Beruflich Dokumente
Kultur Dokumente
Psychiatric Nursing
Hochgeladen von
Milagros Fuertes YosoresCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Psychiatric Nursing
Hochgeladen von
Milagros Fuertes YosoresCopyright:
Verfügbare Formate
Presented by: Dave Jay S. Manriquez, RN.
PSYCHIATRIC NURSING Introduction
MENTAL HEALTH balance in a persons internal life and adaptation to reality
Mental ILL Health state of imbalance characterized by a disturbance in a persons thoughts, feelings and behavior Psychiatric nursing interpersonal process whereby the professional nurse practitioner ,through the therapeutic use of self (art) and nursing theories (science), assist clients to achieve psychosocial well being. Core : interpersonal process Related Terms Mental hygiene measures to promote mental health , prevent mental illness and suffering and facilitate rehabilitation Main tool: therapeutic use of self It requires self-awareness
Methods to increase self-awareness: Introspection Discussion Experience Role play
Assessment (psychosocial processes ) Appearance , behavior or mood Speech , thought content and thought process Sensorium Insight and judgment Family relationships and work habits Level of growth and development Common Behavioral Signs and Symptoms Disturbances in perception Illusion misinterpretation of an actual external stimuli
Hallucinations false sensory perception in the absence of external stimuli
Disturbances in thinking and speech neologism coining of words that people do not understand Circumstantiality over inclusion of inappropriate thoughts and details Word salad incoherent mixture of words and phrases with no logical sequence Verbigeration meaningless repetition of words and phrases Perseveration persistence of a response to a previous question Echolalia pathological repetition of words of others Aphasia speech difficulty and disturbance Expressive , receptive or global
Flight of ideas- shifting of one topic from one subject to another in a somewhat related way Looseness of association-incoherent illogical flow of thoughts (unrelated way) Clang association sound of word gives direction to the flow of thought Delusion persistent false belief, rigidly held Delusions of grandeur: special /important in a way Persecutory: threatened Ideas of reference: situation/events involve them Somatic: body reacting in a particular way
Jealous: thinking that their partner is unfaithful Erotomanic: person, usually of high status, is in love with the client Religious: illogical ideas about God and religion exhibited by extreme or extraneous behavior
Mixed: combination of above without a predominant theme Magical thinking primitive thought process thoughts alone can change events
Autistic thinking regressive thought process; subjective interpretations not validated with objective reality Dereism unorganized thinking
Disturbances of affect Inappropriate disharmony between the stimuli and the emotional reaction Blunted affect severe reduction in emotional reaction Flat affect absence or near absence of emotional reaction Apathy dulled emotional tone Depersonalization feeling of strangeness from ones self Derealization feeling of strangeness towards environment Agnosia lack of sensory stimuli integration Disturbances in motor activity Echopraxia imitation of posture of others Waxy flexibility maintaining position for a long period of time Ataxia loss of balance Akathesia extreme restlessness Dystonia- uncoordinated spastic movements of the body Tardive dyskinesia involuntary twitching or muscle movements Apraxia involuntary unpurposeful movements Disturbances in memory Confabulation filling of memory gaps Dj vu something unfamiliar seems familiar Jamais vu- something familiar seems unfamiliar Amnesia memory loss (inability to recall past events) Retrograde-distant past Anterograde immediate past Anomia lack of memory of items
Dynamics of Human Behavior
Behavior the way an individual reacts to a certain stimulus Conflict situation arising from the presence of two opposing drives
Need - organismic condition that requires a certain activity Dynamics of Human Behavior Personality totality of emotional and behavioral traits that characterize the person in day to day living under ordinary conditions; it is relatively stable and predictable. FORMATION OF PERSONALITY TEMPERAMENT biological-genetic template that interacts with our environment. a set of in-built dispositions we are born with mostly unalterable our nature. CHARACTER the outcome of the process of socialization, the acts and imprints of our environment and nurture on our psyche during the formative years (0-6 years and in adolescence). the set of all acquired characteristics we posses, often judged in a cultural-social context. Sometimes the interplay of all these factors results in an abnormal personality THEORIES OF PERSONALITY DEVELOPMENT Freuds PSYCHOSEXUAL THEORY
Libido inner drive Parts of body focus of gratification Unsuccessful resolution - fixation Structures of personality Id: pleasure principle-instinct Ego: controls action and perception reality principle Superego: moral behavior - conscience 0-18 m0s ;oral mouth trust and discriminating 18 mos. 3 years ; anal bowels holding on or letting go Negativism and toilet training age 3 -6 years phallic ; genitals exploration and discovery ( inc. sexual tension)
Gender identification and genital awareness Oedipus and Electra complex Castration anxiety and penis envy
6-12 years latency (quiet stage) sexual energy diverted to play. Institution of superego: control of instinctual impulses 12 young adult genital ; reawakening of sexual drives relationships Sexual maturation Sexual identity ,ability to love and work Eric Ericksons PSYCHOSOCIAL THEORY
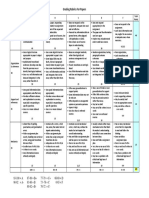
0-12mos 1-3y 3-6 6-12 12-18 18-25 25-60 60 and above TRUST vs. MISTRUST AUTONOMY vs. SHAME & DOUBT INDUSTRY vs. INFERIORITY INITIATIVE vs. GUILT IDENTITY vs. IDENTITY CONFUSION INTIMACY vs. ISOLATION EGO INTEGRITY vs. STAGNATION GENERATIVITY vs. DESPAIR INFANCY CONSISTENT MATERNAL CHILD INTERACTION TRUST INNER FEELING OF SELF WORTH
HOPE TODDLER ALLOW EXPLORATION PROVIDE FOR SAFETY NO, NO NEGATIVISM OFFER CHOICES / REVERSE PSYCHOLOGY TOILET TRAINING 18 MOS.-BOWEL DAYTIME BLADDER: 2 yo NIGHTIME BLADDER: 3 yo REWARD W/ PRAISE AND AFFECTION INDEPENDENCE PRE-SCHOOL PROVIDE PLAY MATERIALS SATISFY CURIOSITY TEACH AND REINFORCE(HYGIENE,SOCIAL BEHAVIOR) SIBLING RIVALRY WILLPOWER SCHOOL AGE HOW TO DO THINGS WELL-SUPPORT EFFORTS CHUMS AND HOBBIES NEEDS TO EXCEL/ACCOMPLISH NEED FOR PRIVACY AND PEER INTERACTION COMPETENCE ADOLESCENCE MAKE DECISION,EMANCIPATION FROM PARENTS BODY IMAGE CHANGES NEED TO CONFORM BUT KEEP INDIVIDUALITY SELF - AWARENESS YOUNG ADULT
COMMITMENT AND FIDELITY RESPONSIBILITY ACHIEVEMENT OF INDEPENDENCE MIDDLE ADULTHOOD SUPPORT-PERIOD OF ROLE TRANSITIONS
MIDLIFE CRISIS ADJUSTMENT AND COMPROMISE MOST PRODUCTIVE AND CREATIVE ALTRUISM LATE ADULTHOOD SELF ACCEPTANCE SELF WORTH WISDOM Jean Piagets COGNITIVE THEORY 0-2 SENSORIMOTOR REFLEXES IMITATIVE REPETITIVE BEHAVIOR SENSE OF OBJECT PERMANENCE AND SELF SEPARATE FROM ENVT.
