Beruflich Dokumente
Kultur Dokumente
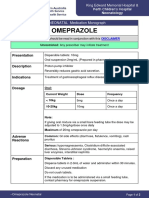
Drug Name
Hochgeladen von
dwyanejinOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Drug Name
Hochgeladen von
dwyanejinCopyright:
Verfügbare Formate
DRUG NAME Generic Name: amiodarone hydrochloride
ACTION
INDICATION Only for treatment of the following documented lifethreatening recurrent ventricular arrhythmias that do not respond to other treatment
CONTRAINDICATION Contraindicated with allergy to amiodarone Sinus node dysfunction Heart block Severe bradycardia Hypokalemia Lactation Use cautiously with thyroid dysfunction and pregnancy.
ADVERSE REACTION CNS: malaise, fatigue, dizziness, tremors, ataxia, lack of coordination CV: cardiac arrhythmias, heart failure, cardiac arrest, hypotension GI: nausea and vomiting, anorexia, constipation, hepatotoxicity RESPIRATORY: pulmonary toxicity, pneumonitis
NURSING RESPONSIBILITIES Monitor cardiac rhythm continuously Monitor for an extended period when dosage adjustment is made. Give drug with meals to decrease GI problems. Arrange for ophthalmologic examinations; reevaluate at any sign of optic neuropathy. Arrange for period of cheat x-ray to evaluate pulmonary status( every3-6 months)
Type III antiarrhythmic: acts directly on cardiac cell membrane; prolong Brand Name: repolarization and Cordarone refractory period; increases ventricular Drug fibrillation threshold; acts Classification: on peripheral smooth Antiarrhythmic muscle to decrease Adrenergic blocker peripheral resistance.
DOSAGE
DRUG NAME Generic Name: adenosine Brand Name: Adenoscan Drug Classification: Antiarrhythmic Diagnostic agent
ACTION Acts rapidly to slow down conduction throughthe AV node via the alpha 1 receptors. It also mediates peripheral and coronary vasodilation by stimulating the alpha 2 receptor
INDICATION Treatment for paroxysmal supraventricular tachycardias Myocardial imaging
CONTRAINDICATION Contraindicated with 2nd or 3rd degree heart block and sick sinus syndrome Astma Hypersensitivity pregnancy
ADVERSE REACTION CV: facial flushing, palpitations, chest pain, bradycardia, sweating, hypotension
NURSING RESPONSIBILITIES Maintain emergency equipment on stand by and monitor continually. Have methylthines available as antidote
DOSAGE Adults: Initially 3 mg by rapid IV injection into a central or large peripheralvein over 2 sec with cardiac monitoring.
DRUG NAME Generic Name: atropine sulfate Brand Name: Sal-tropine Drug Classification: Anticholinergic antidote Antiparkinsonian Belladonna alkaloid parasympatholytic
ACTION Competitively blocks the effect of acetylcholine at muscarinic cholinergic receptors that mediate the effects of parasympatheticpostgangl ionic impulses: also blocks th acethylcholine in the CNS
INDICATION
CONTRAINDICATION
ADVERSE REACTION
NURSING RESPONSIBILITIES
DOSAGE Adults: 0.4-0.6 mg PO, IM.IV or SQ. Surgery: 0.5 IMor IV or SQ before induction of anesthesia Antidote: for cholinesterase poisoning give large doses atleast 23 mg parenterally.
Treatment of Contraindicated with parkinsonism; glaucoma, adhesion between relieves tremors iris and lens, stenosing peptic and rigidity ulcer; bladder neck Restoration of obstruction; bronchial cardiac rate and asthma; cardiac arrhtymias; arterial pressure tachycardia during anesthesia Impaired when vagal metabolic,hepaticor renal stimulation function produce by intra Use cautiously with down abdominal traction syndrome, brain causes a decrease damage,spasticity, in pulse rate. hypertension and lactation. Relieve of bradycardia and syncope due to hyperactive carotid sinus reflex Relaxation of the spasm of biliary and ureteral colic and brochospasm Management of peptic ulcer Relaxation of uterine hypertonicity Antidote for cholinesterase inhibitors
CNS: Blurred vision, cyclopegia, Ensure adequate hydration; provide photophobia,increase IOP, environmental control (temperature) to headache, flushing, weakness, prevent hyperpyrexia. dizziness, mental confusion or Hve patient void before taking medication excitement. if urinary retention s problem. CV: palpitations, bradycardia(low Advise the patient to tkake drugs as dose), tachycardia (high Dose) prescribed, 30 minutes before meals; avoid excessive dosage GI: Dry mouth,altered taste Advise the patient to avoid hot perception, nausea, environment due to heat intolerance. vomiting,dysphagia, heartburn, Advise also to reportif theres rash , paralytic ileus flushing, difficulty of breathing, irregular heartbeat, palpitation, loss of coordination GU: Urinary hesitancy and and tremors. retention; impotence Other: decrease sweating and predisposition to heat prostration
DRUG NAME Generic Name: epinephrine Brand Name: Adrenaline chloride
ACTION Naturally occurring neurotransmitter. Effects on alpha receptors, vasoconstriction, contraction of the muscle dilator of the iris. Effects on Beta receptors includes positive chronotropic and inotropic effects of the heart (beta-1 receptor) bronchodilation, vasodilation and uterine relaxation (beta-2 receptors) DOSAGE Adults: Epinephrine ijection Cardiac arrest: 0.51mg(5-10ml of 1:10,000 solution) IV or intracardiac injection into left ventricular chamber, during resuscitation, 0.5 mg every 5 minutes. Inhalation (aerosol) Begin treatment at first symptom of bronchospasm.
