Beruflich Dokumente
Kultur Dokumente
Heart Failure
Hochgeladen von
niklukOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Heart Failure
Hochgeladen von
niklukCopyright:
Verfügbare Formate
Print: Chapter 19.
Heart Failure
Pgina 1 de 15
Print Close Window
Note: Large images and tables on this page may necessitate printing in landscape mode. Copyright 2007 The McGraw-Hill Companies. All rights reserved. Current Family Medicine > Chapter 19. Heart Failure >
Essentials of Diagnosis
Left ventricular failure: Paroxysmal nocturnal dyspnea, orthopnea, dyspnea on exertion, fatigue, and peripheral edema. Third or fourth heart sound, increased jugular venous pressure, hepatojugular reflux, displaced cardiac apex, rales, wheezing, murmur, or peripheral edema. Any electrocardiographic (ECG) abnormality, radiographic evidence of pulmonary venous congestion, cardiomegaly, or pleural effusion; elevated B-type natriuretic peptide; echocardiographic evidence of left ventricular dysfunction. Right ventricular failure: increased jugular venous pressure, hepatomegaly, peripheral edema.
General Considerations
Increased survivorship after acute myocardial infarction (MI) and improved treatment of hypertension, valvular heart disease, and coronary artery disease (CAD) have led to a significant increase in the prevalence of heart failure in the United States. Overall prevalence of any congestive heart failure (CHF) diagnosis is estimated at
2.6% (2.7% in men; 1.7% in women). In addition, 5.6% of the population may have isolated moderate to severe diastolic dysfunction, with age greater than 65 years and female gender being consistent predictors of preserved left ventricular systolic function. Diastolic dysfunction is rarely associated with acute MI. Based on this apparent underlying reasons for the increased likelihood of diastolic heart failure in these populations.
bias, the possibility of biological changes associated with increasing age and female gender have been proposed as The prevalence of any type of heart failure increases with age. Asymptomatic left ventricular systolic dysfunction (LVSD) has been found to be as prevalent as symptomatic LVSD: 1.4% and 1.5%, respectively. Moderate or severe isolated diastolic dysfunction appears to be as common as systolic dysfunction, and systolic dysfunction
Pathogenesis
appears to increase with the severity of diastolic dysfunction.
Heart failure results from a complex interplay of compensatory mechanisms used by the body to adjust for
decreased cardiac output in response to stresses placed on the myocardium (Table 191). These compensatory
mechanisms are rooted in the activation of the sodium-retaining renin-angiotensin-aldosterone and sympathetic nervous systems (neurohormonal adaptations). The purpose is to maintain blood pressure and tissue perfusion. However, these compensatory mechanisms, which increase afterload, lead to myocardial deterioration and worsening myocardial contractility. The heart then enters into a vicious cycle of increasing release of
neurohormones (norepinephrine, angiotensin II, aldosterone, endothelin, vasopressin, and cytokines) that further increases afterload, allowing the heart to spiral into failure in a progressive fashion through cardiac remodeling. myocardial cell performance and phenotype. These neurohormones act both in an indirect and in a directly toxic fashion to affect hemodynamic stressors and
Table 191. Possible Causes of Heart Failure.
Coronary artery disease, including myocardial infarction Diabetes mellitus Hypertension Increased BMI (overweight) Increased age Smoking Primary valvular heart disease Congenital heart disease Cardiomyopathies (dilated [idiopathic], hypertrophic, and restrictive)
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Viral myocarditis (including HIV) Pericardial disease Infiltrative disease (hemochromatosis, sarcoidosis, amyloidosis) Recent pregnancy Connective tissue disease Hyperthyroid or hypothyroid disease Toxin (chemotherapy, substance abuse [especially alcohol or cocaine], heavy metal) High-output failure secondary to anemia or thiamine deficiency (beriberi) Cor pulmonale and pulmonary hypertension (in right-sided failure) BMI, body mass index.
Pgina 2 de 15
Causes of Cardiac Failure
With the advent of improved hypertension treatment, earlier identification of valvular heart disease, and improved survival following MI, CAD and diabetes mellitus are now the leading causes of heart failure in the United States. CAD is a substantial predictor of developing clinically evident heart failure or symptomatic versus asymptomatic significant factors for developing heart failure in women. Even in women with increased hyperglycemia but no diagnosis of diabetes mellitus, the risk of heart failure is increased compared with normoglycemic women. LVSD. CHF has also been found to be twofold higher in all diabetic patients. Diabetes mellitus is one of the most
Evidence points to a diabetic cardiomyopathy independent of CAD that is more prominent in diabetic women. This be related to the overt effect of diabetes on progression of CAD. It is also unknown whether treatment of longstanding diabetes mellitus decreases the risk of developing heart failure. Poorly controlled hypertension and valvular heart disease remain major precipitants of heart failure. Often-
raises the question of the direct effect of diabetes on the myocardium and endothelium. This association could also
overlooked risk factors in the development of heart failure are smoking, physical inactivity or obesity, and lower socioeconomic status. Tobacco is estimated to cause approximately 17% of CHF cases in the United States. The effect of cigarettes may be direct or indirect in relation to promoting CAD risk. Lower socioeconomic status may such as hypertension, diabetes mellitus, and CAD.
limit access to higher quality health care, resulting in decreased adherence to treatment of modifiable risk factors Aurigemma GP et al: Predictive value of systolic and diastolic function for incident congestive heart failure in the
elderly: The Cardiovascular Health Study. J Am Coll Cardiol 2001;37: 1042. [PMID: 11263606] 2004:110:1424. [PMID: 15353499]
Bibbins-Domingo K et al: Predictors of heart failure among women with coronary disease. Circulation He J et al: Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med 2001;161:996. [PMID: 11295963] 2003;41:217. [PMID: 12535812] Masoudi FA et al: Gender, age, and heart failure with preserved left ventricular systolic function. J Am Coll Cardiol Rogers VL et al: Trends in heart failure incidence and survival in a community-based population. JAMA 2004;292:344. [PMID: 15265849] Stratton IM et al: Association of glycaemia with macrovascular and microvascular complications type 2 diabetes (UKPDS 35): Prospective observational study. BMJ 2000;321:405. [PMID: 10938048]
Classification & Prevention
The American College of Cardiology (ACC)/American Heart Association (AHA) classification of heart failure
emphasizes the progressive nature of the syndrome. This classification replaced the New York Heart Association (NYHA) classification with four stages that help define appropriate therapy at each level. The new classification recognizes that there are risk factors and structural prerequisites for the development of heart failure and that onset of clinically evident disease (Table 192).
therapeutic interventions initiated early in the disease process can reduce morbidity and mortality and delay the
Table 192. Progression of Heart Failure and Recommended Evidence-Based Therapies.
