Beruflich Dokumente
Kultur Dokumente
Blacktown Clinical Competencies
Hochgeladen von
Eriya JufriOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Blacktown Clinical Competencies
Hochgeladen von
Eriya JufriCopyright:
Verfügbare Formate
BLACKTOWN INTENSIVE CARE UNIT Clinical Competencies
Name:_____________________________________
Commencement Date:___________________
Rationale- To provide safe and effective care for patients requiring management in the intensive care environment. Clinical competencies are to be completed within set time frame Clinical competencies are to be assessed by CNE, NUM or CNS working in ICU or your appointed Mentor Compiled by Larissa McTegg ACNE Danielle Callaghan ACNE Kaye Williams CNS Using ICU Competency & Professional Development Record
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
COMPETENCY:- VENTILATION / O2 THERAPY Aim of competency Physical assessment of patients respiratory function Assessment of patients ventilation and oxygenation status Provide safe and effective care to patients receiving ventilatory and/or oxygenation support
Elements of competency 1. 2. 3. 4. 5. 6. 7. 8. 9. Respiratory assessment O2 therapy Care of ventilated patient BIPAP / CPAP Intubation Extubation Oxylog Transport ventilator Tracheostomy Care Under Water Seal Drains (UWSDs)
-2-
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 1- Respiratory physical assessment Observable Criteria Inspects the patients chest, observing for equal rise & fall of chest, any structural abnormalities or abnormal chest wall movement Questions to be asked by assessor Why is it important to assess rise & fall of chest? What structural abnormalities may indicate a problem? (Tracheal shift, flail chest) Shown Safe Competent Actions
Auscultates the patients chest. Checks for equal air entry and identifies abnormal breath sounds
What are the types of breath sounds & what do they indicate?
Observes colour of mucous membranes
Why is mucous membrane colour important?
Inspects patients CXR and identifies landmarks
Identifies any abnormalities on CXR and outlines what the abnormality represents
-3-
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 2- O2 therapy Observable Criteria NASAL CANNULA (PRONGS) Outlines appropriate flow rates o 1-4lpm providing 23-35% O2 Questions to be asked by assessor What are the advantages of nasal prongs? Is CO2 retention a problem for patients who are using nasal prongs? Shown Safe Competent Actions
Outlines disadvantages of NP o Local irritation & drying of mucous membranes o low concentrations of O2
Can nasal prongs have a higher flow rate than 4lpm? When would you use NP when other forms of O2 therapy are in use?
HUDSON MASK Outlines flow rates o 5-10lpm providing 35-50% O2
How does expired gas leave a Hudson mask? What is a major disadvantage of the Hudson mask, with regards to delivered and received fio2?
VENTURI MASK Outlines flow rates o 50% o 40% o 35 o 31% o 28% o 24%) Outlines venturi principle
What is the advantage of the venturi mask over the Hudson mask? Does the patient re breathe their own Co2?
Explain the venturi principle
NON REBREATHER Outlines flow rates o 15lpm providing 90-100% O2 o Flow great enough to prevent reservoir bag collapsing on inspiration
What is the importance of the reservoir bag on the mask? How do you inflate the reservoir bag if it does not inflate spontaneously before you put it on the patient?
-4-
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 3- Care of Ventilated patient Observable Criteria Set up of Evita 4 Ventilator Gathers equipment for set up Can demonstrate set up and testing of circuit. Questions to be asked by assessor Shown Safe Competent Actions
Why is it important to do a self-test on the ventilator? When changing part of ventilator circuit what test must be performed?
Demonstrates ability to measure & accurately document ventilation observations How often should you download and validate Adheres to unit practice in documentation of observations? ventilator observations Downloads & validates ventilator observations correctly in CIS adds appropriate information to CIS Correctly distinguishes between controlled, assisted & spontaneous breathes Takes best of three breathes when documenting tidal volumes Adds appropriate information to CIS o type of tube (ETT / Tracheostomy) o Evita 4 / Evita 2 Discusses rationale for humidification & rationale for set temperature Why is it important to have humidification set at the proper temperature, and what is that temperature? What extra information should be added to the CIS that is not automatically downloaded?
How do you distinguish between controlled, assisted and spontaneous breaths? Why is it important to take the best of three breaths when recording the tidal volume?
Demonstrates the appropriate settings and check of ventilator alarms What is this alarm? Apnea alarm limits Why is it important that we check and set this o ensures alarm is on alarm for each individual patient? o apnea delay o apnea Vt & rate High Vt What is this alarm? Why do we set a high Vt alarm? What is this alarm? Why do we set a high pressure limit alarm? What does minute volume indicate? Why do we set a low minute volume limit? What is the lowest limit acceptable? What is tube compensation? Why is it used?
