Beruflich Dokumente
Kultur Dokumente
Drug Analysis: Submitted By: GALICINAO, Gretta Shalou G
Hochgeladen von
ggalicinaoOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Drug Analysis: Submitted By: GALICINAO, Gretta Shalou G
Hochgeladen von
ggalicinaoCopyright:
Verfügbare Formate
Submitted by: GALICINAO, Gretta Shalou G.
Section 3 Year 5 RLE 1 UST Pedia Ward | MTW 7-12
DRUG ANALYSIS
GENERIC NAME CLASSIFICATI ON Corticosteroid, Glucocorticoid Hormone ACTION INDICATION CONTRAINDICATIO NS Oedema, hypertension, arrhythmia; CNS, endocrine, metabolic and GI effects; hirsutism, acne, skin atrophy, bruising, hyperpigmentation; transient leukocytosis; arthralgia, muscle weakness, osteoporosis, fractures, cataracts, glaucoma; infections, hypersensitivity reactions, avascular necrosis, secondary malignancy, intractable hiccups. ADVERSE EFFECTS Serious infections except septic shock or tuberculous meningitis; viral, fungal and tubercular skin lesions; admin of live virus vaccines. Preparations containing benzyl alcohol preservative are contraindicated in infants. NURSING RESPONSIBILITI ES Assessment History: Infections; kidney or liver disease, hypothyroidism, ulcerative colitis, diverticulitis, active or latent peptic ulcer, inflammatory bowel disease, CHF, hypertension, thromboembolic disorders, osteoporosis, seizure disorders, diabetes mellitus; pregnancy; lactation Physical: Weight, T, reflexes and grip strength, affect and orientation, P, BP, peripheral perfusion prominence of superficial veins, R and adventitious sounds, serum electrolytes, blood glucose Interventions Use caution with
1)methylprednisolo ne
Methylprednisolo ne is a synthetic corticosteroid that decreases inflammation by suppressing the migration of polymorphonucle ar leukocytes and reversal of increased capillary permeability. > antiinflammatory ang immunosuppressi ve effects
> Short-term management of various inflammatory and allergic disorders, such as rheumatoid arthritis, collagen diseases (eg, SLE), dermatologic diseases (eg, pemphigus), status asthmaticus, and autoimmune disorders > Hematologic disorders: Thrombocytopeni a purpura, erythroblastopeni a > Ulcerative colitis, acute exacerbations of MS, and palliation in some leukemias and lymphomas >Trichinosis with neurologic or myocardial
involvement >Prevention of nausea and vomiting associated with chemotherapy > Unlabeled use: Septic shock, respiratory distress syndrome, acute spinal cord injury
the 24-mg tablets marketed as Medrol; these contain tartrazine, which may cause allergic reactions, especially in people who are allergic to aspirin. Give daily dose before 9 to mimic normal peak corticosteroid blood levels. Increase dosage when patient is subject to stress. WARNING: Taper doses when discontinuing highdose or long-term therapy to allow adrenal recovery. WARNING: Do not give live virus vaccines with immunosuppressive doses of corticosteroids. Teaching points Do not to stop taking the oral drug without consulting your health care provider. Avoid exposure to infections. Report unusual weight gain,
2) Vincristine sulfate
Antineoplastic Mitotic inhibitor
Arrests mitosis at metaphase, thereby, inhibiting cell division.