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Progression of Heart Failure At Risk for Heart Failure ACC/AHA stage Stage A: high risk Heart Failure
Pgina 3 de 15
Stage B: Stage C: symptomatic or Stage D: refractory asymptomatic, history of heart failure end-stage heart cardiac structural failure abnormalities or remodeling Class I: asymptomatic Class II: symptoms with significant exertion Goals: Class III: symptoms on minor exertion Class IV: symptoms at rest
NYHA classification
Not applicable
Therapy Beneficial and effective; recommended Goals: Disease management:
Goals: Hypertension1 Lipid disorders1 Diabetes mellitus3 Thyroid disease3 Secondary prevention of atherosclerotic
3
Goals:
Stage A measures Drugs (in appropriate patients): ACEI1 or ARB2 -Blockers (history of MI1; no MI3)
Stage A and B measures Stage A, B, and C measures Dietary sodium Meticulous fluid restriction3 retention control2 Drugs/Devices: Routine use: Diuretics3 (fluid retention) ACEI1 -Blockers1 In selected patients: ARB
1
Decision regarding appropriate level of care and referral to heart failure program1 Options: End-of-life care or hospice3 Extraordinary measures: heart transplantation2
vascular disease3 Behavior change :
Smoking cessation Regular exercise Avoidance of alcohol and illicit drug use
Aldosterone antagonists2 Implantable cardioverterdefibrillator2 Cardiac resynchronization
Reasonably beneficial and probably recommended
Drugs (in appropriate
patients): ACEI1 or ARB3 (in patients with vascular disease or diabetes mellitus)
therapy1
Drugs/Devices (in selected patients): Digitalis2 Hydralazine or nitrates1
Options (extraordinary measures): permanent mechanical support2
ACC/AHA, American College of Cardiology/American Heart Association; NYHA, New York Heart Association; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker.
1 2
3
Level of evidence A (evidence from multiple randomized trials, meta-analysis). Level of evidence B (evidence from single randomized or nonrandomized trials).
Data, in part, from Hunt SA et al: ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult. Circulation 2005;112:e154.
Level of evidence C (expert opinion, case studies, standard of care).
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Pgina 4 de 15
Patients in ACC/AHA stages A and B do not have clinical heart failure but are at risk for developing heart failure. Stage A includes those at risk but not manifesting structural heart disease. Early identification and aggressive treatment of modifiable risk factors remain the best prevention for heart failure. Life-style modification,
pharmacologic therapy, and counseling can improve or correct conditions such as CAD, hypertension, diabetes
mellitus, hyperlipidemia, obesity, tobacco abuse, and alcohol or illicit substance abuse. Stage B represents persons who are asymptomatic but have structural heart disease or impaired left ventricular function. Stage C comprises the bulk of persons with heart failure who have past or current symptoms and associated underlying structural heart disease. Stage D includes refractory patients with heart failure who may need advanced and specialized treatment strategies.
The NYHA classification gauges the severity of symptoms for patients with stage C and D heart failure. This is a
Clinical Findings
subjective assessment that can change frequently, secondary to treatment response.
A high index of suspicion is necessary to diagnose the syndrome of heart failure early in its clinical presentation, because it is frequently manifested by nonspecific signs and symptoms. Patients are often elderly with comorbidity, symptoms may be mild, and routine clinical assessment lacks specificity. A prompt diagnosis allows for early treatment with therapies proven to delay the progression of heart failure and improve quality of life. establishing severity, and guiding response to therapy. Heart failure is a clinical diagnosis for which no single examination or test can establish the presence or absence with 100% certainty. Evaluation is directed at confirming the presence of heart failure, determining cause, identifying comorbid illness,
Hunt SA et al; American College of Cardiology; American Heart Association Task Force on Practice Guidelines;
American College of Chest Physicians; International Society for Heart and Lung Transplantation; Heart Rhythm Circulation 2005;112:e154. [PMID: 16160202] SYMPTOMS AND SIGNS
Society: ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult.
The primary manifestations of symptomatic heart failure are dyspnea and fatigue. Limited exercise tolerance and fluid retention may eventually lead to pulmonary congestion and peripheral edema. Neither of these symptoms necessarily dominates the clinical picture at the same time. Dyspnea, whether at rest or with exertion, is present in nearly all patients with heart failure and indicates left ventricular dysfunction. Its absence makes heart failure ventricular dysfunction in a predominantly symptomatic population with a reported 100% sensitivity. highly unlikely. The absence of dyspnea on exertion essentially rules out the presence of heart failure due to left Other symptoms that are helpful in diagnosing heart failure include orthopnea, paroxysmal nocturnal dyspnea orthopnea, or edema are not present the likelihood of heart failure decreases. Nonspecific symptoms include upper quadrant pain secondary to hepatic congestion and peripheral edema.
(PND), and peripheral edema. PND has the highest specificity of any symptom for heart failure. Likewise, if PND, chronic nonproductive cough, wheezing, and nocturia. Patients with right ventricular failure may present with right No single clinical symptom has been shown to be both sensitive and specific. A substantial portion of the
population has asymptomatic left ventricular dysfunction and the history, alone, is insufficient to make the identifying the cause of heart failure and assessing response to therapy. PHYSICAL EXAMINATION
diagnosis of heart failure. However, a detailed history and review of symptoms remain the best approach in
The clinical examination can provide important information concerning the degree to which cardiac output is
reduced and the degree of volume overload and ventricular enlargement. It can also provide clues to noncardiac causes of dyspnea. The presence of a third heart sound, S3 (ventricular filling gallop), increases the likelihood of gallop), are specific for increased left ventricular end-diastolic pressure and decreased left ventricular ejection fraction. The presence of an S3 has been found to be superior to S4 in identifying patients with abnormal left ventricular function. Gallop rhythm (S3 and S4) and displacement of cardiac apex have also been found to be specific predictors of left ventricular dysfunction.
heart failure with the most specificity of any physical examination finding. An S3 or a fourth heart sound, S4 (atrial
The presence of jugular venous distention, pulmonary rales, pitting peripheral edema, and hepatojugular reflux also helps to make the diagnosis, and the absence of the first three of these findings is useful for lowering the likelihood of heart failure. Cardiac murmurs may be an indication of primary valvular disease. Asymmetric rales or
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Pgina 5 de 15
rhonchi on the pulmonary examination may indicate primary pulmonary pathology such as pneumonia or chronic obstructive pulmonary disease (COPD). Examination of the thyroid can exclude thyromegaly or goitercauses of abnormal thyroid function that can precipitate heart failure. Dullness to percussion or auscultation of the lungs findings alone does little to help rule out heart failure. LABORATORY FINDINGS
could indicate pleural effusion. Hepatomegaly can indicate passive hepatic congestion. The absence of any of these
A complete blood count is necessary to rule out anemia as a cause of high-output failure. Electrolyte analysis may reveal deficiencies, commonplace with treatment, that can make the patient prone to arrhythmias. Hyponatremia is a poor prognostic sign indicating significant activation of the renin-aldosterone-angiotensin system.
Abnormalities on liver tests can indicate hepatic congestion. Thyroid function tests can detect hyper- or hypothyroidism. Fasting lipid profile, fasting glucose, and hemoglobin A1c level can reveal comorbid conditions that or an alcoholic and presents with high-output failure, thiamine testing is indicated to rule out deficiency related to beriberi. Further testing to determine etiologic factors of heart failure must be based on historical findings. B-Type Natriuretic Peptide
may need to be better controlled. Iron studies can detect iron deficiency or overload. If the patient is malnourished
More specific laboratory testing includes evaluation of B-type natriuretic peptide (BNP) levels. BNP is a cardiac pressure overload. Circulating BNP levels are increased in patients with heart failure and have rapid turnover,
neurohormone secreted from the ventricles and, to some extent, the atrial myocardium in response to volume and indicating that BNP responds in proportion to the size of the exacerbation and in turn increases and decreases with each individual exacerbation. Although no BNP threshold indicates the presence or absence of heart failure with and physical examination, helps differentiate between pulmonary and cardiac causes of dyspnea (Table 193). 100% certainty, the BNP level is the most accurate predictor of heart failure and, in conjunction with the history
Table 193. Factors Influencing B-Type Natriuretic Peptide (BNP) Levels.
