Beruflich Dokumente
Kultur Dokumente
Nephrotic Syndrome
Hochgeladen von
Sonny WijanarkoCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nephrotic Syndrome
Hochgeladen von
Sonny WijanarkoCopyright:
Verfügbare Formate
NEPHROTIC SYNDROME Definition: Nephrotic syndrome is defined by the associ-ation of a proteinuria higher than 3.
5 g/24 hours, hypoalbuminaemia, oedema and dyslipidaemia.Remission: Up/c <0.2 or Albustix-negative or trace for3 days. Relapse: After remission, an increase in the first morning Up/c to >=2orAl-bustix reading of>=2 for 3 of 5 consecutive days. Frequently relapsing: 2 or more re-lapses within 6 months after initial therapy or >=4 relapses in any 12month period. Steroid dependent: Relapse during taper or within 2 weeks of discontinu-ation of steroid therapy. Steroid resistant: Inability to induce a remission with 4weeks of daily steroid therapy. Classification
Histologic classification of Nephrotic syndrome: 1. 2. 3. 4. minimal change (MCNS) (77.1%), focal segmental glomerulosclerosis (FSGS) (7.9%), membranoproliferative glomerulonephritis (6.2%), others (8.8%) Atypical Features <1yr, >10years Hypertensive Elevated Creatinine Macroscopic Haematuria
Typical Features Age 1-10 years Normotensive Normal Adrenal Function +/- microscopic haematuria
Pathophysiology Classic hypothesis/Underfill hypothesis: classic hypothesis, also called the underfill hypothesis, postulates that sodium retention in NS is secondary to decreased effective arterial blood volume, hence the term underfill. The hypothesis suggests the following sequence of events: urinary loss of proteins in NS, especially albumin, causing hypoalbuminaemia, which in turn causes a decrease in plasma oncotic pressure.
This decrease in plasma oncotic pressure would then cause an imbalance in Starling forces, movement of fluid from the intravascular space to the interstitial space, causing a decrease in effective arterial blood volume and consequently, relative hypovolaemia. This would then result in activation of the renin-angiotensin-aldosterone and sympathetic nervous systems, increased antidiuretic hormone release and inhibition of atrial natriuretic peptide release. Activation of these systems would cause sodium and water retention in the kidneys, with subsequent oedema. However, several experimental and clinical observations made over the years do not support this hypothesis. Nephrotic syndrome -> Albuminuria ->Hypoalbuminaemia ->Reduction in plasma oncotic pressure -> Translocation of fluid from the intravascular space to the interstitial space -> Decrease in effective arterial blood volume Classic or underfill hypothesis of oedema formation in nephrotic syndrome Albuminuria
Hypoalbuminaemia
Reduction in plasma oncotic pressure Translocation of fluid from the intravascular space to the interstitial space
Decrease in effective arterial blood volume
Renin-angiotensin-aldosterone system Sympathetic nervous system Arginine-vasopressin Atrial natriuretic peptide Sodium and water retention by the kidney Oedema
Arguments against the underfill hypothesis of oedema formation in nephrotic syndrome: 1. Patients and laboratory rats with low serum albumin levels do not develop oedema or sodium retention. 2. Natriuresis in the recovery phase of nephrotic syndrome begins when proteinuria disappears but before serum albumin returns to normal levels. 3. The absolute decrease in plasma oncotic pressure does not affect the volume of the intravascular space in nephritic syndrome. 4. Plasma and blood volumes are normal or increased in nephrotic syndrome. 5. Intravascular space expansion with albumin does not increase natriuresis in patients with nephrotic syndrome. 6. The activation of the renin-angiotensin-aldosterone system is not involved in the development of oedema in nephritic syndrome. 7. Bilateral adrenalectomy does not prevent sodium retention in nephrotic syndrome in laboratory rats.
