical Laboratory Sciences, Health Science Centre, Kuwait University, Kuwait Molecular Chemotherapy, Centre for Infectious Diseases, University of Edinburgh, Edinburgh EH16 4SB, UK
Received 1 June 2005 Accepted 3 January 2006
Two hundred and fty-one unique patient isolates of Klebsiella pneumoniae (123), Escherichia coli (114), Klebsiella oxytoca (7), Enterobacter cloacae (5) and Citrobacter freundii (2), agged as extended-spectrum b-lactamase (ESBL) positive by the Vitek system (GNS-526 card), were collected. These strains were isolated from a variety of clinical specimens submitted to the clinical bacteriology laboratories of the Royal Inrmary of Edinburgh (RIE), Edinburgh, UK (and associated GP practices), Hairmyers Hospital, Glasgow, UK, and the Amiri and Farwania Hospitals, Kuwait. Of the 101 RIE strains tested, 15 E. coli strains were found to be ESBL negative by Etest ESBL strips. On retesting the 15 E. coli strains with the Vitek GNS-532 card, 14 were found to be ESBL negative, despite being originally agged as ESBL positive. The remaining 236 ESBL-producing strains were also subjected to the double disc-diffusion (DDD) technique for the detection of ESBLs. Of these, two were false negatives by Etest ESBL test strips (using both cefotaxime and ceftazidime strips), and 38 were false negatives by the DDD method. The Etest false-negative ESBL-producing strains of K. pneumoniae were positive by DDD. Technically, the Vitek method was the least demanding method to perform, as it was an integral part of the routine susceptibility test card. Etest strips were reliable, but were the most expensive of all the techniques used. The DDD test, while relatively inexpensive, was technically subjective, and in our hands, seven of the ESBL-positive strains that were conrmed by the other two techniques were not detected. Despite the false-positive ESBL-producing E. coli strains, the Vitek susceptibility card with its integral ESBL test offers the clinical laboratory a valuable and quick option to screen for ESBL-producing Klebsiella spp. and E. coli as part of the routine laboratory methodology.
INTRODUCTION
Since their introduction into clinical practice, oxyimino cephalosporins have been excessively used in hospitals (Du Bois et al., 1995; Heritage et al., 1999). The effectiveness of these b-lactam antibiotics has been diminished by Klebsiella spp. which have become resistant to their mode of action. This resistance has spread to strains of Escherichia coli and to other Gram-negative bacteria as well (Sanders et al., 1996). Investigations into the mechanism responsible for this resistance have revealed the presence of extended-spectrum b-lactamase (ESBL) enzymes derived from the widespread
Abbreviations: DDD, double disc-diffusion; ESBL, extended-spectrum b-lactamase; RIE, Royal Inrmary of Edinburgh.
TEM-1/2 and SHV-1 family. To date, there are over 110 derivatives of TEM b-lactamases and more than 63 derivatives of SHV b-lactamases (Bush et al., 1995; Bradford et al., 1995; Bradford, 2001; Hawkey & Munday, 2004; Sanders et al., 1996). These enzymes are usually less efcient at hydrolysis than their parent enzymes, and consequently their detection by currently used routine susceptibility tests is difcult. Therefore, ESBL-producing Klebsiella spp. and E. coli may falsely appear to be susceptible to newer cephalosporins (Gibb & Crichton, 2000). Because current breakpoints for cephalosporin sensitivity are set for clinical efcacy, they are too high to detect ESBL mutations; therefore, there is clearly a requirement to detect the resistance mechanism itself rather than to rely on in vitro susceptibi rieux) has an ESBL lity testing. The Vitek system (bioMe
417
46177 G 2006 SGM
Printed in Great Britain
A. A. Dashti and others antibiotics (10, 10 and 1 mg, respectively) with the addition of clavulanate (Oxoid). A broth culture of the test organism was adjusted to a 0?5 McFarland standard and inoculated onto MuellerHinton agar (Oxoid). The combination discs and the corresponding standard cephalosporin disc were placed at the recommended distance from each other on the plate. The plates were incubated at 37 uC for 18 h aerobically before the zone sizes were recorded. A positive result was indicated by a zone-size difference of 5 mm diameter between the combination disc and the corresponding standard antibiotic disc, as recommended by the manufacturer. For all ESBL detection methods, the known ESBL-producing E. coli strains SA1636 (TEM-3) and SA1652 (SHV-2) were used as positive controls. E. coli NCTC 10418 was used as a negative control.
detection test as an integral part of the routine susceptibility test card. There have been several studies of the efcacy on the Vitek system with known ESBL-producing strains (Gibb & Crichton, 2000; Sanders et al., 1996). The current study was performed to assess the behaviour of ESBLs in clinical strains detected by the Vitek system, in comparison with two other commercial ESBL detection methods. Screening and conrmation of the test were done following National Committee for Clinical Laboratory Standards (NCCLS) rules (National Committee for Clinical Laboratory Standards, 1999).
METHODS
Bacterial isolates. One hundred and forty-one clinical isolates
were collected in Scotland. One hundred and one isolates consisted of Klebsiella pneumoniae (69) and E. coli (32) obtained from various clinical samples sent to the clinical bacteriology laboratories of the Royal Inrmary of Edinburgh (RIE), Edinburgh, UK, and 40 Enterobacteriaceae clinical isolates [K. pneumoniae (16), E. coli (10), Klebsiella oxytoca (7), Ent. cloacae (5) and C. freundii (2)] were obtained from various clinical samples sent to the clinical bacteriology laboratories of the Hairmyers Hospital, Glasgow, UK. The 101 RIE isolates had previously been identied and reported as ESBL positive by the Vitek system. From Kuwait, 110 isolates, consisting of K. pneumoniae (38) and E. coli (63) were collected from Al-Amiri hospital, and nine E. coli isolates were from Farwania hospital. Isolates were collected from various clinical samples and submitted to the clinical laboratories of the Al-Amiri hospital between June and December 2003. All Isolates were stored on nutrient agar slopes at room temperature until tested.
