Beruflich Dokumente
Kultur Dokumente
Laryngeal and Tracheal Stents
Hochgeladen von
DrTarek Mahmoud Abo KammerCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Laryngeal and Tracheal Stents
Hochgeladen von
DrTarek Mahmoud Abo KammerCopyright:
Verfügbare Formate
Laryngeal and Tracheal Stents Treatment & Management
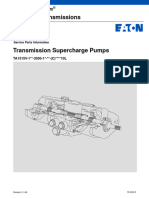
Background Laryngeal and tracheal stents are solid or hollow absorbable or nonabsorbable tubes of various shapes, sizes, and materials. Stents are used as primary treatment for lumen collapse or to stabilize a reconstructive effort of the larynx or trachea to prevent collapse. Stents can be used for the larynx and the trachea individually, or they can be used interchangeably or concomitantly. This article reviews (1) various laryngeal, tracheal, and combination stents; (2) disease processes for which stents are used; and (3) new stent designs.
An image depicting laryngeal and tracheal stents can be seen below.
History of the Procedure
For excellent patient education resources, see eMedicineHealth's patient education article Bronchoscopy.
Side view of a Montgomery laryngeal stent.
The word stent is derived from Charles B. Stent, a British dentist who practiced in the late 19th century. Stent developed material that was used for dental impressions and, later, to support skin grafts. In current practice, the word stent refers to material that supports some form of tissue against collapse. Most often, stent describes devices that maintain the lumens of tubular organs. In 1965, Montgomery described the use of silicone prostheses for tracheal stenting. Surgeons in other subspecialties, such as gastroesophageal, genitourinary, and vascular surgery, developed stents that remain useful in expanding lumens in these areas. This evolution increased the interest of otolaryngologists to develop stents for the larynx and tracheobronchial tree. Problem See the Indications section. Indications Laryngeal stents are often used to keep the airway expanded after surgical reconstruction or trauma. Occasionally, laryngeal stents can be used for expansion of a disease process. Stents can be used for similar reasons in the trachea,
especially to maintain lumen patency to prevent death. Stenting in the tracheobronchial tree is usually used as a last resort for severe conditions such as recurrent carcinoma and severe tracheal collapse that results in periods of prolonged apnea.
The most common indication for laryngeal stenting follows reconstruction of laryngotracheal stenosis (LTS; see the Medscape Reference articles Glottic Stenosis and Subglottic Stenosis in Children). Laryngeal stents can be used to keep the laryngeal lumen open and the reconstruction supported and stable. Occasionally, laryngeal stents are used following trauma to the larynx resulting in laryngeal fracture or injury. Stenting may help maintain lumen patency and prevent mucosal lacerations from scarring. Laryngotracheal stenosis The first reason to use stents in cases of LTS is to support the larynx, typically with some form of autologous cartilage, after a reconstructive technique has been performed. A stent can be used to stabilize the cricoid plate once it has been divided anteriorly or posteriorly, with or without cartilage placement, to keep the complex in an expanded formation during healing. Stenting to help stabilize the laryngeal structure normally lasts for 2-6 weeks. Zalzal has showed that when a cartilage graft is inserted, the minimum time necessary for a posterior cricoid split to heal in a distracted manner is 2 weeks. If stenting is performed for a shorter duration, the graft may prolapse into the lumen.
For anterior graft placement only, stenting commonly lasts for a week or less, which usually occurs while a patient is endotracheally intubated in an intensive care unit (ICU). If the cartilage graft is made into a boat formation with flanges over the edge of the intraluminal portion of the graft, thus providing stabilization and preventing prolapse, see the images below, then ventilation with an endotracheal tube is not necessarily used for support but for protection of the airway while the edema resolves and the air leak around the reconstructive effort seals.
Note the diamond-shaped internal intraluminal component. The shape of the rib is seen on the reverse side of the carved-out diamond-shaped wound.
Another anterior graft with a diamond shape. Note that it is approximately 1.7 mm long. Again, the intraluminal site is seen facing up.
Laryngeal web or atresia
The second reason for stent placement in LTS repair is to counteract scar contraction. Theoretically, this requires stenting for a 6-month period. In general, guidelines to determine the duration of stenting depend on the consistency of the stenosis, the anatomical distortion of the disease process, and the stability of the reconstructive areas.
This helps prevent pneumomediastinum, pneumothorax, or both in concert. Often, a child can be extubated within a few days following surgery. With this graft design, a stent is not always required because the reconstructive area is already stabilized, provided no air leak has developed.
For a child with laryngeal web or atresia, a keel stent, shown below, is often placed to prevent the laryngeal web from reforming. Frequently, this stent is left in place for several weeks.
Tracheal lesions
Laryngeal keel.