Factors That Cause Elevated BNP (> 100 pg/mL) Heart failure Advanced age Renal failure1 Acute coronary syndromes Lung disease with cor pulmonale Acute large pulmonary embolism High-output cardiac states NYHA, New York Heart Association.
1Adjusted
Factors That Lower BNP in the Setting of Heart Failure Acute pulmonary edema Stable NYHA class I disease with low ejection fraction Acute mitral regurgitation Mitral stenosis Atrial myxoma
levels are based on glomerular filtration rate (GFR). GFR 6089 mL/min: no adjustment in the 100 pg/mL threshold (see text). GFR 3059 mL/min: BNP > 201. GFR 1529 mL/min: BNP > 225. GFR < 15 mL/min: unknown utility of BNP levels. Adapted, with permission, from Wang CS et al: Does this dyspneic patient in the emergency department have congestive heart failure? JAMA 2005;294:1944. The likelihood of heart failure increases with BNP levels above 100 pg/mL, as follows:
Less than 100 pg/mL: diagnosis of heart failure is unlikely; consider alternate diagnoses. 100400 pg/mL: increased likelihood of heart failure; history, physical examination, and other tests are required to improve the probability of the diagnosis. Greater than 400 pg/mL: diagnosis of heart failure is highly likely.
Electrocardiography
LVSD is unlikely to be present if the ECG is normal (sensitivity of 94%). Left bundle branch block, left ventricular hypertrophy, and evidence of MI all significantly increase the likelihood of left ventricular dysfunction. Atrial fibrillation is the most important predictor of heart failure in a dyspneic patient, followed by new T-wave changes and any abnormal ECG finding. An abnormal ECG does not mean the patient has chronic heart failure but is an
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Pgina 6 de 15
indication for echocardiography to determine whether a structural abnormality is present. The ECG also identifies detect arrhythmias once heart failure is confirmed. The finding of left bundle branch block is an unfavorable any cause, including sudden death.
possible causes of heart failure, including signs of ischemic heart disease or possible infiltrative processes, and can prognostic indicator in patients with heart failure, among whom there is an increased 1-year mortality rate from Knudsen CW et al: Diagnostic value of B-type natriuretic peptide and chest radiographic findings in patients with acute dyspnea. Am J Med 2004;116:363. [PMID: 15006584] Krishnaswamy P et al: Utility of B-natriuretic peptide levels in identifying patients with left ventricular systolic or diastolic dysfunction. Am J Med 2001;111:274. [PMID: 11566457] Circulation 2002;105:2328. [PMID: 12021215] Engl J Med 2002;347:161. [PMID: 12124404] Med 2004;350:647. [PMID: 14960741] Maisel A: B-type natriuretic peptide levels: Diagnostic and prognostic in congestive heart failure: What's next? Maisel AS et al: Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Mueller C et al: Use of B-type natriuretic peptide in the evalua tion and management of acute dyspnea. N Engl J Tang WH et al: Plasma B-type natriuretic peptide levels in ambulatory patients with established chronic symptomatic systolic heart failure. Circulation 2003;108:2964. [PMID: 14662703] IMAGING STUDIES Chest Radiography
The chest radiograph can provide valuable clues in patients presenting with acute dyspnea. The presence of
venous congestion, interstitial edema, alveolar edema, cardiomegaly, or pleural effusion increases the likelihood of heart failure in dyspneic patients. Cardiomegaly (cardiac-to-thoracic width ratio > 50%) was the best predictor of decreased ejection fraction, whereas redistribution (upper lobe pulmonary vein dilation and lower lobe pulmonary vein constriction in response to a rise in pulmonary venous pressure secondary to increased left ventricular
preload) and hilar haze were the best predictors of increased preload. The absence of cardiomegaly and pulmonary venous congestion were the most useful findings on chest radiography for lowering the likelihood of heart failure. Cardiac Doppler Echocardiography Echocardiography is of undeniable utility in the evaluation of suspected and newly diagnosed heart failure (Table 194). An echocardiography study is recommended for all patients diagnosed with heart failure. It provides important information concerning cardiac systolic (ejection fraction or fractional shortening) and diastolic function.
Table 194. Electrocardiographic Parameters Useful in the Diagnosis of Heart Failure.
Parameter Left ventricular function (ejection fraction) Information Provided Normal value: 60% 40%
Abnormal value: < 50%
Diastolic function Pulmonary artery pressure
Alteration of left ventricular compliance Normal value: 35 mm Hg
Significant systolic dysfunction value:
Estimation of left ventricular filling pressure Adapted, with permission, from Vitarelli A et al: The role of echocardiography in the diagnosis and management of heart failure. Heart Fail Rev 2003;8:181. Echocardiographic findings can help differentiate among the various causes of heart failure, including ischemic heart disease, idiopathic cardiomyopathy, hypertensive heart disease, and valvular heart disease. Echocardiography helps to distinguish segmental wall motion abnormalities, which can correlate with ischemia. An
increase in cardiac mass (left ventricular hypertrophy) can be associated with hypertensive cardiomyopathy versus cardiac remodeling, which is an adaptive phenomenon associated with myocardial injury. The echocardiogram also helps to elucidate differences between dilated (idiopathic), hypertrophic, and restrictive cardiomyopathies. Diastolic changes can be elucidated by Doppler imaging. Left ventricular hypertrophy and a dilated left atrium are clues to the possible presence of left ventricular diastolic dysfunction. Dobutamine stress echocardiography is an
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Pgina 7 de 15
important tool to assess for myocardial ischemia and viability in the form of ischemic, stunned, or hibernating
myocardium. In addition to ischemia and valvular abnormalities, potential reversible etiologies of heart failure that echocardiography can help to uncover include pericardial disorders such as effusion or tamponade. It can help left ventricular dysfunction, ventricular size, and shape add important prognostic information. determine appropriate timing of therapy by uncovering asymptomatic LVSD in high-risk populations. The degree of The routine reevaluation with echocardiography of clinically stable patients in whom no change in management is contemplated is not recommended. If the body habitus of the patient makes echocardiography impractical, radionuclide ventriculography can be performed to assess left ventricular ejection fraction and volumes. Cardiac Catheterization
Coronary angiography is recommended for patients with new-onset heart failure of uncertain etiology, despite the absence of anginal symptoms or negative findings on exercise stress testing. Coronary angiography should be testing (echocardiography or nuclear imaging). Wall motion abnormalities seen on echocardiography or strongly considered for patients with LVSD and a strong suspicion of ischemic myocardium based on noninvasive hibernating myocardium detected by dobutamine stress echocardiography are particularly useful indicators
because they appear shortly after ischemia or infarction. The extent and severity of wall motion abnormalities
have been shown to correlate with the size of the myocardium at risk. A strong association has been demonstrated between decreased mortality and revascularization (80% relative reduction in risk of death) only in patients found to have myocardial viability by thallium perfusion imaging, dobutamine echocardiography, or positron emission these abnormalities may have significant implications for urgency of treatment, resultant pump function, and subsequent morbidity and mortality. tomography scanning; with no apparent benefit in the absence of demonstrated viability. Therefore, evaluation of
Using clusters of clinical findings from the history, physical examination, and diagnostic tests is a better diagnostic
strategy than using isolated findings. The clinical examination enables the clinician to categorize patients as having low, intermediate, and high pretest probabilities for the diagnosis of heart failure. More specialized testing, such as BNP results, helps clarify the diagnosis in patients determined to have an intermediate probability of heart failure. artery disease and left ventricular dysfunction: A meta-analysis. J Am Coll Cardiol 2002;39:1151. [PMID: 11923039] Allman KC et al: Myocardial viability testing and impact of revascularization on prognosis in patients with coronary
Marcus GM et al: Association between phonocardiographic third and fourth heart sounds and objective measures of left ventricular function. JAMA 2005;293:2238. [PMID: 15886379] 2003;8:181. [PMID: 12766498] Vitarelli A et al: The role of echocardiography in the diagnosis and management of heart failure. Heart Fail Rev Wang CS et al: Does this dyspneic patient in the emergency department have congestive heart failure? JAMA 2005;294:1944. [PMID: 16234501]
Differential Diagnosis
Because heart failure is estimated to be present in only about 30% of patients with dyspnea in the primary care lung disease, pulmonary embolism, anemia, thyrotoxicosis, carbon monoxide poisoning, arrhythmia, anginal
setting, clinicians need to consider differential diagnoses for dyspnea such as asthma, COPD, infection, interstitial equivalent (CAD), valvular heart disease, cardiac shunt, obstructive sleep apnea, and severe obesity causing
Treatment
hypoventilation syndrome.