INDICATION IV: Treatment & prophylaxis of cardiac arrest and attacks of transitory AV heart block with syncopal seizures ( stokes-adam syndrome) ; acute hypersensitivity (anaphylactoid) reactions,serum sickness, in acute asthmatic attacks to relieve bronchospasm not controlled b inahalation or subcutaneous injection. Injection: Relieffrom respiratory distress of bronchial asthma,chronic bronchitis and emphysema, other COPDs 0.1% ophthalmic solution: Cojunctivitis, during eye surgery to control bleeding.
CONTRAINDICATION Contraindicated with hypersensitivity to epinephrine. Narrow angle glaucoma Shock other than anaphylactic shock Hypovolemia General anesthesia with cyclopropane Organic brain damage Cardiac dilation and insufficiency DM Hyperthyroidism Lactation Use cautiously with prostatic hypertrophy (may cause bladder sphincter spasm, difficult and painful urination), Hiistory of seizure disorder, labor and delivery (may delay 2nd stage of labor, can accelerate fetal heart beat; may cause fetal and maternal hypoglycemia)
ADVERSE REACTION CNS: Fear, anxiety, restlessness, headache, lightheadedness, dizziness, drowsiness, tremor CV: Arrythmias, hypertension resulting in intracranial hemorrhage, CV collapse with hypotension, palpitations GI: nausea, vomiting, anorexia. GU:Constriction of renal blood vesselsand decrease urine formation, dysuria, vesical sphincter spasm Other: Pallor, respiratory difficulty, sweating Local injection Necrosis at site of repeat injection (due to intense vasoconstriction) Nasal Solution Rebound congestion, local burning and stinging
NURSING RESPONSIBILITIES Warning: Use extreme caution when calculatimng and preparing doses; epinephrine is very potent drug Use minimal doses for minimal periods of time Protect drug solution from light, extreme heat and freezing; DO NOT USE PINK OR BROWN SOLUTIONS. Drug solution should be clear and colorless Shake the suspension for injectionwell before withdrawing the dose Rotate SQ injection sites to prevent necrosis; monitor injection site frequently Do not exceed recommended dosage of inhalation products.
Drug Classification: Alpha-adrenergic agonist Antasmathic Beta-1 and Beta-2 adrenergic agonist Bronchodilator Cardiac stimulant Nasal decongestant Symphatomimetic vasopressor
DRUG NAME Generic Name: furosemide Brand Name: Lasix
ACTION Inhibits reabsorption of sodium and chloride from the proximal and distal tubules and ascending limb of the loop of henle, leading to a sodium-rich dieresis.
INDICATION Oral, IV: edema associated with heart failure, cirrhosis, renal disease IV: acute pulmonary edema Oral: Hypertension
CONTRAINDICATION Contraindicated with allergy to furosemide, sulfonamides, allergy to tartrazine, anurai, severe renal failure, hepatic coma, pregnancy; lactation Use Cautiosly with SLE, gout, DM.
ADVERSE REACTION CNS: Dizziness, vertigo, paresthesias, headache, drowsinees, fatigue, blurred vision, tinnitus CV: Orthostatic hypotension, volume deplation, cardiac arrhythmias, thrombophlebitis Dermatologic: Photosensitivity, rash, pruritus, urticaria GI: Nuausea, vomiting, anorexia, oral and gastric irritation,constipation GU: Urinary bladder spasm Other: muscle cramps and muscle spasm
NURSING RESPONSIBILITIES Adminester with food or milk to prevent GI upset Reduce dosage if given with other hypertensive; readjust dosage gradually as BP responds. Give early in the day so that increase urination will not disturb sleep. Avoid IV use if Oral use is all possible Do not expose to light, which may discolor tablets or solution. Discard diluted solution after 24hours Refrigerate oral solution Measure and monitor weight to monitor fluid changes Arrange for potassium rich diet or supplemental potassium as needed.
