Beruflich Dokumente
Kultur Dokumente
NCP Impaired Physical Mobility
Hochgeladen von
Christian Apelo SerquillosOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
NCP Impaired Physical Mobility
Hochgeladen von
Christian Apelo SerquillosCopyright:
Verfügbare Formate
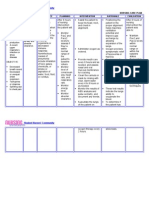
NCM104b BSN220/Group 8 0 Cues Nursing Diagnosis Analysis Planning Interventio n Rationale Evaluation Subjective: Ang hirap ng may ganito
(traction). Bawal kumilos, hindi man lang ako makapunta s a banyo para maligo. Hinihintay ko pa na may bisita ako para lang makapaglinis ng sarili ko verbalized by the client. Objective: Client is on modified bucks extension traction. Client is on semi- fowlers position. Client had fracture on the proximal 3rd of his left femur due to gunshot. Client had three gunshots on his abdomen with mainly his duodenum and jejunum as well as in his right leg. Provisional Diagnosis: Hypovolemic shock 2 to multiple GSW Measurement: Red Blood Cells 3.77 x 10^12/L Impaired Physical Mobility related to musculoskeletal impairment possibly evidenced by in ability to move purposefully within the physical environment, imposed restriction. Impaired Physical Mobility Limitation in independent, purposeful physical movement of the body or of one or more extremities. (Nurses Pocket Guide-Diagnoses, Prioritized Intervent ions, and Rationales by Marilynn E. Doenges, Mary Frances Moorhouse, Alice C. Murr p.457) Alteration in mobility may be a temporary or more permanent problem. Most disease and rehabilitative states involve some d egree of immobility (e.g., as seen in strokes, leg fracture, trauma, morbid obesity, and multiple sclerosis ). With the longer life expectancy for most Americans, the incidence of disease and disability continues to grow. And with shorter hospital stays, patients are being transferred to rehabilitation Goals: After 8 hours of nursing intervention, the client will be able to verbalize unde rstanding of situation and individual treatment regimen and safety measures inde pendently. Objectives: After 1 hour of nursing intervention, the client will be able to: 1.To identify at least five out of eight causative/contributing factors
Determine diagnosis that contributes to immobility
Note factors affecting current situation and potential time involved.
Assess clients developmental level, motor skills, ease and capability of movement , posture and gait. Note older clients general health status
These conditions can cause physiological and psychological problems that can ser iously impact physical, social, and economic well-being. Identifies potential impairments and determines type of interventions needed to provide for clients safety To determine presence of characteristics of clients unique impairment and to guid e choiceofinterventions Identified mobility as the most important functional ability that determines the degree of independence and healthcare needs among older persons.2 While aging per se does not cause impaired mobility, several The goal was met.
Met. The client was able to identify five out of eight causative/contributing fa ctors. Normal Findings: (Males) 5.5-6.5 x10^12/L Hemoglobin 11.80 g/dL Normal Findings: (Males) 14-16 g/dL Hematocrit 0.33 L/L Normal Findings: (Males) 0.42-0.52 L/L Lymphocytes 0.21 Normal Findings: 0.25-0.35 Eosinophils 0.01 Normal Findings 0.03-0.05 facilities or sent home for physical therapy in the home environment. Mobility is also related to body changes from aging. Loss of muscle mass, reduct ion in muscle strength and function, stiffer and less mobile joints, and gait ch anges affecting balance can significantly compromise the mobility of elderly pat ients. Mobility is paramount if elderly patients are to maintain any independent living. Restricted movement affects the performance of most activities of daily living (ADLs). Elderly patients are also at increased risk for the complications of immobility. Nursing goals are to maintain functional ability, prevent additio nal impairment of physical activity, and ensure a safe environment. (Nursing Care Plans: Nursing Diagnosis and Intervention by Gulanick, Myers,
2.To report three out of five of his functional ability
Evaluate for presence/degree of pain, listening to clients description about mann er in which pain limits mobility. Ascertain clients perception of activity/exercise needs and impact of current sit uation. Identify cultural beliefs and expectations affecting recovery/response to long-t erm limitations. Assessnutritionalstatusand clientsreportofenergylevel.
Determinehistoryoffallsand relatednesstocurrentsituation.
Determine degree of immobility in relation to 04 scale, noting muscle strength and tone, jointmobility,cardiovascular status,balance,andendurance.
