Beruflich Dokumente
Kultur Dokumente
Tranmucosal Fixation
Hochgeladen von
lippincott2011Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Tranmucosal Fixation
Hochgeladen von
lippincott2011Copyright:
Verfügbare Formate
Competing interests
None declared.
Ethical approval
Not required.
References
1. Aoki T, Naito H, Ota Y, Shiiki K.
Myositis ossicans traumatica of the mas-
ticatory muscles: review of the literature
and report of a case. J Oral Maxillofac
Surg 2002: 60: 10831088.
2. Arima R, Shiba R, Hayashi T. Traumatic
myositis ossicans in the masseter muscle.
J Oral Maxillofac Surg 1984: 42: 521526.
3. Arrington ED, Miller MD. Skeletal
muscle injuries. Orthop Clin North Am
1995: 26: 411422.
4. Carey EJ. Multiple bilateral parosteal
bone and callus formations of the femur
and left innominate bone. Arch Surg
1924: 8: 592603.
5. Conner GA, Duffy M. Myositis ossi-
cans: a case report of multiple recurrences
following third molar extractions and
review of the literature. J Oral Maxillofac
Surg 2009: 67: 920926.
6. Cushner FD, Morwessel RM. Myositis
ossicans traumatica. Orthop Rev 1992:
21: 13191326.
7. Dimitroulis G. The interpositional der-
mis-fat graft in the management of tem-
poromandibular joint ankylosis. Int J Oral
Maxillofac Surg 2004: 33: 755760.
8. Kim DD, Lazow SK, Berger JR Har-
ELG. Myositis ossicans traumatica of
the masticatory musculature: a case report
and literature review. J Oral Maxillofac
Surg 2002: 60: 10721076.
9. Narang R, Dixon RA. Myositis ossi-
cans: medial pterygoid musclea case
report. Br J Oral Surg 1974: 12: 229234.
10. ParkashH, GoyalM. Myositis ossicans
of medial pterygoidmuscle. Oral SurgOral
Med Oral Pathol 1992: 73: 2728.
11. RattanV, Rai S, Vaiphei K. Useof buccal
pad of fat to prevent heterotopic bone for-
mation after excision of myositis ossicans
of medial pterygoid muscle. J Oral Max-
illofac Surg 2008: 66: 15181522.
12. Shirkhoda A, Armin AR, Bis KG,
Makris J, Irwin RB, Shetty AN. MR
imaging of myositis ossicans: variable
patterns at different stages. J Magn Reson
Imaging 1995: 5: 287292.
13. Spinazze RP, Heffez LB, Bays RA.
Chronic progressive limitation of mouth
opening. J Oral Maxillofac Surg 1998: 56:
11781186.
14. Takahashi K, Sato K. Myositis ossi-
cans traumatica of the medial pterygoid
muscle. J Oral Maxillofac Surg 1999: 57:
451456.
15. Woolgar JA, Beirne JC, Triantafyl-
lou A. Myositis ossicans traumatica of
sternocleidomastoid muscle presenting as
cervical lymph-node metastasis. Int J
Oral Maxillofac Surg 1995: 24: 170173.
Address:
Annamalai Thangavelu
Division of Oral and Maxillofacial Surgery
Rajah Muthiah Dental College and Hospital
Chidambaram 608002
Tamil Nadu
India
Tel.: +91 94432 44213
Fax: +91 41442 38080.
Email: omfsvat@hotmail.com
doi:10.1016/j.ijom.2010.10.024
Case Report
Trauma
Transmucosal xation of the
fractured edentulous mandible
G. A. Wood, D. F. Campbell, L. E. Greene: Transmucosal xation of the fractured
edentulous mandible. Int. J. Oral Maxillofac. Surg. 2011; 40: 549552. # 2010
Published by Elsevier Ltd on behalf of International Association of Oral and
Maxillofacial Surgeons.
G. A. Wood, D. F. Campbell,
L. E. Greene
Regional Maxillofacial Unit, Southern General
Hospital, Glasgow, UK
Abstract. Transmucosal xation is a new strategy for the treatment of edentulous
mandibular fractures using external xation principles within the oral cavity. The
component parts of this technique are not new. External xation, locking plates and
transmucosal implants represent the foundations of this technique; the authors
development has been to bring these established methods together as a transmucosal
intra oral locking plate xation technique. The rst eight patients treated with this
technique have achieved bony union, they have no long-term sensory decit and all
patients were able to eat a soft diet with minimal discomfort the day after surgery.
The rst ve of eight patients on long-term review showed bony union conrmed
radiographically. For the remainder and subsequent patients, radiographs have not
been scheduled at review, in the absence of symptoms.
Accepted for publication 29 October 2010
Available online 23 December 2010
Myositis ossicans traumatica of the medial pterygoid 549
Treatment of the edentulous fractured
mandible presents special difculties
3,8
.
