Beruflich Dokumente
Kultur Dokumente
Endophthalmitis
Hochgeladen von
Ar JayCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Endophthalmitis
Hochgeladen von
Ar JayCopyright:
Verfügbare Formate
7/7/13
Endophthalmitis
Medscape Reference Reference
News Reference Education MEDLINE
Endophthalmitis
Author: Daniel J Egan, MD; Chief Editor: Robert E O'Connor, MD, MPH more... Updated: May 6, 2013
Background
Endophthalmitis is an inflammatory condition of the intraocular cavities (ie, the aqueous and/or vitreous humor) usually caused by infection. Noninfectious (sterile) endophthalmitis may result from various causes such as retained native lens material after an operation or from toxic agents. Panophthalmitis is inflammation of all coats of the eye including intraocular structures.
Severe endophthalmitis. Image courtesy of Joan W. Miller, MD, and Mehran Afshari, MD, Massachusetts Eye and Ear Infirmary, Boston, Mass.
The 2 types of endophthalmitis are endogenous (ie, metastatic) and exogenous. Endogenous endophthalmitis results from the hematogenous spread of organisms from a distant source of infection (eg, endocarditis). Exogenous endophthalmitis results from direct inoculation of an organism from the outside as a complication of ocular surgery, foreign bodies, and/or blunt or penetrating ocular trauma.
Pathophysiology
Under normal circumstances, the blood-ocular barrier provides a natural resistance against invading organisms. In endogenous endophthalmitis, blood-borne organisms (seen in patients who are bacteremic in situations such as endocarditis) permeate the blood-ocular barrier either by direct invasion (eg, septic emboli) or by changes in vascular endothelium caused by substrates released during infection. Destruction of intraocular tissues may be due to direct invasion by the organism and/or from inflammatory mediators of the immune response.
emedicine.medscape.com/article/799431-overview 1/5
7/7/13
Endophthalmitis
Endophthalmitis may be as subtle as white nodules on the lens capsule, iris, retina, or choroid. It can also be as ubiquitous as inflammation of all the ocular tissues, leading to a globe full of purulent exudate. In addition, inflammation can spread to involve the orbital soft tissue. Any surgical procedure that disrupts the integrity of the globe can lead to exogenous endophthalmitis (eg, cataract, glaucoma, retinal, radial keratotomy, intravitreal injections).
Epidemiology
Frequency
United States Endogenous endophthalmitis is rare, occurring in only 2-15% of all cases of endophthalmitis. Average annual incidence is about 5 per 10,000 hospitalized patients. In unilateral cases, the right eye is twice as likely to become infected as the left eye, probably because of its more proximal location to direct arterial blood flow from the right innominate artery to the right carotid artery. Since 1980, candidal infections reported in IV drug users have increased. The number of people at risk may be increasing because of the spread of AIDS, more frequent use of immunosuppressive agents, and more invasive procedures (eg, bone marrow transplantation). Most cases of exogenous endophthalmitis (about 60%) occur after intraocular surgery. When surgery is implicated in the cause, endophthalmitis usually begins within 1 week after surgery. In the United States, postcataract endophthalmitis is the most common form, with approximately 0.1-0.3% of operations having this complication, which has increased over the last 3 years.[1] Although this is a small percentage, large numbers of cataract operations are performed each year making the chances that physicians may encounter this infection higher. Endophthalmitis may also occur after intravitreal injections, although this risk in an analysis of over 10,000 injections is estimated at 0.029% per injection.[2] Posttraumatic endophthalmitis occurs in 4-13% of all penetrating ocular injuries. Incidence of endophthalmitis with perforating injuries in rural settings is higher when compared with nonrural settings.[3] Delay in the repair of a penetrating globe injury is correlated with increased risk of developing endophthalmitis.[4] Incidence of endophthalmitis with retained intraocular foreign bodies is 7-31%.
