Beruflich Dokumente
Kultur Dokumente
Cortical Blindness
Hochgeladen von
jbahalkehCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Cortical Blindness
Hochgeladen von
jbahalkehCopyright:
Verfügbare Formate
Cortical Blindness in Children: A Study of Etiology and Prognosis
Virginia C.N. Wong, MBBS, MRCP
Thirty-four children (20 boys, 14 girls) with congenital and acquired cortical blindness were analyzed for visual outcome in relation to etiology, visual evoked potentials, electroencephalography, and cranial computed tomography. All 7 children with congenital cortical blindness remained blind on subsequent examination. Of the 27 children with acquired blindness, 16 (59%) had poor visual outcome. Poor visual outcome occurred in those with cardiac arrest, hypoxia, status epilepticus, intracranial hemorrhage, cerebral thrombosis, and head trauma. Good visual outcome occurred in children with hypotensive episodes after cardiac surgery. Of the 12 children with recovery of vision, the interval from acute loss of vision to partial or total recovery was 2 weeks to 5 months. Seven children had complete recovery of vision with no residual visual field defect. The majority of children (87%) had focal or multifocal spike-and-waves and slow sharp-wave discharges on electroencephalography. None had photic recruitment response or occipital spike-and-wave discharges. Flash visual evoked potential studies performed during acute episodes of cortical blindness documented 11 with absent response, 10 with bilateral increases in latency, and 6 with normal responses. There was no correlation b e t w e e n n o r m a l visual evoked potentials and a good visual outcome. Only 2 of 6 children with normal responses had normal vision. Abnormal or absent responses are more predictive of a poor recovery of vision because only 3 of 21 (14%) had normal vision on subsequent examination. Abnormal electroencephalographic findings with focal or multifocal spike-and-wave discharges or cerebral atrophy on cranial computed tomography are also poor prognostic signs.
mus with preservation of pupillary response, normal eye motility, and normal retina [ 1]. Cortical visual impairment (CVI) has been recommended as a better term because it encompasses a spectrum of visual loss ranging from absent to some residual vision [2,3]. Various causes of CB have been reported in children, including cardiac arrest [4,5], status epilepticus [6,7], hypoxia or perinatal asphyxia [8], cerebral infarction [9], meningitis, encephalitis [ 10-13], subacute sclerosing leukoencephalitis [14], hypoglycemia [15,16], uremia [17. 18 ], hydrocephalus, shunt malfunction [19,20], head trauma [21-25], cardiac surgery [26,27], cerebral or vertebral angiography [28-35], drugs (i.e., cyclosporin A and steroids) [36,37], acute carbon monoxide poisoning 138], and the ictal state in occipital lobe epilepsy [39,401 or postictal phenomenon [41 ]. Other causes reported in adults include subclavian vein catheterization [42], pre-eclampsia [43, 44], postpartum pulmonary embolus [45], acupuncture [46], Wegener's granulomatosis [47], sarcoidosis [48 l, and posterior fossa tumor [49], In this study, the clinical features and laboratory investigations of 34 children with cortical blindness are analyzed to determine the prognosis of visual outcome in relation to etiology, visual evoked potential (VEP), electroencephalographic (EEG), and computed tomographic (CT) findings.
Methods
Thirty-lour CB children (20 boys, 14 girls), ages I month to 14 years, admitted to the Department of Paediatrics, University of Hong Kong at the Queen Mary Hospital from 1985 to 1990. were analyzed. Patients were included when severe visual loss occurred in the presence of normal pupillary response and normal fundi. Patients were excluded when the duration of visual loss lasted less than 48 hours. All children had multidisciplinary evaluations, including clinical assessment by ophthalmologists, a developmental pediatrician, and a child neurologist. Investigations, including flash VEP, EEG, photic stimulation, and cranial CT, were performed for most children. They were examined subsequently at the Child Assessment Centre of the Duchess of Kent Children's Hospital for I-5 years. ~)'sual Z?sting. The test of visual acuity was difficult in yotmger patients. Therefore, visual acuity was graded as "blind" when no apparent vision was present, including light perception or protective blinking; "'poor" when only light perception was evident; "l'~.6r" when there was ~m ability to see a 1 inch red woolen ball or I cm chocolate candy
Wong VCN. Cortical blindness in children: A study of etiology and prognosis. Pediatr Neurol 1991 ;7:178-85.
Introduction
Cortical blindness (CB) has been defined as complete loss of all visual sensation and loss of optokinetic nystag-
From the Department of Pediatrics; University of Hong Kong; Queen Mary Hospital; Pokfulam, Hong Kong.
Communications should be addressed to: Dr. Wong; Department of Pediatrics; University of Hong Kong; Queen Mary Hospital; Pokfulam, Hong Kong. Received September 11, 1990; accepted October 30, 1990.
