Beruflich Dokumente
Kultur Dokumente
Pheo
Hochgeladen von
antonijevicuOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pheo
Hochgeladen von
antonijevicuCopyright:
Verfügbare Formate
P
Clini Nati
Pheochromocytoma
What is a pheochromocytoma?
A pheochromocytoma (fee o kromo sy toma) is a tumor arising most commonly from the adrenal gland. These tumors can cause headaches, sweating, rapid rise and fall in blood pressure, fast heartbeat, and other symptoms.
What is the adrenal gland?
An adrenal gland is a small, orange gland. There are two adrenal glands in the human body: one on top of each kidney. The adrenal cortex makes other hormones (cortisol and aldosterone) that maintain the body's fluid and electrolyte balance. Eighty percent of the tumors are found on one adrenal gland (unilateral). Ten percent are found on both adrenal glands (bilateral), and 20 percent are found outside the adrenal glands. This disorder can be inherited, as in von Hippel-Lindau syndrome and neurofibromatomatosis type 1, or it can occur with other endocrine tumors such as multiple endocrine neoplasia type 2 (MEN-2) or familial paraganglioma syndrome caused by succinate dehydrogenase gene mutation (e.g. SDHB). About 80 percent of pheochromocytomas are benign; 20 percent are malignant.
The center of the adrenal gland is called the medulla. The outer part of the gland is called the cortex. The medulla makes adrenaline (and adrenaline-like chemicals called catecholamines). The body needs adrenaline to maintain blood pressure and to help cope with stressful situations.
Patient Education
Pheochromocytoma
What are the signs and symptoms of a pheochromocytoma?
Symptoms include headache (usually severe), excessive sweating, generalized racing of the heart (tachycardia, palpitations), anxiety/ panic attacks, nervous shaking, tremors, nausea, vomiting, weight loss, pain in the lower chest and upper abdomen, weakness, fever, heat intolerance, sugar intolerance, and sometimes low blood pressure when standing up.
and metaiobenzylguanidine (MIBG) scintigraphy. Blood tests Special blood tests for pheochromocytomas measure how much adrenaline or noradrenaline and their breakdown products (metanephrines) are in the blood or urine. Further tests include the glucagon stimulation test and clonidine suppression test. Glucagon stimulation test Because glucagon causes patients with pheochromocytomas to have symptoms of the disorder, this test is used for patients who have occasional signs and symptoms. Blood samples are drawn at specific times to measure adrenaline and noradrenaline levels. During this test, glucagon is injected into a vein while blood pressure and heart rate are monitored. This test takes about 30 minutes. Clonidine suppression test The clonidine suppression test also involves measuring adrenaline and noradrenaline as well as metanephrines in the blood over time. Clonidine normally lowers blood levels of catecholamines, but if a tumor is present, catecholamine levels do not decrease when clonidine is given. For this test, patients are asked to swallow a tablet of clonidine, and over the next 3 hours, blood samples are taken. Blood pressure and heart rate are checked during this time period.
When do they occur?
Signs and symptoms usually follow a pattern of high blood pressure followed by low blood pressure. High blood pressure usually begins with a change in breathing and a pounding or forceful heartbeat. This may occur several times a week and last for up to 15 to 60 minutes. Often, these episodes of high blood pressure are started by activities that press on the tumor, such as changes in position, exercise, lifting, defecation, or emotional distress or anxiety.
How are pheochromocytomas diagnosed?
