Beruflich Dokumente
Kultur Dokumente
Jurnal Penyakit Ginjal Karena Analgetik
Hochgeladen von
Aditya Prasetya SOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Jurnal Penyakit Ginjal Karena Analgetik
Hochgeladen von
Aditya Prasetya SCopyright:
Verfügbare Formate
The CARI Guidelines Caring for Australasians with Renal Impairment
Analgesic-Associated Kidney Disease
Date written: July 2005 Final submission: September 2005 Author: Merlin Thomas
GUIDELINES a. Analgesic intake should be discontinued in patients with analgesic nephropathy. (Level II III evidence) b. Non-selective COX-1 and COX-2 inhibitors (with the specific exception of low dose aspirin) should be avoided, where possible, in patients with hypertension, as their use is associated with loss of BP control and reduction in efficacy of antihypertensive drug therapy. (Level I evidence) c. Analgesic and anti-inflammatory therapy form an important component of the management of a variety of chronic degenerative diseases. (Level I evidence) The beneficial effects of these agents should be balanced against the risk of progressive renal damage and hypertension associated with their chronic and habitual use.
SUGGESTIONS FOR CLINICAL CARE
(Suggestions are based on Level III and IV evidence)
Continued analgesic intake is associated with an increased faster rate of decline of renal function and increased risk of end-stage kidney disease (ESKD) in patients with analgesic nephropathy. (Level II-III evidence; large prospective cohort studies; clinically relevant outcomes; consistent strong effects). Cessation of analgesic use has been associated with retardation of kidney failure progression. (Level II-III evidence; several retrospective cohort studies; clinically relevant outcomes; variable effects). The use of non-selective COX-1 and COX-2 inhibitors is associated with loss of BP control and reduction in efficacy of antihypertensive drug therapy. (Level I-II evidence; large meta-analyses and RCTs, clinically relevant outcomes; consistent strong effects)
Background
Combinations of antipyretic analgesics taken in large doses over long periods of time are associated with the development of a slowly progressive kidney disease characterised by papillary necrosis and interstitial scarring. Currently, at least 6% of patients reaching ESKD in Australia have analgesic nephropathy (ANZDATA). The objective of this guideline is to evaluate the available clinical evidence pertaining to the impact of interventions on renal functional decline in analgesic nephropathy (AN).
Prevention of Progression of Kidney Disease (April 2006) Page 1
The CARI Guidelines Caring for Australasians with Renal Impairment
This guideline does not address the known associations between AN and malignancy, peptic ulcer disease and cardiovascular disease that may be positively influenced by habitual analgesic use.
Search strategy
Databases searched: The search for MeSH terms and text words for analgesic nephropathy was carried out in Medline (1966 to September Week 2 2004). Date of search: 17 September 2004.
What is the evidence?
Habitual analgesic use has been associated with renal impairment and progression to ESKD in a number of large prospective cohort studies: 200 patients with active analgesic abuse were followed for 7 years and the rate of decline in renal function compared to age-matched controls. Renal function decline was significantly greater in patients with ongoing analgesic abuse, including a 6.1 times relative risk of renal impairment compared to the control population (Elseviers et al, 1995). In a large prospective, longitudinal, epidemiological study of 623 healthy women 3049 years old who had evidence of a regular intake of phenacetin and a matched control group of 621 women, the relative risk for deaths due to urological or kidney disease was 16.1 (95%CI: 3.966.1) (Dubach UC, 1986 87).
There are no randomised controlled trials (RCTs) in AN. Australia and New Zealand Dialysis Registry data shows a progressive decline in AN as a cause of ESKD after the withdrawal of phenacetin from compound analgesics in Australia (McCredie 1989). In prospective, observational, cohort studies, continued use of analgesics has been associated with an accelerated rate of progression of renal insufficiency in AN (MacKinnon et al 1989, Hauser et al 1991) In retrospective, cohort studies, patients with analgesic nephropathy who discontinued using analgesics were less likely to develop ESKD, than those who continued their consumption of analgesics (Gonwa et al 1981, Kindler et al 1990). Cessation of analgesic intake may also slow the rate of loss of renal function, even when renal insufficiency is well advanced (McCredie et al 1989). Recent case-control studies have raised the possibility that habitual analgesic use could increase the likelihood or rate of progression of chronic kidney disease (CKD) per se. In the study by Sandler et al (1989), the odds ratios for the development of CKD was highest for patients with interstitial nephritis and renal insufficiency of unknown cause who habitually used analgesics. However, there was a borderline increase in the odds ratios for patients with a diagnosis of nephrosclerosis, diabetic nephropathy, and glomerulonephritis. Similarly, Perneger et al (1994) found the
Prevention of Progression of Kidney Disease (April 2006) Page 2
The CARI Guidelines Caring for Australasians with Renal Impairment
increased risk of CKD was similar in the four groups of patients with renal disease due to diabetic nephropathy, hypertension, other specific causes, and unknown causes. However, there is currently insufficient evidence for a causal association between habitual use of analgesic and an increased risk of ESKD. Regular use of analgesic drugs containing phenacetin is associated with an increased risk of hypertension (a know risk factor for progressive nephropathy). In a large prospective, longitudinal epidemiological study of 623 healthy women 3049 years old who had evidence of a regular intake of phenacetin and a matched control group of 621 women, the odds ratio for the incidence of hypertension was 1.6 (95%CI: 1.2 2.1) (Dubach et al 1991). Some of this reflects the increased risk of cardiovascular disease and kidney disease.
