Beruflich Dokumente
Kultur Dokumente
Wyden Keynote Speech at Accountable Care Organization Summit
Hochgeladen von
Senator Ron WydenCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Wyden Keynote Speech at Accountable Care Organization Summit
Hochgeladen von
Senator Ron WydenCopyright:
Verfügbare Formate
Keynote Speech (As Prepared for Delivery) U.S.
Senator Ron Wyden National Accountable Care Organization Summit June 13, 2013 Thank you for the opportunity to open this Accountable Care Organization summit. Being asked to comment on the issues and possibilities surrounding Accountable Care Organizations by Dr. Elliott Fisher and Dr. Mark McClellan means having the chance to run with the right crowd. This audience has decades of experience and a passion for health reform, so this morning Id like to put before you what I believe is the premier challenge for Americas premier health program. Of course, that program is Medicare. Notwithstanding the recent bit of good news from the Medicare Trustees, Medicare faces unsustainably high costs because the program has never been about what most drives costs chronic disease. Seniors entering the Medicare program today are sicker than when their parents enrolled, with more cancer, more heart disease, and more diabetes. Unfortunately, too few policy makers and health providers have recognized this fact, and that needs to change. That covers just about everybody in my profession and most people in yours. Currently, about 70% of Medicare patients have two or more chronic health conditions and account for more than 90% of Medicare spending, or almost $500 billion a year. Yet when chronic care even gets a rare mention with policy makers in Washington, it is usually dismissed with a weve got to improve care coordination and everybody nods and moves on. Similarly, conversations with providers rarely seem to move beyond reimbursement. The Medicare guarantee is a godsend and lifeline for millions of older and disabled Americans. Improving quality and controlling spiraling costs for the chronically ill deserves a more thoughtful response than the health care equivalent of whatever. Ill start by describing our chronic care challenges through the experiences of a fictional heroine, Mrs. Jones. While fictional, Mrs. Jones is quite typical of senior Medicare patients today. She illustrates the urgent need to refocus the program on chronic care. Lets say Mrs. Jones turns 65 and isnt feeling so hot. She hasnt been to the doctor in a while, and wants to find someone who specializes in treating seniors. Unfortunately, there are no geriatric practitioners available in her area. But after considerable hassle she finds a family physician willing to see new Medicare patients. Mrs. Jones goes to her Welcome to Medicare visit, and her physician finds evidence of three chronic conditions - Type 2 diabetes, chronic obstructive pulmonary disease and heart disease. The family doctor refers Mrs. Jones to a cardiologist and pulmonologist for further examination and tests, and also recommends visiting a nutritionist to review her diet and exercise regime. Medicare fully covers Mrs. Jones first doctors visit thanks to the Affordable Care Act. Unfortunately, thats her last real break. Her specialist visits will require a 20% co-pay after she
reaches her Part B deductible. Shell also have co-pays for any new prescriptions or tests. While Medicare covers nutrition therapy, she decides she can manage her diet on her own and doesnt go to the nutritionist. Despite her efforts at self-treatment, the diabetes gets worse. Since the family doctor referred Mrs. Jones to specialists outside his group practice, the fact that Mrs. Jones skipped the specialists visits was not reported to the family doctor. Soon after, Mrs. Jones forgets to take her insulin and she ends up at the emergency room. She gets admitted to the hospital because of the risk factors associated with her worsening diabetes. Shes stabilized, told to keep up her insulin regimen, and sent home with a bill for the inpatient hospital deductible - $1,184 to be exact. At this point, Mrs. Jones cant remember the name of her family doctor, or provides the wrong name, so the hospital does not know