Mortality/Morbidity
Decreased vision and permanent loss of vision are common complications of endophthalmitis. Patients may require enucleation to eradicate a blind and painful eye. Mortality is related to the patient's comorbidities and the underlying medical problem, especially when considering the etiology of hematogenous spread in endogenous infections.
Age
An association appears to exist between the development of endophthalmitis in cataract surgery and age greater than or equal to 85 years.[5]
Contributor Information and Disclosures
Author Daniel J Egan, MD Associate Attending Physician, Associate Residency Director, Department of Emergency Medicine, St Luke's Roosevelt Hospital Center; Assistant Professor of Clinical Medicine, Columbia University College of Physicians and Surgeons Daniel J Egan, MD is a member of the following medical societies: Alpha Omega Alpha, American College of Emergency Physicians, and Society for Academic Emergency Medicine Disclosure: Nothing to disclose.
emedicine.medscape.com/article/799431-overview 2/5
7/7/13
Endophthalmitis
Coauthor(s) Jessica Radin Peters MD, Attending Physician, Urgent Care Center, Newton-Wellesley Hospital Jessica Radin Peters is a member of the following medical societies: American College of Emergency Physicians, Massachusetts Medical Society, and Society for Academic Emergency Medicine Disclosure: Nothing to disclose. David A Peak, MD Assistant Residency Director of Harvard Affiliated Emergency Medicine Residency, Attending Physician, Massachusetts General Hospital; Consulting Staff, Department of Hyperbaric Medicine, Massachusetts Eye and Ear Infirmary David A Peak, MD is a member of the following medical societies: American College of Emergency Physicians, American Medical Association, Society for Academic Emergency Medicine, and Undersea and Hyperbaric Medical Society Disclosure: Pfizer Salary Employment Specialty Editor Board Richard Lavely, MD, JD, MS, MPH Lecturer in Health Policy and Administration, Department of Public Health, Yale University School of Medicine Richard Lavely, MD, JD, MS, MPH is a member of the following medical societies: American College of Emergency Physicians, American College of Legal Medicine, and American Medical Association Disclosure: Nothing to disclose. Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference Disclosure: Medscape Salary Employment Douglas Lavenburg, MD Clinical Professor, Department of Emergency Medicine, Christiana Care Health Systems Douglas Lavenburg, MD is a member of the following medical societies: American Society of Cataract and Refractive Surgery Disclosure: Nothing to disclose. John D Halamka, MD, MS Associate Professor of Medicine, Harvard Medical School, Beth Israel Deaconess Medical Center; Chief Information Officer, CareGroup Healthcare System and Harvard Medical School; Attending Physician, Division of Emergency Medicine, Beth Israel Deaconess Medical Center John D Halamka, MD, MS is a member of the following medical societies: American College of Emergency Physicians, American Medical Informatics Association, Phi Beta Kappa, and Society for Academic Emergency Medicine Disclosure: Nothing to disclose. Chief Editor Robert E O'Connor, MD, MPH Professor and Chair, Department of Emergency Medicine, University of Virginia Health System Robert E O'Connor, MD, MPH is a member of the following medical societies: American Academy of Emergency Medicine, American College of Emergency Physicians, American College of Physician Executives, American Heart Association, American Medical Association, Medical Society of Delaware, National Association of EMS Physicians, Society for Academic Emergency Medicine, and Wilderness Medical Society
emedicine.medscape.com/article/799431-overview 3/5
7/7/13
Endophthalmitis
Disclosure: Nothing to disclose.