Causes
Nephrotic syndrome may result from either primary glomerular or systemic disease leading to renal insult. Primary glomerular diseases associated with nephrotic syndrome: 1. 2. 3. 4. 5. 6. 7. 8. 9. Primary glomerular diseases (frequent; rare) Membranous glomerulopathy Focal and segmental glomerulosclerosis Minimal change disease (MCD) glomerulopathy IgA nephropathy Membranopoliferative glomerulonephritis C1q glomerulopathy Fibrillar glomerulopathy Congenital podocyte anomaly
Causes of secondary Nephrotic syndrome (most frequent). 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. Medications (non exhaustive) Allergens, immunisations NSAIDs, pamidronate, rifampicin, IFN alpha, gold, lithium, Pollens, seric illness, vaccines, bee stin interferon alpha Infections Systemic illnesses (most frequent) Bacterial: Endocarditis, syphilis, tuberculosis, mycoplasma infections Systemic lupus erythematosus (SLE), Viral: HIV, HBV, HCV, EBV, CMV,VZV Rheumatoid polyarthritis, Protozoal:Toxoplasmosis, malaria Schonlein-Henoch purpura Helminthic: Schisostomiasis, trypanosomiasis, filariasis MGUS, amyloidosis Neoplasia Metabolic diseases and heredofamilia Solid tumours Type I and II diabetes Haemo- or lymphopathies Hypothyroidism Multiple myeloma Alport syndrome GVHD post marrow transplantation Graves disease Fabry disease Miscellanous (examples) Pregnancy-associated Chronic allograft failure Nephronic reduction Renal artery stenosis Obesity Heart failure (right/left) and pericarditis
Clinical Presentation History The first sign of nephrotic syndrome in children is usually swelling of the face; this is followed by swelling of the entire body. Adults can present with dependent edema. Foamy urine may be a presenting feature. A thrombotic complication, such as deep venous thrombosis of the calf veins or even a pulmonary embolus, may be the first clue indicating nephrotic syndrome. Additional historical features can be related to the cause of nephrotic syndrome. Thus, the recent start of a nonsteroidal anti-inflammatory drug (NSAID) or a 10-year history of diabetes may be very relevant. Physical Examination Edema is the predominant feature of nephrotic syndrome and initially develops around the eyes and legs. With time, the edema becomes generalized and may be associated with an increase in weight, the development of ascites, or pleural effusions.
Hematuria and hypertension manifest in a minority of patients. Additional features on exam will vary according to cause and as a result of whether or not renal function impairment exists. Thus, in the case of longstanding diabetes, there may be diabetic retinopathy, which correlates closely with diabetic nephropathy. If the kidney function is reduced, there may be hypertension and/or anemia.
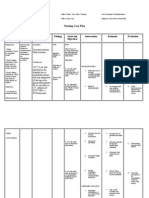
Diagnosis and Lab Recommendations for initial evaluation include: urinalysis; first morning Up/c; serum electrolytes, serum urea ni-trogen, creatinine, and glucose; cholesterol level; serum albumin level; complement 3 level; antinuclear antibody level (for children aged >=10 years or with any other signs of systemic lupus erythematosus);
hepatitis B, hepatitis C, and HIV se-rology in high-risk populations; purified protein derivative level; and kidney biopsy for children aged >=12 years Treatment On the basis of the ISKDC study, 95% of children with steroid-responsive nephrotic syndrome will demonstrate resolution of proteinuria with 4 weeks of daily glucocorticoid therapy and 100% after an additional 3 weeks of alternate-day therapy. This consensus guideline uses a 4-week oral glucocorticoid limit to define ste-roid resistance; however, therapy may be continued during the subsequent evaluation for steroid-resistant ne-phrotic syndrome, allowing the capture of late responders. Initial Therapy for Childhood Nephrotic Syndrome prednisone 2 mg/kg per day for 6 weeks (maximum: 60 mg); thenprednisone1.5mg/kg on alternate days for 6weeks (maximum: 40mg); no steroid taper is required at the conclusion of this initial therapy.