Most evidence-based treatment strategies have focused on patients with systolic rather than diastolic heart failure; hence, stage-specific outpatient management of patients with chronic systolic heart failure is the focus of the discussion that follows. Although stages A through D of the ACC/AHA heart failure classification represent and recommended for later stages (see Table 192).
progressive cardiac risk and dysfunction, the treatment strategies recommended at earlier stages are applicable to SYSTOLIC HEART FAILURE High Risk for Systolic Heart Failure (Stage A)
Individuals with conditions and behaviors that place them at high risk for heart failure but who do not have
structurally abnormal hearts are classified as ACC/AHA stage A and should be treated with therapies that can delay
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Pgina 8 de 15
progression of cardiac dysfunction and development of heart failure. Optimizing hypertension treatment based on the current guidelines from the Seventh Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) can reduce new-onset heart failure by 50%. Therapies such as
diuretics, -blockers, angiotensin-converting enzyme inhibitors (ACEIs), and angiotensin II receptor blockers (ARBs) are proven to be more effective than calcium channel blockers and doxazosin in preventing heart failure. on current hyperlipidemia guidelines (the updated Adult Treatment Panel III [ATP III]) can also reduce the incidence of heart failure by 20%.
Use of hydroxymethylglutaryl coenzyme A (HMG CoA) reductase inhibitors or statin therapy in CAD patients based
Evidence-based disease management strategies for diabetes mellitus, atherosclerotic vascular disease, and thyroid disease, as well as patient avoidance of tobacco, alcohol, cocaine, amphetamines, and other illicit drugs that can be cardiotoxic, are also important components of early risk modification for prevention of heart failure. In diabetic patients, both ACEIs and ARBs (specifically losartan and irbesartan) have been shown to reduce new-onset heart the EUROPA (European Trial on Reduction of Cardiac Events with Perindopril in Stable Coronary Artery Disease) well as reduced mortality, MIs, and cardiac arrest. failure compared with placebo. In CAD or atherosclerotic vascular disease patients without heart failure, reviews of and HOPE (Heart Outcomes Prevention Trial) results show a 23% reduction in heart failure with ACEI therapy as ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group: Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288:2981. [PMID: 12479763] Baker DW: Prevention of heart failure. J Card Fail 2002;8:333. [PMID: 12411985] Brenner BM et al: Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001;345:861. [PMID: 11565518] Fox KM: Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: Randomized, double-blind, placebo-controlled, multicentre trial (the EUROPA study). Lancet 2003;362:782. [PMID: 13678572]
Yusuf S et al: Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 2000;342:145. [PMID: 10639539] Asymptomatic with Cardiac Structural Abnormalities or Remodeling (Stage B)
Patients who do not have clinical symptoms of heart failure but who have a structurally abnormal heart, such as a previous MI, evidence of left ventricular remodeling (left ventricular hypertrophy or low ejection fraction), or valvular disease, are at a substantial risk of developing symptomatic heart failure. Prevention of further condition.
progression in these at-risk patients is the goal, and appropriate therapies are dependent on the patient's cardiac In all patients with a recent or remote history of MI, regardless of ejection fraction, ACEIs and -blockers are the mainstay of therapy. Both therapies have been demonstrated in randomized control trials to cause a significant reduction in cardiovascular death and heart failure. These therapies are vital in post-MI patients, as is evidencebased management of an ST-elevation MI and chronic stable angina, to help further achieve reduction in heart failure morbidity and mortality. In asymptomatic patients who have not had an MI but have a reduced left ventricular ejection fraction
(nonischemic cardiomyopathy), clinical trials reported an overall 37% reduction in heart failure when treated with ACEI therapy. The SOLVD (Studies of Left Ventricular Dysfunction) trial and a 12-year follow-up study confirmed the long-term benefit of ACEIs regarding onset of symptomatic heart failure and mortality. A substudy of the SOLVD trial showed how enalapril attenuates progressive increases in left ventricular dilation and hypertrophy,
thus inhibiting left ventricular remodeling. Despite a lack of evidence from randomized controlled trials, the ACC/AHA guidelines recommend -blockers in patients with stage B heart failure given the significant survival benefit these agents provide in worsening stages of heart failure. The RACE (Ramipril Cardioprotective Evaluation) trial provided a clue to why ACEIs are advantageous over -blockers for nonischemic cardiomyopathy by demonstrating that ramipril is more effective than the -blocker atenolol in reversing left ventricular hypertrophy in hypertensive patients.
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Pgina 9 de 15
There is no clear evidence for use of ARBs in asymptomatic patients with reduced left ventricular ejection fraction; however, ARB therapy is a reasonable alternative in ACEI-intolerant patients. The VALIANT (Valsartan in Acute Myocardial Infarction) trial showed that the ARB valsartan was as effective as but not superior to captopril, an ventricular ejection fraction. The combination of both therapies was no better than captopril alone.