High Pressure limit (PAW)
Low minute volume
Tube compensation on/off
-5-
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc Element 3- Care of Ventilated patient Observable Criteria Managing Alarms Outline the reasons behind and management of these alarms o tidal Volume High o Low Minute Volume o High Pressure Alarm o Apnea Questions to be asked by assessor Why do you need to press the alarm-reset button after the apnea alarm has sounded? How do you tell if the apnea alarm is turned on? What is the immediate action for management of these alarms? Shown Safe Competent Actions
Modes of Ventilation Is able to differentiate between various modes of ventilation
What is CPAP & PEEP What is PS What is SIMV PCV APRV CPAP & PEEP PS SIMV PCV APRV
Outlines the advantages / disadvantages of each mode
Notes size & position of ETT / Tracheostomy Is able to explain importance of correct positioning & size of tube
When do you chart the size and position of the ETT? Why is it important to chart the position of the ETT? Why is it important to confirm position on CXR prior to repositioning? What equipment is needed to reposition tube? Who should assist with this procedure? Why is it necessary to recheck cuff pressure? Why do we listen to air entry? Why is it necessary to observe the patient following repositioning? Why is a CXR necessary following repositioning of ETT
Repositions tube as ordered by medical staff o Confirms ETT position on CXR before repositioning o Repositions ETT to correct placement and secures ETT appropriately Checks cuff pressure following repositioning Listens for equal air entry Observes for respiratory distress post repositioning Informs MO ETT is repositioned and organizes CXR
-6-
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc Element 3- Care of Ventilated patient Observable Criteria Questions to be asked by assessor Demonstrates methods of securing ETT and Tracheostomy How many nurses are required to secure an ETT Adheres to unit practice in securing or a trachy? ETT Tracheostomy Ensures tube is secure Observes skin integrity What are some preventive measures to ensure good skin integrity? Shown Safe Competent Actions
Maintains adequate ETT / tracheostomy cuff seal & correct measurement of cuff pressure Maintains cuff pressure within acceptable range What is the acceptable range for both the ETT and trachy cuff pressure? Correctly records cuff pressure in CIS Why is it important to chart the cuff pressure in the CIS? Why do we need to check cuff pressure regularly? How do you tell if you have a cuff leak and what action should you take?
Checks cuff pressure 4/24 Discusses management of cuff leaks
Suctioning ETT / Tracheostomy Outlines reasons for suctioning Explains procedure to patient where necessary Gathers equipment Uses correct PPE for procedure Pre-oxygenates patient prior to procedure
Why do patients with an artificial airway require suctioning?
What is the importance of pre-oxygenating a patient prior to suctioning? How long should you have the suction catheter down the patients airway for?
Attempts two passes according to unit protocol
Flushes trache care and suction tubing after procedure
Nebulisers Can demonstrate the connection / disconnection of Nebuliser to circuit Adheres to units policy with PPE How do you safely disconnect the ventilator circuit to avoid a splash injury when adding a Nebuliser to the circuit? Why is timing important when administering an MDI?
Demonstrates the use of MDI
-7-
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 3- Care of Ventilated patient Observable Criteria Ventilator Emergency Explain what a ventilator emergency is Laerdel Bag Demonstrate laerdel bag set up in < 1 minute Demonstrates the appropriate testing of a Leardel bag Outlines the signs of a ventilator emergency Outlines the protocol for dealing with a ventilator emergency What is your first priority during a ventilator emergency? Questions to be asked by assessor Shown Safe Competent Actions
What is one of the main mistakes when setting up a Leardel bag? Why is it important to test a Leardel bag if the previous shift has done it? Why should you still have a facemask at the bedside, even when you have a ventilated patient?
Explain the principle of a PEEP valve Demonstrates manual ventilation using laerdel bag
Humidification Justify the use of humidification in the circuit Set correct temperature on humidifier for ventilator circuit and explain the reasons behind the temperatures
Why do we humidify our ventilator circuit?
-8-
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 4- BIPAP Observable Criteria Set up of BiPAP Vision machine Gathers equipment for set up Can demonstrate set up Tests exhalation port appropriately Why do you need to test the exhalation port? Questions to be asked by assessor Shown Safe Competent Actions
Demonstrates ability to measure & accurately document BIPAP observations What is IPAP and EPAP? Correctly distinguishes between ST and CPAP Should the BiPAP be turned on or off before modes connecting the patient? Adheres to unit practice in documentation of BIPAP observations Takes best of three breathes when documenting tidal volumes Enters BIPAP observations correctly in CIS adds appropriate information to CIS Adds appropriate information to CIS: Type of mode Discusses rationale for humidification & identifies correct set temperature Why is it important to press Learn Base Flow when connecting / disconnecting Nebuliser? What would you check if your patient was not receiving the required pressures? Why is it important to take the best of three breaths? What values should be charted on the CIS and why?
Choice of mask Explain the positive and negative effects of using: Regular mask Full face mask
How do you get a claustrophobic patient used to the BiPAP mask?
Demonstrates the appropriate settings of BIPAP alarms How do you tell if the apnea alarm is on or off? Apnea alarm limits Ensures alarm is on Apnea delay Apnea rate High Vt What is the importance of the high-pressure alarm?
High Pressure limit Low minute volume
-9-
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 4- BIPAP Observable Criteria Contraindications Explain why you would use caution when feeding a patient Questions to be asked by assessor What is a possible side effect of a patient who has just eaten and then swallows air at high pressure? Shown Safe Competent Actions
Humidification Explain the importance of humidification Set correct temperature on humidifier for BiPAP circuit and explain the reasons behind the set temperature
Do you set the same temperature for BiPAP that you would set for a patient with an ETT?
Element 5- Intubation Observable Criteria Discusses indications for intubation Assembles equipment Demonstrates application of cricoid pressure Questions to be asked by assessor Shown Safe Competent Actions
Explain the importance of all the equipment required for intubation. What is the importance of cricoid pressure? When do you release cricoid pressure?
Explains reasons for drugs that may be used Fentanyl Propofol Aramine Midazolam Rocuronium Explain the importance of a set ventilator mode as opposed to a spontaneous mode when using some of these drugs.
Suxamethonium
Post Intubation Secure ETT Explains importance of CXR to locate ETT and NGT Ensures adequate sedation ordered and administered Where is the appropriate position for the ETT to sit on the CXR? Why is sedation needed post intubation?