Initial or Infrequent-Relapse Therapy prednisone 2 mg/kg per day until urine protein test results are nega-tive or trace for 3 consecutive days; then prednisone 1.5 mg/kg on alter-nate days for 4 weeks Frequently Relapsing Nephrotic Syndrome Therapy Options prednisone 2 mg/kg per day until proteinuria normalizes for 3 days, 1.5 mg/kg on alternate days for 4 weeks, and then taper over 2 months by 0.5 mg/kg on alternate days (total: 34 months); oral cyclophosphamide 2mg/kg per day for 12 weeks (cumulative dose: 168 mg/kg) based on ideal body weight started during prednisone (2 mg/kg per day) induced remis-sion, decrease prednisone dose to 1.5 mg/kg on alternate days for 4 weeks, and then taper over 4weeks; mycophenolate mofetil 25 to 36 mg/kg per day (maximum: 2 g/day) divided twice daily (BID) for 1 to 2 years with a taperingdoseof prednisone; and cyclosporineA3to5mg/kg per day di-videdBID for anaverageof 2 to5 years.
Steroid-Dependent NephroticSyndrome Therapy glucocorticoidsarepreferred in theab-senceof significant steroid toxicity; secondary alternatives should be cho-senon thebasis of risk/benefit ratio; cyclosporineA3to5mg/kg per daydivided BID; tacrolimus 0.05 to 0.1mg/kg per daydivided BID; and mycophenolate mofetil 24 to 36 mg/kg per day or 1200 mg/m2 per day divided BID (maximum: 2 g/day)
Steroid-Resistant Nephrotic Syndrome Management kidney biopsy; tailor therapeutic regimen accord-ing to kidney histology; and provide optimal supportive therapy
ACE-I and ARB Therapy ACE-I or ARB therapy is recom-mended for steroid-resistant ne-phrotic syndrome; consider use of ACE-Is or ARBs with steroid-dependent or frequently re-lapsing nephrotic syndrome; counsel regarding contraindications of ACE-I or ARB therapy duringpregnancy
Edema Management counsel caregivers regarding po-tential complications of edema; and consider treatment with low-sodium diet, modest fluid restriction, diuretics, andalbumin infusions.
Hypertension Management control blood pressure to <90th percentile of normal
recommend low-salt diet, exercise, and weight reduction if obesity is present; and ACE-Is and/or ARBs for chronic pharmacologic management
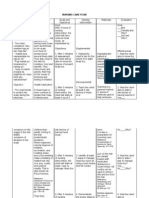
Complications The complications of childhood ne-phrotic syndrome are associated with disease activity and therapy. Active ne-phrotic syndrome increases the risk for therapy-associated growth compli-cations, dyslipidemia, infections, and thromboembolism. Obesity and Growth monitor BMI and linear growth; provide counseling on weight con-trol; and consider glucocorticoid alterna-tives when short stature or obesity is present.
Dyslipidemia low-fat diet; consider low-density lipoprotein cholesterol-lowering drug therapy when fasting low-density lipoprotein cholesterol levels are persistently 160 to 190 mg/dL; and counsel regarding contraindica-tions of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors during pregnancy
Infection counsel regarding signs and symp-toms of infections such as cellulitis, peritonitis, and bacteremia; and provide empiric therapy for peritonitis until culture results areavailable
Thromboembolism evaluate children with a thromboembolism for an underlying hypercoagulopathy; and
provide anticoagulation therapy forchildren with nephrotic syndrome and thromboembolism
Vaccinations immunize with the 23-valent and heptavalent conjugated pneumo-coccal vaccines; immunize the immunosuppressed or actively nephrotic patient and household contacts with inactivated influenza vaccine yearly; defer immunization with live vaccines: until prednisone dose is2 mg/kg per day (maximum: 20mg); for 3 months from completion of therapy with cytotoxic agents; or for 1 month from completion of other daily immunosuppression; provide varicella immunization if nonimmune, on the basis of immu-nization history, disease history, or serologic evaluation; provide postexposure immunoglob-ulin for nonimmune immunocom-promised patients; and consider intravenous acyclovir for immunosuppressed children at the onset of chicken pox lesions.