ESBL detection methods Vitek system. The Vitek is an automated system for identication
RESULTS
UK strains Of the 101 strains from the RIE originally tested, 15 were negative for ESBL production by both cefotaxime and ceftazidime Etest strips. These 15 Etest-negative strains (all E. coli) were retested with Vitek (GNS-532 card), and 14 of these strains were subsequently found to be ESBL negative. One strain still agged ESBL positive by Vitek. The 14 retested ESBL-negative strains were not subjected to further study. The cefotaxime ESBL strip detected the presence of ESBL activity in 84 (96?5 %) of the remaining 87 isolates tested. Of these, 19 (22 %) demonstrated phantom phenomena that indicated them to be ESBL positive, as described in the manufacturers interpretation guide. Three strains (two E. coli and one K. pneumoniae) were negative for ESBL activity with cefotaxime ESBL strips. With ceftazidime Etest strips, ESBL activity was detected in 47 (54 %) of the study isolates. Of these, three (3?5 %) were positive by demonstration of phantom phenomena. The use of the combination of both cefotaxime and ceftazidime Etest ESBL strips detected ESBLs in 86 of the 87 test isolates (98?8 %). From these data, it appears that the use of both strips is essential for optimal detection of ESBL activity. Only one strain of K. pneumoniae that demonstrated positive ESBL activity with the Vitek system was not detected by Etest ESBL strips. This strain remained positive when retested with Vitek. Using the DDD method, the combination disc containing cefotaxime detected the presence of ESBL activity in 74 strains (85 %) (64 K. pneumoniae and 10 E. coli), whilst the cefpodoxime combination disc detected ESBL activity in 64 strains (73?5 %) (54 K. pneumoniae and 10 E. coli). The ceftazidime combination disc had the poorest sensitivity, detecting the presence of ESBL activity in only 40 strains (46 %) (31 K. pneumoniae and 9 E. coli). The strain of K. pneumoniae that demonstrated no ESBL activity by Etest was ESBL positive with the DDD method. When the results of all three cephalosporin combination discs were taken into
Journal of Medical Microbiology 55
and/or susceptibility testing. Vitek susceptibility test results are expressed as MIC values, and interpreted as susceptible, intermediate or resistant by reference to a National Committee for Clinical Laboratory Standards breakpoint (National Committee for Clinical Laboratory Standards, 1999). This system is able to detect ESBL production by an automated version of the synergy test, which is based on detection of the inhibitory effect of clavulanic acid on ESBLs in the presence of either cefotaxime or ceftazidime. The test is interpreted by measuring the difference in bacterial growth with or without inhibitor. All isolates were originally tested with Gram-negative susceptibility (GNS-526) cards. Etestnegative strains were retested with GNS-532 cards. In the course of the study, GNS-532 cards superseded GNS-526 cards, with a subsequent software upgrade.
Etest ESBL strips. Etest ESBL strips (AB Biodisk) are double-
ended strips with antibiotic and antibiotic/inhibitor gradients. These strips yield the MIC as well as the MIC ratio, which determines the presence of an ESBL. The strips used in this study were ceftazidime+clavulanic acid (TZ/TZL) and cefotaxime+clavulanic acid (CT/CTL), for which the recommended ratio value indicates the presence of an ESBL. Interpretation of the result was as recommended by the manufacturer.
Double disc-diffusion (DDD) method. This method was used to
reconrm the strains that were ESBL positive by Etest and/or Vitek GNS-532 card. The DDD method that was used here employed six discs, three containing ceftazidime (30 mg), cefotaxime (30 mg) or cefpodoxime (10 mg), and three with a combination of the same 418
Commercial ESBL-testing systems
consideration, 80 (92 %) of the 87 ESBL-positive strains were detected. All 40 strains tested from Hairmyers Hospital, Glasgow, were ESBL positive. ESBL activity in all these isolates was reconrmed by the Etest ESBL strip and DDD methods. The cefotaxime ESBL strip detected the presence of ESBL activity in 38 (95 %) of the tested isolates. Of these, 19 (48 %) were phantom phenomena ESBL positive, as described in the manufacturers interpretation guide. Two strains (two E. coli) were negative for ESBL activity with cefotaxime ESBL strips. With ceftazidime Etest strips, ESBL activity was detected in 32 (80 %) of the study isolates. Of these, seven (17?5 %) were positive by demonstration of phantom phenomena. The use of the combination of both cefotaxime and ceftazidime Etest ESBL strips detected ESBLs in all of the isolates tested (100 %). From these data, it appears that the use of both strips is essential for optimal detection of ESBL activity. Using the DDD method, the combination disc containing cefotaxime detected the presence of ESBL activity in 35 strains (87?75 %) (16 K. pneumoniae, 10 E. coli, six K. oxytoca and three Ent. cloacae), whilst the cefpodoxime combination disc detected ESBL activity in 31 strains (77?5 %) (15 K. pneumoniae, nine E. coli, four K. oxytoca and three Ent. cloacae). The ceftazidime combination disc was the least efcacious, detecting the presence of ESBL activity in only 17 strains (42?5 %) (eight K. pneumoniae, four E. coli, three Ent. cloacae and two C. freundii). The strains that demonstrated no ESBL activity by the DDD method were ESBL positive with the Etest method. When the results of all three cephalosporin combination discs were taken into consideration, 37 (92?5 %) of the 40 ESBL-positive strains were detected (see Table 1). Kuwait strains Sixty-three strains were obtained from non-repeat isolates from Amiri Hospital patients, and nine strains were isolated from neonates in Farwania Hospital in 1994. The Amiri isolates originated from many departments, and 27 of the 62 patients were >60 years old. Etest ceftazidime and cefotaxime/clavulanate strips detected ESBLs in 71 of 72
isolates (98?6 %), whereas cefpodoxime, which performed best in the DDD test, showed clear results in 46 of 72 isolates (64 %). Of the 38 K. pneumoniae strains tested, one showed no synergy with both cefotaxime and ceftazidime Etest strips. The cefotaxime ESBL strips detected the presence of ESBL activity in 29 (76?3 %) of the tested isolates, and nine strains were ESBL negative by cefotaxime strips. With ceftazidime Etest strips, ESBL activity was detected in 32 (84?4 %) of the isolates. The use of a combination of both cefotaxime and ceftazidime Etest ESBL strips detected the enzyme in 37 of the isolates (97?4 %) (see Table 2). From these data it appears that the use of both strips is essential for optimal detection of ESBL activity, particularly as the ceftazidime Etest strip appeared less sensitive in detecting ESBL activity. Only one isolate that was reported ESBL positive by the Vitek method was not detected by Etest ESBL strips; however, this strain remained positive when retested with Vitek.
