Beruflich Dokumente
Kultur Dokumente
Pathophysio of Heart Failure
Hochgeladen von
Yhr YhOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pathophysio of Heart Failure
Hochgeladen von
Yhr YhCopyright:
Verfügbare Formate
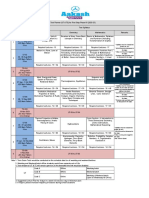
Pathophysiology of Heart Failure
The pathophysiology of heart failure involves changes in
cardiac function neurohumoral status systemic vascular function blood volume integration of cardiac and vascular changes
Cardiac dysfunction precipitates changes in vascular function, blood volume, and neurohumoral status. These changes serve as compensatory mechanisms to help maintain cardiac output (primarily by the Frank-Starling mechanism) and arterial blood pressure (by systemic vasoconstriction). However, these compensatory changes over months and years can worsen cardiac function. Therefore, some of the most effective treatments for chronic heart failure involve modulating non-cardiac factors such as arterial and venous pressures by administering vasodilator and diuretic drugs.
Cardiac Function
Overall, the changes in cardiac function associated with heart failure result in a decrease in cardiac output. This results from a decline in stroke volume that is due to systolic dysfunction, diastolic dysfunction, or a combination of the two. Briefly, systolic dysfunction results from a loss of intrinsic inotropy (contractility), most likely due to alterations in signal transduction mechanisms responsible for regulating inotropy. Systolic dysfunction can also result from the loss of viable, contracting muscle as occurs following acute myocardial infarction. Diastolic dysfunction refers to the diastolic properties of the ventricle and occurs when the ventricle becomes less compliant (i.e., "stiffer"), which impairs ventricular filling. Both systolic and diastolic dysfunction result in a higher ventricular end-diastolic pressure, which serves as a compensatory mechanism by utilizing the FrankStarling mechanism to augment stroke volume. In some types of heart failure (e.g., dilated cardiomyopathy), the ventricle dilates as preload pressures increase in order to to recruit the Frank-Starling mechanism in an attempt to maintain normal stroke volumes. Therapeutic interventions to improve cardiac function in heart failure include the use of cardiostimulatory drugs (e.g., beta-agonists and digitalis) that stimulate
heart rate and contractility, and vasodilator drugs that reduce ventricular afterload and thereby enhance stroke volume.
Neurohumoral Status
Neurohumoral responses include activation of sympathetic nerves and the reninangiotensin system, and increased release of antidiuretic hormone (vasopressin) and atrial natriuretic peptide. The net effect of these neurohumoral responses is to produce arterial vasoconstriction (to help maintain arterial pressure), venous constriction (to increase venous pressure), and increased blood volume. In general, these neurohumoral responses can be viewed as compensatory mechanisms, but they can also aggravate heart failure by increasing ventricular afterload (which depresses stroke volume) and increasing preload to the point where pulmonary or systemic congestion and edema occur. Therefore, it is important to understand the pathophysiology of heart failure because it serves as the rationale for drug therapy. There is also evidence that other factors such as nitric oxide and endothelin (both of which are increased in heart failure) may play a role in the pathogenesis of heart failure. Some drug treatments for heart failure involve attenuating the neurohumoral changes. For example, certain beta-blockers have been shown to provide significant long-term benefit, quite likely because they block the effects of excessive sympathetic activation on the heart. Angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and aldosterone receptor antagonists are commonly used to treat heart failure by inhibiting the actions of the reninangiotensin-aldosterone system.
Systemic Vascular Function
In order to compensate for reduced cardiac output during heart failure, feedback mechanisms within the body try to maintain normal arterial pressure by constricting arterial resistance vessels through activation of the sympathetic adrenergic nervous system, thereby increasing systemic vascular resistance. Veins are also constricted to elevate venous pressure. Arterial baroreceptors are important components of this feedback system. Humoral activation, particularly the renin-angiotensin system and antidiuretic hormone (vasopressin) also contribute to systemic vasoconstriction. Heightened sympathetic activity, and increased circulating angiotensin II and increased vasopressin contribute to an increase in systemic vascular resistance. Drugs that block some of these mechanisms, such angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, improve ventricular stroke volume by reducing afterload on the ventricle. Arterial and venous dilators such as hydralazine and sodium nitroprusside are also used to reduce afterload on the ventricle.