Determinedegreeof perceptual/cognitiveimpairment andabilitytofollowdirections predisposing factors inadditiontoage-relatedchanges canleadtoimmobility Todetermineneededinterventions forpainmanagement
Helps to determine clients expectations/beliefs related to activity and potential long-term effectofcurrentimmobility.Also identifiesbarriersthatmaybe a ddressed
Deficiencies in nutrients and water,electrolytesandminerals cannegativelyaffecte nergyand activitytolerance. Client may be restricting activity because of weakness/debilitation, actual inju ry during a fall, or from psychological distressthatcanpersistafterafall. Identifies strengths and deficits impaired physical mobility and may provide information regarding potential for recovery Impairments related to age, chronic or acute disease condition, trauma,
Met. The client was able to report three out of five of his functional ability. Klop, Galanes, Gradishar and Puzas)
Observemovementwhenclient isunawareofobservation Noteemotional/behavioral responsestoproblemsof immobility
Determinepresence of complicationsrelatedto immobility surgery, or medications require alternative interventions or changes in plan of care. To note any incongruence with reportsofabilities. Can negatively affect self- concept and self-esteem, autonomy, and independence. Feelings of frustration and powerlessness may impede attainment of goals. Social, occupational, and relationship roles can change, leading to isolation, depression, and economic co nsequences Studies have shown that as much as 5.5% of muscle strength can be lost each day of rest and immobility.5 Other complications include changes in circulation and impairments of organ function affecting the whole person 3.To explain at least five of the optimal level of function and measures on how to prevent complications. Assistwithtreatmentof underlyingcondition(s)
Discuss discrepancies in movement with client aware and unaware of observation a nd methodsfordealingwith identifiedproblems. Assist/haveclientrepositionself To maximize potential for mobility and optimal function. May be necessary when client is using avoidance or controlling behavior, or is not aware of own abilities due to anxiety/fear. To enhance circulation to Met. The client was able to explain at least five of the optimal level of functi on and measures on how to prevent complications. onaregularscheduleasdictated byindividualsituation Review/encourageuseofproper bodymechanics Demonstrate/assistwithuseof siderails,overhead trapeze,roller pads,hydrauliclift s/chairs Supportaffected body parts/jointsusingpillows/rolls, footsupports/shoes,gelpads, etc., Provide/recommend egg-crate, alternatingair-pressure, orwater mattress. Usepaddingandpositioning devices
Encourage clients participation in self-care activities, physical/occupational th erapies as well as diversional/recreational activities. Provide client with ample time to perform mobility-related tasks. Schedule activ ities with adequaterestperiodsduringthe day Avoidroutinelyassistingor doingforclientthoseactivities thatclientcandoforself. Identify/encourageenergy- conservingtechniquesfor tissues, reduce risk of tissue ischemia. Topreventinjurytoclientand caregiver Forpositionchanges/transfers. Instructinsafeuseofwalker/cane forambulation. Tomaintainpositionoffunction andreduce riskofpressureulcers. Reduces tissue pressureandaidsinmaximizing cellularperfusiontopreventdermal inju ry. To prevent stress on tissues and reduce potential for disusecomplications. Reduces sensory deprivation, enhances self- concept andsenseofindependence,and i mprovesbodystrengthand function. Toreducefatigue.
Caregivers cancontributetoimpairedmobility bybeingoverprotective orhelping toomu ch. Limits fatigue, maximizing ADLs. Notechangeinstrengthtodo moreorlessself-care
Administermedicationsbefore activityasneededforpainrelief Perform/encourageregular skin examinationandcare
Encourageadequate intakeof fluids/nutritiousfoods Encourageclients/SOs involvementindecisionmaking asmuchaspossible participation. To promote psychological and physical benefits of self-care and to adjust level of assistance asindicated. To permit maximal effort/involvementinactivity. To reduce pressure on sensitive areas and to prevent development of problems wit h skin integrity. Promotes well-being and maximizes energy production. Enhances commitment to plan, optimizing outcomes.