References
1. Taban M, Behrens A, Newcomb RL. Acute endophthalmitis following cataract surgery: a systematic review of the literature. Arch Ophthalmol. May 2005;123(5):613-20. [Medline]. 2. Englander M, Chen TC, Paschalis EI, Miller JW, Kim IK. Intravitreal injections at the Massachusetts Eye and Ear Infirmary: analysis of treatment indications and postinjection endophthalmitis rates. Br J Ophthalmol. Apr 2013;97(4):460-5. [Medline]. 3. Boldt HC, Pulido JS, Blodi CF, Folk JC, Weingeist TA. Rural endophthalmitis. Ophthalmology. Dec 1989;96(12):1722-6. [Medline]. 4. Thompson JT, Parver LM, Enger CL, Mieler WF, Liggett PE. Infectious endophthalmitis after penetrating injuries with retained intraocular foreign bodies. National Eye Trauma System. Ophthalmology. Oct 1993;100(10):1468-74. [Medline]. 5. Lundstrom M, Wejde G, Stenevi U, Thorburn W, Montan P. Endophthalmitis after cataract surgery: a nationwide prospective study evaluating incidence in relation to incision type and location. Ophthalmology. May 2007;114(5):866-70. [Medline]. 6. Ness T, Pelz K, Hansen LL. Endogenous endophthalmitis: microorganisms, disposition and prognosis. Acta Ophthalmol Scand. Dec 2007;85(8):852-6. [Medline]. 7. Connell PP, O'Neill EC, Fabinyi D, et al. Endogenous endophthalmitis: 10-year experience at a tertiary referral centre. Eye (Lond). Jan 2011;25(1):66-72. [Medline]. [Full Text]. 8. Han DP, Wisniewski SR, Wilson LA, et al. Spectrum and susceptibilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am J Ophthalmol. Jul 1996;122(1):1-17. [Medline]. 9. Stein JD, Grossman DS, Mundy KM, Sugar A, Sloan FA. Severe adverse events after cataract surgery among medicare beneficiaries. Ophthalmology. Sep 2011;118(9):1716-23. [Medline]. [Full Text]. 10. Melo GB, Bispo PJ, Regatieri CV, Yu MC, Pignatari AC, Hofling-Lima AL. Incidence of endophthalmitis after cataract surgery (2002-2008) at a Brazilian university-hospital. Arq Bras Oftalmol. Dec 2010;73(6):505-7. [Medline]. 11. Alfaro DV, Roth D, Liggett PE. Posttraumatic endophthalmitis. Causative organisms, treatment, and prevention. Retina. 1994;14(3):206-11. [Medline]. 12. Miller JJ, Scott IU, Flynn HW Jr, et al. Endophthalmitis caused by Bacillus species. Am J Ophthalmol. May 2008;145(5):883-8. [Medline]. 13. Verbraeken H, Rysselaere M. Post-traumatic endophthalmitis. Eur J Ophthalmol. Jan-Mar 1994;4(1):1-5. [Medline]. 14. Faghihi H, Hajizadeh F, Esfahani MR, et al. Posttraumatic endophthalmitis: report No. 2. Retina. Jan 2012;32(1):146-51. [Medline]. 15. Gupta A, Srinivasan R, Gulnar D, Sankar K, Mahalakshmi T. Risk factors for post-traumatic endophthalmitis in patients with positive intraocular cultures. Eur J Ophthalmol. Jul-Aug 2007;17(4):642-7. [Medline]. 16. Kohanim S, Daniels AB, Huynh N, Eliott D, Chodosh J. Utility of ocular ultrasonography in diagnosing infectious endophthalmitis in patients with media opacities. Semin Ophthalmol. Sep-Nov 2012;27(56):242-5. [Medline]. 17. Ng JQ, Morlet N, Pearman JW, et al. Management and outcomes of postoperative endophthalmitis since
emedicine.medscape.com/article/799431-overview 4/5
7/7/13
Endophthalmitis