Blood Volume
In heart failure, there is a compensatory increase in blood volume that serves to increase ventricular preload and thereby enhance stroke volume by the FrankStarling mechanism. Blood volume is augmented by a number of factors. Reduced renal perfusion results in decreased urine output and retention of fluid. Furthermore, a combination of reduced renal perfusion and sympathetic activation of the kidneys stimulates the release of renin, thereby activating the renin-angiotensin system. This, in turn, enhances aldosterone secretion. There is also an increase in circulating arginine vasopressin (antidiuretic hormone) that contributes to renal retention of water. The final outcome of humoral activation is an increase in renal reabsorption of sodium and water. The resultant increase in blood volume helps to maintain cardiac output; however, the increased volume can be deleterious because it raises venous pressures, which can lead to pulmonary and systemic edema. When edema occurs in the lungs, this can result in exertional dyspnea (shortness of breath during exertion). Therefore, most patients in heart failure are treated with diuretic drugs to reduce blood volume and venous pressures in order to reduce edema.
Integration of Cardiac and Vascular Changes
As described above, both systolic and diastolic heart failure lead to changes in systemic vascular resistance, blood volume, and venous pressures. These changes can be examined graphically by using cardiac and vascular function curves as shown below. The decrease in cardiac performance causes a downward shift in the slope of the cardiac function curve. This alone would lead to an increase in right atrial or central venous pressure (point B) as well as a large decrease in cardiac output. The increase in blood volume and venoconstriction (decreased venous compliance) causes a parallel shift to the right of the systemic vascular function curve (point C). Because systemic vascular resistance also increases, the slope of the vascular function curve shifts downward (point D). These changes in vascular function, coupled with the downward shift in the cardiac function curve, result in a large increase in right atrial or central venous pressure, which helps to partially offset the large decline in cardiac output that would occur in the absence of the systemic vascular responses. Therefore, the systemic responses help to compensate for the loss of cardiac performance; however, this compensation is at the expense of a large increase in venous pressure that can lead to edema and at the expense of an increase in systemic vascular resistance that increases the afterload on the left ventricle, which can further depress its output.
Measurement of Cardiac Output
Several direct and indirect techniques for measurement of cardiac output are available. The thermodilution technique uses a special thermistor-tipped catheter (Swan-Ganz catheter) that is inserted from a peripheral vein into the pulmonary artery. A cold saline solution of known temperature and volume is injected into the right atrium from a proximal catheter port. The injectate mixes with the blood as it passes through the ventricle and into the pulmonary artery, thus cooling the blood. The blood temperature is measured by a thermistor at the catheter tip, which lies within the pulmonary artery, and a computer is used to acquire the thermodilution profile; that is, the computer quantifies the change in blood temperature as it flows over the thermistor surface. The cardiac output computer then calculates flow (cardiac output from the right ventricle) using the blood temperature information, and the temperature and volume of the injectate. The injection is normally repeated a few times and the cardiac output averaged. Because cardiac output changes with respiration, it is important inject the saline at a consistent time point during the respiratory cycle. In normal practice this is done at the end of expiration.
Echocardiographic techniques and radionuclide imaging techniques can be used to estimate real-time changes in ventricular dimensions, thus computing stroke volume, which when multiplied by heart rate, gives cardiac output. An old technique based on the Fick Principle can be used to compute cardiac output (CO) indirectly from whole body oxygen consumption (VO2) and the mixed venous (O2ven) and arterial oxygen contents (O2art); however, this technique is seldom used. The CO is calculated as follows:
CO = VO2/(O2art O2ven)
To calculate CO, the oxygen contents of arterial and venous blood samples are measured, and at the same time, whole body oxygen consumption is measured by analyzing expired air. The blood contents of oxygen are expressed as ml O2/ml blood, and the VO2 is expressed in units of ml O2/min. If O2art and O2ven contents are 0.2 ml and 0.15 ml O2/ml blood, respectively, and VO2 is 250 ml O2/minute, then CO = 5000 ml/min, or 5 L/min. Ventricular stroke volume would simply be the cardiac output divided by the heart rate.