ACEI, in reducing cardiovascular morbidity and mortality in post-MI patients with heart failure or a reduced left Agabiti-Rosei E et al: ACE inhibitor ramipril is more effective than the beta-blocker atenolol in reducing left RACE study group. J Hypertens 1995;13:1325. [PMID: 8984131]
ventricular mass in hypertension. Results of the RACE (ramipril cardioprotective evaluation) study on behalf of the Flather MD et al: Long-term ACE-inhibitor therapy in patients with heart failure or left-ventricular dysfunction: A systematic overview of data from individual patients. ACE-Inhibitor Myocardial Infarction Collaborative Group. Lancet 2000;355:1575. [PMID: 10821360]
Greenberg B et al: Effects of long-term enalapril therapy on cardiac structure and function in patients with left ventricular dysfunction. Results of the SOLVD echocardiography substudy. Circulation 1995;91:2573. [PMID: 7743619] Maggioni AP, Fabbri G: VALIANT (VALsartan In Acute myocardial iNfarcTion) trial. Expert Opin Pharmacother 2005;6:507. [PMID: 15794740] Symptomatic Systolic Heart Failure (Stage C)
Patients with a clinical diagnosis of heart failure have current or prior symptoms of heart failure and comprise
ACC/AHA stage C. This stage encompasses NYHA classes II, III, and IV, excluding patients who develop refractory end-stage heart failure (see Table 192). In symptomatic patients with heart failure, neurohormonal activation creates deleterious effects on the heart, leading to pulmonary and peripheral edema, persistent increased
afterload, pathologic cardiac remodeling, and a progressive decline in cardiac function. The overall goals in this the patient's long-term morbidity and mortality.
stage are to improve the patient's symptoms, slow or reverse the deterioration of cardiac functioning, and reduce Accurate assessment of the cause and severity of heart failure, the incorporation of previous stage A and B
treatment recommendations, and correction of any cardiovascular, systemic, and behavioral factors (Table 195) are important to achieve control in patients with symptomatic heart failure. Moderate dietary sodium restriction (34 g daily) with daily weight measurement further enhance volume control and allow for lower and safer doses of diuretic therapies. Exercise training is beneficial and should be encouraged to prevent physical deconditioning, which can contribute to exercise intolerance in patients with heart failure.
Table 195. Factors Contributing to Worsening Heart Failure.
Cardiovascular Factors Superimposed ischemia or infarction Uncontrolled hypertension Unrecognized primary valvular disease Worsening secondary mitral regurgitation New-onset or uncontrolled atrial fibrillation Excessive tachycardia Pulmonary embolism Systemic Factors Inappropriate medications Superimposed infection Anemia Uncontrolled diabetes mellitus Thyroid dysfunction Electrolyte disorders Pregnancy
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Patient-related Factors Medication noncompliance Dietary indiscretion Alcohol consumption Substance abuse
Pgina 10 de 15
Adapted, with permission, from Colucci WS: Overview of the therapy of heart failure due to systolic dysfunction. In Rose BD, ed: UpToDate Version 13.3. UpToDate, 2005. Patients with symptomatic heart failure should be routinely managed with a standard therapy of a diuretic, an ACEI (or ARB if intolerant), and a -blocker (see Table 192). The addition of other pharmacologic therapies should be guided by the need for further symptom control versus the desire to enhance survival and long-term prognosis. A stepwise approach to therapy is presented in Table 196 and expanded upon below.
Table 196. Pharmacologic Steps in Symptomatic Heart Failure.1
Pharmacotherapy Standard Therapy Loop diuretic Angiotensin-converting enzyme inhibitor (ACEI) -Blocker Titrate accordingly for fluid control and symptom relief (dyspnea, edema) Initiate at low dose, titrating to target, during or after optimization of diuretic therapy for survival benefit2 Initiate at low dose once stable on ADEI (or ARB) for survival benefit May initiate before achieving ACEI (or ARB) target doses and should be titrated to target doses unless symptoms become limiting Indications and Considerations
Additional Therapies3 Angiotensin II receptor blocker (ARB) Aldosterone antagonist Digoxin Hydralazine plus isosorbide dinitrate NYHA, New York Heart Association.
1 2 3
Used in ACEI-intolerant patients, as above, for survival benefit May be effective for persistent symptoms and survival (NYHA class IIIV) For worsening symptoms and survival in moderately severe to severe heart failure (NYHA class III with decompensations) For persistent symptoms and to reduce hospitalizations Should be maintained at preferred serum digoxin concentration Effective for persistent symptoms and survival, particularly in blacks
Assessment of clinical response and tolerability should guide decision making and allow for variations. ARBs are recommended in patients who are intolerant to ACEIs.
Decisions about whether or not to use additional therapy are guided by the need for symptom control versus mortality benefit.
Sources: Overview of the therapy of heart failure due to systolic dysfunction. In Rose BD, ed: UpToDate Version 13.3. UpToDate, 2005; Hunt SA et al: ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult. Circulation 2005;112:e154. DIURETICS
Patients with heart failure who present with common congestive symptoms (pulmonary and peripheral edema) are given a diuretic to manage fluid retention and achieve and maintain a euvolemic state. Diuretic therapy is activation of the renin-angiotensin-aldosterone system. specifically aimed at treating the compensatory volume expansion driven by renal tubular sodium retention and Loop diuretics are the treatment of choice because they increase sodium excretion 2025% and substantially enhance free water clearance. Furosemide is most commonly used, but patients may respond better to bumetanide or torsemide because of superior, more predictable absorptions and longer durations of action. To
minimize the risk of over- and underdiuresis, the diuretic response should guide the dosage of loop diuretics (Table
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
maintain active diuresis and sustained volume and weight control.
Pgina 11 de 15
197), with dose increases until a response is achieved. Frequency of dosing is guided by the time needed to
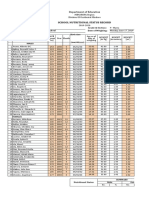
Table 197. Medications Used in the Treatment of Symptomatic Heart Failure in Patients with Reduced Left Ventricular Ejection Fraction.
Drug Therapy Loop Diuretics Bumetanide Furosemide Torsemide ACE Inhibitors Captopril Enalapril Fosinopril Lisinopril Perindopril Quinapril Ramipril Trandolapril Angiotensin II Receptor Blockers Candesartan Losartan Valsartan -Blockers Bisoprolol Carvedilol Metoprolol succinate, extended release (CR/XL) Aldosterone Antagonists Eplerenone Spironolactone Other Medication Digoxin Hydralazine plus isosorbide dinitrate 0.1250.25 mg once daily Serum concentration 0.51.1 ng/mL 37.5 mg/20 mg three times daily 75 mg/40 mg three times daily 25 mg once daily 12.525 mg once daily 50 mg once daily 25 mg once or twice daily 1.25 mg once daily 3.125 mg twice daily 12.525 mg once daily 10 mg once daily 25 mg twice daily (50 mg twice daily, if > 85 kg [187 lb]) 200 mg once daily 100 mg once daily 48 mg once daily 2550 mg once daily 2040 mg twice daily 32 mg once daily 50100 mg once daily 160 mg twice daily 6.25 mg three times daily 50100 mg three times daily 2.5 mg twice daily 510 mg once daily 2.55 mg once daily 2 mg once daily 5 mg twice daily 1.252.5 mg once daily 1 mg once daily 1020 mg twice daily 2040 mg once daily 2040 mg once daily 816 mg once daily 20 mg twice daily 5 mg twice daily 4 mg once daily 1.0 mg/dose 40 mg/dose 10 mg/dose 48 mg/dose 160200 mg/dose 100200 mg/dose Initial Daily Dose Target or Maximum Daily Dose
Metoprolol tartrate, immediate release 12.525 mg once daily
Source: ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult. Circulation 2005;112:e154. Thiazide diuretics also have a role in heart failure, principally as antihypertensive therapy, but they can be used in increase sodium excretion only 510% and tend to decrease free water clearance overall.
combination with loop diuretics to provide a potentiated or synergistic diuresis. As a lone treatment, however, they Symptom improvement with diuretics occurs within hours to days as compared with weeks to months for other
heart failure therapies. For long-term clinical stability, diuretics are not sufficient and exacerbations can be greatly reduced when they are combined with ACEI and -blocker therapies.