The purpose of stenting for tracheal lesions varies from palliation, to cure, to stabilization while a reconstructive effort heals. In adults, primary cancer of the tracheobronchial tree or cancer from the head, neck, or chest that extends into the tracheobronchial tree frequently causes lumen compromise and airway obstruction.
The intraluminal component can be removed with laser treatment, mechanical debulking, electrocautery, brachytherapy, photodynamic therapy, or cryotherapy. A stent can then be placed to maintain the airway lumen following debridement to counteract collapse or edema. Alternatively, stents can be placed that help compress any lesion extending into the trachea or bronchi, without the need for debulking. Stents have been used successfully to palliate patients with inoperable bronchogenic cancer, primary tracheal tumors, and metastatic malignancies. Placing a stent in a patient with a terminal illness allows that patient to breathe comfortably and prevents death from asphyxiation. Tracheomalacia and bronchomalacia Tracheomalacia and bronchomalacia (sometimes called tracheobronchomalacia) may be primary or secondary in nature. These conditions usually occur in children, but they can be observed in adults. Tracheomalacia and bronchomalacia are termed primary if they arise from primary cartilage abnormalities of the trachea, such as immature formation of the cartilaginous rings in neonates or relapsing polychondritis in children and adults. Primary tracheomalacia is often observed with a tracheoesophageal fistula. Secondary tracheomalacia or bronchomalacia is caused by extrinsic compression from a structure in the mediastinum. These structures may be normal vascular structures (eg, aortic artery, heart) or abnormal vascular structures (eg, aortic arch ring, pulmonary artery sling, other congenital vascular abnormality). Additionally, secondary
tracheomalacia or bronchomalacia can be caused by mediastinal cysts or neoplasms, including teratomas, lymphomas, and neuroblastomas. Stenting of the trachea following surgical resection or reconstruction If tracheomalacia or stenosis occurs following the resection of lesions, stents can be placed in the trachea to prevent scarring or to provide support for the operated segment while it heals.
In most situations, surgical correction as primary treatment for a disease process is preferred to stenting alone because complications are decreased. However, situations arise in which patients cannot undergo formal corrective surgery, and stent placement is the only way to prevent a severe apneic event or death. Tracheal stents have been placed following unsuccessful tracheal repairs, postanastomotic stricture after sleeve resection for lung transplantation, and following malacia from infections such as tuberculosis. Following lesion excision Any time the airway is opened to excise a lesion of the larynx, a stent can be considered for stabilization, scar prevention, or airway protection while edema resolves and the area heals. Frequently, this requires several days of intubation in the ICU, with the endotracheal tube acting as a temporary stent.
Types of stents
Different stents have different indications. Types include primarily laryngeal stents, primarily tracheal stents, combination tracheal and laryngeal stents, and stents that can be used either in the larynx or trachea. Laryngeal stents If stenosis is confined to the larynx (ie, glottis, subglottis), stenting can be short- or long-term. Short-term stenting is defined as stenting for less than 6 weeks. Long-term stenting is defined as stenting for more than 6 weeks.
Place a short stent for 6 weeks or less because granulation tissue forms at the lower end of the stent above the tracheotomy, potentially leading to tracheal stenosis or collapse above the tracheotomy site. Use short-term stenting for stabilization of cartilage grafts following laryngotracheal reconstruction (LTR) and/or for separation of mucosal surfaces during healing following laryngeal trauma, repair of web formation or atresia, or excision of a laryngeal lesion. Stents for these indications include Aboulker stents, silicone stents, Montgomery laryngeal stents, endotracheal tubes, and laryngeal keels. See the images below.
Representative (noninclusive) sample demonstrating various sizes of Aboulker stents, ranging from 15 mm in diameter on the left to 3 mm in diameter on the right. These stents are hollow and coated with Teflon.
An end view of an Aboulker stent, showing the central opening. These stents are hollow and coated with Teflon.
Side view of a Montgomery laryngeal stent.
Occasionally, long-term stenting is required when the trachea above the tracheotomy tube requires stenting for either collapse or stenosis following reconstruction. In this case, a long stent wired to the trachea, shown in the images below, or a tracheal tube (T-tube), such as the Montgomery T-tube, shown below, can be used.
Laryngeal keel.
Radiographic lateral neck view of a long stent connected to a metal Jackson tracheotomy tube at the bright inferior portion of the picture. The stent is seen in the airway as an oblong translucent area, with a rim of opacification around it that extends up through the larynx. A thin wire is seen connecting the stent and the tracheotomy tube.
A long Aboulker stent wired to a metal Jackson tracheotomy tube. A Jackson tracheotomy tube wired to a long Aboulker stent.
Relevant Anatomy Larynx
Montgomery T-tube (7 mm) stent with caps.
