Beruflich Dokumente
Kultur Dokumente
Implications of The Prostate Intervention Versus Observation Trail (PIVOT)
Hochgeladen von
GeeleegoatOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Implications of The Prostate Intervention Versus Observation Trail (PIVOT)
Hochgeladen von
GeeleegoatCopyright:
Verfügbare Formate
Asian Journal of Andrology (2012) 14, 803804 2012 AJA, SIMM & SJTU.
. All rights reserved 1008-682X/12 $32.00
www.nature.com/aja
RESEARCH HIGHLIGHT
Implications of the prostate intervention versus observation trial (PIVOT)
Oliver Sartor
Asian Journal of Andrology (2012) 14, 803804; doi:10.1038/aja.2012.93; Published online: 10 September 2012
SA screening improves early detection of prostate cancer but can lead to overtreatment if all of these cancers are treated. The first randomized treatment study for men with PSA detected cancers has now been reported. The PIVOT (prostatectomy intervention versus observation trial) results are noteworthy. There were no overall or cancer-specific survival benefits from radical prostatectomy versus observation. This result was primarily driven by the largest subset, men with low risk prostate cancer (organ-confined, Gleason 6, and PSA ,10 ng ml-1). Even though men enrolled in PIVOT were older and sicker as compared to most radical prostatectomy series, there was a strong tendency toward improved prostate cancer specific survival for participants with a PSA .10 ng ml-1 or Gleason scores of 7 or higher. This important study underscores the benefits of observation for those with low risk prostate cancer and the potential benefits of surgery for those in higher risk categories. The first randomized trial of radical prostatectomy versus observation trial (PIVOT) performed in PSA screened patients has now been reported.1 The headline results indicate that neither overall survival nor prostate cancer-specific survival is prolonged by radical prostatectomy. This is an important study with many implications. The PIVOT study was not perfect by any means. Both the age at treatment (mean age: 67 years) and the non-prostate cancer mortality rate were quite high relative to other studies utilizing radical prostatectomy.2 Over 40% of patients died by 12 years after study enrollment and the vast majority of patients died from non-prostate cancer
Departments of Medicine and Urology, Tulane University School of Medicine, New Orleans, LA 70112, USA Correspondence: Dr O Sartor (osartor@tulane.edu)
causes. There was an explicit entry criterion that excluded patients with a less than 10-year life expectancy; however, the non-cancerous death rate at 10 years was much higher than I would have expected.2 Because the vast majority of the deaths in PIVOT within 10 years of treatment were not due to prostate cancer, it is clear that a very significant number of patients were too old or too sick at study entry to have benefited from radical prostatectomy. In truth, these patients should never have been enrolled on PIVOT and their inclusion biases results against intervention. No cross-sectional imaging (CT or MRI scanning) was required in PIVOT, despite a number of these patients being in the high risk DAmico category.3 Thus, it is conceivable that some patients already had detectable metastatic disease, but were operated on anyway. This would render surgery futile, again biasing results against intervention. A number of PIVOT patients did not actually have prostate-specific antigen (PSA)-detected prostate cancer; only 75% of the cancers were detected because of an elevated PSA. Of the 364 patients randomized to radical prostatectomy, only 281 (76.6%) actually received surgery. Further, in the control arm, 74/367 (20.2%) had some form of local definitive therapy. Thus, both compliance and contamination issues were potentially significant. None of the reported PIVOT analysis took these contamination and compliance issues into account. Further, a number of subset analyses were performed and these subsets were almost all underpowered. It is well known that underpowered analyses have a significant potential to underestimate benefit. All that being said, there is much to learn from PIVOT. Despite the many limitations in study design, patient selection and analyses of multiple underpowered subsets, there was a strong trend toward benefit for both intermediate and high risk prostate cancer
