Beruflich Dokumente
Kultur Dokumente
Cross-Covering The Well Baby Nursery and Pedi-Med Service: Intensive Care Nursery House Staff Manual
Hochgeladen von
Sedaka DonaldsonOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Cross-Covering The Well Baby Nursery and Pedi-Med Service: Intensive Care Nursery House Staff Manual
Hochgeladen von
Sedaka DonaldsonCopyright:
Verfügbare Formate
Intensive Care Nursery House Staff Manual
Cross-Covering the Well Baby Nursery and Pedi-Med Service
INTRODUCTION: This section of helpful tips was prepared with the help of past residents who suffered through cross-covering infants on the Well-Baby and Pedi-Med Service without the benefit of a readily available manual. ATTENDING PHYSICIANS: The attendings for the Well Baby and Pedi-Med Service are your direct backup and should be called for questions about clinical management, complications, and for all admissions to the Special Care Nursery under the Pedi-Med Service. Remember to identify the on-call attending at evening sign-out rounds. Pager Attending Pager Attending Jane Anderson 719-1884 Thomas Newman 719-1262 David Becker 719-6089 Marina Tan 719-8995 Jane Lee 719-5355 Alan Uba 719-2126 Carol Miller 719-3837 CRITERIA FOR PLACING INFANTS ON THE VARIOUS SERVICES: 1. Well Baby Nursery (WBN) is intended for term and near-term infants who are sufficiently stable for rooming-in with their mothers. All infants admitted to the WBN must satisfy all of the following criteria: Gestation 36 weeks Birth weight 2200 grams No major congenital anomalies Temperature is stable without the need of an incubator or warmer No need for continuous electronic cardio-respiratory monitoring No need for intravenous lines, nasal/oral gastric tubes, or similar interventions 2. Pedi-Med Service: Infants who require more medical observation or treatment than the well babies. These infants should be placed in the High Observation Nursery or Special Care Nursery and must satisfy all of the following criteria: Gestation 33 weeks No significant apnea or bradycardia Birth weight 2200 grams No ventilator support No central vascular catheters No intravenous alimentation No baby determined to be unstable Note: These criteria can be modified only by the attending physician. Infants who do not meet the criteria for either the Well Baby Nursery or the Pedi-Med Service are to be placed on the ICN Service. BREASTFEEDING is to be encouraged. Our goal is to assure that all families who elect to breastfeed their infants will have a successful and satisfying experience. Please note the following: Infants are to be put to breast as soon after birth as feasible for both mother and infant, ideally within the first hour after birth. Breastfeeding mother-infant pairs are encouraged to room-in together on a 24h basis. Encourage the infant to nurse at least q2-3h for a minimum of 8 feedings per 24h.
74
Copyright 2004 The Regents of the University of California
Well Baby Nursery Pedi-Med Service
No supplementary water or milk is to be given unless ordered by a physician or nurse practitioner for medical indications. Please refer to the document Breastfeeding Well Newborns in the Well Baby Nursery Manual, a black notebook kept in the WBN chart rack. VITAMIN K1 ADMINISTRATION: Every neonate should receive a single parenteral 0.5-1.0 mg dose of vitamin K oxide or phytonadione (AquaMEPHYTON) within 1h of birth for prevention of vitamin K deficiency bleeding (Hemorrhagic Disease of the Newborn). Occasionally parents will refuse vitamin K or request oral administration. If you encounter this situation: Discuss this with parents. Try to use a non-confrontational tone. Be respectful and listen attentively to the parents reasoning and concerns. Provide honest answers and be sure to clarify the purpose of our recommendation. It is often helpful to describe vitamin K deficiency bleeding to parents. Orally