Beruflich Dokumente
Kultur Dokumente
WakeMed Non-Hemorrhagic Stroke-TIA Admission Orders Rev 12-07i
Hochgeladen von
Nafilah SyellaOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
WakeMed Non-Hemorrhagic Stroke-TIA Admission Orders Rev 12-07i
Hochgeladen von
Nafilah SyellaCopyright:
Verfügbare Formate
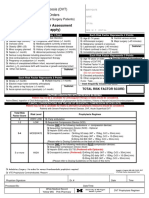
Ischemic (Non-Hemorrhagic Stroke) or TIA Orders
Check boxes of appropriate orders
PHYSICIANS ORDERS
108002
Date: Admit Status Admit to Admit to Diagnosis Condition Consults
Time:
Observation - For Medicare/Medicaid: Only appropriate for adverse outcomes post- op/post-procedure. Acute Inpatient - Document necessity of acute care and plan of care.
Service of Dr. _________________________________________
Labs
; ; ; ; ; ; ;
5B Monitored Bed
Diagnostics
Ischemic Stroke Stable Unstable Neurology Consult with Dr. _______________________________________________ Other: _________________________________________________________________ Physical Therapy; may advance activity per consult Occupational Therapy Speech Language Pathology Evaluation Rehab Evaluation Case Management Protocol Dietitian Evaluation If EKG report shows atrial fibrillation, Cardiology Consult with Dr. ________________ Nurse deliver Stroke Education information to patient. CBC with Diff CK with isoenzymes and Troponin stat and q 6hr x1 BMP C-RP Hepatic Function Panel U/A with urine culture and sensitivity PT Urine Drug screen PTT RPR Fasting Lipid Panel ESR Fasting Homocysteine Other ____________________________________ Fasting Lpa In AM: _______________________________________ Hemoglobin A1c Consider young stroke work-up for patients <55 years: Factor V Lieden Protein S activity Fibrinogen Level Protein C activity Antithrombin III Act Assay Lupus Inhibitor Anticardiolipin Antibody ANA Prothrombin Gene Mutation Other: __________________________ Sickle Cell Screen Head CT without contrast with contrast MRI of Brain without contrast with contrast MRA of Brain Circle of Willis neck blood vessels 2D Echocardiogram with bubble study read by ________________________________MD Carotid Ultrasound read by _________________________________MD EEG EKG CXR Other: ____________________________________________________
Other Monitored Bed NICU TIA R/O Stroke/TIA Other
Patient Identification:
Origin: 6/99 Last Rev: R12/07i Page 1 of 3
WakeMed Physicians Orders
Stroke Orders Folder Link in Medicine Folder
Ischemic (Non-Hemorrhagic Stroke) or TIA Orders
Nursing
108002
; Vital Signs q2hrs x 24 hours then q4hrs OR Other_______________________ ; Neurochecks q2hrs x 24 hours then q4hrs OR Other_______________________
Other: Oxygen SATS q ___________ If Sat less than 95% on room air, start O2 at _________________via ______________: Check oxygen sats with vital signs. If pulse oximetry is greater than 94% check sat on room air; If room air oxygen sat greater than 93% discontinue O2, then check sats q 2 hrs x 2. Notify MD if less than 92%. If on 6L of oxygen and SATS still less than 92% or change in resp. status, notify MD office and respiratory therapy for a bronchial hygiene evaluation consult. ; NIH Stroke Scale done on admission and at discharge ; Smoking Cessation Counseling if patient has smoked in the last year. ; IF blood glucose is greater than 150mg/dL OR history of diabetes initiate WakeMed Diabetes Glycemic Med-Surg Orders for Non-pregnant Adult: Standing Regimen: Home Other: ______________________________________________
Supplemental: (based on BMI) with Lispro Insulin (Humalog) Regular Insulin (Humulin R) and BG Target:____ Activity
; ;
Keep HOB elevated greater than or equal to 30 degrees Fall Precautions Seizure Precautions Strict Bed rest Advance activity level per Physical Therapy recommendation OOB with assistance
Treatments
IV NS _______mL/hr with ________mEq/L KCL Saline Lock Other:____________________________________________________________________________
Bowel Protocol:
Bladder and Bowel Mgmt
Bisacodyl (Dulcolax) 10mg PO/PR every other day in the morning AND add Docusate Sodium
(Colace) 100mg PO at bedtime if taking PO (Circle Preference: CAPS or LIQUID). Hold for loose stools. OR Docusate sodium (Colace) 100mg unit dose liquid at bedtime via feeding tube. Hold for loose stools. If no bowel movement every 3rd day, may give Bisacodyl (Dulcolax) 10mg or Sodium Biphosphate (Fleets) Enema 4.5 ounces x 1 PR. Bladder scan x 1 for post voiding residual; I&O cath if greater than 150mL and prn for incontinence
Diet
; Aspiration Precautions ; NPO including meds until dysphagia screen by nursing passed. Then advance diet per Speech and
Language Pathology recommendations or as tolerated to ___________.
