Beruflich Dokumente
Kultur Dokumente
2003 - Journal of Endodontics - 29 - 4 - 265 - 267 - Tissue Levels of Immunoreactive Substance P Are Increase PDF
Hochgeladen von
Namrata SachdevaOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
2003 - Journal of Endodontics - 29 - 4 - 265 - 267 - Tissue Levels of Immunoreactive Substance P Are Increase PDF
Hochgeladen von
Namrata SachdevaCopyright:
Verfügbare Formate
JOURNAL OF ENDODONTICS Copyright 2003 by The American Association of Endodontists
Printed in U.S.A. VOL. 29, NO. 4, APRIL 2003
CLINICAL ARTICLES Tissue Levels of Immunoreactive Substance P are Increased in Patients with Irreversible Pulpitis
Walter R. Bowles, DDS, MS, John C. Withrow, DDS, MS, Allen M. Lepinski, DDS, MS, and Kenneth M. Hargreaves, DDS, PhD
Odontogenic pain often involves inflammation of dental pulp tissue. Dental pulp is highly innervated with a subpopulation of sensory neurons containing neuropeptides. Substance P, released from afferent fibers (e.g. nociceptors) is associated with the development of neurogenic inflammation. In this study, we tested the hypothesis that irreversible pulpitis is associated with increased activity of peptidergic neurons, as measured by increased pulpal levels of immunoreactive substance P (iSP). We determined in vivo pulpal levels of immunoreactive substance P in human teeth with a diagnosis of normal pulp or irreversible pulpitis using CMA/20 microdialysis probes inserted into vital pulps of 24 teeth from 21 patients. Probes were perfused with a modified Locke-Ringers buffer and immunoreactive substance P levels in the dialysate were measured using a radioimmunoassay. Mean extracellular levels of immunoreactive substance P were significantly higher (>8-fold) in teeth diagnosed with irreversible pulpitis than immunoreactive substance P levels in dental pulp diagnosed as normal (147.7 34.0 pM versus 18.2 6.2 pM). These observations suggest that biochemical measures of inflammatory mediators exhibit significant change during irreversible pulpitis and may contribute to clinical signs and symptoms.
Odontogenic pain is the most common orofacial pain and often involves inflammation of the dental pulp. Many classic studies have failed to detect a histologic change with pulpitis (1 4), yet changes at the biochemical level are not amenable to histological studies and thus are still under investigation. The dental pulp by nature is exposed to anatomic, iatrogenic, and pathologic factors that contribute to induction and maintenance of inflammation.
265
These factors often contribute to pain or to altered pain conditions, such as hyperalgesia or allodynia. Moreover, recent research has demonstrated complicated, dynamic interactions taking place among the neural elements, pulp cells, immunocompetent cells, pulpal tissue fluid, and vasculature to produce pain (5). Dental pulp is highly innervated with a subpopulation of sensory neurons containing neuropeptides, such as substance P (SP). These neuropeptides are released from peptidergic afferent fibers and are associated with the development of neurogenic inflammation and wound healing. A predominant form of inflammation in dental pulp is thought to be neurogenically mediated (6), suggesting that biochemical measures of inflammatory mediators exhibit significant change during irreversible pulpitis and contribute to clinical signs and symptoms. SP is a proinflammatory neuropeptide causing plasma extravasation and edema (7, 8, for review see 9). The neurogenic inflammation resulting from peripheral release of neuropeptides evokes vascular changes and permeability alterations in dental pulp. SP evokes vasodilation and endothelial cell contraction, resulting in increased leakage of plasma proteins (10). These effects are mediated through the G-protein coupled receptor NK-1. Although not as fast acting as ionic channels, G-protein coupled receptors have a much broader effect through second messengers. In this study, we tested the hypothesis that irreversible pulpitis is associated with increased activity of peptidergic neurons, as measured by increased pulpal levels of immunoreactive substance P (iSP). To evaluate this hypothesis, we determined the in vivo levels of iSP in extracellular fluid from dental pulp with a diagnosis of irreversible pulpitis compared with levels measured in normal pulp. Microdialysis is an appropriate method because it measures extracellular levels of substances of interest (in this case, inflammatory mediators). By examining extracellular levels of the neuropeptide, we measure the concentration that is physiologically active, because this is the concentration that is available to activate the NK-1 receptor. In contrast, immunohistochemical studies indicate the location of tissue content but do not provide information on actual extracellular concentrations. Levels of SP were measured using microdialysis probes (Fig. 1), which have advantages over previous methods of neuropeptide collection, including exclusion of peptidases, and no dilution of the sample. Additionally, micro-
266
Bowles et al.
