Beruflich Dokumente
Kultur Dokumente
Hydronephrosis and Orif
Hochgeladen von
marieOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Hydronephrosis and Orif
Hochgeladen von
marieCopyright:
Verfügbare Formate
Definition agent is then injected.
Retrograde pyelography is usually performed
if intravenous urography provides inadequate visualization
Hydronephrosis is the swelling of the kidneys when urine flow is of the collecting systems. It may also be used before
obstructed in any of part of the urinary tract. Swelling of the ureter, which extracorporeal shock-wave lithotripsy or in patients with urologic
always accompanies hydronephrosis, is called hydroureter. cancer who need follow-up and are allergic to intravenous contrast
agents. Possible complications include infection, hematuria, and
Hydronephrosis implies that a ureter and the renal pelvis (the connection
perforation of the ureter. Retrograde pyelography is used infrequently
of the ureter to the kidney) are overfilled with urine.
because of improved techniques in excretory urography.
Description
The kidneys filter urine out of the blood as a waste product. It collects in Each kidney contains about 1 million nephrons, the functional
the renal pelvis and flows down the ureters into the bladder. The ureters units of the kidney. Each kidney is capable of providing adequate
are not simple tubes, but muscular passages that actively propel urine renal function if the opposite kidney is damaged or
into the bladder. At their lower end is a valve (the ureterovesical junction) becomes nonfunctional. The nephron consists of a glomerulus
that prevents urine from flowing backward into the ureter. The bladder containing afferent and efferent arterioles, Bowman’s capsule,
stores urine. The prostate gland surrounds the bladder outlet in males. proximal tubule, loop of Henle, distal tubule, and collecting ducts
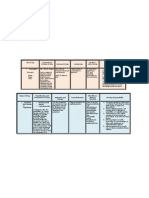
Urine then flows through the urethra and out of the body as a waste (Fig. 43-2). Collecting ducts converge into papillae, which empty Signs and symptoms Why
product. into the minor calices, which drain into three major calices that Signs and symptoms
open directly into the renal pelvis. Acute: extreme flank plain on affected Buildup of pressure in the kidney
Because the urinary tract is closed save for the one opening at the Nephrons are structurally divided into two types: cortical and or
bottom, urine cannot escape. Instead, the parts distend. Rupture is rare juxtamedullary. Cortical nephrons are found in the cortex of the side; pain may radiate to groin ureter due to backflow of urine
unless there is violent trauma like an automobile accident. kidney, and juxtamedullary nephrons sit adjacent to the medulla. Chronic: mild discomfort over affected Kidney shifts downward, causing
The juxtamedullary nephrons are distinguished by their long side (sometimes described as dull overfilling of the renal pelvis or
Obstructed flow anywhere along the drainage route can cause swelling of
loops of Henle and the vasa recta, long capillary loops that dip and aching) blockage of the ureters
the upper urinary tract, but if the obstruction is below the bladder, the
into the medulla of the kidney. Anuria, oliguria, hematuria, polyuria Blockage of the urethra or ureters
ureterovesical valve will protect the upper tract to a certain extent. Even
The glomerulus is composed of three filtering layers: the capillary Urinary tract infection Backflow or stasis of the urine
then, with no place to go, the urine will back up all the way to its source.
endothelium, the basement membrane, and the epithelium. encourages bacterial growth
Eventually, the back pressure causes kidney function to deteriorate.
The glomerular membrane normally allows filtration of fluid and Nausea, vomiting, abdominal pain Body’s immune response
Obstruction need not be complete for problems to arise. Intermittent or small molecules yet limits passage of larger molecules, such as Asymptomatic If progression of hydronephrosis is
partial obstruction is far more common than complete blockage, allowing blood cells and albumin. Kidney function begins to decrease at a slow there may be no symptoms for
time for the parts to enlarge gradually. Furthermore, if a ureterovesical rate of approximately 1% each year beginning at approximately awhile
valve is absent or incompetent, the pressure generated by bladder Palpable mass over flank area Seen only in extreme cases; due to
emptying will force urine backward into the ureter and kidney, causing age 30. enlargement of obstructed area
dilation even without mechanical obstruction. related to the collection of urine
Strictures of the Ureter Hydronephrosis
Some patients are born with a narrowing of the ureter where it leaves the What is it?
kidney or where it enters the bladder. Scar tissue from previous surgery When urine outflow is obstructed, a large fluctuating collection—or
mass—of urine forms in the kidney. This mass subsides as retained urine What can harm my client?