Similarly, regular use of non-selective COX-1 and COX-2 inhibitors is associated with an increased risk of hypertension and destabilisation of blood pressure control in patients with hypertension. Two separate meta-analyses that examine the effects of non-selective COX-1 inhibitors including over-the-counter preparations such as naproxen, indomethacin, and ibuprofen implicate them as contributing to loss of BP control and reduction in efficacy of antihypertensive drug therapy (Johnson et al 1994, Pope et al 1993). COX-2 inhibitors have also been associated with destabilization of blood pressure control in RCTs (Sowers et al 2005). It should be noted that chronic low-dose aspirin has not been associated with detrimental effects on blood pressure control (Avanzini et al 2000, Johnson 1994; Nawarskas et al 1999).
Summary of the evidence
Therapy with non-selective COX-1 and COX-2 inhibitors is associated with loss of BP control and reduction in efficacy of antihypertensive drug therapy in some patients. As blood pressure control is a key component part of the management of patients with CKD, it is recommended that these agents should be avoided, where possible, in patients with CKD. This recommendation does not apply to low dose aspirin, which has neutral effects on BP control, together with beneficial effects on cardiovascular outcomes. Analgesic intake should be discontinued in patients with analgesic nephropathy, as early as possible, to have the greatest likelihood of slowing the progressive kidney scarring associated with habitual analgesic use. Analgesic and anti-inflammatory therapy form an important component part of the management of a variety of chronic degenerative diseases. The beneficial effects of these agents should be balanced against the risk of progressive kidney damage and hypertension associated with their chronic and habitual use.
Prevention of Progression of Kidney Disease (April 2006)
Page 3
The CARI Guidelines Caring for Australasians with Renal Impairment
What do the other guidelines say?
Kidney Disease Outcomes Quality Initiative: Attempts should be made to prevent and correct acute decline in GFR. Frequent causes of acute decline in GFR include non-steroidal anti-inflammatory agents, including cyclo-oxygenase type 2 inhibitors; UK Renal Association: No recommendation. Canadian Society of Nephrology: No recommendation. European Best Practice Guidelines: No recommendation. International Guidelines: Analgesic-Associated Kidney Disease. NIH Consensus Statement 1984: (Kindler et al 1990). The main strategies of management must include: 1. Avoidance of antipyretic-analgesic agents, as well as non-steroidal antiinflammatory drugs. 2. Prompt treatment of proven urinary tract infections. 3. Awareness that a necrotic papilla may slough and obstruct the urinary tract, sometimes requiring prompt intervention to prevent further loss of renal function. 4. Careful supervision of hypertension. 5. Recognition that tumours of the urinary tract may occur more frequently in patients with analgesic nephropathy. Unexplained episodes of haematuria, including a marked increase in microscopic haematuria, should therefore be evaluated carefully. 6. Consideration of the non-renal manifestations of the analgesic abuse syndrome. Ad Hoc Committee of the International Study Group on Analgesics and Nephropathy: (Feinstein AR, et al. 2000) 1. There is insufficient evidence to associate non-phenacetin combined analgesics with nephropathy. 2. New studies should be done to provide appropriate data to resolve the question. US Food and Drug Administration (FDA): Analgesic combination containing paracetamol, aspirin, and caffeine is safe and effective for the use in uncomplicated migraine.
Implementation and audit:
No recommendation.
Prevention of Progression of Kidney Disease (April 2006)
Page 4
The CARI Guidelines Caring for Australasians with Renal Impairment
Suggestions for future research:
The recent reintroduction of compound analgesics containing paracetamol and caffeine as OTC medications in New Zealand and Asia (but not Australia) should be closely monitored by renal physicians.
