Beruflich Dokumente
Kultur Dokumente
Case Study
Hochgeladen von
Mikko Anthony Pingol AlarconCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Case Study
Hochgeladen von
Mikko Anthony Pingol AlarconCopyright:
Verfügbare Formate
Alarcon, Mikko Anthony P BSN406
Case Study: Carpal Tunnel Syndrome
I. Clinical Overview
Carpal tunnel syndrome is a progressively painful hand and arm condition caused by a pinched nerve in your wrist. A number of factors can contribute to carpal tunnel syndrome, including the anatomy of your wrist, certain underlying health problems and possibly patterns of hand use. Bound by bones and ligaments, the carpal tunnel is a narrow passageway about as big around as your thumb located on the palm side of your wrist. This tunnel protects a main nerve to your hand and nine tendons that bend your fingers. Compression of the nerve produces the numbness, pain and, eventually, hand weakness that characterize carpal tunnel syndrome. Fortunately, for most people who develop carpal tunnel syndrome, proper treatment usually can relieve the pain and numbness and restore normal use of their wrists and hands.
II. Risk Factors a) Anatomic Factors - a wrist fracture or dislocation that alters the space within the carpal tunnel that can create extraneous pressure on the median nerve. b) Nerve damaging conditions - diabetes can increase risk of nerve damage. c) Inflammatory conditions - rheumatoid can affect tendons in your wrists, exerting pressure on your median nerve. d) Alterations in the balance of body fluids - fluid retention may increase the pressure within the carpal tunnel, irritating the median nerve. e) Workplace factors - extensive computer use. Working with vibrating tools or an assembly line that requires prolonged or repetitive flexing of the wrist may create harmful pressure on the median nerve. III. Clinical Manifestations
Tingling or numbness in your fingers or hand, especially your thumb and index, middle or ring fingers, but not your little finger. This sensation often occurs while holding a steering wheel, phone or newspaper or upon awakening. Many people "shake out" their hands to try to relieve their symptoms. As the disorder progresses, the numb feeling may become constant. b. Pain radiating or extending from your wrist up your arm to your shoulder or down into your palm or fingers, especially after forceful or repetitive use. This usually occurs on the palm side of your forearm. c. A sense of weakness in your hands and a tendency to drop objects.
a.
IV. Diagnosis
a.
b.
c. d.
e.
History of symptoms. The pattern of your signs and symptoms may offer clues to their cause. For example, since the median nerve doesn't provide sensation to your little finger, symptoms in that finger may indicate a problem other than carpal tunnel syndrome. Another clue is the timing of the symptoms. Typical times when you might experience symptoms due to carpal tunnel syndrome include while holding a phone or a newspaper, gripping a steering wheel, or waking up during the night. Physical exam. Your doctor will want to test the feeling in your fingers and the strength of the muscles in your hand, because these can be affected by carpal tunnel syndrome. Pressure on the median nerve at the wrist, produced by bending the wrist, tapping on the nerve or simply pressing on the nerve, can bring on the symptoms in many people. X-ray. Some doctors may recommend an X-ray of the affected wrist to exclude other causes of wrist pain, such as arthritis or a fracture. Electromyogram. Electromyography measures the tiny electrical discharges produced in muscles. A thin-needle electrode is inserted into the muscles your doctor wants to study. An instrument records the electrical activity in your muscle at rest and as you contract the muscle. This test can help determine if muscle damage has occurred. Nerve conduction study. In a variation of electromyography, two electrodes are taped to your skin. A small shock is passed through the median nerve to see if electrical impulses are slowed in the carpal tunnel.