administered vitamin K has not been shown to be as effective and puts infants at risk for late onset vitamin K deficiency bleeding which is associated with a higher incidence of intracranial hemorrhage. If parents persist in their refusal, they must sign the Refusal to Permit Medical Treatment form. These forms are kept in the file cabinet behind the unit clerks desk in the WBN. Circumcision will not be performed on any infant who has not received vitamin K by injection. EYE PROPHYLAXIS against gonococcal opthalmia neonatorum is mandatory for all neonates. A 1-2cm ribbon of sterile ophthalmic ointment containing 0.5% erythromycin should be administered within 1 hour of birth. Although California state law mandates neonatal eye prophylaxis, parents who refuse may sign a special waiver. This form is entitled Refusal to Allow Treatment of Eyes of Infant with Prophylactic-Efficient Agent and is located in the cabinet behind the unit clerks desk in the WBN. HYPERBILIRUBINEMIA: Risk factors for non-physiologic hyperbilirubinemia include: Blood group or Rh incompatibility, especially if there is a positive Direct Antiglobulin Test (Coombs Test) Presence of excessive bruising or cephalohematoma Breastfeeding Excessive weight loss Gestational age < 37 weeks Maternal diabetes Polycythemia Consider ordering a total serum bilirubin for jaundiced neonates with risk factors. Start phototherapy as follows: Age(hours) Total Bilirubin(mg/dL) <48 15 49-72 18 >72 20
75
Copyright 2004 The Regents of the University of California
Well Baby Nursery Pedi-Med Service
Further testing to determine the etiology of hyperbilirubinemia should be individualized, taking into account the maternal/prenatal and family history, physical exam and general clinical setting. HYPOGLYCEMIA: Risk factors for hypoglycemia include: SGA/IUGR with birth weight 2500 grams LGA (birth weight 4200 grams) Preterm (<36 weeks gestation) Post-term (42 weeks gestation) Infant of a diabetic mother or GIP (glucose intolerance of pregnancy) Polycythemia An initial blood glucose level is checked on all neonates within 2 hours post delivery by the One-Touch Glucometer method. Neonates with any risk factor are monitored with repeated glucose levels at the following ages: hour (insulin dependent mothers only), 1h, 2h, 4h, 6h, 9h, 12h, and 24h post delivery. Treatment of hypoglycemia: If blood glucose is 40 mg/dL, no intervention or oral supplementation is needed. If blood glucose is 20-40 mg/dL: -Recheck value. If still low, send blood sample to Clinical Laboratories STAT for glucose level. -Nipple feed immediately D5W, a minimum of 5-10 cc/kg. -Recheck blood glucose 20-30 min after nipple feed has been completed. -If low glucose level persists, repeat oral glucose supplementation and consider IV infusion (see below). -Continue to monitor blood glucose levels per above protocol. If blood glucose is <20 mg/dL: -Send blood sample to Clinical Laboratories for STAT glucose measurement. -Immediately nipple feed D5W at 10 cc/kg. -Recheck blood glucose 20 min after oral supplement. If blood glucose is still low transfer to SCN for intravenous infusion. Intravenous infusion for persistent hypoglycemia: -Give initial bolus of D10W IV at 2-4 cc/kg. -Continue IV infusion of D10W at 4-8 mg/kg/min. -Recheck blood glucose 20 min after starting infusion. If glucose is still low, consider increasing infusion by 2-4 mg/kg/min. -If infusion rate reaches >140 cc/kg/24h, increase glucose concentration to D12.5W. -Central line placement is required if D15W is necessary to maintain normal blood glucose level. If central line placement becomes necessary, transfer infant to Neonatology team. Do not use 25% or 50% glucose as IV treatment. These will raise blood glucose to very high levels and cause rebound hypoglycemia. SEPSIS, HIV, AND HEPATITIS: Please refer to the sections on infectious diseases in this manual.
