Beruflich Dokumente
Kultur Dokumente
Burns - Fluid Volume, Risk For Deficient
Hochgeladen von
makyofrancis20Originaltitel
Copyright
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Burns - Fluid Volume, Risk For Deficient
Hochgeladen von
makyofrancis20Copyright:
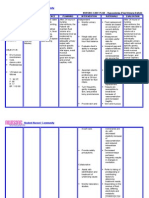
NURSING DIAGNOSIS: Fluid Volume, risk for deficient Risk factors may include Loss of fluid through abnormal
routes, e.g., burn wounds Increased need: hypermetabolic state, insufficient intake Hemorrhagic losses Possibly evidenced by [Not applicable; presence of signs and symptoms establishes an actual diagnosis.] DESIRED OUTCOMES/EVALUATION CRITERIAPATIENT WILL: Hydration (NOC) Demonstrate improved fluid balance as evidenced by individually adequate urinary output with normal specific gravity, stable vital signs, moist mucous membranes.
ACTIONS/INTERVENTIONS
Shock Prevention (NIC)
RATIONALE
Independent
Monitor vital signs, central venous pressure (CVP). Note capillary refill and strength of peripheral pulses. Serves as a guide to fluid replacement needs and assesses cardiovascular response. Note: Invasive monitoring is indicated for patients with major burns, smoke inhalation, or preexisting cardiac disease, although there is an associated increased risk of infection, necessitating careful monitoring and care of insertion site. Generally, fluid replacement should be titrated to ensure average urinary output of 3050 mL/hr (in the adult). Urine can appear red to black (with massive muscle destruction) because of presence of blood and release of myoglobin. If gross myoglobinuria is present, minimum urinary output should be 75100 mL/hr to reduce risk of tubular damage and renal failure. Increased capillary permeability, protein shifts, inflammatory process, and evaporative losses greatly affect circulating volume and urinary output, especially during initial 2472 hr after burn injury. Massive/rapid replacement with different types of fluids and fluctuations in rate of administration require close tabulation to prevent constituent imbalances or fluid overload. Fluid replacement formulas partly depend on admission weight and subsequent changes. A 15%20% weight gain can be anticipated in the first 72 hr during fluid replacement, with return to preburn weight approximately 10 days after burn.
Monitor urinary output and specific gravity. Observe urine color and Hematest as indicated.
Estimate wound drainage and insensible losses.
Maintain cumulative record of amount and types of fluid intake.
Weigh daily.
ACTIONS/INTERVENTIONS
RATIONALE
Shock Prevention (NIC)
Independent
Measure circumference of burned extremities as indicated. Investigate changes in mentation. May be helpful in estimating extent of edema/fluid shifts affecting circulating volume and urinary output. Deterioration in the level of consciousness may indicate inadequate circulating volume/reduced cerebral perfusion. Stress (Curlings) ulcer occurs in up to half of all severely burned patients and can occur as early as the first week. Patients with burns more than 20% TBSA are at risk for mucosal bleeding in the gastrointestinal (GI) tract during the acute phase because of decreased splanchnic blood flow and reflex paralytic ileus.
Observe for gastric distension, hematemesis, tarry stools. Hematest nasogastric (NG) drainage and stools periodically.
Collaborative
Insert/maintain indwelling urinary catheter. Allows for close observation of renal function and prevents urinary retention. Retention of urine with its byproducts of tissue-cell destruction can lead to renal dysfunction and infection. Accommodates rapid infusion of fluids. Fluid resuscitation replaces lost fluids/electrolytes and helps prevent complications, e.g., shock, acute tubular necrosis (ATN). Replacement formulas vary (e.g., Brooke, Evans, Parkland) but are based on extent of injury, amount of urinary output, and weight. Note: Once initial fluid resuscitation has been accomplished, a steady rate of fluid administration is preferred to boluses, which may increase interstitial fluid shifts and cardiopulmonary congestion. Identifies blood loss/RBC destruction and fluid and electrolyte replacement needs. Urine sodium less than 10 mEq/L suggests inadequate fluid resuscitation. Note: During first 24 hr after burn, hemoconcentration is common because of fluid shifts into the interstitial space.