> Acute leukemia > Hodgkins lymphoma, rhabdomyosarco ma, neuroblastoma, Wilms tumor as part of combination therapy
> allergy to vincristine, leucopenia, acute infection, pregnancy, lactation, demyelinating form, use cautiously with neuromuscular disease, diabetes insipidus, hepatic impairment
CNS: Peripheral neuropathy, neuritic pain, paresthesias, especially of hands and feet; foot and hand drop, sensory loss, athetosis, ataxia, loss of deep tendon reflexes, muscle atrophy, dysphagia, weakness in larynx and extrinsic eye muscles, ptosis, diplopia, mental depression. Special Senses: Optic atrophy with blindness; transient cortical blindness, ptosis, diplopia, photophobia. GI: Stomatitis, pharyngitis,
swelling of the extremities, muscle weakness, black or tarry stools, fever, prolonged sore throat, colds or other infections, worsening of disorder. Assessment & Drug Effects Monitor I&O ratio and pattern, BP, and temperature daily. Weigh patient under standard conditions weekly or more often if ordered. In the presence of edema or ascites, patient's ideal weight is used to determine dosage. Report a steady gain or sudden weight change to physician. Lab tests: Monitor serum electrolytes and CBC with differential. Complete bone marrow remission in leukemia varies widely and may not occur for as long as 100 d after therapy is started. Be aware that neuromuscular
anorexia, nausea, vomiting, diarrhea, abdominal cramps, severe constipation (upper-colon impaction), paralytic ileus (especially in children), rectal bleeding; hepatotoxicity. Urogenital: Urinary retention, polyuria, dysuria, SIADH (high urinary sodium excretion, hyponatremia, dehydration, hypotension); uric acid nephropathy. Skin: Urticaria, rash, alopecia, cellulitis and phlebitis following extravasation (at injection site). Body as a Whole: Convulsions with hypertension, malaise, fever,
adverse effects, most apt to appear in the patient with preexisting neuromuscular disease, usually disappear after 6 wk of treatment. Children are especially susceptible to neuromuscular adverse effects. Assess for hand muscular weakness, and check deep tendon reflexes (depression of Achilles reflex is the earliest sign of neuropathy). Also observe for and report promptly: Mental depression, ptosis, double vision, hoarseness, paresthesias, neuritic pain, and motor difficulties. Provide special protection against infection or injury during leukopenic days. Leukopenia occurs in a significant number of patients; leukocyte count in children usually reaches nadir on
headache, pain in parotid gland area, weight loss. Metabolic: Hyperuricemia, hyperkalemia. CV: Hypertension, hypotension. Respiratory: Bronchospasm.
fourth day and begins to rise on fifth day after drug administration. Avoid use of rectal thermometer or intrusive tubing to prevent injury to rectal mucosa. Check patient's ability to ambulate and supply support if necessary. Walking may be impaired. Take care to distinguish between the depression associated with realization of neoplastic disease and that which is drug-induced. Patient & Family Education Notify physician promptly of stomach, bone, or joint pain, and swelling of lower legs and ankles. Start a prophylactic regimen against constipation and paralytic ileus (adequate fluids, high-fiber diet, laxatives) at
3) Folinic Acid
folic acid derivative
active reduced form of folic acid; required for neucloprotein synthesis and maintenance of normal hematopoiesis
In combination with fluoruracil to treat cancers such as; colon and rectal, head and neck, esophageal, and other cancers of the gastrointestinal tract. As an antidote to effects of certain chemotherapy drugs such as
> allergy to leucovorin on previous exposure, pernicious anemia or other megaloblastic anemias in which vitamin B12 is deficient
Hypersensitivit y: allergic reaction Local: Pain, discomfort at injection site
beginning of treatment and report changes in bowel habit to health care providers as soon as manifested (paralytic ileus is most likely to occur in young children). Reversible hair loss is reportedly the most common adverse reaction and may persist for the duration of therapy. Regrowth may start before end of treatment. This is a distressing adverse effect because the scalp hair will drop out in large clumps. Do not breast feed while taking this drug. Interventions: > Begin leucovorin rescue within 24 hours of methotrexate administration. arrange for fluid loading and urine alkalinization during this procedure to decrease methotrexate toxicity. > give drug orally
methotrexate. Treatment of megaloblastic anemia when folic acid deficiency is present. > Leucovorin rescue after highdose methotrexate therapy for various cancers > to decrease toxicity of methotrexate caused by decreased elimination or for inadvertent overdose of folic acid antagonists such as trimethoprim
unless intolerance to oral route develops due to nausea and vomiting from chemotherapy or clinical condition. Switch to oral drug when feasible. Doses more than 25 mg should be divided or given IV > Monitor patient for hypersensitivity reactions, especially if drug has been used previously. Keep supportive equipment and emergency drugs readily available in case of serious allergic response. > Report rash, difficulty breathing, pain, or discomfort at injection site. > Mark calendars with treatment days > Protect solution fro inhalation from light. Store unused vials in foil pouch. > use nebulizer mouthpiece instead of face mask to avoid blurred vision or aggravation of
4) ipratropium bromide + salbutamol sulfate (nebulizer)
(for ipratropium bromide) Anticholinergic Antimuscarinic Bronchodilator Parasympatholytic
Anticholinergic, chemically related to atropine, which blocks vagally mediated reflexes by antagonizing the action of acetylcholine.