76
Copyright 2004 The Regents of the University of California
Well Baby Nursery Pedi-Med Service
TOXICOLOGY SCREENING: Urine toxicology screen should be ordered under the following circumstances; Maternal history of illicit substance use or abuse of prescription medication. Mother has received 3 prenatal visits. Infant exhibits symptoms of exposure to drugs or alcohol. These include but are not limited to: high-pitched cry, difficult to console, hypertonicity, excessive stooling, sneezing, temperature instability, hyperphagia or poor feeding. Maternal consent is not required to obtain a urine toxicology screen on an infant. However, it is our practice to inform the mother that the test has been ordered. MANAGEMENT OF DRUG WITHDRAWAL SYNDROME: Treatment of infants exhibiting signs and symptoms of drug withdrawal should be tailored according to severity. Use of the Neonatal Abstinence Scoring Sheet is a helpful tool for measuring severity, monitoring progression and monitoring effect of treatment. Fifteen items are assigned a numerical score generally by the nursing staff once during each nursing shift. For total scores <12, non-drug interventions such as swaddling, placement in a quiet location with diminished lighting, and rhythmical motion such as a swing are often sufficient. For total scores 12 or greater, environmental measures may need to be augmented with medication such as Tincture of Opium (DTO), Phenobarbital or other sedatives. Infants housed in the WBN who require medications which may depress respiration should be transferred to the Special Care Nursery and placed on a cardio-respiratory monitor. (See section on Perinatal Substance Abuse, P. 172). POLICE HOLD POLICY: A Police Hold is a process whereby the police place an infant or minor child in temporary protective custody of the Juvenile Court. It removes physical custody from the parents or guardians, and prevents the family from removing the child from the hospital without the express permission of Child Protective Services. While on a police hold, parents retain legal custody and may continue to consent to treatment and procedures. To initiate a police hold, contact the UCSF Police Department. Circumstances which necessitate a police hold include: A parent threatens to remove a baby against medical advice, and the discharge is medically unsound and/or life threatening. A parent is violent or is threatening violence. A parent is incapacitated by drugs or alcohol and the babys immediate safety is in question. A parent is incapacitated by mental illness and the babys immediate safety is in question. Parents must be informed of the hold by the medical staff. A police hold does not necessarily prevent parents from visiting and participating in their infants care. However the hospital has the right to set limits on visitation to ensure patient, staff and visitor safety. Nursing will ensure that all visits are supervised. The entire Police Hold Policy can be found in the Well Baby Nursery Manual.
77
Copyright 2004 The Regents of the University of California
Well Baby Nursery Pedi-Med Service
ADDITIONAL USEFUL TIPS FROM RESIDENTS: The most important thing to remember is that even though you are the ICN resident, these are not ICN babies. Most well babies require no [invasive] interventions. If you write orders in the WBN, tell the nurses because they only run the charts once per shift. If you are called to a delivery, please fill out the Newborn Assessment Part I. If for some reason you do not have time, at least fill out the section on peripartum and postpartum interventions. Call the ICN charge nurse to advise her of Pedi-Med admissions.