178
PEDIATRIC NEUROLOGY
Vol. 7 No. 3
at 1 foot; and "good" when there was an ability to see 1 mm chocolate candy at a 1 foot distance. Visual Evoked Potentials. Flash VEPs were obtained using flash stimuli through LED goggles at a rate of 1 Hz and recorded over the inion (Oz) referenced to the frontal region (Fz) according to the International 10-20 System using the Medelac MS92a machine. The latency to the peak of the positive response (PI00) was measured. Electroencephalagraphy. EEG was performed with scalp electrodes according to the International 10-20 System. The latest EEG finding taken with the scoring of the visual outcome was analyzed for any spike-and-wave or sharp-wave activities, the localization of abnormality, and the response to photic stimulation.
charges occurred in 12, focal slow-and-sharp-wave discharges in 3, focal or diffuse slowing in 4, and was normal in 5. None had photic recruitment responses. None had occipital spike-and-waves. In the congenital group, all had abnormal EEGs with focal or multifocal spike-and-wave or sharp-wave discharges and 2 children had additional burst suppression patterns. Cranial Computed Tomography. The majority of children had cerebral atrophy (11 of 27, 41%). Only 1 had bioccipital infarction.
Results (I) Congenital Cortical Blindness (Patients 1-7). The
clinical features, etiology, and investigation are recorded in Table 1. Of the 7 children (3 boys, 4 girls) with congenital CB, 3 had lissencephaly and I had mitochondrial myopathy. These children had no visual fixation or visual following at 1-4 months of age. All had associated neurologic deficit, including severe mental retardation and myoclonic epilepsy in all children and cerebral palsy (spastic tetraplegic type) in 4. All remained blind except for some degree of light perception in 3. Six had abnormal VEPs (i.e., 2 absent and 4 bilateral prolonged latencies). All had abnormal EEGs with focal or multifocal spikeand-wave or sharp-wave discharges. None had photic recruitment responses. CT scans demonstrated cerebral atrophy in 5 and pachygyria-agyria pattern in 2. (II) Acquired Cortical Blindness (Patients 8-34). The most common cause among these 27 patients (17 boys, 10 girls) was hypoxia (N = 14; 58%) with severe perinatal asphyxia in 1, cardiac arrest in 2, severe hypotensive episodes following cardiac surgery in 5, and status epilepticus in 6. Six had encephalitis or meningitis. Hydrocephalus with shunt malfunction occurred in 1, hydrocephalus with subdural hematoma, cerebral thrombosis, intracranial hemorrhage, and head trauma occurred in 1 each. Of the 6 children with status epilepticus, 3 (Patients 21,24,26) subsequently proved to be suffering from metabolic or degenerative diseases. The vision of these 3 children was normal prior to status epilepticus. In the other 3 children, all investigations failed to reveal an underlying etiology. Hypoxia related to prolonged seizure is the most likely cause of the visual damage. The majority (88%) had associated neurologic deficit with cerebral palsy in 19, mental retardation in 22, myoclonic epilepsy in 7, generalized tonic-clonic epilepsy in 6, complex partial seizure in 1, and deafness in 1. Good recovery of vision occurred in 7 children and partial recovery occurred in 5. Recovery of vision occurred from 2 weeks to 5 months after the insult. VEP. Of the 23 children with acquired CB who had VEPs performed, only 6 had normal responses. Eleven children had absent VEPs and 10 had bilateral increases in P I 0 0 latencies. In the congenital CB group, only 1 had normal VEPs. EEG. EEG was performed in 24 children in the acquired CB group. Focal or multifocal spike-and-wave dis-
Prognoses
Prognoses are listed in Table 2. Visual recovery was poor. Of the 7 congenital patients, 4 were completely blind and 3 had only light perception. In the acquired group, 59% had poor visual outcomes; in the majority of them, hypoxia, cardiac arrest, or status epilepticus was implicated. Normal visual outcomes occurred in 26%; 3 had had hypotensive episodes after cardiac surgery and 3 had had encephalitis or meningitis. All 5 children with fair visual o u t c o m e s (Patients 9,12,17,21,34) attended special schools for the physically and/or mentally handicapped. VEP. Of the 6 children with normal VEPs in the acquired group, only 2 had good recovery of vision, whereas only 3 of 21 (14%) of those with bilateral increases in latency or absent responses had good visual recovery. EEG. Children with focal or multifocal spike-andwaves usually had poor visual outcomes. Children with normal EEGs had good visual recovery. CT. The majority had cerebral atrophy and the visual outcomes were poor (13 of 16, 81%).