Control of Heart Rate
Heart rate is normally determined by the pacemaker activity of the sinoatrial node (SA node) located in the posterior wall of the right atrium. The SA node exhibits automaticity that is determined by spontaneous changes in Ca++, Na+, and K+ conductances. This intrinsic automaticity, if left unmodified by neurohumoral factors, exhibits a spontaneous firing rate of 100-115 beats/min. This intrinsic firing rate decreases with age. Heart rate is decreased below the intrinsic rate primarily by activation of the vagus nerve innervating the SA node. Normally, at rest, there is significant vagal tone on the SA node so that the resting heart rate is between 60 and 80 beats/min. This vagal influence can be demonstrated by administration of atropine, a muscarinic receptor antagonist, which leads to a 20-40 beats/min increase in heart rate depending upon the initial level of vagal tone. For heart rate to increase above the intrinsic rate, there is both a withdrawal of vagal tone and an activation of sympathetic nerves innervating the SA node. This reciprocal change in sympathetic and parasympathetic activity permits heart rate to increase during exercise, for example. Heart rate is also modified by circulating catecholamines acting via 1adrenoceptors located on SA nodal cells. Heart rate is also modified by changes in circulating thyroxin (thyrotoxicosis causes tachycardia) and by changes in body core temperature (hyperthermia increases heart rate). SA nodal dysfunction can lead to sinus bradycardia, sinus tachycardia, or sicksinus syndrome. The maximal heart rate that can be achieved in an individual is estimated by
Maximal Heart Rate 220 beats/min age in years
Therefore a 20-year-old person will have a maximal heart rate of about 200 beats/min, and this will decrease to about 170 beats/min when the person is 50 years of age. This maximal heart rate is genetically determined and cannot be modified by exercise training or by external factors.
Regulation of Stroke Volume
Ventricular stroke volume (SV) is the difference between the ventricular enddiastolic volume (EDV) and the end-systolic volume (ESV). The EDV is the filled volume of the ventricle prior to contraction and the ESV is the residual volume of blood remaining in the ventricle after ejection. In a typical heart, the EDV is about 120 ml of blood and the ESV about 50 ml of blood. The difference in these two volumes, 70 ml, represents the SV. Therefore, any factor that alters either the EDV or the ESV will change SV.
SV = EDV - ESV
For example, an increase in EDV increases SV, whereas an increase in ESV decreases SV. There are three primary mechanisms that regulate EDV and ESV, and therefore SV. Preload Changes in preload affect the SV through the Frank-Starling mechanism. Briefly, an increase in venous return to the heart increases the filled volume (EDV) of the ventricle, which stretches the muscle fibers thereby increasing their preload. This leads to an increase in the force of ventricular contraction and enables the heart to eject the additional blood that was returned to it. Therefore, an increase in EDV results in an increase in SV. Conversely, a decrease in venous return and EDV leads to a decrease in SV by this mechanism.
Afterload Afterload is related to the pressure that the ventricle must generate in order to eject blood into the aorta. Changes in afterload affect the ability of the ventricle to eject blood and thereby alter ESV and SV. For example, an increase in afterload (e.g., increased aortic pressure) decreases SV, and causes ESV to increase. Conversely, a decrease in afterload augments SV and decreases ESV. It is important to note, however, that the SV in a normal, non-diseased ventricle is not strongly influenced by afterload. In contrast, the SV of hearts that are failing are very sensitive to changes in afterload. Inotropy Changes in ventricular inotropy (contractility) alter the rate of ventricular pressure development, thereby affecting ESV and SV. For example, an increase in inotropy (e.g., produced by sympathetic activation of the heart) increases SV and decreases ESV. Conversely, a decrease in inotropy (e.g., heart failure) reduces SV and increases ESV. It is important to note that the effects of changes in EDV and ESV on SV are not independent. For example, an increase in ESV usually results in a compensatory increase in EDV. Furthermore, if SV is increased by increasing EDV, this can lead to a small increase in ESV because of the influence of increased afterload on ESV caused by an increase in aortic pressure. Therefore, while the primary effect of a change in preload, afterload or inotropy may be on either EDV or ESV, secondary changes can occur that can partially compensate for the initial change in SV. For a more detailed description of these interactions, see the web pages describing preload, afterload, or inotropy.
Systolic Dysfunction
Systolic dysfunction refers to impaired ventricular contraction. In chronic heart failure, this is most likely due to changes in the signal transduction mechanisms regulating cardiac excitation-contraction coupling. The loss of cardiac inotropy (i.e., decreased contractility) causes a downward shift in the Frank-Starling curve (Figure 1). This results in a decrease in stroke volume and a compensatory rise in preload (often measured as ventricular end-diastolic pressure or pulmonary capillary wedge pressure). The rise in preload is considered compensatory because it activates the Frank-Starling mechanism to help maintain stroke volume despite the loss of inotropy. If preload did not rise, the decline in stroke volume would be even greater for a given loss of inotropy. Depending upon the precipitating cause of the heart failure, there will be ventricular hypertrophy, dilation, or a combination of the two.