78
Copyright 2004 The Regents of the University of California
Das könnte Ihnen auch gefallen
- ARCS Paediatric IV Fluid GuidelinesDokument16 SeitenARCS Paediatric IV Fluid GuidelinesWidyadarya Triyono PutriNoch keine Bewertungen
- Dischargeplanning: Brian M. BarkemeyerDokument12 SeitenDischargeplanning: Brian M. BarkemeyerAfnizar WAhyu RamadhanNoch keine Bewertungen
- PQCNC 2024 Kickoff LPI ARMC 20240110Dokument41 SeitenPQCNC 2024 Kickoff LPI ARMC 20240110kcochranNoch keine Bewertungen
- Neonatal JaundiceDokument12 SeitenNeonatal JaundiceKim DeyNoch keine Bewertungen
- Neonatal Jaundice Clinical Practice GuidelineDokument35 SeitenNeonatal Jaundice Clinical Practice GuidelineprinsepejesseNoch keine Bewertungen
- Newborn ScreeningDokument18 SeitenNewborn ScreeningKayNoch keine Bewertungen
- G HypoglyDokument39 SeitenG Hypoglykaydee.arNoch keine Bewertungen
- Document 32Dokument3 SeitenDocument 32Grace CruzNoch keine Bewertungen
- 947 Newly Diagnosed Diabetic ChildDokument16 Seiten947 Newly Diagnosed Diabetic ChildRohit BharadwajNoch keine Bewertungen
- Lactation Consultant - Practice & Referral GuidelinesDokument7 SeitenLactation Consultant - Practice & Referral GuidelinesYwagar YwagarNoch keine Bewertungen
- NICU MedsDokument9 SeitenNICU Medshnj43047Noch keine Bewertungen
- BFHIDokument10 SeitenBFHIArchana Sahu100% (1)
- Phototherapy On The Postnatal WardDokument5 SeitenPhototherapy On The Postnatal WardYwagar Ywagar100% (1)
- H1N1 Influenza-: Directorate of Health Services, Kerala GuidelinesDokument5 SeitenH1N1 Influenza-: Directorate of Health Services, Kerala Guidelinesusa01Noch keine Bewertungen
- Post Mature Neonate, Infant of Diabetic and Substance Abuse MotherDokument14 SeitenPost Mature Neonate, Infant of Diabetic and Substance Abuse MotherShilpa JoshiNoch keine Bewertungen
- IMCI Basic Pedia 2015 PPTDokument77 SeitenIMCI Basic Pedia 2015 PPTCharles DoradoNoch keine Bewertungen
- DocumentDokument2 SeitenDocumentAsri Rachmawati100% (1)
- Expanded Newborn ScreeningDokument27 SeitenExpanded Newborn ScreeningCelline Isabelle ReyesNoch keine Bewertungen
- Newborn Care Free Online EditionDokument452 SeitenNewborn Care Free Online EditionMayeso E. ChikwalikwaliNoch keine Bewertungen
- Diarroea Nice Guidlines PDFDokument16 SeitenDiarroea Nice Guidlines PDFFayzaRayesNoch keine Bewertungen
- Diarrhoea and Vomiting in ChildrenDokument16 SeitenDiarrhoea and Vomiting in ChildrenKenny Josef100% (1)
- NUH - Hello BabyDokument32 SeitenNUH - Hello BabyTony AndersonNoch keine Bewertungen
- Newborn Screening: Colegio de San LorenzoDokument38 SeitenNewborn Screening: Colegio de San LorenzoMikhail Joshua PresinculaNoch keine Bewertungen
- Neonatal SepsisDokument20 SeitenNeonatal SepsisJustine Nyangaresi100% (1)
- Newborn ScreeningDokument20 SeitenNewborn Screeningfeva55Noch keine Bewertungen
- Baby Friendly Hospital Initiative and Exclusive Breast FeedingDokument92 SeitenBaby Friendly Hospital Initiative and Exclusive Breast Feedingvarshasharma05Noch keine Bewertungen
- Background : BDH Polices & Procedures On Universal Newborn ScreeningDokument21 SeitenBackground : BDH Polices & Procedures On Universal Newborn ScreeningJnana YumnaNoch keine Bewertungen
- Neonatal Jaundice Pathway PDFDokument35 SeitenNeonatal Jaundice Pathway PDFarjunaquellNoch keine Bewertungen
- Maternal and Child Health Programmes AssignmentDokument11 SeitenMaternal and Child Health Programmes Assignmentannu panchal80% (5)