4.To discuss four out of five of wellness program. Discusssafewaysthatclientcan exercise Assistclient/SOtolearnsafety measuresasindividually indicated. Involve client and SO(s) in care, assisting them to learn ways of managing probl ems of immobility,especiallywhen impairmentisexpected tobe long-term. Multipleoptionsprovideclient choicesandvariety
May need instruction and to givereturndemonstration May need referral for support and community services to provide care, supervisio n, companionship, respite services, nutritional and ADL assistance, adaptive devices or changes to living environment, financial assistance, etc
Met. The client was able to discuss four out of five of wellness program. Demonstrate use of standing aids and mobility devices and have client/careprovid er demostrate knowledge about/safe use of device. Identify appropriate resources for obtaining and maintaining appliances/ equipment. Safe use of mobility aids promotes clients independence and enhances quality of l ifeandsafetyforclientand caregiver (Nurses Pocket Guide- Diagnoses, Prioritized Interventions, and Rationales by M arilynn E. Doenges, Mary Frances Moorhouse, Alice C. Murr p.458-461)
Das könnte Ihnen auch gefallen
- Nursing Care Plan - MergedDokument13 SeitenNursing Care Plan - MergedJuls Flares SycaycoNoch keine Bewertungen
- Care of Elderly - NCP1Dokument2 SeitenCare of Elderly - NCP1ROGEN KATE AZARCONNoch keine Bewertungen
- Tagum Doctors College, Inc.: Mahogany ST., Rabesubd., Tagum City E-MailDokument4 SeitenTagum Doctors College, Inc.: Mahogany ST., Rabesubd., Tagum City E-MailRoel John Atamosa CasilacNoch keine Bewertungen
- Chapter - 021 Case StudyDokument2 SeitenChapter - 021 Case Studydonnam86Noch keine Bewertungen
- Hildegard Peplau's Interpersonal Relations 101Dokument85 SeitenHildegard Peplau's Interpersonal Relations 101Ynaffit Alteza Untal100% (1)
- Rle Week 13Dokument8 SeitenRle Week 13Roselyn Yu QuintoNoch keine Bewertungen
- Care Plan Number 2Dokument5 SeitenCare Plan Number 2Teddy mc Bones100% (1)
- PathophysiologyDokument9 SeitenPathophysiologySuzette PipoNoch keine Bewertungen
- 51 100Dokument18 Seiten51 100Jaessa Feliciano100% (1)
- Atun Maricris Jorre Ca2 Au Legarda Leadership Managemet Research DownloadableDokument2 SeitenAtun Maricris Jorre Ca2 Au Legarda Leadership Managemet Research DownloadableCharissa Magistrado De LeonNoch keine Bewertungen
- Spinal Cord InjuryDokument3 SeitenSpinal Cord InjuryDan Leo UnicoNoch keine Bewertungen
- E. Nursing DiagnosisDokument2 SeitenE. Nursing DiagnosisAle SandraNoch keine Bewertungen
- NCP CvaDokument4 SeitenNCP CvaMariquita BuenafeNoch keine Bewertungen
- Counselling LetterDokument1 SeiteCounselling LetterSeann LorescoNoch keine Bewertungen
- Case Pres A1-RhdDokument11 SeitenCase Pres A1-RhdCharm TanyaNoch keine Bewertungen
- 6 Nursing Care Plan 1Dokument2 Seiten6 Nursing Care Plan 1Denise Louise PoNoch keine Bewertungen
- Nursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDokument2 SeitenNursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDeanne Carla DalilisNoch keine Bewertungen
- Module V ActDokument3 SeitenModule V ActQueencess hayoNoch keine Bewertungen
- Unciano Community OutputDokument18 SeitenUnciano Community OutputKath Mendoza ÜNoch keine Bewertungen
- Moira Mae B. Balite BSN 2A: Post Partum Care DefinitionDokument5 SeitenMoira Mae B. Balite BSN 2A: Post Partum Care DefinitionMoiraMaeBeridoBaliteNoch keine Bewertungen
- 8 Sample Care Plans For ACDFDokument11 Seiten8 Sample Care Plans For ACDFacasulla98Noch keine Bewertungen
- X. Nursing Care Plan: ObjectiveDokument6 SeitenX. Nursing Care Plan: ObjectiveRenea Joy ArruejoNoch keine Bewertungen
- NCP CSDokument4 SeitenNCP CSJM UncianoNoch keine Bewertungen
- Geria Lec Portfolio CasiaDokument9 SeitenGeria Lec Portfolio CasiaMarie Ashley CasiaNoch keine Bewertungen
- NCPDokument2 SeitenNCPMelissa David100% (1)
- GRP 4 CLO 2 Concept Map PT 1 PDFDokument14 SeitenGRP 4 CLO 2 Concept Map PT 1 PDFMaria Lyn Ocariza ArandiaNoch keine Bewertungen
- Nursing Information SystemDokument2 SeitenNursing Information SystemkcarpioNoch keine Bewertungen
- Transcultural Perspective in Nursing Care For Children PDFDokument41 SeitenTranscultural Perspective in Nursing Care For Children PDFJade CatubayNoch keine Bewertungen