TRIAL AND ERROR RESULTS IN PROBLEM SOLVING 2-7Y PRE-OPERATIONAL SELF-CENTERED,EGOCENTRIC CANNOT CONCEPTUALIZE OTHERS VIEW ANIMISTIC THINKING IMAGINARY PLAYMATE SYMBOLIC MENTAL REPRESENTATION CREATIVITY 2-4 PRE-CONCEPTUAL (PRE-LOGICAL) 4-7 INTUITIVE (UNDERSTANDING OF ROLES) 7-12Y CONCRETE OPERATIONAL LOGICAL CONCRETE THOUGHT
INDUCTIVE REASONING (SPECIFIC TO GENERAL) CAN RELATE, PROBLEM SOLVING ABILITY REASONING AND SELF-REGULATION 12-ABOVE: FORMAL OPERATIONAL THOUGHT Abstract thinking Separation of fantasy and fact Reality oriented Deductive reasoning
Apply scientific method Havighursts DEVELOPMENTAL TASKS
Baby to early childhood Right from wrong and Conscience Late childhood Physical skills, wholesome attitude, social roles Conscience morality and values Fundamental skills in academics Personal independence
Adolescence Sexual social roles Relationships Independence and ideology Early adulthood Career Selecting a mate Finding Civic or social responsibility
Middle age Achieving Civic or social responsibility Adjusting to changes Satisfactory career performance Adjusting to aging parents Adjusting to parental roles Old age Adjusting to changes Establishing satisfactory living arrangements and affiliations Kohlbergs MORAL DEVELOPMENT/ THINKING/ JUDGEMENT
PRE-CONVENTIONAL (0-6) PUNISHMENT AND OBEDIENCE OBEDIENCE TO RULES TO AVOID PUNISHMENT
CONVENTIONAL ( 6-12 ) MUTUAL INTERPERSONAL EXPECTATIONS,RELATIONSHIPS AND CONFORMITY SOCIAL SYSTEM AND CONSCIENCE MAINTENANCE BEING GOOD IS IMPORTANT SELF RESPECT OR CONSCIENCE
POST CONVENTIONAL (12 18 Y) PRIOR RIGHT OR SOCIAL CONTRACT UNIVERSAL ETHICAL PRINCIPLE ABIDE FOR COMMON GOOD RATIONAL PERSON-VALIDITY OF PRINCIPLES-AND BECOME COMMITTED TO THEM INNER CONTROL OF BEHAVIOR UNDERSTANDING THE EQUALITY OF HUMAN RIGHTS AND DIGNITY OF HUMAN BEINGS AS INDIVIDUALS Harry Stack Sullivans INTERPERSONAL THEORY INFANCY NEED FOR SECURITY-INFANT LEARNS TO RELY ON OTHERS TO GRATIFY NEEDS AND SATISFY WISHES, DEVELOPS A SENSE OF BASIC TRUST, SECURITY AND SELF WORTH WHEN THIS OCCURS TODDLERHOOD / EARLY CHILDHOOD CHILD LEARNS TO COMMUNICATE NEEDS THROUGH USE OF WORDS AND ACCEPTANCE OF DELAYED GRATIFICATION AND INTERFERENCE OF WISH FULFILLMENT PRE-SCHOOL DEVELOPMENT OF BODY IMAGE AND SELF-PERCEPTION ORGANIZES AND USES EXPERIENCES IN TERMS OF APPROVAL AND DISAPPROVAL RECEIVED BEGINS USING SELCTIVE INATTENTION AND DISASSOCIATES THOSE EXPERIENCES THAT CAUSE PHYSICAL OR EMOTIONAL DISCOMFORT AND PAIN SCHOOL AGE
THE PERIOD OF LEARNING TO FORM SATISFYING RELATIONSHIPS WITH PEERS-USES COMPETITION,COMPROMISE AND COOPERATION THE PRE-ADOLESCENT LEARNS TO RELATE TO PEERS OF THE SAME SEX ADOLESCENCE LEARNS INDEPENDENCE AND HOW TO ESTABLISH SATISFACTORY RELATIONSHIPS WITH MEMBERS OF THE OPPOSITE SEX YOUNG ADULTHOOD BECOMES ECONOMICALLY, INTELLECTUALLY AND EMOTIONALLY SELF SUFICIENT LATER ADULTHOOD LEARNS TO BE INTERDEPENDENT AND ASSUMES RESPONSIBILITY FOR OTHERS SENESCENCE DEVELOPS AN ACCEPTANCE OF RESPONSIBILITY FOR WHAT LIFE IS AND WAS AND OF ITS PLACE IN THE FLOW OF HISTORY TREATMENT MODALITIES REMOTIVATION THERAPY TREATMENT MODALITY THAT PROMOTES EXPRESSION OF FEELINGS THROUGH INTERACTION FACILITATED BY DISCUSSION OF NEUTRAL TOPICS STEPS : climate of acceptance creating bridge to reality sharing the world we live in appreciation of works of the world climate of appreciation
tension
MUSIC THERAPY Involves use of music to facilitate expression of feelings, relaxation and outlet of PLAY THERAPY enables patient to experience intense emotion in a safe environment with the use
of play
children express themselves more easily in play. revealing as reflection of childs situation in the family provide toys and materials facilitate interaction observe and help child resolve problems through play Group therapy Treatment modality involving three or more patients with a therapist to relieve emotional difficulties, increase self esteem, develop insight , LEARN NEW ADAPTIVE WAYS TO COPE WITH STRESS and improve behavior with others
IDEAL 8 10 MEMBERS MILIEU THERAPY Consists of treatment by means of controlled modification of the patients environment to facilitate positive behavioral change Increase patients Awareness of feelings Sense of responsibility and Help return to community clients plan social and group interaction token programs , open wards and self medication are done FAMILY THERAPY A METHOD OF PSYCHOTHERAPY WHICH FOCUSES ON THE TOTAL FAMILY AS AN INTERACTIONAL SYSTEM PROBLEM IS A FAMILY PROBLEM focus on sick members behavior as source of trouble / symptom serve a function for the family members develop sense of identity points out function of the sick member for the rest of the family PSYCHOANALYTIC focuses on the exploration of the unconscious, to facilitate identification of the patients defenses ANXIETY RESULTS BETWEEN CONFLICTS OF ID AND EGO Becomes aware of unconscious thoughts and feelings to understand anxiety and defenses HYPNOTHERAPY Various methods and techniques to induce a trance state where patient becomes submissive to instructions BEHAVIOR MODIFICATION Application of learning principles in order to change maladaptive behavior
Believes that psychological problems are a result of learning
Everything learned can be unlearned BEHAVIOR MODIFICATION OPERANT CONDITIONING Use of rewards to reinforce positive behavior Perceived and self-reinforcement becomes more important than external reinforcement
DESENSITIZATION Slow adjustment or exposure to feared objects (phobias) Periodic exposure until undesirable behavior disappears or lessens
AVERSION THERAPY An example of behavior modification Painful stimulus is introduced to bring about an avoidance of another stimulus End view: behavioral change OTHER THERAPIES HUMOR THERAPY To facilitate expression and enhance interaction ACTIVITY THERAPY Group interaction while working on a task together BIOLOGICAL/ MEDICAL THEORY EMOTIONAL PROBLEM IS AN ILLNESS cause may be inherited or chemical in origin
FOCUS OF TREATMENT IS MEDICATIONS AND ECT BIOLOGICAL THERAPY ELECTROCONVULSIVE THERAPY Artificial induction of a grand mal seizure by passing a controlled electrical current through electrodes applied to one or both temples mechanism of action unclear voltage: 70 150 volts Duration: 0.5 2.0 seconds 6 to 12 treatments intervals of 48 hours indicators of effectiveness occurrence of generalized tonic clonic seizures
indications depression , mania and catatonic schizophrenia s/e: confusion, disorientation, short -term memory loss, seizure (30-60 sec) NPO prior Contraindications Fever, pregnancy Inc ICP, fracture retinal detachment TB with hemoptysis cardiac d/o consent needed Reorient after, supportive care medications given : Atropine sulfate: decrease secretions Succinylcholine (Anectine): promote muscle relaxation
Methohexital Sodium ( Brevital ): serves as an anesthetic agent common complications: loss of memory headache apnea fracture respiratory depression Psychopharmacologic Therapy Benzodiazepines Indications Anxiety Sedation/sleep Muscle spasm Seizure disorder Alcohol withdrawal syndromes Generic Alprazolam Chlordiazepoxide Clorazepate Diazepam Lorazepam Oxazepam Busipirone Anti-anxiety drugs Trade name Xanax Librium Tranxene Valium Ativan Serax BuSpar Side effects
Drowsiness/ sedation Ataxia Feelings of detachment Increase irritability and hostility Anterograde amnesia Increased appetite & weight gain Nausea Headache, confusion Anti-depressants Indications Depression Bipolar depression Panic disorder
Bulimia Obsessive-compulsive d/o
Possibly Attention deficit/Hyperactivity d/o Post Traumatic Stress D/o Conduct d/o Tricyclic (TCA) Generic Trade name Amitriptyline Elavil Imipramine Tofranil Trimipramine Surmontil Nortriptyline Pamelor Trazodone Desyrel Bupropion Wellbutrin Side effects Orthostatic hypertension
Anticholinergic effect Dry mouth, blurred vision, constipation, excessive sweating, urinary hesitancy/ retention, tachycardia, agitation, delirium, exacerbation of glaucoma Neurologic effects sedation, psychomotor slowing, poor concentration, fatigue, ataxia, tremors
Decrease libido and sexual performance
Generic Isocarboxazid Phenelzine Tranylcypromine
Monoamine Oxidase inhibitors Trade name Marplan Nardil Parnate Side effects Postural lightheadedness Constipation Delay ejaculation or orgasm Muscle twitching Drowsiness Dry mouth Dietary restrictions Cheese, esp. aged and matured Fermented or aged protein