Journal of Endodontics
FIG 1. Schematic Fig. illustrating the in vivo placement of a microdialysis probe for collection of extracellular inflammatory mediators. Modified Locke-Ringers buffer is pumped through the microdialysis probe, which is positioned in the pulp chamber of the tooth. The dialysate is collected from the outlet tube and snap frozen. Dialysate levels are subsequently analyzed by radioimmunoassay. The enlarged portion is a schematic of the microdialysis probe demonstrating the exclusion of larger molecules, such as proteases that might degrade the substance of interest.
dialysis permits calculation of extracellular SP levels with minimal disruption of the inflamed tissue, because this method does not require excess solution pumped into the tissue (11), thus making this an ideal method to determine extracellular SP in the dental pulp. MATERIALS AND METHODS Microdialysis of dental pulp tissue was performed using CMA/20 microdialysis probes (CMA Microdialysis, Acton, MA) that are 4 mm long and 0.5 mm in diameter, with a molecular weight cutoff of 20 kD. Our initial studies determined optimal flow rates for neuropeptide collection using a known concentration of SP. Modified Locke-Ringers buffer was perfused through the probe and the dialysate from the outlet line was analyzed using a previously validated radioimmunoassay (12). The modified LockeRingers buffer consisted of: sodium chloride 9.001 g (154 mm/L); calcium chloride 0.2355 g (1.6 mmol/L); magnesium chloride 0.2033 g (1 mmol/L); potassium chloride 0.4175 g (5.6 mmol/L); dextrose 0.5044 g (2.8 mmol/L); sodium citrate 3.5292 g (12 mmol/L); and sodium bicarbonate 0.550406 g (6 mmol/L) added to 1 L of sterile water and sterilized by filtration through a 0.22-m filter under a laminar flow hood. Patients for the study were recruited from the University of Minnesota School of Dentistry and signed an informed consent document approved by our Institutional Review Board. Twentyfour teeth in 21 patients were used. There were 8 normal pulps and 16 with irreversible pulpitis. Patients age ranged from 13 to 53 yr. All patients were treatment planned for either endodontic therapy
or extraction of the tooth. To be included in the study, patients had to have a diagnosis of normal or irreversible pulpitis. A normal pulp diagnosis required the following: (a) a positive vitality test (cold or electric pulp test); (b) no spontaneous pain; (c) no pain to percussion or chewing; (d) no caries present; and (e) no radiographic evidence of periapical pathosis. The criteria for a diagnosis of irreversible pulpitis were the following: (a) a tooth responsive to cold with a positive lingering response; (b) a history of spontaneous pain (assessed by visual analog scale); (c) either a normal or hypersensitive reaction to percussion; and (d) no radiographic evidence of periradicular pathosis. A regional nerve block using local anesthesia (1.8 ml of lidocaine 2% with epinephrine 1:100,000) was administered. If the patient was not comfortable enough to access the pulp chamber through a regional block alone, they were excluded from the study. This was done to minimize the potential complication of lidocaine or epinephrine entering the pulp and potentially altering pulpal iSP release (12). A rubber dam was placed and an endodontic access opening was prepared just short of the pulp. A 556 straight fissure bur was used to create an opening in the roof of the pulp chamber just wide enough to completely insert two microdialysis probes into the pulp tissue. The upper portion of the microdialysis apparatus was stabilized in the access opening using warm gutta-percha from an Obtura II delivery system (Obtura Spartan, Fenton, MO). PE50 tubing was attached to a Gilson minipuls II perfusion pump (Gilson Medical Electronics, Middleton, WI) and connected to the inflow tubing of each microdialysis probe. Outflow tubing for collection of dialysate was attached to a borosilicate test tube placed on ice. Microdialysis probes were perfused with modified Locke-Ringers buffer at a rate of 6 l/min for 1 h. Immediately after collection, microdialysis probes were removed and the test tube containing the dialysate transferred to a freezer and stored at 80 C. A previously validated radioimmunoassay (13) was used to determine levels of iSP in the collected samples. Briefly, 0.1 ml of SP antiserum was added to SP standard in radioimmunoassay