When a laryngeal stent is necessary, place it through and above the true and false vocal cords or a significant distance below the true vocal cords. If the stent is placed directly under the true vocal cords, granulation tissue can form and scarring of the glottis can occur; if at all possible, avoid this problem because repair and correction of glottic stenosis is difficult. Trachea
In infants, the trachea is short. Thus, a tracheotomy tube can often stent the airway open itself, occasionally almost down to the carina. If this does not suffice, then other corrective measures must be performed for tracheomalacia in an infant. Contraindications Larynx Absolute contraindications for use of a laryngeal stent include patients who are medically unstable and not able to undergo general anesthesia or individuals who may have an allergic reaction to the material of a particular stent.
Relative contraindications include risks of particular stents in various patients that could result in a poor outcome or complications. Historically, concern has been voiced regarding use of the Montgomery T-tube in young children (see Montgomery stent). Trachea Absolute and relative contraindications for tracheal stents are similar to contraindications listed for laryngeal stents; however, tracheal stents are often used as a last resort to prevent death by asphyxiation when other measures have failed or are not feasible. Another relative contraindication is the placement of a nonabsorbable stent when other techniques are available. Imaging Studies The criterion standard for evaluating the larynx or the trachea is direct laryngoscopy and bronchoscopy. Fluoroscopy can be used to help define a narrowing of the trachea or abnormal radiographic appearance of the larynx. The diagnostic information yielded from fluoroscopy is inferior to that of direct laryngoscopy and bronchoscopy in the operating room (OR); however, radiopaque stents can be placed under fluoroscopic guidance in adults and children. Occasionally, an imaging study such as MRI, CT scan, or plain x-ray film helps in diagnosing laryngeal lesions that might require stenting or in defining the length of stenosis or malacia in the trachea.
Diagnostic Procedures
The criterion standard for evaluating the larynx and trachea is direct laryngoscopy and bronchoscopy. Using these tools, the segment that requires stenting can be defined. Histologic Findings Graft vascularization Most histological studies have been performed in animals. Concern has been raised that a stent could cause impaired lumen healing, increasing the complication rate; however, a study on 36 white rabbits that had tracheoplasty with autologous cartilage grafting with and without stents showed the rate of vascularization of the graft was equal among both groups and possibly slightly superior in the stented group at 10 days following insertion. Mucociliary transport The laryngotracheal mucociliary transport in guinea pigs with and without stenting was evaluated in studies conducted in 1997 and 2000 by S.Y. Lee of the Department of Otolaryngology, Taiwan University, Taiwan. In these studies, stenting appeared to preserve or increase the mucociliary function of laryngotracheal mucosa in the acute phase of stenting compared to mucosa without stenting.[1, 2]
Tracheal stents Histological evaluation has been accomplished with metal, silicone, and bioabsorbable stents.
For metal stents, the most common (eg, Palmaz stent) are placed intraluminally and are expanded with a balloon. One study reported that the stent was overgrown with tracheal epithelium; granulation tissue formation was the only complication cited. In experimental studies in cats, histological analysis revealed a mild inflammatory reaction with granulation tissue present in all animals in which the stent was not manipulated. When the stent was overexpanded, the reaction was more severe; epithelial ulceration that had sealed the lumen in most animals was noted.
In the same study, researchers opened and closed cats' tracheas with or without stent placement. Increased inflammatory reaction, granulation tissue, and epithelial damage were observed in animals with stents as opposed to control subjects without stents. Based on that study, the Palmaz stent, when used in a normal trachea on which an operation has not been performed, provokes only a very mild and clinically insignificant inflammatory reaction when appropriately expanded. However, once surgery has been performed on the trachea, the inciting inflammatory reaction can cause formation of granulation tissue. A study from Japan examined expandable metallic stents after tracheal patch reconstruction with omentoplasty. Polypoid granulation tissue developed at both ends of the metallic stent. Histologically, epithelium was regenerated in the patched area 4 weeks postoperatively; the patched area was covered with respiratory epithelium 12 weeks postoperatively.[3] Another study investigated the histocompatibility of 4 different types of material used to cover expandable Gianturco metallic stents in dogs: polypropylene mesh, silicone-covered mesh, polyester mesh, and expanded polytetrafluoroethylene. The polypropylene mesh appeared to be the most biocompatible of all the coverings and was histocompatible to the airway.[4]
For bioabsorbable and silicone stents, a comparison of bioabsorbable airway stents, shown in the images below, with a silicone airway stent and metallic stent was performed in Finland on rabbits.
Intraoperative picture showing a solid dissolvable airway stent next to a trachea in a 3-kg New Zealand white rabbit.
Surgical Therapy
Other experimental studies have been performed to evaluate histological events that occur when a bioabsorbable stent is placed, as compared with silicone stents. Silicone stents in one animal study again showed a tendency to become stenosed with encrusted material and to develop a hyperplastic bulge at both ends. Bioabsorbable stents of poly-Llactide material showed no foreign body reaction and had a tendency to penetrate into the tracheal wall. These stents had been reabsorbed at 10-month follow-up.