Discussion
The outcome of CB was poor in the present study. Of the children with CB due to congenital and acquired causes, 68% had poor visual recovery. The prognosis was particularly poor when the cause of CB was hypoxia, cardiac arrest, status epilepticus, or cerebrovascular diseases. Those sustaining hypotensive episodes after cardiac surgery had much better prognoses; 60% had normal vision. In general, the prognoses of CB children are good in other reports [5,8,19,20,22,23]. Of children with CB, 25-50% recovered useful vision, although they may be left with a complex disorder of visual perceptions. This difference may be due to varying CB etiologies and the different duration of hypoxia in our study [5,8,11 ]. Some degree of visual recovery will occur in CB children. Hoyt [50] and Hoyt and Walsh [51] reported recovery of vision in all 43 infants with CB but the rate of recovery was variable; visual recovery continued to occur for more than 2 years after the original insult in some children. There was no correlation between the duration of CB and the extent of visual recovery. Poor prognostic signs were uncontrolled seizures more than 3 months after insult and the development of microcephaly. The mechanism of vision recovery is unknown. It may be due to
Wong: CorticalBlindness 179
Table 1. Patient No./Sex/ Age (yrs)
Clinical features and investigations of cortical blindness Age (yrs) at Loss of Vision Associated Neurologic Deficit Visual Outcome Interval of ROV
Cause
F VEP
EEG
CT
Group I - Congenital
1/M/6.2
0.1
Congenital
CP (ST), severe MR, Myo Epi Severe MR, Myo Epi
B lin d
BL 1" latency Normal
S-W (both frontal), PS-NR Sharp-wave (R parieto-temporal ), PS-NR S-W (multifocal), PS-S-W S-W and poly S-W (multifocal), PS-NR S-W (multifocal) burst suppression protein, PS-NR Spike]poly S-W (multifocal), PS-NR ttypsarrhythmia, burst suppression pattern, PS-NR
Cerebral atrophy Cerebral atrophy
2/M/8
0.3
Congenital
Blind
3/F/5.7
0.8
Congenital
Severe MR, Myo Epi, deafness Severe MR, Myo Epi CP (ST), severe MR, Myo Epi
Blind
BL $ latency BL $ latency BL T latency
Cerebral atrophy Cerebral atrophy Pachygyriaagyria
4/M/9.6
0.3
Mitochondrial myopathy Lissencephaly
Blind
5/F/6.8
0. I
Blind
6/F/2.9
0.3
Lissencephaly
CP (ST), severe MR. Myo Epi CP (ST), severe MR, Myo Epi, deafness
Blind
Absent
Pachygyriaagyria Pachygyriaagyria, L cerebral hemiatrophy
7/F/1.9
0.4
Lissencephaly
Blind
Absent
Group 2 - Acquired
8/F/8.9
0.6
Perinatal asphyxia
CP (ST), severe MR, Myo Epi
Blind
Absent
Spike/sharp-wave (central, posterior) PS-NR S-W (multifocal) PS-NR S-W 0nultifocal especially frontal, temporal) PS-NR Normal
Cerebral atrophy
9/M/5.3
0.4
Cardiac arrest
CP (H), mild MR, Myo Epi CP (ST), severe MR, Myo Epi
Fair
3 mos
BL $ latency Absent
Cerebral atrophy Cerebral alrophy
10/F/4.6
0.6
Cardiac arrest (PCS; TOF)
Blind
t 1/M/17.6
14
PCS (DORV)
Normal
2 wks
BL ? latency BL $ latency
Norlna I
12/M/5. I
PCS (TOF)
Low average intelligence
Fair, visual field defect Blind
5 mos
Normal
BL occipital infarction
13/M/2.3
0.9
PCS (TGA)
CP (ST), severe MR, Myo Epi
Absent
S-W (muhitocal) PS-NR Normal Slow/sharp-wave Icentral) PS-NR
Cerebral atrophy Nomml Cerebral atrophy Porencephalic cyst
14/F/9.4 15/F/4.4
4.4 0.6
PCS (Pul S) PCS (TAPVD) CP (ST), severe MR CP (ST), severe MR
Normal Normal
4 wks 5 mos
16/M/3.9
1.3
Perinatal asphyxia, porencephalic cyst Hydrocephalus with shunt malfunction Hydrocephalus, subdural hematoma
Blind
17/F/3.6
0.1
CP (H)
Fair, visual field defect Blind
5 InOS
Absent
Hydroceph alus
18/F/2.2
0.8
CP (ST), severe MR
Absent
Hydrocephalus
180
PEDIATRIC NEUROLOGY
Vol. 7 No. 3
Table 1. Patient No./Sex/ Age (yrs)
(Continued) Age (yrs) at Loss of Vision Associated Neurologic Deficit Visual Outcome Interval of ROV
Cause
F VEP
EEG Low-voltage slow background, PS-NR Slow waves (R parietal, L frontal), PS-NR S-W (both parietal), sharp slow wave (both posterior), PS-NR S-W(diffuse)
CT Subarachnoid, intracranial hemorrhage BL parietal infarction
19/M/1
0.3
Intracranial hemorrhage
CP (ST), severe MR
Blind
--
Absent
20/1=/10
Cerebral thrombosis
CP (ST), severe MR
Blind
--
Absent
21/M/4
0.1
Urea cycle defect, SE
CP (ST), severe MR, Epi
Fair
5 mos
Normal
Normal
22/M/3
SE
Severe MR, Epi
Blind
--
BL $ latency
Cerebral atrophy Cerebral atrophy
23/F/5
3.1
SE
CP (SD), moderate MR, Epi
Normal
3 mos
Absent
Slow-sharp-wave (posterior), PS-normal
S-W(diffuse), PS-NR
24/F/1.1
0.6
Ceroid-lipofuscinosis, SE SE
CP (ST), severe MR, Epi Moderate MR, deafness CP (ST), severe MR, Epi Moderate MR
Blind
--
Normal
Cerebral atrophy Cerebral atrophy Normal
25/M/6.4
3.9
Blind
--
Normal
Diffuse slowing PS-NR Normal
26/M/6.3
SE, Reye syn
Blind
--
BL 1" latency BL $ latency
27/M/6.2
Encephalitis
Normal
1 mo
Normal
Normal
28/M/4.6 29/M/11
2 6
Encephalitis Encephalitis (influenza)
-MR (mild), Epi (TLE)
Normal Normal
2 wks 1 mo
Normal Normal
Diffuse slowing Diffuse slowing, slow-wave (R temporoparietal), PS-NR Spike/sharp-wave (L temporal) PSslow/sharp-wave, S-W discharges
Normal Normal
30/F/5.6
0.9
Encephalitis (herpes simplex)
CP (ST), severe MR, Epi
Blind
Hypodensity over L temporal region
3 l/M/3
0.6
Meningoencephalitis Meningitis (pneumococcal), PPE Meningitis (pneumococcal) Head trauma
CP (ST), severe MR CP (ST), severe MR, Myo Epi
Blind
--
Absent
S-W (multifocal), PS-NR S-W (multifocal), PS-NR
Cerebral atrophy Cerebral atrophy
32/M/4
Blind
--
BL $ latency
33/M/5
0.4
CP (ST), severe MR, Myo Epi
Blind
--
Absent
S-W (multifocal), PS-NR
Cerebral atrophy
34/M/11.6
CP (dys), severe MR, Myo Epi
Fair
3 mos
Normal
Spike/sharp-waves (R frontal), PS-NR
R epidural hematoma
Abbreviations: BL = Bilateral CP = Cerebral palsy DORV = Double outlet right ventricle Dys = Dyskinetic Epi = Epilepsy F VEP = Flash visual evoked potential
H MR Myo NR PCS PPE
= = = = = =
Hemiplegia Mental retardation Myoclonic No response Post cardiac surgery Post pertussis enceph.