patients. This underscores that patients with a PSA of more than 10, a Gleason score of 7 or higher and a clinical stage of T2b or higher are potentially good candidates for radical prostatectomy provided that they are healthy enough and young enough to live at least 10 years. Estimating life expectancy is an issue that has attracted little attention but post-PIVOT, more thought and more analysis should be placed on this important concept to better define those likely to benefit from aggressive approaches. Failure to do so will not solve the overtreatment issues that are currently problematic.4 The PIVOT patient with a classification of low risk prostate cancer (Gleason 6 on biopsy and clinical stage T1c or T2a and PSA ,10 ng ml21) had a remarkably good prognosis when no treatment is given. Importantly, we learned more about outcomes for these low-risk patients in the PSA era. These patients are doing much better as compared to the much quoted observational studies in the pre-PSA era reported by Albertsen and colleagues.5 Today, there is much controversy of concerning what prostate cancer patients are eligible for surveillance instead of radical treatment. PIVOT basically makes clear that most men with low risk prostate cancer should not be treated with radical treatment as the default option. It is now clear that the risks and side effects of treatment outweigh the benefit of radical surgery for the vast majority of men with low risk prostate cancer. Looking at men followed for 12 years after randomization, the low risk prostate cancer subgroup had only a 2.7% risk of prostate cancer mortality in BOTH arms of the study. Demonstrating that any treatment provides further risk reduction, as compared to observation, is unlikely. We also learned more about surveillance. How to best perform surveillance and when to remove someone from surveillance is a topic of much recent discussion.6 At this
Research Highlight 804
point, it is fairly clear that much of this discussion is not warranted. Perhaps it is possible to detect low risk men at high risk for prostate cancer death, but it will not be easy. Improving upon 97.3% prostate cancer-specific survival at 12 years is probably not going to be accomplished regardless of the intervention. This finding has implications for high intensity focused ultrasound, brachytherapy, external beam radiation, as well as surgery. The PIVOT study demonstrates that a simple combination of biopsy Gleason score, clinical stage and PSA is quite good at predicting who will live and who will die from prostate cancer 12 years later. While parameters such as PSA density, multiparametric MRIs and repeated biopsies are incorporated into many
current surveillance protocols, it is now clear that these factors are not critical for excellent outcomes in the low risk patient population. As we go forward, understanding the heterogeneity of localized prostate cancer is ever more critical. Those patients who entrust us with their care deserve careful consideration before radical prostatectomy is offered as standard of care given the side effects that are well documented from this treatment.7
6 1 Wilt TJ, Brawer MK, Jones KM, Barry MJ, Aronson WJ et al. Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med 2012; 367: 20313. Stephenson AJ, Kattan MW, Eastham JA, Bianco FJ Jr, Yossepowitch O et al. Prostate cancer-specific
mortality after radical prostatectomy for patients treated in the prostate-specific antigen era. J Clin Oncol 2009; 27: 43005. DAmico AV, Whittington R, Malkowicz SB, Schultz D, Blank K et al . Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 1998; 280: 96974. Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol 2010; 28: 111723. Albertsen PC, Hanley JA, Fine J. 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA 2005; 293: 2095101. Cooperberg MR, Carroll PR, Klotz L. Active surveillance for prostate cancer: progress and promise. J Clin Oncol 2011; 29: 366976. Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med 2008; 358: 125061.
