Beruflich Dokumente
Kultur Dokumente
Prostho IV - Lec 3 - Review of The Relevant Anatomy For Maxillary and Mandibular Dentures
Hochgeladen von
براءة أحمد السلاماتOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Prostho IV - Lec 3 - Review of The Relevant Anatomy For Maxillary and Mandibular Dentures
Hochgeladen von
براءة أحمد السلاماتCopyright:
Verfügbare Formate
3
Review of the relevant anatomy for maxillary and mandibular dentures
Razan Tanous
Khalid Al-Hamad
6-10-2013
Review of the relevant anatomy for maxillary and mandibular dentures
Mucosa: stratified squamus epithelium and connective tissue (lamina dura) Submucosa : connective tissues made of dense to loose areolar tissues - if firmly attached : withstands pressure - if loose, thin, traumatized, mobile, flabby: won't be stable to withstand pressure {not resilient} Masticatory Mucosa (keratinized) : hard palate, residual ridges, residual attached gingival Hard palate: - keratinized. - mid palatine suture : submucosa is extremely thin, requires relief! - primary support area: horizontal portion of the hard palate - secondary support area: rugae area (set at right angle to the residual ridge) The palatal gingival vestige: remnants of the lingual gingival margin, it is the remains of the palatal gingival ; after tooth extraction the position of the vestige remains relatively constant (static), the same as the incisive papilla. This can be a very helpful pointer for posterior tooth positioning during denture construction. there are some techniques that are based on these static marks, but we won't be using any of them in our fourth & fifth years! Residual Ridges: 1. Mucus membrane: it's keratinized and firmly attached the submucosa: devoid the glandular tissue. Dense collagenous fibers. It's relatively thin and not sufficient to provide support for the denture base. 2. Crest of the ridges: it is prone to resorption, and of the secondary support area! 3. Inclined facial surfaces: it loses its firm attachment, so it offers little support and cannot be used as a support area.
The Fovea Palatine: 1. Two orifices one on each side of the palatal midline. It is the coalescence of several mucous glands, and it's ALWAYS located in the soft palate! 2. They act as collecting ducts for a group of minor palatine salivary glands.
The most important thing in impressions is to get the BORDERS accurately! It's also important to get all the structures accurately; it's not an easy task to be done accurately. But it's important to know that a denture depends on the peripheral seal (for the primary impression), ok you need good adaptation, good impression, no voids here and there, the choice of the material or the technique.... but this is sort of easy; to fill between the borders! But as we can see there are many structures here at the borders that you have to get in order to have a good final impression. Knowledge of the muscles and structures that produce the borders is a prerequisite to successful impression making. Knowledge of how to activate the muscles and locate the structures is also needed.
Let's start with them one by one...
These are the labial frenum and the buccal frenum...
Then we come to the orbicularis oris, levator labii superioris, levator anguli oris, incisivus labii superioris muscles that form the anterior part of the denture (and the impression). These structures will control the depth and the length of the sulcus.
Then we go to the buccinator muscle... Forming the distal part of the denture (the impression). "the lip form the ant. Part up to the buccal frenum area"
Now the risorius muscle, controlling the width of that area.
Here you ask the patient to open wide and move the mandible to the left and to the right, to get the impression of the coronoid.
The hamular notch should be recorded here, or another name for it is the pterygomaxillary fissure.
The palatine aponeurosis which consists of different structures this area is really important to get, to complete your peripheral seal, by adapting the denture to compress that area. The structures are: tensor veli palatini, levator veli palatini, palatophartngeus, palatoglossus, musculus uvulae muscles.
And there it is all the structures are in this picture.