PS Pul S ROV SD SE ST
= = = = = =
Photic stimulation Pulmonary stenosis Recovery of vision Spastic diplegia Status epilepticus Spastic tetraplegia
S-W = Spike-and-wave TAPVD = Total anomalous pulmonary venous drainage TGA = Transposition of great arteries TLE = Temporal lobe epilepsy TOF = Tetralogy of Fallot
Wong: Conical Blindness
181
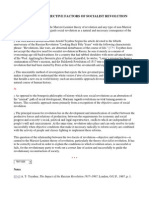
Table 2. Relation of visual outcome and etiology, VEP, EEG, and CT
Visual O u t c o m e
Blind/
Poor Fair Good 'l?otal
Etiology
(1) Congenital (11) Acquired - Cardiac arrest/hypoxia/status epilepticus - Cardiac surgery Hydrocephalus -- lntracranial hemorrhage/cerebral thrombosis/head trauma Encephalitis/meningitis 7 16 7 I 1 3 4 0 4 2 I I 0 0 tt 7 1 3 0 (I 3 7 27 I0 5 2 3 7
VEP*
Bilaterally $ latency Absent response Normal 6 9 3 2 1 1 2 1 2 10 II 6
EEG
Focal/multifocal spike waves Focal slow/sharp waves Focal/diffuse slowing Normal CT Cerebral atrophy Infarction Others Normal * For acquired causes. 13 I 7 [ 1 I 2 I 2 0 l) 0 16 2 9 2 15 2 3 0 3 0 0 I 0 2 2 3 18 4 5 4
resolution of edema, restitution of axonal connections, the use of minute parts of preserved field, or "non-striate vision" [52,53]. The general pattern of recovery from CB was described as denial of the inability to see in some patients followed by perceiving and following light, then perceiving moving objects close to the eyes, and later perceiving large, brightly colored objects. Later, visual acuity improved but visual cognitive and visual-perceptual deficits may persist for a long time or may remain permanently. Some may have residual visual field defects [8,51 ]. The pattern of visual recovery in this study also followed a similar trend. Those who were partially sighted needed special education and 2 patients had residual visual field defects on gross examination. The longest recovery time was 5 months and there was no improvement in visual function during a follow-up period of 9 months to 5 years in others with acquired causes.
The pathogenesis of CB was suggested by Barnet et al. [8] as related to the "border-zone hypothesis" [54] with transient cerebral hypotensive episodes causing more severe tissue hypoxia in the border zones among the 3 major cerebral arteries (i.e., the primary visual, sensory, and motor cortices with their association areas). Speech functions, in the distribution of the middle cerebral artery, are relatively spared. Other hypotheses include cerebral edema with herniation of the medial portions of the temporal lobes into the tentorial opening, thus compressing the posterior cerebral arteries; focal edema of the white matter in uremia [18]; thrombosis of superficial cortical veins in meningitis; and transient alteration of the blood-brain barrier in causing transient edema of the striatal cortex [29]. Many patients suffering from shock or hypoxia will have damage to the optic radiations; therefore, it affects not only the geniculocalcarine system to the striatal cortex which is responsible lot precise macular and peripheral
182
PEDIATRIC N E U R O L O G Y
Vol. 7 No. 3
vision and the identification of objects but also the parietal border zones, thus affecting the colliculo-pulvinar-parietal projection which is responsible for the detection of events and the direction of gaze [52,53]. Children with CB behaved differently from those with peripheral blindness. Nystagmus and roving eye movements are unusual; patients do not appear to be blind and they exhibit inertia, inattention, and variability in visual performance from moment to moment [52,53]. The use of VEP in predicting the prognosis of CB is controversial [3,50,54-63]. Hess et al. [62] investigated the validity of flash-VEP and pattern-reversal VEP in CB and concluded that flash VEP was not useful for differentiation of CB from psychogenic visual disorders and preserved flash VEP in the acute stage of CB was not reliably prognostic of visual recovery [62]. Abolished flash VEPs probably indicate a poor prognosis, whereas preserved flash VEPs do not allow prediction of good visual recovery. Pattern-reversal VEP, however, is more useful for diagnosis because a normal response is unlikely in acute and complete CB. The only possible exception was a small lesion restricted to the striate area 17 with preservation of areas 18 and 19 [59]. Preserved flash and pattern-reversal VEPs were observed in complete CB of a 6-year-old boy where CT revealed bilateral destruction of the occipital lobes (i.e., areas 18,19), the visual