buffer or the unknown sample and allowed to equilibrate at 4C for 24 h. Then, 0.1 ml of [125I-Tyr0]-substance P (approximately 20,000 25,000 cpm) and 50 l of goat anti-rabbit antisera coupled to ferric beads (Polysciences, Inc., Warrington, PA) were added to each sample, vortexed, and allowed to incubate for an additional 24 h at 4C. The radioimmunoassay was stopped by immunomagnetic separation. The liquid was aspirated from each sample and the immunoprecipitated reaction product counted on a gamma counter (Wallac, Inc., Gaithersburg, MA). Standard curves were generated in modified Locke-Ringers buffer and iSP levels determined using logit-log analysis. The radioimmunoassay buffer consisted of modified Locke-Ringers buffer. The minimum detection limit of the assay is 1 to 2 fmol of iSP with intra- and interassay coefficient of variation less than 6% and 12%, respectively. Data were analyzed using a two-sample t test, and a difference was considered significant at p 0.05. Data are expressed as mean SEM.
RESULTS Twenty-one patients participated in the study with 24 samples collected. Two additional patients were excluded from the study due to inability to obtain block anesthesia. Patients with a diagnosis of normal pulp had a pain rating on the visual analog scale (VAS) of 0. Patients with a diagnosis of irreversible pulpitis had a pain rating of 8.15 0.38 (mean SEM) out of a maximum score
Vol. 29, No. 4, April 2003
Irreversible Pulpitis Increases Substance P
267
of 10. Scores above 5 are associated with moderate to very severe pain. Levels of iSP collected by microdialysis were much higher in the irreversibly inflamed pulp versus the normal pulp. The mean iSP concentration in normal pulp was 18.2 6.2 pM (mean SEM), whereas the mean iSP concentration in pulp tissue diagnosed with irreversibly pulpitis was 147.7 34.0 pM (mean SEM). Concentrations of iSP in the irreversibly inflamed pulp were over eight times greater than concentrations found in normal pulp. A statistically significant difference in the level of iSP was found between the two groups (p 0.001). DISCUSSION Prior studies have demonstrated substance P to be involved in both inflammation and pain (14 16). This study demonstrated that extracellular levels of substance P are increased within symptomatic pulp tissue diagnosed with irreversible pulpitis. An 8-fold increase in substance P was noted in pulp tissue diagnosed with irreversible pulpitis versus that of clinically normal pulp tissue. Thus, irreversible pulpitis is associated with significant activation of this peptidergic system. Possible mechanisms for the increase in extracellular substance P include: (a) increased synthesis of the neuropeptide in the trigeminal ganglia; (b) increased rate of transport; (c) increased release; and (d) decreased levels of peptidases, which would result in decreased degradation of substance P (17). Further research in these areas is needed to elucidate the mechanism for this increase in substance P. Increased extracellular substance P may affect the complex interaction between pulp cells, immunocompetent cells, vasculature, and nerve fibers. Because substance P and VAS pain levels are positively associated, we speculate that interactions change among cells of the pulp. Pulpal injury can produce sprouting of peptidergic fibers, which return to normal after healing (18). In denervated teeth, however, there is an accelerated loss of pulp tissue after injury (18). Pulpal healing, therefore, involves neuropeptides. Neuropeptides have an immunomodulatory role by stimulating and recruiting immunocompetent cells (19). Immune cells can also express functional neuropeptide receptors (20). These findings suggest an important role for neuropeptides in dental pulp, not only in pain and inflammation, but also in protection and repair. Classic endodontic research has demonstrated that histopathosis of the pulp does not equate to clinical symptoms. Biochemical measures, however, may correlate better with symptomatic teeth and allow design of novel analgesics. Our intention is to provide a greater knowledge of what happens in irreversible pulpitis and to examine new approaches to prevent or correct pulpal pain. Considering the correlation between the symptomatic teeth with increased substance P levels and patient VAS scores, substance P modulation may provide a novel approach for the treatment of pulpal inflammation and pain.