the endophthalmitis vitrectomy study: the Endophthalmitis Population Study of Western Australia (EPSWA)'s fifth report. Ophthalmology. Jul 2005;112(7):1199-206. [Medline]. 18. Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. Dec 1995;113(12):1479-96. [Medline]. 19. Albert DM, ed; Jakobiec FA. Endogenous endophthalmitis. In: Principles and Practice of Ophthalmology. Vol 5. W B Saunders Co; 1994:3120-3125. 20. Albert DM, Jakobiec FA. Postoperative endophthalmitis. In: Principles and Practice of Ophthalmology. W B Saunders Co; 2000:2441-2462. 21. Mandelbaum S, Forster RK. Postoperative endophthalmitis. Int Ophthalmol Clin. Summer 1987;27(2):95106. [Medline]. 22. Michelson JB, Friedlaender MH. Endophthalmitis of drug abuse. Int Ophthalmol Clin. Summer 1987;27(2):120-6. [Medline]. 23. Okada AA, Johnson RP, Liles WC. Endogenous bacterial endophthalmitis. Report of a ten-year retrospective study. Ophthalmology. May 1994;101(5):832-8. [Medline]. 24. Parrish CM, O'Day DM. Traumatic endophthalmitis. Int Ophthalmol Clin. 1987;27(2):112-9. [Medline]. 25. Rowsey JJ, Jensen H, Sexton DJ. Clinical diagnosis of endophthalmitis. Int Ophthalmol Clin. Summer 1987;27(2):82-8. [Medline]. 26. Uka J, Minamoto A, Shimizu R. A five-year review of patients admitted with the diagnosis of bacterial endophthalmitis. Hiroshima J Med Sci. Jun 2005;54(2):47-51. [Medline]. 27. Wilhelmus KR. The pathogenesis of endophthalmitis. Int Ophthalmol Clin. Summer 1987;27(2):74-81. [Medline]. 28. Wilson FM 2d. Causes and prevention of endophthalmitis. Int Ophthalmol Clin. Summer 1987;27(2):67-73. [Medline]. 29. Wong JS, Chan TK, Lee HM, Chee SP. Endogenous bacterial endophthalmitis: an east Asian experience and a reappraisal of a severe ocular affliction. Ophthalmology. Aug 2000;107(8):1483-91. [Medline]. Medscape Reference 2011 WebMD, LLC
emedicine.medscape.com/article/799431-overview
5/5
Das könnte Ihnen auch gefallen
- Course Outline:: Basic Accounting Principles and Financial ConceptsDokument2 SeitenCourse Outline:: Basic Accounting Principles and Financial ConceptsAr JayNoch keine Bewertungen
- Format of ReportDokument3 SeitenFormat of ReportAr JayNoch keine Bewertungen
- Region II Trauma Center Monthly Consumption ReportDokument2 SeitenRegion II Trauma Center Monthly Consumption ReportAr JayNoch keine Bewertungen
- List of Quality IndicatorsDokument2 SeitenList of Quality IndicatorsAr JayNoch keine Bewertungen
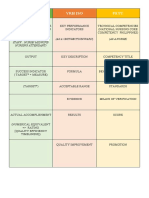
- CSC SPMS PDFDokument56 SeitenCSC SPMS PDFAr JayNoch keine Bewertungen
- Daily Performance Output ReportDokument5 SeitenDaily Performance Output ReportAr JayNoch keine Bewertungen
- Medical Supply Monitoring SheetDokument3 SeitenMedical Supply Monitoring SheetAr JayNoch keine Bewertungen
- Census Remark Code Task Q E T: Surgical Intensive Care UnitDokument1 SeiteCensus Remark Code Task Q E T: Surgical Intensive Care UnitAr JayNoch keine Bewertungen
- Medical and Office Equipment Fuctionality Monitoring SheetDokument3 SeitenMedical and Office Equipment Fuctionality Monitoring SheetAr JayNoch keine Bewertungen
- Emergency Drug Monitoring SheetDokument3 SeitenEmergency Drug Monitoring SheetAr JayNoch keine Bewertungen