V. Nursing management
Monitor level of pain, numbness, paresthesia, and functioning. Monitor for adverse effects of NSAID therapy, especially in elderly. GI distress or bleeding, dizziness, or increased serum creatinine. After surgery, monitor neurovascular status of affected extremity: pulses, color, swelling, movement, sensation, or warmth. Apply wrist splint so wrist is in neutral position, with slight extension of wrist and slight abduction of thumb; make sure that it fits correctly without constriction. Administer NSAIDs and assist with tendon sheath injections as required. Apply ice or cold compress to relieve inflammation and pain. Teach patient the cause of condition and ways to alter activity to prevent flexion of wrists; refer to an occupational therapist as indicated. Advise patient of NSAID therapy dosage schedule and potential adverse effects; instruct patient to report GI pain and bleeding. Teach patient to gentle range-of-motion exercises; refer to a physical therapist as indicated.
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- EFT For Extreme Anxiety and DissociationDokument66 SeitenEFT For Extreme Anxiety and Dissociationolga100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Raminder Nirula - High-Yield Internal Medicine (High-Yield Series) - Lippincott Williams and Wilkins (2006)Dokument228 SeitenRaminder Nirula - High-Yield Internal Medicine (High-Yield Series) - Lippincott Williams and Wilkins (2006)Isah Mohammed100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Understanding & Practices of Weight ManagementDokument445 SeitenUnderstanding & Practices of Weight ManagementOnlineGatha The Endless TaleNoch keine Bewertungen
- Sample Questions For HAAD Prometric and DHA For Nurses PDFDokument23 SeitenSample Questions For HAAD Prometric and DHA For Nurses PDFAasmeetaa Thapa100% (2)
- Widal TestDokument8 SeitenWidal TestSanam BangashNoch keine Bewertungen
- Parathyroid DisordersDokument19 SeitenParathyroid DisordersmatrixtrinityNoch keine Bewertungen
- Combank NotesDokument7 SeitenCombank NotesVee MendNoch keine Bewertungen
- Pharma Long Quiz - KeyDokument3 SeitenPharma Long Quiz - KeyMikko Anthony Pingol AlarconNoch keine Bewertungen
- Health Teaching Plan 1Dokument5 SeitenHealth Teaching Plan 1Mikko Anthony Pingol AlarconNoch keine Bewertungen
- PneumoniaDokument102 SeitenPneumoniaJay Kumar100% (1)
- Case in DutyDokument1 SeiteCase in DutyMikko Anthony Pingol AlarconNoch keine Bewertungen
- Reflection Paper (A Vow To Cherish)Dokument1 SeiteReflection Paper (A Vow To Cherish)Mikko Anthony Pingol AlarconNoch keine Bewertungen
- Reflection-A Vow To CherishDokument2 SeitenReflection-A Vow To CherishMikko Anthony Pingol Alarcon0% (1)
- Date Time Client's Printed Name With Signature Clinical InstructorDokument1 SeiteDate Time Client's Printed Name With Signature Clinical InstructorMikko Anthony Pingol AlarconNoch keine Bewertungen
- Hyperthermia NCPDokument1 SeiteHyperthermia NCPMikko Anthony Pingol AlarconNoch keine Bewertungen
- Ncp3rdrot DocxsDokument4 SeitenNcp3rdrot DocxsMikko Anthony Pingol AlarconNoch keine Bewertungen
- Page 18Dokument1 SeitePage 18Mikko Anthony Pingol AlarconNoch keine Bewertungen
- NPI Feb2,7 And8Dokument14 SeitenNPI Feb2,7 And8Mikko Anthony Pingol AlarconNoch keine Bewertungen
- MSE Ko PoDokument2 SeitenMSE Ko PoMikko Anthony Pingol AlarconNoch keine Bewertungen