- Follow-Up of High-Risk Newborn: DR Ankur PriyadarshiDokument90 SeitenFollow-Up of High-Risk Newborn: DR Ankur PriyadarshiAnkur PriyadarshiNoch keine Bewertungen
- Legal MandatesDokument39 SeitenLegal MandatesMarkGuirhem100% (1)
- Breastfeeding NHS Guidelines 2011-2013Dokument2 SeitenBreastfeeding NHS Guidelines 2011-2013Natalie KwongNoch keine Bewertungen
- Prevention of Mother-To-Child Transmission (PMTCT) ARV ProphylaxisDokument5 SeitenPrevention of Mother-To-Child Transmission (PMTCT) ARV ProphylaxisLassie AbusadoNoch keine Bewertungen
- (P) Neonatal Hypoglycaemia Dec15Dokument11 Seiten(P) Neonatal Hypoglycaemia Dec15kaydee.arNoch keine Bewertungen
- Chapter 71: Acute Gastroenteritis: Is The Child in Shock? Any Child With Shock Go Straight To Treatment Plan CDokument5 SeitenChapter 71: Acute Gastroenteritis: Is The Child in Shock? Any Child With Shock Go Straight To Treatment Plan CKalichandren ArumugamNoch keine Bewertungen
- Newborn Careplan 9-15-2011Dokument17 SeitenNewborn Careplan 9-15-2011Brittany Wood100% (1)
- Neonatal Jaundice PathwayDokument35 SeitenNeonatal Jaundice PathwayMcmac YangoNoch keine Bewertungen
- Teaching Plan On Newborn ScreeningDokument8 SeitenTeaching Plan On Newborn ScreeningQueenie Sicco100% (1)
- Test Sas 16, 17 & 18 Nur 151 Cooa A4: Questions 1 To 10Dokument2 SeitenTest Sas 16, 17 & 18 Nur 151 Cooa A4: Questions 1 To 10Sistine Rose LabajoNoch keine Bewertungen
- Integrated Management of Neonatal and Childhood IllnessDokument44 SeitenIntegrated Management of Neonatal and Childhood IllnessJils SureshNoch keine Bewertungen
- Well Baby 2020 With NotesDokument119 SeitenWell Baby 2020 With NotesSamsam Almarez BacaltosNoch keine Bewertungen
- New Born ClassificationDokument47 SeitenNew Born ClassificationEyob MizanNoch keine Bewertungen
- Baby Friendly Hospital Initiative (Bfhi)Dokument9 SeitenBaby Friendly Hospital Initiative (Bfhi)Ankita BramheNoch keine Bewertungen
- Pediatric RemediationDokument5 SeitenPediatric RemediationAlvin L. Rozier67% (3)
- Hypertensive Disease in Pregnancy - 1Dokument44 SeitenHypertensive Disease in Pregnancy - 1Dr.Senthil KumarNoch keine Bewertungen
- Adaptation of The Integrated Management of Newborn and Childhood Illness (IMNCI) Strategy For IndiaDokument23 SeitenAdaptation of The Integrated Management of Newborn and Childhood Illness (IMNCI) Strategy For IndiaMona MorrisNoch keine Bewertungen
- Cmam in NigeriaDokument27 SeitenCmam in NigeriaFaisalJRahujoNoch keine Bewertungen
- Neonatal JaundiceDokument65 SeitenNeonatal JaundiceAditi BanerjeeNoch keine Bewertungen
- New Born ScreeningDokument30 SeitenNew Born ScreeningJastine Miguel EGUIANoch keine Bewertungen
- NCLEX EndocrineDokument21 SeitenNCLEX EndocrineChristopher Harris100% (7)
- Guidelines For DoctorsDokument4 SeitenGuidelines For DoctorsNazar KaNoch keine Bewertungen
- IMNCIDokument6 SeitenIMNCIleevuanuNoch keine Bewertungen
- Acute Care PathwaysDokument78 SeitenAcute Care PathwaysRachel Niu IINoch keine Bewertungen
- IMNCI Cahrtbooklet 2016-1Dokument82 SeitenIMNCI Cahrtbooklet 2016-1AyenewNoch keine Bewertungen
- NCM 104 Lec Reviewer FinalsDokument11 SeitenNCM 104 Lec Reviewer FinalsFERNANDEZ, RELLY ANDREWNoch keine Bewertungen
- Postnatal Care of Mother and Newborn: WHO Guidelines OnDokument14 SeitenPostnatal Care of Mother and Newborn: WHO Guidelines OnSuman GuptaNoch keine Bewertungen
- IMNCI Part - IDokument72 SeitenIMNCI Part - IKedir AhmedNoch keine Bewertungen
- Newborn Blood Spot Screening: What?Dokument7 SeitenNewborn Blood Spot Screening: What?madimadi11Noch keine Bewertungen
- Basic Surg SkillsDokument32 SeitenBasic Surg Skillszamurd76Noch keine Bewertungen
