Beruflich Dokumente
Kultur Dokumente
Single Visit Root Canal Treatment: Review
Hochgeladen von
Ricky Ferdian Raja0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
48 Ansichten0 SeitenSingle Visit Root Canal Treatment
Copyright
© Attribution Non-Commercial (BY-NC)
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenSingle Visit Root Canal Treatment
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
48 Ansichten0 SeitenSingle Visit Root Canal Treatment: Review
Hochgeladen von
Ricky Ferdian RajaSingle Visit Root Canal Treatment
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 0
80 Saudi Endodontic Journal May-Aug 2012 Vol 2 Issue 2
Address for correspondence:
Dr. Mothanna Al-Rahabi,
Department of Operative Dentistry
and Endodontics, College of Dentistry,
Taibah University, Al-madinah
Al-munawwrah, Kingdom of Saudi Arabia
E-mail: dr.rahabi@yahoo.com
Single visit root canal treatment: Review
Mothanna Al-Rahabi, Abdul Mujeeb Abdulkhayum
Department of Operative Dentistry and Endodontics, College of Dentistry, Taibah University,
Kingdom of Saudi Arabia
INTRODUCTION
O
ver the past decade, nickel titanium
rotary instrumentation, more reliable apex
locators, ultrasonics, microscopic endodontics,
digital radiography, newer obturation systems,
and biocompatible sealing materials have
helped practitioners perform endodontic
procedures more effectively and efficiently than
ever before.
All of these advances increase the incidence of
single-visit Endodontics in the dental clinics and the
rational for this treatment regime are less stressful and
only one anesthesia is needed, which makes it very
well accepted by the patient, less time-consuming,
reduces the risk of inter-appointment contaminations,
less expensive and more productive for the clinician.
Numbers of questions have been raised regarding
the one visit endodontics:
Is the same outcome achieved when we used
single visit regime rather than multiple visit for
the most of the cases?
Is the healing rate is the same in Single and
multiple-visit endodontic treatment for infected
root canals?
Are there any differences between single
and multiple-visit endodontic treatment in
post-obturation pain?
The purpose of this paper is to review some
arguments that are the basis for the effciency and
reliability of single visit root canal treatment.
Treatment protocol differences between single and
multiplevisit endodontic treatment
A major goal of nonsurgical root canal
treatment (NSRCT) is the prevention or treatment
of apical periodontitis, leading to the preservation
of natural teeth. The presence of bacteria inside
the root canal system results in the development
of periapical lesions.
[1]
Traditionally, root canal treatment was performed
in multiple visits, with the use of extra disinfecting
agents (intracanal dressing) besides the irrigants
that is used during the cleaning and shaping
procedure which mainly aims to reduce or
eliminate microorganisms and their by-products
from the root canal system before obturation.
[2]
The most intracanal dressing researched and widely
used is the calcium hydroxide (Ca(OH)
2
) paste.
[3]
Calcium hydroxide a strong alkaline substance,
Access this article online
Quick Response Code:
Website:
www.saudiendodj.com
DOI:
10.4103/1658-5984.108156
ABSTRACT
The main objective of performing root canal therapy is to eliminate bacteria
from the infected root canal system or remove infamed pulp tissue and
close it with a biologically acceptable flling material. If this treatment
managed well, regardless of the number of visits, it will create a favorable
environment for healing. The recent advances in Endodontic technology,
attracts the dental practitioners as well as the Endodontist to perform the
root canal treatment in one visit. The question that we consider in this
review article focuses on the long term prognosis of one-and multiple
appointment endodontic therapy for teeth with vital pulp, necrotic pulp, and
apical periodontitis.
Key words:
Apical periodontitis, multiple visit
root canal treatment, one-visit root
canal treatment, periapical healing,
postoperative pain
R
e
v
i
e
w
A
r
t
i
c
l
e
[Downloadedfreefromhttp://www.saudiendodj.comonFriday,May24,2013,IP:36.73.89.227]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Al-Rahabi and Abdulkhayum: Single visit root canal treatment
81 Saudi Endodontic Journal May-Aug 2012 Vol 2 Issue 2
which has a pH of approximately 12.5. In an aqueous
solution, Ca(OH)
2
dissociates into calcium and
hydroxide ions. The hydroxyl ion OH- is even smaller
and can penetrate through dentin to the cementum.
Calcium hydroxide works by a hydrolysis reaction in
which the OH-ion cuts protein chains and bacterial
endotoxin into pieces as it breaks chemical bonds. It
does this by inserting water molecules between the
carbon-carbon bonds (and breaking C-C bonds by
the process of hydrolysis), the backbone of proteins
and endotoxin. So if the pearls on a pearl necklace
represent atoms and the string between the pearls
represents C-C bonds, Ca(OH)
2
is like a pair of scissors
that cuts the string (hydrolyzes the bonds) between
the atoms breaking the protein down into harmless
non-functional pieces. It is a tissue solvent! It also kills
bacteria and it dissolves the endotoxin (bacterial LPS).
However Ca(OH)
2
was not capable of eliminating all
the bacteria, it helped to reduce the bacteria remaining
in the canal after the irrigation.
[3,4]
The concept of single visit root canal treatment is
based on the entombing theory,
[5]
which the large
number of microorganisms removed during cleaning
and shaping
[6,7]
and the remaining bacteria entombed
by the root canal obturation, therefore it will miss the
essential elements to be survive nutrition and space.