The bioabsorbable spiral stent was manufactured with self-reinforced poly-L-lactide material, and tracheomalacia was created by extramucosal resection of cartilaginous arches of the cervical trachea. Hyperplastic polyps occurred at both ends of the silicone stent, and the internal diameter of the stent became encrusted. The bioabsorbable stent and the metallic stents were tolerated well.
Solid spiral dissolvable stent produced for the trachea of a rabbit. Scale is in centimeters.
The placement of stents in the larynx or trachea is usually performed under anesthesia. Transcervical or transthoracic approaches provide exposure to place the stents under direct vision. Stents can be sutured in place or affixed in other ways. Depending on the clinical situation, laryngeal and tracheal stents can be placed transluminally under endoscopic view in the OR by a surgeon or they can be placed under fluoroscopic control in the radiology suite by a radiologist. Laryngeal stents
Aboulker stent o The most common stent used for stability following LTR in children is the Aboulker stent. In the early 1960s, Aboulker introduced this cigar-shaped prosthesis, which is available in several different outside diameters at a length of 120 mm, as in the image below. Aboulker originally used his stents in adults, after cricoid plate reconstructions. In the late 1960s, Aboulker used a stent to decannulate 3 of 5 children after airway reconstructions. In the early 1970s, Grahne, Cotton, and Crysdale also used this
stent following LTR in children.
Representative (noninclusive)
sample demonstrating various sizes of Aboulker stents, ranging from 15 mm in diameter on the left to 3 mm in diameter on the right. These stents are hollow and coated with Teflon. Zalzal noted that one of the benefits of the Aboulker stent is that the stent is made of highly polished Teflon, which minimizes irritation and granulation tissue formation compared with other stents.[5] However, the stent has been shown to cause some mucosal irritation, with granulation tissue formation occurring at the superior or inferior end. Not uncommonly, the base of the epiglottis is affected, and granulation tissue often forms in this area. The Aboulker stent has been shown effective for counteracting scar contracture and for keeping reconstructed areas stable during healing. Zalzal, Cotton, and others have had good success decannulating children with severe LTS using the Aboulker stent in association with LTR. The Aboulker stent can be used in both a short and long form. In the short form, the stent is used for 6 weeks or less and is placed in the larynx and upper trachea. As with all laryngeal stents, place it between the true and false vocal cords superiorly and suture it in place with a large Prolene stitch tied externally to the strap muscles. Place a portion of an angiocatheter or small feeding tube over this suture to decrease the chance of erosion through the strap muscles. Throw multiple knots for identification during later stent removal. The Aboulker stent can also be used in the long form. When the long form is used, suture the stent to a metal Holinger tracheotomy tube (Holinger T-tube); see the images below. Long stents are used when the suprastomal area needs support or when long-term stenting (ie, > 6 wk) is necessary. Long stents help prevent granulation tissue and secondary stenosis in the suprastomal area.
Radiographic lateral neck view of a long stent connected to a metal Jackson tracheotomy tube at the bright inferior portion of the picture. The stent is seen in the airway as an oblong translucent area, with a rim of opacification around it that extends up through the larynx.
A thin wire is seen connecting the stent and the tracheotomy tube.
o o
A long Aboulker stent wired to a metal Jackson tracheotomy tube. A Jackson tracheotomy tube wired to a long Aboulker stent.
Montgomery stent o The Montgomery T-tube, shown in the image below, is a silicone stent with a long center lumen and a smaller lumen projecting from the side of the stent at either a 90 or 75 angle. Ensure that the upper end extends through the true and false vocal cords. The lower end can extend all the way to the carina, depending on the length of the trachea and stent. The side lumen extends through the tracheostoma. If long-term stenting is required, this tube can be an alternative to a wired stent-tracheotomy complex.
The Montgomery T-tube has been used successfully to stent the adult larynx and trachea following reconstruction and to stent areas of malacia and stenosis. Concern exists regarding the safety of the stent in children because the internal diameter of the stent is small and the tube could become plugged with dried secretions, which could result in obstruction of the stent and could end in airway obstructive symptoms and death if not promptly removed. With an indwelling Montgomery T-tube, plug the side lumen as much as possible and intermittently perform proper suctioning to prevent plugging. Stern and Cotton evaluated the Montgomery T-tube in children, reporting on 26 children who underwent laryngeal procedures including LTR and cricotracheal resection.[6] Most of the stents used had lumens wider than 8 mm in diameter; only 1 had a diameter of 6 mm. Stern et al used the stents from 2 weeks to almost 2 years and did not observe increased granulation tissue formation in children who had stents for longer periods of time. The researchers concluded that the Montgomery T-tube is safe to use in children. In France, Froehlich et al used Montgomery T-tubes in 12 children for an average of 6 months and noted that complications include removal of the T-tube by the child, forward migration resulting in tube expulsion, formation of granulation tissue, and clogging.[7] Neither set of researchers reported deaths from stent malfunction.