Reliable levels of adrenal hormones (adrenaline and noradrenaline) and their breakdown products (metanephrines) through blood or urine can usually help your doctor make a diagnosis. There are three ways your doctor can do this: blood tests, urine tests, and x-ray tests such as computed tomography (CT), magnetic resonance imaging (MRI),
Patient Education
Pheochromocytoma
24-hour urine collection The 24-hour urine collection is also used to measure catecholamines and their breakdown products. High concentrations of these show a positive diagnosis. Imaging: X-Ray and Nuclear Medicine Scans Computed tomography Computed tomography (CT) is a type of x-ray scan that uses a computer to make pictures, like slices of the inside of a part of your body. Magnetic resonance imaging MRI (magnetic resonance imaging) uses magnetic waves to make these pictures. These scans can help locate the tumor by showing the adrenal glands in great detail. MIBG scan MIBG is a type of scan that uses a radioactive compound to find the tumor. For this test, the patient receives a compound (I123 or I-131 metaiodobenzylguanidine) through a vein. The scanner records the radiation given off by the compound, and when the compound has been taken up by the tumor, the camera will show the tumor's location. The thyroid gland is sensitive to iodine, and the compounds used for the MIBG scan are iodine-based. To protect your thyroid during this scan, you will be given 100 milligrams of potassium iodine (SSKI). You must take SSKI 24 hours before the MIBG scan and for several days after it. Even if you take SSKI, your thyroid gland could be affected for a short period of time (hypothyroidism). Report any prolonged feelings of fatigue,
temperature irregularities, or changes in your heartbeat to your doctor. These could be signs that your thyroid is not working properly (hypothyroidism). Selective vena cava sampling This type of blood drawing can be performed when blood tests and scans cannot find the tumor. For this test, a catheter is inserted into a major blood vessel so that blood samples can be taken from veins that supply organs in the neck, chest, abdomen, or pelvis. These samples are tested for levels of adrenaline. High levels of catecholamines pinpoint the tumor's location.
Treatment
Pheochromocytoma can be treated by medications that lower blood pressure and/or surgery to remove the tumor. Medications Alpha-adrenergic blockers are medications commonly used for lowering blood pressure (examples: phenoxybenzamine or prazosin). Propanolol/Inderol, a beta-blocker, may be used for controlling a fast and irregular pulse. Beta-blockers are used once the blood pressure comes back to normal with alpha-blockers. If you are being treated with medications, frequent followup with your doctor is crucial for making sure your blood pressure and heartbeat stay normal. Surgery Ninety percent of patients are cured by surgery. Surgery for suspected tumors is usually done by laparoscopy (a small incision or cut into the abdomen). This incision allows the doctor to examine other organs
Patient Education
Pheochromocytoma
while removing the tumor. Some surgeons prefer to make this incision from the back (posterior); others make the incision from the side (flank) when taking out larger tumors. Once the tumor is removed, blood pressure usually falls to normal or low normal. Patients who have blood pressure that stays too low, or who have poor circulation in the arms and feet, may need transfusions of blood, plasma, or other fluids. After surgery, some patients have a fall in blood pressure followed by a rise in blood pressure. Usually blood pressure returns to normal over the next few weeks. Patients with chronic high blood pressure will need treatment with alpha- and/or beta-blockers. Sometimes surgery is not an option because of the type of tumor growth or because the tumor spreads (metastasizes) to other parts of the patient's body. Current treatments for malignant tumors include chemotherapy, or radioactive MIBG.
These treatments show variable success rates. If the tumor has spread, the usual sites of metastases are the bones and the lymph nodes. Tumors in bone tend to respond well to radiation therapy. A combination of chemotherapy drugs (cyclophosphamide, vincristine, and dacarbazineCVD), has worked to control tumors in soft tissues (lymph nodes). For patients in whom surgery is not successful, or for those who cannot undergo surgery, symptoms are controlled with medications. If you have other questions about pheochromocytoma, please feel free to ask your nurse or doctor.