Many methods of immobilisation have
been suggested over the years, most of
historic interest
1
given the modern accep-
tance of rigid plate xation. Patients are
often elderly
9
with acute and chronic co-
morbidities frequently complicating man-
agement and adding to anaesthetic risks
5
.
The specic problems of edentulous man-
dibular fractures relate to the remaining
mandibular bone height. The difculty of
achieving bony union is well known. Frac-
tures amenable to mini-plate xation often
leave a plate near the denture bearing area
and/or place a screw near the inferior
alveolar neurovascular bundle risking
anaesthesia or paraesthesia in the distribu-
tion of the nerve
4
. Since the screws are
angled laterally in the posterior area, the
benet of bi-cortical xation may be
achieved and there is less risk to the
neurovascular bundle. Anteriorly, the
screws are medial to the inferior dental
canal. In the authors experience, stability
is sufcient with xation through one
cortical plate as STOELINGA et al. described
in the xation of mandibular osteo-
tomies
10
. Bi-cortical xation would
increase the rmness of xation and can
be achieved with this technique.
The aim of this study was to establish
whether rigid xation could be achieved
transmucosally using existing locking
plates and establishedexternal xationcon-
cepts. The rst eight cases are reported.
Materials and method
Patients with an edentulous fractured
mandible that required xation were
selected. If they were unt for a general
anaesthetic the procedure could be carried
out under local anaesthetic with or without
sedation. An impression taken before sur-
gery can facilitate plate contouring prior to
plate placement, alternatively the plate
can be contoured intra-operatively.
The fracture site(s) were palpated and if
there was any problem with the accuracy
of reduction a small incision was made to
visualize the fracture line. A suitably long
mini-locking plate straddling the fracture
site was placed and xed (Fig. 1). Post-
operative and 6-month review radiographs
were taken. There was a buried premolar
in the area of this fracture, the authors
avoided extracting the tooth at the time of
xation, as this would have increased the
risk of non-union. Bony union was con-
rmed by radiography and the tooth
remained buried and asymptomatic. In
later cases, longer plates were used, which
Fig. 1. A suitably long mini-locking plate straddling the fracture site was placed and xed.
Transmucosal xation of a mobile fracture through the right body of the mandible associated
with an unerupted tooth, an ink mark represents the clinical estimate of the fracture position, also
showing xation in position and 6-month review x ray.
Fig. 2. In the retro-molar region the screws are angled from a lingual entry directed downwards
and slightly buccally.
550 Wood et al.
ideally extended fromretro-molar to retro-
molar region where screws were grouped
in three specic regions, both retro-molar
regions and the bone anterior to the mental
foramina. In the retro-molar region the
screws are angled from a lingual entry
directed downwards and slightly buccally
and may engage the lateral cortex but
mono-cortical engagement is adequate
(Fig. 2)
2
. The authors now avoid the man-
dibular body for screw placement.
To avoid mucosal compression a peri-
osteal elevator was used (Fig. 1). The
locking screw could then be engaged fully
without compressing the mucosa.
Although initially two screws were used
on either side of the fracture line, the
authors considered that a minimum of
three mono-cortical screws in the ramus
regions and in the anterior mandible would
be better.
Postoperatively, orthopantomograms
were carried out to conrm satisfactory
reduction. At review, following xation
removal, patients were assessed for mobi-
lity or pain at the fracture site. If patients
remained symptom free 2 weeks after xa-
tion removal they were discharged. The
rst three patients returned for follow-up
and radiography to conrm bony union.
Results
All patients were able to eat a soft break-
fast on the rst postoperative day,
seemed untroubled by the procedure
and did not complain of any signicant
pain.
After xation removal, carried out
under local anaesthesia, all patients had
clinical bony union so radiography was
not considered appropriate at this stage on
clinical grounds and no patient required
further follow-up beyond 3 months. The
rst three patients were recalled at 6
months and agreed to assist the study by
allowing clinical examination and a
review radiograph, all had achieved bony
union (Figs 1c and 3b).
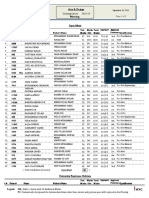
Of the rst eight patients (Table 1), one
had a dense unilateral sensory decit in the
distribution of the mental nerve following
bilateral fracture xation, but this had
resolved by the time xation was
removed. One patient had evidence of
plate bending with plate fracture (Synthes
2.0 locking) at 7 weeks but this did not
cause any signicant discomfort and did
not affect the outcome.
One of the early bilateral fracture
cases had a screw placed in the left
fracture line (Fig. 3a) but the patient
reported no problems and bony union
is seen on the 6-month review radiograph
(Fig. 3b).