If tube feedings indicated, start Promote at 20mL/hr and advance to 50mL/hr. Consult dietician for
tube feeding goal.
Other: _____________________________________________________
Patient Identification:
Origin: 6/99 Last Rev: R12/07i Page 2 of 3
WakeMed Physicians Orders
Stroke Orders Folder Link in Medicine Folder
Ischemic (Non-Hemorrhagic Stroke) or TIA Orders
Medications
108002
Home Meds: (See Medication Reference Sheet) ; Call MD with the names & doses of home meds prior to administering. DVT Prophylaxis: Unless contraindicated, subcutaneously anticoagulation is recommended for DVT prophylaxis over sequential compression devices. Heparin: 5,000 units subcutaneously Q 12hrs OR 5,000 units subcutaneously Q 8hrs
Enoxaparin (Lovenox) 40 mg subcutaneously daily Enoxaparin (Lovenox) 30 mg subcutaneously daily (recommended for CrCl less than 30 mL/min) ; Sequential Compression Device to lower extremities (if anticoagulation not ordered).
Antiplatelet or Anticoagulation (if indicated) not sooner than 24 hours after t-PA (Alteplase), if given:
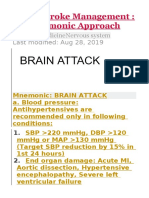
Enteric Coated Aspirin, if no Aspirin allergy or active GI bleed 325 mg PO daily Aspirin Suppository 300 mg PR daily Aspirin 325 mg via NGT daily Clopidogrel (Plavix) 75 mg po/NGT daily Extended Release Dipyridamole 200mg/ Aspirin 25mg (Aggrenox) 1 capsule PO Q 12hrs. Warfarin (Coumadin) ______mg PO/NGT q day at 1800 (if patient has a documented history of prothrombotic disorder or history of atrial fibrillation). Urgent anticoagulation with the goal of preventing early recurrent stroke, halting neurolological worsening, or improving outcomes after acute ischemic stroke is not recommended for treatment of patients with acute ischemic stroke. BLOOD PRESSURE MANAGEMENT: IF Systolic less than 220mm/Hg or Diastolic less than 120mm/Hg: Observe unless end organ involvement IF Systolic greater than 220mmg/Hg or Diastolic 121-140mm/Hg: *Labetalol (Normodyne) 10mg IV over 1-2 minutes. After initial dose, may repeat or double the dose q 10 minutes to up to a total dose of 300mg for a blood pressure of _____________mmHg. * Must be on a monitored bed when on Labetalol OR Nicardipine (Cardene) (25mg in 240 NS for concentration of 0.1 mg/mL) 5mg/hr IV infusion as initial dose and titrate up to a maximum dose of 15mg/hr for a desired blood pressure of _______mmHg by increasing 2.5mg/hr every 5 minutes Lipid Management:
Lipitor (Atorvastatin) 80 mg PO/NGT at bedtime Other Statin ____________________ (specify dose/route/frequency)
PRN Medications: Metoclopramide (Reglan) 10 mg IV/PO/NGT q 6 hrs PRN nausea/vomiting Metoclopramide (Reglan) 5 mg IV/PO/NGT q 6 hrs PRN nausea/vomiting (CrCl less than 40 mL/min) Ondansetron (Zofran) 4mg IV q 6 hrs PRN nausea