or stones in the ureter can also cause narrowing of the ureter with _ End-stage renal failure.
blockage of the flow of urine from the kidney. These abnormalities can be finally passes into the ureters and bladder. Stagnation of urine in the
kidneys leads to infection. Hydronephrosis is distension of the kidney _ Infection.
treated using the ureteroscope to examine the area of narrowing and use _ Improper catheter irrigation technique. For example, using too much
a device through the ureteroscope to incise, or cut, the area of stricture with urine that leads to progressive atrophy and eventual destruction of
the kidney. The kidney ends up looking like a thin-walled shell filled with force can cause fluid and bacteria to travel back up into the kidney,
or scar tissue. After this procedure, a stent (a small tube that passes from
which can cause hydronephrosis.
the kidney, down the ureter to the bladder) is left inside the body for 1-4 fluid. The causative factor, obstruction, has several different types.
weeks. This stent helps to keep the kidney drained, and can usually be
easily removed in the office. If I were your teacher, I would test you on . . .
Retrograde Pyelography _ What is it?
In retrograde pyelography, catheters are advanced through the _ What causes it and why.
ureters into the renal pelvis by means of cystoscopy. A contrast _ Signs and symptoms and why.
_ Care of the client undergoing stent placement. remains exposed (for later extraction). A counter incision over the Pulsed lavage suction irrigator and tip, e.g., Impulse, Simpulse,
_ Care of the client undergoing surgery. fracture MicroAire (optional)
_ Patient education regarding side effects of hormone therapy. site may be needed to effect reduction. Again, care is taken during Supplies
the driving of the nail to avoid injury to the shaft. Use of multiple Ender Antiembolitic stocking, optional
nails can improve rotational stability; fanning of the proximal end helps Webril
control rotation. Small bones or fractures at the insertion site may Tube stockinette
Quickie tests and treatments complicate Esmarch bandage
Tests: use of Ender nails. X-rays are taken to visualize and document the Blades, (2) #10
_ Physical exam: distended kidney is palpable. repair. Hemostasis is assured before the wound is closed. Electrosurgical pencil and cord with holder and scraper
_ Bladder catheterization: detects site of the obstruction. Basin set
_ Urinalysis: increased white blood cells and presence of red blood Preparation of the Patient Needle magnet or counter
cells. An antiembolitic stocking may be placed on the unaffected extremity, Suction tubing (2) or cojoined suction and irrigation tubing for
_ Ultrasound: detects cause of the obstruction. as requested. General anesthesia or regional block anesthetic may be pulsed lavage
_ Intravenous urography: detects flow of urine through the kidneys. employed.The patient is supine; arms may be extended on padded Irrigation solution in bags (for pulsed lavage), or graduated
Treatments: armboards. pitcher, bulb syringes (2), antibiotic solutio
_ Immediate drainage of urine via needle directly into the kidney The safety strap is secured over the blanket-covered unaffected
through the skin. extremity. Sheet wadding and a tourniquet are placed high on the thigh
_ Surgery: remove obstruction. of the operative leg. An electrosurgical dispersive pad is applied.
_ Urethral stent: bypasses obstruction (this is used in chronic Skin Preparation
hydronephrosis). Care is taken to support the extremity to avoid further injury. Begin at
_ Hormone therapy for prostate cancer. the fracture site; prep the entire extremity. Include the leg, thigh (up
_ Prevent and treat infection and/or kidney failure promptly. to the tourniquet), and foot.
Draping
The supported leg is abducted and elevated; the foot is grasped and
covered
by a tube stockinette. A large sheet is draped over the end of the
Open Reduction and Internal Fixation
table.The stockinette is brought up (unrolled) to the level of the
of Fractures of the Tibial Shaft
tourniquet.
Definition
A folded towel (thirds, lengthwise) is wrapped around the top of
Realignment and fixation of a tibial shaft fracture.
the stockinette and secured. A split sheet is draped under the leg, or the
Discussion
leg may be passed through a sheet with a rubberized fenestration.A large
The type of fixation device is determined by the anatomic considerations
drape (or split) sheet is draped cephalad, over the thigh, and secured
of the fracture (e.g., comminuted, spiral, or “open”). Severely
underneath. The leg is passed through a fenestrated sheet (e.g.,
comminuted fractures may have to be treated with prolonged traction
transverse
rather than fixation.
Procedure or laparotomy), or additional drape sheets complete the draping.
