Beruflich Dokumente
Kultur Dokumente
Diphenhydramine
Hochgeladen von
Parker LeethOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Diphenhydramine
Hochgeladen von
Parker LeethCopyright:
Verfügbare Formate
1. Introduction This document presents background information and toxicological assessment of diphenhydramine, a first-generation antihistamine.
Diphenhydramine is most commonly used to treat seasonal allergies, but it is also used as an antiemetic, sleep aid, sedative, and CNS depressant. Because of its many uses, diphenhydramine is a widely used drug. 2. Identification Diphenhydramine is a first-generation antihistamine which has the molecular formula C17H21NO. Some common brand names are as follows: Benadryl, Alledryl, Diphenylhydramine, Benhydramine, Dihidral, Probedryl, Benzhyydraminum. Overall, there are 249 different names for diphenhydramine (or diphenhydramine mixtures) medicine . Diphenhydramine is available in the forms of capsules, injections, tablets, creams, gels and elixirs. 3. Pharmacology Diphenhydramine can be used as a local anesthetic, anti-allergic agent, antiemetic, histamine H1 antagonist and sedative. Antihistamines are used in the treatment of allergies due to inhalant allergens and foods. Antihistamines are used for the symptomatic treatment of itching associated with allergic reactions and cold urticaria. Antihistamines are used with epinephrine for anaphylactic reactions after the acute reactions have been controlled, and to lessen the allergic reactions to blood or plasma. Diphenhydramine is used for the symptomatic treatment of Parkinsons syndrome in combination with centrally acting anticholinergic agents. Diphenhydramine is used as a non-barbiturate cough suppressant for colds or allergies. Diphenhydramine is used for the prevention and treatment of the nausea, vomiting, dizziness, that is associated with vertigo. Diphenhydramine is used for its sedative effect. 3.1 Drug warnings H1 antagonists are most useful when treating the sudden onset of allergic reactions. Diphenhydramine only treats the symptoms; it does not prevent the production of histamines. First-generation H1 antagonists can both stimulate and depress the CNS. Stimulation is rarely observed with correct dosage, but it can be a sign of mild to moderate poisoning. Diphenhydramine typically depresses the CNS. The most common side effect is sedation. For individuals suffering from insomnia, this is the desired reaction. For most individuals, however, this is a negative side effect. If ones case is the latter, they should avoid operating heavy machinery or automobiles. Common side effects that involve the digestive tract are as follows: loss of appetite, vomiting, nausea, stomach pain, and constipation or diarrhea. This effect can be reduced by ingesting the medicine with meals.
Other side effects that are caused by the anticholinergic reactions of diphenhydramine include dry mouth, coughing, urinary retention, urinary frequency, and painful urination. Side effects that impact the cardiovascular system are as follows: palpitations, low blood pressure, migraines and weakness of the hands. [1] Drug allergy rarely occurs from oral exposure. It is more common to see a drug allergy resulting from topical use. Presence in breast milk is rare, but should be avoided in nursing mothers because of transference risk. 3.2 Persons susceptible to negative side effects of diphenhydramine Newborn or premature infants should not be given diphenhydramine because of an increased susceptibility CNS excitation and lowered seizure threshold. Elderly persons should also avoid diphenhydramine because nausea, somnolence, confusion, and hypotension may occur. Also, hematological complications are extremely rare, but can occur. 