Drug Classification: Loop diuretic
DOSAGE Adults Edema: initially 20-80 mg/day PO as a single dose. Hypertension: 40mg bid PO. Pediatric Edema: initially, 2mg/kg/day PO. If needed, increase 1-2 mg/kg in 6-8 hr. Do not exceed 6mg/kg.
DRUG NAME Generic Name: Lidocaine hydrochloride Brand Name: Xylocaine Drug Classification: Antiarrhythmic Local anesthetic
ACTION Type 1 antiarryhtmic: Decreases diastolic depolarization, decreasing automaticity of ventricular cells: increase ventricular fibrillation threshold. Local anesthetic: block the generation and conduction of action potentials in sensory nerves by reducing sodium permeability, reducing height and rate of rise of action potential, increasing excitation threshold and slowing conduction velocity. DOSAGE Adults IM: arrhythmia; use only 10% solution for injection. 300 mg in deltoid or thigh muscle
INDICATION As antiarrhythmic: management of acute ventricular arrhythmias during cardiac surgery and MI(IV use). Use IM when IV administration is not possible or when ECG moinitoring is not available and the danger of ventricular arrhythmia is great. As anesthetic: Infiltration anesthesia, peripheral and sympathetic nerve blocks, central nerve blocks, spinal and caudal anesthesia As local analgesiabefore venipuncture or peripheral IV cannulation when applied to intact skin in children 3-18 years old.
CONTRAINDICATION Contraindicated with allergy to lidocaine or amide-type local anesthesia, heart failure Cardiogenic shock 2nd or 3rd degree heart block Stokes-adam syndrome Use cautiously with hepatic or renal disease, inflammation or sepsis in the region of injection(loa=cal anesthetic)
ADVERSE REACTION Antiarrhythmic with systemic effects: CNS: Dizziness or lightheadedness, fatigue, drowsiness CV: cardiac arrhythmias, hypotension GI: Nausea, Vomiting Hypersensitivity: Rash Injectable local anesthetic for caudal epidural anesthesia: CNS: headache, Backache CV: hypotension due to sympathetic block GU: urinary retention, urinary or fecal incontinence. Topical local anesthetic: Dermatologic: Urticaria., pruritus Local: Burbing, stinging, tenderness, swelling, tissue irritation
NURSING RESPONSIBILITIES Reduce dosage with hepatic or renal failure Continuously monitor response when use as antiarrythmitic or injected as local anesthesia. Use caution to prevent choking. Patient may have difficulty swallowing after using oral topical anesthesia Have patients who received lidocaine as a spinal anesthetic remain lying flat for 6-12 hr afterward, and ensure that they are adequately hydrated to minimize risk of headache.
DRUG NAME Generic Name: Magnesium sulfate Brand Name:
ACTION Prevents and control seizures by blocking neuromuscular transmission; Attracts and retains water in the Intestinal lumen and distends the bowel to promote mass movement and relieve constipation.
INDICATION Acute nephritis(children), to control hypertension IV: hypomagnesemia, replacement therapy IV or IM: preeclampsia and eclampsia PO: short term treatment of constipation PO: evacuation of the colon for rectal and bowel examinations To correct or prevent hypomagnesemia in patient on parenteral nutrition
CONTRAINDICATION Contraindicated with allergy to magnesium products; heart block myocardial damage, abdominal pain, nausea Other symptoms of appendicitis Fecal impaction Intestinal and billiary tract obstruction Hepatitis
ADVERSE REACTION CNS: weakness, dizziness, CV: palpitations GI: excessive bowel activity, perianal irritation(PO)
NURSING RESPONSIBILITIES Reserve IV use in preeclampsia for immediate life threatening situations. Give IM route by deep IM injection of the undiluted (50%) solution for adult Do not give oral magnesium sulfate with abdominal pain, nausea, or vomiting Monitor bowel function; if diarrhea or cramping occur discontinue oral drug Maintain urine output at a level of 100 ml every 4hr during parenteral administration.
Drug Classification: Antiepileptic Electrolyte laxative
DOSAGE Adults Parenteral nutrition: 8-24 mEq/day IV Eclampsia, sever pre eclampsia: total initial dose of 10-14 g. May infuse 4-5 g in 250 ml 5% dextrose injection or 0.9% sodium chloride while giving IM doses up to 10g(5g or 10ml of undiluted 50% solution in each buttocks)
DRUG NAME Generic Name: Magnesium sulfate Brand Name:
ACTION Prevents and control seizures by blocking neuromuscular transmission; Attracts and retains water in the Intestinal lumen and distends the bowel to promote mass movement and relieve constipation.
