Beruflich Dokumente
Kultur Dokumente
Neonatal Cardiopulmonary Arrest in The Delivery Room
Hochgeladen von
Reda SoOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Neonatal Cardiopulmonary Arrest in The Delivery Room
Hochgeladen von
Reda SoCopyright:
Verfügbare Formate
Neonatal Cardiopulmonary Arrest in the Delivery Room
Cardiopulmonary arrest of a healthy term infant in the delivery room after an uneventful vaginal delivery is an extremely rare event. We recently encountered 2 such cases in term infants born after uneventful pregnancies and nonmedicated vaginal deliveries. In the first, infant breastfeeding was initiated in the delivery room, unobserved, immediately after birth. A short time later, the infant was found pale and motionless while still on the breast. After resuscitation and NICU care, the infant was discharged without obvious neurologic deficit. Similarly, the second infant initiated breastfeeding unobserved in the delivery room shortly after birth. A few minutes later, the mother noticed that the infant was motionless. After initial resuscitation, respiratory support and inotropic and anticonvulsive therapies were required. During his 3-month stay in the NICU, the results of all investigations, including septic workup, metabolic screen, and echocardiography, were normal. Follow-up examination has noted that the infant is severely neurologically impaired. Our 2 cases are similar to 8 French cases described previously. All those infants were born to primiparous women after uneventful pregnancies and deliveries. In all of those infants, as with ours cases, the cardiopulmonary arrests occurred with the infants in a prone position on their mothers abdomen during the first breastfeeding maneuver. We suggest 2 possible causes of the cardiorespiratory arrest: upper airway obstruction and/or increased vagal tone. Previous reports of catastrophic deterioration during and after breastfeeding have postulated oronasal obstruction. However, these cases occurred after the infants were discharged from the hospital. The alternative theory, implementing increased vagal tone as the cause of the cardiac arrest, is suggested by several studies. In newborns, during the postdelivery period, there is increased vagal tone, and thus this phenomenon can possibly be activated by the initial sucking by the infant on the mothers nipple and/or compounded by initiation of the gastrin vagal axis. Support for this theory is the recent report of vagal overactivity and sudden infant death syndrome. In this study of 15 families with a history of sudden infant death syndrome in 1 sibling, a high percentage of subsequent siblings were found to have symptoms of vagal hyperreactivity, suggesting an autosomal dominant inheritance pattern for this phenomenon. On the other hand, the fact that all the reported cases of arrest in the delivery room occurred in primiparous (and thus inexperienced) mothers suggests that infant position and maternal feeding technique may be the more likely mechanism. The American Academy of Pediatrics, in its 2005 policy statement regarding breastfeeding, states that [h]ealthy infants should be placed and remain in direct skin-to-skin contact with their mothers immediately after delivery until the first feeding is accomplished. This policy clearly should continue to be encouraged. However, given our observation and the experience of others, we recommend that there be proper supervision and attendance by caregivers during the initial breastfeeding in the delivery room by inexperienced primiparous mothers. It is also clear that the careful monitoring and positioning of the infants during this period of maternal-infant bonding be done in an unobtrusive manner so as to allow the new mother-infant dyad the freedom to interact appropriately.
http://pediatrics.aappublications.org/content/118/2/847.full
Push doesn't come to shove in delivery room
A new study is raising questions about one of the most accepted practices in the delivery room: urging women to push during contractions to help the baby come out.
A new study is raising questions about one of the most accepted practices in the delivery room: urging women to push during contractions to help the baby come out. The researchers, writing in the current issue of The American Journal of Obstetrics & Gynecology, say there is no evidence that bearing down during contractions helps either the mother or the child. They also suggest that women who are encouraged to push may be at higher risk for urinary problems after delivery. The study's authors said the findings did not mean that women should never push. Instead, he said, they encouraged women "to do what feels natural to do -- and for some women that would be no pushing." For the study, researchers looked at the birth experiences of more than 300 women. Half were assigned nurse-midwives who encouraged them to take deep breaths, hold them and bear down for 10 seconds at the peak of a contraction. The other women were assigned nursemidwives who told them to do what felt best. The women who were told to push did have shorter deliveries. On average, the study found, their second stage of labour was about 13 minutes shorter.