Let's Now Concentrate On The Posterior Palatal Seal. We have this line making the junction between the hard and soft palate it's also called Valsalva Maneuver so anterior to it is the hard palate, and posteriorly the soft palate. How do we get that line? you ask the patient to close the nostrils and blow through the nose
Now the soft palate is composed of: immovable part (just behind valsalva maneuver) and movable part The line that separates them is called the Vibrating line. Behind this line, shouldn't be covered for retention! Bcoz the area there is movable Sometimes u need to check the compressibility of the hard palate with a burnisher coz sometimes the tissues there are compressible (50% in average) so can be used for the posterior palatal seal. - measure the depth of soft tissue displacement and make a depth "not more than" 2/3rds that depth"; about one-half of the displacement! And what you do next is you carve the cast at that area "between the hard-soft palate junction & the vibrating line" (spoon shaped); the deepest part is in the middle and zero over the lines as if it flushes all the way up! That's how you make your posterior palatal seal.
We have several advantages of the posterior palatal seal: 1. To increase the maxillary complete denture retention by having the posterior aspect of the denture base slightly compress the posterior portion of the palatal soft tissue (both soft and hard palates) 2. To compensate for the polymerization shrinkage of the resin so the denture base will contact the posterior aspect of the palate and maintain the seal.
Let's start with them one by one...
These are the labial frenum and the buccal frenum.
Then the lip musculature: Depressor labii inferioris, mentalis, incisivus labii inferioris, orbicularis oris muscles. These muscles will form the anterior area of the impression controlling the sulcus depth and width.
Then the buccinator again Forming all the posterior area.
Here is the masseter muscle. it compresses the buccinator muscle forming the masseteric notch. *These structures should not be always present, what u do is that u try to manipulate the muscles and try to see the maximum action of the muscle on the impression material, but if you don't see these things, this doesn't mean your impression is not good!
The temporalis muscle.
And also we have two important structures forming the gap ligually; the superior constrictor muscle and the palatoglossus muscle. You get these impressions by putting your finger on the tip of the tongue and ask the patient to push forward, and you resist this push.
most of the common mistakes in the lower impression is this area it's usually short! So we have to go deep and maximize the stability and retention of the lower denture.
And we have the mylohyoid muscle forming all the lingual portion of your impression.
These are all the structures of the mandibular impression
The buccal shelf area is important for support and also the marginal ridge and all the other structures.
Crest Of The Residual Ridge: 1. Ridge is smaller comparing to that of the upper in a healthy mouth. 2. Attachment varies considerably. In some people the submucosa is loosely attached to the underlying bone. 3. When securely attached to the bone, the mucous membrane is capable of providing support for the denture. However, because the underlying bone is cancellous, the crest of the residual ridge may not be favorable as a primary stress bearing area for the lower denture.
The buccinator muscle, the mandibular raphe, the superior constrictor, masseteric muscle, medial pterygoid .these are the structures that have many things to do with the placement and the relations of the denture in the jaw. - For the buccal shelf area: The mucus membrane is more loosely attached and less keratinized than that covering the residual ridge. Although the mucous membrane may not be as suitable histological to provide support for the denture, the bone of the buccal shelf area is covered by a layer of cortical bone. This, plus the fact that the shelf lies at right angle to the vertical occlusal force, makes it the most suitable primary stress bearing area for the lower denture. - The external oblique ridge does not govern the extension of the buccal flange because the resistance or the lack of it varies widely. The buccal flange may extend to the external oblique ridge, up onto it, or even over it depending on the location of the mucobuccal fold. - The bearing of the denture on the muscle fibers of the buccinator wouldn't be possible except for the fact that the fibers run parallel to the border and not at right angle. - The distobuccal border must converge rapidly to avoid the action of the masseter which pushes inward the buccinator. - The distal extension is limited by: * The ramus * The buccinator * The pterygo-mandibular raphe * Superior constrictor muscle * The sharpness of the boundaries of the retro-molar fossa. ( the denture should extend slightly to the lingual into the pearl shaped retro-molar pad). - The retro-molar pad is a triangular soft pad of tissue. It's mucosa is composed of thin, non-keratinized epithelium. Its submucosa contains: * Glandular tissue.