ACE INHIBITORS
ACEIs are prescribed to all patients with symptomatic heart failure unless contraindicated and have proven benefit
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Pgina 12 de 15
in alleviating heart failure symptoms, reducing hospitalization, and improving survival. Current ACC/AHA
guidelines recommend that all patients with left ventricular dysfunction be started on low-dose ACEI therapy to avoid side effects and raised to a maintenance or target dose (see Table 197). There is, however, some uncertainty regarding target doses achieved in clinical trials, and whether these are more beneficial than lower doses. For ACEIs as a class, there does not appear to be any difference in agents in terms of effectiveness at improving heart failure outcomes.
-BLOCKERS
In patients with NYHA class II or III heart failure, the -blockers bisoprolol, metoprolol succinate (sustained release), and carvedilol have been shown to improve mortality and event-free survival. These benefits are in
addition to ACEI therapy and support the use of -blockers as part of standard therapy in these patients. A similar survival benefit has been shown for patients with stable NYHA class IV heart failure. -Blocker therapy should be initiated near the onset of a diagnosis of left ventricular dysfunction and mild heart failure symptoms, given the added benefit on survival and disease progression. Titrating ACEI therapy to a target dose should not preclude the initiation of -blocker therapy. Starting doses should be very low (see Table 197) but doubled at regular intervals, every 23 weeks as tolerated, to achieve target doses. There is no proven value to achieving a specific resting heart rate, but low doses are beneficial and there appears to be a dose-dependent improvement.
Traditionally the negative inotropic effects of -blockers were thought to be harmful in heart failure, but this impact is outweighed by the beneficial effect of inhibiting sympathetic nervous system activation. Current evidence -blockers. The COMET (Carvedilol or Metoprolol European Trial) findings showed that carvedilol (an 1-, 1-, and 2-receptor inhibitor) is more effective than twice-daily dosed immediate-release metoprolol tartrate (a highly specific inhibitor) in reducing heart failure mortality (40% vs 34%, respectively). Previous trials had investigated even with metoprolol tartrate, a very cost-effective alternative.
1-receptor
metoprolol succinate (sustained-release, once-daily dosing), but the COMET trial showed a mortality reduction Because -blockers may cause a 4- to 10-week increase in symptoms before improvement is noted, therapy should be initiated when patients have no or minimal evidence of fluid retention. Relative contraindications include bradycardia, hypotension, hypoperfusion, severe peripheral vascular disease, a P-R interval greater than 0.24 seconds, second- or third-degree atrioventricular block, severe COPD, or a history of asthma. Race or gender differences in efficacy of -blocker therapy have not been noted.
ANGIOTENSIN II RECEPTOR BLOCKERS
ARBs have been shown in clinical trials to be nearly as effective as, but not superior to, ACEIs as first-line therapy
for symptomatic heart failure. ARBs should be utilized in ACEI-intolerant patients but not preferentially over ACEIs
given the volume of evidence validating ACEIs. Despite unclear evidence, the ACC/AHA guidelines recommend that heart failure.
ARB therapy be considered in addition to ACEI and standard therapy for patients who have persistent symptoms of
ALDOSTERONE ANTAGONISTS
For selected patients with moderately severe to severe symptoms who are difficult to control (NYHA class III with
decompensations or class IV), additional treatment options include the aldosterone antagonists spironolactone and to moderate heart failure.
eplerenone (see Table 197). There is no clear evidence to support the use of these therapies in patients with mild The addition of aldosterone antagonist therapy can cause life-threatening hyperkalemia in patients with heart failure, who are often already at risk because of reduced left ventricular function and associated renal insufficiency. Current guidelines recommend careful monitoring to ensure that creatinine is less than 2.5 mg/dL in men or less than 2.0 mg/dL in women and that potassium is maintained below 5.0 mEq/L (levels > 5.5 mEq/L should trigger discontinuation or dose reduction). Higher doses of aldosterone antagonists and ACEI therapy should also raise concern for possible hyperkalemia, and the use of nonsteroidal anti-inflammatory drugs
(NSAIDs), cyclooxygenase-2 (COX-2) inhibitors, and potassium supplements should be avoided if possible. If the clinical situation does not allow for proper monitoring, the risk of hyperkalemia may outweigh the benefit of aldosterone antagonist therapy.
DIGOXIN
Digoxin therapy is only indicated to reduce hospitalizations in patients with uncontrolled symptomatic heart failure or as a ventricular rate control agent if a patient has a known arrhythmia. The DIG (Digitalis Investigation Group)
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Pgina 13 de 15
trial proved the benefit of digoxin added to diuretic and ACEI therapy in improving heart failure symptom control and decreasing the rate of hospitalization by 6%, but there was no overall mortality benefit. Subsequent retrospective subgroup analysis of the trial discovered some survival improvement at a serum digoxin
concentration of 0.50.8 ng/mL in men. A similar but nonsignificant survival trend was also noted in women.
Because survival is clearly worse when the serum digoxin concentration is greater than 1.2 ng/mL, patients are best managed within the range noted to avoid potential adverse outcomes given the narrow risk/benefit ratio. drug levels. Digoxin should be used cautiously in elderly patients, who may have impaired renal function that adversely affects
HYDRALAZINE AND NITRATES
The combination of hydralazine and isosorbide dinitrate (H-I) is a reasonable treatment in patients, particularly Trial), the mortality of black patients receiving H-I combination therapy was reduced, but mortality of white
blacks, who have persistent heart failure symptoms with standard therapy. In V-HeFT I (Vasodilator Heart-Failure patients was not different than that of the placebo group. In V-HeFT II, a reduction in mortality with the H-I was found in either trial.
combination was seen only in white patients who had been receiving enalapril therapy. No effect on hospitalization The A-HeFT (African-American Heart Failure Trial) findings further supported the benefit of a fixed dose H-I
combination (see Table 197) by showing a reduction in mortality and heart failure hospitalization rates as well as improved quality of life scores in patients with moderate to severe heart failure (NYHA class III or IV) who selfidentified as black. The H-I combination was in addition to standard therapies that included ACEIs or ARBs, blockers, and spironolactone.
ANTICOAGULATION
It is well established that patients with heart failure are at an increased risk of thrombosis from blood stasis in
dilated hypokinetic cardiac chambers and peripheral blood vessels. Despite this known risk the yearly incidence of thromboembolic events in patients with stable heart failure is between 1% and 3%, even in those with lower left ventricular ejection fractions and evidence of intracardiac thrombi. Such low rates limit the detectable benefit of given the major risk of bleeding. Warfarin therapy is only indicated in heart failure patients with a history of a thromboembolic event or those with paroxysmal or chronic atrial fibrillation or flutter. Likewise, the benefit of antiplatelet therapies, such as aspirin, has not been clearly proven, and these therapies could possibly be increase hospitalizations from heart failure decompensation.
