Beruflich Dokumente
Kultur Dokumente
Optic Neuritis
Hochgeladen von
Widodo Adi PrasetyoOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Optic Neuritis
Hochgeladen von
Widodo Adi PrasetyoCopyright:
Verfügbare Formate
Optic Neuritis
Your doctor thinks that you have had an episode of optic neuritis. This is the most common cause of sudden visual loss in a young patient. It is often associated with discomfort in or around the eye, particularly with eye movement. Anatomy: We do not see with our eyes. Our eyes send a message via the optic nerves to the back part of the brain (occipital lobes) where the information is interpreted as an image.
The optic nerve fibers are coated with myelin to help them conduct the electrical signals back to your brain. Physiology: In the most common form of optic neuritis, the optic nerve has been attacked by the body's overactive immune system. The immune system is very important to our well being. It is responsible for fighting off bacteria and viruses that can cause infection. In optic neuritis and other autoimmune diseases, the body's immune system has decided that otherwise normal tissues are foreign and therefore have attacked it. In the case of optic neuritis, the myelin coating the optic nerve has been targeted as foreign material. A viral infection that may have occurred years, or even decades, earlier may have set the stage for an acute episode of optic neuritis. What triggers the sudden loss of vision and optic nerve dysfunction at this time is unknown but probably occurs in individuals with a certain type of immune system. The inflammation associated with optic neuritis can result in discomfort (particularly with movement of the eye). In some cases of optic neuritis there may be more extensive involvement including the other optic nerve, the chiasm (where the two optic nerves come together), or other tissues in the brain. Symptoms: The most common symptom of optic neuritis is sudden decrease in vision. Patients may describe this as blurred vision, dark vision, dim vision or simply loss of vision in the center or part or all of the visual field. In mild cases, it may look like the contrast is turned down or that colors appear washed out. This may vary and, not infrequently, will progress from the time it is first noticed. The second most common symptom associated with optic neuritis is discomfort in or around the eye often made worse by movement of the eye.
Signs: Optic neuritis may be difficult to diagnose, as your eye looks perfectly normal. Often the inside of your eye also looks normal. A few patients with optic neuritis have swelling of the optic disc (the beginning of the optic nerve) at the back of the eye. This is referred to as papillitis. One sign usually detected by your eye doctor is the presence of an afferent pupillary defect. This indicates that there is less light being sensed by the affected eye than the opposite eye. This is found by swinging a bright light back and forth between your two eyes while observing how your pupil reacts. Prognosis: The pain will go away, usually in a few days. The vision problems will improve in the majority (92%) of patients. There are rare patients who have continued progressive loss of vision. Even in the 92% that improve, often they do not return completely to normal. Patients may be left with blurred, dark, dim, or distorted vision. Frequently colors look different or "washed out." Visual recovery usually takes place over a period of weeks to months, although both earlier and later improvement is possible. Late variations in vision are common, often associated with exercise or taking a hot shower or bath. This is known as Uhthoff's phenomena and is probably related to damage to the myelin coating. Patients who notice this problem are not more likely to get worse. Optic neuritis can recur involving the same eye, the other eye or other parts of the central nervous system (brain and spinal cord). This may result in recurrent episodes of decreased or loss of vision or problems with weakness, numbness or other signs of brain involvement. An MRI scan can give us to give a rough guess as to the likelihood of recurrence.