This research was supported by NIH DE09737-08 and the American Association of Endodontists Foundation. The informed consent of all human subjects who participated in the experimental investigation reported or described in this manuscript was obtained after the nature of the procedure and possible discomforts and risks had been fully explained. Dr. Bowles is assistant professor and director, and Drs. Withrow and Lepinski are clinical assistant professors, Division of Endodontics, University of Minnesota School of Dentistry, Minneapolis, MN. Drs. Withrow and Lepinski are in private practice in Minneapolis, MN. Dr. Hargreaves is professor and chair, Department of Endodontics, University of Texas Health Sciences Center, San Antonio, TX. Address requests for reprints to Dr. Walter Bowles, University of Minnesota School of Dentistry, Division of Endodontics, 8-166 Moos Tower, 515 Delaware Street SE, Minneapolis, MN 55455.
References 1. Seltzer S, Bender IB, Ziontz M. The dynamics of pulp inflammation: correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg 1963;16:846 71. 2. Massler M. Pulpal response to dental caries. Int Dent J 1967;17:441 60. 3. Tyldesley WR, Mumford JM. Dental pain and the histological condition of the pulp. Dent Prac 1970;20:333. 4. Langeland K. Management of the inflamed pulp associated with deep carious lesion. J Endodon 1981;7:169 81. 5. Byers MR, Taylor PE, Khayat BG, Kimberly CL. Effects of injury and inflammation on pulpal and periapical nerves. J Endodon 1990;16:78 84. 6. Kim S. Neurovascular interactions in the dental pulp in health and inflammation. J Endodon 1990;16:48 53. 7. Hargreaves KM, Swift JQ, Roszkowski MR, Bowles WR, Garry MG, Jackson DL. Pharmacology of peripheral neuropeptide and inflammatory mediator release. Oral Surg Oral Med Oral Pathol 1994;78:50310. 8. Olgart L, Kerezoudis NP. Nerve-pulp interactions. Arch Oral Biol 1994; 39(Suppl):47S54S. 9. Harrison S, Geppetti P. Substance P. Int J Biochem Cell Biol 2001;33: 55576. 10. Lembeck F, Holzer P. Substance P as neurogenic mediator of antidromic vasodilation and neurogenic plasma extravasation Naunyn Schmiedebergs. Arch Pharmacol 1979;10:175 83. 11. Hargreaves KM, Costello A. Glucocorticoids suppress levels of immunoreactive bradykinin in inflamed tissue as evaluated by microdialysis probes. Clin Pharmacol Ther 1990;48:168 78. 12. Hargreaves KM, Bowles WR, Roszkowski MT, Jackson DL, Richardson JD, Engelstad M. Regulation of neuropeptide secretion from pulp. Proc Int Confer Dentin Pulp Complex 1996;188 92. 13. Grutzner EH, Garry MG, Hargreaves KM. Effect of injury on pulpal levels of immunoreactive substance P and immunoreactive calcitonin generelated peptide. J Endodon 1992;18:5537. 14. Byers MR, Taylor PE. Effect of sensory denervation on the response of rat molar pulp to exposure injury. J Dent Res 1993;72:613 8. 15. Traub RJ. The spinal contribution of substance P to the generation and maintenance of inflammatory hyperalgesia in the rat pain 1996;67:151 61. 16. Dionne RA, Max MB, Gordon SM, et al. The substance P receptor antagonist CP-99,994 reduces acute postoperative pain. Clin Pharmacol Ther 1998;64:562 8. 17. Buck S, Reese K, Hargreaves KM. Pulpal exposure alters neuropeptide levels in inflamed dental pulp and trigeminal ganglia: evaluation of axonal transport. J Endodon 1999;25:718 21. 18. Byers MR, Taylor PE. Effect of sensory denervation on the response of rat molar pulp to exposure injury. J Dent Res 1993;72:613 8. 19. Peck R. Neuropeptides modulating macrophage function. Ann NY Acad Sci 1987;496:264 70. 20. Payan DG, McGillis JP, Organist ML. Binding characteristics and affinity labeling of protein constituents of the human IM-9 lymphoblast receptor for substance P. J Biol Chem 1986;261:143219.