Asian Journal of Andrology
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Blood Tests Types Analysis and Meaning PDFDokument25 SeitenBlood Tests Types Analysis and Meaning PDFRandy Dookheran83% (6)
- Science and Justice: Conference ReportDokument10 SeitenScience and Justice: Conference Reportkhalid safiNoch keine Bewertungen
- NCGT Issue 50 March 2009 PDFDokument85 SeitenNCGT Issue 50 March 2009 PDFGeeleegoatNoch keine Bewertungen
- 20 Canadian Junior Mining CompaniesDokument24 Seiten20 Canadian Junior Mining CompaniesGeeleegoatNoch keine Bewertungen
- Goldman Miller Vaccine Hospitalization Study HETDokument11 SeitenGoldman Miller Vaccine Hospitalization Study HETGeeleegoatNoch keine Bewertungen
- Electromagnetic Disturbances Associated With Earthquakes - Jse - 04 - 2 - ParrotDokument9 SeitenElectromagnetic Disturbances Associated With Earthquakes - Jse - 04 - 2 - ParrotGeeleegoatNoch keine Bewertungen
- Mechanical SystemsDokument107 SeitenMechanical SystemsGeeleegoatNoch keine Bewertungen
- Emissivity of MaterialsDokument11 SeitenEmissivity of MaterialsGeeleegoatNoch keine Bewertungen
- Electrical Connections PowerCircuitsDokument20 SeitenElectrical Connections PowerCircuitsGeeleegoatNoch keine Bewertungen
- Fluoride in Drinking Water: The Problem and Its Possible SolutionsDokument8 SeitenFluoride in Drinking Water: The Problem and Its Possible SolutionsGeeleegoatNoch keine Bewertungen
- Defluoridation Using Activated Alumina (UNICEF)Dokument9 SeitenDefluoridation Using Activated Alumina (UNICEF)GeeleegoatNoch keine Bewertungen
- Defluoridation Using The Nalgonda Technique in Tanzania - Dahi 1996Dokument3 SeitenDefluoridation Using The Nalgonda Technique in Tanzania - Dahi 1996GeeleegoatNoch keine Bewertungen
- Fluorosilicates - Review of Toxicological LiteratureDokument36 SeitenFluorosilicates - Review of Toxicological LiteratureGeeleegoatNoch keine Bewertungen
- Wyeth Rotashield Package InsertDokument19 SeitenWyeth Rotashield Package InsertGeeleegoatNoch keine Bewertungen
- Hidden Disk Areas - HPA and DCODokument8 SeitenHidden Disk Areas - HPA and DCOGeeleegoatNoch keine Bewertungen
- The Physical Meaning of E mc2 - Glenn BorchardtDokument4 SeitenThe Physical Meaning of E mc2 - Glenn BorchardtGeeleegoatNoch keine Bewertungen
- The Rapid Electrical Formation of Stone Spherules, The Scalability of The Results, and The Similarities of The Internal and External Structures of The Spheres With Naturally Occurring ConcretionsDokument20 SeitenThe Rapid Electrical Formation of Stone Spherules, The Scalability of The Results, and The Similarities of The Internal and External Structures of The Spheres With Naturally Occurring ConcretionsGeeleegoat100% (1)
- Powder Contrail WerlepatentDokument4 SeitenPowder Contrail Werlepatentoffgrid7Noch keine Bewertungen
- Magnetic Field of A Moving ChargeDokument10 SeitenMagnetic Field of A Moving ChargeGeeleegoatNoch keine Bewertungen
- Enzalutamida arches-JCO.19.00799Dokument15 SeitenEnzalutamida arches-JCO.19.00799Raul BarcellonaNoch keine Bewertungen
- 11 BPHDokument59 Seiten11 BPHبدرول هشام100% (1)
- Guide For Good Prostate HealthDokument9 SeitenGuide For Good Prostate HealthAlceir FerreiraNoch keine Bewertungen
- Complementary and Alternative Medicines in Prostate Cancer A Comprehensive PDFDokument316 SeitenComplementary and Alternative Medicines in Prostate Cancer A Comprehensive PDFMarcela Osorio DugandNoch keine Bewertungen