- 10 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 6- Extubation Observable Criteria Questions to be asked by assessor Shown Informs ICU Reg and Nursing Team Leader of intention to extubate after medical order has been given and documented. Assembles equipment Suctions patient via ETT Aspirates NG tube and documents aspirate in CIS Why is it important to cease feeds prior to extubation and how long should they be ceased before extubation? Why is it important to aspirate the NG prior to extubation? What oxygen concentration would you put the patient on post extubation? Safe Competent Actions
Connects appropriate O2 mask and turns on O2
Suctions oropharynx Explains procedure to patient Suctions via ETT when extubating Suctions oral cavity after extubation Documents extubation and new O2 therapy in CIS What signs should you observe post extubation? What would you do if your patient failed extubation?
Post Extubation Ensures resp rate monitoring turned on
The CIS automatically downloads the respiratory rate as a part of the routine observations. Should you rely on this post extubation? What are the signs and symptoms of respiratory distress? Why are ABGs attended one hour post extubation?
Closely monitors O2 sats and patients respiratory effort Checks ABGs results 1 hour post extrubation
- 11 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 7- Oxylog transport ventilator Observable Criteria Set up of Oxylog Ventilator Locates Oxylog machine and tubing Questions to be asked by assessor Shown Safe Competent Actions
What do you do with the tubing once you have finished with it?
Gathers big O2 bottle and ensures enough O2 Demonstrates correct set up of Oxylog Performs pre use check of Oxylog Why is it important to do a pre use check on the Oxylog?
Sets appropriate settings on Oxylog Documents parameters in the CIS
Element 8 Tracheostomy Care Observable Criteria Insertion of Tracheostomy List the indications for the insertion of a Tracheostomy Demonstrate the set up of Tracheostomy Questions to be asked by assessor Shown Safe Competent Actions
What equipment is required for a Tracheostomy and why?
Nursing Responsibilities Ensure appropriate equipment is kept at the bedside
What is the appropriate equipment and why should it be at the bedside?
- 12 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 8 Tracheostomy Care Observable Criteria Suctioning Tracheostomy Outlines reasons for suctioning Explains procedure to patient where necessary Gathers equipment Uses correct PPE for procedure Uses sterile gloves Why are sterile gloves needed to suction, when you do not use sterile gloves to suction an ETT? Why is it important to check the Trach care size before you suction a patient with a closed suction system? How often should suctioning of a Tracheostomy be attended? What parameters should you observe when suctioning? Questions to be asked by assessor Shown Safe Competent Actions
Attempts two passes according to unit protocol
Humidification Explain the importance of humidification Set correct temperature on humidifier for Tracheostomy
Why is humidification important for a patient with a tracheostomy?
Types of Tracheostomy Discusses the different Tracheostomy: percutaneous or surgical
Explain why a patient may have a surgical as opposed to a percutaneous tracheostomy.
Tracheostomy dressing Outline the policy for a tracheostomy dressing
How many staff required for a Tracheostomy dressing? When would you do a swab on a tracheostomy?
Demonstrate a tracheostomy dressing
- 13 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 9 Under Water Seal Drains Observable Criteria INDICATIONS FOR INSERTION List the indications for the insertion of an UWSD Questions to be asked by assessor Why would you insert an UWSD? Shown Safe Competent Actions
Insertion Gathers equipment required for the insertion of an UWSD Demonstrates correct set up of equipment Why is it important to maintain a sterile field when setting up the equipment for an UWSD?
Observations Demonstrates correct observations of UWSD
How often should UWSD observations be done? When attending observations, should suction be on or off? Do you clamp the UWSD during routine observations?
Explain the meaning of: Oscillation Bubbling Draining
Suction Demonstrate the set up of a Low Wall suction outlet
Do you use low or high suction for an UWSD? What is the suction to be set at when the UWSD is on low wall suction?
Dressing Demonstrates an occlusive and anchoring dressing to the chest drain.
Why does the dressing need to anchor the chest drain? Why does the dressing need to be occlusive?
Removal Gathers equipment required for removal of UWSD Demonstrates the removal of an UWSD Ensures CXR 4 hours post removal
What equipment is required for removal of a chest drain? What is the idea behind the purse string suture? Why is it important to do post removal CXR?
- 14 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
COMPETENCY:- HEMODYNAMIC MONITORING
Aim of Competency Assessment of patients cardiac function Provide safe and affective care to patients receiving cardiac support
Elements of Competency 1. 2. 3. 4. 5. 6. 7. 8. Cardiac monitoring Managing Arrythmias 12 Lead ECG CVP Arterial lines PICCO Inotropes Pulmonary Artery Catheters
- 15 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 1 Cardiac Monitoring Observable Criteria Marquette Monitor Can identify correct lead placement for cardiac monitoring Displays cardiac rhythm in Lead II Sets appropriate vital sign alarms according to patient and explains reasons for same Downloads and validates vital signs observations and cardiac rhythm in the CIS Questions to be asked by assessor Shown Safe Competent Actions
Why is it important to monitor in Lead II?
What limits would you set for alarms?
What do you do if the downloaded observations are vastly different from what your patient has had all shift? How frequently do you zero your arterial line? Why should you NOT leave the five minute silence alarm on, when things have returned to normal? How do you trouble shoot artifact on your monitor?
Ensures any change in vital signs are downloaded and validated
Transport Monitor Identifies correct lead placement for cardiac monitoring Displays cardiac rhythm in Lead II Sets appropriate alarm limits for the trip outside the unit Do you need to review the alarm limits if you are only going to CT and back?