6/07
Patient Education
Pheochromocytoma
Das könnte Ihnen auch gefallen
- Installing a Garage Door and Opener- Special Bundle: Cake Decorating for BeginnersVon EverandInstalling a Garage Door and Opener- Special Bundle: Cake Decorating for BeginnersNoch keine Bewertungen
- Are You Disaster Ready ? - First Aid: Natural Disaster Survival Series, #3Von EverandAre You Disaster Ready ? - First Aid: Natural Disaster Survival Series, #3Noch keine Bewertungen
- DANNY INSPECTIONS: 203K Consultant's Guide to A SUCCESFUL 203K LOANVon EverandDANNY INSPECTIONS: 203K Consultant's Guide to A SUCCESFUL 203K LOANNoch keine Bewertungen
- Pesticide Applicator: Passbooks Study GuideVon EverandPesticide Applicator: Passbooks Study GuideNoch keine Bewertungen
- The Bed Bugs Crisis In Plain English: What It Means To YouVon EverandThe Bed Bugs Crisis In Plain English: What It Means To YouNoch keine Bewertungen
- Divorce in New Mexico: The Legal Process, Your Rights, and What to ExpectVon EverandDivorce in New Mexico: The Legal Process, Your Rights, and What to ExpectNoch keine Bewertungen
- Make the Grass Greener On Your Side!: The 7 Elements of a Beautiful Groomed LandscapeVon EverandMake the Grass Greener On Your Side!: The 7 Elements of a Beautiful Groomed LandscapeNoch keine Bewertungen
- A Complete Trophy Store & Engraving Service Business Plan: A Key Part Of How To Start A Trophy ShopVon EverandA Complete Trophy Store & Engraving Service Business Plan: A Key Part Of How To Start A Trophy ShopNoch keine Bewertungen
- Survival Medicine for Beginners: A Quick start Guide to Coping with Injury during DisasterVon EverandSurvival Medicine for Beginners: A Quick start Guide to Coping with Injury during DisasterNoch keine Bewertungen
- So You Bought a Golf Cart?: An Owner’s Guide for Learning About Golf CartsVon EverandSo You Bought a Golf Cart?: An Owner’s Guide for Learning About Golf CartsNoch keine Bewertungen
- How to Use Vegetable Oil as Fuel For Your Diesel Engine: Introduction to the Elaboration of Biodiesel and a Waste Oil ProcessorVon EverandHow to Use Vegetable Oil as Fuel For Your Diesel Engine: Introduction to the Elaboration of Biodiesel and a Waste Oil ProcessorNoch keine Bewertungen
- The Home Owner's Guide to HVAC: The Envelope and Green TechnologiesVon EverandThe Home Owner's Guide to HVAC: The Envelope and Green TechnologiesNoch keine Bewertungen
- Automotive Serviceman: Passbooks Study GuideVon EverandAutomotive Serviceman: Passbooks Study GuideNoch keine Bewertungen
- Secrets of the eBay Millionaires: Inside Success Stories -- and Proven Money-Making Tips -- from eBay’s Greatest SellersVon EverandSecrets of the eBay Millionaires: Inside Success Stories -- and Proven Money-Making Tips -- from eBay’s Greatest SellersNoch keine Bewertungen
- Self-Storage vs. Mobile Home vs. RV Park 3: The Best Passive Large Business: MFI Series1, #167Von EverandSelf-Storage vs. Mobile Home vs. RV Park 3: The Best Passive Large Business: MFI Series1, #167Noch keine Bewertungen
- Phone Clones: Authenticity Work in the Transnational Service EconomyVon EverandPhone Clones: Authenticity Work in the Transnational Service EconomyNoch keine Bewertungen
- Propagating MuscadinesDokument8 SeitenPropagating Muscadinesdsrousse7367Noch keine Bewertungen
- eBay Boot Camp: Why You’re Not Selling Anything, and What You Can do About ItVon EverandeBay Boot Camp: Why You’re Not Selling Anything, and What You Can do About ItNoch keine Bewertungen
- Snipers, Shills, and Sharks: eBay and Human BehaviorVon EverandSnipers, Shills, and Sharks: eBay and Human BehaviorBewertung: 2 von 5 Sternen2/5 (1)