The effects of a loss of intrinsic inotropy on stroke volume, and end-diastolic and end-systolic volumes, are best depicted using ventricular pressure-volume loops (Figure 2). Loss of intrinsic inotropy decreases the slope of the endsystolic pressure-volume relationship (ESPVR). This leads to an increase in endsystolic volume. There is also an increase in end-diastolic volume (compensatory increase in preload), but this increase is not as great as the increase in endsystolic volume. Therefore, the net effect is a decrease in stroke volume (shown as a decrease in the width of the pressure-volume loop). Because stroke volume decreases and end-diastolic volume increases, there is a substantial reduction in ejection fraction (EF). Stroke work (area within loop) is also decreased.
The force-velocity relationship provides insight as to why a loss of contractility causes a reduction in stroke volume (Figure 3). Briefly, at any given preload and afterload, a loss of inotropy results in a decrease in the shortening velocity of cardiac fibers. Because there is only a finite period of time available for ejection, a reduced velocity of ejection results in less blood ejected per stroke. The residual volume of blood within the ventricle is increased (increased end-systolic volume) because less blood is ejected. The reason for preload rising as inotropy declines is that the increased end-systolic volume is added to the normal venous return filling the ventricle. For example, if end-systolic volume is normally 50 ml of blood and it is increased to 80 ml in failure, this extra residual volume is added to the incoming venous return leading to an increase in end-diastolic volume and pressure. An important and deleterious consequence of systolic dysfunction is the rise in end-diastolic pressure. If the left ventricle is involved, then left atrial and pulmonary venous pressures will also rise. This can lead to pulmonary congestion and edema. If the right ventricle is in systolic failure, the increase in end-diastolic pressure will be reflected back into the right atrium and systemic venous vasculature. This can lead to peripheral edema and ascites. Treatment for systolic dysfunction involves the use of inotropic drugs, afterload reducing drugs, venous dilators, and diuretics. Inotropic drugs include digitalis (commonly used in chronic heart failure) and drugs that stimulate the heart via beta-adrenoceptor activation or inhibition of cAMP-dependent phosphodiesterase (used in acute failure). Afterload reducing drugs (e.g., arterial vasodilators) augment ventricular ejection by increasing the velocity of fiber shortening (see force-velocity relationship). Venous dilators and diuretics are used to reduce ventricular preload and venous pressures (pulmonary and systemic) rather than augmenting systolic function directly.
Diastolic Dysfunction
Ventricular function is highly dependent upon preload as
demonstrated by the Frank-Starling relationship. Therefore, if ventricular filling (preload) is impaired, this will lead to a decrease in stroke volume. The term "diastolic dysfunction" refers to changes in ventricular diastolic properties that have an adverse effect on stroke volume. About 50% of heart failure patients have diastolic dysfunction, with or without normal systolic function as determined by normal ejection fractions.
Ventricular filling (i.e., end-diastolic volume and hence sarcomere length) depends upon the venous return and the compliance of the ventricle during diastole. A reduction in ventricular compliance, as occurs in ventricular hypertrophy, will result in less ventricular filling (decreased end-diastolic volume) and a greater end-diastolic pressure (and pulmonary capillary wedge pressures) as shown to the right by changes in the ventricular pressure-volume loop. Stroke volume, therefore, will decrease. Depending on the relative change in stroke volume and end-diastolic volume, there may or may not be a small decrease in ejection fraction. Because stroke volume is decreased, there will also be a decrease in ventricular stroke work. A second mechanism can also contribute to diastolic dysfunction: impaired ventricular relaxation (reduced lusitropy). Near the end of the cycle of excitation-contraction coupling in the myocyte, the sarcoplasmic reticulum actively sequesters Ca++ so that the concentration of Ca++ in the vicinity of troponin-C is reduced allowing the Ca++ to leave its binding sites on the troponin-C and thereby permit disengagement of actin from myosin. This is a necessary step to achieve rapid and complete relaxation of the myocyte. If this mechanism is impaired (e.g., by reduced rate of Ca++ uptake by the sarcoplasmic reticulum), or by other mechanisms that contribute to myocyte relaxation, then the rate and perhaps the extent of relaxation are decreased. This will reduce the rate of ventricular filling, particularly during the phase of rapid filling. An important and deleterious consequence of diastolic dysfunction is the rise in end-diastolic pressure. If the left ventricle is involved, then left atrial and pulmonary venous pressures will also rise. This can lead to pulmonary congestion and edema. If the right ventricle is in diastolic failure, the increase in end-diastolic pressure will be reflected back into the right atrium and systemic venous vasculature. This can lead to peripheral edema and ascites. The rise in venous pressures also occur because of an increase in blood volume due to activation of the renin-angiotensin-aldosterone system, which causes renal retention of sodium and water. Therefore, diuretic drugs are commonly given to patients in diastolic failure; however, care must be taken not to reduce blood volume too much because elevated venous pressures are needed to fill the less compliance ventricle.