Das könnte Ihnen auch gefallen
- Apex LocatorDokument10 SeitenApex LocatorNamrata SachdevaNoch keine Bewertungen
- 2003 - Journal of Endodontics - 29 - 4 - 261 - 264 - The Comparative Sealing Ability of Hydroxyapatite Cement PDFDokument4 Seiten2003 - Journal of Endodontics - 29 - 4 - 261 - 264 - The Comparative Sealing Ability of Hydroxyapatite Cement PDFNamrata SachdevaNoch keine Bewertungen
- 2003 Journal-of-Endodontics 29 4 272 274 Secondary-Hyperparathyroidism-A-Case-Report Loushine 009 PDFDokument3 Seiten2003 Journal-of-Endodontics 29 4 272 274 Secondary-Hyperparathyroidism-A-Case-Report Loushine 009 PDFNamrata SachdevaNoch keine Bewertungen
- 2003 - Journal of Endodontics - 29 - 4 - 268 - 271 - Effect of An Intraosseous Injection of Depo Medrol On Pu PDFDokument4 Seiten2003 - Journal of Endodontics - 29 - 4 - 268 - 271 - Effect of An Intraosseous Injection of Depo Medrol On Pu PDFNamrata SachdevaNoch keine Bewertungen
- 2003 - Journal of Endodontics - 29 - 4 - 252 - 256 - Three Dimensional Quantitation of Periradicular Bone Des PDFDokument5 Seiten2003 - Journal of Endodontics - 29 - 4 - 252 - 256 - Three Dimensional Quantitation of Periradicular Bone Des PDFNamrata SachdevaNoch keine Bewertungen
- 2003 - Journal of Endodontics - 29 - 4 - 259 - 260 - Effectiveness of Stannous Fluoride and Calcium Hydroxide PDFDokument2 Seiten2003 - Journal of Endodontics - 29 - 4 - 259 - 260 - Effectiveness of Stannous Fluoride and Calcium Hydroxide PDFNamrata SachdevaNoch keine Bewertungen
- 2003 - Journal of Endodontics - 29 - 4 - 248 - 251 - Effects of NaOCl On Bond Strengths of Resin Cements To R PDFDokument4 Seiten2003 - Journal of Endodontics - 29 - 4 - 248 - 251 - Effects of NaOCl On Bond Strengths of Resin Cements To R PDFNamrata SachdevaNoch keine Bewertungen
- 2003 - Journal of Endodontics - 29 - 4 - 233 - 239 - The Effect of Various Concentrations of Sodium Hypochlor PDFDokument7 Seiten2003 - Journal of Endodontics - 29 - 4 - 233 - 239 - The Effect of Various Concentrations of Sodium Hypochlor PDFNamrata SachdevaNoch keine Bewertungen
- 2003 - Journal of Endodontics - 29 - 4 - 240 - 243 - Induction of Cyclooxygenase 2 mRNA and Protein Expressio PDFDokument4 Seiten2003 - Journal of Endodontics - 29 - 4 - 240 - 243 - Induction of Cyclooxygenase 2 mRNA and Protein Expressio PDFNamrata SachdevaNoch keine Bewertungen
- 2003 - Journal of Endodontics - 29 - 4 - 244 - 247 - Treponema Socranskii in Primary Endodontic Infections As PDFDokument4 Seiten2003 - Journal of Endodontics - 29 - 4 - 244 - 247 - Treponema Socranskii in Primary Endodontic Infections As PDFNamrata SachdevaNoch keine Bewertungen
- Article4 PDFDokument0 SeitenArticle4 PDFNamrata SachdevaNoch keine Bewertungen
- Article5 PDFDokument0 SeitenArticle5 PDFNamrata SachdevaNoch keine Bewertungen
- Article3 PDFDokument0 SeitenArticle3 PDFNamrata SachdevaNoch keine Bewertungen
- Article2 PDFDokument0 SeitenArticle2 PDFNamrata SachdevaNoch keine Bewertungen
- Article1 PDFDokument0 SeitenArticle1 PDFNamrata SachdevaNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Nutrition: Important ConceptsDokument12 SeitenNutrition: Important ConceptshafizaqaiNoch keine Bewertungen