where to turn in describing Mrs. Jones condition to the appropriate physician. Now many of you in the audience may be thinking, Yep, I know patients like Mrs. Jones. Thats why the health care law was passed - to help people like her. In the future, Mrs. Jones will be assisted by ACOs, group practices and health plans in the Medicare Shared Savings program and other demonstration projects. All those thoughts have some validity. Unfortunately, heres why the challenges facing the hypothetical Mrs. Jones are going to remain the norm, rather than the exception, without further reform. Our first hurdle is the attribution rule for ACOs in the Affordable Care Act. Under this wellmeaning rule, ACOs must serve everyone coming through the door. This rule exists because there has been a legitimate fear that too many providers want to shed risk and avoid the sickest patients. However, the unintended consequences of attribution for improved chronic care are significant. In its present form, the attribution rule limits ACOs that want to specialize in chronic care from reaching out to the sickest seniors and providing them with the highest-quality, integrated, affordable chronic care services. The second issue is the current gap between where ACOs are now, and where the largest number of sick seniors live. For example, the evidence shows ACOs are not being set up in Alabama, where there are a lot of seniors in very poor health. But there are going to be plenty of ACOs in Massachusetts, where the seniors have the good fortune of being some of the healthiest in the country. Massachusetts and Alabama have roughly the same percentage of people on Medicare. Massachusetts spends more than the national average on Medicare while Alabama spends less. Healthy seniors in Massachusetts can access six Medicare ACOs, and more vulnerable seniors in Alabama have none.
Third, even if you are a senior in an ACO, you may not be lucky enough to have an individual care plan, which is the centerpiece of top-quality, coordinated chronic care. This is because the current ACO rule is ambiguous about who is entitled to an individual chronic care plan. The rule says that high-risk individuals have to have a plan, but who knows whether Mrs. Jones is going meet that threshold. Even if Mrs. Jones could find an ACO in her area, improbable since she had trouble even finding a doctor, its unlikely she would have received an individual care plan because her physician didnt consider her chronic conditions high risk. Fourth, ACOs are barred from creating incentives, or better health rewards, that encourage seniors to be as healthy as possible. Mrs. Jones doctor saw that she had diabetes, but had no way to encourage her to go for a retina scan or to see a nutritionist. For some people, these may seem like small things. But they often have a huge impact for people like Mrs. Jones, and it can mean much lower costs in the long run. The Cleveland Clinic and the Oregon Health Sciences Center have helped Senator Portman and I pursue bipartisan alternatives along these lines. There are places to look for answers. One of the presenters for this conference, Dr. Ken Coburn of Health Quality Partners in Doylestown, Pennsylvania, is succeeding in promoting quality chronic care for the elderly. Health Quality Partners was created more than a decade ago as a demonstration project. From the beginning, Dr. Coburn and his team at HQP have sought out some of the sickest seniors. These patients are treated using a thoughtful list of interventions tailored to their individual needs. The results have been a clear success - hospitalizations reduced by 39%; net health care costs cut by 28%; and, overall mortality reduced by over 25%. Unfortunately, our government has not given Dr. Coburn the green light to expand and tap the programs full potential. For example, the government has limited his ability to grow the program on the ground that its just a demonstration project. It seems to me, the whole point of demonstrations is to let the successful efforts grow and serve more people. What Dr. Coburn has been able to do doesnt happen by osmosis. Its about active engagement; active management; and, active care coordination from both the