Open Reduction and Internal Fixation of Fractures of the Tibial
Shaft is described. The fracture is exposed.Transverse bone screws or
plates (including compression plates) may be applied to reduce fracture
fragments. In addition, after the fragments have been reduced, an Equipment
intramedullary nail or rod may be employed (e.g., Ender nail or Rush Suction
rod) to fix a fractured tibia and provide improved rotational stability.An ESU
Ender nail is slightly curved and semi-elastic. An incision about the tibial Tourniquet and insufflator (tank of compressed air) with microprocessor
tuberosity is made.A drill reamer penetrates the medullary canal.The regulator
measured nail is inserted and aligned to avoid malrotation or shattering Power sources for drill and saw (unless power equipment is selfcontained)
the shaft of the tibia. Loose fragments and debris may be pulse lavaged Instrumentation
or irrigated with saline or an antibiotic solution.The Ender nail is then Basic orthopedic procedures tray
Bone-holding instruments trayFixation device and insertion
driven past the fracture site into the distal portion until the threaded end instrumentation
High-speed power drill, cord, chuck, key, and drill bits
Das könnte Ihnen auch gefallen
- MCN Print 3 NotesDokument1 SeiteMCN Print 3 NotesmarieNoch keine Bewertungen
- Geography of The BrainDokument1 SeiteGeography of The BrainmarieNoch keine Bewertungen
- Geography of The BrainDokument1 SeiteGeography of The BrainmarieNoch keine Bewertungen
- Newborn PaDokument34 SeitenNewborn PamarieNoch keine Bewertungen
- RNHeals AppformDokument1 SeiteRNHeals AppformmarieNoch keine Bewertungen
- Meet The Piano (So Simple., Made Simple)Dokument5 SeitenMeet The Piano (So Simple., Made Simple)marieNoch keine Bewertungen
- MCN Notes Print 1Dokument2 SeitenMCN Notes Print 1marieNoch keine Bewertungen
- Drug StudyDokument4 SeitenDrug StudymarieNoch keine Bewertungen
- Drug Study1Dokument3 SeitenDrug Study1marieNoch keine Bewertungen
- Behavioral Therapy by Kurt LewinDokument6 SeitenBehavioral Therapy by Kurt LewinmarieNoch keine Bewertungen
- Psychia Review Notes (Incmplt)Dokument3 SeitenPsychia Review Notes (Incmplt)marieNoch keine Bewertungen
- Ordinary QuotesDokument1 SeiteOrdinary QuotesmarieNoch keine Bewertungen
- Inguinal Hernia With LabsDokument10 SeitenInguinal Hernia With LabsmarieNoch keine Bewertungen
- Drug StudyDokument5 SeitenDrug Studymarie67% (3)
- Nursing Practice 1Dokument4 SeitenNursing Practice 1marieNoch keine Bewertungen
- Newborn PaDokument34 SeitenNewborn Pamarie100% (2)
- COPAR PREENTRY PHASE Preliminary Social InvestigationDokument3 SeitenCOPAR PREENTRY PHASE Preliminary Social InvestigationmarieNoch keine Bewertungen
- Colostomy ProcedureDokument2 SeitenColostomy Proceduremarie100% (2)
- Founder: Categories Christianity Confucianism Buddhism Taoism Islam HinduismDokument3 SeitenFounder: Categories Christianity Confucianism Buddhism Taoism Islam HinduismmarieNoch keine Bewertungen
- 11 Core Competencies Part 1 To Part 2Dokument4 Seiten11 Core Competencies Part 1 To Part 2marie100% (2)
- Buddhism BrochureDokument3 SeitenBuddhism Brochuremarie60% (10)
- China BrochureDokument2 SeitenChina BrochuremarieNoch keine Bewertungen
- Administering An Enema EQUIPMENT Prepackaged Enema or Enema Container DisposableDokument3 SeitenAdministering An Enema EQUIPMENT Prepackaged Enema or Enema Container Disposablemarie100% (2)
- Nasogastric Tube InsertionDokument3 SeitenNasogastric Tube Insertionmarie100% (5)
- ECGDokument2 SeitenECGmarie80% (5)
- The Aging Society: Its Effects On Health Care DeliveryDokument15 SeitenThe Aging Society: Its Effects On Health Care Deliverymarie100% (2)
- Nursing Action Rationale Preparatory PhaseDokument6 SeitenNursing Action Rationale Preparatory Phasemarie100% (2)