> obstructive pulmonary disease > bronchodilator for maintenance treatment of bronchospasm associated with COPD, chronic
> hypersensitivity to atropine or its derivatives, soybean or peanut allergies > use cautiously with narrow-angle glaucoma, prostatic hypertrophy, bladder neck obstruction, pregnancy,
Bronchitis, respiratory tract infections. Chest pain, arrhythmia, oedema, hypertension, hypokalaemia, palpitation,
Causes bronchodilation and inhibits secretion from serous and seromucous glands lining the nasal mucosa
bronchitis, emphysema > nasal spray: symptomatic relief of rhinorrhea associated with perennial rhinitis, common cold, seasonal allergic rhinitis
lactation
tachycardia. Headache, dizziness, fatigue, insomnia, tremor, nervousness. GI symptoms e.g. nausea, vomiting, diarrhoea, dyspepsia and constipation. Respiratory: dyspnea, bronchitis, bronchospasms, URI, cough, exacerbation of symptoms, hoarseness, pharyngitis
narrow-angle glaucoma > can mix with albuterol in nebulizer for up to 1 hr > ensure adequate hydration; control environment (temp) to prevent hyperexia > have patient void before taking medication to avoid urinary retention > teach patient proper use of inhaler.
5) D5IMB Balanced Multiple Maintenace Solution with 5% dextrose
Hypertonic solution
Contain a high concentration of solute relative to another solution (e.g. the cell's cytoplasm). When a cell is placed in a hypertonic solution, the water diffuses out of the cell, causing the cell to shrivel
Slow administration essential to prevent overload (100 mL/hr) Water intoxication Severe sodium depletion
-phlebitis, peripheral edema, cellular dehydration
> Do not administer unless solution is clear and container is undamaged. > Caution must be exercised in the administration of parenteral fluids, especially those containing sodium ions to patients receiving corticosteroids or corticotrophin. >Solution containing acetate should be used with caution as excess
administration may result in metabolic alkalosis. >Solution containing dextrose should be used with caution in patients with known subclinical or overt diabetes mellitus. > Discard unused portion. > In very low birth weight infants, excessive or rapid administration of dextrose injection may result in increased serum osmolality and possible intracerebral hemorrhage. 6) Ampicillin 7) Salbutamol 8) Nasal Spray Sodium Chloride
Das könnte Ihnen auch gefallen
- CyclosporineDokument24 SeitenCyclosporinesanchit_J14Noch keine Bewertungen
- Health According To The Scriptures - Paul NisonDokument306 SeitenHealth According To The Scriptures - Paul NisonJSonJudah100% (1)
- Anatomy TerminologyDokument20 SeitenAnatomy Terminologykhabbab hussainNoch keine Bewertungen
- Concise Guide To Forgetting How Much You SuckDokument7 SeitenConcise Guide To Forgetting How Much You SuckihatemakingusernamesNoch keine Bewertungen
- Cases and Doctrines On Legal MedicineDokument44 SeitenCases and Doctrines On Legal MedicineEliza MontemayorNoch keine Bewertungen
