Beruflich Dokumente
Kultur Dokumente
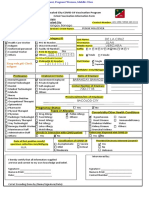
Untitled
Hochgeladen von
api-227612210Originalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Untitled
Hochgeladen von
api-227612210Copyright:
Verfügbare Formate
7 Basic Nursing Skills
Vital signs measurements that show how well the vital organs of the body are working; consist of body temperature, pulse, respirations, blood pressure, and level of pain.
7 Basic Nursing Skills
Monitor, document, and report on the following vital signs: Temperature Pulse Rate of respirations Blood pressure Pain level
7 Basic Nursing Skills
Notify the nurse in any of these cases: Resident has a fever Respiratory or pulse rate is too rapid or slow Blood pressure changes Pain is worsening or unrelieved
7 Basic Nursing Skills
Transparency 7-1: Normal Ranges for Vital Signs Temperature Oral Rectal Axillary Fahrenheit 97.6-99.6 98.6-100.6 96.6-98.6 Celsius 36.5-37.5 37.0-38.1 36.0-37.0
Pulse: 60-100 beats per minute Respirations: 12-20 respirations per minute Blood Pressure: Normal: Systolic 100-119 Diastolic 60-79 Prehypertension: Systolic 120-139 Diastolic 80-89 High: 140/90 or above Low: Below 100/60
7 Basic Nursing Skills
Remember these things about monitoring body temperature: Age, illness, stress, environment, exercise, and the circadian rhythm all affect temperature. There are four sites for measuring (mouth, rectum, armpit, ear). Oral temperatures cannot be taken on someone who is unconscious, has recently had facial or oral surgery, is younger than 5 years old, is confused, is heavily sedated, is likely to have a seizure, is coughing, is using oxygen, has facial paralysis, has a nasogastric tube, has sores, redness, swelling, or pain in the mouth, or has an injury to the face or neck
7 Basic Nursing Skills
Remember when monitoring body temperature (contd.): Mercury-free thermometers are safer than mercury glass thermometers and are required in some states. Mercury-free thermometers and glass thermometers operate identically. Rectal temperatures are most accurate, but taking rectal temperature can be dangerous with some residents. Axillary temperatures are considered least accurate.
7 Basic Nursing Skills
Remember these points about taking rectal temperature: Explain what you will do before starting. Be reassuring. Hold onto thermometer at all times. Wear gloves. The privacy of the resident is important. Thermometer must be lubricated for this procedure. The privacy of the resident is important.
7 Basic Nursing Skills
Remember these things about taking typanic and axillary temperature: Tympanic thermometers are fast and accurate. The tympanic thermometer will only go into the ear 1/4 - 1/2 inch. Axillary temperatures are much less reliable. Axillary temperatures can be safer if residents are confused, disoriented, uncooperative, or have dementia.
7 Basic Nursing Skills
Radial pulse the pulse located on the inside of the wrist, where the radial artery runs just beneath the skin. Brachial pulse the pulse inside the elbow, about 1 to 1 1/2 inches above the elbow.
7 Basic Nursing Skills
Remember these things about monitoring pulse: Pulse is the number of heartbeats per minute. Pulse is commonly taken at the wrist where radial artery runs. Normal rate is 60-100 beats per minute for adults. Normal rate is 100-120 beats per minute for small children, as high as 120-140 for newborns. Pulse may be affected by exercise, fear, anger, anxiety, heat, medications and pain. Rapid pulse may result from fever, infection, or heart failure. Slow/weak pulse may indicate dehydration, infection, or shock.
7 Basic Nursing Skills
Remember these things about counting respirations: A breath includes both inspiration and expiration. Normal adult rate is 12-20 breaths per minute. Normal rate for infants is 30-40 breaths per minute. Do the counting immediately after taking the pulse. Do not let the resident know you are counting breaths.