Discussion
Treating the fractured edentulous mand-
ible is a challenge and the more atrophic
the mandible the greater the challenge
11
.
Problems include the risks of general
anaesthesia in the elderly, nerve injury,
non-rigid union resulting in pain, denture
rehabilitation problems, and psychologi-
cal issues.
The authors reviewed the notes avail-
able for patients in the preceding 2 years
(seven patients) who had been treated with
open reduction with internal xation for
similar fractures and followed this up with
a retrospective questionnaire to determine
the signicant morbidities associated with
conventional techniques. All had sensory
decits as a result of surgery and two had
problems with drooling and would no
longer eat in public. One had returned to
theatre and another was re-admitted with
infection. Five had problems with den-
tures and four had chronic pain.
The authors conclude that the simple
technique of transmucosal xation can
reduce operative complications and out-
come in the treatment of fractures of the
edentulous mandible, including bucket
handle fractures
6,7
. The authors have con-
tinuedwiththis technique andreport further
success in the xation of two patients trea-
ted under local anaesthesia because of med-
ical co-morbidities rendering themunt for
Fig. 3. (a) One of the early bilateral fracture cases had a screw placed in the left fracture line;
and (b) the 6-month review radiograph shows bony union.
Table 1. Clinical outcomes from the rst eight patients are listed.
Total number of patients 8
Plating type Synthes 2.0 locking
Plate fracture 1/8 (patient 3)
Plate bending 1/8 (patient 3)
Rigid union at time of removal 8/8
Subjective sensory decit following surgery Temporary (2 months)
Postoperative infection Nil
Transmucosal xation of the fractured edentulous mandible 551
general anaesthesia. The 2 mm locking
plate showed bending with subsequent
fracture in one case and as a result a more
suitable plate and locking device are being
developed to enhance the technique.
Competing interests
The authors are seeking to commercialize
a new plate based on what they have
learned from this research.
Funding
Scottish Health Innovations Ltd have
funded a patent application total funding
circa US$7K.
Ethical approval
Not required.
References
1. Barber H. Part I: Conservative manage-
ment of the fractured atrophic edentulous
mandible. J Oral Maxillofac Surg 2001:
59: 789791.
2. Borstlap WA, Stoelinga PJW, Hop-
penreijs TJM, vant Hof MA. Stabili-
zation of sagittal split advancement
osteotomies with miniplates: a prospec-
tive study with two-year follow-up. Part
II: Radiographic parameters. Int J Oral
Maxillofac Surg 2004: 33: 535542.
3. Bruce RA, Ellis 3rd E. The second
Chalmers J. Lyons Academy study of
fractures of the edentulous mandible. J
Oral Maxillofac Surg 1993: 51: 904
911.
4. Gerbino G, Roccia F, De Gioanni PP,
Berrone S. Maxillofacial trauma in the
elderly. J Oral Maxillofac Surg 1999: 57:
777782.
5. Jones RL. Anesthesia risk in the geriatric
patient. In: McLeskey CH, ed: Perio-
perative Geriatrics Problems in Anesthe-
sia, vol. 3. Philadelphia: PA Lippincott
1989: 529.
6. Luhr HG, Reidick T, Merten HA.
Results of treatment of fractures of the
atrophic edentulous mandible by com-
pression plating: a retrospective evalua-
tion of 84 consecutive cases. J Oral
Maxillofac Surg 1996: 54: 250254.
7. Mathog RH, Toma V, Clayman L,
Wolf S. Nonunion of the mandible: an
analysis of contributing factors. J Oral
Maxillofac Surg 2000: 58: 746752.
8. Nasser M, Fedorowicz Z, Ebadifar A.
Management of the fractured edentulous
atrophic mandible. Cochrane Database
Syst Rev 2007 Issue 1. Art. No.
CD006087.
9. Scott RF. Oral and maxillofacial trauma
in the geriatric patient. In: Fonseca RJ,
Walker RV, Betts NJ, eds: Oral and
Maxillofacial Trauma, vol. 2. Philadel-
phia: PA Saunders 1997: 10451072.
11. Wittwer G, Adeyemo WL, Turhani D,
Ploder O. Treatment of atrophic man-
dibular fractures based on the degree of
atrophyexperience with different plat-
ing systems: a retrospective study. J Oral
Maxillofac Surg 2006: 64: 230234.
Address:
Duncan Campbell
Regional Maxillofacial Unit
Southern General Hospital
1345 Govan Road
Glasgow
G51 4TF
Scotland
UK
Tel: +44 7801568946
Fax: +44 0141 232 7508
Email: duncan@zygomatics.net
doi:10.1016/j.ijom.2010.10.027
Case Report
Oral Medicine
Non-alcoholic steatohepatitis
(NASH) and oral lichen planus:
a rare occurrence
D. Conrotto, E. Bugianesi, L. Chiusa, M. Carrozzo: Non-alcoholic steatohepatitis
(NASH) and oral lichen planus: a rare occurrence. Int. J. Oral Maxillofac. Surg.