- Anticholinergics Study Drug ListDokument1 SeiteAnticholinergics Study Drug ListDrima Edi100% (1)
- Complete DentureDokument57 SeitenComplete Denturedr_ahmad_zuhdi100% (3)
- Clinical Assessment of The Autonomic Nervous System PDFDokument312 SeitenClinical Assessment of The Autonomic Nervous System PDFAndrija100% (1)
- St. Paul University Dumaguete St. Paul University System College of Nursing ISO 9001Dokument16 SeitenSt. Paul University Dumaguete St. Paul University System College of Nursing ISO 9001Dinarkram Rabreca EculNoch keine Bewertungen
- Management of Tuberculosis: A guide for clinicians (eBook edition)Von EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Noch keine Bewertungen
- 302 PpJ. Grayson, Freedom From Obsessive Compulsive Disorder A Personalized Recovery Program For LivingDokument2 Seiten302 PpJ. Grayson, Freedom From Obsessive Compulsive Disorder A Personalized Recovery Program For LivingMohammad Shoyyad L IkhsanNoch keine Bewertungen
- Norepinephrine Drug StudyDokument2 SeitenNorepinephrine Drug StudyIrish LigayaNoch keine Bewertungen
- Magnesium Hydroxide (Milk of Magnesia)Dokument1 SeiteMagnesium Hydroxide (Milk of Magnesia)ENoch keine Bewertungen
- Labor LawDokument11 SeitenLabor LawggalicinaoNoch keine Bewertungen
- Milestones G&D-Page 1Dokument3 SeitenMilestones G&D-Page 1ggalicinaoNoch keine Bewertungen
- Anes Drugs TableDokument20 SeitenAnes Drugs TableKathleen Grace ManiagoNoch keine Bewertungen
- Pemasangan Kateter UrinDokument12 SeitenPemasangan Kateter UrinYULI222100% (1)
- BrivaracetamDokument110 SeitenBrivaracetamBendisDacicaNoch keine Bewertungen
- AzathioprineDokument3 SeitenAzathioprineAdela abboudNoch keine Bewertungen
- AcetylcysteineDokument2 SeitenAcetylcysteineJonah Camille Yap FortunaNoch keine Bewertungen
- IndomethacinDokument9 SeitenIndomethacinQuiKe PvNoch keine Bewertungen
- OxytocinDokument2 SeitenOxytocinshefawNoch keine Bewertungen
- Warfarin Mechanism of ActionDokument7 SeitenWarfarin Mechanism of ActionIna GrigorasNoch keine Bewertungen
- CyclophosphamideDokument2 SeitenCyclophosphamideksumanpharma8801Noch keine Bewertungen
- Antibiotics.: Prepared by L.Mbise OCTOBER 2012Dokument40 SeitenAntibiotics.: Prepared by L.Mbise OCTOBER 2012Moses MberwaNoch keine Bewertungen
- Zyloprim Drug CardDokument1 SeiteZyloprim Drug CardSheri490Noch keine Bewertungen
- PrevacidDokument1 SeitePrevacidAdrianne BazoNoch keine Bewertungen
- Diuretic Drugs PHMDokument36 SeitenDiuretic Drugs PHMshenae3Noch keine Bewertungen
- KetoconazoleDokument2 SeitenKetoconazoleMD. DELWAR HOSSAINNoch keine Bewertungen
- Ciprofloxacin CiproDokument1 SeiteCiprofloxacin CiproKristi WrayNoch keine Bewertungen
- Daptomycin (Cubicin)Dokument1 SeiteDaptomycin (Cubicin)Adrianne BazoNoch keine Bewertungen
- Pharma CardsDokument5 SeitenPharma CardsazancheNoch keine Bewertungen
- Macrobid, Macrodantin (Nitrofurantoin) Dosing, Indications, Interactions, Adverse Effects, and More 2 PDFDokument2 SeitenMacrobid, Macrodantin (Nitrofurantoin) Dosing, Indications, Interactions, Adverse Effects, and More 2 PDFNailis Sa'adahNoch keine Bewertungen