Pickled or smoked fish Beer, red wine, sherry; liquor & cognac Yeast Fava or broad beans Beef or chicken liver Spoiled/ overripe fruits; banana peel yogurt Hypertensive Crisis Signs Sudden elevation of BP Explosive headache, occipital may radiate frontally Head & face flushed Palpitations, chest pain Sweating, fever Nausea, vomiting Dilated pupils, photophobia Intracranial bleeding Treatment Hold next MAO dose Dont let pt. lie down IM chlorpromazine 100 mg Fever: manage by external cooling techniques Serotonin Reuptake Inhibitors Generic Trade name Fluoxetine Prozac Sertraline Zoloft Paroxetine Paxil Venlafaxine Effexor Side effects Nausea Diarrhea Insomnia Dry mouth Nervousness Headache Male sexual dysfunction
Drowsiness Dizziness Sweating Mood stabilizing drugs Indications Acute mania Bipolar prophylaxis Possibly Bulimia Alcohol abuse Aggressive behavior schizoaffective
Mode of action Normalizes the reuptake of certain neurotransmitters such as serotonin, norepinephrine, acetylcholine and dopamine Reduces the release of norepinephrine thru competition with calcium Effects intracellularly
Lag period: 7-10 to 14 days Lithium carbonate
Trade names Eskalith Lithotabs Lithane Lithonate MOA: unclear; interfere with metabolism of neurotransmitters; alter Na transport in nerves and muscle cells Prelithium workup Urinalysis (BUN and creatinine) ECG, FBC, CBC Side effects Early Nausea and diarrhea Anorexia Fine hand tremor (propranolol) Thirst, Polydipsia (dec. crea, inc. albumin) Metallic taste Fatigue
Lethargy Late Weight gain acne Contraindications Brain damage/ CV disease Epilepsy Elderly/ debilitated Thyroid and renal disease Severe dehydration Pregnancy (1st trimester)
Can augment the effects of anti-depressants Nursing considerations Therapeutic serum level: 0.5 1.2 meq/L Maintenance level: 0.6 -1.2 meq/L Toxic Mild to moderate: 1.5 to 2 meq/L Moderate to severe: 2 2.5 meq/L Needs dialysis: 3 meq and above Early signs of toxicity Lethargy, mild nausea, vomiting, fine hand tremors, anorexia, polyuria, polydipsia, metallic taste, fatigue Late signs of toxicity Ataxia, giddiness, tinnitus, blurred vision, polyuria Nursing considerations Lithium levels should be checked q 2-3 mos Serum drawn in the AM, 12H after last dose Common causes of inc. levels Dec. Na intake Diuretic therapy Dec. renal functioning F&E loss Medical illness Overdose NSAIDS Nursing considerations Diet: adequate Na+ and fluid
3g NaCl/ day 6-8 glasses of H2O No caffeine No driving: wait for clinical effect Management Moderately severe toxicity Osmotic diuresis: urea/ mannitol Aminophylline & PLR IV Adequate NaCl Peritoneal/ hemodialysis Severe toxicity Assess hx quickly Hold next lithium dose Check BP, rectal T, RR, LOC, support O2 Obtain labs ECG Emetic, NGT lavage Hydrate: 5-6L/day c PLR; FBC-CDU Other drugs Carbamazepine (Tegretol) Side effects Dizziness Ataxia Clumsiness Sedation Dysarthria Diplopia Nausea & GI upset Preparation: liq, tab, chewable tab Nursing considerations Assess drug levels q 3-4 days Monitor salt and fluid intake Avoid alcohol and non-prescription drugs Refer dec. in UO Dont stop abruptly C/I: pregnancy Take with meals Other drugs Valproic acid (Depakote, Depakene)
Side effects Nausea Hepatoxicity Neurotoxicity Hematological toxicity Pancreatitis Prep: tab, cap, sprinkles
MOA: inc. levels of GABA; inhibits the kindling process or snoball-like effect seen in mania & seizures Nursing considerations Therapeutic level: 50 100 ug/mL
Dose: 1, 000 1,500 mg/day Monitor serum levels 12H after last dose Toxic effects Severe diarrhea, vomiting, drowsiness, mm. weakness, lack of coordination Renal failure, coma, death Anti-psychotic drugs Indications Psychotic symptoms of schizophrenia, acute mania and depression Gilles de Tourette disorder Treatment-resistant bipolar disorder Huntingtons disease and other movement disorder Possibly Paranoid Childhood psychoses
MOA: block receptors of dopamine (D2, D3, D4) If unresponsive after 6 weeks of therapy, another class is tried
General considerations Calms without producing impairment of sleep High therapeutic index Non addicting, no tolerance Avoided in pregnancy TYPICAL: High Potency Fluphenazine (Prolixin) Haloperidol (Haldol) Thiothexene (Navane) Trifluoperazine (Stelazine)
Moderate Potency Loxapine (Loxitane) Molindone (Moban) Perphenazine (Trilafon) Low Potency Chlopromazine (Thorazine) Chlorprothixene (Taractan) Mesoridazine (Serentil) Thioridazine (Mellaril) ATYPICAL Clozapine (Clozaril) Resperidone (Risperdal) Olanzapine (Zyprexa) Quetiapine (Seroquel) Sertindole (Serlect) Ziprasidone (Zeldox)
Contraindications CNS depression: brain damage, excess alcohol/ narcotics Parkinsons disease Allergy Blood dyscrasias Acute narrow angle glaucoma BPH Side effects Hypotension Sedation Dermal and ocular syndrome Neuroleptic malignant syndrome Anticholinergic syndrome Movement syndrome (Extrapyramidal Syndrome) Atropine psychosis Agranulocytosis Seizures Neuroleptic Malignant Syndrome A potentially fatal, idiosyncratic reaction to an antipsychotic drug 10-20% mortality rate Sx: rigidity, high fever,
autonomic instability (BP, diaphoresis, pallor, delirium, elev. CPK), confused or mute, fluctuate from agitation to stupor Occurs in the first 2 weeks of therapy Risk: high dose of high-potency drugs; dehydration, poor nx, concurrent med illness Movement Syndromes Akathisia
Dystonia Tardive dyskinesia Bradykinesia Parkinsonism Other s/e Atropine psychosis (geriatrics) Hyperactivity, agitation, confusion, flushed skin, sluggish reactive pupils TTT: IM physostigmine Agranulocytosis (Clozapine) Occurs 3-8 wks after Medical emergency s/s: fever, malaise, sore throat, leukopenia TTT: d/c, reverse iso, antibiotics Seizures (Clozapine) Occurs in 5% of patients; TTT: D/c drug Anticholinergics Benztropine (Cogentin) Trihexyphenidyl (Artane) Biperiden (Akineton) Procyclidine (Kemadrin)
Not withdrawn abruptly Provide cool environment
ANTIPARKINSONIAN MEDICATIONS Adjunct to anti-psychotic agents to balance dopamine/ acetylcholine in the brain s/e: glaucoma, tachycardia, HPN, cardiac dx, asthma, duodenal ulcer A/e: blurred vision, photosensitivity, drowsiness, orthostatic hypotension, CHF, hallucinations
COMMON DRUGS: Trihexyphenidyl (Artane) benztropine (Cogentin) Biperiden (Cogentin) Selegiline (Eldepryl) Pergolide (Permax) ANTIHISTAMINE Diphenhydramine HCl (BENADRYL) DOPAMINE RELEASING AGENT Amantadine (SYMMETREL) Nursing considerations Best taken after meals Avoid driving Check BP Alcohol increases sedative effects Avoid sudden position change Drug is not withdrawn abruptly PSYCHIATRIC DISORDERS ANXIETY DISORDERS
PANIC DISORDERS SPECIFIC PHOBIA SOCIAL PHOBIA OCD PTSD ACUTE STRESS DISORDER
GENERALIZED ANXIETY DISORDER PANIC ATTACKS Discrete period of intense fear or discomfort in which at least 4 if the ff sx develop abruptly and peak within 10 mins: Palpitations, pounding heart, or accelerated HR Sweating Trembling or shaking Sensations of SOB and smothering Feeling of choking
Chest pain or discomfort
Nausea or abd. Pain Feeling dizzy, unsteady, lightheaded or faint Derealization or depersonalization Fear of losing control or going crazy Fear of dying Paresthesias Chills or hot flashes
SPECIFIC PHOBIA SOCIAL Excessive and unreasonable cued by the presence or anticipation of a specific object or situation Defense mech commonly used include repression and displacement Fear of social performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others OBSESSION COMPULSION Recurrent and persistent thoughts, impulses, or images are experienced during the disturbance as intrusive and inappropriate Cause anxiety or distress Px knows that these are just product of ones own mind. Px feels driven to perform repetitive behaviors or mental acts in response to obsession or according to the rules that one deems must be applied rigidly. Aimed at reducing anxiety OBSESSION COMPULSION Fear of dirt & germs Fear of burglary or robbery Worries about discarding something important Concerns about contracting a serious illness Worries that things must be symmetrical or matching Excessive hand washing Repeated checking of door and window locks Counting and recounting of objects in everyday life Hoarding of objects Excessive straightening, ordering, or of arranging things Repeating words or prayers silently
POST TRAUMATIC STRESS SYNDROME Person has experienced, witnessed or been confronted with an event that involved actual or threatened death or serious injury, or a threat to physical integrity Person reexperiences these in the mind