- 16 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc Element 2 Managing Arrhythmias Observable Criteria Detects each rhythm below & discusses management Normal Sinus Rhythm Sinus Tachycardia Sinus Bradycardia Atrial Fibrillation Atrial Flutter Supraventricular Tachycardia Ventricular Tachycardia Ventricular Fibrillation Asystole Questions to be asked by assessor What actions would you take for each rhythm? What rhythms would you defibrillate? What is the difference between defibrillation and cardio version? What do you do if you are unsure of a rhythm? Shown Safe Competent Actions
- 17 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 3 12 Lead ECG Observable Criteria Identifies indication for an ECG to be performed Questions to be asked by assessor Identifies indications for 12 lead ECG Shown Safe Competent Actions
Performs 12 Lead ECG Gathers appropriate equipment Identifies correct patient Explains procedure to patient Maintains patients privacy Applies leads in correct position Removes jewelry How often do you change the ECG dots on your patient? Why should jewelry be removed before an ECG is attended?
Clips hair if necessary does not shave Positions patient correctly Acquires EGC on monitor and prints How do you get the ECG to download to the CIS? How do you trouble shoot artifact when trying to do an ECG?
Shows ICU team the ECG to review and sign Places printed ECG into patients folder Documents appropriately in CIS Returns monitor to display Lead II and turns off V2-V6 fail Why do you change the monitor to monitoring rather than diagnostic after the ECG?
- 18 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 4 Central Venous Pressure (CVP) Observable Criteria Discusses units policy for taking CVP measurement Ensures correct set up to take a CVP measurement including correct lumen placement Takes CVP measurement as per units policy Questions to be asked by assessor What is the CVP measuring? Why is it important for the patient to be lying flat? What lumen must the CVP be attached to and why? What effect does PEEP have on CVP? How frequently are CVPs attended? Shown Safe Competent Actions
Documents CVP correctly in CIS Competently removes CVC as per unit policy How is patient positioned for CVC removal During what part of the respiratory cycle is CVC removed What maneuver do you ask the patient to undertake for removal (if able to)
Element 5 Managing Arterial lines Observable Criteria Indications for Insertion of Arterial line Lists indications for arterial line insertions Demonstrates and explains reason for Allans test Outlines the potential risks of an Arterial line What actions would you take if the observations altered to both the insertion site and limb observations? Why is it important to observe the insertion site regularly? Questions to be asked by assessor Name the different insertion sites of an arterial line Shown Safe Competent Actions
Demonstrates the set up of an arterial line insertion Gathers equipment to set up Attaches label with Date and Time
Why is it important to maintain an appropriate pressure in your pressure bag? What pressure should your pressure bag be kept at?
- 19 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 5 Managing Arterial lines Observable Criteria Management of an Arterial line Performs and correctly documents arterial line observations on the CIS Questions to be asked by assessor Checks alarm limits for arterial line at the beginning of shift and documents same correctly in CIS Demonstrates correct procedure for zeroing the transducer Demonstrates an arterial line dressing as per unit protocol How would you assess the accuracy of arterial lines? How can you tell if you have a dampened arterial trace? How do you know what the alarm limits should be set at? Why is it necessary to zero transducers and how often should it be done? How frequently should your arterial line dressing be attended? Shown Safe Competent Actions
Demonstrates the method of securing an arterial line as per unit protocol
Why is it important to make sure that your securing tape is not too close to the arterial insertion site?
Removal of Arterial line Checks coag results before removal Checks with ICU team for any bloods to be taken before removal Demonstrates the removal of an arterial line as per units policy Documents removal of line correctly on CIS
Why do coags need to be checked prior to removal of arterial line?
How long do you need to apply pressure to the insertion site for post removal of line? Why is it important to document removal of the arterial line in the CIS?
- 20 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 6 PICCO Observable Criteria Insertion of PiCCO line: Lists indications for PiCCO line insertions Questions to be asked by assessor Gathers machine and equipment required Demonstrates the set up of an PiCCO line insertion Outlines the potential risks of an PiCCO line What are the possible insertion sites for PiCCO lines and what is the reason for this? Why do we need a CVC and where would it need to be? Shown Safe Competent Actions
Management of a PiCCO line Performs and correctly documents PiCCO line observations hourly on the CIS
How would you assess the accuracy of PiCCO lines? What parameters do you document each hour? What do the following abbreviations stand for: CO / CI? SVR / SVRI? EVLW / EVLWI?
Checks alarm limits for PiCCO on Marquette monitor at the beginning of shift and documents same correctly in CIS Demonstrates correct procedure for gaining accurate waveform on Marquette monitor Demonstrates PiCCO calibration procedure Why is it necessary to zero transducers and how often should it be done? How often do we need to calibrate the PiCCO? What lumen on the CVC is needed for effective calibration of the PiCCO? Why do we need a CVP to calibrate the PiCCO?
Documents extra parameters once machine calibrated Demonstrates an PiCCO line dressing as per unit protocol Demonstrates the method of securing an PiCCO line Why is it important to observe the insertion site regularly?
- 21 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc Element 6 PICCO Observable Criteria Removal of PiCCO line Checks coagulation results before removal Checks with ICU team for any bloods to be taken before removal of line Demonstrates the removal of an PiCCO line as per units policy Documents removal of line correctly on CIS How long should a PiCCO line remain in? Questions to be asked by assessor Why do coags need to be checked prior to removal Shown Safe Competent Actions
How long do you need to apply pressure for at the insertion site post removal?