http://www.canada.com/topics/lifestyle/parenting/story.html?id=c940bc2f-1b4f-4088-aca1-f23b557f1873
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- CHAPTER 27 - Heart Failure With A Preserved Ejection FractionDokument15 SeitenCHAPTER 27 - Heart Failure With A Preserved Ejection FractionReda SoNoch keine Bewertungen
- CHAPTER 61: Diabetes and The Cardiovascular System: Ma. Arnee V. Anico-Tondo, M.D., FPCP (CGH)Dokument1 SeiteCHAPTER 61: Diabetes and The Cardiovascular System: Ma. Arnee V. Anico-Tondo, M.D., FPCP (CGH)Reda SoNoch keine Bewertungen
- Chinese General Hospital and Medical Center Department of Medical Education and Research Research Ethics Review Board (Rerb)Dokument11 SeitenChinese General Hospital and Medical Center Department of Medical Education and Research Research Ethics Review Board (Rerb)Reda SoNoch keine Bewertungen
- CHAPTER 55 - Percutaneous Coronary InterventionDokument1 SeiteCHAPTER 55 - Percutaneous Coronary InterventionReda SoNoch keine Bewertungen
- Trials SummaryDokument12 SeitenTrials SummaryReda SoNoch keine Bewertungen
- Mitral Valve Disease QuizDokument5 SeitenMitral Valve Disease QuizReda SoNoch keine Bewertungen
- Braunwald Chapter KeypointersDokument6 SeitenBraunwald Chapter KeypointersReda SoNoch keine Bewertungen
- Chapter 32 - Genetic Cardiac ArrythmiasDokument7 SeitenChapter 32 - Genetic Cardiac ArrythmiasReda SoNoch keine Bewertungen
- CH 50 - Approach To Patient With Chest PainDokument1 SeiteCH 50 - Approach To Patient With Chest PainReda SoNoch keine Bewertungen
- Answer Key-Mitral ValveDokument6 SeitenAnswer Key-Mitral ValveReda SoNoch keine Bewertungen
- Ward Reflection PaperDokument1 SeiteWard Reflection PaperReda SoNoch keine Bewertungen
- Rapid Response and Cardiac Arrest TeamsDokument11 SeitenRapid Response and Cardiac Arrest TeamsReda SoNoch keine Bewertungen
- Name: - Year LevelDokument6 SeitenName: - Year LevelReda SoNoch keine Bewertungen
- Private Ward Admission Census 1Dokument6 SeitenPrivate Ward Admission Census 1Reda SoNoch keine Bewertungen
- Risk Factors in Developing Diabetic Foot Ulcers Among Patients in DM Foot Clinic at East Avenue Medical Center From January 2013 To January 2015Dokument7 SeitenRisk Factors in Developing Diabetic Foot Ulcers Among Patients in DM Foot Clinic at East Avenue Medical Center From January 2013 To January 2015Reda SoNoch keine Bewertungen
- Tilt Table Testing: Name Age/Sex APDokument1 SeiteTilt Table Testing: Name Age/Sex APReda SoNoch keine Bewertungen
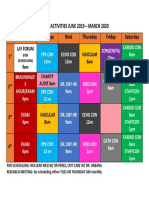
- Vascular Conference: JUNE 2018 - MARCH 2019Dokument2 SeitenVascular Conference: JUNE 2018 - MARCH 2019Reda SoNoch keine Bewertungen
- Evidence-Based Approach to Heart Failure History and Physical ExamDokument5 SeitenEvidence-Based Approach to Heart Failure History and Physical ExamReda SoNoch keine Bewertungen
- Daily Activities 2019Dokument1 SeiteDaily Activities 2019Reda SoNoch keine Bewertungen
- Heart Institute Team Building April 2019Dokument1 SeiteHeart Institute Team Building April 2019Reda SoNoch keine Bewertungen
- Aortic ExamDokument3 SeitenAortic ExamReda SoNoch keine Bewertungen
- Coronary Blood Flow & Myocardial Ischemia Cardiology Fellows Exam July 23, 2018Dokument3 SeitenCoronary Blood Flow & Myocardial Ischemia Cardiology Fellows Exam July 23, 2018Reda SoNoch keine Bewertungen
- Coronary Blood Flow & Myocardial Ischemia Cardiology Fellows Exam July 23, 2018Dokument3 SeitenCoronary Blood Flow & Myocardial Ischemia Cardiology Fellows Exam July 23, 2018Reda SoNoch keine Bewertungen
- 2011 PadDokument19 Seiten2011 PadReda SoNoch keine Bewertungen
- Tilt Table Testing: Name Age/Sex APDokument1 SeiteTilt Table Testing: Name Age/Sex APReda SoNoch keine Bewertungen
- Cardiology census and patient detailsDokument9 SeitenCardiology census and patient detailsReda SoNoch keine Bewertungen
- Marijuana LegalizationDokument5 SeitenMarijuana LegalizationMatt ImpellusoNoch keine Bewertungen