- Propecia ConsentDokument3 SeitenPropecia ConsentEbenezer FrimpongNoch keine Bewertungen
- 001SCH19159071 1Dokument1 Seite001SCH19159071 1Naeem33Noch keine Bewertungen
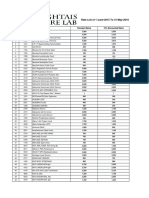
- Rate List of 1-June-2015 To 31-May-2016: S.No Code Test Name Standard Rates 15% Discounted RatesDokument25 SeitenRate List of 1-June-2015 To 31-May-2016: S.No Code Test Name Standard Rates 15% Discounted RatesMirza BabarNoch keine Bewertungen
- NMT11 Urology Special NoteDokument36 SeitenNMT11 Urology Special NoteYiba Zul100% (4)
- Surgery For Pathological T3a, T3b and Lymph Node Positive, Prostae Cance PDFDokument11 SeitenSurgery For Pathological T3a, T3b and Lymph Node Positive, Prostae Cance PDFMuhammad RifkiNoch keine Bewertungen
- Diagnosis and Treatment of Bacterial ProstatitisDokument5 SeitenDiagnosis and Treatment of Bacterial ProstatitislobeseyNoch keine Bewertungen
- Analitical ErrorDokument15 SeitenAnalitical Errorlabor baiturrahimNoch keine Bewertungen
- Hormone Therapy For Prostate Cancer Exploring Current ControversiesDokument8 SeitenHormone Therapy For Prostate Cancer Exploring Current ControversiesNenad MladenovicNoch keine Bewertungen
- 10) One Word That Can Save Your LifeDokument4 Seiten10) One Word That Can Save Your LifeParesh PathakNoch keine Bewertungen
- BicalutamideDokument30 SeitenBicalutamideRoberto AmbrosioNoch keine Bewertungen
- Abstracts USICON2017Dokument618 SeitenAbstracts USICON2017rdLuis1Noch keine Bewertungen
- Liaquat University of Medical & Health Sciences, JamshoroDokument7 SeitenLiaquat University of Medical & Health Sciences, JamshoroShireen Panhwar100% (1)
- EAU 2022 - Prostate CancerDokument229 SeitenEAU 2022 - Prostate Cancerpablo penguinNoch keine Bewertungen
- State of The ArtDokument3 SeitenState of The ArtArne HeyerickNoch keine Bewertungen
- Prostate Cancer ThesisDokument5 SeitenProstate Cancer Thesisaflozmfxxranis100% (2)
- ProstateDokument204 SeitenProstatevonicaNoch keine Bewertungen
- Advances in Prostatic Diagnostics in Dogs 2018Dokument4 SeitenAdvances in Prostatic Diagnostics in Dogs 2018Orlando Karim Shiro Jr.Noch keine Bewertungen
- Prostate: Erbil Polytechnic University Soran Technical Institute Nursing DPTDokument13 SeitenProstate: Erbil Polytechnic University Soran Technical Institute Nursing DPTKazm AbdullaNoch keine Bewertungen
- International Journal of Adhesion & AdhesivesDokument6 SeitenInternational Journal of Adhesion & AdhesivesAshwary Sheel Wali Research Scholar, Dept of Mech Engg., IIT (BHU)Noch keine Bewertungen
- Fullerton Health - AIA Ancillary Services 2017Dokument12 SeitenFullerton Health - AIA Ancillary Services 2017william pianoNoch keine Bewertungen
- Dépistage Par PSA Du Cancer de La Prostate V2: Rapport Bénéfices RisquesDokument1 SeiteDépistage Par PSA Du Cancer de La Prostate V2: Rapport Bénéfices RisquesJean-Philippe RivièreNoch keine Bewertungen
- Biochemistry: Investigation Observed Value Unit Biological Reference IntervalDokument15 SeitenBiochemistry: Investigation Observed Value Unit Biological Reference IntervalAshutoshNoch keine Bewertungen
- PSA Elisa: Specimen Collection and PreparationDokument3 SeitenPSA Elisa: Specimen Collection and PreparationAsesor Bioquímico de Licitaciones BiotecNoch keine Bewertungen
- TPSA-ML Flex InsertDokument16 SeitenTPSA-ML Flex InsertisitalamasbonitaNoch keine Bewertungen