7 Basic Nursing Skills
Systolic first measurement of blood pressure; phase when the heart is at work, contracting and pushing the blood from the left ventricle of the heart. Diastolic second measurement of blood pressure; phase when the heart relaxes or rests.
7 Basic Nursing Skills
Remember these facts about blood pressure: The two parts are systolic (top number) and diastolic (bottom number). Normal range is: S=100 to 119, D=60 to 79. Blood pressure measurements between 120/80 and 139/89 were once considered normal but are now considered prehypertension. Brachial artery at the elbow is used. Equipment used is stethoscope and sphygmomanometer. An electronic sphymomanometer may be available. If so, you will be trained in its use. The cuff must first be completely deflated.
7 Basic Nursing Skills
Facts about blood pressure (contd.): Never measure blood pressure on an arm that has an IV, a dialysis shunt, or any medical equipment. Avoid a side with a cast, recent trauma, paralysis from a stroke, burns, or mastectomy. One-step method does not include getting an estimated systolic before beginning. Two-step method does require getting an estimated systolic.
7 Basic Nursing Skills
2. Explain the importance of monitoring vital signs REMEMBER: It is not always easy to perfect the skill of hearing the first and last sounds of the blood pressure. You may have to do the procedure over and over again before you are comfortable with it.
7 Basic Nursing Skills
2. Explain the importance of monitoring vital signs Remember the following about pain management: Pain is as important to monitor as vital signs. Pain is an experience that is uncomfortable and different for each person. Take complaints of pain seriously. Observe and report carefully since care plans are based on your reports. Ask questions to get accurate information. Pain is not a normal part of aging.
7 Basic Nursing Skills
2. Explain the importance of monitoring vital signs Observe and report these signs and symptoms of pain: Increased pulse, respirations, and blood pressure Sweating Nausea Vomiting Tightening the jaw Squeezing eyes shut Holding a body part tightly Frowning Grinding teeth
7 Basic Nursing Skills
2. Explain the importance of monitoring vital signs Signs and symptoms of pain (contd.): Increased restlessness Agitation or tension Change in behavior Crying Sighing Groaning Breathing heavily Difficulty moving or walking
7 Basic Nursing Skills
Review the following points about weight: Resident will be weighed repeatedly during his or her stay, and any change in weight should be reported immediately. Some residents will be weighed on a wheelchair scale. The weight of the wheelchair may need to be subtracted from a residents weight. Residents may need to be weighed on a bed scale.
7 Basic Nursing Skills
Restraint a physical or chemical way to restrict voluntary movement or behavior. Restraint-free the state of being free of restraints and not using restraints for any reason. Restraint alternatives any intervention used in place of a restraint or that reduces the need for a restraint.
7 Basic Nursing Skills
4. Explain restraints and how to promote a restraint-free Restraints were Keep person Keep person Keep person Prevent falls used from from from in the past for the following reasons: hurting self or others pulling out tubing wandering
7 Basic Nursing Skills
4. Explain restraints and how to promote a restraint-free REMEMBER: Restraint usage is illegal in many states. Restraints can only be used with a doctors order. It is against the law for staff to apply restraints for convenience or discipline.
7 Basic Nursing Skills
Transparency 7-2: Problems from Restraint Use Reduced blood circulation Stress on the heart Incontinence Constipation Weakened muscle and bones Loss of bone mass Muscle atrophy Pressure sores Risk of suffocation Pneumonia
7 Basic Nursing Skills
Transparency 7-2: Problems from Restraint Use (contd.) Less activity leading to poor appetite Sleep disorders Loss of dignity Loss of independence Increased agitation or depression Poor self-esteem Possible injury or death
7 Basic Nursing Skills
Handout 7-3: Restraint Alternatives Improve safety measures. Keep call light within reach. Answer call lights promptly. Ambulate the person when he or she is restless. Provide activities for those who wander at night. Encourage activities and independence. Give frequent help with toileting. Offer food or drink. Offer reading materials.