2011; 40: 552555. # 2010 International Association of Oral and Maxillofacial
Surgeons. Published by Elsevier Ltd. All rights reserved.
D. Conrotto
1
, E. Bugianesi
2
,
L. Chiusa
3
, M. Carrozzo
4
1
Division of Otorhinolaryngology, Department
of Clinical Physiopathology, Oral Medicine
Section, University of Turin, Italy;
2
Division of
Gastro-Hepatology, Department of Internal
Medicine, University of Turin, Italy;
3
Department of Biomedical Sciences and
Human Oncology, Pathology Section,
University of Turin, Italy;
4
Department of Oral
Medicine, University of Newcastle upon Tyne,
UK
Abstract. Oral lichen planus (OLP) is frequently associated with hepatitis C virus
infection but uncommonly with other causes of liver disorder. The authors report the
case of a 41-year-old male patient with a clinical and histological diagnosis of OLP
who presented with a marked alteration of the transaminase values, with no signs of
past or present HBV, HCV, HGV or TTV infection. The patient did not consume
alcohol and no exposure to hepatotoxic substances was reported. All autoantibodies
were negative. Hepatic ne needle biopsy showed macrovesicular steatosis with a
slight chronic portal inammatory inltrate and signs of siderosis. Iron metabolism
was slightly altered. Genetic tests showed a heterozygotic mutation for hereditary
552 Wood et al.
Das könnte Ihnen auch gefallen
- Distal Humeral Fractures-Current Concepts PDFDokument11 SeitenDistal Humeral Fractures-Current Concepts PDFRina AlvionitaNoch keine Bewertungen
- Pharmacology of Ocular Therapeutics (2016)Dokument541 SeitenPharmacology of Ocular Therapeutics (2016)Marin Crangaci100% (1)
- Mr. Jose Ferdinand M. Rojas Ii: FPCP, FPSMO, Recommended Her To Undergo Chemotherapy For Her Spinal Column WhichDokument3 SeitenMr. Jose Ferdinand M. Rojas Ii: FPCP, FPSMO, Recommended Her To Undergo Chemotherapy For Her Spinal Column Whichglenn padernalNoch keine Bewertungen
- 1998-2005 I-MDokument23 Seiten1998-2005 I-Mlippincott2011100% (1)
- Mallet Finger Suturing TechniqueDokument5 SeitenMallet Finger Suturing TechniqueSivaprasath JaganathanNoch keine Bewertungen
- Etnobotanica Ingles Web PDFDokument294 SeitenEtnobotanica Ingles Web PDFipahei100% (2)
- Oet Wrıtıng Brıtısh Academy 01 315 376 With AnswerDokument62 SeitenOet Wrıtıng Brıtısh Academy 01 315 376 With Answersaramma mathewNoch keine Bewertungen
- Mixoma 9Dokument4 SeitenMixoma 9Nicolás MedinaNoch keine Bewertungen
- Treatment Distal Radius Fracture With Volar Buttre PDFDokument5 SeitenTreatment Distal Radius Fracture With Volar Buttre PDFZia Ur RehmanNoch keine Bewertungen
- Ort 7Dokument2 SeitenOrt 7Siddharth DhanarajNoch keine Bewertungen
- Jurnal RADIO PDFDokument4 SeitenJurnal RADIO PDFCita ChotimahNoch keine Bewertungen
- 2005 Laster Width Distraction OsteogenesisDokument7 Seiten2005 Laster Width Distraction Osteogenesislisal1saNoch keine Bewertungen
- Materials: A Modified Ridge Splitting Technique Using Autogenous Bone Blocks-A Case SeriesDokument10 SeitenMaterials: A Modified Ridge Splitting Technique Using Autogenous Bone Blocks-A Case SeriesLouis HutahaeanNoch keine Bewertungen
- Reconstrução de Severa Reabsorção Maxilar Com Distração OsteogenicaDokument7 SeitenReconstrução de Severa Reabsorção Maxilar Com Distração OsteogenicaNelson UzunNoch keine Bewertungen
- Brief Resume of Intended WorkDokument7 SeitenBrief Resume of Intended WorkNavin ChandarNoch keine Bewertungen
- Huang 2018Dokument6 SeitenHuang 2018zj7n2rhtb4Noch keine Bewertungen
- Complications and Outcomes of The Transfibular Approach For Posterolateral Fractures of The Tibial Plateau PDFDokument19 SeitenComplications and Outcomes of The Transfibular Approach For Posterolateral Fractures of The Tibial Plateau PDFSergio Tomas Cortés MoralesNoch keine Bewertungen
- Fotos OclusalesDokument6 SeitenFotos OclusalesMarco Antonio García LunaNoch keine Bewertungen