It will not completely exclude the possibility of future episodes or guarantee that they will happen. Other testing techniques are sometimes used to confirm the suspicion of optic neuritis. These may include visual evoked potentials (a test where you are shown a checkerboard of light and signals are recorded fromelectrodes on your scalp) that can show a delay in conduction due to the damage to the myelin. Treatment: A study (the Optic Neuritis Treatment Trial (ONTT)) suggested that the likelihood of recovery at 6 months was equal whether they were treated with steroids or sugar pills. Patients treated with oral (pills) steroids seemed to have a higher chance of recurrent episodes. Therefore, steroid pills are not recommended as treatment. Patients who were treated with intravenous (given by needle) steroids did have a slightly more rapid recovery of their vision, although the final visual outcome was not better than in those who were not treated. Thus, IV steroids can be recommended for patients with severe involvement or involvement of both eyes. The ONTT also suggested that IV steroids in those patients at high risk (as determined by their MRI scan) could have a reduction in the chances of a second episode over the next three years. Recent studies have suggested that the chance of developing a recurrent episode may be
reduced by starting other medications after IV steroids in those patients at high risk. MRI is important in suggesting the chance of recurrence or progression. Your doctor can address questions about possible treatment with you. Frequently asked questions:
What caused this to happen? We don't have a complete understanding of optic neuritis at this time. It is likely that it represents a combination of a particular form of immune system combined with a previous stimulation possibly a virus. What's going to happen to my vision? In the vast majority of patients, your vision will improve. It may not improve to normal, but it is likely that there will be a substantial improvement whether or not you are treated. Can treatment with steroids make this better? Treatment with IV steroids has been demonstrated to accelerate recovery but it will not change the ultimate level of recovery on average. We have no way to guarantee that vision will recover and in some patients it will not. Do I have MS? Multiple sclerosis (MS) is a disease process where the body's immune system attacks multiple areas in multiple episodes. An episode of optic neuritis may be the first indication of multiple sclerosis. With a single episode, without other evidence of involvement, we usually cannot make the diagnosis at that time. An MRI scan may be helpful in dividing those patients into high and low risks. Finding evidence of other areas of inflammation on MRI scanning suggests you may be at higher risk for recurrent episodes and thus MS. Your doctor may suggest consultation with a neurologist to discuss treatments that might reduce the risk of recurrent disease. Even a normal scan does not guarantee that episodes may not recur over years. Whether or not this turns out to be MS in the future, the prognosis in terms of visual recovery is still good for this particular episode. Can I prevent MS? The ONTT demonstrated that the use of high dose intravenous steroids in patients at high risk (2 or more spots on MRI scan) may delay the onset of MS. Recent data suggests that some of the newer medications may also decrease the chance of having another neurologic event. Thus it may be important to recognize those patients at higher risk to start earlier treatment. This is best determined by MRI. There is no treatment that will absolutely prevent the development of multiple sclerosis.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Social Welfare Administrartion McqsDokument2 SeitenSocial Welfare Administrartion McqsAbd ur Rehman Vlogs & VideosNoch keine Bewertungen
- FreezingDokument59 SeitenFreezingManoj Rathod100% (1)
- Packaged Drinking Water Project ProfileDokument5 SeitenPackaged Drinking Water Project ProfileArpna BhatiaNoch keine Bewertungen