3.3 Toxicity and Lethal Dose In infants, severe toxicity occurs around 10 to 15 mg/kg; lowest lethal dose was 11.6 mg/kg. In young children, oral doses of less than 7.5 mg/kg should have little to no toxic effect. In adults, severe toxicity typically occurs after ingesting 1 or more grams. The lowest lethal dose for an adult was 25 mg/kg. Prolonged exposure/ high volume exposure to topical treatment can result in toxicity. [4] 3.4 Toxicity symptoms Mild overdose symptoms are as follows: sedation, anticholinergic effects, tachycardia, hypertension, nausea and vomiting. Moderate overdose symptoms are as follows: confusion, distress, hallucinations. Severe poisoning symptoms are as follows: neurosis, seizures, coma, hypotension and rare but possible renal failure
3.5 Treatment for overexposure In the case of oral exposure, for mild toxicity, closely monitor the affected person. Charcoal tablets could be beneficial if taken soon after ingestion of the drug. In the case of severe toxicity, tracheal intubation will maintain open airways, and stomach pumping could be beneficial if ingestion of the drug (more than 1 gram) was recent. 4. Pharmacodynamics Diphenhydramine belongs to the ethanolamine class of antihistamines. Ethanolamine antihistamines have significant antimuscarinic effects and cause sedation in majority of individuals 5. Biomedical Effects 5.1 Mechanism of action Antihistamines are used to treat allergies not by eliminating histamine, but by competing with histamine for H1-receptor sites on effector cells. They thereby prevent, responses mediated by histamine. H1 antagonists inhibit most effects of histamine on smooth muscle. For example, diphenhydramine antagonizes the constrictor action of histamine on smooth muscle in the respiratory tract. Diphenhydramine counteracts the effects of histamine on the capillaries, which in turn can reduce the intensity of allergy symptoms. Diphenhydramine also crosses the bloodbrain barrier and antagonizes the H1 receptors centrally. A side effect of this is sedation. Like many other first-generation antihistamines, diphenhydramine is an effective antimuscarinic. Diphenhydramine is an effective antiparkinson treatment because it has blocking properties on the muscarinic acetylcholine receptors in the brain. Diphenhydramine can be used as a local anesthetic because it can act as an intracellular sodium channel blocker. Diphenhydramine can inhibit the reabsorption of serotonin. 5.2 Absorption Diphenhydramine is absorbed with maximum activity occurring in approximately one hour. It is relatively well absorbed, and its plasma concentration is quickly increased after oral
administration. The intestinal absorption mechanisms of diphenhydramine, have been explained by the passive diffusion of nonionic compounds according to the pH-partition theory. [3] 5.2 Distribution Diphenhydramine is widely distributed, and it crosses into the placenta, enters breast milk, and crosses the blood-brain barrier. 5.3 Protein binding 98-99% 5.4 Metabolism Diphenhydramine is metabolized by the liver and kidneys. Approximately 95% of the ingested dose is metabolized by the liver. 5.5 Excretion Minute unaltered amounts of diphenhydramine are excreted in the urine. Most excretion appears as the products of metabolic transformation in the liver, which are often excreted within 24 hours. H1 antagonists are eliminated more rapidly by children than by adults and more slowly in those with severe liver disease. [1] 5.6 Half-life 1-4 hours [2] 5.7 Interactions Concurrent use of ototoxic medications with diphenhydramine may mask the symptoms of ototoxicity such as tinnitus, dizziness, or vertigo. [2] Concurrent use of monoamine oxidase (MAO) inhibitors with diphenhydramine may prolong and intensify the anticholinergic and CNS depressant effects of diphenhydramine. Therefore, concurrent use is not recommended. Concurrent use with alcohol or other CNS depression-producing medications may cause the CNS depressant effects of either these medications or antihistamines. Anticholinergic effects may occur when anticholinergics are used concurrently with diphenhydramine. Patients should report occurrence of gastrointestinal problems in a timely manner since paralytic ileus may occur with concurrent therapy.