DISCUSSION
There is currently a great need for reliable and efcient tests to detect ESBLs in clinical isolates of Enterobacteriaceae. Conventional susceptibility testing methods, on their own, fail to offer reliable susceptibility results for b-lactam antibiotics when testing those species that harbour ESBLs. Currently, most UK clinical laboratories do not use a standard method for the detection of ESBLs, and many clinical laboratories do not routinely identify Enterobacteriaceae to genus and species level. The Vitek system addresses this issue. It will only validate a susceptibility result once the organism has been identied to species level. If the system detects the presence of an ESBL resistance mechanism in strains of Klebsiella spp. and E. coli, it then utilizes its expert software and applies it to the nal susceptibility results. If b-lactams are found to be susceptible to ESBL activity, the strain is then agged as resistant, regardless of whether the in vitro test indicates susceptibility. This study has shown that the Vitek system, in our hands, whilst easy to perform and without any subjective interpretation of results, reported false-positive detection of ESBL activity with 14 strains of E. coli. On retesting these
Table 1. Results obtained with Etest ESBL strips and the DDD method for detecting the presence of ESBLs in 127 strains of E. coli, K. pneumoniae, K. oxytoca, Ent. cloacae and C. freundii isolated from UK hospitals
Combination disc/strip Cefotaxime Ceftazidime Cefpodoxime Total ESBL positive (%) No. of positive ESBL isolates (%) DDD method 109 57 95 117 (85?8) (44?8) (74?8) (92?1) Etest ESBL strip 122 (96) 79 (62?2) Not tested 126 (99?2)
Table 2. Results obtained with Etest ESBL strips and the DDD method for detecting the presence of ESBLs in 110 strains of E. coli and K. pneumoniae isolated from Kuwait hospitals
Combination disc/strip Cefotaxime Ceftazidime Cefpodoxime Total ESBL positive (%) No. of positive ESBL isolates (%) DDD method 43 35 54 82 (39) (31?8) (49) (75) Etest ESBL strip 95 (86) 84 (76?4) Not tested 108 (98?2)
http://jmm.sgmjournals.org
419
A. A. Dashti and others
strains with Vitek (GNS-532 card), they were correctly reported as ESBL negative. One of the retested E. coli isolates was found to be ESBL positive by the Vitek system and by the DDD method; however, ESBL activity could not be detected by Etest. All these strains were initially tested with the same batch number of Vitek (GNS-526 card). When retested, the GNS-532 card was used; this card has superseded the GNS526, with accompanying software upgrades. Although internal quality control (QC) is performed on these cards, an ESBLproducing E. coli is not used as part of the QC battery. It was initially thought that the 14 false-positive ESBL E. coli results might have been the result of a faulty batch of GNS-526 cards. However, recent work in this laboratory, with ten recently isolated Vitek ESBL-positive E. coli has shown two of these ten strains to be ESBL negative by Etest. On retesting with the same batch of Vitek GNS-532, these two strains were subsequently reported as ESBL negative. Although the percentage of false-positive E. coli ESBL strains fell from approximately 50 to 20 % with the new GNS-532 card, it was still a concern that these strains were misreported as ESBL producers with subsequent expert rules for antibiotic susceptibility to b-lactam antibiotics applied. There appears to be no obvious reason for these results. They are unlikely to arise from a technical error, as the Vitek is a highly standardized system. These strains have been forwarded to rieux for further studies. bioMe The DDD test requires careful spacing of discs for accurate results and careful interpretation of zone sizes. It is therefore technically demanding. In previous studies, the DDD test was able to detect 82 and 88 % of ESBL-positive strains, respectively (Gibb & Crichton, 2000; Thomson & Sanders, 1992). The limitations of this test have been described elsewhere (Bush, 1996; Thomson & Sanders, 1992). A recent study has reported that cepodoxime achieves a 100 % sensitivity rate in detecting ESBLs in tested isolates, cefotaxime 92 %, and ceftazidime 82 % (Appleton & Hall, 2000). In contrast, the results of isolates from the UK used in this study showed that cefotaxime was the most efcient cephalosporin for the detection of ESBLs, with a sensitivity rate of 85?8 %; the values for cepodoxime and ceftazidime were 74?8 % and 44?8 %, respectively. The results from Kuwait hospital isolates showed that cepodoxime was the most efcient cephalosporin for the detection of ESBLs, with a sensitivity rate of 49 %; the values for cefotaxime and ceftazidime were 39 % and 31?8 %, respectively. Overall, the DDD method was able to detect ESBL activity in 75 % of the Kuwait isolates and 92?1 % of the UK isolates. This may reect the type of ESBLs in our isolates, and emphasizes the importance of testing more than one cephalosporin. The commercially available ESBL Etest strip is a quantitative technique, and is widely regarded as the gold standard for detection in clinical laboratories of ESBL production (MZali et al., 2000). In our hands, it detected 99?2 % of the UK test isolates and 98 % of the Kuwait isolates, but only if both cefotaxime and ceftazidime strips were used in conjunction. As noted above, the ceftazidime Etest strip was less sensitive;