- Form Daily Individual Performance Management ChecklistDokument4 SeitenForm Daily Individual Performance Management ChecklistAr JayNoch keine Bewertungen
- Level III Evaluation - Behavioral LevelDokument2 SeitenLevel III Evaluation - Behavioral LevelAr JayNoch keine Bewertungen
- PArts Please PrintDokument1 SeitePArts Please PrintAr JayNoch keine Bewertungen
- CompetencyDokument7 SeitenCompetencyAr JayNoch keine Bewertungen
- List of Quality IndicatorsDokument2 SeitenList of Quality IndicatorsAr JayNoch keine Bewertungen
- Infection Control RiskDokument2 SeitenInfection Control RiskAr JayNoch keine Bewertungen
- CSC SPMS PDFDokument56 SeitenCSC SPMS PDFAr JayNoch keine Bewertungen
- Civil Service VRH Iso Petu: (As Individual Staff Nurse/ Midwife/ Nursing Attendant) (As A Unit/Section/Ward) (As A Nurse)Dokument1 SeiteCivil Service VRH Iso Petu: (As Individual Staff Nurse/ Midwife/ Nursing Attendant) (As A Unit/Section/Ward) (As A Nurse)Ar JayNoch keine Bewertungen
- b1 FinelliDokument42 Seitenb1 FinelliAr JayNoch keine Bewertungen
- Ipcr Kabisote Ob orDokument2 SeitenIpcr Kabisote Ob orAr JayNoch keine Bewertungen
- Introductory Article - OPDDokument1 SeiteIntroductory Article - OPDAr JayNoch keine Bewertungen
- Com-Spms Form No. 3 (Ipcr) : (Please Add Rows If Necessary)Dokument3 SeitenCom-Spms Form No. 3 (Ipcr) : (Please Add Rows If Necessary)Ar Jay100% (13)
- Department of SurgeryDokument2 SeitenDepartment of SurgeryAr Jay100% (1)
- Quality IndicatorsDokument152 SeitenQuality IndicatorsAr JayNoch keine Bewertungen
- Etoshow QuityDokument8 SeitenEtoshow QuityAr JayNoch keine Bewertungen
- Surgical Intensive Care Unit-Nuerovital Signs Monitoring ToolDokument1 SeiteSurgical Intensive Care Unit-Nuerovital Signs Monitoring ToolAr JayNoch keine Bewertungen
- Quality IndicatorsDokument45 SeitenQuality IndicatorsAr JayNoch keine Bewertungen
- Assessing A PatientDokument1 SeiteAssessing A PatientAr JayNoch keine Bewertungen
- Rheumatic Heart DiseaseDokument21 SeitenRheumatic Heart DiseaseAr JayNoch keine Bewertungen
- Give Psychological Support To The Patient and FamilyDokument2 SeitenGive Psychological Support To The Patient and FamilyNílo StárnNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Urology ST3 Portfolio Self-Assessment Guidance 2018Dokument6 SeitenUrology ST3 Portfolio Self-Assessment Guidance 2018kaNoch keine Bewertungen
- Robert G. Gish, MD Full Curriculum Vitae & Biography - Updated January 2015Dokument231 SeitenRobert G. Gish, MD Full Curriculum Vitae & Biography - Updated January 2015Robert G. Gish, MDNoch keine Bewertungen
- Orthopedic Surgery Complete IMG ListDokument153 SeitenOrthopedic Surgery Complete IMG ListF AbdullaNoch keine Bewertungen
- Regulations and Rules For MRCPCH and DCH ExaminationsDokument18 SeitenRegulations and Rules For MRCPCH and DCH ExaminationsSyed Danish AliNoch keine Bewertungen
- INICET July 22 Result MDMS - MDS For WebsiteDokument565 SeitenINICET July 22 Result MDMS - MDS For WebsiteSwetha pugazhNoch keine Bewertungen
- UntitledDokument955 SeitenUntitledمزاجية المودNoch keine Bewertungen
- MCQ Sin Medical Physiology 1Dokument2 SeitenMCQ Sin Medical Physiology 1priyaNoch keine Bewertungen