Prevention of Progression of Kidney Disease (April 2006)
Page 5
The CARI Guidelines Caring for Australasians with Renal Impairment
References
Avanzini F, Palumbo G, Alli C et al. Effects of low-dose aspirin on clinic and ambulatory blood pressure in treated hypertensive patients. Collaborative Group of Primary Prevention Project (PPP) Hypertension study. Am J Hypertens. 2000; 13: 61116. Dubach UC, Rosner B, Sturmer T. An epidemiologic study of abuse of analgesic drugs. Effects of phenacetin and salicylate on mortality and cardiovascular morbidity (196887) N Engl J Med 1991; 324:15560. Elseviers MM, De Broe ME. A long-term prospective controlled study of analgesic abuse in Belgium. Kidney Int 1995; 48: 19123 Feinstein AR, Heinemann LA, Curhan GC et al. Relationship between nonphenacetin combined analegesics and nephropathy: A review. Ad Hoc Committee of the International Study Group on Analgesics and Nephropathy. Kidney International 2000, 58:225964 Gonwa TA, Hamilton RW, Buckalew VM Jr. Chronic renal failure and end-stage renal disease in northwest North Carolina. Importance of analgesic-associated nephropathy. Arch Intern Med 1981; 141: 4625. Hauser AC, Derfler K, Balcke P. Progression of renal insufficiency in analgesic nephropathy: impact of continuous drug abuse. J Clin Epidemiol 1991; 44: 536. Johnson AG, Nguyen TV, Day RO. Do nonsteroidal anti-inflammatory drugs affect blood pressure? A meta-analysis. Ann Intern Med 1994; 121: 289300. Kindler J, Giani G, Handt S, Sieberth HG. The effect of various factors on the progression of kidney insufficiency cause by analgesic nephropathy. Klin Wochenschr 1990; 68: 10429. MacKinnon B, Boulton-Jones M, McLaughlin K. Analgesic-associated nephropathy in the West of Scotland: a 12-year observational study. Nephrol Dial Transplant 2003; 18: 18005. McCredie M, Stewart JH, Mathew TH et al. The effect of withdrawal of phenacetincontaining analgesics on the incidence of kidney and urothelial cancer and renal failure Clinical Nephrol. 1989; 31: 359. McDonald SP, Russ G. New Patients, pp. 814. ANZDATA Registry Report 2003. Australia and New Zealand Dialysis and Transplant Registry, Adelaide, South Australia. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease; Evaluation, Classification and Stratification. Am J Kidney Dis 2002; 39 (suppl 1): S1S266.
Prevention of Progression of Kidney Disease (April 2006)
Page 6
The CARI Guidelines Caring for Australasians with Renal Impairment
Nawarskas JJ, Townsend RR, Cirigliano MD et al. Effect of aspirin on blood pressure in hypertensive patients taking enalapril or losartan. Am J Hypertens 1999; 12: 784 89. Perneger TV, Whelton PK, Klag MJ. Risk of kidney failure associated with the use of acetaminophen, aspirin, and nonsteroidal antiinflammatory drugs. N Engl J Med 1994; 331: 16759. Pope JE, Anderson JJ, Felson DT. A meta-analysis of the effects of nonsteroidal anti-inflammatory drugs on blood pressure. Arch Intern Med 1993; 153: 477484. Sandler DP, Smith JC, Weinberg CR et al. Analgesic use and chronic renal disease. N Engl J Med 1989; 320:123843. Sowers JR, White WB, Pitt B et al. Celecoxib Rofecoxib Efficacy and Safety in Comorbidities Evaluation Trial (CRESCENT) Investigators. The effects of cyclooxygenase-2 inhibitors and nonsteroidal anti-inflammatory therapy on 24-hour blood pressure in patients with hypertension, osteoarthritis, and type 2 diabetes mellitus. Arch Intern Med 2005; 165: 1618.