- Platinum Wholesale ListDokument296 SeitenPlatinum Wholesale ListSedaka Donaldson100% (2)
- Obstetrical History FormatDokument7 SeitenObstetrical History FormatSedaka DonaldsonNoch keine Bewertungen
- Emergency MedicineDokument71 SeitenEmergency MedicineSedaka DonaldsonNoch keine Bewertungen
- Emergency Care SeminarDokument136 SeitenEmergency Care SeminarSedaka DonaldsonNoch keine Bewertungen
- 1000 WholesalersDokument102 Seiten1000 WholesalersSedaka Donaldson0% (1)
- Anesthesiology Goals and ObjectivesDokument261 SeitenAnesthesiology Goals and ObjectivesSedaka DonaldsonNoch keine Bewertungen
- Bed Sore 48Dokument45 SeitenBed Sore 48Sedaka DonaldsonNoch keine Bewertungen
- Wound Closure ManualDokument127 SeitenWound Closure ManualDougyStoffell100% (5)
- DM Foot CareDokument27 SeitenDM Foot CareKatrina KattNoch keine Bewertungen
- European Urology Residency Curriculum by EBU - Web FormDokument43 SeitenEuropean Urology Residency Curriculum by EBU - Web FormParpauts KarolinaNoch keine Bewertungen
- 2001 RecentDokument5 Seiten2001 RecentSedaka DonaldsonNoch keine Bewertungen
- Diabetic-Foot-Ulcer Presentation MUST 22Dokument161 SeitenDiabetic-Foot-Ulcer Presentation MUST 22Sedaka DonaldsonNoch keine Bewertungen
- Braden ScaleDokument1 SeiteBraden ScaleRandall StevensNoch keine Bewertungen
- Obstetric ComplicationsDokument171 SeitenObstetric Complications2012100% (1)
- Neurology HX and Physical (NUR53-1061)Dokument6 SeitenNeurology HX and Physical (NUR53-1061)Sedaka DonaldsonNoch keine Bewertungen
- Fluid and Electrolyte Balance in NeurosurgeryDokument92 SeitenFluid and Electrolyte Balance in NeurosurgerySedaka DonaldsonNoch keine Bewertungen
- Anesthesiology Clerkship Rotation Handbook2004Dokument59 SeitenAnesthesiology Clerkship Rotation Handbook2004Sedaka DonaldsonNoch keine Bewertungen
- Talk05 SouweidaneBigHeadsDokument40 SeitenTalk05 SouweidaneBigHeadsSedaka DonaldsonNoch keine Bewertungen
- Barry E. Kosofsky, MD, PHD Adapted From Wayne Blount, MDDokument34 SeitenBarry E. Kosofsky, MD, PHD Adapted From Wayne Blount, MDSedaka DonaldsonNoch keine Bewertungen
- Tulane Surgery Resident Policy and Procedures Manual: Updated July 1, 2011Dokument57 SeitenTulane Surgery Resident Policy and Procedures Manual: Updated July 1, 2011sedaka26Noch keine Bewertungen
- 2001 SystemicDokument5 Seiten2001 SystemicSedaka DonaldsonNoch keine Bewertungen
- 2001 RecentDokument5 Seiten2001 RecentSedaka DonaldsonNoch keine Bewertungen
- New Patient FormDokument5 SeitenNew Patient FormSedaka DonaldsonNoch keine Bewertungen
- Obstetrics Study Guide 3 Mitra Ahmad Soltani 2008Dokument172 SeitenObstetrics Study Guide 3 Mitra Ahmad Soltani 2008Sedaka DonaldsonNoch keine Bewertungen
- 2001 BasicDokument5 Seiten2001 BasicSedaka DonaldsonNoch keine Bewertungen
- 2001 NeonatalDokument5 Seiten2001 NeonatalSedaka DonaldsonNoch keine Bewertungen
- International Observership HandbookDokument51 SeitenInternational Observership HandbookSedaka DonaldsonNoch keine Bewertungen
- Essentials For Students Preface A Career in Plastic SurgeryDokument3 SeitenEssentials For Students Preface A Career in Plastic SurgerySedaka DonaldsonNoch keine Bewertungen
- Introduction Table of Contents and Preface - Updatedaug2012Dokument8 SeitenIntroduction Table of Contents and Preface - Updatedaug2012Sedaka DonaldsonNoch keine Bewertungen
- Office of The Information and Privacy Commissioner of Alberta - Public Inquiry 005994, University of Alberta Freedom of Information RequestDokument60 SeitenOffice of The Information and Privacy Commissioner of Alberta - Public Inquiry 005994, University of Alberta Freedom of Information RequestWilliam Makis100% (3)