7 Basic Nursing Skills
Intake the fluid a person consumes; also called input. Output all fluid that is eliminated from the body; includes fluid in urine, feces, vomitus, perspiration, and moisture in the air that is exhaled. Fluid balance taking in and eliminating equal amounts of fluid.
7 Basic Nursing Skills
Transparency 7-4: Conversion Table A milliliter (mL or ml) is a unit of measure equal to one cubic centimeter (cc). 1 oz. = 30 cc or 30 ml 2 oz. = 60 cc 3 oz. = 90 cc 4 oz. = 120 cc 5 oz. = 150 cc 6 oz. = 180 cc 7 oz. = 210 cc 8 oz. = 240 cc cup = 2 oz. = 60 cc cup = 4 oz. = 120 cc 1 cup = 8 oz. = 240 cc
7 Basic Nursing Skills
Specimen a sample. Hat in health care, a collection container that is sometimes inserted into a toilet to collect and measure urine or stool. Mid-stream specimen a type of urine specimen in which the first and last urine are not included in the sample.
7 Basic Nursing Skills
5. Define fluid balance and explain intake and output (I&O) Remember these things about collecting specimens: NAs must wear gloves for these procedures. Tagging and storing specimens correctly is important. Be sensitive to the fact that residents may find it embarrassing or uncomfortable to have others handling their body wastes. If you feel the task is unpleasant, do not make it known. Remain professional. Remind students after they discard their gloves after collecting specimens, they must wash their hands.
7 Basic Nursing Skills
5. Define fluid balance and explain intake and output (I&O) Remember these things about collecting a routine urine specimen: Do not include toilet paper with sample. Help with perineal care after urination if necessary. Fill container at least half full. Do not touch the inside of container. Complete label accurately. Wash your hands after completing the procedure.
7 Basic Nursing Skills
Catheter a thin tube inserted into the body used to drain or inject fluids. Straight catheter a catheter that does not remain inside the person; it is removed immediately after urine is drained. Indwelling catheter a catheter that remains inside the bladder for a period of time; the urine drains into a bag Condom catheter catheter that has an attachment on the end that fits onto the penis; also called an external or Texas catheter.
7 Basic Nursing Skills
5. Define fluid balance and explain intake and output (I&O) Remember these guidelines for catheter care: Keep drainage bag lower than the residents hips or bladder to prevent infection. Keep the drainage bag off the floor. Prevent kinks and twists in tubing. Keep genital area clean.
7 Basic Nursing Skills
5. Define fluid balance and explain intake and output (I&O) Observe and report when providing catheter care: Bloody urine Catheter bag does not fill after several hours Catheter bag fills suddenly Catheter is not in place Urine leaks from catheter Resident reports pain or pressure Odor
7 Basic Nursing Skills
5. Define fluid balance and explain intake and output (I&O) REMEMBER: Always wear gloves and wash hands when dealing with catheters.
7 Basic Nursing Skills
Combustion the process of burning. Flammable easily ignited and capable of burning quickly.
7 Basic Nursing Skills
6. Explain care guidelines for different types of tubing Remember these guidelines for oxygen safety: Remove fire hazards. Post No Smoking and Oxygen in Use signs. Do not allow smoking around oxygen equipment. Do not allow flames around oxygen (this includes candles). Learn how to turn oxygen off in case of fire if facility allows this. Never adjust oxygen level. Report skin irritation.