association cortex with sparing of the striatal cortex (i.e., area 17), or the primary receiving area of the geniculocortical visual pathway [58]. Preserved flash VEPs were also reported in complete CB with postmortem findings of extensive bilateral posterior cerebral infarcts. The VEP was probably mediated by extra geniculocalcarine connections between the optic nerve and the secondary visual cortex of the occipital convexity [63]. Celesia et al. reported the complete destruction of bilateral areas 17 with relative preservation of areas 18 and 19 in a woman with CB for more than 2 years and normal VEPs; they proposed the origin of VEP as mediated by extrageniculocalcarine pathways to the secondary visual cortices which are not capable of providing conscious visual perceptions in humans [59]. In a study of VEPs in 6 children with CB following meningitis and head trauma, changes in short-latency VEPs were correlated with visual ability and changes in longer latency VEPs correlated with levels of psychomotor function on subsequent examination [64]. It has been demonstrated that diffuse light and coarse moving stimuli can activate a "second visual system" which generates flash VEPs [62]. This system originates in cells in the periphery of the retina and projects along the geniculostriatal pathway and the structures of the extrastriatal visual pathway, such as the midbrain (primary superior colliculus), with indirect mediation to the thalamus or parietal cortex. Cells of the center of the retina are responsible for shape and pattern recognition. Responses are projected through the lateral geniculate nucleus to the striatal cortex and generate the pattern VEP. Thus,
preserved flash VEPs in CB could indicate a certain advantage over absent responses because the ability to have some rough spatial orientation could be achieved through the extrastriatal visual system. In our study, however, absent flash VEPs during acute episodes of CB usually had poor visual recovery and only 3 (20%) regained partial to normal vision. A study of EEG in 40 children with CB revealed multifocal disturbances because of diffuse cerebral involvement [2]. Isolated occipital spikes were rare and photic stimulation was of little use in diagnosis. Children with some residual vision usually had alpha rhythms, while multihandicapped children had multifocal abnormalities and suppressed posterior waking backgrounds, but no alpha rhythms. The presence or absence of alpha rhythms appeared to reflect the residual activity of the striatal cortex. Absent alpha rhythm in CB was observed in children and adults [55,65]. The majority of children (65%) in our study had spikeand-wave or sharp-wave abnormalities on EEG. Most of these patients have multiple handicaps due to diffuse cerebral involvement and poor visual function. None of the children had occipital spikes or photic recruitment responses. Alpha rhythm was also rarely observed except in those patients with ultimate recovery of vision. CT and magnetic response imaging (MRI) were helpful in evaluating 30 children with hypoxic CB [66]. Only 2 children had normal scans of the posterior visual pathway and both had favorable visual outcomes. Visual recovery differed significantly with respect to the age at which the hypoxic insult occurred and the CT and MRI abnormalities in the areas of the optic radiations, but not with abnormalities in the striatal or parastriatal cortices. Bioccipital abnormalities on CT were also reported to be associated with poor prognoses [54]. The majority of our patients had cerebral atrophy on CT and visual recovery was poor. Even the 2 children with normal CT scans did not have good outcomes. In general, this study demonstrated that the prognosis of visual recovery in children with cortical blindness, both congenital and acquired, is poor. Those with absent or abnormal VEPs or abnormal EEG and CT had poorer prognoses probably due to more diffuse cerebral damage.
The author acknowledges Teresa Wong for secretarial assistance.
References [1] Marquis DG. Effects of removal of visual cortex in mammals with observations on the retention of light discrimination in dogs. Proc Assoc Res Nerv Ment Dis 1934;13:588-92. [2] Robertson R, Jan JE, Wong PKH. Electroencephalograms of children with permanent cortical visual impairment. Can J Neurol Sci 1986;13:256-61. [3] Whiting S, Jan JE, Wong PKH, Flodmark O, Farrell K, McCormick AQ. Permanent cortical visual impairment in children. Dev Med Child Neurol 1985;27:730-9.