Concurrent use of other photosensitizing medications with diphenhydramine may cause additive photosensitizing effects. [2]
1. (Gilman, A.G., T.W. Rall, A.S. Nies and P. Taylor (eds.). Goodman and Gilman's The Pharmacological Basis of Therapeutics. 8th ed. New York, NY. Pergamon Press, 1990., p. 584) 2. (USP Convention. USPDI - Drug Information for the Health Care Professional. 15 th ed. Volume 1. Rockville, MD: United States Pharmacopeial Convention, Inc., 1995. (Plus updates.), p. 305) 3. http://jpet.aspetjournals.org/content/290/1/388.full.pdf+html) 4. ([Rumack BH POISINDEX(R) Information System Micromedex, Inc., Englewood, CO, 2013; CCIS Volume 156, edition expires May, 2013. Hall AH & Rumack BH (Eds): TOMES(R) Information System Micromedex, Inc., Englewood, CO, 2013; CCIS Volume 156, edition expires May, 2013.] **PEER REVIEWED** )
Das könnte Ihnen auch gefallen
- Medication Card LisinoprilDokument1 SeiteMedication Card LisinoprilTSPANNoch keine Bewertungen
- Celecoxib (Drug Study)Dokument3 SeitenCelecoxib (Drug Study)Franz.thenurse6888100% (1)
- Medication DilutionDokument22 SeitenMedication DilutionYaser Salman100% (1)
- DM NCPDokument2 SeitenDM NCPVirgilio Reyes ManuelNoch keine Bewertungen
- Internal MedicineDokument190 SeitenInternal MedicineNisreen Al-shareNoch keine Bewertungen
- The Invisalign Appliance Today A Thinking Person S Orthodontic Appliance 2017 Seminars in OrthodonticsDokument53 SeitenThe Invisalign Appliance Today A Thinking Person S Orthodontic Appliance 2017 Seminars in Orthodonticsdruzair007Noch keine Bewertungen
- Solomon Sallfors: Ambulatory Morning Report 1: AcneDokument3 SeitenSolomon Sallfors: Ambulatory Morning Report 1: AcneSolomon Seth SallforsNoch keine Bewertungen
- ImipramineDokument1 SeiteImipramineMuhammad ArsalanNoch keine Bewertungen
- Type of Solution Classificati ON Content Mechanism of Action Indication Contra-Indication HOW Supplied Dose Nursing ResponsibilitiesDokument1 SeiteType of Solution Classificati ON Content Mechanism of Action Indication Contra-Indication HOW Supplied Dose Nursing ResponsibilitiesAloyan Rose JoyNoch keine Bewertungen
- DRUGSDokument5 SeitenDRUGSDanica EspejoNoch keine Bewertungen
- Coreg (Carvedilol)Dokument1 SeiteCoreg (Carvedilol)Adrianne BazoNoch keine Bewertungen
- Oral Rehydration SolutionDokument4 SeitenOral Rehydration SolutionMomerNoch keine Bewertungen
- Phenylephrine: 1568 Cough Suppressants Expectorants Mucolytics and Nasal DecongestantsDokument2 SeitenPhenylephrine: 1568 Cough Suppressants Expectorants Mucolytics and Nasal DecongestantsRanny LaidasuriNoch keine Bewertungen
- MinoxidilDokument2 SeitenMinoxidilHenna AhmedNoch keine Bewertungen
- Infective Endocarditis CaseDokument3 SeitenInfective Endocarditis CaseMershen GaniaNoch keine Bewertungen
- Dextroamphetamine SulfateDokument3 SeitenDextroamphetamine Sulfateapi-3797941100% (1)
- Xylocard PiDokument11 SeitenXylocard PiRamakant SharmaNoch keine Bewertungen
- Chlorphenamine MaleateDokument2 SeitenChlorphenamine Maleateasep budiyantoNoch keine Bewertungen
- DigoxinDokument18 SeitenDigoxinApril Mergelle LapuzNoch keine Bewertungen
- Acetaminophen and HydrocodoneDokument2 SeitenAcetaminophen and Hydrocodonejack080653Noch keine Bewertungen
- DimenhydrinateDokument2 SeitenDimenhydrinateNinoska Garcia-Ortiz100% (1)