Element 7 Vasoactive / anti arrhythmic drug therapy Observable Criteria Questions to be asked by assessor Outline the properties of these drugs & the management of the infusions Why is it important to keep vasoactive drugs on the same lumen? Which lumen do the vasoactive drugs run on? What are the nursing responsibilities when running vasoactive drugs? Adrenaline Noradrenaline Dobutamine Vasopressin Levosimendin GTN Amioderone Why does Amiodarone have to go in a glass bottle after the initial loading dose? Shown Safe Competent Actions
- 22 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 8 Pulmonary Artery Catheters Observable Criteria Indications for PA Catheter Outline the need for PAC insertion Questions to be asked by assessor What are the indications for PA monitoring Shown Safe Competent Actions
Set up for PAC insertion Gathers equipment needed for line insertion Assists Dr with insertion What are the risks of PAC insertion? What is the importance of ECG monitoring during line insertion?
Nursing Responsibilities with PACs Outlines the need for measuring placement of catheter regularly Outlines the need to ensure balloon syringe is not depressed when not doing a measurement Outlines importance of continuous PA monitoring
Why is placement important?
What if balloon is inflated?
Why is it important to continuously visualize PA trace on monitor? What is the importance of recording the measurement regularly?
Performing a PCWP measurement Informs the patient about the procedure that is about to take place Demonstrates appropriate positioning of patient for acquiring a wedge pressure Demonstrates ability to correctly zero pulmonary artery catheter and record pressures in the CIS Demonstrates ability to perform a wedge safely for no longer than the maximum time limit.
Who routinely performs a PCWP measurement? Where does the balloon inflate when doing a measurement? What is the absolute time limit for balloon inflation? Why is it important not to leave the balloon wedged for too long? What is a major, serious side effect of over inflating or prolonged wedging of balloon? Why is this important?
Demonstrates the locking off of the wedging syringe and safe securing of same
- 23 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
COMPETENCY:- FLUIDS AND ELECTROLYTES
Aim of Competency Assessment of patients fluids and electrolytes Provide safe and affective care to patients receiving renal support such as dialysis
Elements of Competency 1. 2. 3. 4. 5. Fluids / Electrolytes / Pathology Results Peritoneal Dialysis CVVHDF EDD-f IDC
- 24 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 1 Fluids Observable Criteria Fluids Accurately documents fluid balance chart in CIS Outline the difference between a crystalloid and colloid. Questions to be asked by assessor What are the signs and symptoms of fluid overload? What are the signs and symptoms for dehydration? Shown Safe Competent Actions
What is the difference between a crystalloid and a colloid?
Blood products Demonstrate the correct procedure for administering blood products
Why is it important to warm pack cells when administering through a CVC? What other fluids can blood products run with on a single lumen?
Electrolytes Can locate pathology results on the CIS Can identify acceptable electrolyte levels What are the potential risks for a patient with an abnormal potassium level? How fast can potassium be given via a: Central line? Peripheral cannula?
Element 2 Peritoneal Dialysis Observable Criteria Outlines reasons for peritoneal dialysis Questions to be asked by assessor Why would a patient need to receive peritoneal dialysis? Shown Safe Competent Actions
PD set up Verifies order in Fluid Balance Chart Gathers equipment needed for procedure Warms PD fluid to appropriate temperature Why does PD fluid need to be warmed?
- 25 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 2 Peritoneal Dialysis Observable Criteria Managing PD Connects bag to patients catheter aseptically Drains dwelling fluid and records weight in fluid balance chart Runs PD fluid into abdominal cavity Once completed, attaches new cap to patients catheter aseptically Questions to be asked by assessor Why is asepsis important when the patient would normally do this procedure at home? Why is it important to accurately chart both the input and the output of peritoneal dialysis? How much fluid do you need to remove during PD? Shown Safe Competent Actions
Element 3 CVVHDF Observable Criteria Indications for CVVHDF Outlines the indications for CVVHDF Questions to be asked by assessor What does CVVHDF stand for? What is the difference between dialysis and filtration? Shown Safe Competent Actions
CVVHDF Set up Gathers machine and equipment needed to set up CVVHDF Checks electrolyte levels and fluid orders from team Demonstrates set up and priming of Prisma Prismaflex Why is it important to check the patients electrolyte levels? What is osmosis? What is the difference between pre and post filter?
Sets treatment parameters on machine Removes Heparin lock from Vas Cath If there are no labels on the lumen how do you know if the lumen has been heparin locked or not?
Connects patient and observes hemodynamic status once treatment is commenced
- 26 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc Element 3 CVVHDF Observable Criteria Running CVVHDF Can appropriately troubleshoot alarms Questions to be asked by assessor What actions would you take for the following alarms High access pressure? Monitors patients hemodynamic status during treatment Documents correct parameters in the CIS Access disconnection? Shown Safe Competent Actions
What parameters must be observed when starting treatment and why? Why is it important to chart pressure levels on the CIS when they have no bearing of the fluid status Why is this important When would you increase the amount of fluid to be removed from the prisma/prisma flex?
Ensures regular EUCs are taken during treatment Changes fluid removal appropriately to maintain desired balance
Ceasing treatment Returns blood back to patient once treatment ceased
Why is it necessary to return blood? When would it not be appropriate to return the blood? What parts of the circuit are disposable?
Disposes of circuit appropriately, cleans machine and returns machine to storage area
Vascath line care Demonstrates a Heparin lock of a Vascath
What is the concentration of Heparin used in a Heparin lock and how much do you inject to Heparin lock a Vas Cath? Why is it important to be able to se the line insertion site once the dressing is completed? How frequently should a line dressing be attended?
Outlines the dressing protocol for a Vascath
- 27 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 4 EDD-f Observable Criteria EDD-f Set up Outlines the indications for EDD-f Gathers machine and equipment needed to set up EDD-f Checks electrolyte levels and fluid orders from team What does EDD-f stand for? Explain equipment needed to perform EDD-f. Questions to be asked by assessor Shown Safe Competent Actions
Why is it important to check the potassium and sodium bicarbonate orders before set up of the machine? What needs to be checked on the machine before priming can take place? What is the difference between pre and post filter? What are the correct parameters?