7 Basic Nursing Skills
6. Explain care guidelines for different types of tubing Remember your role in caring for a resident with an IV: NAs never insert or remove IV lines. NAs do not care for the IV site. NAs only observe the site for changes or problems and report if Needle falls out Tubing disconnects Dressing is loose Blood is in tubing
7 Basic Nursing Skills
6. Explain care guidelines for different types of tubing NAs role in caring for a resident with an IV (contd.): Site is swollen or discolored Resident complains of pain IV bag breaks or fluid level does not decrease IV fluid not dripping IV fluid nearly gone Pump beeps Pump is dropped
7 Basic Nursing Skills
6. Explain care guidelines for different types of tubing In caring for residents with IVs, DO NOT Take blood pressure on an arm with an IV Get the site wet Pull or catch the tubing in anything Leave the tubing kinked Lower the IV bag below the IV site Touch the clamp Disconnect IV from pump or turn off alarm
7 Basic Nursing Skills
6. Explain care guidelines for different types of tubing REMEMBER: Do not get an IV site wet or lower the bag below the IV site. Special care is needed when performing some care procedures on a resident with an IV. Never pull or catch on IV tubing when assisting with care.
7 Basic Nursing Skills
7. Discuss a resident's unit and related care REMEMBER: A residents unit is his or her home and must be treated with respect. Always knock on the door and wait for permission to enter. A residents items must not be moved without permission.
7 Basic Nursing Skills
7. Discuss a resident's unit and related care Equipment usually found in a residents unit includes the following: Electric or manual bed Bedside stand Urinal/bedpan and covers Wash basin Emesis basin Soap dish and soap Bath blanket
7 Basic Nursing Skills
7. Discuss a resident's unit and related care Certain items may not be placed on an overbed table: Soiled items Bedpans Urinals
7 Basic Nursing Skills
7. Discuss a resident's unit and related care Remember the following about call lights: They must always be placed within residents reach. They must be answered immediately, no matter how many times a resident has used the call light. NAs should respond kindly each time a resident uses his or her call light.
7 Basic Nursing Skills
7. Discuss a resident's unit and related care Remember these guidelines for caring for a residents unit: Clean the overbed table after each use. Keep equipment clean and in good condition. Report problems with equipment to nurse or according to facility guidelines. Keep call light within reach. Remove meal trays promptly, then remove crumbs and straighten linens. Change linens if they are wet, soiled, or wrinkled.
7 Basic Nursing Skills
8. Explain the importance of sleep and perform proper Lack of sleep can cause the following problems: Decreased mental function Reduced reaction time Irritability Decreased immune system function
7 Basic Nursing Skills
8. Explain the importance of sleep and perform proper Watch for these things when a resident is not sleeping well: Sleeping too much during the day Consuming too much caffeine Dressing in night clothes during the day Eating too late at night Refusing medication ordered for sleep Taking new medications TV, radio, or light on late at night Pain
7 Basic Nursing Skills
Occupied bed a bed made while a person is in the bed. Unoccupied bed a bed made while nobody is in the bed. Closed bed a bed completely made with the bedspread and blankets in place. Open bed a bed made with linen fanfolded down to the foot of the bed.
7 Basic Nursing Skills
Consider these reasons for careful bedmaking: Damp and wrinkled sheets keep the resident from sleeping well. Microorganisms thrive in moist, warm places and damp, unclean bedding may cause infection or disease. Sheets that are not flat increase risk for pressure sores.
7 Basic Nursing Skills
Remember these guidelines for bedmaking: Keep linens wrinkle-free and tidy. Wash hands before handling clean linen. Hold soiled linens away from your body. If dirty linen touches your uniform, your uniform becomes contaminated. Do not shake linen or clothes. Put on gloves before removing bed linens. Look for personal items before removing linens. When removing linens, fold or roll linen so the dirtiest area is inside.
7 Basic Nursing Skills
REMEMBER: NAs do not change sterile dressings,which cover open or draining wounds. Non-sterile dressings are for wounds that have less chance of infection. NAs may assist with non-sterile dressing changes.
7 Basic Nursing Skills
9. Discuss dressings and bandages Remember these points: Non-sterile bandages hold dressings in place, secure splints, and support and protect body parts. They may decrease swelling from an injury. NAs may assist with use of an elastic bandage. Some states allow NAs to apply and remove elastic bandages. Follow your facilitys policy.