- Physiology of Aging 2005Dokument42 SeitenPhysiology of Aging 2005marie100% (2)
- Nasogastric Tube FeedingDokument6 SeitenNasogastric Tube Feedingmarie100% (5)
- Blood TransfusionDokument3 SeitenBlood TransfusionmarieNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Multiple Sclerosis: Asif KianiDokument37 SeitenMultiple Sclerosis: Asif Kianiasifk124100% (2)
- Urinary Tract InfectionDokument17 SeitenUrinary Tract InfectionMuhammad Shayan FarooqNoch keine Bewertungen
- Exercise Prescription Softwares PDFDokument5 SeitenExercise Prescription Softwares PDFNujella BalajiNoch keine Bewertungen
- Performance-Based Reward System Performance and Development Plan and Review DocumentDokument8 SeitenPerformance-Based Reward System Performance and Development Plan and Review DocumentMusyimi TitusNoch keine Bewertungen
- TivaDokument6 SeitenTivapaulina7escandar100% (1)
- Acupuncture For Cancer Baraye 1Dokument134 SeitenAcupuncture For Cancer Baraye 1mehranerezvani100% (3)
- HDF Vs HDDokument80 SeitenHDF Vs HDAndreea Livia DumitrescuNoch keine Bewertungen
- Guidance & Counseling": Rajesh Kumar LecturerDokument19 SeitenGuidance & Counseling": Rajesh Kumar LecturerLove DhaliwalNoch keine Bewertungen
- Narrative Chapter AssignDokument28 SeitenNarrative Chapter AssignAbrar RiazNoch keine Bewertungen
- Shiatsu and AcupressureDokument233 SeitenShiatsu and AcupressureYuan Xu86% (7)
- Joint Commission Tracers 2011: What Hospitals Need To KnowDokument223 SeitenJoint Commission Tracers 2011: What Hospitals Need To KnowAndreasAndokoNoch keine Bewertungen
- PCL's Avulsion FractureDokument22 SeitenPCL's Avulsion FractureNey da OnneyNoch keine Bewertungen
- Leadership Program BrochureDokument2 SeitenLeadership Program BrochureGeorge VascanNoch keine Bewertungen
- Older AdultsDokument4 SeitenOlder Adultsapi-293182319Noch keine Bewertungen
- CompexDokument17 SeitenCompexSilvia RuizNoch keine Bewertungen
- Century High SC ProDokument1 SeiteCentury High SC Proapi-406529580Noch keine Bewertungen
- Pharmacology MCQ PebcDokument36 SeitenPharmacology MCQ Pebcsnowden1100% (6)
- PSYB32 Final Exam ReviewDokument29 SeitenPSYB32 Final Exam Reviewraeesah9171Noch keine Bewertungen
- JAUNDICE Internal Medicine PresentationDokument34 SeitenJAUNDICE Internal Medicine PresentationNano BaddourNoch keine Bewertungen
- Case Presentation Output Checklist and Format and Master OutputDokument18 SeitenCase Presentation Output Checklist and Format and Master OutputVenRussAbestaNoch keine Bewertungen
- Feeding Minds The Impact of Foods On Mental Health PDFDokument69 SeitenFeeding Minds The Impact of Foods On Mental Health PDFDiana Elena Purdel100% (1)
- Ingle's EndodonticsDokument35 SeitenIngle's EndodonticsAndrei AntipinNoch keine Bewertungen
- Imaging of Sports Injuries in The Foot: James M. LinklaterDokument9 SeitenImaging of Sports Injuries in The Foot: James M. Linklaterpjanu86Noch keine Bewertungen
- Drug Abuse (Social Issue)Dokument2 SeitenDrug Abuse (Social Issue)IslamicGeneralKnowleNoch keine Bewertungen
- медицинаDokument10 SeitenмедицинаDariaNoch keine Bewertungen
- Positive End-Expiratory Pressure and Lung ComplianDokument6 SeitenPositive End-Expiratory Pressure and Lung ComplianElfahime HamzaNoch keine Bewertungen
- Carl Rogers - Person-Centered Theory PDFDokument21 SeitenCarl Rogers - Person-Centered Theory PDFAiden Lee50% (2)
- Analysis of Avi Kremer CaseDokument5 SeitenAnalysis of Avi Kremer CasejangveerNoch keine Bewertungen
- The New Somatic Symptom Disorder in DSM-5 Risks Mislabeling Many People As Mentally IllDokument2 SeitenThe New Somatic Symptom Disorder in DSM-5 Risks Mislabeling Many People As Mentally IllfortisestveritasNoch keine Bewertungen
- Coaching Worksheet BPD ResidentialDokument1 SeiteCoaching Worksheet BPD ResidentialAmy PowersNoch keine Bewertungen