; Keep Normothermic: temp greater than 99F (fevers detrimental to acute brains). If not effective, consider external cooling. ; Acetaminophen (Tylenol)* 650mg PO/Per tube q 4hrs PRN mild to moderate pain or temp greater than or equal to 99F (fevers detrimental to acute brains). If not effective, consider external cooling. *Do Not Exceed 4000mg acetaminophen in 24 hours. Consider all sources.* For liver impairment or chronic liver disease, do not exceed 2000 mg acetaminophen in 24 hours. (To be checked by MD) Consider all sources. Other: Physician signature required: ____________________________ Beeper #:______---__________ Patient Identification: Transcribed by: ______________________________ Date: __________ Time: _______ Origin: 6/99 Last Rev: R12/07i Page 3 of 3 Checked by (Nurse): ____________________________ Date: _________ Time: _____
WakeMed Physicians Orders
Stroke Orders Folder Link in Medicine Folder
Das könnte Ihnen auch gefallen
- Acute Gastritis CPG FINALDokument5 SeitenAcute Gastritis CPG FINALkimadlo656Noch keine Bewertungen
- Admit OrdersDokument2 SeitenAdmit OrdersTariq Niaz Ahmad, MDNoch keine Bewertungen
- VTE Risk AssessmentDokument2 SeitenVTE Risk AssessmentpriyopanjiNoch keine Bewertungen
- Aripiprazole AbilifyDokument2 SeitenAripiprazole AbilifyKristi Wray100% (2)
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingVon EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNoch keine Bewertungen
- Fluoxetine Duloxetine SertralineDokument7 SeitenFluoxetine Duloxetine SertralineReneé Camille100% (1)
- General Surgery Admission Order Set - Sample Template: Code StatusDokument4 SeitenGeneral Surgery Admission Order Set - Sample Template: Code StatusEricka SwordNoch keine Bewertungen
- Clinical Pathway - Stroke Without Thrombolytic TherapyDokument4 SeitenClinical Pathway - Stroke Without Thrombolytic TherapysiusiuwidyantoNoch keine Bewertungen
- Cadiac Surgery Vascular SurgeryDokument12 SeitenCadiac Surgery Vascular SurgeryRaJeev K SookunNoch keine Bewertungen
- Cardene IV Order SetDokument2 SeitenCardene IV Order SetJoe McCoyNoch keine Bewertungen
- Purpose: CVA (Stroke) Patients (Ischemic and Hemorrhagic), Management ofDokument4 SeitenPurpose: CVA (Stroke) Patients (Ischemic and Hemorrhagic), Management ofRoxanne AlvarezNoch keine Bewertungen
- Nursing Module For Brain StrokeDokument27 SeitenNursing Module For Brain StrokeziadabiakarNoch keine Bewertungen
- Practice Midterm Test.Dokument16 SeitenPractice Midterm Test.Marku LeeNoch keine Bewertungen
- Miami Dade College Care Plan ModelDokument11 SeitenMiami Dade College Care Plan ModelllubicabarkovicNoch keine Bewertungen
- ICU Admission Orders Page 1 of 5Dokument5 SeitenICU Admission Orders Page 1 of 5ramzicard943Noch keine Bewertungen
- CCU HandoverDokument9 SeitenCCU Handoverapi-192342497Noch keine Bewertungen
- Thrombosis Risk Factor Assessment (Choose All That Apply) : Deep Vein Thrombosis (DVT) Prophylaxis OrdersDokument2 SeitenThrombosis Risk Factor Assessment (Choose All That Apply) : Deep Vein Thrombosis (DVT) Prophylaxis OrdersPutu Gizha Satrya GautamaNoch keine Bewertungen