- Case Protocol 3Dokument2 SeitenCase Protocol 3Reda SoNoch keine Bewertungen
- Case Protocol 3Dokument5 SeitenCase Protocol 3Reda SoNoch keine Bewertungen
- Computed Tomography Findings for 8 Cardiovascular PatientsDokument1 SeiteComputed Tomography Findings for 8 Cardiovascular PatientsReda SoNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- B.SC Nursing2018Question PapersFirst YearNursing Foundations FR 4firstDokument1 SeiteB.SC Nursing2018Question PapersFirst YearNursing Foundations FR 4firstJagdeesh PrasadNoch keine Bewertungen
- Merged Document 14 PDFDokument9 SeitenMerged Document 14 PDFMurali SmatNoch keine Bewertungen
- ActTherapyDokument33 SeitenActTherapyRita PokharelNoch keine Bewertungen
- Aubf Module 3 Laboratory Assignment - Macabanding - PrincessDokument5 SeitenAubf Module 3 Laboratory Assignment - Macabanding - PrincessNailah MacabandingNoch keine Bewertungen
- Lec-1h-Excretory System ReviewerDokument12 SeitenLec-1h-Excretory System ReviewerProfessor GhoulNoch keine Bewertungen
- Pauling Therapy Case SummariesDokument29 SeitenPauling Therapy Case SummariesDharmaMaya Chandrahas100% (2)
- Barrier Free ArchitectureDokument3 SeitenBarrier Free ArchitectureAmarjit SahNoch keine Bewertungen
- Combination of Lisinopril and Nifedipine GITS.10Dokument7 SeitenCombination of Lisinopril and Nifedipine GITS.10Andi PermanaNoch keine Bewertungen
- Aconitum NapellusDokument12 SeitenAconitum NapellusMuhammad Mustafa IjazNoch keine Bewertungen
- Hyper-Reflexia in Guillain - Barré Syndrome: Systematic ReviewDokument7 SeitenHyper-Reflexia in Guillain - Barré Syndrome: Systematic ReviewVladimir BasurtoNoch keine Bewertungen
- Teaching Project - BPDokument22 SeitenTeaching Project - BPapi-283482759Noch keine Bewertungen
- Notice To Employer (Final 5.2.24)Dokument12 SeitenNotice To Employer (Final 5.2.24)Khasyafsufi AdminNoch keine Bewertungen
- Placenta FunctionsDokument46 SeitenPlacenta Functionsvenkata sryanamala50% (2)
- Reading Task 1-Breast Cancer and The ElderlyDokument6 SeitenReading Task 1-Breast Cancer and The ElderlyJats_Fru_1741100% (5)
- Nigeria Essential MedicinesDokument57 SeitenNigeria Essential MedicinesportosinNoch keine Bewertungen
- DiagramDokument12 SeitenDiagramJessica CindyNoch keine Bewertungen
- Advantages and Disadvantages of Traditional Fermentation of Dairy ProductsDokument4 SeitenAdvantages and Disadvantages of Traditional Fermentation of Dairy ProductsEkoh EnduranceNoch keine Bewertungen
- New Microsoft Office Word DocumentDokument2 SeitenNew Microsoft Office Word DocumentAnam BukhariNoch keine Bewertungen
- Cardiovascular DisorderDokument6 SeitenCardiovascular DisorderClara De GuzmanNoch keine Bewertungen
- E NihssDokument5 SeitenE NihssNayeli SánchezNoch keine Bewertungen
- CNS Microbiology MeningitisDokument26 SeitenCNS Microbiology MeningitisSaransh GhimireNoch keine Bewertungen
- Whole Blood Coagulation Analyzer PDFDokument1 SeiteWhole Blood Coagulation Analyzer PDFmorton1472Noch keine Bewertungen
- Hormone Levels For Fertility Patients1Dokument4 SeitenHormone Levels For Fertility Patients1Kunbi Santos-ArinzeNoch keine Bewertungen
- NorovirusDokument3 SeitenNoroviruskolita kamalNoch keine Bewertungen
- HPNDokument4 SeitenHPNFlorianne AdlawanNoch keine Bewertungen
- NLR As Biomarker of DeleriumDokument9 SeitenNLR As Biomarker of DeleriumbrendaNoch keine Bewertungen
- Vastarel MR 35mgDokument1 SeiteVastarel MR 35mgPhil Edgar Contreras RNNoch keine Bewertungen
- Prevalence of Gestational Diabetes and Contributing Factors Among Pregnant Jordanian Women Attending Jordan University HospitalDokument8 SeitenPrevalence of Gestational Diabetes and Contributing Factors Among Pregnant Jordanian Women Attending Jordan University HospitalManar ShamielhNoch keine Bewertungen
- PharmacotherapyDokument15 SeitenPharmacotherapyPrincess RonsableNoch keine Bewertungen
- E-Poster PresentationDokument1 SeiteE-Poster PresentationOvamelia JulioNoch keine Bewertungen