- Drug Study inDokument3 SeitenDrug Study inaycee0316Noch keine Bewertungen
- TrihexyphenidylDokument5 SeitenTrihexyphenidylZepHemaNoch keine Bewertungen
- DRUG StudyDokument6 SeitenDRUG StudyJheryck SabadaoNoch keine Bewertungen
- Colchicine FDADokument24 SeitenColchicine FDACatalina BanuNoch keine Bewertungen
- CyclosporineDokument24 SeitenCyclosporinesanchit_J14Noch keine Bewertungen
- PSYCHIAdrugstudyDokument5 SeitenPSYCHIAdrugstudyJss Rosete-De GuzmanNoch keine Bewertungen
- Calcium GluconateDokument9 SeitenCalcium Gluconatemarkus_danusantosoNoch keine Bewertungen
- Drug StudyDokument7 SeitenDrug StudyDiana Laura LeiNoch keine Bewertungen
- Chromium and DiabetesDokument29 SeitenChromium and DiabetesTri Kusuma Agung PuruhitaNoch keine Bewertungen
- ActemraDokument7 SeitenActemraLinda KvastadNoch keine Bewertungen
- Aminophylline GuidelinesDokument2 SeitenAminophylline GuidelinesA. Shamshir A. MoktiNoch keine Bewertungen
- Nuevaespana, Jayne Angelie A. BSN 2A: GI: NauseaDokument7 SeitenNuevaespana, Jayne Angelie A. BSN 2A: GI: NauseaJayne Angelie A. NuevaespañaNoch keine Bewertungen
- What Is Radioactive PollutionDokument4 SeitenWhat Is Radioactive PollutionJoy MitraNoch keine Bewertungen
- Duragesic (Fentanyl Citrate)Dokument4 SeitenDuragesic (Fentanyl Citrate)E100% (1)
- Module 3 Activity 2 Drug Study Ciprofloxacin PaxilDokument6 SeitenModule 3 Activity 2 Drug Study Ciprofloxacin PaxilEugene MananganNoch keine Bewertungen
- Cefixime: Suprax Class and CategoryDokument3 SeitenCefixime: Suprax Class and CategoryArianne Joy SalvadorNoch keine Bewertungen
- Compute For The Total Body Surface Area Affected by The BurnsDokument2 SeitenCompute For The Total Body Surface Area Affected by The BurnsVAL ASHLIE ACEBARNoch keine Bewertungen
- Complete One Sheet Per Drug: Milk. Metabolism: in Liver (CYP2D6) - Feces. Half-Life: 5-9 HDokument2 SeitenComplete One Sheet Per Drug: Milk. Metabolism: in Liver (CYP2D6) - Feces. Half-Life: 5-9 HMikeNoch keine Bewertungen
- Manuscript Case Report Addison's Disease Due To Tuberculosis FinalDokument22 SeitenManuscript Case Report Addison's Disease Due To Tuberculosis FinalElisabeth PermatasariNoch keine Bewertungen
- Phenylephrine Hydrochloride PDFDokument5 SeitenPhenylephrine Hydrochloride PDFVinz Khyl G. CastillonNoch keine Bewertungen
- Disease Spotlight: Diabetes Mellitus: Insulin Insulin Is A Drug That Is Used To ControlDokument7 SeitenDisease Spotlight: Diabetes Mellitus: Insulin Insulin Is A Drug That Is Used To ControlMIR SARTAJNoch keine Bewertungen
- Linezolid: Antibiotic ClassDokument2 SeitenLinezolid: Antibiotic ClassEdison Patricio Vallejo PasquelNoch keine Bewertungen
- Ephedrine: DR Henny RachdiatiDokument20 SeitenEphedrine: DR Henny Rachdiatitiara rizkiaNoch keine Bewertungen
- Magnesium SulfateDokument1 SeiteMagnesium SulfateSilinna May Lee Sanico0% (1)
- HEMARATE FA Hemarate FA Consists of Folic AcidDokument2 SeitenHEMARATE FA Hemarate FA Consists of Folic AcidMarhina Asarabi MukimNoch keine Bewertungen
- Concept MapDokument9 SeitenConcept MapAllene PaderangaNoch keine Bewertungen
- Alzheimer Dementia: Starting, Stopping Drug Therapy: ReviewDokument6 SeitenAlzheimer Dementia: Starting, Stopping Drug Therapy: ReviewAnonymous ZUaUz1wwNoch keine Bewertungen
- ORS Package InsertDokument1 SeiteORS Package InsertwhothehellisarcticmonkeysNoch keine Bewertungen
- HyoscineDokument4 SeitenHyoscineHana HanaNoch keine Bewertungen
- Drug StudyDokument4 SeitenDrug StudyArdy PadamadaNoch keine Bewertungen
- PhenytoinDokument5 SeitenPhenytoinRhawnie B. GibbsNoch keine Bewertungen
- Humalog - Uses, Dosage & Side Effects - DrugsDokument4 SeitenHumalog - Uses, Dosage & Side Effects - Drugsremyde07100% (1)
- Drug StudyDokument2 SeitenDrug Studypopoyoio100% (2)