- Pathophysiology of Pain in BiliodigestiDokument19 SeitenPathophysiology of Pain in Biliodigestiprabowoaji12Noch keine Bewertungen
- Pricing Reimbursement of Drugs and Hta Policies in FranceDokument20 SeitenPricing Reimbursement of Drugs and Hta Policies in FranceHananAhmedNoch keine Bewertungen
- Low VisionDokument7 SeitenLow VisionUme HabibaNoch keine Bewertungen
- Assingment Food Mic 245Dokument2 SeitenAssingment Food Mic 245Ainnur SyamiraNoch keine Bewertungen
- MalariaDokument21 SeitenMalariayusak tapakedingNoch keine Bewertungen
- Atracurium BesylateDokument3 SeitenAtracurium BesylateAP TOROBXNoch keine Bewertungen
- Va Inspector Report 3Dokument100 SeitenVa Inspector Report 3Jeff MorrisNoch keine Bewertungen
- A Collective Expression of Indignation and A Call To ActionDokument5 SeitenA Collective Expression of Indignation and A Call To ActionRapplerNoch keine Bewertungen
- Magnesium SulphateDokument9 SeitenMagnesium SulphateNatália A. OliveiraNoch keine Bewertungen
- Altamash Shabbir Maniyar Resume 22-05-2023-04-03-54 230601 200613Dokument3 SeitenAltamash Shabbir Maniyar Resume 22-05-2023-04-03-54 230601 200613Kanhaiya VermaNoch keine Bewertungen
- Perioperative Patient CareDokument6 SeitenPerioperative Patient CareClark LlameraNoch keine Bewertungen
- Oral SURGERY REVALIDA1Dokument27 SeitenOral SURGERY REVALIDA1Bea Y. Bas-ongNoch keine Bewertungen
- Sujok Global MagazineDokument52 SeitenSujok Global MagazineNidhi ShahNoch keine Bewertungen
- Case Study Orientation SlidesDokument88 SeitenCase Study Orientation SlidesJoseph Emmanuel CandaNoch keine Bewertungen
- Drug Safety Priorities 2021: Center For Drug Evaluation and ResearchDokument52 SeitenDrug Safety Priorities 2021: Center For Drug Evaluation and ResearchSamaa Al TabbahNoch keine Bewertungen
- Nursing Care Plan: Course InstructorsDokument11 SeitenNursing Care Plan: Course InstructorsFatema AlsayariNoch keine Bewertungen
- For PrintDokument17 SeitenFor Printexample mailNoch keine Bewertungen
- SAFE520bP - Injury ReportDokument1 SeiteSAFE520bP - Injury ReportMiracle DavidNoch keine Bewertungen
- Suture Size: SmallestDokument2 SeitenSuture Size: SmallestGeraldine BirowaNoch keine Bewertungen
- Acute Poststreptococcal GlomerulonephritisDokument58 SeitenAcute Poststreptococcal GlomerulonephritisALI MUMTAZNoch keine Bewertungen
- Resume Template PharmacistDokument1 SeiteResume Template PharmacistHammad AslamNoch keine Bewertungen
- Alemnesh MandeshDokument94 SeitenAlemnesh MandeshDNoch keine Bewertungen
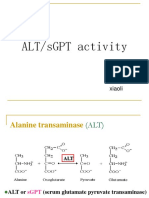
- SgotsgptDokument23 SeitenSgotsgptUmi MazidahNoch keine Bewertungen
- Comparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyDokument9 SeitenComparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyBaru Chandrasekhar RaoNoch keine Bewertungen
- (Ped-W1) (Dr. Zuhair M. Al Musawi) Repiratory 2Dokument43 Seiten(Ped-W1) (Dr. Zuhair M. Al Musawi) Repiratory 2Haider Nadhem AL-rubaiNoch keine Bewertungen
- DGN ExamDokument5 SeitenDGN ExamMaiga Ayub HusseinNoch keine Bewertungen
- Anti Dumping DietDokument3 SeitenAnti Dumping DietFelixDrummaruNoch keine Bewertungen
- Draft Examination Timetable For Msu Mid-Semester Examination, February 2016 SessionDokument279 SeitenDraft Examination Timetable For Msu Mid-Semester Examination, February 2016 SessionRebecca ChenNoch keine Bewertungen
- Presented by Amir Sadaula BVSC & Ah, 8 Sem Rampur Campus Roll No: 01Dokument19 SeitenPresented by Amir Sadaula BVSC & Ah, 8 Sem Rampur Campus Roll No: 01naturalamirNoch keine Bewertungen