- Severe TBI 2017Dokument18 SeitenSevere TBI 2017DM internaNoch keine Bewertungen
- Post Op CABG OrdersDokument4 SeitenPost Op CABG OrdersMaria Nadia MihalikNoch keine Bewertungen
- 16464-Article Text-54657-1-10-20170124Dokument4 Seiten16464-Article Text-54657-1-10-20170124Aashish KalikaNoch keine Bewertungen
- Total Hip and Knee ReplacementsDokument57 SeitenTotal Hip and Knee ReplacementsBryndenNoch keine Bewertungen
- Anemia-Careplan For AdultDokument29 SeitenAnemia-Careplan For AdultdjbhetaNoch keine Bewertungen
- Acute Stroke ManagementDokument8 SeitenAcute Stroke ManagementГурам ЧахвадзеNoch keine Bewertungen
- Post-Op Orders - Reginald W. Martin, M.DDokument2 SeitenPost-Op Orders - Reginald W. Martin, M.DIbrahim AlmohiniNoch keine Bewertungen
- Drug Study AdalatDokument4 SeitenDrug Study AdalatLea CelestialNoch keine Bewertungen
- Problem 2Dokument9 SeitenProblem 2Chan Myae NaingNoch keine Bewertungen
- Client Information Sheet (CIS)Dokument10 SeitenClient Information Sheet (CIS)Christine RombawaNoch keine Bewertungen
- A I - E M: Drenal Nsufficiency Mergency AnagementDokument12 SeitenA I - E M: Drenal Nsufficiency Mergency AnagementCaity YoungNoch keine Bewertungen
- Medication FlashcardsDokument10 SeitenMedication FlashcardsSilvio PerezNoch keine Bewertungen
- Medically Compromised PaftientsDokument21 SeitenMedically Compromised PaftientsLedjon KaciNoch keine Bewertungen
- Pediatric Acute Sepsis: Physician'S OrdersDokument4 SeitenPediatric Acute Sepsis: Physician'S OrdersSughosh MitraNoch keine Bewertungen
- Apixaban Eliquis MonographDokument14 SeitenApixaban Eliquis MonographTran Minh NgocNoch keine Bewertungen
- Nursing Care PlansDokument11 SeitenNursing Care PlansBryan Neil GarmaNoch keine Bewertungen
- Doctor's OrdersDokument6 SeitenDoctor's OrdersKryza Dale Bunado BaticanNoch keine Bewertungen
- Admission OrdersDokument3 SeitenAdmission Ordersoyim sNoch keine Bewertungen
- Pharmacology-Final Na JudDokument17 SeitenPharmacology-Final Na JudDizerine Mirafuentes RolidaNoch keine Bewertungen
- COVID-19 Protocol KGMU Version 6.0 17-4-21Dokument34 SeitenCOVID-19 Protocol KGMU Version 6.0 17-4-21Kirtivaan MishraNoch keine Bewertungen
- Grave's Diseases ManagementDokument18 SeitenGrave's Diseases ManagementHidvardNoch keine Bewertungen
- Volume 2 GDVs and More - Rev1 Ed6jvjDokument39 SeitenVolume 2 GDVs and More - Rev1 Ed6jvjErhan ErtuçNoch keine Bewertungen
- Traumatic Brain Injury 2023Dokument17 SeitenTraumatic Brain Injury 2023Fernando Martinez AguilarNoch keine Bewertungen
- IV Iron Orders Outpatient 11.2018 PDFDokument1 SeiteIV Iron Orders Outpatient 11.2018 PDFMuhammad SaeedNoch keine Bewertungen
- MRCP Part 1Dokument38 SeitenMRCP Part 1走过一些路Noch keine Bewertungen
- Ventura County Medical Center: Mi Thrombolysis, Management ofDokument3 SeitenVentura County Medical Center: Mi Thrombolysis, Management ofblackcat657Noch keine Bewertungen