- Yoshimoto 2004Dokument5 SeitenYoshimoto 2004r1comfupchNoch keine Bewertungen
- MandibulaDokument4 SeitenMandibulaMohamed MukhrizNoch keine Bewertungen
- Taub - Nonunion of Mandibular MidlineDokument4 SeitenTaub - Nonunion of Mandibular MidlineChristopher McMullinNoch keine Bewertungen
- Comparative Study of Proximal Humerus Fractures Treated With Percutaneous Pinning and Augmented by External FixatorDokument3 SeitenComparative Study of Proximal Humerus Fractures Treated With Percutaneous Pinning and Augmented by External FixatorRahul ReddyNoch keine Bewertungen
- Onlay Bone Graft Augmentation For Refined Correction of Coronal SynostosisDokument9 SeitenOnlay Bone Graft Augmentation For Refined Correction of Coronal Synostosisbalab2311Noch keine Bewertungen
- Comlicaciones Osteotomia Saguital de RamaDokument4 SeitenComlicaciones Osteotomia Saguital de RamaLeonardCarreraDiazNoch keine Bewertungen
- Cleft PalateDokument4 SeitenCleft PalateShoaib A. KaziNoch keine Bewertungen
- Горизонтальная дистракцияDokument7 SeitenГоризонтальная дистракцияIrinaBorodulinaNoch keine Bewertungen
- Bong 2011 PDFDokument14 SeitenBong 2011 PDFkarenchavezalvanNoch keine Bewertungen
- Exostosis MandibularDokument6 SeitenExostosis MandibularCOne Gomez LinarteNoch keine Bewertungen
- Immediate One-Stage Postextraction Implant: A Human Clinical and Histologic Case ReportDokument6 SeitenImmediate One-Stage Postextraction Implant: A Human Clinical and Histologic Case ReportBagis Emre GulNoch keine Bewertungen
- Tecnica de ChampyDokument7 SeitenTecnica de Champyboye022694Noch keine Bewertungen
- Modified Gap Arthroplasty and Myrhaugs Incision As A Treatment Option in Management of Temporomandibular Joint Ankylosis A Study of 10 CasesDokument6 SeitenModified Gap Arthroplasty and Myrhaugs Incision As A Treatment Option in Management of Temporomandibular Joint Ankylosis A Study of 10 CasesS EllurNoch keine Bewertungen
- 23 03 09 07 03 11 - ExpansionDokument5 Seiten23 03 09 07 03 11 - ExpansionRaed Abu HamadNoch keine Bewertungen
- A Long-Term Study of 370 Autotransplanted Premolars.Dokument11 SeitenA Long-Term Study of 370 Autotransplanted Premolars.jing.zhao222Noch keine Bewertungen
- Novel Surgical Technique For Clavicle Graft HarvestDokument5 SeitenNovel Surgical Technique For Clavicle Graft Harvestsanchaita kohliNoch keine Bewertungen
- Benech 2013 International Journal of Oral and Maxillofacial SurgeryDokument4 SeitenBenech 2013 International Journal of Oral and Maxillofacial SurgerysebitadesantaNoch keine Bewertungen
- Aps 39 345Dokument9 SeitenAps 39 345isabelNoch keine Bewertungen
- Management of Infected Radicular Cyst by Marsupialization: Case ReportDokument5 SeitenManagement of Infected Radicular Cyst by Marsupialization: Case Reportvivi hutabaratNoch keine Bewertungen
- Ams 5 108Dokument4 SeitenAms 5 108Alice EmailsNoch keine Bewertungen
- Mermigos 11 01Dokument4 SeitenMermigos 11 01Sankurnia HariwijayadiNoch keine Bewertungen
- Endodontc Surgical Management of Mucosal FenistrationDokument3 SeitenEndodontc Surgical Management of Mucosal Fenistrationfun timesNoch keine Bewertungen
- Anehosur Et Al 2020 Concepts and Challenges in The Surgical Management of Edentulous Mandible Fractures A Case SeriesDokument7 SeitenAnehosur Et Al 2020 Concepts and Challenges in The Surgical Management of Edentulous Mandible Fractures A Case SeriesHenry Adhy SantosoNoch keine Bewertungen
- A Long-Term Study of 370 Autotransplanted Premolars. Part II. Tooth Survival and Pulp Healing Subsequent To TransplantationDokument11 SeitenA Long-Term Study of 370 Autotransplanted Premolars. Part II. Tooth Survival and Pulp Healing Subsequent To TransplantationRudnapon AmornlaksananonNoch keine Bewertungen