Das könnte Ihnen auch gefallen
- NetBank - TransactionsDokument1 SeiteNetBank - TransactionsYhr YhNoch keine Bewertungen
- Pathophysiology On ArrhythmiaDokument34 SeitenPathophysiology On ArrhythmiaYhr Yh100% (1)
- Pathophysiology of Myocardial InfarctionDokument4 SeitenPathophysiology of Myocardial InfarctionYhr YhNoch keine Bewertungen
- Robin Goh: This Is To Certify ThatDokument1 SeiteRobin Goh: This Is To Certify ThatYhr YhNoch keine Bewertungen
- The Pale Yellow in The Aorta Are The Earliest Lesion of AtherosclerosisDokument1 SeiteThe Pale Yellow in The Aorta Are The Earliest Lesion of AtherosclerosisYhr YhNoch keine Bewertungen
- Hyperlipidaemias (MRCP+ Step 1)Dokument2 SeitenHyperlipidaemias (MRCP+ Step 1)Yhr YhNoch keine Bewertungen
- Bets - DunningrDokument5 SeitenBets - DunningrYhr YhNoch keine Bewertungen
- CP 111Dokument246 SeitenCP 111Yhr YhNoch keine Bewertungen
- CCCCDokument1 SeiteCCCCYhr YhNoch keine Bewertungen
- Reviewer's Report Title: Cutaneous Squamous Cell Carcinoma Metastatic To Parotid - Analysis ofDokument2 SeitenReviewer's Report Title: Cutaneous Squamous Cell Carcinoma Metastatic To Parotid - Analysis ofYhr YhNoch keine Bewertungen
- Microsoft Word - Choice of Superannuation Fund Form - HESTADokument2 SeitenMicrosoft Word - Choice of Superannuation Fund Form - HESTAYhr YhNoch keine Bewertungen
- JVPDokument5 SeitenJVPYhr YhNoch keine Bewertungen
- Orientation - Booklet DeclarationDokument1 SeiteOrientation - Booklet DeclarationYhr YhNoch keine Bewertungen
- Fair Work Information Statement Acknowledgement FormDokument1 SeiteFair Work Information Statement Acknowledgement FormYhr YhNoch keine Bewertungen
- Feasibidlity For AustraliaDokument13 SeitenFeasibidlity For AustraliaYhr YhNoch keine Bewertungen
- LBU F VL MR9 VehicleTransferDokument6 SeitenLBU F VL MR9 VehicleTransferYhr YhNoch keine Bewertungen
- HESTA Product Disclosure Statement September 2012Dokument28 SeitenHESTA Product Disclosure Statement September 2012Yhr YhNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Fundamental Rights-Right To Equality, Prohibition of Discrimination, Right To Equality of OpportunityDokument76 SeitenFundamental Rights-Right To Equality, Prohibition of Discrimination, Right To Equality of OpportunityutkarshNoch keine Bewertungen
- Practice Test 4 For Grade 12Dokument5 SeitenPractice Test 4 For Grade 12MAx IMp BayuNoch keine Bewertungen
- Apache Hive Essentials 2nd PDFDokument204 SeitenApache Hive Essentials 2nd PDFketanmehta4u0% (1)
- Forever Living Presentation PDFDokument34 SeitenForever Living Presentation PDFCasey Rion100% (1)
- UT & TE Planner - AY 2023-24 - Phase-01Dokument1 SeiteUT & TE Planner - AY 2023-24 - Phase-01Atharv KumarNoch keine Bewertungen
- Jesus Died: Summary: Jesus Died We Need To Have No Doubt About That. Without Jesus' Death We Would Have NoDokument6 SeitenJesus Died: Summary: Jesus Died We Need To Have No Doubt About That. Without Jesus' Death We Would Have NoFabiano.pregador123 OliveiraNoch keine Bewertungen
- GN No. 444 24 June 2022 The Public Service Regulations, 2022Dokument87 SeitenGN No. 444 24 June 2022 The Public Service Regulations, 2022Miriam B BennieNoch keine Bewertungen