Montgomery T-tube (7 mm) stent with caps.
Silastic sheet (Swiss roll) o This stent, shown in the image below, was reported by Evans in 1977 as a form of stenting for laryngotracheoplasty.[8] The silastic sheet was initially one of the main stents used following reconstructive efforts in children. The silastic sheet is rolled up and inserted into the larynx and upper trachea, where it is fixed in place with a suture. The roll has a constant tendency to unroll, producing general pressure on the mucosa. This pressure allows obliteration of any dead space and allows mucosal regeneration to occur. Because of its propensity to form granulation tissue, the silastic sheet was replaced by the Teflon Aboulker stent .
Tracheobronchial stents
Foam and a finger cot were used initially in the larynx, especially following acute laryngeal traumatic injuries. Most of these stents have been replaced by Aboulker stents, Montgomery T-tubes, or Montgomery laryngeal stents. Endotracheal tubes: Originally reported by Brick in 1970, the use of endotracheal tubes made from polyvinyl chloride was reported again from a series in India in 1995. These tubes were used to stent the laryngotracheal area following LTR. Fibrosis, inflammation, and granulation tissue occurred after 4 weeks. Brick believed these stents should only be used for 4 weeks or less to prevent permanent laryngeal damage. Silicone stents: Silicone stents used in the larynx have mainly been reported in adults. These stents are placed endoscopically after dilating the larynx up to 18 mm. If dilation does not enlarge the larynx enough to place the stent, carbon dioxide laser excision of the scar is occasionally performed to enlarge the subglottic stenosis. Suspend the patient in the OR, and place the stent through the vocal cords into the subglottis. Place an external stitch by passing it through the skin into the stent and then out to the skin again, and secure it in position. In adults, place stents 5-30 mm below the vocal folds. Complications and concerns of this stent include transient vocal fold edema, stent migration, and recurrence of stenosis following stent removal, which has occurred even after leaving stents for 11 months. Inflatable stents: Over the last few years, inflatable stents composed of a small balloon attached to a port to allow expansion with air have been evaluated at the Cleveland Clinic. These stents have been used only in experimental canine models.[9] Inflatable stents are inflated slowly and expanded over 3-46 days. Complications included small superficial ulceration of the true vocal cords, minor polypoid changes, and granulomas. Of these experimental dogs, 20-30% exhibited inflammation extending into the underlying cartilages. Based on this information, the stent was associated with minimum local tissue reaction. o
Roll of silastic sheeting.
Silicone stents were the first developed in the mid 1960s. Most studies report that the tracheal mucosa tolerates longterm use of these stents relatively well. Silicone stents can be left in place for several years and, generally, are easily removable. Because this stent has the propensity to slide well over the mucosa, stent migration is the most common problem. Metal stents are usually composed of a mesh and become incorporated into the mucosa, making them extremely difficult to remove in some cases.
Tracheobronchial stents can be broadly divided into metal or silicone stents. General differences exist between these 2 categories.
This same propensity for mucosa to grow around the metallic stents allows for better mucociliary clearance and function. Mucociliary flow is hindered by the silicone stents, which are mostly solid. Silicone stents are thicker than metallic stents and, thus, cause more restrictive airflow than the thin metal stents that can self-expand or be expanded to adhere closely to the tracheal wall. Additionally, metal stents have the potential to be expanded intermittently as the
airway enlarges or changes. Metal stents are more distensible and conform better to the airway than silicone stents, especially if the airway is somewhat tortuous.
Metal stents are easier to use in the distal trachea and bronchi because they are mesh and do not obstruct primary or secondary bronchi that come into contact with the side of the stent. A bronchus could become obstructed with a silicone stent, unless a port has been fashioned into the side of the stent. The Dumon stent, shown in the image below, comes with some stents open to the side.
Generally, more reaction and granulation tissue is seen with metallic stents than with silicone stents, although reports vary, some significantly. Metallic stents can be coated with various materials that seem to reduce the rate of granulation tissue formation.
Specific stents are discussed below. Metal stents include the categories of balloon- and self-expandable stents. Bioabsorbable stents are also discussed and compared.
Generally, both types of stents are structurally strong, and they resist forces that cause stent collapse. Metal stents are usually used in the radiological suite because they are radiopaque; silicone stents are used in the OR because they are radiolucent, do not expand, and generally require some type of affixation.
The Dumon stent with its opening for the right mainstem bronchus.