420
the reason for this was not obvious, but it is possible that there were other ceftazidime-hydrolysing b-lactamases in some strains that were not sensitive to clavulanic acid, which could have reduced the sensitivity of the test. Thus, Etests with both cephalosporins are recommended; however, this makes the technique expensive, and most clinical laboratories would use it only for conrmation rather than as a routine test. The majority of clinical laboratories do not have the resources to identify ESBL-producing strains by molecular methods; therefore, it is important to have an easy-toperform methodology that can be used in the routine laboratory. This study shows the importance of identication of Enterobacteriaceae to species level and the usefulness of the Vitek system for routine detection of ESBLs if accurate and consistent results are to be reported to clinicians. This has been clearly demonstrated in a recent report that describes the retrospective detection of ESBLs in ve of 20 strains of K. pneumoniae isolated from blood cultures. In some of these cases, patients were treated with an inappropriate third-generation cephalosporin, and treatment in these patients was changed after clinical failure (Crowley, 2001). If an ESBL detection test had been available at the time of the original susceptibility testing, appropriate results would have reported to the clinician. It should be noted that in our hands, some E. coli were falsely reported as ESBL positive. For ESBL-positive K. pneumoniae in this study, the Vitek test was accurate, but it should be noted that this study only included Vitek ESBL-positive strains, and was therefore not an evaluation of the Vitek ESBL test itself. In conclusion, the Vitek ESBL test was cost-effective as an ESBL screen in as much as the ESBL test is an integral part of the susceptibility card and is performed simultaneously with the susceptibility tests. In addition, the Vitek test is interpreted by the system itself, which removes any errors of subjectivity. No additional outlay of resources is required. We would recommend that strains of E. coli be conrmed as ESBL positive by an additional method, such as Etest.
ACKNOWLEDGEMENTS
We would like to thank Dr D. Baird of Hairmyers Hospital, Glasgow, UK, and Dr M. Johny of Amiri Hospital, Kuwait, for the generous gift of strains. We are also grateful to Jenan Kawaf for excellent technical assistance.
REFERENCES
Appleton, A. & Hall, S. (2000). Comparison of three combination discs for the detection of extended spectrum b-lactamases. Poster presented
at the Third European Congress of Chemotherapy, Madrid, Spain, May 710 2000.
Bradford, P. A. (2001). Extended-spectrum beta-lactamases in the
21st century: characterization, epidemiology and detection of this important resistance threat. Clin Microbiol Rev 14, 933951. Journal of Medical Microbiology 55
Commercial ESBL-testing systems
Bradford, P. A., Urban, C., Jaiswal, A., Mariano, N., Rasmussen, B. A., Projan, S. J., Rahal, J. J. & Bush, K. (1995). SHV-7, a novel cefotaximehydrolyzing b-lactamase identied in E. coli isolated from hospitalized
Heritage, J., MZali, F. H., Gascoyne-Biniz, D. & Hawkey, P. M. (1999). Evolution and spread of SHV extended-spectrum b-lactamases
in Gram-negative bacteria. J Antimicrob Chemother 44, 309318.
MZali, F. H., Chanawong, A., Kerr, K. G., Birkenhead, D. & Hawkey, P. M. (2000). Detection of extended-spectrum b-lactamases in
nursing home patients. Antimicrob Agents Chemother 39, 899905.
Bush, K. (1996). Is it important to identify extended-spectrum b-
lactamase producing isolates? Eur J Clin Microb Infect Dis 15, 361364.
Bush, K., Jacoby, G. A. & Medeiros, A. A. (1995). A functional classication scheme for b-lactamases and its correlation with
members of the family Enterobacteriaceae: comparison of the MAST DD test, the double disc and the Etest ESBL. J Antimicrob Chemother 45, 881885.
National Committee for Clinical Laboratory Standards (1999).
molecular structure. Antimicrob Agents Chemother 39, 12111233.
Crowley, D. B. (2001). Extended-spectrum b-lactamases in blood
culture isolates of Klebsiella pneumoniae: seek and you may nd! J Antimicrob Chemother 47, 728729.
Du Bois, S. K., Marriott, M. S. & Amyes, S. G. B. (1995). TEM- and SHV-derived extended-spectrum b-lactamases: relationship between
Performance Standards for Antimicrobial Susceptibility; Ninth Informational Supplement M100-S9. Villanova, PA, USA: National Committee for Clinical Laboratory Standards.
Sanders, C. C., Barry, A. L., Washington, J. A., Shubert, C., Moland, E. S., Traczewski, M. M., Knapp, C. & Mulder, R. (1996). Detection of extended-spectrum b-lactamase-producing members of the family
selection, structure and function. J Antimicrob Chemother 35, 722.
Gibb, A. P. & Crichton, M. (2000). Cefpodoxime screening of Escherichia
Enterobacteriaceae with the Vitek ESBL test. J Clin Microbiol 34, 29973001.