ADVERSE THERAPIES
warfarin therapy, and retrospective data analysis of warfarin with heart failure show conflicting results, especially
detrimental because of their known interaction with ACEIs. Aspirin can decrease ACEI effectiveness and potentially
Therapies that adversely affect the clinical status of patients with symptomatic heart failure should be avoided. failure. Nondihydropyridine calcium channel blockers (eg, diltiazem and verapamil) and older, short-acting
Other than for control of hypertension, calcium channel blockers offer no morbidity or mortality benefit in heart dihydropyridines (eg, nicardipine and nisoldipine) can worsen symptoms of heart failure, especially in patients with moderate to severe heart failure. The newer long-acting dihydropyridine calcium channel blockers amlodipine and felodipine appear to be safe when used in the treatment of hypertension but do not improve heart failure outcomes. NSAIDs can also exacerbate heart failure through peripheral vasoconstriction and by interfering with the renal effects of diuretics and the unloading effects of ACEIs. Most antiarrhythmic drugs (except amiodarone and dofetilide) have an adverse impact on heart failure and survival because of their negative inotropic activity
and proarrhythmic effects. Phosphodiesterase inhibitors (cilostazol, sildenafil, vardenafil, and tadalafil) can cause hypotension and are potentially hazardous in patients with heart failure. Thiazolidinediones and metformin, both used in treatment of diabetes, can be detrimental in patients with heart failure because they increase the risk of excessive fluid retention and lactic acidosis, respectively.
IMPLANTABLE DEVICES
Nearly one third of all heart failure deaths occur as a result of sudden cardiac death. The ACC/AHA
recommendations include use of implantable cardioverter-defibrillators (ICDs) for secondary prevention of sudden cardiac death in patients with symptomatic heart failure, a reduced left ventricular ejection fraction, and a history of cardiac arrest, ventricular fibrillation, or hemodynamically destabilizing ventricular tachycardia. ICDs are and a reasonable 1-year survival with no recent MI (within 40 days).
recommended for patients with NYHA class II or III heart failure, a left ventricular ejection fraction less than 35%, As heart failure progresses, ventricular dyssynchrony can also occur. This is defined by a QRS duration greater
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Pgina 14 de 15
than 0.12 msec in patients with a low left ventricular ejection fraction (usually < 35%) and NYHA class III or IV heart failure. Clinical trials have shown that cardiac resynchronization therapy with biventricular pacing can improve quality of life, functional class, exercise capacity, exercise distance, left ventricular ejection fraction, and receive a combined device, unless contraindicated. 2001;134:550. [PMID: 11281737]
survival in these patients. Patients who meet criteria for cardiac resynchronization therapy and an ICD and should Brophy JM et al: Beta-blockers in congestive heart failure. A Bayesian meta-analysis. Ann Intern Med de Vries RJ et al: Efficacy and safety of calcium channel blockers in heart failure: Focus on recent trials with second-generation dihydropyridines. Am Heart J 2000;139(2 Pt 1):185. [PMID: 10650289] the experience in the MERIT-HF study. J Am Coll Cardiol 2001;38:932. [PMID: 11583861] Cardiol 2002;39:463. [PMID: 11823085] Goldstein S et al: Metoprolol controlled release/extended release in patients with severe heart failure: Analysis of
Jong P et al: Angiotensin receptor blockers in heart failure: Meta-analysis of randomized controlled trials. J Am Coll
Jong P et al: Effect of enalapril on 12-year survival and life expectancy in patients with left ventricular systolic dysfunction: A follow-up study. Lancet 2003;361:1843. [PMID: 12788569] 2003;289:1652. [PMID: 12672733] Juurlink DN et al: Drug-drug interactions among elderly patients hospitalized for drug toxicity. JAMA McMurray JJ et al: Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting-enzyme inhibitors: the CHARM-Added trial. Lancet 2003;362:767. [PMID: 13678869] Pitt B et al: The EPHESUS trial: Eplerenone in patients with heart failure due to systolic dysfunction complicating 2001;15:79. [PMID: 11504167]
acute myocardial infarction. Eplerenone Post-AMI Heart Failure Efficacy and Survival Study. Cardiovasc Drugs Ther Poole-Wilson PA et al: Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): Randomised controlled trial. Lancet 2003;362:7. [PMID: 12853193] Rochon PA et al: Use of angiotensin-converting enzyme inhibitor therapy and dose-related outcomes in older adults with new heart failure in the community. J Gen Intern Med 2004;19:676. [PMID: 15209607] 2004;351:2049. [PMID: 15533851] Taylor AL et al: Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med Refractory End-Stage Heart Failure (Stage D)
Despite optimal medical therapy some patients deteriorate or do not improve and experience symptoms at rest
(NYHA class IV). These patients can have rapid recurrence of symptoms, leading to frequent hospitalizations and a significant or permanent reduction in their activities of daily living. Before classifying patients as being refractory or having end-stage heart failure, providers should verify an accurate diagnosis, identify and treat contributing conditions that could be hindering improvement, and maximize medical therapy. Control of fluid retention to improve symptoms is paramount in this stage, and referral to a program with
expertise in refractory heart failure or referral for cardiac transplantation should be considered. Other specialized treatment strategies, such as mechanical circulatory support, continuous intravenous positive inotropic therapy, and other surgical management can be considered, but there is limited evidence in terms of morbidity and mortality to support the value of these therapies. Careful discussion of the prognosis and options for end-of-life care should also be initiated with patients and their families. In this scenario, patients with ICDs should receive information about the option to inactivate defibrillation. DIASTOLIC HEART FAILURE
Clinically, diastolic heart failure is as prevalent as LVSD, and the presentation of clinically evident diastolic heart failure is indistinguishable from clinically apparent LVSD. Elderly women, usually with a heavy prevalence of hypertension and diabetes mellitus, appear to be most at risk. When considering the diagnosis of diastolic heart
failure, conditions that mimic heart failureincluding obesity, lung disease, poorly controlled atrial fibrillation, and
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Print: Chapter 19. Heart Failure
Pgina 15 de 15
occult coronary ischemiahave to be ruled out. Management focuses on controlling systolic and diastolic blood to exert effects on ventricular relaxation. Diuretics are used to control symptoms of pulmonary congestion and preload, manifesting as worsening heart failure.
pressure, ventricular rate, and volume status, and reducing myocardial ischemia, because these entities are known peripheral edema, but care must be taken to avoid overdiuresis, which can cause decreased volume status and Dosh SA: Diagnosis of heart failure in adults. Am Fam Physician 2004;70:2145. [PMID: 15606063]
Prognosis
Despite favorable trends in survival and advances in treatment of heart failure and associated comorbidities, 50% of patients die within 5 years of diagnosis. Mortality increases in patients both with and without CHF as systolic function declines. Even patients with diastolic heart failure have significantly higher mortality rates compared with
Web Sites
persons who have normal left ventricular systolic function and no CHF.
American College of Cardiology clinical guidelines: http://www.acc.org/qualityandscience/clinical/statements.htm American Heart Association (AHA): http://www.americanheart.org AHA heart disease and stroke statistics update: http://www.americanheart.org/presenter.jhtml?identifier= 3036355 AHA patient information: http://www.americanheart.org/presenter.jhtml?identifier=1486
Copyright 2007 The McGraw-Hill Companies. All rights reserved.