Balloon-expandable metallic stents o Palmaz stent This stent (Johnson & Johnson; New Brunswick, NJ and Interventional Systems; Warren, NJ) was initially developed as a vascular prosthesis. The Palmaz stent reportedly is the most common stent used in children, in part because of its small size. The stent consists of 150-m slotted stainless steel in a tubular mesh configuration with lengths varying from 10-40 mm. A balloon of 6- to 10-mm diameter fits inside the stent for manual expansion of as much as 6-12 mm. An appropriate size for expansion of the trachea and bronchi in children is 8 mm and 6 mm in diameter, respectively. After balloon expansion, the stent does not exert a continual outward pressure on the airway wall. The stent has been used in primary tracheomalacia or bronchomalacia, external compression of the trachea or bronchi, or collapse of the trachea or bronchi from previous surgery. Fraga et al from the Hospital for Sick Children in Toronto, Ontario, Canada, reported results in 16 patients who required 30 stents. Half of these patients had primary tracheomalacia, and all did well, with relief of symptoms following stent placement. The stents were easily removable, and granulation tissue was seen in approximately 20% of the group. Additionally, the children who required stenting following stenosis at the site of a previous surgical repair did well and underwent stent removal without complications, except for some granulation tissue. In the 4 children who had stents placed for external compression, 2 had stent migration and 1 had bronchial erosion. Three patients died of underlying cardiac disease, but stenting provided
good palliation of respiratory symptoms. Sommer and Forte believe use of this stent is the preferred management for significant tracheobronchomalacia in children. o Strecker stent This stent is made of a tantalum filament that is structured into a cylindrical wire mesh. The stent is flexible, whether compressed or expanded. When expanded, the stent does not change length. The Strecker stent is 2-4 cm long and can be expanded from 8 to 11 mm. This stent is being used successfully in tracheobronchial obstructions. Self-expanding metallic stents: These stents have "memory" that allows a return to normal shape after compression for placement in the airway. The device self-expands but occasionally requires balloon inflation for complete expansion. Self-expanding metallic stents include the Gianturco-Z (William Cook, Bjaeverskov, Denmark), the Wallstent (Boston Scientific; Natick, Mass), and the Nitinol. o Gianturco-Z stent Developed by Cesare Gianco in the 1980s, this stent was initially designed for stenting obstructions in the vascular system; it has been the most widely used of the expandable metallic stents in adults. The Gianturco-Z is composed of 460-m stainless steel filaments arranged in a zigzag configuration. The stent has been modified several times since initial development. One modification added small hooks to the outer perimeter to prevent migration, but they contributed to difficulty with stent removal. The diameter of the stent when expanded is 15-40 mm. The stent is available in 2- and 2.5-cm lengths. Two stents can be combined to double the length. The Gianturco-Z stent has been used to expand benign disease and with posterior anastomotic strictures, tracheal stenosis, and tracheobronchomalacia. The stent exerts good radial force and does not shorten when deployed, but it has a tendency to spring forward if released too quickly. Complications are sometimes reported and include breakdown or unraveling of the stent and fatal hemoptysis after erosion into the pulmonary artery 10 days after insertion. o Wallstent The Wallstent (Schneider; Minneapolis, Minn) is a stainless steel device composed of approximately 15-20 braided (100-m diameter) filaments. The filaments are arranged in a criss-cross fashion to form a cylindrical mesh. The individual alloy filaments make a precise number of turns to maintain the mesh pattern and are good in tortuous airways because they maintain shape. Stent diameters range from 6-25 mm; lengths range from 2-7 cm. Ensure that the diameter of the stent is at least 2 mm wider than the diameter measured at the proximal region of the normal airway. The stent exerts good radial force and good flexibility but shortens to 20-40% upon deployment. The Wallstent can be delivered with a rigid bronchoscope or flexible telescope. Initially, this stent had difficulty with tumor in-growth, and a silicone body covering was developed. An important advantage of this stent is the ability to cut small openings into the mesh of a stent that lies across bronchial openings. o Nitinol/InStent/Ultraflex stent This stent is thermally triggered and changes shape in response to temperature changes. This response is known as a Marmen effect and occurs in certain metals or alloys that distort at low temperatures (martensitic state) then revert to the original shape when reheated (austenitic state). The Nitinol wire is heated and made into a helical shape and is then cooled for deployment. With release into the target site, high body temperature causes the Nitinol stent to coil back to its original helical shape. Alternatively, a current of 1.5-3 amperes or 3-5 volts can be applied to this stent for 1-2 seconds to heat it to 40C, thus converting it to the fully expanded state. A group from Japan noted that Teflon coating of this stent decreased tissue reactivity. The stent was found to have poor visualization under fluoroscopy. Haeck compared this stent to the Strecker stent and found it preferable because of ease of use, greater flexibility, and faster deployment.