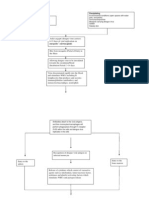
- Schematic Diagram: Precipitating PredisposingDokument4 SeitenSchematic Diagram: Precipitating PredisposingMikko Anthony Pingol AlarconNoch keine Bewertungen
- VI. Laboratory Results Date Laboratory Procedure Component Normal Finding Actual Findings Interpretation and Analysis 04/18/2013Dokument3 SeitenVI. Laboratory Results Date Laboratory Procedure Component Normal Finding Actual Findings Interpretation and Analysis 04/18/2013Mikko Anthony Pingol AlarconNoch keine Bewertungen
- Case StudyDokument27 SeitenCase StudyMikko Anthony Pingol AlarconNoch keine Bewertungen
- Cowden S Disease A Rare Cause of Oral Sis 2002 Journal of Laryngology and OtologyDokument3 SeitenCowden S Disease A Rare Cause of Oral Sis 2002 Journal of Laryngology and Otologydasea01Noch keine Bewertungen
- Parasitology International: ReviewDokument7 SeitenParasitology International: ReviewAhmad PradhanaNoch keine Bewertungen
- Translate TineaDokument12 SeitenTranslate TineaIndah Permata SariNoch keine Bewertungen
- Modal & Phrasal VerbsDokument5 SeitenModal & Phrasal VerbsPaf VenancioNoch keine Bewertungen
- HMIS 105 Health Unit Outpatient Monthly ReportDokument32 SeitenHMIS 105 Health Unit Outpatient Monthly ReportOdetteNoch keine Bewertungen
- Descriptive Research Regarding The COVID-19Dokument5 SeitenDescriptive Research Regarding The COVID-19Mish Lei FranxhNoch keine Bewertungen
- Endocrine Problems of The Adult ClientDokument18 SeitenEndocrine Problems of The Adult ClientMarylle AntonioNoch keine Bewertungen
- CH 14 Antepartum Nursing Assessment NotesDokument8 SeitenCH 14 Antepartum Nursing Assessment NotesMary LowryNoch keine Bewertungen
- Larsen, J.K. (2017)Dokument8 SeitenLarsen, J.K. (2017)Ale ValenciaNoch keine Bewertungen
- Healing For All (Raymond T. Richey (Richey, Raymond T.) ) (Z-Library)Dokument3 SeitenHealing For All (Raymond T. Richey (Richey, Raymond T.) ) (Z-Library)Delcide Teixeira100% (1)
- Intensive Care Unit Acquired WeaknessDokument35 SeitenIntensive Care Unit Acquired WeaknessEviNoch keine Bewertungen
- MAKING SENSE OF PSYCHIATRY: Our Impenetrable Personal ComputerDokument16 SeitenMAKING SENSE OF PSYCHIATRY: Our Impenetrable Personal ComputerPaul Minot MDNoch keine Bewertungen
- 5 6323480972671058006Dokument195 Seiten5 6323480972671058006Anonymous QOCn5dNoch keine Bewertungen
- Single Squamous EpitheliumDokument28 SeitenSingle Squamous EpitheliumLyndonn Santos100% (1)
- Sarcoidosis Pathophysiology, Diagnosis AtfDokument6 SeitenSarcoidosis Pathophysiology, Diagnosis AtfpatriciaNoch keine Bewertungen
- Urinary Infections in The ElderlyDokument29 SeitenUrinary Infections in The ElderlyChris FrenchNoch keine Bewertungen
- Understanding AuriculotherapyDokument4 SeitenUnderstanding AuriculotherapyFelipe de Jesus HernandezNoch keine Bewertungen
- Cherry Eye: Prolapse of Third Eyelid Gland in Dog-A Case ReportDokument4 SeitenCherry Eye: Prolapse of Third Eyelid Gland in Dog-A Case ReportRocioNoch keine Bewertungen
- Cerebral Palsy An Overview 2018Dokument11 SeitenCerebral Palsy An Overview 2018Yhuliana AcostaNoch keine Bewertungen
- Flu Vaccine: Information For People at RiskDokument8 SeitenFlu Vaccine: Information For People at Riskkovi mNoch keine Bewertungen
- C1 Ob-Gyn-2020Dokument33 SeitenC1 Ob-Gyn-2020yabsera mulatuNoch keine Bewertungen
- Toxoplasmosis BrochureDokument2 SeitenToxoplasmosis Brochurethecatisgay100% (1)