Das könnte Ihnen auch gefallen
- By DR - Tosif Ahmad TMO-PediatricsDokument27 SeitenBy DR - Tosif Ahmad TMO-PediatricskamalNoch keine Bewertungen
- Acute Glomerulonephritis in ChildrenDokument6 SeitenAcute Glomerulonephritis in ChildrenAnsu MaliyakalNoch keine Bewertungen
- AGE Case StudyDokument71 SeitenAGE Case StudyJm BernardoNoch keine Bewertungen
- Nephrotic SyndromeDokument36 SeitenNephrotic SyndromedrtpkNoch keine Bewertungen
- NCP Poststreptococcal GlomerulonephritisDokument12 SeitenNCP Poststreptococcal GlomerulonephritisScarlet ScarletNoch keine Bewertungen
- Acute GlomerulonephritisDokument12 SeitenAcute Glomerulonephritiskuchaibaru90Noch keine Bewertungen
- Typhoid FeverDokument23 SeitenTyphoid FeverAs ShahirahNoch keine Bewertungen
- Lupus Case ReportDokument1 SeiteLupus Case ReportMendy HararyNoch keine Bewertungen
- COPD and Pneumonia Nursing CareDokument13 SeitenCOPD and Pneumonia Nursing CareÍam KristineNoch keine Bewertungen
- Pathophysiology of ESRD: Organ Dysfunctions & Associated AbnormalitiesDokument5 SeitenPathophysiology of ESRD: Organ Dysfunctions & Associated AbnormalitiesCarl JardelezaNoch keine Bewertungen
- Dengue: Dengue Hemorrhagic Fever, Resulting in Bleeding, Low Levels of Blood Platelets andDokument5 SeitenDengue: Dengue Hemorrhagic Fever, Resulting in Bleeding, Low Levels of Blood Platelets andFrance John Evangelista TorresNoch keine Bewertungen
- IVIgDokument2 SeitenIVIgernestjohnNoch keine Bewertungen
- Manage Fluid Volume Excess in Renal FailureDokument3 SeitenManage Fluid Volume Excess in Renal FailureMichael Baylon DueñasNoch keine Bewertungen
- Febrile SeizureDokument6 SeitenFebrile SeizurepipimseptianaNoch keine Bewertungen
- Case StudyDokument41 SeitenCase StudyAubrey Ann FolloscoNoch keine Bewertungen
- Glomerulonephritis vs GlomerulopathiesDokument58 SeitenGlomerulonephritis vs GlomerulopathiesRahmailla Khanza Diana FebriliantriNoch keine Bewertungen
- Measles (Rubeola) VirusDokument16 SeitenMeasles (Rubeola) Virusstudymedic100% (1)
- Discharge PlanDokument1 SeiteDischarge PlanKamille Bianca Macapagal ÜNoch keine Bewertungen
- Aspiration Pneumonia Diagnosis and TreatmentDokument27 SeitenAspiration Pneumonia Diagnosis and TreatmentReya Awali SuasoNoch keine Bewertungen
- Predisposing Conditions, Management and Prevention of Chronic Kidney DiseaseDokument52 SeitenPredisposing Conditions, Management and Prevention of Chronic Kidney DiseaseSaad MotawéaNoch keine Bewertungen
- PTB Case-StudyDokument64 SeitenPTB Case-StudyBeverly DatuNoch keine Bewertungen
- Itp 210530123628Dokument26 SeitenItp 210530123628Sakthi DeviNoch keine Bewertungen
- Case StudyDokument18 SeitenCase StudyJonathan Delos ReyesNoch keine Bewertungen
- Case Study 102Dokument6 SeitenCase Study 102Cheska Lopez100% (1)
- COPD Therapeutics CaseDokument34 SeitenCOPD Therapeutics CaseCindy NoufalNoch keine Bewertungen
- Nursing Care Plan For Type1 DiabetesDokument1 SeiteNursing Care Plan For Type1 DiabetesBushra AlkhdourNoch keine Bewertungen
- Liver CirrhosisDokument30 SeitenLiver CirrhosisMelody PardilloNoch keine Bewertungen
- Case AnalysisDokument12 SeitenCase AnalysisFroilan TaracatacNoch keine Bewertungen
- Case Scenario Dengue FeverDokument2 SeitenCase Scenario Dengue FeverJaslir MendozaNoch keine Bewertungen