Prevention of Progression of Kidney Disease (April 2006)
Page 7
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Shnider and Levinsons Anesthesia For Obstetrics, 5th EdDokument879 SeitenShnider and Levinsons Anesthesia For Obstetrics, 5th EdSri Hari50% (2)
- The Expanded Program On ImmunizationDokument26 SeitenThe Expanded Program On ImmunizationJudee Marie MalubayNoch keine Bewertungen
- Hb transports O2 & CO2; blood doping increases levelsDokument2 SeitenHb transports O2 & CO2; blood doping increases levelsAmir BaNoch keine Bewertungen
- Anesthesia Professional Coding For McKesson Anesthesia Care™Dokument2 SeitenAnesthesia Professional Coding For McKesson Anesthesia Care™McKesson Surgical SolutionsNoch keine Bewertungen
- ProP - Differentiating Nuclear Sclerosis From CataractsDokument6 SeitenProP - Differentiating Nuclear Sclerosis From CataractsDita TaepangNoch keine Bewertungen
- What Is GerontologyDokument44 SeitenWhat Is GerontologyPalwasha Khan100% (1)
- Interview QuestionsDokument7 SeitenInterview QuestionsRitesh KumarNoch keine Bewertungen
- ITLS Patient EvaluationDokument15 SeitenITLS Patient Evaluationjoepz1982100% (1)
- Conservative Management of Cutaneous Sinus Tract of Dental Origin Report of Two CasesDokument4 SeitenConservative Management of Cutaneous Sinus Tract of Dental Origin Report of Two CasesInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Riza T. Calixtro: ObjectivesDokument2 SeitenRiza T. Calixtro: ObjectivesLorinel MendozaNoch keine Bewertungen
- Inputs or Factors or Regulators: That Control Hormone SecretionDokument13 SeitenInputs or Factors or Regulators: That Control Hormone SecretionAbdul MoqeetNoch keine Bewertungen
- A Comprehensive Introduction To Abdominal Acupuncture 1519537480Dokument5 SeitenA Comprehensive Introduction To Abdominal Acupuncture 1519537480Marco GutzNoch keine Bewertungen
- Chemotherapy Extravasation: Establishing A National Benchmark For Incidence Among Cancer CentersDokument9 SeitenChemotherapy Extravasation: Establishing A National Benchmark For Incidence Among Cancer CentersRiri AmalinaNoch keine Bewertungen
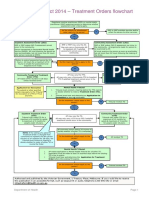
- Flowchart - Mental Health Act Treatment OrderDokument1 SeiteFlowchart - Mental Health Act Treatment OrderEdwin100% (1)
- First Diagnosis of Systemic Lupus Erythematosus in HospitalizedDokument35 SeitenFirst Diagnosis of Systemic Lupus Erythematosus in HospitalizedFranco PacelloNoch keine Bewertungen
- S19640en PDFDokument47 SeitenS19640en PDFDrSyeda RimaNoch keine Bewertungen
- Protocol For PT With Avulsed ToothDokument3 SeitenProtocol For PT With Avulsed ToothAyeshaNoch keine Bewertungen
- Spotters 1Dokument10 SeitenSpotters 1elavarkuzhali2019Noch keine Bewertungen
- Lumbosacral Plexus # 6Dokument6 SeitenLumbosacral Plexus # 6Arcel De Luca G.Noch keine Bewertungen
- Caesarean Section Performing Caesarean SectionDokument13 SeitenCaesarean Section Performing Caesarean SectionBlablabla BlablablaNoch keine Bewertungen
- Indonesia Ophthalmologic Anesthesia Society (IOAS) : Susunan Acara Pertemuan Ilmiah Tahunan Ke - 4 16 - 17 Juli 2022Dokument4 SeitenIndonesia Ophthalmologic Anesthesia Society (IOAS) : Susunan Acara Pertemuan Ilmiah Tahunan Ke - 4 16 - 17 Juli 2022ruthameliapNoch keine Bewertungen
- Autism Spectrum DisorderDokument14 SeitenAutism Spectrum DisorderAngie McaNoch keine Bewertungen
- Policy For Exemption From Assessment and Examination FinalDokument28 SeitenPolicy For Exemption From Assessment and Examination FinalGloria JaisonNoch keine Bewertungen
- Central SensitizationDokument14 SeitenCentral SensitizationdracoscribdNoch keine Bewertungen
- Registered Pharmacist Affidavit FormatDokument1 SeiteRegistered Pharmacist Affidavit FormatSyed NawazNoch keine Bewertungen
- Hypertensive EmergenciesDokument28 SeitenHypertensive EmergenciesluonganhsiNoch keine Bewertungen
- Top 100 Study Items For The Otolaryngology (ENT) Board ExaminationDokument8 SeitenTop 100 Study Items For The Otolaryngology (ENT) Board ExaminationsduxNoch keine Bewertungen
- Bone Marrow Biopsy SheetDokument2 SeitenBone Marrow Biopsy SheetSouvik BairagyaNoch keine Bewertungen
- Diseases of The MouthDokument4 SeitenDiseases of The MouthAhmed Gh Al-zechrawiNoch keine Bewertungen
- Freedom TherapeuticDokument2 SeitenFreedom TherapeuticAna WongNoch keine Bewertungen