Demonstrates set up and priming of Fresenius machine
Sets treatment parameters on machine: UF Menu Dialysate menu Removes Heparin lock from Vas Cath Connects patient and observes hemodynamic status once treatment is commenced
How do you remove a heparin lock from a vas cath What parameter must be observed when starting treatment and why? Why is it important to monitor the patients Appt during treatment?
Running EDD-f Can appropriately troubleshoot alarms What actions would you take for the following alarms: High access pressure? Monitors patients hemodynamic status during treatment Documents correct parameters in the CIS Access disconnection?
- 28 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 4 EDD-f Observable Criteria Ceasing treatment Returns blood back to patient once treatment ceased Ensures EUCs are taken after treatment Why is this necessary? When would it be inappropriate to return blood? Why should EUCs be attended post treatment? What is the concentration of Heparin used in a Heparin lock and how much do you inject to Heparin lock a Vas Cath? Questions to be asked by assessor Shown Safe Competent Actions
Heparin locks Vas Cath once treatment ends
Disposes of circuit appropriately, cleans machine and returns machine to storage area
Element 4 IDC Insertion Observable Criteria Insertion Outline the indications for IDC insertion Questions to be asked by assessor How much urine does the patient pass if they are: Anuric? Gathers equipment needed Polyuric? Oliguric? Shown Safe Competent Actions
How do you assess the catheter size for each person?
Inserts IDC as per policy for Male Female
Outlines the reasons and times for collecting a urine culture
Removal of IDC Demonstrates removal of IDC
If the patient has not passed urine after removal, how long do we wait before re insertion of IDC?
- 29 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
COMPETENCY:- GASTROINTESTINAL CARE
Aim of Competency Assessment of patients Gastrointestinal system Provide safe and affective care to patients receiving entral feeding
Elements of Competency 1. 2. 3. 4. Gastrointestinal Assessment Nasogastric Tube Insertion Entral Feeding Total Parental Nutrition (TPN)
- 30 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 1 GIT Assessment Observable Criteria Questions to be asked by assessor Shown Safe Competent Actions
Inspects & palpates the patients abdomen, observing for bruising or marks and any structural abnormalities Auscultates the patients abdomen. Checks for bowel sounds in all four quadrants Checks condition of stomas or colostomies Inspects patients abdomen X Ray, identifies any abnormalities. Documents all findings in CIS
What is the difference between guarding and rebound pain?
How long should you listen for bowel sounds until you can say they are absent? What should stomas look like?
Element 2 Nasogastric Tube Insertion Observable Criteria Nursing Responsibilities Aspirates regularly and records amount in Fluid Balance Chart Ensures patent airway opened if NG is on free drainage Records amount of drainage in Fluid Balance Chart and changes bag every 12 hours Ensures Low Wall outlet is set appropriately when NG is on Low Wall suction Records drainage amount in Fluid Balance Chart When does gastric drainage get charted when a patient is on low wall suction? Should there be an airway or a spigot in place when the NG is on low wall suction? Questions to be asked by assessor How often do we aspirate NG tubes? Do fine bore tubes get aspirated? How do you troubleshoot a blocked fine bore tube? What type of medications can not be given via an NG tube? Do you aspirate an NG tube that is on low wall suction? Shown Safe Competent Actions
- 31 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 2 Nasogastric Tube Insertion Observable Criteria Indications for insertion Outline the reasons for NG tube insertion Questions to be asked by assessor What is the difference between a Salem sump and fine bore? Shown Safe Competent Actions
Insertion Gathers equipment for insertion Explains procedure to patient Measure correct insertion length for patient Inserts NG tube
What equipment is required for NG insertion?
How do you measure correct length of the NG? How do you tell if the NG has gone in the right place? What are the complications of insertion? Why is a post insertion X-ray important?
Organises CXR post insertion to confirm placement
Element 3 Enteral Feeding Observable Criteria Indications for enteral feeding Outlines the indications of enteral feeding Questions to be asked by assessor Shown Safe Competent Actions
What is the importance of starting NG feeds early in a patients ICU stay?
Set up of Feeds Gathers equipment Confirms correct feed formula with doctors Aspirates NG prior to NG Feeds commencing
Why should you aspirate the NG prior to commencing feeds?
Begins feeds at a rate of 30ml/hr
- 32 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 3 Enteral Feeding Observable Criteria Running NG Feeds Aspirates NG after 4 hours Turns rate up by 30ml/hr every 4 hours until goal rate is reached Aspirate every 4 hours and document amount aspirated in Fluid Balance Chart Questions to be asked by assessor Shown Safe Competent Actions
What is the amount of aspirate required to stop NG Feeds? Why is it important to slowly turn up NG feeds slowly rather than going straight to goal rate?
Ceasing NG Feeds Outlines the reasons for ceasing NG Feeds Checks with team when ceasing NG Feeds
Why is it important to check BSL and actrapid levels on completion of NG feeds? How long before extubation should NG Feeds be ceased?