- 5 - Circulation GraysDokument33 Seiten5 - Circulation GraysdrmanojkulNoch keine Bewertungen
- Nose Fracture and Deviated SeptumDokument17 SeitenNose Fracture and Deviated Septummimi2188Noch keine Bewertungen
- ECCO 2 Hemodynamics TestDokument3 SeitenECCO 2 Hemodynamics TestpamoralesNoch keine Bewertungen
- 5937 Understanding Nonverbal Communication Guidebook PDFDokument116 Seiten5937 Understanding Nonverbal Communication Guidebook PDFSalomao RodriguesNoch keine Bewertungen
- Descriptive Text: Report Text About Turtle - Giant Tortoise GalapagosDokument5 SeitenDescriptive Text: Report Text About Turtle - Giant Tortoise GalapagospujayantiriskaNoch keine Bewertungen
- Vitamin KDokument15 SeitenVitamin KTooba Sd100% (2)
- Hachi's PermitDokument1 SeiteHachi's PermitBebelyn AlquizarNoch keine Bewertungen
- Reproduction SystemDokument38 SeitenReproduction SystemNurfatin AdilaNoch keine Bewertungen
- Cheat Sheet 2Dokument2 SeitenCheat Sheet 2oushaNoch keine Bewertungen
- Airway Management 1Dokument17 SeitenAirway Management 1kamel6Noch keine Bewertungen
- VSR PDFDokument12 SeitenVSR PDFDrkrunal badaniNoch keine Bewertungen
- Nipah Virus Infection: ImportanceDokument9 SeitenNipah Virus Infection: ImportanceSivaNoch keine Bewertungen
- CT Mbbs by DR ShamolDokument197 SeitenCT Mbbs by DR ShamolSiva Sandeep Chennimalai50% (2)
- Friesen C4ST Amended Input HC Safety Code 6 - 140 Omitted Studies 224pDokument224 SeitenFriesen C4ST Amended Input HC Safety Code 6 - 140 Omitted Studies 224pSeth BarrettNoch keine Bewertungen
- Asphyxia 2Dokument55 SeitenAsphyxia 2api-19916399100% (1)
- Note GuideDokument2 SeitenNote GuideDemetrius Hobgood0% (1)
- The Physiological Changes of PregnancyDokument16 SeitenThe Physiological Changes of PregnancycchaitukNoch keine Bewertungen
- Great Andamanese Lexicon EnglishDokument65 SeitenGreat Andamanese Lexicon EnglishSai VenkateshNoch keine Bewertungen
- Minnesota State High School LeagueDokument2 SeitenMinnesota State High School Leagueapi-301794844Noch keine Bewertungen
- Breast Care in BreastfeedingDokument11 SeitenBreast Care in BreastfeedingBella Cy LopezNoch keine Bewertungen
- Blake VegliaDokument4 SeitenBlake Vegliaapi-400338931Noch keine Bewertungen
- Talasemia de HB S y Talasemia de HB CDokument10 SeitenTalasemia de HB S y Talasemia de HB CAlejandra NúñezNoch keine Bewertungen
- CiprofloxacinDokument2 SeitenCiprofloxacinNika Joy Cabrera AlarconNoch keine Bewertungen
- Chest RadiographyDokument65 SeitenChest RadiographyMunish Dogra100% (1)
- BSCI 4001 Transcript MidtermDokument4 SeitenBSCI 4001 Transcript MidtermLynell Caraang BarayugaNoch keine Bewertungen
- Follow Site Quarantine ProceduresDokument67 SeitenFollow Site Quarantine ProceduresJohn James100% (3)
- Annotated BibliographyDokument31 SeitenAnnotated BibliographyLara MelissaNoch keine Bewertungen
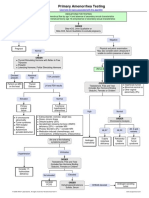
- Primary Amenorrhea Testing AlgorithmDokument1 SeitePrimary Amenorrhea Testing AlgorithmGabriella AguirreNoch keine Bewertungen
- Glossary English - Romanian Medical TermsDokument4 SeitenGlossary English - Romanian Medical TermsGhita Geanina0% (1)