- Acs 11 190524110746Dokument46 SeitenAcs 11 190524110746Obakeng MandaNoch keine Bewertungen
- Medical Toxicology Part 2Dokument68 SeitenMedical Toxicology Part 2chuck kieNoch keine Bewertungen
- Drug Monograph XareltoDokument2 SeitenDrug Monograph XareltoBenNoch keine Bewertungen
- 508 Medication PreAssignmentDokument9 Seiten508 Medication PreAssignmentMikeNoch keine Bewertungen
- Lisinopril, TAB: Generic Name of Medication: Brand/trade Name of MedicationDokument6 SeitenLisinopril, TAB: Generic Name of Medication: Brand/trade Name of MedicationCliff by the seaNoch keine Bewertungen
- Case Study, Chapter 54, Management of Patients With Kidney DisordersDokument4 SeitenCase Study, Chapter 54, Management of Patients With Kidney DisordersInsieNoch keine Bewertungen
- Inclusion Criteria:: Urinary Tract Infection Care MapDokument9 SeitenInclusion Criteria:: Urinary Tract Infection Care MapMoh. H.AlObaidyNoch keine Bewertungen
- Stroke by Dr. Amit RoyDokument32 SeitenStroke by Dr. Amit RoyDr Sutanwi DasNoch keine Bewertungen
- Acute Coronary Syndrome (ACS) : Basic Principles For ACSDokument4 SeitenAcute Coronary Syndrome (ACS) : Basic Principles For ACSRendra DananjayaNoch keine Bewertungen
- PRE ANAESTHETIC ASSESSMENT New 1Dokument41 SeitenPRE ANAESTHETIC ASSESSMENT New 1lokeswara reddyNoch keine Bewertungen
- Laparoscopic AdrenalectomyDokument21 SeitenLaparoscopic AdrenalectomyHu EyongNoch keine Bewertungen
- Clonidine Hydrochloride (Drug Study)Dokument2 SeitenClonidine Hydrochloride (Drug Study)Franz.thenurse688875% (4)
- Acute Myocardial Infarction: Recognition and AssessmentDokument7 SeitenAcute Myocardial Infarction: Recognition and AssessmentHasnainKhimjiNoch keine Bewertungen
- Discharge Advice After Your Coronary Angiogram, Angioplasty or Stent Insertion (PCI)Dokument16 SeitenDischarge Advice After Your Coronary Angiogram, Angioplasty or Stent Insertion (PCI)Nazmul Alam FarukiNoch keine Bewertungen
- Drugs ACSDokument5 SeitenDrugs ACSGilbert NeahNoch keine Bewertungen
- 6 - Fahad Class 6 Cardiac AnesthesiaDokument18 Seiten6 - Fahad Class 6 Cardiac AnesthesiaOne ClickNoch keine Bewertungen
- IFM+Toolkit+Table+of+Contents v19Dokument13 SeitenIFM+Toolkit+Table+of+Contents v19khaled dewanNoch keine Bewertungen
- Open Heart Surgery CaabgDokument6 SeitenOpen Heart Surgery CaabgGopi KrishnanNoch keine Bewertungen
- 2017 Spine CPT Code Changes: Kim Pollock, RN, MBA, CPC, CMDPDokument4 Seiten2017 Spine CPT Code Changes: Kim Pollock, RN, MBA, CPC, CMDPZakariaAwaludinNoch keine Bewertungen
- Icu-Related Dysphagia Epidemiology, Pathophysiology, Diagnostics and TreatmentDokument6 SeitenIcu-Related Dysphagia Epidemiology, Pathophysiology, Diagnostics and TreatmentLuis De jesus SolanoNoch keine Bewertungen