7 Basic Nursing Skills
9. Discuss dressings and bandages Guidelines for elastic bandages (contd.): Check bandage often to be sure it doesnt become wrinkled or loose. 15 minutes after bandage is applied check for signs of poor circulation; loosen if any of these signs are present: Swelling Bluish (cyanotic) skin Shiny, tight skin Skin cold to touch Sores Numbness Tingling Pain or discomfort
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- 4 Body Systems and Related Conditions: Urinary IncontinenceDokument86 Seiten4 Body Systems and Related Conditions: Urinary Incontinenceapi-227612210Noch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- 10 Caring For Yourself: 1. Describe How To Find A JobDokument25 Seiten10 Caring For Yourself: 1. Describe How To Find A Jobapi-227612210Noch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- 4 Body Systems and Related Conditions: HomeostasisDokument78 Seiten4 Body Systems and Related Conditions: Homeostasisapi-227612210Noch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Nurse Aide TestDokument13 SeitenNurse Aide TestDiana KennedoNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- 4 Body Systems and Related Conditions: HomeostasisDokument68 Seiten4 Body Systems and Related Conditions: Homeostasisapi-227612210Noch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Respiratory SystemDokument81 SeitenThe Respiratory Systemapi-227612210Noch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- 9 Rehabilitation and Restorative Care: Define The Following TermsDokument21 Seiten9 Rehabilitation and Restorative Care: Define The Following Termsapi-227612210Noch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- UntitledDokument43 SeitenUntitledapi-227612210Noch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Chapter 6: Personal Care Skills: HygieneDokument41 SeitenChapter 6: Personal Care Skills: Hygieneapi-227612210Noch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- UntitledDokument32 SeitenUntitledapi-227612210Noch keine Bewertungen
- 4 Body Systems and Related Conditions: HomeostasisDokument59 Seiten4 Body Systems and Related Conditions: Homeostasisapi-227612210Noch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Chapter 5: Confusion, Dementia & Alzheimer's DiseaseDokument29 SeitenChapter 5: Confusion, Dementia & Alzheimer's Diseaseapi-227612210Noch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Chapter 3: Understanding Your Residents: Psychosocial NeedsDokument32 SeitenChapter 3: Understanding Your Residents: Psychosocial Needsapi-227612210Noch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- UntitledDokument56 SeitenUntitledapi-227612210Noch keine Bewertungen
- Chapter 3: Understanding Your Residents: Psychosocial NeedsDokument32 SeitenChapter 3: Understanding Your Residents: Psychosocial Needsapi-227612210Noch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Chapter 2: Foundations of Resident Care: CommunicationDokument43 SeitenChapter 2: Foundations of Resident Care: Communicationapi-227612210Noch keine Bewertungen
- UntitledDokument56 SeitenUntitledapi-227612210Noch keine Bewertungen
- UntitledDokument32 SeitenUntitledapi-227612210Noch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Summary Hivaids SetDokument747 SeitenSummary Hivaids Setv8qwxqb2shNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Trimax General Hospital & Maternity I.C.U Crash Cart Check ListDokument4 SeitenTrimax General Hospital & Maternity I.C.U Crash Cart Check ListShaky AhmedNoch keine Bewertungen