Element 4 Total Parental Nutrition (TPN) Observable Criteria Set up of TPN lines Gathers equipment needed to commence TPN Follows unit protocol for TPN set up and connection including aseptic technique Documents appropriate rates in Fluid Balance Chart Why is aseptic technique required during set up of TPN? Why is it important that NO drugs or fluids are to be given via the TPN line? What is the only infusion that can run with TPN? Questions to be asked by assessor Shown Safe Competent Actions
- 33 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
COMPETENCY:- NEUROLOGICAL CARE
Aim of Competency Assessment of patients Neurological system Provide safe and affective care to patients with altered Neuro status
Elements of Competency 1. Neurological Assessment 2. Chemical / Physical Restraints
- 34 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 1 Neurological Assessment Observable Criteria Questions to be asked by assessor Shown Safe Competent Actions
Accurately performs assessment of conscious level using the GCS
What are the three aspects assessed when using the GCS? What is the lowest score you can get on a GCS?
Documents appropriately in CIS Demonstrates best method of applying a central painful stimulus Demonstrates accurate assessment of pupilary function Performs assessment of limb movements Why is it important to make commands achievable for your patient, i.e. poking your tongue out rather than raising your arms and legs? When assessing a motor response, why is it important to request that your patient both squeeze and release your fingers? Why is assessing central painful stimuli preferable over assessing peripheral painful stimuli?
Element 2 Chemical / Physical restraints Observable Criteria Sedation Can appropriately document sedation scale in CIS Questions to be asked by assessor How often should a sedation scale be done on patients with sedation running? Shown Safe Competent Actions
Restraints Charts restraints appropriately in the CIS
Why is it important to chart both the GCS and sedation scale when restraints are applied? What physiological/environmental/ psychological factors can contribute to the need for restraints?
Removes restraints when not necessary Adheres to hourly limb observations when patient restrained
Why do limb obs need to be charted when a patient is restrained? Why is it important not to tie restraints to the top of the bed rail?
- 35 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 2 Chemical / Physical restraints Observable Criteria AWS Chart AWS accurately in CIS and notifies health care team accordingly Questions to be asked by assessor Why is it important to get the patient to stretch their fingers wide apart when checking for a tremor as a part of the AWS? Shown Safe Competent Actions
- 36 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
COMPETENCY:- SKIN AND WOUND CARE
Aim of Competency Assessment of patients dressings, lines, drains and pressure areas Provide safe and aseptic wound dressing changes
Elements of Competency 1. Dressings 2. Drains
- 37 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 1 Dressings Observable Criteria Basic Dressing Demonstrate the dressing of a basic dressing Questions to be asked by assessor Shown Safe Competent Actions
Should Chlorhexadine or sterile water be used for a basic dressing? What is the rationale for one clean and one dirty forceps during a basic dressing?
CVC / Vascath / Arterial line Demonstrate a line dressing as per units protocol Explain the units protocol on frequency of line dressings
Why is it important to be able to se the line insertion site once the dressing is completed? How frequently should a line dressing be attended?
Element 2 - Drains Observable Criteria Bellovac Drain Ensure patency of Bellovac Drain Document relevant information in Fluid Balance Chart When should the bellovac drain bag be marked for drainage? Why is it important to clamp the drainage line before emptying the concertina section of the bellovac drain? Questions to be asked by assessor Shown Safe Competent Actions
Demonstrate dressing of Bellovac Drain
- 38 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 1 Pressure Area Care Observable Criteria Turns How often do we do pressure area care on a: Ventilated patient Bed bound patient Ambulatory patient Questions to be asked by assessor Shown Safe Competent Actions
Why is documentation of turns important? What should you do if your patient refuses a turn?
Dressings Demonstrate the appropriate dressing of a pressure area
Why is PAC documentation so important with regard to pressure sores? Should water filled gloves be used to disperse pressure from the heel profligately?
Air Mattress Set up of Air Mattress
When would you consider the use of an air mattress for a patient?
Proning Explain the reasoning behind proning Demonstrates the preparation of a patient prior to proning.
How can proning improve a patients lung function? How many staff are required to safely turn a patient to the prone position? What preparations are needed to ensure a smooth turn to the prone position?
Explains to the patient if appropriate what is going to happen Demonstrates the safe turning of a patient to the prone position Ensures appropriate sedation is ordered for the patient post turning. Monitors Hemodynamics and ventilation parameters post turning. Documents turn and appropriate PAC in CIS. How do you monitor a patient in the prone position? What Hemodynamic and ventilator changes may be seen when turning a patient prone? What are some of the PAC and general body concerns when turning a patient prone?
- 39 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
COMPETENCY:- WARD ROUTINES
Aim of Competency Admit a patient into the CIS and provide base line admission information Discharge a patient to the ward/other hospital with appropriate documentation
Elements of Competency 1. Admission 2. Discharge
- 40 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 1 Admission Observable Criteria Ensure all necessary equipment needed to set up bed area Enters patients name and MRN into CIS and monitor Ensures patient label is put into red admission book and patients name is on the whiteboard Attaches leads to patient for monitoring Ensure patient identification band and allergy band are insitu Even though ICU nursing is usually one to one, why is it important to ensure patient ID band and allergy band is on patient? What initial tests/ procedures are carried out on all patients at admission? Questions to be asked by assessor What equipment is essential at all bed areas prior to patient admission? How many digits are required in the MRN to be added to the CIS correctly? Shown Safe Competent Actions
Ensures admission tests are carried out: 12 Lead ECG CXR
- 41 -
S:\ICCMU\iccmu_website\iccmu2\five\doc\education_packages\blacktown\blacktown_clinical_competencies.doc
Element 2 - Discharge Observable Criteria Checks with TL regarding the discharge ward and time the bed is available Ensures discharge checklist is completed What is the importance of a properly filled out discharge checklist? Why should the arterial line be removed before discharge? Why is it important to have a patient ID band on the patient prior to discharge? Why is it important to put an entry in the patients notes prior to discharge? Questions to be asked by assessor Shown Safe Competent Actions
Removes arterial line as per protocol
Collects patients belongings and completes the internal transfer checklist Ensures patients notes are up to date and prints out computer notes Organises patients notes for transfer including written medication chart and fluid order chart Make up infusions with ward giving set Ring receiving ward to inform of any required equipment (pumps, suction set up) Page wards man Remove patient from monitor and transfer to ward Ensure patient is discharged from CIS and Marquette monitor
Why should the receiving ward be rung before transfer?