Involves intense fear, helplessness, or horror and numbing of general responsiveness (PSYCHIC NUMBING) ACUTE GENERALIZED STRESS ANXIETY Meets the criteria for exposure to a traumatic event and person experiences 3 of the ff sx: sense of detachment, reduced awareness of ones surroundings, derealization, depersonalization, dissociated amnesia Excessive anxiety or worry, occurring in more days than not for at least 6 mos, about a number of events or activities Finds it difficult to control the worry MOOD/ AFFECTIVE DISORDERS
BIPOLAR D/O BIPOLAR I: current or past experience of manic episode, lasting at least a week, that is severe enough to cause extreme impairment in social or occupational functioning. MANIA: hyperactivity DEPRESSED: extreme sadness or withdrawal MIXED BIPOLAR II: hx of 1 or more mj depressive episodes & at least 1 hypomanic episode; no mania
MAJOR DEPRESSIVE D/O @ least 5 sx of same 2- wk period with one being either depressed mood or loss of interest or pleasure. Single episode or recurrent Other sx: wt loss, insomnia, fatigue, recurrent thoughts of death, diminished ability to think, psychomotor agitation or retardation, feelings of worthlessness.
CYCLOTHYMIC D/O Hx of 2 yrs of hypomania with numerous periods of abnormally elevated, expansive or irritable moods. Does not meet the criteria of mania or depression.
DYSTHYMIC D/O @ least 2 yrs of usually depressed mood and at least 1 of the sx of mj depression without meeting the criteria for it SEASONAL AFFECTIVE D/O
Depression that comes with shortened daylight in fall and winter that disappears during spring and summer. Dealing with Inappropriate Behaviors AGGRESSIVE BEHAVIOR Assist the client in identifying feelings of frustration and aggression Encourage the client to talk out instead of acting out feelings of frustration Assist the client in identifying precipitating events or situations that lead to aggressive behavior Describe the consequences of the behavior on self and others Assist in identifying previous coping mechanisms Assist the client in the problem-solving techniques to cope with frustration or aggression DEESCALATION TECHNIQUES Maintain safety Maintain large personal space and use nonaggressive posture Use calm approach and communicate with a calm, clear tone of voice (be assertive not aggressive Determine what the client considers to be his or her need Avoid verbal struggles Provide clear options that deal with behavior Assist with problem-solving and decision making regarding the options MANIPULATIVE BEHAVIORS Set clear, consistent, realistic, and enforceable limits and communicate expected behaviors Be clear about consequences associated with exceeding set limits
Discuss behavior in nonjudgmental and nonthreatening manner Avoid power struggles
Assist in developing means of setting limits on own behavior SCHIZOPHRENIA characterized by impairments in the perception or expression of reality and by significant social or occupational dysfunction. Once considered as a deadly disease There is lack of insight in behavior Dx: late adolescence and early adulthood 15-25 y.o. (men); 25-35 y.o. (women) Obsolete term: dementia praecox = cognitive deterioration early in life Eugene Bleuler: schiz split; phren mind Risk factors Genetics: identical twins 50%, 15% for fraternal twins
Biochemical factors Dopamine hypothesis: overactive Serotonin imbalance Decreased brain volume, enlarged ventricles, deeper fissures, and loss or underdeveloped brain tissue Psychoanalytic lack of trust during the early stages Weak ego Defenses: REPRESSION, REGRESSION, PROJECTION Environment influences: poverty, lack of social support, hostile home environment, isolation, unsatisfactory housing, disruption in interpersonal relationships (divorce or death), job pressure or unemployment Subtypes Catatonic type prominent psychomotor disturbances are evident. Symptoms can include catatonic stupor and waxy flexibility Disorganized type where thought disorder and flat affect are present together
Paranoid type where delusions and hallucinations are present but thought disorder, disorganized behavior, and affective flattening are absent
Residual type where positive symptoms are present at a low intensity only Undifferentiated type
psychotic symptoms are present but the criteria for paranoid, disorganized, or catatonic types has not been met Symptoms According to Bleuler: 4 As Affect is inappropriate Associative looseness Autistic thinking Ambivalence Symptoms
Positive symptoms delusions, auditory hallucinations and thought disorder and are typically regarded as manifestations of psychosis. Negative symptoms considered to be the loss or absence of normal traits or abilities
E.G. flat, blunted or constricted affect and emotion, poverty of speech and lack of motivation. Symptoms Social isolation Catatonic behavior Hallucinations Incoherence (marked looseness of association) Zero/ lack of interest, energy and initiative Obvious failure to attain expected level of devt Peculiar behavior Hygiene and grooming impaired Recurrent illusions and unusual perception experiences Exacerbations and remissions are common No organic factors accounts for the symptoms Inability to return to baseline functioning after relapse Affect is inappropriate Nsg Dx: Abnormal thought process BLOCKING: sudden cessation of a thought in the middle of a sentence, unable to continue the train of thought CIRCUMSTANTIALITY: before getting to the point of answering a question, the individual gets caught up in countless details and explanations CONFABULATION LOOSENESS OF ASSOCIATION NEOLOGISM WORD SALAD Interventions Assess physical needs Set limits Maintain safety Initiate one-on-one interaction & progress to small groups Spend time with clients Monitor for altered thought process Maintain ego boundaries, avoid touching Limit time of interaction Be neutral Do not make promises that cant be kept
Establish daily routines Do not go along with the clients delusions or hallucinations Provide simple complete activities Reorient
Speak to the client in simple direct and concise manner Set realistic goals Explain everything that is being done Decrease stimuli Monitor for suicide risk
Environment Provide safe environment Limit stimuli Psychological Ttt Behavior therapy Social skills training Self-monitoring Social ttt Milieu therapy Family therapy Group therapy (long-term ttt) Related psychotic disorders SCHIZOAFFECTIVE DISORDER schiz + mood disorder (mania/ depression)
BRIEF PSYCHOTIC DISORDER sudden onset of psychotic symptoms, lasts less than 2 mos and client returns to premorbid level of functioning SCHIZOPHRENIFORM DISORDER schiz sx lasting between 1 month and <6mos DELUSIONAL DISORDER characterized by prominent, nonbizarre delusions PERSONALITY DISORDERS
CLUSTER A (odd & eccentric) paranoid, schizoid, schizotypal CLUSTER B (bad, dramatic & erratic) antisocial, borderline, histrionic, narcissistic CLUSTER C (anxious & fearful) avoidant, dependent, OCD CLUSTER A: ODD & ECCENTRIC PARANOID chronic hostility projected to others; suspicious and mistrusts people Seen mostly in men SCHIZOID
social detachment = loner & introvert Restriction of emotions Attention fixed on objects rather than people Functions well in vocations SCHIZOTYPAL: interpersonal deficits Magical thinking, telepathy Apparent in childhood or adolescence Interventions for PARANOID D/O Asses for suicide risk Avoid direct eye contact Establish trusting relationship Promote increased self-esteem Remain calm, nonthreatening and nonjudgmental Provide continuity of care Respond honestly to the client Follow thru on commitments Provide a daily schedule of activities Gradually introduce client to groups Do not argue with delusions Use concrete, specific words
Do not be secretive with client Do not whisper in presence of client Assure that the client will be safe Provide opportunity to complete small tasks Monitor eating, drinking, sleeping and elimination patterns Limit physical contact Monitor for agitation and decrease stimuli as needed CLUSTER B: ERRATIC, DRAMATIC, OR EMOTIONAL ANTISOCIAL Syn: sociopath, psychopathic & semantic d/o Etiology: Genetics interfere in the devt of positive interpersonal relationships Brain damage or trauma Low socioeconomic status
Faulty family relationships: neglect Secondary gains 15-40 y.o.