INDICATION Acute nephritis(children), to control hypertension IV: hypomagnesemia, replacement therapy IV or IM: preeclampsia and eclampsia PO: short term treatment of constipation PO: evacuation of the colon for rectal and bowel examinations To correct or prevent hypomagnesemia in patient on parenteral nutrition
CONTRAINDICATION Contraindicated with allergy to magnesium products; heart block myocardial damage, abdominal pain, nausea Other symptoms of appendicitis Fecal impaction Intestinal and billiary tract obstruction Hepatitis
ADVERSE REACTION CNS: weakness, dizziness, CV: palpitations GI: excessive bowel activity, perianal irritation(PO)
NURSING RESPONSIBILITIES Reserve IV use in preeclampsia for immediate life threatening situations. Give IM route by deep IM injection of the undiluted (50%) solution for adult Do not give oral magnesium sulfate with abdominal pain, nausea, or vomiting Monitor bowel function; if diarrhea or cramping occur discontinue oral drug Maintain urine output at a level of 100 ml every 4hr during parenteral administration.
Drug Classification: Antiepileptic Electrolyte laxative
DOSAGE Adults Parenteral nutrition: 8-24 mEq/day IV Eclampsia, sever pre eclampsia: total initial dose of 10-14 g. May infuse 4-5 g in 250 ml 5% dextrose injection or 0.9% sodium chloride while giving IM doses up to 10g(5g or 10ml of undiluted 50% solution in each buttocks)
DRUG NAME Generic Name: Morphine sulfate Brand Name: Astramorph PF Drug Classification: Opioid agonist analgesic
ACTION Acts as agonist at specific opioid receptors in the CNS to produce analgesia, euphoria, sedation.
INDICATION Relief of moderate to severe acute and chronic pain Preoperative medication to sedate and allay apprehension, facilitate induction of anesthesia , and reduce anesthetic dosage Treatmenyt of pain following major surgery, ER liposome injection for single dose administration by epidural route at lumbar level
CONTRAINDICATION Contraindicated with hypersensitivity to opioids ; during labor and delivery of a premature infant Pregnancy Labor: respiratory depression in neonate: may prolong labor
ADVERSE REACTION CNS: lightheadedness, dizziness , sedation CV: peripheral circulatory collapse, tachycardia, bradycardia and palpitations Dermatologic: pruritus, urticaria, laryngo spasm, edema GI: nausea, vomiting, dry mouth, anorexia GU: urine retention or hesitancy, oliguria, antidiuretic effect Other: sweating
NURSING RESPONSIBILITIES Dilute and administer slowly IV to minimize likelihood of adverse effect Tell patient to lie downduroing IV administration Reassure patients that they are unlikely to become addicted; most patients who receives opiates for medical reason do not develop dependence syndrome.
DOSAGE Adults IM or SQ: 10mg (range 5-20 mg)/70 kg every 4 hr or as directed by the physician IV: 2.5-15mg/70 kg of body weight in 4-5 ml water for injection administered over 4-5 minutes.
DRUG NAME Generic Name: Naloxone HCL Brand Name: Narcan Drug Classification: Diagnostic agent Opioid antagonist
ACTION Pure opioid antagonist ; reverses the effects of opioids, including respiratory depression, sedation, hypotention
INDICATION Complete or partial reversal of opioid depression induced by opioids, including natural and synthetic narcotics Diagnosis of suspected acute opioid overdose Unlabeled uses: Improvement of circulation in refractory shock, reversal of alcoholic coma.
CONTRAINDICATION Contraindiacated with allergy to opioid antagonist Use cautiously with opioid addiction, CV disorders, pregnancy, lactation.
ADVERSE REACTION CNS: Reversal of analgesia an excitement Acute opioid abstenance syndrome: Nausea, vomiting, sweating, tachycardia, increased BP, tremulousness. CV: Hypotension, hypertension, ventricular tachycardai
NURSING RESPONSIBILITIES Monitor patient continuously after iuse of naloxone; reoeat doses maybe needed, depending on duration of opioid and time of last dose Ask thepatient to report sweating, feelings of tremulousness.