- Narratives Case NotesDokument4 SeitenNarratives Case NotesKnigh RiderNoch keine Bewertungen
- Impaired Physical MobilityDokument2 SeitenImpaired Physical MobilityAl-Qadry NurNoch keine Bewertungen
- Concept Map FinalDokument1 SeiteConcept Map Finalapi-383763177Noch keine Bewertungen
- 1.MOD On GERON (1) CommunicationDokument19 Seiten1.MOD On GERON (1) CommunicationPatricia VasquezNoch keine Bewertungen
- Hepatocellula R CarcinomaDokument45 SeitenHepatocellula R Carcinomamhean azneitaNoch keine Bewertungen
- Im Case Study 04Dokument49 SeitenIm Case Study 04Shaine BalverdeNoch keine Bewertungen
- Week 7 - Rheumatoid ArthritisDokument1 SeiteWeek 7 - Rheumatoid ArthritisTuTitNoch keine Bewertungen
- Case Study FormatDokument5 SeitenCase Study FormatEden OlasabNoch keine Bewertungen
- Cerebral Aneurysm Case Analysis and Concept MapDokument5 SeitenCerebral Aneurysm Case Analysis and Concept Mapate NarsNoch keine Bewertungen
- Nusing CareplanDokument3 SeitenNusing Careplanardec_143Noch keine Bewertungen
- NCP PainDokument2 SeitenNCP PainApril_Ivy_Raga_3835Noch keine Bewertungen
- HemodialysisDokument2 SeitenHemodialysisjustin_saneNoch keine Bewertungen
- Post-Partum Hemorrhage Pathophysiology PaperDokument5 SeitenPost-Partum Hemorrhage Pathophysiology Paperapi-399619969Noch keine Bewertungen
- Lyceum of The Philippines University - Batangas CollegeDokument120 SeitenLyceum of The Philippines University - Batangas CollegeKMNoch keine Bewertungen
- Spinal Cord InjuryDokument28 SeitenSpinal Cord InjuryLouie John AbilaNoch keine Bewertungen
- BioethicsCasesEEI 316232215 PDFDokument38 SeitenBioethicsCasesEEI 316232215 PDFAman UllahNoch keine Bewertungen
- Case 1Dokument9 SeitenCase 1Joselyn M. LachicaNoch keine Bewertungen
- Care of Adults 26 Endocrine ManagementDokument26 SeitenCare of Adults 26 Endocrine ManagementGaras AnnaBerniceNoch keine Bewertungen
- Bioethical Components of CareDokument2 SeitenBioethical Components of CarekeiitNoch keine Bewertungen
- Sample PSADokument4 SeitenSample PSAjudssalangsangNoch keine Bewertungen
- NCPDokument4 SeitenNCPJoseph Dableo ParreñoNoch keine Bewertungen
- VSIM Clinical Worksheet 07.16.2020Dokument6 SeitenVSIM Clinical Worksheet 07.16.2020Jackie GriffisNoch keine Bewertungen
- Nursing Interventions CHFDokument3 SeitenNursing Interventions CHFbanyenye25100% (1)
- Vulva HeamatomaDokument16 SeitenVulva Heamatomaabeer saadNoch keine Bewertungen
- NCM 114 Gerontology - WeeK 1Dokument38 SeitenNCM 114 Gerontology - WeeK 1Jmarie Brillantes Popioco0% (1)
- Age Related ChangesDokument8 SeitenAge Related ChangesEricson CandelariaNoch keine Bewertungen
- CHP 4 Patient and Caregiver Teaching StudentDokument24 SeitenCHP 4 Patient and Caregiver Teaching StudentSwetaNoch keine Bewertungen
- Communication With Older AdultsDokument22 SeitenCommunication With Older AdultsNathaniel Karl Enin PulidoNoch keine Bewertungen
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideVon EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNoch keine Bewertungen
- Online Nursing Education ProgramsDokument13 SeitenOnline Nursing Education ProgramsChristian Apelo SerquillosNoch keine Bewertungen
- Report MANS 110 Curriculum DevtDokument3 SeitenReport MANS 110 Curriculum DevtChristian Apelo SerquillosNoch keine Bewertungen
- Current Trends and Issues: Nursing EducationDokument12 SeitenCurrent Trends and Issues: Nursing EducationChristian Apelo Serquillos100% (1)
- 4.13 Parameters For Department of Mental Health Peer AdvocatesDokument5 Seiten4.13 Parameters For Department of Mental Health Peer AdvocatesChristian Apelo SerquillosNoch keine Bewertungen
- Assessment Diagnosis Planning Intervention Rationale EvaluationDokument2 SeitenAssessment Diagnosis Planning Intervention Rationale EvaluationChristian Apelo SerquillosNoch keine Bewertungen
- BricanylDokument4 SeitenBricanylianecunarNoch keine Bewertungen
- Nursing Interventions in SchizophreniaDokument24 SeitenNursing Interventions in SchizophreniaChristian Apelo Serquillos0% (1)
- NCP Impaired Physical MobilityDokument9 SeitenNCP Impaired Physical MobilityChristian Apelo SerquillosNoch keine Bewertungen
- NCP PneumoniaDokument2 SeitenNCP PneumoniaChristian Apelo Serquillos100% (2)
- Family Nursing Care PlanDokument5 SeitenFamily Nursing Care PlanChristian Apelo SerquillosNoch keine Bewertungen