- UK Code of Practice For Tampon Manufactures and DistributorsDokument9 SeitenUK Code of Practice For Tampon Manufactures and DistributorsFuzzy_Wood_PersonNoch keine Bewertungen
- A. Define Infertility: Objectives: Intended Learning Outcomes That TheDokument2 SeitenA. Define Infertility: Objectives: Intended Learning Outcomes That TheJc Mae CuadrilleroNoch keine Bewertungen
- Pharmacology Mock Exam MCQDokument8 SeitenPharmacology Mock Exam MCQanaeshklNoch keine Bewertungen
- IFCC Visiting LectureDokument3 SeitenIFCC Visiting LectureMaruhum NurNoch keine Bewertungen
- Isolation and Identification of Bacteria ThesisDokument7 SeitenIsolation and Identification of Bacteria Thesisafbtbegxe100% (2)
- SITXWHS001 Assessment 1 (4) Incident ReportDokument7 SeitenSITXWHS001 Assessment 1 (4) Incident Reportpra Deep100% (1)
- Perioperative NursingDokument8 SeitenPerioperative NursingGil Platon Soriano100% (3)
- MicroMaxx 3.3 UG ENG P06435-02B e 1 - 1Dokument200 SeitenMicroMaxx 3.3 UG ENG P06435-02B e 1 - 1Waheed MidoNoch keine Bewertungen
- Dental Restorative Digital Workflow: Digital Smile Design From Aesthetic To Function PDFDokument12 SeitenDental Restorative Digital Workflow: Digital Smile Design From Aesthetic To Function PDFCamilo GuerreroNoch keine Bewertungen
- 32 Vol4 EpaperDokument32 Seiten32 Vol4 EpaperThesouthasian TimesNoch keine Bewertungen
- Qatar Healthcare Facilities Contact GuideDokument3 SeitenQatar Healthcare Facilities Contact GuideShibu KavullathilNoch keine Bewertungen
- Scoring BPSDDokument4 SeitenScoring BPSDayu yuliantiNoch keine Bewertungen
- Prevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDDokument7 SeitenPrevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDMusainah FeisalNoch keine Bewertungen
- Management of Class I Type 3 Malocclusion Using Simple Removable AppliancesDokument5 SeitenManagement of Class I Type 3 Malocclusion Using Simple Removable AppliancesMuthia DewiNoch keine Bewertungen
- Earth Leakage Testing Report: Panel Name: Testing Device: Rccb (Iδn) : 30 MaDokument1 SeiteEarth Leakage Testing Report: Panel Name: Testing Device: Rccb (Iδn) : 30 MaAmjad AlbahtiNoch keine Bewertungen
- MalariaDokument11 SeitenMalariaWynli Fullo AncogNoch keine Bewertungen
- OCPD: Symptoms, Diagnosis and TreatmentDokument4 SeitenOCPD: Symptoms, Diagnosis and TreatmentRana Muhammad Ahmad Khan ManjNoch keine Bewertungen
- 'No Evidence That CT Scans, X-Rays Cause Cancer' - Medical News TodayDokument3 Seiten'No Evidence That CT Scans, X-Rays Cause Cancer' - Medical News TodayDr-Aditya ChauhanNoch keine Bewertungen
- Influence of Social Capital On HealthDokument11 SeitenInfluence of Social Capital On HealthHobi's Important BusinesseuNoch keine Bewertungen
- "PASS" Principles For Predictable PDFDokument10 Seiten"PASS" Principles For Predictable PDFkishan bordaNoch keine Bewertungen
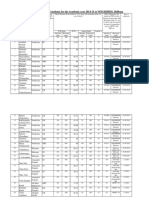
- Admission For 1st Year MBBS Students For The Academic Year 2014-2015Dokument10 SeitenAdmission For 1st Year MBBS Students For The Academic Year 2014-2015Guma KipaNoch keine Bewertungen
- As 2550.5-2002 Cranes Hoists and Winches - Safe Use Mobile CranesDokument8 SeitenAs 2550.5-2002 Cranes Hoists and Winches - Safe Use Mobile CranesSAI Global - APACNoch keine Bewertungen
- Food Production (409) : Sample Question Paper Class X (2018-19) (NSQF)Dokument2 SeitenFood Production (409) : Sample Question Paper Class X (2018-19) (NSQF)Janavi M SNoch keine Bewertungen
- Chapter 22 The First Heart SoundDokument5 SeitenChapter 22 The First Heart SoundAbhilash ReddyNoch keine Bewertungen
- Facts of MaintenanceDokument9 SeitenFacts of Maintenancegeorge youssefNoch keine Bewertungen
- CG A022 01 Shortened Dental ArchDokument5 SeitenCG A022 01 Shortened Dental ArchmahmoudNoch keine Bewertungen
- Case Report: Communication Strategies For Empowering and Protecting ChildrenDokument9 SeitenCase Report: Communication Strategies For Empowering and Protecting ChildrennabilahNoch keine Bewertungen