Thomson, K. S. & Sanders, C. C. (1992). Detection of extendedspectrum b-lactamases in members of the family Enterobacteriaceae comparison of the double-disk and 3-dimensional tests. Antimicrob Agents Chemother 36, 18771882.
coli and Klebsiella spp. by Vitek for detection of organisms producing extended-spectrum b-lactamases. Diagn Microbiol Infect Dis 38, 255257.
Hawkey, P. M. & Munday, C. J. (2004). Multiple resistance in Gram-
negative bacteria. Rev Med Microbiol 15, 5161.
http://jmm.sgmjournals.org
421
Das könnte Ihnen auch gefallen
- 2016 January FebruaryDokument45 Seiten2016 January FebruaryAndriusjo100% (1)
- Chemotherapy DrugsDokument43 SeitenChemotherapy Drugsbrigette_lagat100% (2)
- Electro-Acupuncture - An Introduction and Its Use For Peripheral Facial ParalysisDokument19 SeitenElectro-Acupuncture - An Introduction and Its Use For Peripheral Facial ParalysiserwindorinaldoNoch keine Bewertungen
- Burger PPT CH 15Dokument30 SeitenBurger PPT CH 15Necelle YuretaNoch keine Bewertungen
- NCM 100 SKILLS Nursing Process HandoutsDokument10 SeitenNCM 100 SKILLS Nursing Process HandoutsPearl IbisateNoch keine Bewertungen
- Equator MANTA TERMICADokument68 SeitenEquator MANTA TERMICALizet Ceron100% (1)
- The Drug Interaction Probability ScaleDokument1 SeiteThe Drug Interaction Probability ScaleFina Ahmad Fitriana0% (1)
- Irwin and Rippes Intensive Care Medicine PDFDokument3 SeitenIrwin and Rippes Intensive Care Medicine PDFRidho Wahyutomo0% (1)
- BSAC AntimicrobialStewardship FromPrinciplestoPractice EbookDokument347 SeitenBSAC AntimicrobialStewardship FromPrinciplestoPractice EbookAndrea Gallerani100% (1)
- ESBL Producing Klebsiella Pneumoniae Susceptibility PatternsDokument6 SeitenESBL Producing Klebsiella Pneumoniae Susceptibility PatternsPutri Nilam SariNoch keine Bewertungen
- Prevalence of ESBL-Producing Enterobacteriaceae in Saudi HospitalDokument4 SeitenPrevalence of ESBL-Producing Enterobacteriaceae in Saudi HospitalMohammad K AlshomraniNoch keine Bewertungen
- Cpe Paper 2Dokument21 SeitenCpe Paper 2obakhit91Noch keine Bewertungen
- Frequency and Sensitivity of ESBL Isolates in Pakistan HospitalDokument4 SeitenFrequency and Sensitivity of ESBL Isolates in Pakistan HospitalPutri Nilam SariNoch keine Bewertungen
- Clin Microbiology Infect - 2007 - Wilson - The Use of Antibiotic Containing Agars For The Isolation of Extended SpectrumDokument3 SeitenClin Microbiology Infect - 2007 - Wilson - The Use of Antibiotic Containing Agars For The Isolation of Extended SpectrumYousra SoumaNoch keine Bewertungen
- Evaluation of A Diagnostic Flow Chart For Detection and Confirmation of Extended Spectrum B-Lactamases (ESBL) in EnterobacteriaceaeDokument11 SeitenEvaluation of A Diagnostic Flow Chart For Detection and Confirmation of Extended Spectrum B-Lactamases (ESBL) in EnterobacteriaceaeRaffaharianggaraNoch keine Bewertungen
- Antibiotic Impregnated Tablets For Screening Esbl and Ampc Beta LactamasesDokument4 SeitenAntibiotic Impregnated Tablets For Screening Esbl and Ampc Beta LactamasesIOSR Journal of PharmacyNoch keine Bewertungen
- Performance of chromID ESBL, a chromogenic medium for detection of Enterobacteriaceae producing extended-spectrum beta-lactamasesDokument6 SeitenPerformance of chromID ESBL, a chromogenic medium for detection of Enterobacteriaceae producing extended-spectrum beta-lactamasesMiriam LeiNoch keine Bewertungen
- Klebsiella Pneumoniae: Trends in The Hospital and Community SettingsDokument5 SeitenKlebsiella Pneumoniae: Trends in The Hospital and Community SettingskhanfahsNoch keine Bewertungen
- Sorloz DiagMicrobiolInfDis51Dokument3 SeitenSorloz DiagMicrobiolInfDis51Nidia MaradiagaNoch keine Bewertungen
- PIIS1201971205001438Dokument5 SeitenPIIS1201971205001438YHCT K45 Bùi Ngọc Bảo TrânNoch keine Bewertungen
- Efficacy of Practised Screening Methods For Detection of Cephalosporin-Resistant EnterobacteriaceaeDokument4 SeitenEfficacy of Practised Screening Methods For Detection of Cephalosporin-Resistant EnterobacteriaceaeCoquelicot Éphémère ÉphémèreNoch keine Bewertungen
- Multi-Centre Evaluation of A Phenotypic Extended Spectrum B-Lactamase Detection Guideline in The Routine SettingDokument7 SeitenMulti-Centre Evaluation of A Phenotypic Extended Spectrum B-Lactamase Detection Guideline in The Routine SettingYHCT K45 Bùi Ngọc Bảo TrânNoch keine Bewertungen