* Fibers of the buccinator and superior constrictor. * Pterygo-mandibular raphe. * Fibers of the temporalis. Because of these structures the denture base should only extend to one half to two thirds of the retro-molar pad.
The Retro-molar Pad: It is split into two sections. The anterior section is usually firm and fibrous, it's important for denture support and preventing distal displacement.
The Mylohyoid Ridge: It becomes more prominent following the extraction of natural teeth and subsequent resorption. This can result in mucosal soreness beneath the denture bearing area over the mylohyoid ridge.
When we talk about the mylohyoid muscle why do we look for the S shape? Because of the way the mylohyoid muscle is attached to the bone; The retro-molar pad area is deep, so the denture can go slightly in, and so will be close to the bone. (The sulcus is close to the bone). While here the mylohyoid attachment is quite high, so the denture will be away from the bone (closer to the tongue). So close to the bone posteriorly, then away (towards the tongue), then down closer to the bone (because the muscle attachment is low there). (IN , OUT , IN) This is the nice S shape u get on your lower impression.
You get that S shape by properly manipulating the tongue, but you don't always get it, not because your technique is wrong, but because sometimes the anatomy is not clear (the place of the attachment, the resorption of the ridges). But we are talking about the ideal situation. "The doctor skipped many slides, but I wrote everyth. here, so u don't have to go back to the slides"
Notes about: The Mylohyoid Muscle: 1. It is a thin sheet of fibers and in a relaxed state will not resist the impression material. 2. Carrying the border under the mylohyoid cannot be tolerated. The contraction of this muscle will displace the denture. 3. Fortunately, the denture in the posterior area of the mylohyoid can beyond its attachment because the fold isn't in this area. 4. In the retro-mylohyoid fossa the border of the denture can move back toward the body of the mandible producing the S curve of the lingual flange. 5. In the anterior region, a depression (the pre-mylohyoid fossa) can be palpated, and a corresponding prominence (the per-mylohyoid eminence) is seen on the impression. The doctor played some videos about how to activate the muscles during impression making? But he refused to give them to us. Sorry about this Here are two videos that cover most of the information needed
http://www.youtube.com/watch?v=W87YVwMy4fo http://www.youtube.com/watch?v=Z3Um3z4Zo88
Das könnte Ihnen auch gefallen
- Pulp Capping Part1Dokument9 SeitenPulp Capping Part1براءة أحمد السلاماتNoch keine Bewertungen
- Pulp Capping Part 2Dokument7 SeitenPulp Capping Part 2براءة أحمد السلاماتNoch keine Bewertungen
- Operative DentistryDokument45 SeitenOperative Dentistryبراءة أحمد السلامات100% (1)
- Flu RideDokument4 SeitenFlu Rideبراءة أحمد السلاماتNoch keine Bewertungen
- Pulp Capping Part 2Dokument7 SeitenPulp Capping Part 2براءة أحمد السلاماتNoch keine Bewertungen
- Osteoporois and PeriodontitisDokument4 SeitenOsteoporois and Periodontitisبراءة أحمد السلاماتNoch keine Bewertungen
- Cons Occlusal ConsedrationDokument20 SeitenCons Occlusal Consedrationبراءة أحمد السلاماتNoch keine Bewertungen