Why is it important to remove the patient from the CIS on discharge
- 42 -
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Equine Dorsoscapular LigamentDokument7 SeitenEquine Dorsoscapular Ligamentcharlie100% (1)
- Castration of Large AnimalsDokument17 SeitenCastration of Large AnimalsAqsa Zahoor Ahmad NadeemNoch keine Bewertungen
- ENT Batch 2022 Annual Paper-1Dokument9 SeitenENT Batch 2022 Annual Paper-1mudassirahmedNoch keine Bewertungen
- EndocarditisDokument27 SeitenEndocarditisruchikakaushal1910Noch keine Bewertungen
- Tehnik Dasar Laparoskopik - Pneumoperatonium-Veress NeedleDokument31 SeitenTehnik Dasar Laparoskopik - Pneumoperatonium-Veress NeedleDaniel LesmanaNoch keine Bewertungen
- (2014) Capnography During Cardiopulmonary Resuscitation - Current Evidence and Future DirectionsDokument10 Seiten(2014) Capnography During Cardiopulmonary Resuscitation - Current Evidence and Future DirectionsDominik Chirito PastorNoch keine Bewertungen
- Anesthesia Anesthetic DrugsDokument6 SeitenAnesthesia Anesthetic DrugsYesi SaputriNoch keine Bewertungen
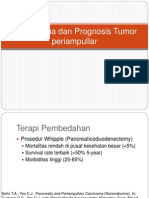
- Tatalaksana Dan Prognosis Tumor PeriampullarDokument16 SeitenTatalaksana Dan Prognosis Tumor PeriampullarVerico PratamaNoch keine Bewertungen
- Nejm How To PericardiocentesisDokument5 SeitenNejm How To Pericardiocentesispkapur8552Noch keine Bewertungen
- WW.11.01G-Surgical Count Policy (9179)Dokument5 SeitenWW.11.01G-Surgical Count Policy (9179)EyySiEffVeeNoch keine Bewertungen
- Code Blue PresentationDokument22 SeitenCode Blue PresentationNurhayatiNoch keine Bewertungen
- CBCT Patterns of Bone Loss and Clinical Predictors For The Diagnosis of Cracked Teeth and Teeth With Vertical Root FractureDokument7 SeitenCBCT Patterns of Bone Loss and Clinical Predictors For The Diagnosis of Cracked Teeth and Teeth With Vertical Root FractureAssem HNoch keine Bewertungen
- Tog 12685Dokument3 SeitenTog 12685saeed hasan saeedNoch keine Bewertungen
- Driving Pressure Study OLVDokument13 SeitenDriving Pressure Study OLVlucasNoch keine Bewertungen
- Drug Eluting StentDokument14 SeitenDrug Eluting StentUday KiranNoch keine Bewertungen
- Contemporary Diagnosis and Management of Patients With MINOCADokument10 SeitenContemporary Diagnosis and Management of Patients With MINOCAAlirio Angulo QuinteroNoch keine Bewertungen
- Normal & Abnormal Uterine ActionDokument39 SeitenNormal & Abnormal Uterine ActionAy Alex100% (2)
- 11.sudden Natural Death 3Dokument55 Seiten11.sudden Natural Death 3Hasabo AwadNoch keine Bewertungen
- Choque HemorragicoDokument9 SeitenChoque HemorragicoAna NevesNoch keine Bewertungen
- Chapter 102: Laryngeal Trauma From Intubation: Endoscopic Evaluation and Classification Bruce BenjaminDokument16 SeitenChapter 102: Laryngeal Trauma From Intubation: Endoscopic Evaluation and Classification Bruce BenjaminPrisia AnantamaNoch keine Bewertungen
- 1) BiopsyDokument30 Seiten1) BiopsySosa GeorgeNoch keine Bewertungen
- Instructions: Operation ManualDokument104 SeitenInstructions: Operation ManualLatif Fathul EvendiNoch keine Bewertungen
- Maret 2018 26-50Dokument10 SeitenMaret 2018 26-50daniel_alexander_susenoNoch keine Bewertungen
- Goniometric Reliability of Shoulder MeasurementsDokument6 SeitenGoniometric Reliability of Shoulder MeasurementssaswepakNoch keine Bewertungen
- Inguinal HernioplastyDokument10 SeitenInguinal HernioplastyfiansisNoch keine Bewertungen
- Surgical Nursing (III)Dokument32 SeitenSurgical Nursing (III)Opio MosesNoch keine Bewertungen
- Osteoarthritis 191016103144Dokument49 SeitenOsteoarthritis 191016103144dr.abouzaid098Noch keine Bewertungen
- MTP Single-Use Products: 2nd EDITION 2/2019Dokument244 SeitenMTP Single-Use Products: 2nd EDITION 2/2019Derkis MarcanoNoch keine Bewertungen
- 1 s2.0 S0378603X16301486 Main PDFDokument4 Seiten1 s2.0 S0378603X16301486 Main PDFexaNoch keine Bewertungen
- Pulseless Pumps & Artificial HeartsDokument23 SeitenPulseless Pumps & Artificial HeartscafemedNoch keine Bewertungen