- 2 Comparacion BD Phoenix Vitek MicroscanDokument10 Seiten2 Comparacion BD Phoenix Vitek MicroscanBenjamin MendozaNoch keine Bewertungen
- Pattern of CTX-M and SHV Genes in Esbl Producing Klebsiella PneumoniaeDokument9 SeitenPattern of CTX-M and SHV Genes in Esbl Producing Klebsiella Pneumoniaeijmb333Noch keine Bewertungen
- Escherichia Coli in A Rural Medical College of Himachal PradeshDokument5 SeitenEscherichia Coli in A Rural Medical College of Himachal PradeshIOSR Journal of PharmacyNoch keine Bewertungen
- Niveditha ArticleDokument2 SeitenNiveditha ArticleIJAMNoch keine Bewertungen
- Journal Homepage: - : Manuscript HistoryDokument10 SeitenJournal Homepage: - : Manuscript HistoryIJAR JOURNALNoch keine Bewertungen
- Expert Systems: Web SitesDokument6 SeitenExpert Systems: Web SitesNidia MaradiagaNoch keine Bewertungen
- Multi-Biochemical Test System For: Distinguishing Enteric and Other Gram-Negative BacilliDokument7 SeitenMulti-Biochemical Test System For: Distinguishing Enteric and Other Gram-Negative BacilliSyazmin KhairuddinNoch keine Bewertungen
- A Ten Disk Procedure For The Detection of Antibiotic Resistance in EnterobacteriacaeDokument7 SeitenA Ten Disk Procedure For The Detection of Antibiotic Resistance in EnterobacteriacaeNguyen Huu HienNoch keine Bewertungen
- Natalie Williams-Bouyer, Barbara S. Reisner, Gail L. WoodsDokument4 SeitenNatalie Williams-Bouyer, Barbara S. Reisner, Gail L. WoodsBaruna AtmajaNoch keine Bewertungen
- Cefoxitin For AmpcDokument6 SeitenCefoxitin For AmpcmemossaNoch keine Bewertungen
- 18 35 1 SMDokument10 Seiten18 35 1 SMhud_fNoch keine Bewertungen
- Antibiotic Resistance Profile and Random AmplificationDokument10 SeitenAntibiotic Resistance Profile and Random Amplificationdanish.mahaitNoch keine Bewertungen
- Screening Canine Microbiota For Extended Spectrum Beta-LactamasesDokument5 SeitenScreening Canine Microbiota For Extended Spectrum Beta-LactamasesAjay SinghNoch keine Bewertungen
- Journal Homepage: - : Manuscript HistoryDokument6 SeitenJournal Homepage: - : Manuscript HistoryIJAR JOURNALNoch keine Bewertungen
- Auer 2010Dokument3 SeitenAuer 2010fsdfNoch keine Bewertungen
- ESBLDokument2 SeitenESBLCla ValenciaNoch keine Bewertungen
- Marulappa Kapil 2009 Simple Tests For Rapid Detection of Canine Parvovirus Antigen and Canine Parvovirus SpecificDokument5 SeitenMarulappa Kapil 2009 Simple Tests For Rapid Detection of Canine Parvovirus Antigen and Canine Parvovirus Specificara.lv007Noch keine Bewertungen
- 1 s2.0 S0167701213001899 MainDokument6 Seiten1 s2.0 S0167701213001899 MainMohammad Yusuf AlamudiNoch keine Bewertungen
- Molecular Characterization of Extended Spectrum BDokument6 SeitenMolecular Characterization of Extended Spectrum Banvet.fkhNoch keine Bewertungen
- Prevalence of Mec A Gene Positive Coagulase Negative StaphyloDokument6 SeitenPrevalence of Mec A Gene Positive Coagulase Negative Staphylosuresh151971Noch keine Bewertungen
- Klebsiella Pneumoniae Isolated From Urine ofDokument9 SeitenKlebsiella Pneumoniae Isolated From Urine ofInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- IMVicDokument3 SeitenIMVicSundus LiaquatNoch keine Bewertungen
- A Study On Antibiotic Susceptibility Pattern of Escherichia Coli Isolates From Extra Intestinal Infections in A Tertiary Care HospitalDokument8 SeitenA Study On Antibiotic Susceptibility Pattern of Escherichia Coli Isolates From Extra Intestinal Infections in A Tertiary Care HospitalIJAR JOURNALNoch keine Bewertungen
- Modified CLSIDokument8 SeitenModified CLSIGajah NauliNoch keine Bewertungen
- Analysis of molecular epidemiologic characteristics of extended-spectrum β-lactamase (ESBL)-producing Escherichia coliDokument6 SeitenAnalysis of molecular epidemiologic characteristics of extended-spectrum β-lactamase (ESBL)-producing Escherichia coliMiriam LeiNoch keine Bewertungen
- Pattern of Tem and SHV Genes in Esbl Producing Klebsiella PneumoniaeDokument9 SeitenPattern of Tem and SHV Genes in Esbl Producing Klebsiella Pneumoniaeijmb333Noch keine Bewertungen
- Detection of Genes TEM, OXA, SHV and CTX-M in 73 Clinical Isolates of Escherichia Coli Producers of Extended Spectrum Betalactamases and Determination of Their Susceptibility To Antibiotics.Dokument6 SeitenDetection of Genes TEM, OXA, SHV and CTX-M in 73 Clinical Isolates of Escherichia Coli Producers of Extended Spectrum Betalactamases and Determination of Their Susceptibility To Antibiotics.International Medical PublisherNoch keine Bewertungen