- A Study On Management of Bothbones Forearm Fractures With Dynamic Compression PlateDokument5 SeitenA Study On Management of Bothbones Forearm Fractures With Dynamic Compression PlateIOSRjournalNoch keine Bewertungen
- Rajiv Gandhi University of Health Sciences, Bengaluru, KarnatakaDokument9 SeitenRajiv Gandhi University of Health Sciences, Bengaluru, KarnatakaNavin ChandarNoch keine Bewertungen
- Assessment of Occlusal Appliance For The Reposition of Temporomandibular Joint Anterior Disc Displacement With ReductionDokument4 SeitenAssessment of Occlusal Appliance For The Reposition of Temporomandibular Joint Anterior Disc Displacement With ReductionSTEPHANIE JARAMILLONoch keine Bewertungen
- Malocclusion As A Common Occurrence in Temporomandibular Joint Arthroscopic Disc Repositioning - Outcomes at 49 Days After Surgery 2Dokument7 SeitenMalocclusion As A Common Occurrence in Temporomandibular Joint Arthroscopic Disc Repositioning - Outcomes at 49 Days After Surgery 2Ario LovellyNoch keine Bewertungen
- International Journal of Health Sciences and ResearchDokument6 SeitenInternational Journal of Health Sciences and ResearchDentist HereNoch keine Bewertungen
- Split Technique 2Dokument8 SeitenSplit Technique 2Alejandro RuizNoch keine Bewertungen
- Botticelli 2004Dokument9 SeitenBotticelli 2004medNoch keine Bewertungen
- Bahan Jurnal Neglected Fractures of FemurDokument5 SeitenBahan Jurnal Neglected Fractures of Femurgulamg21Noch keine Bewertungen
- Osteogenesis InglesDokument4 SeitenOsteogenesis InglesJulio TorresNoch keine Bewertungen
- Prosthetic Management of Hemimandibulectomy Patient - A Case ReportDokument3 SeitenProsthetic Management of Hemimandibulectomy Patient - A Case ReportIOSRjournalNoch keine Bewertungen
- Broken Dental Needle Retrieval Using A S PDFDokument5 SeitenBroken Dental Needle Retrieval Using A S PDFStefanNoch keine Bewertungen
- Intrusion of Incisors in Adult Patients With Marginal Bone LossDokument10 SeitenIntrusion of Incisors in Adult Patients With Marginal Bone LossYerly Ramirez MuñozNoch keine Bewertungen
- Core Decompression in Foot and AnkleDokument9 SeitenCore Decompression in Foot and AnkleAnonymous kdBDppigENoch keine Bewertungen
- Results and Complications of Alveolar Distraction Osteogenesis To Enhance Vertical Bone HeightDokument7 SeitenResults and Complications of Alveolar Distraction Osteogenesis To Enhance Vertical Bone HeightKeval ModiNoch keine Bewertungen
- Abstracts de Publicaciones Sobre Pilón TibialDokument15 SeitenAbstracts de Publicaciones Sobre Pilón TibialAyler AguilarNoch keine Bewertungen
- Management of Proximal Humeral FracturesDokument16 SeitenManagement of Proximal Humeral FracturesAustine OsaweNoch keine Bewertungen
- Alveolar Bone Preservation Subsequent To Miniscrew Implant Placement in A Canine ModelDokument9 SeitenAlveolar Bone Preservation Subsequent To Miniscrew Implant Placement in A Canine ModelSamuel OtavioNoch keine Bewertungen
- Distraction Osteogenesis EbookDokument27 SeitenDistraction Osteogenesis EbookSundeep SharmaNoch keine Bewertungen
- Microsaw and Piezosurgery in Harvesting Mandibular Bone Blocks From The Retromolar Region: A Randomized Split-Mouth Prospective Clinical TrialDokument8 SeitenMicrosaw and Piezosurgery in Harvesting Mandibular Bone Blocks From The Retromolar Region: A Randomized Split-Mouth Prospective Clinical TrialdivyaNoch keine Bewertungen
- Two Years Outcome of Cemented Austin Moore HemiartDokument7 SeitenTwo Years Outcome of Cemented Austin Moore HemiartIkram HussainNoch keine Bewertungen
- Cleft Maxillary Distraction Versus Orthognathic Surgery: Clinical Morbidities and Surgical RelapseDokument13 SeitenCleft Maxillary Distraction Versus Orthognathic Surgery: Clinical Morbidities and Surgical RelapseRohan BhagatNoch keine Bewertungen
- Management of A Failed Mandibular Staple Implant A Clinical ReportDokument5 SeitenManagement of A Failed Mandibular Staple Implant A Clinical ReportAhmad ShoeibNoch keine Bewertungen