Insert/maintain large-bore IV catheter(s). Administer calculated IV replacement of fluids, electrolytes, plasma, albumin.
Monitor laboratory studies (e.g., Hb/Hct, electrolytes, random urine sodium).
Administer medications as indicated: Diuretics, e.g., mannitol (Osmitrol);
May be indicated to enhance urinary output and clear tubules of debris/prevent necrosis if acute renal failure (ARF) is present. Although hyperkalemia often occurs during first 2448 hr (tissue destruction), subsequent replacement may be necessary because of large urinary losses. Antacids may reduce gastric acidity; histamine inhibitors decrease production of hydrochloric acid to reduce risk of gastric irritation/bleeding.
Potassium;
Antacids, e.g., calcium carbonate (Titralac), magaldrate (Riopan); histamine inhibitors, e.g., cimetidine (Tagamet)/ranitidine (Zantac).
ACTIONS/INTERVENTIONS
RATIONALE
Shock Prevention (NIC)
Collaborative
Add electrolytes to water used for wound debridement, as indicated. Washing solution that approximates tissue fluids may minimize osmotic fluid shifts.
Das könnte Ihnen auch gefallen
- Burns - Airway Clearance, Risk For IneffectiveDokument2 SeitenBurns - Airway Clearance, Risk For Ineffectivemakyofrancis20Noch keine Bewertungen
- Decrease Cardiac OutputDokument6 SeitenDecrease Cardiac OutputGerardeanne ReposarNoch keine Bewertungen
- NCP Ineffective Cardiopulmonary PerfusionDokument3 SeitenNCP Ineffective Cardiopulmonary PerfusionjamiemapanaoNoch keine Bewertungen
- NCP For CHF 3 Activity IntoleranceDokument2 SeitenNCP For CHF 3 Activity IntoleranceAngelyn ArdinesNoch keine Bewertungen
- NCP AneurysmDokument4 SeitenNCP AneurysmJanielle Christine Monsalud100% (1)
- Care Plan ExampleDokument2 SeitenCare Plan Exampleincess27100% (1)
- NCP FVDDokument1 SeiteNCP FVDsisjing88510Noch keine Bewertungen
- "Mayroong Namuong Dugo Sa Utak Niya Kaya Hindi Maayos Ang Daloy NG Dugo Rito" As Verbalized by The Patient's MotherDokument6 Seiten"Mayroong Namuong Dugo Sa Utak Niya Kaya Hindi Maayos Ang Daloy NG Dugo Rito" As Verbalized by The Patient's MotherAllisson BeckersNoch keine Bewertungen
- Ineffective Tissue PerfusionDokument2 SeitenIneffective Tissue PerfusionDiane ReyNoch keine Bewertungen
- NCP CKDDokument3 SeitenNCP CKDRiel TumandaNoch keine Bewertungen
- Nursing Care PlanDokument11 SeitenNursing Care Planaycee0316100% (1)
- NCP Impaired Gas Exhange CHEST INJURYDokument4 SeitenNCP Impaired Gas Exhange CHEST INJURYMa. Elaine Carla Tating100% (2)
- Nueva Ecija University of Science and TechnologyDokument7 SeitenNueva Ecija University of Science and TechnologyKym RonquilloNoch keine Bewertungen
- Pathophysiology of NephrosclerosisDokument2 SeitenPathophysiology of NephrosclerosisJessica Damasen Caballero0% (1)
- Deficit)Dokument2 SeitenDeficit)Lee DeeNoch keine Bewertungen
- 6639burn NCPDokument18 Seiten6639burn NCPDivina Grace Renon Camba100% (1)
- Resulting in Damage To Brain Tissue.: Definition: Independent: IndependentDokument4 SeitenResulting in Damage To Brain Tissue.: Definition: Independent: Independentalliahjoyce ignacioNoch keine Bewertungen