- Oxytocin (Pitocin) : Slide 1Dokument16 SeitenOxytocin (Pitocin) : Slide 1Kalesha JonesNoch keine Bewertungen
- Brunner CTEA CH 62Dokument6 SeitenBrunner CTEA CH 62Avani PatelNoch keine Bewertungen
- Vancomycin Protocol RQHRDokument15 SeitenVancomycin Protocol RQHRl1o2stNoch keine Bewertungen
- Antibiotics 9Dokument11 SeitenAntibiotics 9Beth Morales100% (1)
- See Full Prescribing Information For Complete Boxed WarningDokument43 SeitenSee Full Prescribing Information For Complete Boxed WarningParishan SaeedNoch keine Bewertungen
- PethidineDokument6 SeitenPethidineAnonymous NQDRERPcjNoch keine Bewertungen
- Aerovent, Apovent Atronase, Ipraxa, Ipvent Rhinovent, Rinatecrinovagos, Atrovent, Atrovent HfaDokument4 SeitenAerovent, Apovent Atronase, Ipraxa, Ipvent Rhinovent, Rinatecrinovagos, Atrovent, Atrovent HfaGwyn RosalesNoch keine Bewertungen
- Drug AdvilDokument1 SeiteDrug AdvilDiana Laura LeiNoch keine Bewertungen
- Dapsone PIDokument7 SeitenDapsone PInsucopyNoch keine Bewertungen
- InsulinDokument1 SeiteInsulinamaliea234Noch keine Bewertungen
- Cyclizine Hydrochloride - Summary of Product CharacteristicsDokument28 SeitenCyclizine Hydrochloride - Summary of Product CharacteristicsBrown and Burk UK LtdNoch keine Bewertungen
- Drug StudyDokument8 SeitenDrug StudyGian Era100% (1)
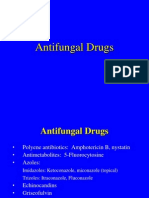
- Antifungal DrugsDokument20 SeitenAntifungal DrugsboeykhNoch keine Bewertungen
- Stimulates Peripheral Glucose Uptake, Inhibits Hepatic Glucose Production, Inhibits Lipolysis and Proteolysis, Regulating Glucose MetabolismDokument4 SeitenStimulates Peripheral Glucose Uptake, Inhibits Hepatic Glucose Production, Inhibits Lipolysis and Proteolysis, Regulating Glucose MetabolismKey CelestinoNoch keine Bewertungen
- ClindamycinDokument3 SeitenClindamycinShaira TanNoch keine Bewertungen
- OB Drug StudyDokument12 SeitenOB Drug StudyCj AttoNoch keine Bewertungen
- EzetimibeDokument3 SeitenEzetimibeapi-3797941Noch keine Bewertungen
- Drug Study (Pe)Dokument15 SeitenDrug Study (Pe)Jobelle AcenaNoch keine Bewertungen
- Drug StudyDokument11 SeitenDrug StudyJay VillasotoNoch keine Bewertungen
- (Generic Name) ® Drotaverine 40mgDokument2 Seiten(Generic Name) ® Drotaverine 40mgSangar Sardar100% (1)
- EMERGENCY DRUGS: A Drug StudyDokument8 SeitenEMERGENCY DRUGS: A Drug StudyShaine WolfeNoch keine Bewertungen
- MupirocinDokument13 SeitenMupirocinkurutalaNoch keine Bewertungen
- Sangobion Full Report v1Dokument18 SeitenSangobion Full Report v1aqibazizkhanNoch keine Bewertungen
- Drug StudyDokument16 SeitenDrug StudyJhann0% (1)
- Augmenten (Amoxicillin Clavulan)Dokument2 SeitenAugmenten (Amoxicillin Clavulan)Adrianne BazoNoch keine Bewertungen
- Mesalazine: Mesalazine (INN, BAN), Also Known As Mesalamine (USAN) or 5-Aminosalicylic AcidDokument4 SeitenMesalazine: Mesalazine (INN, BAN), Also Known As Mesalamine (USAN) or 5-Aminosalicylic AcidAnkan PalNoch keine Bewertungen
- Triamcinolone (Topical) - Drug InformationDokument5 SeitenTriamcinolone (Topical) - Drug InformationMauricio Sv0% (1)