- Chicken Run Plans 4x8Dokument21 SeitenChicken Run Plans 4x8Ivan RochfordNoch keine Bewertungen
- Turning Dirt: A step-by-step guide for turning dreams of campground ownership into realityVon EverandTurning Dirt: A step-by-step guide for turning dreams of campground ownership into realityNoch keine Bewertungen
- Ada Checklist Word Fillable FormDokument96 SeitenAda Checklist Word Fillable FormchinchouNoch keine Bewertungen
- 43 Miles Per Gallon: Get Better Gas Mileage: Select Your Electric Car, #1Von Everand43 Miles Per Gallon: Get Better Gas Mileage: Select Your Electric Car, #1Noch keine Bewertungen
- CHP 8 BVBVDokument32 SeitenCHP 8 BVBVklmNoch keine Bewertungen
- G165/G166/G167 G181/G183/G184 Service ManualDokument298 SeitenG165/G166/G167 G181/G183/G184 Service ManualJosineison RochaNoch keine Bewertungen
- Visit For More DIY ProjectsDokument7 SeitenVisit For More DIY ProjectsAvi KarmonNoch keine Bewertungen
- SRS PDFDokument60 SeitenSRS PDFМиша ШаулаNoch keine Bewertungen
- Easyseed 1-2-3 Steps To Planting Bermuda Grass LawnsDokument4 SeitenEasyseed 1-2-3 Steps To Planting Bermuda Grass LawnsJelaiNoch keine Bewertungen
- Octagon Picnic TableDokument24 SeitenOctagon Picnic TableAttila Dienes100% (2)
- 2007 Nissan Xterra 25Dokument36 Seiten2007 Nissan Xterra 25Roma Roma100% (1)
- Autel Maxicheck Pro. User ManualDokument145 SeitenAutel Maxicheck Pro. User ManualJesus Almanzar SantosNoch keine Bewertungen
- SharpeningwDMT 2016 PDFDokument15 SeitenSharpeningwDMT 2016 PDFPat peartersNoch keine Bewertungen
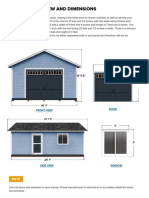
- Basic Overview and Dimensions: Front View DoorDokument6 SeitenBasic Overview and Dimensions: Front View DooraditzuNoch keine Bewertungen
- Weedeater One Service ManualDokument20 SeitenWeedeater One Service ManualBrandon HarveyNoch keine Bewertungen
- E 1Dokument57 SeitenE 1Luis FilipeNoch keine Bewertungen
- How To Tile A ShowerDokument8 SeitenHow To Tile A ShowerRi SovannaphumiNoch keine Bewertungen
- 3× Annual "Best Of" Apple Podcasts 700+ Million Episodes Downloaded 10,000+ 5-STAR REVIEWSDokument35 Seiten3× Annual "Best Of" Apple Podcasts 700+ Million Episodes Downloaded 10,000+ 5-STAR REVIEWSnarang.gp5704Noch keine Bewertungen
- Briggs and Stratton Power Washer PartsDokument30 SeitenBriggs and Stratton Power Washer Partsdelboy1974Noch keine Bewertungen
- Sheetrock Gypsum Panels Installation GuideDokument26 SeitenSheetrock Gypsum Panels Installation Guidew_christopher_miller@gmail_comNoch keine Bewertungen
- 791VX Installation ManualDokument58 Seiten791VX Installation Manual65gearp100% (1)
- 100 Dollars PDFDokument247 Seiten100 Dollars PDFJai Ganesh SadavanniNoch keine Bewertungen
- David 8Dokument1 SeiteDavid 8antonijevicuNoch keine Bewertungen
- Syncing With Subtitle EditDokument3 SeitenSyncing With Subtitle EditantonijevicuNoch keine Bewertungen
- 1 BrnoStudiesEnglish 42-2016-2 7 PDFDokument22 Seiten1 BrnoStudiesEnglish 42-2016-2 7 PDFantonijevicuNoch keine Bewertungen
- Zarathustra and The Children ofDokument20 SeitenZarathustra and The Children ofantonijevicuNoch keine Bewertungen
- ANNIHILATIONDokument1 SeiteANNIHILATIONantonijevicuNoch keine Bewertungen
- Klasična Muzika - Youtube ListaDokument6 SeitenKlasična Muzika - Youtube ListaantonijevicuNoch keine Bewertungen
- Episodes: List of Lost EpisodesDokument5 SeitenEpisodes: List of Lost EpisodesantonijevicuNoch keine Bewertungen
- EeeDokument3 SeitenEeeantonijevicuNoch keine Bewertungen
- Plan AlfaDokument1 SeitePlan AlfaantonijevicuNoch keine Bewertungen