Signs Lack of remorse or indifference to persons hurt Immediate gratification Failure to accept social norms Impulsivity Consistent irresponsibility Aggressive behavior Reckless behavior that disregards the safety of others 80-90% of all crime is committed by antisocials (NIHM, 2000) BORDERLINE Latent, ambulatory and abortive schizophrenics Between moderate neurosis and frank psychosis but quite stable Theories faulty separation from mother; parent and child are bound by guilt Trauma at 18 mos (weakening of ego) Unfulfilled need for intimacy
Signs instability Impulsivity: unpredictable gambling, shoplifting, sex & substance abuse hypersensitivity, self-destructive, profound mood shifts unstable & intense relations Disturbance in self concept Common in women Defenses: denial, projection, splitting, projective identification
HISTRIONIC Pattern of theatrical or overtly dramatic behavior Signs
Discomfort when the client isnt the center of attention Self-dramatization and exaggerated emotions uses physical appearance, sexually seductive and provocative behavior Excessively impressionistic speech lacking in detail (labile emotions) Problems in dependence & helplessness More frequent in women NARCISSISTIC Exaggerated or grandiose sense of self-importance Develop early in childhood Preoccupied with fantasies of unlimited success, power and beauty Signs arrogance, need for admiration, lack of empathy, seductive, socially exploitative, manipulative Occurs more in men CLUSTER C: ANXIOUS OR FEARFUL
AVOIDANT Sensitive to rejection, criticism, humiliation, disapproval, or shame Interferes with participation in occupational activities, devt of relationships, and take personal risks social inhibition, longs for relationships Anxiety, anger and depression are common Social phobia may occur Seen in 10% of clients in mental clinics
DEPENDENT Lacks confidence and unable to function in an independent role Allows other persons to be responsible of their lives Most frequent personality disorder in the mental health clinic submissive behavior, low self-esteem, inadequate, helpless
OBSESSIVE-COMPULSIVE Preoccupied with rules & regulations, overly concerned about trivial detail, excessively devoted to their work Depression is common Men are more affected than women UNDER STUDY PERSONALITY D/O
PASSIVE-AGGRESSIVE: sullen and argumentative, resents others, resists fulfilling responsibilities, complains of being unappreciated DEPRESSIVE: gloomy, brooding pessimistic, guilt-prone, highly critical of self and others, cheerless. Interventions Maintain safety against self-destructive behaviors Allow the client to make choices and be as independent as possible Encourage the client to discuss feelings rather than act them out Provide consistency in response to the clients acting out Discuss expectations and responsibilities with the client Inform the client that harm to self, others, and property is unacceptable
Identify splitting behavior Assist the client to deal directly with anger Develop a written contract with the client
Encourage the client to participate in group activities, and praise nonmanipulative behavior Set and maintain limits Remove the client from group situations in which attention-seeking behaviors Provide realistic praise for positive behaviors in social situations PSYCHOLOGICAL SEXUAL D/O Hypoactive sexual disorder (asexuality) Sexual aversion disorder (avoidance of or lack of desire for sexual intercourse) Female sexual arousal d/o (failure of normal lubricating arousal response) Male erectile d/o Female orgasmic disorder Male orgasmic disorder Premature ejaculation Vaginismus Secondary sexual dysfxn Paraphilias Gender identity d/o PTSD due to genital mutilation or childhood sexual abuse occur
Other sexual problems Sexual dissatisfaction (non-specific)
Lack of sexual desire anorgasmia Impotence STD
Infidelity Delay or absence of ejaculation, despite adequate stimulation Inability to control timing of ejaculation Inability to relax vaginal muscles enough to allow intercourse Inadequate vaginal lubrication preceding and during intercourse Burning pain on the vulva or in the vagina with contact to those areas
Unhappiness or confusion related to sexual orientation Persistent sexual arousal syndrome Sexual addict hypersexuality Post Ejaculatory Guilt Syndrome, the feeling of guilt after the male orgasm SEXUAL EXPRESSION HETEROSEXUALITY HOMOSEXUALITY BISEXUALITY TRANSVESTISM
PARAPHILIAS EXHIBITIONISM: the recurrent urge or behavior to expose one's genitals to an unsuspecting person. FETISHISM: the use of non-sexual or nonliving objects or part of a person's body to gain sexual excitement. Partialism refers to fetishes specifically involving nonsexual parts of the body. FROTTEURISM: the recurrent urges or behavior of touching or rubbing against a nonconsenting person.
SEXUAL MASOCHISM: the recurrent urge or behavior of wanting to be humiliated, beaten, bound, or otherwise made to suffer. SEXUAL SADISM: the recurrent urge or behavior involving acts in which the pain or humiliation of the victim is sexually exciting.
TRANSVESTIC FETISHISM: a sexual attraction towards the clothing of the opposite gender. PEDOPHILIA: the sexual attraction to prepubescent or peripubescent children.
VOYEURISM: the recurrent urge or behavior to observe an unsuspecting person who is naked, disrobing or engaging in sexual activities, or may not be sexual in nature at all.
Other paraphilias not otherwise specified ("Sexual Disorder NOS") telephone scatalogia (obscene phone calls) necrophilia (corpses) partialism (exclusive focus on one part of the body) zoophilia(animals) coprophilia (feces) klismaphilia (enemas) urophilia (urine)
SOMATOFORM D/O SOMATIZATION D/O: hx of many physical complaints beginning before the age of 30 occurring over a pd of several yrs resulting in ttt being sought or significant occupational or social fxning. CONVERSION D/O: 1 or more sx of deficits affecting voluntary motor or sensory function suggesting a neurological or general medical condition; preceded by conflicts or stressors; cant be explained and sanctioned by cultural behavior. Most common: blindness, deafness, paralysis, inability to talk La belle indifference
HYPOCHONDRIASIS: preoccupation with fears of having, or ideas that one has, a serious dse based on the persons misinterpretation of bodily sx and persist despite appropriate medical eval and reassurance and has existed for @ least 6 mos. (e.g.:extensive use of home remedies) PAIN D/O: pain in 1 or more anatomical sites severe enough to warrant clinical attention and causes clinically significant distress or impairment in fxning. Interventions Do not reinforce the sick role
Discourage verbalization about physical symptoms by not responding with positive reinforcement Explore with the client the needs being met by the physical symptoms
Convey understanding that the physical symptoms are real to the client
Report and assess any new physical complaint next EATING DISORDER BEHAVIORS BINGE: rapid consumption of large quantities of food in a discrete period of time. (A: hundrends of Cal; B: thousands of Cal at a sitting) PURGE: Maladaptive eating regulation response that includes excessive exercise, forced vomiting, OCD Rx diuretics, diet pills, laxatives and steroids. FAST/ RESTRICT: Includes vegetarian diet eliminating all meat without substituting nonanimal sources of protein, OC about food choices, and eating habits. ANOREXIA BULIMIA Rare vomiting or diuretic/laxative abuse More severe wt loss Slightly younger More introverted Hunger denied Eating behavior may be considered normal and a source of esteem Sexually inactive Obsessional and perfectionist features dominate Frequent Less wt loss Slightly older More extroverted Hunger experienced Eating behavior considered foreign and source of distress More sexually active Avoidant, dependent, or borderline features as well as obsessional features ANOREXIA BULIMIA complications Death from starvation (or suicide, in chronically ill) Amenorrhea
Fewer behavioral problems (these increase with level of severity) Death from hypokalemia or suicide Menses irregular or absent Drug and alcohol abuse, self-mutilation, and other behavioral problems DELIRIUM The medical dx term that describes an organic mental disorder characterized by a cluster of cognitive impairments with an acute onset with a specific precipitating factor. Sx: diminished awareness of the environment, disturbances in psychomotor activity and sleep-wake cycle. COGNITIVE: the mental process characterized by knowing, thinking, and judging.