provider and the patient. As he would tell you, this has required an intense and impressive system of protocols, standards, training, advanced analytics and the list goes on. Its also meant doing something really innovative - seeing patients at home. The current system remains mired in the assumption that patients need to do what theyve always done - go to the doctors office. That ignores the fact that its very difficult for many patients to get to their doctor whether they live in a city or a rural area. Now, another system, Montefiore in the Bronx, demonstrates why Dr. Coburns principles of care management are important no matter where you live. Montefiore doctors understand the challenges their Medicare patients face because they visit them in their homes at the top of old,
seven-story buildings without elevators. Access isnt just a problem for people living in rural area. A third promising approach is used by Providence Health and Services, which operates in my home state of Oregon and four other western states. Providence functions as both a provider and a Medicare Advantage plan. Even in my low-cost state of Oregon, they are successfully managing the needs of chronically ill seniors by working closely with their patients, and by rewarding physicians who deliver results. These patients are less likely to be hospitalized than those in traditional Medicare, and they are getting better treatment at a lower cost which is really something in a low-cost state like mine. Why shouldnt people in Alabama have access to what Oregon has? The Medicare guarantee should not depend on where you live. Because many think the Pacific Northwest is unique, I asked Dr. Jack Wennberg, the amazing and pioneering researcher from Dartmouth, to examine the latest Medicare data from across the country. He looked at high-quality, high-performing systems that treat patients with the most intense needs in high- and low- cost states. As usual, he did some great work, and found that chronically ill patients can be treated at lower costs all around the country. In fact, the evidence shows high-performing systems spent 13 to 24 percent less than the state averages for patients with the same needs. Those are huge savings. Heres my take on how they are doing it. First, high-performing systems are successfully identifying high-need patients during their first visit. This allows them to implement a coordinated chronic care plan early, and, as a result, they keep more patients out of the hospital. They have a different approach. Patients are cared for differently, and thats what Medicare should be all about. Washington has been stuck for ages in tired, circular Medicare debates about increasing premiums on the wealthy and raising the age of eligibility. Those are important issues. They do not, however, reform the health care delivery system for the sickest seniors. That ought to be a priority for the days ahead. Fortunately, this room is full of people who care about Medicare and the millions of seniors who rely on it. To recap, here are several solutions to the challenges described this morning: One, the attribution rule needs to be changed to allow providers to specialize in chronic care. Our objective should be to make the adverse selection issue disappear, by creating specific consumer protections for seniors in plans that specialize in senior chronic care, while fully retaining the current protections against discrimination for all other seniors under current law. Two, Medicare should guarantee high-quality, coordinated care to chronically ill seniors throughout the country. Medicare reimbursement should be reconfigured to target areas with the highest incidence of chronic illness, and reward practitioners, in those areas, who improve care and hold down costs.