- NCP and DStudyDokument8 SeitenNCP and DStudyJessica Rosan Hewald ManapatNoch keine Bewertungen
- Diarrhea Care PlanDokument2 SeitenDiarrhea Care Planzepoli_zepoly6232100% (1)
- NCPDokument3 SeitenNCPJezza RequilmeNoch keine Bewertungen
- Glaucoma NCPDokument4 SeitenGlaucoma NCPChantal CaraganNoch keine Bewertungen
- NCM 118L/ 119L (Related Learning Experience) Day 3-ActivityDokument4 SeitenNCM 118L/ 119L (Related Learning Experience) Day 3-ActivityNicole Villanueva, BSN - Level 3ANoch keine Bewertungen
- Aubrey Rose A. Vidon BSN 3Y1 - 2Dokument2 SeitenAubrey Rose A. Vidon BSN 3Y1 - 2Aria100% (1)
- Cancer Nursing Care Plan (NCP) - Risk For InfectionDokument2 SeitenCancer Nursing Care Plan (NCP) - Risk For InfectionAngie MandeoyaNoch keine Bewertungen
- NCP ShockDokument5 SeitenNCP ShockJanina Patricia BuddleNoch keine Bewertungen
- NCP Inffective Tissue PerfusionDokument3 SeitenNCP Inffective Tissue PerfusionPaul Cubacub0% (1)
- NCP HyperthermiaDokument1 SeiteNCP HyperthermiaPastor James PacadaljenNoch keine Bewertungen
- Cu 5Dokument2 SeitenCu 5Clareze AbadNoch keine Bewertungen
- NCP Ineffective Tissue Perfusion and Self Care DeficitDokument5 SeitenNCP Ineffective Tissue Perfusion and Self Care DeficitFrances Anne Pasiliao100% (3)
- Concept Map - Abby !Dokument2 SeitenConcept Map - Abby !Abegail Abaygar100% (3)
- NCP - Fluid Volume DeficitDokument2 SeitenNCP - Fluid Volume DeficitPatrice LimNoch keine Bewertungen
- Risk For InfectionDokument1 SeiteRisk For InfectionEuanne OrellanoNoch keine Bewertungen
- CVA Case StudyDokument20 SeitenCVA Case Studybetchai18100% (5)
- NCP Tissue PerfusionDokument2 SeitenNCP Tissue PerfusionNiña Montejo Ealdama100% (1)
- SchistosomiasisDokument92 SeitenSchistosomiasisIvan Juan75% (4)
- NCP - Fluid RetentionDokument3 SeitenNCP - Fluid RetentionMichelle Teodoro100% (1)
- Septic Shock Student Case StudyDokument6 SeitenSeptic Shock Student Case StudyJenn GallowayNoch keine Bewertungen
- DIAGNOSIS Hyperthermia Related To Increased Metabolic Rate, Illness. ASSESSMENT SubjectiveDokument1 SeiteDIAGNOSIS Hyperthermia Related To Increased Metabolic Rate, Illness. ASSESSMENT Subjectivemawel100% (1)
- NCP AidsDokument16 SeitenNCP AidstferdianingsihNoch keine Bewertungen
- NCP in BurnsDokument2 SeitenNCP in BurnsMayet De Castro Lejano80% (5)
- NCP PROPER Pain and Decreased Cardiac OutputDokument3 SeitenNCP PROPER Pain and Decreased Cardiac OutputErienne Lae Manangan - CadalsoNoch keine Bewertungen
- Leukemia NCPDokument1 SeiteLeukemia NCPPaulo ZamoraNoch keine Bewertungen
- 3 NCP Ineffective Tissue PerfusionDokument2 Seiten3 NCP Ineffective Tissue PerfusionSteffi MurielNoch keine Bewertungen
- Nursing 215 Care Plan 2 FinalDokument7 SeitenNursing 215 Care Plan 2 Finalapi-283303129Noch keine Bewertungen
- Pathophysiology of HCVD DM2 CVD Left Basal GangliaDokument1 SeitePathophysiology of HCVD DM2 CVD Left Basal GangliaJake Caballo100% (1)