COGNITIVE DISSONANCE: arises when 2 opposing beliefs exists at the same
time. COGNITIVE DISTORTIONS: (+) or (-) distortions of reality that might include errors of logic, mistakes in reasoning, or individualized view of the world that do not reflect reality. Term: confusion = cognitive impairment See dementia DEMENTIA The medical dx term that describes an organic mental d/o characterized by a cluster of cognitive impairments of generally gradual onset and irreversible without identifiable precipitating stressors. Types: VASCULAR or MULTI-INFARCT VASCULAR WITH ALZHEIMERS DSE AD: most common DEMENTIA WITH LEWY BODIES: 2nd most common; neurofilament material PARKINSONIAN DEMENTIA AIDS DEMENTIA COMPLEX
FRONTAL LOBE DEMENTIA or PICKS DSE: cytoplasmic collections; 3rd most common; loss of expressive language & comprehension CREUTZFELDT-JAKOB DSE: prion (proteinaceous infectious particles) = spongy brain; related to TSE & BSE in mad cow dse CORTICOBASAL DEGENERATION or HUNTINGTONS DSE/CHOREA: jerky movts SUPRANUCLEAR PALSY: clumping of protein tau = slow movt, weak eye movt (esp. downward), impaired walking &balance
Reversible Causes: Subdural hematoma Tumor (meningioma) Cerebral vasculitis Hydrocephalus Terms: disorientation, memory loss (sensory, primary, secondary, tertiary, working memory), confabulation, confusion Disturbing behaviors Aggressive psychomotor Nonaggressive psychomotor Verbally aggressive Passive Functionally impaired: loss of ability to do self-care DELIRIUM vs. DEMENTIA Rapid onset w/ wide fluctuations
Hyperalert to difficult to arouse LOC Fluctuating affect Disoriented, confused Attention & sleep disturbed Memory impaired Disordered reasoning Gradual, chronic with continuous decline Normal LOC Labile affect Disoriented, confused Attention intact, sleep usually normal Memory impaired Disordered reasoning & calculation DELIRIUM vs. DEMENTIA Incoherent, confused, delusional, stereotyped Illusions, hallucinations Poor judgment Insight may be present in lucid moment Poor but variable in MSE
next Disorganized, rich in content, delusional, paranoid No change in perception Poor judgment No insight Consistently poor & progressively worsens in MSE ALZHEIMERS DEMENTIA Most common type of dementia
Stages: MILD: impaired memory, insidious loses in ADL, subtle personality changes, socially normal MODERATE: obvious memory loss, overt ADL impairment, prominent behavioral difficulties, variable social skills, supervision needed SEVERE: fragmented memory, no recognition of familiar people, assistance needed with basic ADL, fewer troublesome behaviors, reduced mobility (4 As)
Symptoms AGNOSIA: Difficulty recognizing well-known objects APHASIA: Difficulty in finding the right word
APRAXIA: Inability or difficulty in performing a purposeful organized task or similar skilled activities
AMNESIA: Significant memory impairment in the absence of clouded consciousness or other cognitive symptoms PSYCHIATRIC D/O IN CHILDREN MENTAL RETARDATION PERVASIVE DEVTAL D/O AUTISM RETTS D/O CHILDHOOD DISINTEGRATIVE D/O ASPERGERS D/O PDD NOS LEARNING D/O READING MATHEMATICS WRITTEN EXPRESSION ACADEMIC PROBLEM LEARNING D/O NOS MOTOR SKILLS D/O COMMUNICATION D/O EXPRESSIVE LANGUAGE MIXED RECEPTIVE/EXPRESSIVE PHONOLOGICAL STUTTERING SELECTIVE MUTISM COMMUNICATION D/O NOS MOVT & TIC D/O DEVTAL COORDINATION TRANSIENT TIC CHRONIC MOTOR&VOCAL TIC TOURETTES D/O STEREOTYPIC MOVT D/O TIC D/O NOS DISORDERS OF INTAKE & ELIMINATION PICA RUMINATION FEEDING D/O ENURESIS ENCOPRESIS
OTHER: BULIMIA, ANOREXIA ADHD & DISRUPTIVE BEHAVIOR D/O ADHD ADHD NOS CONDUCT D/O OPPOSITIONAL DEFIANT CHILD ANTISOCIAL DISRUPTIVE BEHAVIOR NOS MOOD D/O MJ DEPRESSIVE D/O BIPOLAR I OR II DYSTHYMIC MIXED EPISODE HYPOMANIC EPISODE MOOD D/O DUE TO MEDICAL CONDITION SUBSTANCE-INDUCED MOOD D/O ANXIETY D/O
D/O OF RELATIONSHIP SEPARATION ANXIETY REACTIVE ATTACHMENT OF INFANCY OR EARLY CHILDHOOD PARENT-CHILD RELATIONAL PROBLEM SIBLING RELATIONAL PROBLEM PROBLEMS RELATED TO ABUSE OR NEGLECT MENTAL RETARDATION an IQ below 70, significant limitations in two or more areas of adaptive behavior (i.e., ability to function at age level in an ordinary environment), and evidence that the limitations became apparent in before 18 y.o. The following ranges, based on the Wechsler Adult Intelligence Scale (WAIS), are in standard use today: Class IQ Terms Profound Below 20 Idiot Severe 2034 Imbecile Moderate 3549 Moron Mild 5069 Borderline 7079 RETTS D/O Development is normal until 6-18 months, when language and motor milestones regress, purposeful hand use is lost Acquired deceleration in the rate of head growth (resulting in microcephaly in some)
Hand stereotypes are typical and breathing irregularities such as hyperventilation, breath holding, or sighing are seen in many. Early on, autistic-like behavior may be seen Common in females CHILDHOOD DISINTEGRATIVE D/O or HELLERS SYNDROME CDD has some similarity to autism, but an apparent period of fairly normal development is often noted before a regression in skills or a series of regressions in skills. characterized by late onset (>3 years of age) of devtal delays in language, social function and motor skills; skills apparently attained are lost ASPERGERS D/O characterized by difference in language and communication skills, as well as repetitive or restrictive patterns of thought and behavior. Signs: unable to interpret or understand the desires or intentions of others and thereby are unable to predict what to expect of others or what others may expect of them Narrow interests or preoccupation with a subject to the exclusion of other activities Repetitive behaviors or rituals Peculiarities in speech and language Extensive logical/technical patterns of thought Socially and emotionally inappropriate behavior and interpersonal interaction Problems with nonverbal communication Clumsy and uncoordinated motor movts CHRONIC MOTOR/ VOCAL TIC TIC is a sudden, repetitive, stereotyped, nonrhythmic, involuntary movement (motor tic) or sound (phonic tic) that involves discrete groups of muscles. can be invisible to the observer (e.g. abdominal tensing or toe crunching) TOURETTES D/O characterized by the presence of multiple physical (motor) tics and at least one vocal (phonic) tic; these tics characteristically wax and wane TTT: Neuroleptic medications haloperidol (Haldol) pimozide (Orap) ADHD Inattention: Failure to pay close attention to details or making careless mistakes when doing schoolwork or other activities Trouble keeping attention focused during play or tasks Appearing not to listen when spoken to Failure to follow instructions or finish tasks Avoiding tasks that require a high amount of mental effort and organization, such as school projects