Three, individual care plans need to be the rule, rather than the exception, for seniors with more than one chronic condition. And four, incentives should be available to help keep seniors as healthy as possible. These solutions are within our grasp, and, I hope, this will be considered the beginning of a new debate. I know that Ive given you a lot to chew on. Over the coming months, I intend to work with colleagues from both political parties to turn these proposals into legislation. These ideas will protect the sacred guarantee that is Medicare, and help tackle one major force behind Americas debt and deficit. Seniors and taxpayers deserve no less. Thank you very much.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Senators Urge Trump To Keep Promises On Medicare and MedicaidDokument8 SeitenSenators Urge Trump To Keep Promises On Medicare and MedicaidTom UdallNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Combined College Affordability ClipsDokument40 SeitenCombined College Affordability ClipsSenator Ron WydenNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
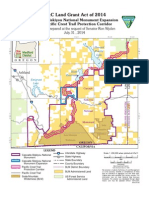
- Bill Text O&C Act 2014Dokument157 SeitenBill Text O&C Act 2014Senator Ron WydenNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- O&C Act of 2014 Section by SectionDokument8 SeitenO&C Act of 2014 Section by SectionSenator Ron WydenNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Wyden: Floor Statement - Interrogation ReportDokument11 SeitenWyden: Floor Statement - Interrogation ReportSenator Ron WydenNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Map06 MoistDry 073114Dokument1 SeiteMap06 MoistDry 073114Senator Ron WydenNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- O&C Act of 2014 Section by SectionDokument8 SeitenO&C Act of 2014 Section by SectionSenator Ron WydenNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Wyden Amdts To Cybersecurity and Information Sharing Act (CISA)Dokument6 SeitenWyden Amdts To Cybersecurity and Information Sharing Act (CISA)Senator Ron WydenNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- O&C Act of 2014 Covered LandsDokument1 SeiteO&C Act of 2014 Covered LandsSenator Ron WydenNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- Remarks of Senator Ron Wyden at TechFestNWDokument5 SeitenRemarks of Senator Ron Wyden at TechFestNWSenator Ron WydenNoch keine Bewertungen
- O&C Land Grant Act of 2014Dokument1 SeiteO&C Land Grant Act of 2014Senator Ron WydenNoch keine Bewertungen
- Map07C ClackamasWater 073114Dokument1 SeiteMap07C ClackamasWater 073114Senator Ron WydenNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The O&C Act of 2014 Bill TextDokument163 SeitenThe O&C Act of 2014 Bill TextSenator Ron WydenNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Map02 ForestryEmphasis 073114Dokument1 SeiteMap02 ForestryEmphasis 073114Senator Ron WydenNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Map03 ConservationNetwork 073114Dokument1 SeiteMap03 ConservationNetwork 073114Senator Ron WydenNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Map08B IllinoisValley 073114Dokument1 SeiteMap08B IllinoisValley 073114Senator Ron WydenNoch keine Bewertungen
- Map07B HillsboroWater 073114Dokument1 SeiteMap07B HillsboroWater 073114Senator Ron WydenNoch keine Bewertungen
- Map08A CSNM Expansion 073114Dokument1 SeiteMap08A CSNM Expansion 073114Senator Ron WydenNoch keine Bewertungen
- Map01 CoveredLands 073114Dokument1 SeiteMap01 CoveredLands 073114Senator Ron WydenNoch keine Bewertungen
- Map05 LegacyOldGrowth 073114Dokument1 SeiteMap05 LegacyOldGrowth 073114Senator Ron WydenNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Map04 ConservationEmphasis 073114Dokument1 SeiteMap04 ConservationEmphasis 073114Senator Ron WydenNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Map08G WellingtonWildlands 073114Dokument1 SeiteMap08G WellingtonWildlands 073114Senator Ron WydenNoch keine Bewertungen
- Map06 MoistDry 073114Dokument1 SeiteMap06 MoistDry 073114Senator Ron WydenNoch keine Bewertungen
- Map07A McKenzieWater 073114Dokument1 SeiteMap07A McKenzieWater 073114Senator Ron WydenNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Map08I BrummittFir 073114Dokument1 SeiteMap08I BrummittFir 073114Senator Ron WydenNoch keine Bewertungen
- Map07D SpringfieldWater 073114Dokument1 SeiteMap07D SpringfieldWater 073114Senator Ron WydenNoch keine Bewertungen
- Map08D MolallaNationalRecArea 073114Dokument1 SeiteMap08D MolallaNationalRecArea 073114Senator Ron WydenNoch keine Bewertungen