- 1E Star Trek Customizable Card Game - 6 First Contact Rule SupplementDokument11 Seiten1E Star Trek Customizable Card Game - 6 First Contact Rule Supplementmrtibbles100% (1)
- Counselling Goes To The Movies: Antwone Fisher (2002)Dokument12 SeitenCounselling Goes To The Movies: Antwone Fisher (2002)Azizul MohamadNoch keine Bewertungen
- Druze ScriptureDokument15 SeitenDruze ScriptureChristopher DeMott100% (2)
- Book of Dynamic Assessment in Practice PDFDokument421 SeitenBook of Dynamic Assessment in Practice PDFkamalazizi100% (1)
- La Navassa Property, Sovereignty, and The Law of TerritoriesDokument52 SeitenLa Navassa Property, Sovereignty, and The Law of TerritoriesEve AthanasekouNoch keine Bewertungen
- A2B1 Unit 11bDokument2 SeitenA2B1 Unit 11bTheToan.Noch keine Bewertungen
- Influencing Factors Behind The Criminal Attitude: A Study of Central Jail PeshawarDokument13 SeitenInfluencing Factors Behind The Criminal Attitude: A Study of Central Jail PeshawarAmir Hamza KhanNoch keine Bewertungen
- Analog Electronic CircuitsDokument2 SeitenAnalog Electronic CircuitsFaisal Shahzad KhattakNoch keine Bewertungen
- A Guide To Relativity BooksDokument17 SeitenA Guide To Relativity Bookscharles luisNoch keine Bewertungen
- Accounting 110: Acc110Dokument19 SeitenAccounting 110: Acc110ahoffm05100% (1)
- 19 Amazing Benefits of Fennel Seeds For SkinDokument9 Seiten19 Amazing Benefits of Fennel Seeds For SkinnasimNoch keine Bewertungen
- Springfield College Lesson Plan Template PHED 237: The Learning and Performance of Physical ActivitiesDokument5 SeitenSpringfield College Lesson Plan Template PHED 237: The Learning and Performance of Physical Activitiesapi-285421100Noch keine Bewertungen
- Insung Jung An Colin Latchem - Quality Assurance and Acreditatión in Distance Education and e - LearningDokument81 SeitenInsung Jung An Colin Latchem - Quality Assurance and Acreditatión in Distance Education and e - LearningJack000123Noch keine Bewertungen
- Complete PDFDokument495 SeitenComplete PDFMárcio MoscosoNoch keine Bewertungen
- Lead Workplace CommunicationDokument55 SeitenLead Workplace CommunicationAbu Huzheyfa Bin100% (1)
- Fansubbers The Case of The Czech Republic and PolandDokument9 SeitenFansubbers The Case of The Czech Republic and Polandmusafir24Noch keine Bewertungen
- Service and Maintenance Manual AFPX 513 PDFDokument146 SeitenService and Maintenance Manual AFPX 513 PDFManuel Amado Montoya AgudeloNoch keine Bewertungen
- 206f8JD-Tech MahindraDokument9 Seiten206f8JD-Tech MahindraHarshit AggarwalNoch keine Bewertungen
- Djordje Bubalo BiografijaDokument12 SeitenDjordje Bubalo BiografijaМилан КрстићNoch keine Bewertungen
- Percy Bysshe ShelleyDokument20 SeitenPercy Bysshe Shelleynishat_haider_2100% (1)
- ''Want To Learn To Speak Latin or Greek This (2018) Summer''Dokument10 Seiten''Want To Learn To Speak Latin or Greek This (2018) Summer''ThriwNoch keine Bewertungen
- Quarter 3 Week 6Dokument4 SeitenQuarter 3 Week 6Ivy Joy San PedroNoch keine Bewertungen
- Algebra. Equations. Solving Quadratic Equations B PDFDokument1 SeiteAlgebra. Equations. Solving Quadratic Equations B PDFRoberto CastroNoch keine Bewertungen