- Cons Occlusal ConsedrationDokument20 SeitenCons Occlusal Consedrationبراءة أحمد السلاماتNoch keine Bewertungen
- Pulp Capping Part1Dokument9 SeitenPulp Capping Part1براءة أحمد السلاماتNoch keine Bewertungen
- Cons Occlusal ConsedrationDokument20 SeitenCons Occlusal Consedrationبراءة أحمد السلاماتNoch keine Bewertungen
- Sealants For Preventing Dental Decay in The Permanent Teeth (Review)Dokument4 SeitenSealants For Preventing Dental Decay in The Permanent Teeth (Review)براءة أحمد السلاماتNoch keine Bewertungen
- Patient's File DocumentationDokument1 SeitePatient's File DocumentationPrince Ahmed100% (1)
- 8 - Pediatric Dentistry 1Dokument10 Seiten8 - Pediatric Dentistry 1براءة أحمد السلاماتNoch keine Bewertungen
- Fluoride Supplements (Tablets, Drops, Lozenges or ChewingDokument4 SeitenFluoride Supplements (Tablets, Drops, Lozenges or Chewingبراءة أحمد السلاماتNoch keine Bewertungen
- Pedo 3Dokument6 SeitenPedo 3Salam BataienehNoch keine Bewertungen
- 6 - Pedeatric Dentistry 2 PDFDokument15 Seiten6 - Pedeatric Dentistry 2 PDFبراءة أحمد السلاماتNoch keine Bewertungen
- 4 - 10) Pulp Therapy For The Young Permanent DentitionDokument15 Seiten4 - 10) Pulp Therapy For The Young Permanent Dentitionبراءة أحمد السلاماتNoch keine Bewertungen
- 3) Early Caries - Developmantal AnamoliesDokument27 Seiten3) Early Caries - Developmantal AnamoliesEman NazzalNoch keine Bewertungen
- 1) Pulp Therapy For Primary TeethDokument16 Seiten1) Pulp Therapy For Primary TeethEman NazzalNoch keine Bewertungen
- Pedo Script 8Dokument19 SeitenPedo Script 8Prince AhmedNoch keine Bewertungen
- Script Number (-), Title ++++++++, Date ++++Dokument3 SeitenScript Number (-), Title ++++++++, Date ++++براءة أحمد السلاماتNoch keine Bewertungen
- 1 - Pedo-7Dokument15 Seiten1 - Pedo-7براءة أحمد السلاماتNoch keine Bewertungen
- Script Number (-), Title ++++++++, Date ++++Dokument3 SeitenScript Number (-), Title ++++++++, Date ++++براءة أحمد السلاماتNoch keine Bewertungen
- Case Report - True Hemifacial Hyperplasia-CRIM - dentISTRY2013-152528Dokument7 SeitenCase Report - True Hemifacial Hyperplasia-CRIM - dentISTRY2013-152528براءة أحمد السلاماتNoch keine Bewertungen
- Preventive Dentistry TampleteDokument3 SeitenPreventive Dentistry Tampleteبراءة أحمد السلاماتNoch keine Bewertungen
- Crown and Bridges TampletDokument3 SeitenCrown and Bridges Tampletبراءة أحمد السلاماتNoch keine Bewertungen
- Report Case - Conjoined Primery Molar and PremolarDokument4 SeitenReport Case - Conjoined Primery Molar and Premolarبراءة أحمد السلاماتNoch keine Bewertungen
- Script Number (-), Title ++++++++, Date ++++Dokument3 SeitenScript Number (-), Title ++++++++, Date ++++براءة أحمد السلاماتNoch keine Bewertungen
- Script Number (-), Title ++++++++, Date ++++Dokument3 SeitenScript Number (-), Title ++++++++, Date ++++براءة أحمد السلاماتNoch keine Bewertungen
- Script Number (-), Title ++++++++, Date ++++Dokument3 SeitenScript Number (-), Title ++++++++, Date ++++براءة أحمد السلاماتNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Understanding Poultry Game BirdsDokument33 SeitenUnderstanding Poultry Game BirdsThoyyibNoch keine Bewertungen
- Ethical Guidelines PsychologyDokument3 SeitenEthical Guidelines PsychologyManal_99xoNoch keine Bewertungen