Frequently losing items required to facilitate tasks or activities, such as school supplies Excessive distractibility Forgetfulness Procrastination, inability to begin an activity Difficulties with household activities (cleaning, paying bills, etc.) Difficulty falling asleep, may be due to too many thoughts at night Frequent emotional outbursts Easily frustrated Easily distracted Hyperactivity-impulsive behaviour Fidgeting with hands or feet or squirming in seat Leaving seat often, even when inappropriate Running or climbing at inappropriate times Difficulty in quiet play Frequently feeling restless Excessive speech Answering a question before the speaker has finished Failure to await one's turn Interrupting the activities of others at inappropriate times Impulsive spending, leading to financial difficulties
Frequently prescribed stimulants are methylphenidate (Ritalin and Concerta), amphetamines (Adderall) and dextroamphetamines (Dexedrine) Feingold diet which involves removing salicylates, artificial colors and flavors, and certain synthetic preservatives from children's diets. CONDUCT D/O repetitive and persistent pattern of behavior in which the basic rights of others or major age-appropriate societal norms or rules are violated, AGGRESSION TO PEOPLE & ANIMALS DESTRUCTION OF PROPERTY DECEITFULNESS OR THEFT SERIOUS VIOLATIONS OF RULES Beginning before age 13 OPPOSITIONAL DEFIANT characterized by an ongoing pattern of disobedient, hostile, and defiant behavior toward authority figures that goes beyond the bounds of normal childhood behavior Signs Losing temper Arguing with adults Refusing to follow the rules Deliberately annoying people Blaming others
Easily annoyed Angry and resentful Spiteful or even revengeful next
SUBSTANCE ABUSE Excessive or unhealthy use of substances, such as alcohol, tobacco or drugs, or use of products such as food Terms: TOLERANCE: the declining effect of the same drug dose when it is taken repeatedly over time HABITUATION: a psychological dependence of the use of a drug ADDICTION: the biological and/ or psychological behaviors related to substance dependence WITHDRAWAL SYMPTOMS: result from a biological need that develops when the body becomes adapted to having an addictive drug in the system; occurs when serum levels decrease ADDICTION ALCOHOL: blood alcohol levels of 0.1% (100mg alcohol/dl of blood) or higher WITHDRAWAL Anorexia Anxiety Easily startled Hyperalertness HPN Insomnia Irritability Jerky movt Possibly: hallucinations, illusions or vivid nightmares Seizures (7-48 hrs after cessation) Tachycardia tremors
WITHDRAWAL DELIRIUM Agitation Anorexia Anxiety Delirium Diaphoresis Disorientation with fluctuating levels of consciousness Fever (100 to 103 F) Hallucinations and delusions Insomnia Tachycardia and HPN Disulfiram (Antabuse) therapy
Nursing care Obtain info about drug type and amount consumed Assess v/s Remove unnecssary obj from environment Provide one-on-one supervision if necessary Provide a quiet, calm environment with minimal stimuli Maintain orientation Ensure safety Use restraints Provide physical needs Provide food and fluids as tolerated Administer medications Collect blood and urine samples for drug screening SPOUSE ABUSE Battering precipitates 1:4 suicide attempts of all women Wives explain the injuries as being self-inflicted or accidental Phases Tension-building: series of small incidents that leads to beating Acute beating phase: wife becomes object of assault behavior Loving phase: batterer is remorseful and assures spouse that he will not harm her again. This leads to reconciliation.
Myths They believe that if they try not to antagonize with their husband, he will change. Efforts to coerce the wife out of the victim role can be fruitful. Facts Women stay in relationships with men who batter because they feel guilty or responsible of the husbands behavior Wife develops little sense of self-worth, immobilized and unable to remove self from the relationship. Assessment: injuries, other evidence Interventions: with consent CHILD ABUSE
PHYSICAL BATTERING EMOTIONAL SEXUAL NEGLECT ELDERLY ABUSE
A variety of behaviors that threaten the health, comfort, and possibly the lives of the elderly, including physical and emotional neglect, emotional abuse, violation of personal rights, financial abuse, and direct physical abuse. Commonly committed by care givers. SEXUAL ABUSE Components Sexual Misuse: inappropriate sexual activity Rape: there is actual penetration Incest: refers to the relationship between the victim and abuser blood relative or step parent role Interventions Children: thru play or role playing with puppets Prevention of further sexual abuse next COMPLETED SUICIDE Self-inflicted death
LEVELS OF SUICIDE Ideation: thought Attempt: acted upon but failed Completed CHEMICAL RESTRAINT CHEMICAL RESTRAINTS: Medications used to restrict the patients freedom of movement or for emergency control of behavior but are not a standard treatment for the pxs medical or psychiatric condition. PHYSICAL RESTRAINTS: Are any manual method or physical or mechanical device attached to or adjacent to the pxs body that he or she cannot easily remove and that restricts freedom of movement or normal access to ones body, material or equipment. SECLUTION AND RESTRAINTS SECLUTION: the involuntary confinement of a person alone in a room from which the person is physically prevented from leaving. No therapeutic evidence other than a last resort to ensure safety. Evidence suggest that it adds to further trauma and physical harm
GUIDELINES All hospital staff who have direct contact with the px should have ongoing education and training in the proper use of seclusion and restraints and other alternatives Physician or licensed practitioner should evaluate need within 1 hour after the initiation of this intervention.
Max of 4 hours for adults, 2 hours for ages 9-17, and 1 hour for children under 9 yrs Orders may be renewed for 24 hrs before another face to face evaluation Continuous assessment, monitoring and evaluation; recorded Good nursing care For both restrained and secluded: constant monitoring face to face or by both audio and video equipment. Px should be released ASAP OTHER GUIDELINES SECLUSION Room should allow observation and communication with px Remove all items that px might use to harm self Document: rationale, response to intervention, physical condition, nsg care, & rationale for termination RESTRAINTS Give support & reassurance Position in anatomical position Privacy is important v/s & Circulation check Should be released q 2hrs Avoid tying to the side rails of bed Assist in periodic change in body positions
TERMINATING THE INTERVENTION As soon as met the criteria for release
Review with px the behavior that precipitated the intervention & pxs capacity to exercise control over behavior DEBRIEFING: reviewing the facts related to an event & processing the response to them; can be used after any stressful event next THERAPEUTIC IMPASSES Are blocks in the progress of the nurse-pt relationship
oneself
Provokes intense feelings in both the nurse and patient RESISTANCE TRANSFERENCE COUNTERTRANSFERENCE BOUNDARY VIOLATIONS RESISTANCE Reluctance or avoidance of verbalizing or experiencing troubling aspects of
Eg: suppression or repression, intensification of sx, self-devaluation or hopelessness, intellectual inhibitions, acting out or irrational behavior, superficial talk, intellectual insight/ intellectualization, transference reactions.