- Faculty Registration Details HistoryDokument3 SeitenFaculty Registration Details HistorySunny Kashyap0% (1)
- List of Candidates Selected For PG DEGREE /DIPLOMA / 6yr M.Ch. (NEURO SURGERY) 2012 - 2013 SESSION ON 16/05/2012Dokument7 SeitenList of Candidates Selected For PG DEGREE /DIPLOMA / 6yr M.Ch. (NEURO SURGERY) 2012 - 2013 SESSION ON 16/05/2012Reuben JosephNoch keine Bewertungen
- Health Family Welfare 3Dokument225 SeitenHealth Family Welfare 3Gopala Sundararaj SNoch keine Bewertungen
- Final Govt MD Ms PG Dip Mds 2016Dokument37 SeitenFinal Govt MD Ms PG Dip Mds 2016rahulNoch keine Bewertungen
- PIMS AICET PG II BrochureDokument53 SeitenPIMS AICET PG II BrochureAnweshaBoseNoch keine Bewertungen
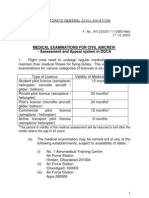
- Medical - Appeal Procedure DGCADokument6 SeitenMedical - Appeal Procedure DGCAБисвас АнупамNoch keine Bewertungen
- Ed 304 Catiag FinalDokument34 SeitenEd 304 Catiag FinalDEXTER LLOYD CATIAGNoch keine Bewertungen
- Booklet For PHMC (Revised)Dokument24 SeitenBooklet For PHMC (Revised)Govt Ayurvedic Teaching Hospital WarangalNoch keine Bewertungen
- ASTMH Diploma Course List 8 - 19Dokument10 SeitenASTMH Diploma Course List 8 - 19saurabh pandeyNoch keine Bewertungen
- Self-Reported Dental Student Stressors and ExperiencesDokument8 SeitenSelf-Reported Dental Student Stressors and ExperiencesVíctor RodríguezNoch keine Bewertungen
- Full Download Ebook Ebook PDF Nelson Essentials of Pediatrics 8th Edition PDFDokument41 SeitenFull Download Ebook Ebook PDF Nelson Essentials of Pediatrics 8th Edition PDFdavid.anderson198100% (37)
- Obstetricia y Ginecología Beckman 8a EdicionDokument477 SeitenObstetricia y Ginecología Beckman 8a EdicionAlejandro Mora100% (2)
- ProspectusDokument52 SeitenProspectusRabinder BakhshiNoch keine Bewertungen
- The Malaysian Qualifications Framework PDFDokument39 SeitenThe Malaysian Qualifications Framework PDFDsgSyedNasRul100% (1)
- Physical Medicine & Rehabilitation - Randall BraddomDokument1.482 SeitenPhysical Medicine & Rehabilitation - Randall BraddomSimona Chirică90% (10)
- EndocrinologyDokument31 SeitenEndocrinologyDevi VaraNoch keine Bewertungen
- Critical Care of Children With Heart Disease 2010Dokument735 SeitenCritical Care of Children With Heart Disease 2010Haikel Mhamed100% (1)
- Orthopaedic Rehabilitation of The Athlete Getting Back in Game 1st Edition Ebook PDF VersionDokument62 SeitenOrthopaedic Rehabilitation of The Athlete Getting Back in Game 1st Edition Ebook PDF Versionkevin.smart540100% (42)
- Xavier BrochureDokument20 SeitenXavier BrochureJohn PareraNoch keine Bewertungen
- Avery's Diseases of The Newborn, Eleventh Edition - 2024Dokument1.849 SeitenAvery's Diseases of The Newborn, Eleventh Edition - 2024Brillence M SammyNoch keine Bewertungen
- DME AP Recruitment 2021 Notification For 326 Assistant Professor Posts Apply OnlineDokument6 SeitenDME AP Recruitment 2021 Notification For 326 Assistant Professor Posts Apply OnlineRajesh K KumarNoch keine Bewertungen
- Neuropsychology in IndiaDokument16 SeitenNeuropsychology in IndiaRahula RakeshNoch keine Bewertungen
- Doctors Blank CV TemplateDokument10 SeitenDoctors Blank CV TemplateMostafa ElkaramanyNoch keine Bewertungen