- A Case Study On PuemoniaDokument32 SeitenA Case Study On Puemoniaxyzert100% (1)
- Community-Acquired Pneumonia GuideDokument37 SeitenCommunity-Acquired Pneumonia GuideKristine-Joy Legaspi FrancoNoch keine Bewertungen
- Compilation Drugstudy, NCP Cva (1) - BadetDokument14 SeitenCompilation Drugstudy, NCP Cva (1) - BadetLizette Villanueva-UntalanNoch keine Bewertungen
- ST - Lukes Casepress.Dokument31 SeitenST - Lukes Casepress.Justin EduardoNoch keine Bewertungen
- Poststreptococcal Glomerulonephritis - UpToDateDokument21 SeitenPoststreptococcal Glomerulonephritis - UpToDateHandre Putra100% (1)
- Hepatic EncephalopathyDokument3 SeitenHepatic EncephalopathyAnonymous GIGXKjfLNoch keine Bewertungen
- HemorrhoidsDokument15 SeitenHemorrhoidspologroNoch keine Bewertungen
- Acute BronchitisDokument25 SeitenAcute BronchitisCherish Panopio RoadillaNoch keine Bewertungen
- Nursing AssessmentDokument3 SeitenNursing AssessmentJanine PelayoNoch keine Bewertungen
- NCP AgnDokument2 SeitenNCP AgnMichael Vincent DuroNoch keine Bewertungen
- NCP-Case Presentation (CHF)Dokument4 SeitenNCP-Case Presentation (CHF)Jessamine EnriquezNoch keine Bewertungen
- Case+Study AGN MINEDokument66 SeitenCase+Study AGN MINEJm BernardoNoch keine Bewertungen
- Biliary AtresiaDokument25 SeitenBiliary Atresiajulius billiNoch keine Bewertungen
- Rabies: Ragina AguilaDokument55 SeitenRabies: Ragina AguilaCharles Lester AdalimNoch keine Bewertungen
- USC Case 04 - SinusitisDokument9 SeitenUSC Case 04 - SinusitisDisti Damelia SebayangNoch keine Bewertungen
- Acute Gastroenteritis Case StudyDokument6 SeitenAcute Gastroenteritis Case StudyKiyla920% (1)
- San Luis, Trio - ActivityDokument4 SeitenSan Luis, Trio - ActivityTrio San Luis100% (1)
- NTB Control Program ObjectivesDokument46 SeitenNTB Control Program ObjectivesJai AdoraNoch keine Bewertungen
- Biliary AtresiaDokument8 SeitenBiliary AtresiaBrooke MauriNoch keine Bewertungen
- Case AGNDokument66 SeitenCase AGNMohaima PanditaNoch keine Bewertungen
- Dyspepsia (Gastritis) Case StudiesDokument9 SeitenDyspepsia (Gastritis) Case StudiesJessica Nurin Graman100% (1)
- GlomerulonephritisDokument35 SeitenGlomerulonephritisapi-19916399Noch keine Bewertungen
- Case Study For Chronic Renal FailureDokument6 SeitenCase Study For Chronic Renal FailureGabbii CincoNoch keine Bewertungen
- Chapter 1 Fundamental Concepts SPSS - Descriptive StatisticsDokument4 SeitenChapter 1 Fundamental Concepts SPSS - Descriptive StatisticsAvinash AmbatiNoch keine Bewertungen
- Acute Cholecystitis SeminarDokument42 SeitenAcute Cholecystitis SeminarNatnaelNoch keine Bewertungen
- Overview of Nephrotic SyndromeDokument19 SeitenOverview of Nephrotic Syndromefarmasi_hm100% (1)
- Nephroticsyndrome 171015133308Dokument52 SeitenNephroticsyndrome 171015133308shravaniNoch keine Bewertungen
- Nephrotic Syndrome 5th Year Lecture 2011Dokument7 SeitenNephrotic Syndrome 5th Year Lecture 2011Gutierrez MarinellNoch keine Bewertungen
- Nephrotic Syndrome in ChildrenDokument36 SeitenNephrotic Syndrome in ChildrenMalueth AnguiNoch keine Bewertungen
- Nephrotic Syndrome PDFDokument36 SeitenNephrotic Syndrome PDFanwar jabariNoch keine Bewertungen