- Direct comparison of antimicrobial susceptibility testing methodsDokument5 SeitenDirect comparison of antimicrobial susceptibility testing methodsRoela GeeNoch keine Bewertungen
- Microbiology and Immunology - 2010 - Iorio - A Combination of Methods To Evaluate Biofilm Production May Help To DetermineDokument6 SeitenMicrobiology and Immunology - 2010 - Iorio - A Combination of Methods To Evaluate Biofilm Production May Help To DetermineAriane Barcellos Dos SantosNoch keine Bewertungen
- Susceptibility of Gram-Positive Cocci From 25 UK Hospitals To Antimicrobial Agents Including LinezolidDokument0 SeitenSusceptibility of Gram-Positive Cocci From 25 UK Hospitals To Antimicrobial Agents Including LinezolidGabriel MataNoch keine Bewertungen
- Ijaret 06 10 008Dokument6 SeitenIjaret 06 10 008IAEME PublicationNoch keine Bewertungen
- K.N.ravichitra, Et AlDokument5 SeitenK.N.ravichitra, Et AldindaNoch keine Bewertungen
- 11 0207 Umoluidia AmDokument7 Seiten11 0207 Umoluidia AmJohn Zedric Villanueva ArciagaNoch keine Bewertungen
- KJCM2018 75Dokument5 SeitenKJCM2018 75Jackie ChongNoch keine Bewertungen
- Journal of Clinical Microbiology 1975 Butler 322.fullDokument5 SeitenJournal of Clinical Microbiology 1975 Butler 322.fullRajNoch keine Bewertungen
- The Development and Application of An Indirect ELISA Test For The Detection of Antibodies To Bovine Respiratory Syncytial Virus in Blood SerumDokument6 SeitenThe Development and Application of An Indirect ELISA Test For The Detection of Antibodies To Bovine Respiratory Syncytial Virus in Blood SerumRani Khoiriyah Az-zahraNoch keine Bewertungen
- Vetsci 08 00249 v2Dokument8 SeitenVetsci 08 00249 v2hamza rahimNoch keine Bewertungen
- 5 Psae Egypt 2014Dokument9 Seiten5 Psae Egypt 2014Khoa Vi Sinh BVCRNoch keine Bewertungen
- Rapid Diagnosis of Entamoeba Infection by Using Entamoeba and Entamoeba Histolytica Stool Antigen Detection KitsDokument4 SeitenRapid Diagnosis of Entamoeba Infection by Using Entamoeba and Entamoeba Histolytica Stool Antigen Detection Kitsزيكو زيكوNoch keine Bewertungen
- Assessment of prevalence and changing epidemiology of extended-spectrum beta-lactamase-producing Enterobacteriaceae fecal carriers using a chromogenic mediumDokument4 SeitenAssessment of prevalence and changing epidemiology of extended-spectrum beta-lactamase-producing Enterobacteriaceae fecal carriers using a chromogenic mediumMiriam LeiNoch keine Bewertungen
- 2015 Article 436Dokument9 Seiten2015 Article 436Angie ZapataNoch keine Bewertungen
- GramocefcvDokument7 SeitenGramocefcvSilvio BarbosaNoch keine Bewertungen
- The Egg Hatch Test 2019Dokument7 SeitenThe Egg Hatch Test 2019maria elenaNoch keine Bewertungen
- 1153 Mic075762Dokument9 Seiten1153 Mic075762Abid SiddiquiNoch keine Bewertungen
- Candida MicDokument5 SeitenCandida MicKalpanaNoch keine Bewertungen
- COMPARATIVE ASSESSMENT OF ANTIBIOTIC SUSCEPTIBILITY IN ESBL AND NON-ESBL Klebsiella Pneumoniae IN A TERTIARY HOSPITALDokument8 SeitenCOMPARATIVE ASSESSMENT OF ANTIBIOTIC SUSCEPTIBILITY IN ESBL AND NON-ESBL Klebsiella Pneumoniae IN A TERTIARY HOSPITALijmb333Noch keine Bewertungen
- 3.8.1 Handout - Antibiotic Selection by Organism and Specimen TypeDokument7 Seiten3.8.1 Handout - Antibiotic Selection by Organism and Specimen TypeRidho WahyutomoNoch keine Bewertungen
- Teori Dasar Fluida: DR Ridha Wahyutomo, M.Arch, SPMK, FisquaDokument6 SeitenTeori Dasar Fluida: DR Ridha Wahyutomo, M.Arch, SPMK, FisquaRidho WahyutomoNoch keine Bewertungen
- 3.8.1 Handout - Antibiotic Selection by Organism and Specimen TypeDokument7 Seiten3.8.1 Handout - Antibiotic Selection by Organism and Specimen TypeRidho WahyutomoNoch keine Bewertungen
- Ambulans WskoDokument10 SeitenAmbulans WskoRidho WahyutomoNoch keine Bewertungen
- Core GP 2.1Dokument8 SeitenCore GP 2.1Ridho WahyutomoNoch keine Bewertungen
- Pathogenesis of Viral InfectionsDokument3 SeitenPathogenesis of Viral InfectionsRidho WahyutomoNoch keine Bewertungen
- J Clin Invest-Airway Remodelling-2003Dokument9 SeitenJ Clin Invest-Airway Remodelling-2003Ridho WahyutomoNoch keine Bewertungen
- Diabetes 6-4Dokument8 SeitenDiabetes 6-4Ridho WahyutomoNoch keine Bewertungen
- Diagram DNADokument2 SeitenDiagram DNARidho WahyutomoNoch keine Bewertungen
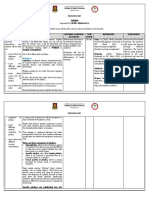
- PHARMACEUTICAL CARE PLAN-Pelatihan Dasar UGM 2006Dokument18 SeitenPHARMACEUTICAL CARE PLAN-Pelatihan Dasar UGM 2006Ridho WahyutomoNoch keine Bewertungen