TRANSFERENCE Unconscious response in which the px experiences feelings and attitudes toward the nurse that were originally associatated with other significant figures in his or her life. HOSTILE TRANSFERENCE: anger and hostility, resistance DEPENDENT TRANSFERENCE: submissive, subordinate and regards the nurse as a god-like figure; views relationship as magical
What do you do? LISTEN CLARIFY REFLECT EXPLORE/ ANALYZE
COUNTERTRANSFERENCE Created by the nurses specific emotional response to the qualities of the patient; inappropriate in the context, content and intensity of emotion; nurses identify the px with individuals from their past, and personal needs Types: Reactions of INTENSE love or caring Disgust or hostility Anxiety, often in response to resistance by the px
Eg. Difficulty empathizing Feelings of depression before or after the session Carelessness about implementing the contract Drowsiness during the sessions Encouragement of the pxs dependency Arguments with the px Personal or social involvement with the px Sexual or aggressive fantasies toward the px Tendency to focus on only one aspect or way of looking at information presented by the px Attempts to help the px with matters not related to the identified nursing problems Feelings of anger or impatience because of the pxs unwillingness to change Dreams about or preoccupation with the px
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Who Is DiagnosableDokument3 SeitenWho Is DiagnosableHamna Shahid100% (1)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Performance Checklist For Perineal Care: FemaleDokument1 SeitePerformance Checklist For Perineal Care: FemaleMilagros Fuertes YosoresNoch keine Bewertungen
- Performance Checklist For Perineal Care: FemaleDokument1 SeitePerformance Checklist For Perineal Care: FemaleMilagros Fuertes YosoresNoch keine Bewertungen
- What Is Drug Education and TreatmentDokument6 SeitenWhat Is Drug Education and TreatmentAdrian BagayanNoch keine Bewertungen
- Special Problems in Marital RelationshipDokument43 SeitenSpecial Problems in Marital RelationshipMilagros Fuertes YosoresNoch keine Bewertungen
- Developmental Task of Parents To BeDokument3 SeitenDevelopmental Task of Parents To BeMilagros Fuertes YosoresNoch keine Bewertungen
- Rubrics For EssayDokument1 SeiteRubrics For EssayMilagros Fuertes YosoresNoch keine Bewertungen
- 1psych Pre TestDokument2 Seiten1psych Pre TestMilagros Fuertes YosoresNoch keine Bewertungen
- Grading Rubrics For Papers PDFDokument1 SeiteGrading Rubrics For Papers PDFMilagros Fuertes YosoresNoch keine Bewertungen
- The Concept of FamilyDokument22 SeitenThe Concept of FamilyMilagros Fuertes YosoresNoch keine Bewertungen
- Rubrics For EssayDokument1 SeiteRubrics For EssayMilagros Fuertes YosoresNoch keine Bewertungen
- Grad Thesis ProposalDokument3 SeitenGrad Thesis Proposalgio477Noch keine Bewertungen
- Psychiatric NursingDokument46 SeitenPsychiatric NursingMilagros Fuertes YosoresNoch keine Bewertungen
- PTSDDokument3 SeitenPTSDMilagros Fuertes YosoresNoch keine Bewertungen
- Community Health NursingDokument11 SeitenCommunity Health NursingMilagros Fuertes YosoresNoch keine Bewertungen
- Shock ExamDokument3 SeitenShock ExamMilagros Fuertes Yosores100% (1)
- Legal and Ethical IssuesDokument6 SeitenLegal and Ethical IssuesMilagros Fuertes YosoresNoch keine Bewertungen
- CA Exam UndergraduateDokument3 SeitenCA Exam UndergraduateMilagros Fuertes YosoresNoch keine Bewertungen
- Revised Disaster NursingDokument25 SeitenRevised Disaster NursingLlana Pauline JacintoNoch keine Bewertungen
- Triage Level 5Dokument78 SeitenTriage Level 5DanielKnows100% (1)
- Care For The ElderlyDokument223 SeitenCare For The ElderlyMilagros Fuertes Yosores100% (1)
- PTSDDokument3 SeitenPTSDMilagros Fuertes YosoresNoch keine Bewertungen
- Care For The ElderlyDokument223 SeitenCare For The ElderlyMilagros Fuertes Yosores100% (1)
- Clerkship Exam Information 9 15Dokument9 SeitenClerkship Exam Information 9 15Ehab AzarNoch keine Bewertungen
- And Related Disorders (DSM V)Dokument10 SeitenAnd Related Disorders (DSM V)Aqsa ArshadNoch keine Bewertungen
- Utilizing The DSM-5 Anxious Distress Specifier To Develop Treatment Strategies For Patients With Major Depressive DisorderDokument12 SeitenUtilizing The DSM-5 Anxious Distress Specifier To Develop Treatment Strategies For Patients With Major Depressive DisorderRosemarie FritschNoch keine Bewertungen
- Attention Deficit Hyperactivity Disorder ADHD in DSM 5 A Trial For Cultural Adaptation in BangladeshDokument4 SeitenAttention Deficit Hyperactivity Disorder ADHD in DSM 5 A Trial For Cultural Adaptation in BangladeshEditor IJTSRDNoch keine Bewertungen
- AripripazoleDokument13 SeitenAripripazoleOneng IfayaniNoch keine Bewertungen
- 2017 Mental Health Nursing PHD SyllabiDokument6 Seiten2017 Mental Health Nursing PHD SyllabiJoel John Dela MercedNoch keine Bewertungen
- IJCM-Psychoses in MangaloreDokument2 SeitenIJCM-Psychoses in MangaloreANKUR BARUANoch keine Bewertungen
- The Differentiation of Psychosis and Spiritual EmergencyDokument0 SeitenThe Differentiation of Psychosis and Spiritual Emergencymayoi_19607098100% (2)
- Death by Excited Delirium-PowerpointDokument17 SeitenDeath by Excited Delirium-PowerpointRosie AlviorNoch keine Bewertungen
- Psychiatry: Mental State ExaminationDokument3 SeitenPsychiatry: Mental State ExaminationSok-Moi Chok100% (3)
- Davidson Trauma Scale (DTS) - Normative Scores in The General Population and Effect Sizes in Placebo-Controlled SSRI TrialsDokument4 SeitenDavidson Trauma Scale (DTS) - Normative Scores in The General Population and Effect Sizes in Placebo-Controlled SSRI Trialsericaduran4824100% (1)
- Changes From Icd 10 To 11Dokument9 SeitenChanges From Icd 10 To 11Daniel John ArboledaNoch keine Bewertungen
- 356 Mastering Psychiatry Term-Paper PDFDokument356 Seiten356 Mastering Psychiatry Term-Paper PDFdragutinpetricNoch keine Bewertungen
- Trauma Assessment: John Briere, PH.DDokument10 SeitenTrauma Assessment: John Briere, PH.DZawawi Ibnu RosyidNoch keine Bewertungen
- NCP - Bipolar (Manic Phase) PDFDokument3 SeitenNCP - Bipolar (Manic Phase) PDFCarla Tongson MaravillaNoch keine Bewertungen
- Brainwave Entrainment To Improve Problem-Solving Skills in People With The Neurodevelopmental Disorder ADHDDokument8 SeitenBrainwave Entrainment To Improve Problem-Solving Skills in People With The Neurodevelopmental Disorder ADHDRaul Morales VillegasNoch keine Bewertungen
- Kurt Cobain Case StudyDokument11 SeitenKurt Cobain Case StudyKC Respicio67% (3)
- Fetal Alcohol Spectrum Disorders: What Are Fasds?Dokument2 SeitenFetal Alcohol Spectrum Disorders: What Are Fasds?Bernadette BeltranNoch keine Bewertungen
- Ocd Prac Teach Plan Rescue FileDokument14 SeitenOcd Prac Teach Plan Rescue Filevikas tak100% (2)
- Borderline Personality Disorder and Bipolar Disorder: Joel Paris, MD and Donald W. Black, MDDokument5 SeitenBorderline Personality Disorder and Bipolar Disorder: Joel Paris, MD and Donald W. Black, MDMia BlackattNoch keine Bewertungen
- English TestingDokument3 SeitenEnglish TestingFaozzan Affandi100% (2)
- PECS Example SLD Dyslexia ADHD ReportDokument60 SeitenPECS Example SLD Dyslexia ADHD ReportgenerjustnNoch keine Bewertungen
- Project Echo Didactic On Somatic Symptom Disorder 04022015Dokument25 SeitenProject Echo Didactic On Somatic Symptom Disorder 04022015Iswaran AmpalakanNoch keine Bewertungen
- Cannabis Use and Disorder - Epidemiology, Comorbidity, Health Consequences, and Medico-Legal Status - UpToDate PDFDokument36 SeitenCannabis Use and Disorder - Epidemiology, Comorbidity, Health Consequences, and Medico-Legal Status - UpToDate PDFMarcos RamosNoch keine Bewertungen
- Schizophrenia Research PaperDokument12 SeitenSchizophrenia Research Paperapi-534301945Noch keine Bewertungen
- January First by Michael Schofield - ExcerptDokument13 SeitenJanuary First by Michael Schofield - ExcerptCrown Publishing Group50% (10)
- Annotated Bibliography On Internet AddictionDokument4 SeitenAnnotated Bibliography On Internet AddictionJanet Martel100% (3)
- Substance Abuse BrochureDokument2 SeitenSubstance Abuse Brochureapi-285178079Noch keine Bewertungen