- Map08L SpecialEnvironmentalZones 073114Dokument1 SeiteMap08L SpecialEnvironmentalZones 073114Senator Ron WydenNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Map08J CrabtreeValley 073114Dokument1 SeiteMap08J CrabtreeValley 073114Senator Ron WydenNoch keine Bewertungen
- Implementing Collaborative Care in LMICDokument5 SeitenImplementing Collaborative Care in LMICDr DangalNoch keine Bewertungen
- Cultivating A Thinking Surgeon New Perspectives On Clinical TeaDokument294 SeitenCultivating A Thinking Surgeon New Perspectives On Clinical TeaKatherine Jones100% (1)
- Literature ReviewDokument24 SeitenLiterature ReviewAdamuNoch keine Bewertungen
- Final SBFR Training PPT 19th April 2022 MoHDokument113 SeitenFinal SBFR Training PPT 19th April 2022 MoHDaniel Firomsa100% (6)
- Doctor Royal Raymond Rife-The End of All DiseasesDokument3 SeitenDoctor Royal Raymond Rife-The End of All DiseasesnailsssNoch keine Bewertungen
- Ethics of Health Care A Guide For Clinical Practice 3rd EditionDokument420 SeitenEthics of Health Care A Guide For Clinical Practice 3rd EditionAnvic BernardoNoch keine Bewertungen
- Medical Tourism and SingaporeDokument4 SeitenMedical Tourism and SingaporeDr Jason Yap100% (1)
- (Chapter IV) : Data Privacy Act of 2012Dokument26 Seiten(Chapter IV) : Data Privacy Act of 2012Rhea PaguigbaoNoch keine Bewertungen
- Results of HSRC Study On South African Healthcare Workers Mental Health and Covid 19Dokument64 SeitenResults of HSRC Study On South African Healthcare Workers Mental Health and Covid 19Laura Lopez GonzalezNoch keine Bewertungen
- The Hahnemannian Monthly. 1905pdfDokument37 SeitenThe Hahnemannian Monthly. 1905pdfBruntNoch keine Bewertungen
- Manila Hotel Corp vs NLRC Jurisdiction CaseDokument12 SeitenManila Hotel Corp vs NLRC Jurisdiction Caselilackill LorNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Curriculum Vitae English MedicineDokument7 SeitenCurriculum Vitae English Medicineafiwgjbkp100% (2)
- 2020 HS ProspectusDokument249 Seiten2020 HS Prospectustangwanlu9177Noch keine Bewertungen
- Nurse's Role and Responsibilities in Administration of MedicationDokument88 SeitenNurse's Role and Responsibilities in Administration of MedicationSonia Singh88% (33)
- Guidance To Understanding Implications of IRMERDokument52 SeitenGuidance To Understanding Implications of IRMERrochimNoch keine Bewertungen
- Advanced Nursing PracticeDokument12 SeitenAdvanced Nursing PracticeKish KimzNoch keine Bewertungen
- Sa332a-1702en PDokument6 SeitenSa332a-1702en PBobby Chipping0% (2)
- The Malabar ExperienceDokument46 SeitenThe Malabar ExperienceBalakrishna GopinathNoch keine Bewertungen
- Reshaping Herbal Medicine - Knowledge, Education and Professional Culture (2005) PDFDokument200 SeitenReshaping Herbal Medicine - Knowledge, Education and Professional Culture (2005) PDFLuiz FelipeNoch keine Bewertungen
- Medical Ethics (2 Course)Dokument6 SeitenMedical Ethics (2 Course)Divine ElyaNoch keine Bewertungen
- Leoncio General Hospital: Medical CertificateDokument33 SeitenLeoncio General Hospital: Medical Certificatefranchiser6Noch keine Bewertungen
- AgoniaDokument24 SeitenAgoniaTunjung Manhatanti AviantaraNoch keine Bewertungen
- An Australian Surgical Team in Vietnam, Long Xuyen October 1967 To October 1968.Dokument198 SeitenAn Australian Surgical Team in Vietnam, Long Xuyen October 1967 To October 1968.CliveBond100% (1)
- FINAL MEMORIAL Medical NegligenceDokument17 SeitenFINAL MEMORIAL Medical Negligenceajay narwalNoch keine Bewertungen
- Physician's White CoatDokument44 SeitenPhysician's White CoatApril AmyBabyNoch keine Bewertungen
- PFCM - Technical Paper Preventive MedicineDokument2 SeitenPFCM - Technical Paper Preventive MedicineYolanda Primrosa NurhanNoch keine Bewertungen
- John Ure Licensed Revoked by Missouri BoardDokument9 SeitenJohn Ure Licensed Revoked by Missouri BoardEntercomSTLNoch keine Bewertungen
- Three Years of H CL TherapyDokument50 SeitenThree Years of H CL TherapyVíctor ValdezNoch keine Bewertungen
- History of Fairfield County, OhioDokument339 SeitenHistory of Fairfield County, OhiorollypollyintrainingNoch keine Bewertungen
- RTMC 2008-Registration SessionsDokument4 SeitenRTMC 2008-Registration SessionsAamir HamaadNoch keine Bewertungen
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisVon EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (13)