- RevisionDokument17 SeitenRevisionMatt RenaudNoch keine Bewertungen
- DrugStudy MetoclopramideDokument2 SeitenDrugStudy MetoclopramideAshknee Khainna AlejoNoch keine Bewertungen
- Tiotropium BromideDokument2 SeitenTiotropium BromidejulieNoch keine Bewertungen
- Antiemetics: Dr. Bikram TewariDokument31 SeitenAntiemetics: Dr. Bikram TewariRajkamal SarmaNoch keine Bewertungen
- HyoscineDokument4 SeitenHyoscineHana HanaNoch keine Bewertungen
- Omeprazole, Potassium Chloride, Citicoline, GlimepirideDokument5 SeitenOmeprazole, Potassium Chloride, Citicoline, GlimepirideJenivic Empig PuedanNoch keine Bewertungen
- Generic Name: BudesonideDokument8 SeitenGeneric Name: BudesonidemeangelmeNoch keine Bewertungen
- RetinaDokument1 SeiteRetinaggalicinaoNoch keine Bewertungen
- Beneficence NonmaleficenceDokument1 SeiteBeneficence NonmaleficenceggalicinaoNoch keine Bewertungen
- PneumoniaDokument4 SeitenPneumoniaggalicinaoNoch keine Bewertungen
- ReferenceDokument2 SeitenReferenceggalicinaoNoch keine Bewertungen
- Beneficence NonmaleficenceDokument1 SeiteBeneficence NonmaleficenceggalicinaoNoch keine Bewertungen
- Problem SetDokument2 SeitenProblem SetggalicinaoNoch keine Bewertungen
- Theoretical Analysis of The FamilyDokument2 SeitenTheoretical Analysis of The Familyggalicinao0% (1)
- Thyroid GlandDokument7 SeitenThyroid GlandggalicinaoNoch keine Bewertungen
- Rerum NovarumDokument2 SeitenRerum NovarumggalicinaoNoch keine Bewertungen
- Surgical Safety ChecklistDokument2 SeitenSurgical Safety ChecklistggalicinaoNoch keine Bewertungen
- Pediatric Community Acquired PneumoniaDokument50 SeitenPediatric Community Acquired PneumoniaggalicinaoNoch keine Bewertungen
- Review of Systems (Pedia) : Skin, Hair, & Nails Mouth, Oropharynx, NoseDokument3 SeitenReview of Systems (Pedia) : Skin, Hair, & Nails Mouth, Oropharynx, NoseggalicinaoNoch keine Bewertungen
- Maternal and Child Health: 2001 Nepal Demographic and Health Survey Ministry of Health, New ERA, ORC MacroDokument36 SeitenMaternal and Child Health: 2001 Nepal Demographic and Health Survey Ministry of Health, New ERA, ORC MacroWardiati YusufNoch keine Bewertungen
- Sauces BabyDokument1 SeiteSauces BabyggalicinaoNoch keine Bewertungen
- EpiDokument5 SeitenEpiMarie Dinah SalvinoNoch keine Bewertungen
- Environmental SanitationDokument46 SeitenEnvironmental SanitationggalicinaoNoch keine Bewertungen
- Water and Sanitation ProjectDokument27 SeitenWater and Sanitation ProjectggalicinaoNoch keine Bewertungen
- ImmunDokument1 SeiteImmunggalicinaoNoch keine Bewertungen
- HistoryDokument4 SeitenHistoryggalicinaoNoch keine Bewertungen
- EconomicsDokument8 SeitenEconomicsggalicinaoNoch keine Bewertungen
- Foundation Engineering - Building Construction - Equipment RentalDokument2 SeitenFoundation Engineering - Building Construction - Equipment RentalggalicinaoNoch keine Bewertungen
- 32321Dokument45 Seiten32321Atika AkbariNoch keine Bewertungen
- Polsci Lec 1Dokument38 SeitenPolsci Lec 1ggalicinaoNoch keine Bewertungen
- EconomicsDokument8 SeitenEconomicsggalicinaoNoch keine Bewertungen