DOSAGE Adults Opioids overdose: Initial dose is 0.01 mg/kg IV. Post operative opioids depression: inject in increments of 0.005-0.01 mg IV at 2-3 min intervals to the desired degree of reversal
Das könnte Ihnen auch gefallen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- OmeprazoleDokument2 SeitenOmeprazolephawphawphawNoch keine Bewertungen
- Pathophysiology of TetanusDokument2 SeitenPathophysiology of TetanusAnitha SuprionoNoch keine Bewertungen
- 11 - Chapter 7 PDFDokument41 Seiten11 - Chapter 7 PDFRakesh RakiNoch keine Bewertungen
- Canine and Feline Mega EsophagusDokument10 SeitenCanine and Feline Mega Esophagustaner_soysurenNoch keine Bewertungen
- Funny StoriesDokument5 SeitenFunny Storiesamin jamalNoch keine Bewertungen
- Cardiac Stent PriceDokument4 SeitenCardiac Stent PriceMahmudul Hasan TusharNoch keine Bewertungen
- Conization of CervixDokument4 SeitenConization of Cervixdrnareshkumar3281Noch keine Bewertungen
- Optimum Detox Foot Pads, Natural Cleansing Ginger Detox Foot PatchesDokument1 SeiteOptimum Detox Foot Pads, Natural Cleansing Ginger Detox Foot PatchesBrooke GuntherNoch keine Bewertungen
- CDC Isolation 2007 PDFDokument219 SeitenCDC Isolation 2007 PDFwahyu nandaNoch keine Bewertungen
- Metatron Resonance Brochure WebsiteDokument3 SeitenMetatron Resonance Brochure WebsiteShaun DennisNoch keine Bewertungen
- Whitepaper Cohort of ConcernDokument4 SeitenWhitepaper Cohort of ConcernwoodsjaNoch keine Bewertungen
- SDokument34 SeitenSRam Kumar YadavNoch keine Bewertungen
- Post Dam and Relief Chamber FullDokument35 SeitenPost Dam and Relief Chamber FullnaomiNoch keine Bewertungen
- CerebrolysinDokument1 SeiteCerebrolysineiad-mahmoudNoch keine Bewertungen
- John O. Agwunobi MD Mba MPHDokument1 SeiteJohn O. Agwunobi MD Mba MPHStalyn DíazNoch keine Bewertungen
- Curriculum Vitae (CV)Dokument4 SeitenCurriculum Vitae (CV)wubeshetNoch keine Bewertungen
- Abductive Inference Computation Philosophy TechnologyDokument314 SeitenAbductive Inference Computation Philosophy Technologyusernameabout100% (1)
- Dilip K. Ghosh, R. B. Smarta-Pharmaceuticals To Nutraceuticals - A Shift in Disease Prevention-Taylor & Francis - CRC Press (2017)Dokument274 SeitenDilip K. Ghosh, R. B. Smarta-Pharmaceuticals To Nutraceuticals - A Shift in Disease Prevention-Taylor & Francis - CRC Press (2017)davidNoch keine Bewertungen
- Teknik MRI DasarDokument45 SeitenTeknik MRI DasarDeki Kurnia JayaNoch keine Bewertungen
- Adrian Jess Galindo: DefinitionDokument2 SeitenAdrian Jess Galindo: DefinitionAdrian MangahasNoch keine Bewertungen
- Radiopharmaceuticals & Nuclear PharmacyDokument39 SeitenRadiopharmaceuticals & Nuclear PharmacyKhalid HussainNoch keine Bewertungen
- Trace Element and Oral Health PedoDokument49 SeitenTrace Element and Oral Health PedoFourthMolar.com100% (1)
- Product English 6Dokument16 SeitenProduct English 6rpepNoch keine Bewertungen
- AJODO-90 Petrovic Et Al Role of The Lateral Pterigoid Muscle and Menisco Temporomandibular...Dokument12 SeitenAJODO-90 Petrovic Et Al Role of The Lateral Pterigoid Muscle and Menisco Temporomandibular...ortodoncia 2018Noch keine Bewertungen
- Pharmaceutical SciencesDokument5 SeitenPharmaceutical SciencesiajpsNoch keine Bewertungen
- 2022 Society of Critical Care Medicine Clinical.15Dokument37 Seiten2022 Society of Critical Care Medicine Clinical.15diegorojasNoch keine Bewertungen
- Parts of The Body and Health ProblemDokument13 SeitenParts of The Body and Health ProblemSonia Tri AgustinaNoch keine Bewertungen
- History Taking and MSE AIIMS PatnaDokument34 SeitenHistory Taking and MSE AIIMS PatnaShivendra Kumar100% (1)
- YogaDokument4 SeitenYogakunalNoch keine Bewertungen
- Romsons All ProductDokument53 SeitenRomsons All ProductBoyke WinterbergNoch keine Bewertungen