- NCP For CTTDokument1 SeiteNCP For CTTJen Rhae LimNoch keine Bewertungen
- NCP MiDokument4 SeitenNCP MiPitaca Madiam Annabehl PaulNoch keine Bewertungen
- Pathophysiology of AMLDokument1 SeitePathophysiology of AMLjake251996100% (1)
- Case Scenario: Hot Spells, Porous BonesDokument10 SeitenCase Scenario: Hot Spells, Porous Bonesjaira magbanua100% (1)
- Decreased Cardiac Output FinalDokument2 SeitenDecreased Cardiac Output FinalSandraDeeNoch keine Bewertungen
- Nursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisDokument19 SeitenNursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisRiza Angela BarazanNoch keine Bewertungen
- Concept Map of Nasal ObstructionDokument2 SeitenConcept Map of Nasal ObstructionChad Viajar100% (1)
- Burns - Tissue Perfusion, IneffectiveDokument3 SeitenBurns - Tissue Perfusion, Ineffectivemakyofrancis20100% (1)
- Impaired Urinary EliminationDokument3 SeitenImpaired Urinary EliminationAgcopra MtchNoch keine Bewertungen
- Ineffective Tissue PerfusionDokument2 SeitenIneffective Tissue PerfusionClaidelyn De Leyola100% (1)
- Fluid Volume DeficitDokument12 SeitenFluid Volume DeficitKersee GailNoch keine Bewertungen
- Fluid Management & Blood Component Therapy: Key ConceptsDokument31 SeitenFluid Management & Blood Component Therapy: Key ConceptsMohammad Pino HakimNoch keine Bewertungen
- Acute Renal Failure Nursing Care PlanDokument15 SeitenAcute Renal Failure Nursing Care PlanRanusha AnushaNoch keine Bewertungen
- HemodialysisDokument4 SeitenHemodialysisJon Adam Bermudez SamatraNoch keine Bewertungen
- Seminars 2019 PDFDokument200 SeitenSeminars 2019 PDFpaingmyintNoch keine Bewertungen
- Burns - Pain, AcuteDokument3 SeitenBurns - Pain, Acutemakyofrancis20Noch keine Bewertungen
- Burns - Infection, Risk ForDokument4 SeitenBurns - Infection, Risk Formakyofrancis20Noch keine Bewertungen
- Burns - Tissue Perfusion, IneffectiveDokument3 SeitenBurns - Tissue Perfusion, Ineffectivemakyofrancis20100% (1)
- Peritoneal DialysisDokument23 SeitenPeritoneal Dialysismakyofrancis20Noch keine Bewertungen
- Burns - Nutrition, Imbalanced, Less Than Body RequirementsDokument2 SeitenBurns - Nutrition, Imbalanced, Less Than Body Requirementsmakyofrancis20Noch keine Bewertungen
- Burns - Skin Integrity, ImpairedDokument2 SeitenBurns - Skin Integrity, Impairedmakyofrancis20Noch keine Bewertungen
- Burns - Knowledge, DeficientDokument2 SeitenBurns - Knowledge, Deficientmakyofrancis20Noch keine Bewertungen
- Burns - Body Image Disturbed Role Performance, IneffectiveDokument2 SeitenBurns - Body Image Disturbed Role Performance, Ineffectivemakyofrancis20Noch keine Bewertungen
- Burns - Mobility, Impaired PhysicalDokument2 SeitenBurns - Mobility, Impaired Physicalmakyofrancis20Noch keine Bewertungen
- Renal Dialysis: Care SettingDokument1 SeiteRenal Dialysis: Care Settingmakyofrancis20Noch keine Bewertungen
- RENAL DIALYSIS - Constipation, Risk ForDokument1 SeiteRENAL DIALYSIS - Constipation, Risk Formakyofrancis20Noch keine Bewertungen