- NEET UG Biology Evolution PDFDokument22 SeitenNEET UG Biology Evolution PDFamsaeangovanNoch keine Bewertungen
- Comparative Anatomy Classification ChartDokument2 SeitenComparative Anatomy Classification Chartapi-613673827Noch keine Bewertungen
- The Endangered Bambo 3Dokument2 SeitenThe Endangered Bambo 3yejuNoch keine Bewertungen
- Lower Genital Tract InfectionDokument51 SeitenLower Genital Tract InfectionSarisa SupawimonNoch keine Bewertungen
- VSDDokument4 SeitenVSDtikabdullahNoch keine Bewertungen
- 2nd QRTR Anet ReteachDokument13 Seiten2nd QRTR Anet Reteachapi-310709379Noch keine Bewertungen
- Brucellosis in horses causes fistulous withers and poll evilDokument6 SeitenBrucellosis in horses causes fistulous withers and poll evilMaceface JimenezNoch keine Bewertungen
- AACC 10 AbstractBook PDFDokument276 SeitenAACC 10 AbstractBook PDFmsnsaikiranNoch keine Bewertungen
- Grammar Exercises - Simple Past TenseDokument6 SeitenGrammar Exercises - Simple Past TensePatty JonasNoch keine Bewertungen
- Story-Telling Competition Title: The Milkmaid and Her PailDokument6 SeitenStory-Telling Competition Title: The Milkmaid and Her PailCoffee&LoveNoch keine Bewertungen
- Play QuotationsDokument11 SeitenPlay QuotationsJennifer KableNoch keine Bewertungen
- Hep ADokument2 SeitenHep Aapi-237098034Noch keine Bewertungen
- Office Head Titles MunicipalityDokument2 SeitenOffice Head Titles MunicipalityGeo AngeloNoch keine Bewertungen
- ACUP306Dokument4 SeitenACUP306raysklineNoch keine Bewertungen
- Crocheted Uterus PatternDokument2 SeitenCrocheted Uterus Patternweasley123100% (4)
- Main Idea 2Dokument3 SeitenMain Idea 2api-234576762100% (3)
- Science P1 Mid Test 1 & 2Dokument4 SeitenScience P1 Mid Test 1 & 2Stefani PanjaitanNoch keine Bewertungen
- Indian import duty rates for live animals, meat, fish and aquatic productsDokument98 SeitenIndian import duty rates for live animals, meat, fish and aquatic productsGopal UNoch keine Bewertungen
- CH 12 Word ListDokument3 SeitenCH 12 Word ListtigertiaNoch keine Bewertungen
- Cure - Family Health MatterzDokument14 SeitenCure - Family Health MatterzGeorge AniborNoch keine Bewertungen
- Stretching and FlexibilityDokument47 SeitenStretching and Flexibilitymartin.wilfred7257Noch keine Bewertungen
- Argumentative EssayDokument4 SeitenArgumentative Essayapi-527619279Noch keine Bewertungen
- EN Tinycorn and Friends PDF Ebook by AhookADokument39 SeitenEN Tinycorn and Friends PDF Ebook by AhookAPato camaradas100% (1)
- Getting The Main Idea Answer KeyDokument2 SeitenGetting The Main Idea Answer KeyMuh Azan100% (1)
- THE STAG - Class NotesDokument3 SeitenTHE STAG - Class Notesmishka100% (1)
- Sex of Camel On Tick Infestation Rates in One-Humped Camel (Camelus Dromedarius) Population in The Northeast of IranDokument7 SeitenSex of Camel On Tick Infestation Rates in One-Humped Camel (Camelus Dromedarius) Population in The Northeast of IranMulugeta TesfayeNoch keine Bewertungen
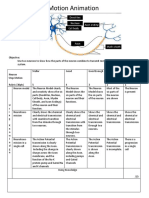
- Neurons Stop Motion AnimationDokument2 SeitenNeurons Stop Motion Animationapi-495006167Noch keine Bewertungen
- Vence Ferrell - The Vaccination CrisisDokument177 SeitenVence Ferrell - The Vaccination CrisisIna Hasim100% (1)