- Biolase TimelineDokument19 SeitenBiolase Timelinemohamed radwanNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Funda ExamDokument18 SeitenFunda Examis_aradanasNoch keine Bewertungen
- OPHTHA Case Report Diabetic RetinopathyDokument51 SeitenOPHTHA Case Report Diabetic RetinopathyJessa MeaNoch keine Bewertungen
- Focus On Adult Health Medical Surgical Nursing Pellico Edition Test BankDokument8 SeitenFocus On Adult Health Medical Surgical Nursing Pellico Edition Test BankCarolineAndersoneacmg100% (33)
- 901-Article Text-1856-1-10-20221129Dokument6 Seiten901-Article Text-1856-1-10-20221129Made NujitaNoch keine Bewertungen
- Vaccination Form (Sample)Dokument1 SeiteVaccination Form (Sample)Godfrey Loth Sales Alcansare Jr.Noch keine Bewertungen
- Amniotic Fluid EmbolismDokument13 SeitenAmniotic Fluid EmbolismMARIANN JEAN ANDREA CULANAG MATALINESNoch keine Bewertungen
- 2 - 5201750207762531221 EntDokument561 Seiten2 - 5201750207762531221 EntArun Raj100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Mci Psychiatry SyllabusDokument14 SeitenMci Psychiatry SyllabusDasharath SawantNoch keine Bewertungen
- Nurs208 K4yDokument12 SeitenNurs208 K4yapi-347145789100% (2)
- African Swine Fever: Pesti Porcine Africaine, Peste Porcina Africana, Maladie de MontgomeryDokument52 SeitenAfrican Swine Fever: Pesti Porcine Africaine, Peste Porcina Africana, Maladie de MontgomeryDecereen Pineda Rodrigueza100% (1)
- Pre Op GuidelinesDokument11 SeitenPre Op GuidelinesHanif FebrianNoch keine Bewertungen
- Nama Obat Indikasi / Kegunaan Komposisi /nama Generik: Brochifar Plus Kap PCT, DMP, Ppa, CTM Batuk, Flu, DemamDokument52 SeitenNama Obat Indikasi / Kegunaan Komposisi /nama Generik: Brochifar Plus Kap PCT, DMP, Ppa, CTM Batuk, Flu, Demamrio1995Noch keine Bewertungen
- Cqi Indicators As Per Nabh 5Th Edition: S. No. Standard Ref. Deptt. KPI Formula FrequencyDokument3 SeitenCqi Indicators As Per Nabh 5Th Edition: S. No. Standard Ref. Deptt. KPI Formula FrequencyNatasha Bhasin91% (11)
- UntitledDokument8 SeitenUntitledapi-271638639Noch keine Bewertungen
- BVCCT-501 Cardiac Catheterization Laboratory BasicsDokument52 SeitenBVCCT-501 Cardiac Catheterization Laboratory BasicsManisha khan100% (1)
- Spex Practice Test1Dokument29 SeitenSpex Practice Test1nowNoch keine Bewertungen
- Philippine Heart Association Bls-Acls Online Training ProgramDokument9 SeitenPhilippine Heart Association Bls-Acls Online Training ProgramJoyNoch keine Bewertungen
- Nutri QuizDokument5 SeitenNutri QuizAngel Kaye FabianNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Cardiolab Practical-PharmacologyDokument2 SeitenCardiolab Practical-PharmacologyGul HassanNoch keine Bewertungen
- Herbs or Natural Products CancerDokument16 SeitenHerbs or Natural Products CancerANGELO NHAR100% (1)
- Psychiatric Mental Health Nursing Concepts of Care in Evidence Based Practice Townsend 7th Edition Test BankDokument24 SeitenPsychiatric Mental Health Nursing Concepts of Care in Evidence Based Practice Townsend 7th Edition Test BankAnitaCareyfemy100% (35)
- Golongan ObatDokument29 SeitenGolongan ObatMala PanoNoch keine Bewertungen
- Biotechnology & Drug Discovery.Dokument35 SeitenBiotechnology & Drug Discovery.IrsaNoch keine Bewertungen
- Pulmonary EdemaDokument10 SeitenPulmonary EdemaNader Smadi100% (6)
- Basic Anaestetic DrugsDokument1 SeiteBasic Anaestetic DrugsLuthfi AfiatNoch keine Bewertungen
- Dialysis MachineDokument1 SeiteDialysis MachineMarifer NazNoch keine Bewertungen
- BAT and KCL Study ProposalDokument4 SeitenBAT and KCL Study ProposalAnuNoch keine Bewertungen