- A Brief History of Data CommunicationsDokument13 SeitenA Brief History of Data Communicationsggalicinao0% (1)
- Patterns of KnowingDokument9 SeitenPatterns of KnowingggalicinaoNoch keine Bewertungen
- Benign Paratesticlar Cyst - A Mysterical FindingDokument2 SeitenBenign Paratesticlar Cyst - A Mysterical FindingInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Kidney CancerDokument6 SeitenKidney CancerAKHILNoch keine Bewertungen
- Normal Microbial Flora of The Human BodyDokument12 SeitenNormal Microbial Flora of The Human BodyJustinNoch keine Bewertungen
- LAB 4 - StreptococcusDokument31 SeitenLAB 4 - Streptococcussajad abasNoch keine Bewertungen
- English XIIDokument12 SeitenEnglish XIIdanielNoch keine Bewertungen
- Youst TryingDokument5 SeitenYoust TryingVictoria Campos GonzálezNoch keine Bewertungen
- History of Nursing and The Development of The ProfessionDokument4 SeitenHistory of Nursing and The Development of The Professionastraia celesteNoch keine Bewertungen
- UntitledDokument75 SeitenUntitledMelissa DrakeNoch keine Bewertungen
- COVID 19 Guideline To Resume Paediatric Dental Services in MalaysiaDokument29 SeitenCOVID 19 Guideline To Resume Paediatric Dental Services in MalaysiaEnrita DianNoch keine Bewertungen
- Cyclooxygenase PathwayDokument8 SeitenCyclooxygenase PathwayIradatullah SuyutiNoch keine Bewertungen
- Rubber Dam Isolation For Endodontic Treatment in Difficult Clinical SituationsDokument8 SeitenRubber Dam Isolation For Endodontic Treatment in Difficult Clinical SituationsDavid ColonNoch keine Bewertungen
- Urtica Urens William Boericke Cyrus Maxwell Bogar Adolf Zur Lippe John Henry ClarkeDokument9 SeitenUrtica Urens William Boericke Cyrus Maxwell Bogar Adolf Zur Lippe John Henry ClarkeShah FaisalNoch keine Bewertungen
- Drug InteractionsDokument11 SeitenDrug InteractionssamNoch keine Bewertungen
- How Does Global Warming Affect Our Living?Dokument19 SeitenHow Does Global Warming Affect Our Living?Minahil QaiserNoch keine Bewertungen
- Understanding Cancer Treatment and OutcomesDokument5 SeitenUnderstanding Cancer Treatment and OutcomesMr. questionNoch keine Bewertungen
- Python Ieee Projects 2021 - 22 JPDokument3 SeitenPython Ieee Projects 2021 - 22 JPWebsoft Tech-HydNoch keine Bewertungen
- Mag MicroDokument67 SeitenMag MicroAneesh AyinippullyNoch keine Bewertungen
- Makabuhay IpDokument7 SeitenMakabuhay IpButterflyCalmNoch keine Bewertungen
- Negative IonDokument2 SeitenNegative IonDekzie Flores MimayNoch keine Bewertungen
- Genetic Recombination in Bacteria Horizon of The BDokument9 SeitenGenetic Recombination in Bacteria Horizon of The BAngelo HernandezNoch keine Bewertungen
- Prof. Eman Rushdy Sulphonylurea A Golden Therapy For DiabetesDokument51 SeitenProf. Eman Rushdy Sulphonylurea A Golden Therapy For Diabetestorr123Noch keine Bewertungen
- 6 Months Creditors Aging Reports: PT Smart Glove Indonesia As of 30 Sept 2018Dokument26 Seiten6 Months Creditors Aging Reports: PT Smart Glove Indonesia As of 30 Sept 2018Wagimin SendjajaNoch keine Bewertungen