- WHONET 8.cluster Detection and SaTScanDokument12 SeitenWHONET 8.cluster Detection and SaTScanRizaNoch keine Bewertungen
- Tugas MikroDokument9 SeitenTugas MikroRidho WahyutomoNoch keine Bewertungen
- Virus InfectionDokument9 SeitenVirus InfectionRidho WahyutomoNoch keine Bewertungen
- Tugas Mikro Satya BayuDokument10 SeitenTugas Mikro Satya BayuRidho WahyutomoNoch keine Bewertungen
- Materi Dr. Fera Ibrahim Share-TerkunciDokument41 SeitenMateri Dr. Fera Ibrahim Share-TerkunciRidho WahyutomoNoch keine Bewertungen
- BacLink 1.getting StartedDokument5 SeitenBacLink 1.getting StartedRidho WahyutomoNoch keine Bewertungen
- Dear ProfDokument2 SeitenDear ProfRidho WahyutomoNoch keine Bewertungen
- MICROBIOLOGYDokument25 SeitenMICROBIOLOGYRidho WahyutomoNoch keine Bewertungen
- Tugas Idk 4Dokument14 SeitenTugas Idk 4Ridho WahyutomoNoch keine Bewertungen
- Balanced Scorecard Slide 1Dokument11 SeitenBalanced Scorecard Slide 1Ridho WahyutomoNoch keine Bewertungen
- 2019-Ncoronavirus ADW 2020 PDFDokument60 Seiten2019-Ncoronavirus ADW 2020 PDFRidho WahyutomoNoch keine Bewertungen
- Bacterial InfectionsDokument6 SeitenBacterial InfectionsRidho WahyutomoNoch keine Bewertungen
- Group A StreptococcDokument3 SeitenGroup A StreptococcRidho WahyutomoNoch keine Bewertungen
- 3.1 Exercise Specimen ProcessingDokument2 Seiten3.1 Exercise Specimen ProcessingRidho WahyutomoNoch keine Bewertungen
- 3.3.1 Handout - Specimen MGTDokument5 Seiten3.3.1 Handout - Specimen MGTRidho WahyutomoNoch keine Bewertungen
- WHO Safety BoxDokument22 SeitenWHO Safety BoxRidho WahyutomoNoch keine Bewertungen
- Efecto de La Psicoeducación en Muejeres Que Realizan Estudios de MamografiaDokument14 SeitenEfecto de La Psicoeducación en Muejeres Que Realizan Estudios de MamografiaJessicaNoch keine Bewertungen
- Intimidation: A Tool of Learning? Do We Learn Better Under The Gun?Dokument39 SeitenIntimidation: A Tool of Learning? Do We Learn Better Under The Gun?Budi Iman SantosoNoch keine Bewertungen
- AcetazolamideDokument3 SeitenAcetazolamidejeihanalkhairNoch keine Bewertungen
- RSBY Hospital Manual 28072010Dokument44 SeitenRSBY Hospital Manual 28072010chimera03Noch keine Bewertungen
- Sexual terms dictionaryDokument3 SeitenSexual terms dictionaryGabriela L MarinNoch keine Bewertungen
- Interview QuestionsDokument4 SeitenInterview QuestionsJilian McGuganNoch keine Bewertungen
- Cpa PaperDokument4 SeitenCpa Paperapi-300623329Noch keine Bewertungen
- Contoh BAP Puskesmas BuntuliaDokument31 SeitenContoh BAP Puskesmas BuntuliaFathan BahilaNoch keine Bewertungen
- Interpret urinalysis results with this biochem lab finals reviewerDokument2 SeitenInterpret urinalysis results with this biochem lab finals reviewerMigs BernalNoch keine Bewertungen
- Drug Study BISACODYLDokument1 SeiteDrug Study BISACODYLAnna Sofia ReyesNoch keine Bewertungen
- LabelDokument9 SeitenLabelNadya Alkadza100% (1)
- UntitledDokument8 SeitenUntitledapi-86749355Noch keine Bewertungen
- Sp11 HE325 Sports NutritionDokument28 SeitenSp11 HE325 Sports NutritionHaydee CuencoNoch keine Bewertungen
- Seretide: What Is in This LeafletDokument6 SeitenSeretide: What Is in This LeafletJazmaine Karyle ChuaNoch keine Bewertungen
- F1-000728 MSDSDokument7 SeitenF1-000728 MSDScolinyNoch keine Bewertungen
- Coffea - The Best Homeopathic Medicine For Insomnia: Insomnia Treatment in HomeopathyDokument4 SeitenCoffea - The Best Homeopathic Medicine For Insomnia: Insomnia Treatment in HomeopathysharmadxNoch keine Bewertungen
- PHOBIADokument12 SeitenPHOBIAAbdul Azis G. CamidNoch keine Bewertungen
- Applejuice As DegreaserDokument26 SeitenApplejuice As DegreaserKaryle Anne Surban TabianNoch keine Bewertungen
- Counseling Methods ExplainedDokument10 SeitenCounseling Methods ExplainedSha CalsesNoch keine Bewertungen
- Pretest Intravenous Therapy and Blood Transfusion NCM 118-RLE Part 1. Label The Following. 39 PointsDokument5 SeitenPretest Intravenous Therapy and Blood Transfusion NCM 118-RLE Part 1. Label The Following. 39 Pointsgabrielle magdaraogNoch keine Bewertungen
- 21 Doxofylline PDFDokument10 Seiten21 Doxofylline PDFBaru Chandrasekhar RaoNoch keine Bewertungen
- 01 01 08Dokument12 Seiten01 01 08brains26100% (1)
- OesophagusDokument15 SeitenOesophagusIBRAHEM JUMAHNoch keine Bewertungen
- Pre Op NursingDokument11 SeitenPre Op NursingS01164503Noch keine Bewertungen