Privacy Notice. Any use is subject to the Terms of Use and Notice. Additional Credits and Copyright Information.
mk:@MSITStore:C:\Users\ANDRE\Documents\MED\MEDICAL_LIBRARY\FAMILY_MEDICI...
11/07/2013
Das könnte Ihnen auch gefallen
- TG1652A User Guide - STANDARD - 1.3 - Similar - DeviceDokument44 SeitenTG1652A User Guide - STANDARD - 1.3 - Similar - DeviceniklukNoch keine Bewertungen
- Acupuncture Anatomical AproachDokument232 SeitenAcupuncture Anatomical AproachRicardo TeixeiraNoch keine Bewertungen
- Manual-1812 ARRIS PDFDokument55 SeitenManual-1812 ARRIS PDFniklukNoch keine Bewertungen
- NHC Healthcare Systems - FolliculitisDokument10 SeitenNHC Healthcare Systems - FolliculitisniklukNoch keine Bewertungen
- Acupuncture, Trigger Points & Musculoskeletal PainDokument362 SeitenAcupuncture, Trigger Points & Musculoskeletal PainThezza Lion100% (1)
- Revisão Crítica Da Acupuntura MédicaDokument9 SeitenRevisão Crítica Da Acupuntura MédicaniklukNoch keine Bewertungen
- Topical Antibiotics Appropriate Skin InfectionsDokument4 SeitenTopical Antibiotics Appropriate Skin InfectionsniklukNoch keine Bewertungen
- Bacterial Skin and Soft Tissue InfectionsDokument5 SeitenBacterial Skin and Soft Tissue InfectionsFarid Gusranda100% (2)
- Biliary Microlithiasis, Sludge, Crystals, MicrocrystallizationDokument6 SeitenBiliary Microlithiasis, Sludge, Crystals, MicrocrystallizationniklukNoch keine Bewertungen
- HICCUPS - Clinical Sign of VolvulusDokument4 SeitenHICCUPS - Clinical Sign of VolvulusniklukNoch keine Bewertungen
- GUIDELINES FOR MICROSCOPIC HEMATURIADokument4 SeitenGUIDELINES FOR MICROSCOPIC HEMATURIAArian SuryaNoch keine Bewertungen
- Cook Medical Device To Prevent Leg AmputationsDokument2 SeitenCook Medical Device To Prevent Leg AmputationsniklukNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Cell Membrane Anatomy and FunctionsDokument20 SeitenCell Membrane Anatomy and FunctionsSarahNoch keine Bewertungen
- Importance of Healthy EatingDokument4 SeitenImportance of Healthy Eatingandreeagabriela28Noch keine Bewertungen
- 2018 - 2019 Nutritional Status 9-NarraDokument4 Seiten2018 - 2019 Nutritional Status 9-Narraariane may malicseNoch keine Bewertungen
- Sistem Pencernaan (Digestion System)Dokument28 SeitenSistem Pencernaan (Digestion System)PaRaDoX eLaKSaMaNaNoch keine Bewertungen
- Community Needs AssessmentDokument7 SeitenCommunity Needs Assessmentapi-287639257Noch keine Bewertungen
- METs and MeDokument2 SeitenMETs and MePraveen JujjavarapuNoch keine Bewertungen
- DyslipidemiaDokument50 SeitenDyslipidemiaTitin Tria UtamiNoch keine Bewertungen
- The Control of Partitioning Between Protein and FaDokument19 SeitenThe Control of Partitioning Between Protein and FaChoi Joon-HyunNoch keine Bewertungen
- Microencapsulated Lipid Powder SolutionDokument20 SeitenMicroencapsulated Lipid Powder SolutionManuel RodrìguezNoch keine Bewertungen
- Foaming Capacity of Soaps Investigatory Projects Chemistry Class 12 CbseDokument17 SeitenFoaming Capacity of Soaps Investigatory Projects Chemistry Class 12 CbseChandan Kumar SharmaNoch keine Bewertungen
- Ben Johnson's Weight Training Program by Coach Charlie FrancisDokument7 SeitenBen Johnson's Weight Training Program by Coach Charlie Francismichal900_40834675350% (2)
- Nutrition Essentials For Nursing Practice Dudek 7th Edition Test BankDokument15 SeitenNutrition Essentials For Nursing Practice Dudek 7th Edition Test BankScarlett Bryant100% (32)
- Essential workout guideDokument31 SeitenEssential workout guidejo nemesisNoch keine Bewertungen
- Deurenberg Formula Imc para %grasaDokument10 SeitenDeurenberg Formula Imc para %grasaAna Cecilia VegaNoch keine Bewertungen
- Understanding Coronary Artery Disease: Causes, Symptoms and Treatments /TITLEDokument122 SeitenUnderstanding Coronary Artery Disease: Causes, Symptoms and Treatments /TITLEShannie PadillaNoch keine Bewertungen
- Meredith Shirk, CPT, WLS, BCS, FNSDokument27 SeitenMeredith Shirk, CPT, WLS, BCS, FNSfisieresalvate100% (22)
- Careplan Medication ListDokument17 SeitenCareplan Medication ListGiorgia ScorsoneNoch keine Bewertungen
- CHN Prioritization of Health ProblemsDokument16 SeitenCHN Prioritization of Health ProblemsANNIE SHINE MAGSACAYNoch keine Bewertungen
- Screening Nutrition Care ProcessDokument70 SeitenScreening Nutrition Care ProcessSiwonniekyubum DijaNoch keine Bewertungen
- Carbohydrates Explained: Classification, Structures and FunctionsDokument41 SeitenCarbohydrates Explained: Classification, Structures and FunctionsHastuti RahmasariiNoch keine Bewertungen
- Blood Glucose-Insulin Administration-Study GuideDokument8 SeitenBlood Glucose-Insulin Administration-Study GuideChandra MuraliNoch keine Bewertungen
- Metabolism of Carbohydrates, Lipids, Amino Acids and its Regulation Test QuestionsDokument209 SeitenMetabolism of Carbohydrates, Lipids, Amino Acids and its Regulation Test Questionsninas1112Noch keine Bewertungen
- 1.facies R Flores B N PDFDokument16 Seiten1.facies R Flores B N PDFDenys PQNoch keine Bewertungen
- National School Food Policies: Mapping of Across The EU28 Plus Norway and SwitzerlandDokument46 SeitenNational School Food Policies: Mapping of Across The EU28 Plus Norway and SwitzerlandLindsey FletcherNoch keine Bewertungen
- Be Fruitful: The Essential Guide To Maximizing Fertility and Giving Birth To A Healthy ChildDokument29 SeitenBe Fruitful: The Essential Guide To Maximizing Fertility and Giving Birth To A Healthy ChildSimon and Schuster0% (1)
- Choose My Plate ProjectDokument3 SeitenChoose My Plate Projectapi-309612338Noch keine Bewertungen
- Partus & LactationDokument27 SeitenPartus & LactationfrankyNoch keine Bewertungen
- Anorexia NervosaDokument18 SeitenAnorexia NervosaJosephine Valdez HanrathNoch keine Bewertungen
- In Brief: Inguinal HerniaDokument4 SeitenIn Brief: Inguinal HerniaSaf DicamNoch keine Bewertungen