- Burns: Thermal/Chemical/Electrical (Acute and Convalescent Phases)Dokument4 SeitenBurns: Thermal/Chemical/Electrical (Acute and Convalescent Phases)makyofrancis20Noch keine Bewertungen
- RENAL DIALYSIS - Self-Care Deficit (Specify)Dokument1 SeiteRENAL DIALYSIS - Self-Care Deficit (Specify)makyofrancis20Noch keine Bewertungen
- RENAL DIALYSIS - Nutrition, Imbalanced, Less Than Body RequirementsDokument3 SeitenRENAL DIALYSIS - Nutrition, Imbalanced, Less Than Body Requirementsmakyofrancis20Noch keine Bewertungen
- NURSING DIAGNOSIS: Fear/Anxiety May Be Related To: Actions/Interventions RationaleDokument2 SeitenNURSING DIAGNOSIS: Fear/Anxiety May Be Related To: Actions/Interventions Rationalemakyofrancis20Noch keine Bewertungen
- RENAL DIALYSIS - Thought Processes, Risk For DisturbedDokument2 SeitenRENAL DIALYSIS - Thought Processes, Risk For Disturbedmakyofrancis20Noch keine Bewertungen
- RENAL DIALYSIS - Knowledge, DeficientDokument2 SeitenRENAL DIALYSIS - Knowledge, Deficientmakyofrancis20Noch keine Bewertungen
- RENAL DIALYSIS - Mobility, Impaired PhysicalDokument2 SeitenRENAL DIALYSIS - Mobility, Impaired Physicalmakyofrancis20Noch keine Bewertungen
- Test 1Dokument1 SeiteTest 1makyofrancis20Noch keine Bewertungen
- RENAL DIALYSIS - Anxiety (Specify Level) FearDokument2 SeitenRENAL DIALYSIS - Anxiety (Specify Level) Fearmakyofrancis20Noch keine Bewertungen
- RENAL DIALYSIS - Body Image Disturbed Self-Esteem, Situational LowDokument2 SeitenRENAL DIALYSIS - Body Image Disturbed Self-Esteem, Situational Lowmakyofrancis20Noch keine Bewertungen
- ROS ChecklistDokument2 SeitenROS Checklistmindful33Noch keine Bewertungen
- SeizureDokument9 SeitenSeizuremakyofrancis20Noch keine Bewertungen
- Pathognomonic SignsDokument1 SeitePathognomonic Signsmakyofrancis20Noch keine Bewertungen
- AbstractDokument1 SeiteAbstractmakyofrancis20Noch keine Bewertungen
- 6th Central Pay Commission Salary CalculatorDokument15 Seiten6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Graham RecipeDokument2 SeitenGraham Recipemakyofrancis20Noch keine Bewertungen
- 6th Central Pay Commission Salary CalculatorDokument15 Seiten6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Module: Lie Detection Techniques (3/1) : at The End of This Chapter The Student's Should Be Able To UnderstandDokument84 SeitenModule: Lie Detection Techniques (3/1) : at The End of This Chapter The Student's Should Be Able To Understandjonas ventolinaNoch keine Bewertungen
- Chapter 2. Acute and Chronic InflammationDokument6 SeitenChapter 2. Acute and Chronic InflammationWaseem Khan AfridiNoch keine Bewertungen
- Digestive SystemDokument17 SeitenDigestive SystemTricia GorozaNoch keine Bewertungen
- Fetal Movements As A Predictor of HealthDokument8 SeitenFetal Movements As A Predictor of HealthWordtreader PtNoch keine Bewertungen
- Human-Anatomy Kids PDFDokument1 SeiteHuman-Anatomy Kids PDFZeltzin FloresNoch keine Bewertungen