- LAS For Summative Assessment (Written Work Performance Task)Dokument2 SeitenLAS For Summative Assessment (Written Work Performance Task)Angel Dela CruzNoch keine Bewertungen
- All India Institute of Medical Sciences, Nagpur Result NotificationDokument4 SeitenAll India Institute of Medical Sciences, Nagpur Result NotificationNayan ChaudhariNoch keine Bewertungen
- Acosta, Joyce Ara T. Week 7 & 8 Drug StudyDokument11 SeitenAcosta, Joyce Ara T. Week 7 & 8 Drug StudyJoyce Ara Tumbaga AcostaNoch keine Bewertungen
- Final PhysicalDokument409 SeitenFinal PhysicalAbhishiktaAbhiNoch keine Bewertungen
- Case Obsos SellyDokument24 SeitenCase Obsos SellyDwi CahyaNoch keine Bewertungen
- MSE DepressionDokument3 SeitenMSE DepressionSam Raven AndresNoch keine Bewertungen
- Dr. Mohammed Shahedur Rahman Khan Bronchial Asthma Management Aspects - Current and FutureDokument32 SeitenDr. Mohammed Shahedur Rahman Khan Bronchial Asthma Management Aspects - Current and FutureShahadat Hossain BabuNoch keine Bewertungen
- Somniferous Poisons: DR M. Malleswari Asso. Prof Nri Medical CollegeDokument58 SeitenSomniferous Poisons: DR M. Malleswari Asso. Prof Nri Medical CollegeSudheera RachamallaNoch keine Bewertungen
- White Blood Cells TugasDokument6 SeitenWhite Blood Cells TugasanisaNoch keine Bewertungen
- Medical DeviceDokument45 SeitenMedical DevicewardaddyNoch keine Bewertungen
- Asthma Treatment GuidlineDokument56 SeitenAsthma Treatment GuidlineEsther OdumanyeNoch keine Bewertungen
- Cardiac GlycosidesDokument5 SeitenCardiac Glycosidesapi-347182709100% (1)
- 4 Circulation Disorders PDFDokument69 Seiten4 Circulation Disorders PDFSetiawan SukmadjaNoch keine Bewertungen
- Renal Function TestsDokument23 SeitenRenal Function TestsKer YehunNoch keine Bewertungen
- India's 1 Health Management LabDokument14 SeitenIndia's 1 Health Management LabAjay Kumar dasNoch keine Bewertungen
- Hematology LaboratoryDokument3 SeitenHematology LaboratoryDee GeeNoch keine Bewertungen
- Sahi ExportDokument8 SeitenSahi ExportHeena ChoudharyNoch keine Bewertungen
- Muscular System FunctionDokument2 SeitenMuscular System FunctionLachlan PalmerNoch keine Bewertungen
- Therapeutic Conference: FacilitatorsDokument4 SeitenTherapeutic Conference: FacilitatorsJolaine ValloNoch keine Bewertungen
- Small Pox: A Child Infected With SmallpoxDokument5 SeitenSmall Pox: A Child Infected With SmallpoxJavee_Viccent__5618Noch keine Bewertungen
- Prolapse Lumbar DiscDokument40 SeitenProlapse Lumbar DiscAlfred BantigueNoch keine Bewertungen
- A Patient of Poisoning in ICU (Ankit Jain)Dokument48 SeitenA Patient of Poisoning in ICU (Ankit Jain)SharryNoch keine Bewertungen
- Immunochemistry and BiosensorsDokument13 SeitenImmunochemistry and BiosensorsPalak AgarwalNoch keine Bewertungen
- Quiz TraumaDokument1 SeiteQuiz Traumaaqsa rehmanNoch keine Bewertungen
- Surgery Surgical Nursing Objs With AnsDokument136 SeitenSurgery Surgical Nursing Objs With AnsmintahmeshackbenjaminNoch keine Bewertungen