- EeeeeeerrrrrttDokument1 SeiteEeeeeeerrrrrttantonijevicuNoch keine Bewertungen
- Adrenal Carcinoma - A Case StudyDokument3 SeitenAdrenal Carcinoma - A Case StudyНиколина ГроздановскаNoch keine Bewertungen
- Pheochromocytoma PresentationDokument28 SeitenPheochromocytoma PresentationMoriel PimentelNoch keine Bewertungen
- Sample MedSurg Exam NursingDokument16 SeitenSample MedSurg Exam Nursingteabagman0% (1)
- NBME 11 Answers To All SectionsDokument101 SeitenNBME 11 Answers To All SectionsBenjaminTan100% (5)
- Parathyroid Gland and Other Endocrine GlandsDokument35 SeitenParathyroid Gland and Other Endocrine GlandsDrRahma Ali HeissNoch keine Bewertungen
- Mnemonics For USMLE Step 1Dokument33 SeitenMnemonics For USMLE Step 1Sara Sabra100% (9)
- Pheochromocytoma and HomoeopathyDokument13 SeitenPheochromocytoma and HomoeopathyDr. Rajneesh Kumar Sharma MD HomNoch keine Bewertungen
- Endocrine System BulletsDokument28 SeitenEndocrine System Bulletswinner gift flowersNoch keine Bewertungen
- PheochromocytomaDokument24 SeitenPheochromocytomacamelle sisonNoch keine Bewertungen
- Internal Medicine Practice Questions 131224154809 Phpapp02Dokument184 SeitenInternal Medicine Practice Questions 131224154809 Phpapp02MAI100% (1)
- Dr. Faiza Hashim SoomroDokument25 SeitenDr. Faiza Hashim SoomroFaiza Hashim SoomroNoch keine Bewertungen
- Bexarotene Induced Central HypothyroidisDokument257 SeitenBexarotene Induced Central HypothyroidisAnghel Ana-MariaNoch keine Bewertungen
- ENDOCRINE DISORDERS (Autosaved)Dokument81 SeitenENDOCRINE DISORDERS (Autosaved)Princewill SeiyefaNoch keine Bewertungen
- 2016 Imitadores de PreeclmapsiaDokument9 Seiten2016 Imitadores de PreeclmapsiaMaria del Pilar Devis MoralesNoch keine Bewertungen
- Essentials of Diagnosis: Pheochromocytoma & ParagangliomaDokument10 SeitenEssentials of Diagnosis: Pheochromocytoma & ParagangliomaAbdul QuyyumNoch keine Bewertungen
- Milion So2al SurgeryDokument261 SeitenMilion So2al Surgerydocmaaas100% (2)
- NCCN NeuroendokrinDokument187 SeitenNCCN NeuroendokrinDavid DwiputeraNoch keine Bewertungen
- Endocrine Quiz AnswersDokument31 SeitenEndocrine Quiz AnswersDr Sumant Sharma100% (2)
- Pheochromocytoma Poster FINALDokument1 SeitePheochromocytoma Poster FINALJulie-Thuy Nguyen100% (1)
- 2018 - Dr. Mahatma - Syndrome MetabolikDokument79 Seiten2018 - Dr. Mahatma - Syndrome MetabolikDEWI MULYANINoch keine Bewertungen
- Question Bank: Chapterwise (Wbuhs)Dokument188 SeitenQuestion Bank: Chapterwise (Wbuhs)Saikat MondalNoch keine Bewertungen
- Addison+conn+cush+feo+adr IncidentalomaDokument65 SeitenAddison+conn+cush+feo+adr IncidentalomaMjn BausatNoch keine Bewertungen
- X FilesDokument47 SeitenX FilespopNoch keine Bewertungen
- Chemical Shift MRI of The Adrenal GlandDokument19 SeitenChemical Shift MRI of The Adrenal Glandjturos2003Noch keine Bewertungen
- Path Lab Name: Onyedika Egbujo No: #671 Topic: PheochromocytomaDokument4 SeitenPath Lab Name: Onyedika Egbujo No: #671 Topic: PheochromocytomaOnyedika EgbujoNoch keine Bewertungen
- Hesi Exit Exam RN 2017 2018 Most Recent UpdatedDokument38 SeitenHesi Exit Exam RN 2017 2018 Most Recent Updatedbhangglassilyihpok100% (12)
- Pheochromocytoma: Dr. Suvyl Rodricks Dr. Meera KharbandaDokument74 SeitenPheochromocytoma: Dr. Suvyl Rodricks Dr. Meera KharbandaRichgirl DayawonNoch keine Bewertungen
- Comp ReDokument8 SeitenComp RervanguardiaNoch keine Bewertungen
- Learning Objectives:: Pathophysiology & Therapeutics, I (MSPR 521) Lecture No. 14Dokument9 SeitenLearning Objectives:: Pathophysiology & Therapeutics, I (MSPR 521) Lecture No. 14adzhangNoch keine Bewertungen