Wong: Cortical Blindness
183
[4] Rossen R, Jeub RE Cortical blindness after cardiac arrest, report of two cases with recovery. Clin Electroencephalogr 1970;1: 165-70. [51 Weinberger HA, Van de Woude R, Maier HC. Prognosis of cortical blindness following cardiac arrest in children. JAMA 1962; 179:126-9. [6] Ashby H, Stephenson S. Amaurosis following infantile convulsions. Lancet 1903; 1: 1294-6. [7] Kosnik E, Paulson GW, L a g u n a JF. Postictal blindness. Neurology 1976;26:248-50. 18] Barnet AB, Manson Jl, Wilner E. Acute cerebral blindness in childhood: Six cases studied clinically and electrophysiologically. Neurology 1970;20:1147-56. 19] Symonds C, Mackenzie I. Bilateral loss of vision from cerebral infarction. Brain 1957;80:415-55. [10] Acers TE, Cooper WC. Cortical blindness secondary to bacterial meningitis. Am J Ophthalmol 1965;59:226-9. I111 Aekroyd RS. Cortical blindness following bacterial meningitis: A case report with reassessment of prognosis and etiology. Dev Med Child Neurol 1984;26:227-30. 112] Blasco GL, Peris VA, Hernandez MR, Escribano MA. Cortical blindness in meningococcal meningitis. An Esp Pediatr 1988;29: 175-6. 1131 Newton NL, Reynolds JD, Woody RC. Cortical blindness following hemophilus influenzae meningitis. Ann Ophthalmol 1985;17: 193-4. 114] R a m b a c h L, Roth T, Garcia F, Pitre F, Brini A, Collard M. Cortical blindness disclosing subacute sclerosing leukoencephalitis. Rev Otoneuroophtalmol 1984;56:463-6. 115] Garty BZ, Dianrai G, Nitzan M. Transient acute cortical blindness associated with hypoglycemia. Pediatr Neurol 1987;3:169-70. 1161 Mnkamel M, Weitz R, Nissenkorn E, Yassur 1, Varsano 1. Acute cortical blindness associated with hypoglycemia. J Pediatr 1981; 98:583-4. [17] Moel DI, Kwun YA. Cortical blindness as a complication of hemodialysis. J Pediatr 1978;93:890-1. [18] Tyler HR. Neurologic disorders in renal failure. Am J Med 1968;44:734-48. [19] Lorber J. Recovery of vision following prolonged blindness in children with hydrocephalus or following pyogenic meningitis. Clin Pediatr 1967;6:699-703. [20] Tyehsen L, Hoyt WF. Hydrocephalus and transient cortical blindness. Am J Ophthalmol 1984;98:819-21. [21] Bodian M. Transient loss of vision following head trauma. New York State J Med 1964;64:916-20. [22] Eldrige PR, Punt JA. Transient traumatic cortical blindness in children. Lancet 1988;1:815-6. 123] Gjerris F, Mellemgaard L. Transitory cortical blindness in head injury. Acta Neurol Scand 1969;45:623-31. [24] Griffith JF, Dodge PR. Transient blindness following head injury in children. N Engl J Med 1968;278:648-51. [251 Ichikawa T, Koizumi J, Sakuma K, Nagase S, Shimizu F, Nose T. A long-term cortical blindness after head trauma. Jpn J Psychiatry Neurol 1987;41 : 19-23. 1261 Gilman S. Cerebral disorders after own-heart operations. N Engl J Med 1965;272:489-99. [27] Smith JL, Cross SA. Occipital lobe infarction after open heart surgery. J Ctin Neurol Ophthalmol 1983;3:23-30. [28] Falls HF, Bassett RC, Lamberts AE. Ocular complications encountered in intracranial arteriography. Arch Ophthalmol 1951;45: 623-6. [291 Horwitz NH, Wener L. Temporary cortical blindness following angiography. Neurology 1974;40:583-7. [30] Kaplan AD, Walker AE. Complications of cerebral angiography. Neurology 1954;4:643-56. [31] Lantos G. Cortical blindness due to osmotic disruption of the blood-brain barrier by angiographic contrast material: CT and MRI studies. Neurology 1989;39:567-71.
[32] Niezabitowski K, K o j d e r 1, G i e r g i e l e w i c z J, Fryze C, Domanski Z. Transient cortical blindness as a complication of vertebral arteriography. Pol Przegl Radiol 1984;48:137-40. [33] Prendes JL. Transient cortical blindness following vertebral angiography. Headache t978;18:222-4. [34] Shyn PB, Bell KA. Transient cortical blindness lbllowing cerebral angiography. J La State Med Soc 1989; 141:35-7. [35] Silverman SM, Bergman PS, Bender MB. The dynanucs of transient cerebral blindness: Report of nine episodes following vertebral angiography. Arch Neurol 1961 ;4:333-48. [36] Decsi T, Kosztolanyi G, Dzopf J. Sudden cortical blindness following transient enhancement of steroids administered in congenital adrenal hyperplasia (case report). Acta Paediatr Hung 1990;30:107-1(I. [371 Wilson SE, de Groen PC, Akstunit AJ, Wiesner RH, Garrity JA, Krom RA. Cyclosporin A-induced reversible cortical blindness. J Clin Neurol Ophthalmol 1988;8:215-21/. 