Silicone stents: Available stents include the Montgomery T-tube, Dumon (Novatech; Aubagne, France), Reynder (Reynder's Medical Supply; Lennik, Belgium), dynamic (Rusch AG; Duluth, Ga), Polyflex (Rusch AG; Duluth, Ga), and Nova (Novadis; Saint-Victoret, France). The Montgomery T-tube and laryngeal stents were discussed earlier. A form of the Montgomery T-tube can be extended to include the trachea and upper bronchi. o Dumon stent In the late 1980s, Dumon introduced a tracheobronchial stent that could be inserted through a bronchoscope. This stent is a cylindrical silicone stent with external studs placed at regular intervals to prevent stent migration and to reduce mucosal ischemia by limiting contact with the airway wall. The Dumon is the most widely used silicone stent. The stent is widely available in varying widths and lengths from 10-35 mm. Once placed in the airway, the stent can be adjusted with a forceps and bronchoscope. These stents have been used more commonly in the adult population. Dumon's series of 574 stents placed between 1987 and 1994 indicated the stents were tolerated for as long as years. The Dumon stent has a thick wall, but a thin-walled stent in pediatric sizes has been developed. o Reynder stent: This stent is a cylindrical silicone prosthesis that is more rigid than regular silicone tubes but requires a special introducer and a bronchoscope for placement. o Dynamic stent: The dynamic stent is a silicone Y-stent with anterior and lateral walls reinforced to simulate the tracheal wall. Special forceps are available for insertion within the rigid laryngoscope. o Polyflex: This device is a self-expandable stent made of polyester wire mesh within layers of silicone. o Novastent: The Novastent is a thin silicone sheet containing a small metallic hoop of Nitinol alloy. The silicone bands on the ends are designed to prevent migration. Bioabsorbable tracheal stents: Corpela from Finland described absorbable stents in animal models. These stents have been efficacious in preventing airway collapse in rabbit models and in created tracheomalacia, although no current publications report studies on the use of bioabsorbable stents in humans.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Rxexam'S Biostatistics Questions & Answers: 2019-2020 EditionDokument15 SeitenRxexam'S Biostatistics Questions & Answers: 2019-2020 EditionPrakash100% (2)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Indigo Airlines - Final ReportDokument22 SeitenIndigo Airlines - Final Reportanand_lihinarNoch keine Bewertungen
- The Development of The Middle Ear Spaces and Their Surgical SignificanceDokument15 SeitenThe Development of The Middle Ear Spaces and Their Surgical SignificanceDrTarek Mahmoud Abo Kammer100% (2)
- Hygiene PassportDokument133 SeitenHygiene PassportAsanga MalNoch keine Bewertungen
- Biostatistics A Sample of Questions For The Final ExamDokument3 SeitenBiostatistics A Sample of Questions For The Final ExamDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- BiostatisticsQUIZ AnswersDokument5 SeitenBiostatisticsQUIZ AnswersDipankar RoyNoch keine Bewertungen
- AP Statistics Final Examination Multiple-Choice Questions Answers in BoldDokument17 SeitenAP Statistics Final Examination Multiple-Choice Questions Answers in BoldDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Tympanoplasty 120522063636 Phpapp01Dokument29 SeitenTympanoplasty 120522063636 Phpapp01DrTarek Mahmoud Abo Kammer100% (1)
- Answers To Practice Exam 2Dokument3 SeitenAnswers To Practice Exam 2monerch JoserNoch keine Bewertungen
- StridorDokument3 SeitenStridorDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- PGRTPPTDokument95 SeitenPGRTPPTDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Practice Guidelines For Family Physicians 4 Infection by MansdocsDokument92 SeitenPractice Guidelines For Family Physicians 4 Infection by MansdocsDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Blood Supply of CochleaDokument2 SeitenBlood Supply of CochleaDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Cochlear Rotation and Its RelevanceDokument7 SeitenCochlear Rotation and Its RelevanceDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Cholesterol Granuloma of Maxillary SinusDokument6 SeitenCholesterol Granuloma of Maxillary SinusDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Rhinitis in InfancyDokument3 SeitenRhinitis in InfancyDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Eponymous Signs in ENTDokument11 SeitenEponymous Signs in ENTDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- CH 22 - Olfactory Function and DysfunctionDokument3 SeitenCH 22 - Olfactory Function and DysfunctionDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Courses in Ainshams - Doc Reviewed 2010 10Dokument1 SeiteCourses in Ainshams - Doc Reviewed 2010 10DrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Stridor 1Dokument5 SeitenStridor 1DrTarek Mahmoud Abo KammerNoch keine Bewertungen