- 11 Exercises For MyopiaDokument4 Seiten11 Exercises For MyopiaarifiqNoch keine Bewertungen
- ScoliosisDokument7 SeitenScoliosisAbdur Rasyid50% (2)
- LaryngoceleDokument7 SeitenLaryngoceleM Grecu CeptureanuNoch keine Bewertungen
- Dissociative Identity DisorderDokument6 SeitenDissociative Identity DisorderElean Dash Mae Abatol0% (2)
- PediculosisDokument3 SeitenPediculosisDarkCeades50% (4)
- Rationale: Most Patients Prescribed To Receive Platelet Transfusions Exhibit Moderate ToDokument2 SeitenRationale: Most Patients Prescribed To Receive Platelet Transfusions Exhibit Moderate TojoanneNoch keine Bewertungen
- Invasive SpeciesDokument1 SeiteInvasive SpeciesHelly SoteloNoch keine Bewertungen
- Ventilator PortableDokument1 SeiteVentilator PortableAamer MumtazNoch keine Bewertungen
- Edwards Syndrome NotesDokument2 SeitenEdwards Syndrome Notesapi-386407615Noch keine Bewertungen
- Concurrent Validity of Two Observer-Rated Alexithymia MeasuresDokument6 SeitenConcurrent Validity of Two Observer-Rated Alexithymia MeasuresLolo LoloNoch keine Bewertungen
- Ambu BagDokument29 SeitenAmbu BagJessa Borre100% (2)
- Prof Qaisar Khan TrialsDokument56 SeitenProf Qaisar Khan TrialsAsim NajamNoch keine Bewertungen
- Hair-Grooming Syncope SeizuresDokument5 SeitenHair-Grooming Syncope Seizurestototm4480Noch keine Bewertungen
- Surgery CssDokument13 SeitenSurgery CssNaren ShanNoch keine Bewertungen
- EndokrinoDokument78 SeitenEndokrinoJulian TaneNoch keine Bewertungen
- Complaints Data Collection LetterDokument4 SeitenComplaints Data Collection LetterthrinathNoch keine Bewertungen
- Drug StudyDokument9 SeitenDrug StudyStephanie ValerioNoch keine Bewertungen
- Topographical Relationship of The Greater Palatine Artery and The Palatal Spine. Significance For Periodontal SurgeryDokument13 SeitenTopographical Relationship of The Greater Palatine Artery and The Palatal Spine. Significance For Periodontal SurgerycristianNoch keine Bewertungen
- ICU LogbookDokument37 SeitenICU Logbookrinus5100% (1)
- Course Syllabus (Sample)Dokument11 SeitenCourse Syllabus (Sample)Gelaie Salangsang100% (3)
- Coxa PlanaDokument8 SeitenCoxa PlanaLorebell100% (2)
- Principles of Pharmacokinetics and PharmacodynamicsDokument136 SeitenPrinciples of Pharmacokinetics and PharmacodynamicsDidiNoch keine Bewertungen
- Rift Valley FeverDokument9 SeitenRift Valley Feverapi-390015550Noch keine Bewertungen
- A Case of Sarcoidosis Cured With HomoeopathyDokument3 SeitenA Case of Sarcoidosis Cured With HomoeopathyDr. Rajneesh Kumar Sharma MD HomNoch keine Bewertungen
- Divine Healing Codes and How To Use Them - HTMLDokument68 SeitenDivine Healing Codes and How To Use Them - HTMLs.rajasekar100% (6)
- Orthodontics in 3 Millennia.Dokument7 SeitenOrthodontics in 3 Millennia.ningNoch keine Bewertungen
- Full Project of Shruthi RaiDokument60 SeitenFull Project of Shruthi RaiDeepak Rao RaoNoch keine Bewertungen
- Case Osteoarthritis NewDokument33 SeitenCase Osteoarthritis NewQueenie P. Manalo67% (3)
- PPE-Lecture-13-Documentation Pharmacy Services-2021Dokument15 SeitenPPE-Lecture-13-Documentation Pharmacy Services-2021LaylaNoch keine Bewertungen
- Pediatric Fluid and Electrolyte AlterationsDokument51 SeitenPediatric Fluid and Electrolyte AlterationsMatthew Ryan100% (1)