138] Katafuchi Y, Nishimi T, Yamaguchi WY, et at. Cortical blindhess in acute carbon monoxide poisoning. Brain Dev 1985:7:516-9. [39] Jaffe SJ, Roach ES. Transient cortical blindness with occipital lobe epilepsy. J Clin Neurol Ophthalmol 1988;8:221-4. 140] Aldrich MS, Vanderzant CW, Alessi AG, Abou-Khalil B, Sackellares JC. Ictal cortical blindness with permanent visual loss. Epilepsia 1989:30:116-20. [41] Skolik SA, Mizen TR, Burde RM. Transient postictal cortical blindness. J Clin Neurol Ophthalmol 1987;3:151-4. 1421 Acalovsehi I, Corbaciu D, Paraianu 1. Cortical blindness after subclavian vein catheterization. JPEN J Parenter Enteral Nutr 1988;12: 526-7. [43] Levavi H, Neri A, Zoldan J, Segal J, Ovadia J. Pre-eclampsia, "HELP" syndrome and postictal cortical blindness. Acta Obstet Gynecol Scand 1987;66:91-2. [44] Stein LB, Roberts RI, Marx J, Rossoff L. Transient cortical blindness following an acute hypotensive event in the postpartum peri od. New York State J Med 1989;89:682-3. [45] Stiller RJ, Leone-Tomaschoff S, Cuteri J, Beck L. Postpartum pulmonary embolus as an unusual cause of cortical blindness. Am J Obstet Gynecnl 1990; 162:696-7. [46] Liu SD. Cure of 2 cases of cortical blindness with acupuncture therapy. J Tradit Chin Med 1982;2:303-5. 1471 Payton CD, Jones JM. Cortical blindness complicating Wegener's granulomatosis. Br Med J (Clin Res) 1985;290:676. [481 Powers JM. Sarcoidosis of the tentorium with cortical blindness. J Clin Neurol Ophthalmol 1985:5:112-5. [491 Bran RH. Lameiro J, Llagunn AV, Riflcinson N. Metamorphopsia and permanent cortical blindness alter a posterior fossa tmnor. Neurosurgery 1986; 19:263-6. [50] ]toyt CS. Cortical blindness in infancy. Trans New Orleans Acad Ophthalmol 1986;:235-43. [511 ltoyt W E Walsh FB. Cortical blindness with partial recovery following acute cerebral anoxia from cardiac arrest. Arch Ophthalmol 1958;60:1061-9. [52] Foley J. Central visual disturbances. Dev Med Child Neurol 1987;29:110-20. [531 Foley J, Gordon N. Recovery from cortical blindness. Dev Med Child Neurol 1985;27:383-9 I. [54] Lindenberg R, Spatz H. Ober die thromboendarteritis obliterans der Hirngefasse. Virchow Arch (Path Anat) 1939;305:531-57. 155] Aldrich MS, Alessi AG, Beck RW, Gilman S. Cortical blindness: Etiology, diagnosis, and prognosis. Ann Neurol 1987;21:149-58. [561 A b r a h a m FA, Melamed E, Lavy S. Prognostic value of visual evoked potentials in occipital blindness following basilar artery occlu sion. Appl Neurophysiol 1975:38:126-35. [57] Bodis-Wollner 1. Recovery from cerebral blindness: Ew)ked potential and psychophysical measurements. Electroencephalogr Clin Neurophysiol 1977;42:178-84. [58] Bodis-Wollner I, Atkin A, Raab E, Wolkstein M. Visual association cortex and vision in man: Pattern-evoked occipital potentials in a blind boy. Science 1977:198:629-3 I.
184
PEDIATRIC NEUROLOGY
Vol. 7 No. 3
[59] Celesia GG, Archer CR, Kuroiwa Y, Goldfader PR. Visual function of the extrageniculo-calcarine system in man: Relationship to cortical blindness. Arch Neurol 1980;37:704-6. [60] Egan D, Regal DM, Tibbles JAR. Evoked potentials during recovery from blindness recorded serially from an infant and his normally sighted twin. Electroencepbalogr Clin Neurophysiol 1982;54: 465-8. [61] Frank Y, Tones E Visual evoked potentials in the evaluation of"cortical blindness" in children. Ann Neurol 1979;6:126-9. [62] Hess CW, Meienberg O, Ludin HP. Visual evoked potentials in acute occipital blindness: Diagnostic and prognostic value. J Neurol 1982;227:193-200. [63] Spehlmann R, Gross RA, Ho SU, Leestma JE, Norcross KA. Visual evoked potentials and postmortem findings in a case of cortical blindness. Ann Neurol 1977;2:531-4.
[64] Duchowny MS, Majlessi H, Bamet AB. Visual evoked responses in childhood cortical blindness after head trauma and meningitis. Neurology 1974;24:933-40. [65] Bergman PS. Cerebral blindness: An analysis of twelve cases, with special reference to the electroencephalogram and patterns of recovery. Arch Neurol Psychiatry 1957;78:568-84. [66] Lambert SR, Hoyt CS, Jan JE, Barkovich J, Flodmark O. Visual recovery from hypoxic cortical blindness during childhood. Computed tomographic and magnetic resonance imaging predictors. Arch Ophthalmol 1987;105:1371-7.