- Dislocation of the Temporomandibular Joint: A Guide to Diagnosis and ManagementVon EverandDislocation of the Temporomandibular Joint: A Guide to Diagnosis and ManagementNigel Shaun MatthewsNoch keine Bewertungen
- Minor Salivary Gland Tumors Diagnosis and ManagementDokument80 SeitenMinor Salivary Gland Tumors Diagnosis and Managementlippincott2011Noch keine Bewertungen
- Straight and Tilted Implants For Supporting Screw-Retained Full-Arch Dental Prostheses in Atrophic Maxillae: A 2-Year Prospective StudyDokument9 SeitenStraight and Tilted Implants For Supporting Screw-Retained Full-Arch Dental Prostheses in Atrophic Maxillae: A 2-Year Prospective Studylippincott2011Noch keine Bewertungen
- Plain Films of The SkullDokument10 SeitenPlain Films of The Skulllippincott2011Noch keine Bewertungen
- Midfacial Degloving Approach For Management of The Maxillary Fibrous Dysplasia: A Case ReportDokument9 SeitenMidfacial Degloving Approach For Management of The Maxillary Fibrous Dysplasia: A Case Reportlippincott2011Noch keine Bewertungen
- Tilted Implants An Alternative For MaxillaDokument11 SeitenTilted Implants An Alternative For Maxillalippincott2011Noch keine Bewertungen
- Dierks - Buccal Fat Pad and Tongue Flaps Indy 2019Dokument76 SeitenDierks - Buccal Fat Pad and Tongue Flaps Indy 2019lippincott2011Noch keine Bewertungen
- Immediate Occlusal Loading and Tilted Implants For The Rehabilitation of The Atrophic Edentulous Maxilla: 1-Year Interim Results of A Multicenter Prospective StudyDokument6 SeitenImmediate Occlusal Loading and Tilted Implants For The Rehabilitation of The Atrophic Edentulous Maxilla: 1-Year Interim Results of A Multicenter Prospective Studylippincott2011Noch keine Bewertungen
- Detecting Oral Cancer: A Guide For Health Care ProfessionalsDokument19 SeitenDetecting Oral Cancer: A Guide For Health Care Professionalslippincott2011Noch keine Bewertungen
- Mronj Position Paper PDFDokument26 SeitenMronj Position Paper PDFctrplieff2669Noch keine Bewertungen
- 2 IntrotoeyeexamDokument6 Seiten2 Introtoeyeexamlippincott2011Noch keine Bewertungen
- NullDokument123 SeitenNullARLibraryNoch keine Bewertungen
- St. Christophers Cover LetterDokument1 SeiteSt. Christophers Cover Letterlippincott2011Noch keine Bewertungen
- UConn Dental: Prosthodontics Clinic Manual 11-12Dokument67 SeitenUConn Dental: Prosthodontics Clinic Manual 11-12lippincott2011Noch keine Bewertungen
- Plain Films of The SkullDokument10 SeitenPlain Films of The Skulllippincott2011Noch keine Bewertungen
- 2000-2008 I-NDokument22 Seiten2000-2008 I-Nlippincott2011Noch keine Bewertungen
- Frontal Sinus FX Slides 070117Dokument48 SeitenFrontal Sinus FX Slides 070117lippincott2011Noch keine Bewertungen
- AAOMS Resident MembershipDokument1 SeiteAAOMS Resident Membershiplippincott2011Noch keine Bewertungen
- Plain Films of The SkullDokument10 SeitenPlain Films of The Skulllippincott2011Noch keine Bewertungen
- John Dempsey Hospital Cleft Lip and Palate ProtocolDokument5 SeitenJohn Dempsey Hospital Cleft Lip and Palate Protocollippincott2011Noch keine Bewertungen
- Prein - Manual of Internal Fixation in The Cranio-Facial SkeletonDokument244 SeitenPrein - Manual of Internal Fixation in The Cranio-Facial Skeletonlippincott201167% (3)
- Tranmucosal FixationDokument4 SeitenTranmucosal Fixationlippincott2011Noch keine Bewertungen
- Ranula and Sublingual Salivary Gland ExcisionDokument4 SeitenRanula and Sublingual Salivary Gland Excisionnnmey20Noch keine Bewertungen
- Tranmucosal FixationDokument4 SeitenTranmucosal Fixationlippincott2011Noch keine Bewertungen
- N2o Effects On RocuroniumDokument5 SeitenN2o Effects On Rocuroniumlippincott2011Noch keine Bewertungen
- Sample Meta AnalysisDokument3 SeitenSample Meta Analysislippincott2011Noch keine Bewertungen