- Drug StudyDokument8 SeitenDrug Studysarah1217Noch keine Bewertungen
- SucralfateDokument3 SeitenSucralfateViziteu AlexandraNoch keine Bewertungen
- Succinylcholine ChlorideDokument19 SeitenSuccinylcholine ChlorideAgungBudiPamungkas100% (1)
- Psychotherapeutic AgentsDokument2 SeitenPsychotherapeutic AgentsjustinahorroNoch keine Bewertungen
- SabutamolDokument1 SeiteSabutamolKathzkaMaeAgcaoiliNoch keine Bewertungen
- Antihistamine and DecongestantDokument22 SeitenAntihistamine and DecongestantAngeline de GalaNoch keine Bewertungen
- Rangkuman Book ReadingDokument7 SeitenRangkuman Book ReadingBlackswannnNoch keine Bewertungen
- DiphenhydramineDokument9 SeitenDiphenhydramineFhey Bernadette BeltranNoch keine Bewertungen
- DiphenhydramineDokument10 SeitenDiphenhydramineFebry Dian SinagaNoch keine Bewertungen
- Mod14 TerminologyDokument6 SeitenMod14 Terminologypilsen_01Noch keine Bewertungen
- I. Topic: Pertussis II. ObjectivesDokument7 SeitenI. Topic: Pertussis II. ObjectivesKaren PanganibanNoch keine Bewertungen
- Anesthesia, Perioperative Care, and Sedation: Randall C. WetzelDokument18 SeitenAnesthesia, Perioperative Care, and Sedation: Randall C. WetzelAnonymous X56eFt6Noch keine Bewertungen
- PTSD Criteria DSM 5Dokument2 SeitenPTSD Criteria DSM 5Liv MNoch keine Bewertungen
- Acute Appendicitis PowerpointDokument34 SeitenAcute Appendicitis PowerpointJaysonPangilinanAban100% (1)
- ETEC 520 Assignment #1Dokument14 SeitenETEC 520 Assignment #1Diana NgNoch keine Bewertungen
- OcclusionDokument14 SeitenOcclusionpasser byNoch keine Bewertungen
- Positive Pressure VentilationDokument20 SeitenPositive Pressure VentilationRayhan ShariffNoch keine Bewertungen
- Congenital Muscular TorticollisDokument5 SeitenCongenital Muscular TorticollisKevin Paul ZuñigaNoch keine Bewertungen
- General AnaesthesiaDokument53 SeitenGeneral Anaesthesiapeter singal100% (2)
- Common Ent EmergenciesDokument69 SeitenCommon Ent EmergenciesSyawqia SalsabylaNoch keine Bewertungen
- 1 s2.0 S0377123714001750 MainDokument7 Seiten1 s2.0 S0377123714001750 MainMarlon Cespedes AlccaNoch keine Bewertungen
- Hemiplegia Is Total Paralysis of The ArmDokument3 SeitenHemiplegia Is Total Paralysis of The ArmRaveen mayi100% (1)
- Understanding Virtues and Vices of The Healthcare ProviderDokument3 SeitenUnderstanding Virtues and Vices of The Healthcare ProviderChariss OdlosNoch keine Bewertungen
- Ethics in Abnormal PregnanciesDokument123 SeitenEthics in Abnormal PregnanciesspicylaingNoch keine Bewertungen
- IgG Vs IgEDokument2 SeitenIgG Vs IgEvyasakandarpNoch keine Bewertungen
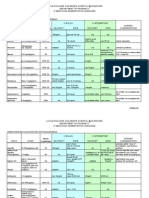
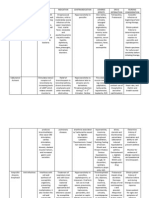
- Student Nurses' Community: Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDokument2 SeitenStudent Nurses' Community: Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationVen Belista86% (14)
- Stroke Imaging FINALDokument90 SeitenStroke Imaging FINALChaitanya Jsk100% (1)
- Kavo1 1058 Primus MaintenanceDokument30 SeitenKavo1 1058 Primus MaintenanceVoulgaris KostasNoch keine Bewertungen
- Effects of Adoption 1Dokument10 SeitenEffects of Adoption 1api-353918742Noch keine Bewertungen
- Infection ControlDokument6 SeitenInfection ControlhiyahninjaNoch keine Bewertungen
- Minimum Standards of RehabDokument61 SeitenMinimum Standards of Rehabbharat vermaNoch keine Bewertungen
- IntroductiontoEpidemiologyandPublicHealth AnswersDokument17 SeitenIntroductiontoEpidemiologyandPublicHealth AnswersDiamond_136100% (2)
- gl0087 PDFDokument58 Seitengl0087 PDFNurul HikmahNoch keine Bewertungen
- Clinical Trial Protocol TemplateDokument33 SeitenClinical Trial Protocol TemplateNasilNoch keine Bewertungen
- Pharmacy Information SystemsDokument3 SeitenPharmacy Information SystemsEköw Santiago Javier60% (5)