- Abdominal Wall: Muh. Iqbal Basri Anatomy Department Hasanuddin UniversityDokument33 SeitenAbdominal Wall: Muh. Iqbal Basri Anatomy Department Hasanuddin UniversityDavid ChristianNoch keine Bewertungen
- Assessment of Left Ventricular Fraction by Real-Time,: Ejection and Volumes Two-DimensionalDokument8 SeitenAssessment of Left Ventricular Fraction by Real-Time,: Ejection and Volumes Two-DimensionalAinil MardiahNoch keine Bewertungen
- Respiratory FailureDokument39 SeitenRespiratory FailureMuntasir BashirNoch keine Bewertungen
- Cytokines, Cytokine Receptors and Chemokines: Sept. 11, 2014Dokument101 SeitenCytokines, Cytokine Receptors and Chemokines: Sept. 11, 2014ANJU0709Noch keine Bewertungen
- Biology Exemplar ProblemsDokument5 SeitenBiology Exemplar ProblemsAkshatha NayakNoch keine Bewertungen
- Jace's PoV Manor SceneDokument4 SeitenJace's PoV Manor Sceneisa soaresNoch keine Bewertungen
- Strength and HealthDokument37 SeitenStrength and HealthhugocoutoNoch keine Bewertungen
- Hyper Bilirubin Emi ADokument36 SeitenHyper Bilirubin Emi ASai Krishna MaddiralaNoch keine Bewertungen
- Meyer 2020Dokument12 SeitenMeyer 2020Administrador OccimetricNoch keine Bewertungen
- Haemonetics MCS+ Analyzer - User Manual PDFDokument110 SeitenHaemonetics MCS+ Analyzer - User Manual PDFPedro Villanueva C.Noch keine Bewertungen
- Genetic Basis of Blood Group Diversity: ReviewDokument13 SeitenGenetic Basis of Blood Group Diversity: ReviewHasna F BidayahNoch keine Bewertungen
- 1st PUC Biology Nov 2017Dokument2 Seiten1st PUC Biology Nov 2017Abhi50% (2)
- BCM 202 Quality AssuranceDokument18 SeitenBCM 202 Quality AssuranceTeeNoch keine Bewertungen
- What Are Proteins and What Do They DoDokument11 SeitenWhat Are Proteins and What Do They Domuhammad aslamNoch keine Bewertungen
- Rapid Learning in RoboticsDokument169 SeitenRapid Learning in RoboticsMatthew PadillaNoch keine Bewertungen
- 2012 Guidelines StableIschemicHeartDisease 11-20-12Dokument121 Seiten2012 Guidelines StableIschemicHeartDisease 11-20-12cephalicaNoch keine Bewertungen
- Pengaruh Warna Cahaya Terhadap Pertumbuhan TanamanDokument8 SeitenPengaruh Warna Cahaya Terhadap Pertumbuhan TanamanCalon InsinyurNoch keine Bewertungen
- Arterial Lines Mark Hammerschmidt, RN FromDokument9 SeitenArterial Lines Mark Hammerschmidt, RN FromMark Hammerschmidt100% (3)
- Final ThesisDokument86 SeitenFinal ThesisNisa FatimaNoch keine Bewertungen
- Block Diagram PT MonitorDokument7 SeitenBlock Diagram PT MonitorAbabil Academy KannanNoch keine Bewertungen
- The Split Brain in ManDokument6 SeitenThe Split Brain in ManAKISNoch keine Bewertungen
- Paths of DiscoveryDokument365 SeitenPaths of DiscoverycarlodolciNoch keine Bewertungen
- Gut MorphologyDokument27 SeitenGut MorphologyrezqNoch keine Bewertungen
- Cardiac Physiology NotesDokument11 SeitenCardiac Physiology Notespunter11100% (1)
- The Cervical & Thoracic Spine - Mechanical Diagnosis & Therapy - Vol 2Dokument288 SeitenThe Cervical & Thoracic Spine - Mechanical Diagnosis & Therapy - Vol 2booksbearreading100% (6)