- The Sistrunk ProcedureDokument4 SeitenThe Sistrunk ProcedureDrTarek Mahmoud Abo Kammer100% (1)
- CSF LeaksDokument3 SeitenCSF LeaksDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Anatomy of A Long BoneDokument4 SeitenAnatomy of A Long BoneDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Mastoidectomy and EpitympanectomyDokument18 SeitenMastoidectomy and EpitympanectomyDrTarek Mahmoud Abo KammerNoch keine Bewertungen
- Paper 2 With Solution MathematicsDokument17 SeitenPaper 2 With Solution MathematicsFaiz AhmadNoch keine Bewertungen
- Deva Surya - 19MF02Dokument30 SeitenDeva Surya - 19MF02SaravananNoch keine Bewertungen
- Sew Gear ReducerDokument772 SeitenSew Gear Reducerrahimi mohamadNoch keine Bewertungen
- 1.1 - Selectividad Acti9Dokument34 Seiten1.1 - Selectividad Acti9Bladimir MichelNoch keine Bewertungen
- TA1515VDokument4 SeitenTA1515VLeo LeiNoch keine Bewertungen
- CopernikDokument2 SeitenCopernikSinister JinNoch keine Bewertungen
- Caption Sheet 4-Kailynn BDokument4 SeitenCaption Sheet 4-Kailynn Bapi-549116310Noch keine Bewertungen
- Microscope MaintenanceDokument2 SeitenMicroscope MaintenanceCharlyn KeithNoch keine Bewertungen
- RA9275Dokument49 SeitenRA9275znarf_ryanNoch keine Bewertungen
- Scientific Exploration and Expeditions PDFDokument406 SeitenScientific Exploration and Expeditions PDFana_petrescu100% (2)
- Daoyin Physical Calisthenics in The Internal Arts by Sifu Bob Robert Downey Lavericia CopelandDokument100 SeitenDaoyin Physical Calisthenics in The Internal Arts by Sifu Bob Robert Downey Lavericia CopelandDragonfly HeilungNoch keine Bewertungen
- Volvo PDFDokument218 SeitenVolvo PDFNelio Lara Ricaldi0% (1)
- Basic Principles of Remote SensingDokument24 SeitenBasic Principles of Remote Sensingfelipe4alfaro4salas100% (1)
- TR189 Kathuria PDFDokument168 SeitenTR189 Kathuria PDFuqiNoch keine Bewertungen
- Diesel Rotary UPS Configurations V1 - 00 - Jan2008Dokument10 SeitenDiesel Rotary UPS Configurations V1 - 00 - Jan2008Karim SenhajiNoch keine Bewertungen
- 1 28701-FGC+101+3441+Router+6471+Datasheet+Rev+FDokument2 Seiten1 28701-FGC+101+3441+Router+6471+Datasheet+Rev+FВладимир ЕгоровNoch keine Bewertungen
- Guide To Greyhawk PDFDokument108 SeitenGuide To Greyhawk PDFAnonymous PtMxUHm9RoNoch keine Bewertungen
- 100 Yer PM PPM 0605Dokument40 Seiten100 Yer PM PPM 0605biplabpal2009Noch keine Bewertungen
- Panasonic Refrigeraor NR-B472TZ - B412TZ v1.1Dokument24 SeitenPanasonic Refrigeraor NR-B472TZ - B412TZ v1.1Anonymous 2iQ1B59Noch keine Bewertungen
- Cateora2ce IM Ch012Dokument9 SeitenCateora2ce IM Ch012Priya ShiniNoch keine Bewertungen
- Output Process Input: Conceptual FrameworkDokument4 SeitenOutput Process Input: Conceptual FrameworkCHRISTINE DIZON SALVADORNoch keine Bewertungen
- Mathematics For Engineers and Scientists 3 PDFDokument89 SeitenMathematics For Engineers and Scientists 3 PDFShailin SequeiraNoch keine Bewertungen
- Schneider Modicon M580 CatalogueDokument268 SeitenSchneider Modicon M580 CatalogueKhaerul Imam HermanNoch keine Bewertungen
- Diwali Pujan BookletDokument10 SeitenDiwali Pujan Bookletman_ishkumarNoch keine Bewertungen
- Electric Bike Monitoring and Controlling System Based On Internet of ThingsDokument8 SeitenElectric Bike Monitoring and Controlling System Based On Internet of ThingsEarl PhamtonhiveNoch keine Bewertungen
- Feature Writing EnglishDokument2 SeitenFeature Writing EnglishAldren BababooeyNoch keine Bewertungen
- CADS Revit Scia Engineer Link Best PracticesDokument32 SeitenCADS Revit Scia Engineer Link Best PracticestrevorNoch keine Bewertungen
- Modern Views Catalogue/Sotheby's BenefitDokument36 SeitenModern Views Catalogue/Sotheby's BenefitStudio AdjayeNoch keine Bewertungen