Wong: Cortical Blindness
185
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- 100 Days of Sunlight by Abbie EmmonsDokument315 Seiten100 Days of Sunlight by Abbie EmmonsJessie Ann Aquino100% (11)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Horkheimer - Traditional and Critical Theory (1937)Dokument28 SeitenHorkheimer - Traditional and Critical Theory (1937)timsvh7059Noch keine Bewertungen
- Phrasal Verbs Cut Do GetDokument26 SeitenPhrasal Verbs Cut Do Getjbahalkeh100% (1)
- Antimalarial DrugsDokument18 SeitenAntimalarial DrugsjbahalkehNoch keine Bewertungen
- Karl Marx Poverty of PhilosophyDokument84 SeitenKarl Marx Poverty of PhilosophyjbahalkehNoch keine Bewertungen
- Inverse Function: DefinitionsDokument11 SeitenInverse Function: Definitionsjbahalkeh100% (1)
- IC RetinoblastomaDokument10 SeitenIC RetinoblastomajbahalkehNoch keine Bewertungen
- All Quiet On The Western FrontDokument73 SeitenAll Quiet On The Western FrontjbahalkehNoch keine Bewertungen
- Sudoku ChallengeDokument3 SeitenSudoku ChallengejbahalkehNoch keine Bewertungen
- Structure of A PaperDokument6 SeitenStructure of A PaperjbahalkehNoch keine Bewertungen
- Berlin - THE PURPOSE OF PHILOSOPHYDokument8 SeitenBerlin - THE PURPOSE OF PHILOSOPHYjbahalkeh7570Noch keine Bewertungen
- Research Method (DLM Slide)Dokument5 SeitenResearch Method (DLM Slide)sahirbuleNoch keine Bewertungen
- International System of UnitsDokument11 SeitenInternational System of UnitsjbahalkehNoch keine Bewertungen
- 5a. Marx - The Fetishism of CommoditiesDokument2 Seiten5a. Marx - The Fetishism of Commoditiescs1702Noch keine Bewertungen
- Zakaria Dont Rush To War With IranDokument1 SeiteZakaria Dont Rush To War With Iranjbahalkeh7570Noch keine Bewertungen
- Objective Plus Subjective Factors of Socialist RevolutionDokument13 SeitenObjective Plus Subjective Factors of Socialist RevolutionjbahalkehNoch keine Bewertungen
- Education: Early Years Arts and Sciences Bachelor in LebanonDokument6 SeitenEducation: Early Years Arts and Sciences Bachelor in LebanonjbahalkehNoch keine Bewertungen
- Impact Factor Ranking JournalDokument2 SeitenImpact Factor Ranking JournaljbahalkehNoch keine Bewertungen
- Maastricht Treaty: Navigation SearchDokument7 SeitenMaastricht Treaty: Navigation SearchjbahalkehNoch keine Bewertungen
- Koffi Annan Freedon From Fear Ch3Dokument12 SeitenKoffi Annan Freedon From Fear Ch3jbahalkehNoch keine Bewertungen
- Sanders DR Clinical Trial of The Implantable Contact Lens For Moderate To High MyopiaDokument25 SeitenSanders DR Clinical Trial of The Implantable Contact Lens For Moderate To High MyopiajbahalkehNoch keine Bewertungen
- Frederick Engels Socialism Utopian and ScientificDokument23 SeitenFrederick Engels Socialism Utopian and ScientificjbahalkehNoch keine Bewertungen
- 400 Bad Request 400 Bad Request Nginx/1.2.9Dokument48 Seiten400 Bad Request 400 Bad Request Nginx/1.2.9jbahalkehNoch keine Bewertungen
- 400 Bad Request 400 Bad Request Nginx/1.2.9Dokument17 Seiten400 Bad Request 400 Bad Request Nginx/1.2.9jbahalkehNoch keine Bewertungen
- Khrushchev Secret Speech The Cult of The IndividualDokument27 SeitenKhrushchev Secret Speech The Cult of The IndividualjbahalkehNoch keine Bewertungen
- CSA HistoryDokument33 SeitenCSA HistoryjbahalkehNoch keine Bewertungen
- 400 Bad Request 400 Bad Request Nginx/1.2.9Dokument128 Seiten400 Bad Request 400 Bad Request Nginx/1.2.9jbahalkehNoch keine Bewertungen
- A Man For All SeasonsDokument75 SeitenA Man For All SeasonsSamik DasguptaNoch keine Bewertungen
- APC Info for Kowsar JournalsDokument4 SeitenAPC Info for Kowsar JournalsjbahalkehNoch keine Bewertungen
- Refractive Surgery Yanoff 2Dokument4 SeitenRefractive Surgery Yanoff 2jbahalkehNoch keine Bewertungen
- Ludwig WittgensteinDokument22 SeitenLudwig WittgensteinjbahalkehNoch keine Bewertungen
- Visual Anosognosia (Anton-Babinski Syndrome) : Report of Two Cases Associated With Ischemic Cerebrovascular DiseaseDokument5 SeitenVisual Anosognosia (Anton-Babinski Syndrome) : Report of Two Cases Associated With Ischemic Cerebrovascular DiseaseHanna EnitaNoch keine Bewertungen
- Cli&Exa&Oph&2 NDDokument420 SeitenCli&Exa&Oph&2 NDPink FongNoch keine Bewertungen
- Cortical Visual Impairment Rehabilitation StrategiesDokument55 SeitenCortical Visual Impairment Rehabilitation StrategiesIntanOktavianaAdiyanto100% (1)
- The Occipital Lobes: The Primary Visual Cortex (Area 17) The Striate AreaDokument4 SeitenThe Occipital Lobes: The Primary Visual Cortex (Area 17) The Striate AreaHarshad MalganiNoch keine Bewertungen
- Postoperative Blindness After Spine Surgery in The Prone PositionDokument17 SeitenPostoperative Blindness After Spine Surgery in The Prone Positionwidget_13Noch keine Bewertungen
- Delayed Visual Maturation in Infants: Andrew Tatham, Saurabh JainDokument12 SeitenDelayed Visual Maturation in Infants: Andrew Tatham, Saurabh JainAffannul HakimNoch keine Bewertungen
- Occipital LobesDokument46 SeitenOccipital LobesLakshya J Basumatary100% (1)
- Cortical Visual Impairment and Blindness: by Komal SharmaDokument15 SeitenCortical Visual Impairment and Blindness: by Komal SharmaOphthalmology DiscussionNoch keine Bewertungen
- Anton'S Syndrome and Cortical Blindness: Case ReportDokument3 SeitenAnton'S Syndrome and Cortical Blindness: Case ReportDevasyaNoch keine Bewertungen