- Topical Vs N2o For IV AccessDokument4 SeitenTopical Vs N2o For IV Accesslippincott2011Noch keine Bewertungen
- Penn Dental License AppDokument8 SeitenPenn Dental License Applippincott2011Noch keine Bewertungen
- AAOMS Residency Program ListDokument12 SeitenAAOMS Residency Program Listlippincott2011Noch keine Bewertungen
- Attachment Protocol Summary: Situation Default Size/Placement ExamplesDokument1 SeiteAttachment Protocol Summary: Situation Default Size/Placement ExamplesramoramoniNoch keine Bewertungen
- Cataract Surgery in Retina PatientsDokument21 SeitenCataract Surgery in Retina PatientsAnonymous 4OnqyBErNoch keine Bewertungen
- Tutor: Dr. Vera Dr. Haerani: Skenario Problems Learning Objectives Main Map ReferensiDokument36 SeitenTutor: Dr. Vera Dr. Haerani: Skenario Problems Learning Objectives Main Map ReferensiAdeLia Nur FitrianaNoch keine Bewertungen
- Damage Control Orthopaedics DR Bambang SpOT (Salinan Berkonflik Enggar Yusrina 2015-10-14)Dokument37 SeitenDamage Control Orthopaedics DR Bambang SpOT (Salinan Berkonflik Enggar Yusrina 2015-10-14)SemestaNoch keine Bewertungen
- Clincal 1 SAS v2022 (1) - 104-111Dokument8 SeitenClincal 1 SAS v2022 (1) - 104-111Jannah Mikhaela Alibay VillarinNoch keine Bewertungen
- Biology Project Class 12Dokument16 SeitenBiology Project Class 12Anshika Singh100% (1)
- A 25-Year-Old Man With New-Onset Seizures PDFDokument8 SeitenA 25-Year-Old Man With New-Onset Seizures PDFMr. LNoch keine Bewertungen
- Trauma ThoraksDokument35 SeitenTrauma ThoraksmayaNoch keine Bewertungen
- MeritListFinal (2018) 7 PDFDokument71 SeitenMeritListFinal (2018) 7 PDFFaisal AmeenNoch keine Bewertungen
- Roleplay Discharge PlanningDokument3 SeitenRoleplay Discharge PlanningAnonymous KQKONmD9H100% (1)
- Telemedicine Seminar HMTI v1.5Dokument25 SeitenTelemedicine Seminar HMTI v1.5PriaTongNoch keine Bewertungen
- Fifty Years Hence EssayDokument5 SeitenFifty Years Hence EssaynineeNoch keine Bewertungen
- Yoga Sudha Jan 2016Dokument44 SeitenYoga Sudha Jan 2016ewealthcreatorNoch keine Bewertungen
- Fee Paying FreshDokument3 SeitenFee Paying FreshQuame HazyNoch keine Bewertungen
- Evaluation of Depression and Suicidal Patients in The Emergency RoomDokument15 SeitenEvaluation of Depression and Suicidal Patients in The Emergency RoomjuanpbagurNoch keine Bewertungen
- Strategic Preparedness and Response PlanDokument28 SeitenStrategic Preparedness and Response PlanPeter MeierNoch keine Bewertungen
- ENDOCRINE 1.3 Incidentallomas, Conn's SyndromeDokument5 SeitenENDOCRINE 1.3 Incidentallomas, Conn's SyndromeJem QuintoNoch keine Bewertungen
- Medication Calculation Worksheet Disclosure of A No Harm IncidentDokument3 SeitenMedication Calculation Worksheet Disclosure of A No Harm IncidentAngelica AmandoNoch keine Bewertungen
- Hypothyroidism Pregnancy BrochureDokument2 SeitenHypothyroidism Pregnancy BrochureNungky KusumaNoch keine Bewertungen
- NSG ASSESSMENT TOOL TorralbaAubreyDyniseC.,sectionFDokument4 SeitenNSG ASSESSMENT TOOL TorralbaAubreyDyniseC.,sectionFAubrey Dynise C. TorralbaNoch keine Bewertungen
- Tatalaksana Low Vision Pada Severe Visual Impairment Dengan Aphakia Dan Amblyopia DeprivatifDokument12 SeitenTatalaksana Low Vision Pada Severe Visual Impairment Dengan Aphakia Dan Amblyopia DeprivatifAURA PUTRINoch keine Bewertungen
- National Institute of Ayurveda: BrochureDokument10 SeitenNational Institute of Ayurveda: BrochureKopal AgarwalNoch keine Bewertungen
- GRH D 16 00001 ManuscriptDokument224 SeitenGRH D 16 00001 ManuscriptsrividyargNoch keine Bewertungen
- Journal Club On N Corona VirusDokument20 SeitenJournal Club On N Corona VirusNandha KumarNoch keine Bewertungen
- Hunayn Ibn Ishaq-Nestorian Christian 809-873Dokument14 SeitenHunayn Ibn Ishaq-Nestorian Christian 809-873Leanna Cinquanta100% (1)
- KyphosisDokument3 SeitenKyphosismnatuelNoch keine Bewertungen