[8-10]
In addition, the antimicrobial activity of the sealer or
the zinc (Zn) ions of gutta-percha can kill the residual
bacteria.
[11,12]
Microbiological basis for endodontic treatment
Carefully conducted electron microscopic studies have
indicated that it is from within the confines of the
root canal system that bacteria initiate and maintain
periapical pathosis.
[13-16]
An advanced anaerobic bacteriological technique has
been conducted by S JGREN
[17]
to investigate the role
of infection in the prognosis of endodontic therapy
by following-up teeth that had had their infected
canals were cleaned and obturated during a single
appointment. Post-instrumentation samples were taken
and the teeth were then root-filled during the same
appointment. The teeth were followed for 5 years. They
detected a number of bacteria in 22 of 55 root canals.
Complete periapical healing occurred in 94% of cases
that yielded a negative culture. They concluded that
their fndings emphasize the importance of completely
eliminating bacteria from the root canal system before
obturation. They add that this objective cannot be
reliably achieved in a one-visit treatment because it is
not possible to eradicate all infection from the root
canal without the support of an inter-appointment
antimicrobial dressing.
Several reports have further drawn attention to the
possibility that some bacterial species may establish
themselves in the body of the infammatory process.
Tronstad et al.
[18]
examined eight asymptomatic
periapical infammatory lesions which were refractory
to conventional endodontic therapy in the presence of
bacteria. Access to the periapical lesions was gained
using an aseptic surgical technique. Microbiological
samples were taken from the soft tissue lesions
and the surface of the root tips. The samples were
processed using a continuous anaerobic technique.
Bacterial growth was evident in all samples. Two lesions
exclusively yielded anaerobic bacteria and 5 lesions were
heavily dominated by anaerobes. Their fndings clearly
showed that anaerobic bacteria are able to survive and
maintain an infectious disease process in periapical
tissues.
Similar fndings were reported by Sunde et al.
[19]
in situ
hybridization with probes specifc for the domain of
bacteria and speciesspecifc probes, including techniques
for spatial distribution.
The pulps of teeth with apical periodontitis harbored
high levels of LPS, and speculated this may be
a mechanism by which bacteria produce the apical
lesion.
[20]
The bacterial metabolites and breakdown
products playing a signifcant role in the pathogenesis
of apical periodontitis.
[21]
Status of the pulp
In an infected vital pulp due to a caries exposure the
infection is normally found only at the wound surface,
where it has resulted in a localized inflammatory
response. This means that more apically, and in
particular in the most apical portion of the tissue,
bacterial organisms are usually not present.
[22]
The aim
of root canal treatment in this case is to maintain
sterile apical conditions in order to optimize the healing
potential. On the other hand an infected necrotic
pulp produces an apical infammatory lesion and the
aim of root canal treatment in is to eliminate the
microorganisms from the canal to promote healing of
apical periodontitis.
[Downloadedfreefromhttp://www.saudiendodj.comonFriday,May24,2013,IP:36.73.89.227]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Al-Rahabi and Abdulkhayum: Single visit root canal treatment
82 Saudi Endodontic Journal May-Aug 2012 Vol 2 Issue 2
Bacterial elimination
Debridement of the root canal by instrumentation
and irrigation is considered the most important
single factor in the prevention and treatment of
endodontic diseases and there is a general agreement
that the successful elimination of the causative agents
in the root canal system is the key to health.
[23]
Sodium
hypochlorite (NaOCl) irrigation plus mechanical
instrumentation rendered 33% of the canals
bacteriafree after the frst appointment.
[24]
Even with
the most modern instrumentation techniques (using
of a rotary instrumentation technique) attainment of
complete bacterial elimination would be farfetched.
[6,25,26]
Although irrigation with NaOCl provides a number
of features attractive to root canal therapy, it appears
that it is not possible to attain complete bacterial
elimination by this adjunctive measure. Therefore
intracanal medication, specially calcium hydroxide,
has been widely used in attempts to kill any bacteria
remaining after instrumentation and irrigation. The
effectiveness of Ca(OH)
2
in completely removing
bacteria in infected root canals in less than 4 weeks is
under debate.
[27-29]
Although the use of intracanal medication will lower
the bacterial count in infected root canals, it fails to
obtain the total elimination of bacterial organisms on
a consistent basis.
[30,31]
Bacterial endotoxins elimination
The objective of root canal treatment on necrotic
teeth should be not only the elimination of living
bacteria but also the inactivation of the toxic effects
of bacterial endotoxins. The lipopolysaccharide (LPS),
is a powerful endotoxin capable of having a strong
toxic action over the periapical tissues.
[32,33]
LPS is
released during disintegration, multiplication, or
bacterial death and is capable of penetrating into the
periradicular tissues, acting as endotoxin in the host
organism and leading to periradicular inflammation
and bone destruction. The lipid A is the bioactive
component of LPS responsible for the majority of
the immunoresponse.The accumulation of bacteria
components in an infected area, particularly
endotoxins (including lipoteichoic acid, peptidoglycan,
lipopolysaccharide, and others), can stimulate the release
of proinflammatory cytokines by different cell lines
through TLR2 and -4 activation. The inflammatory
tissue present in periradicular lesions is populated
predominantly by a macrophage, which is the major
source of interleukin-1b (IL-1b), and almost the
exclusive producer of tumor necrosis factor a (TNF-a)
in the presence of bacteria or LPS.
[34,35]
The irrigation solutions were ineffective against LPS,
while the intracanal medication dressing with Ca(OH)
2
appeared to inactivate the cytotoxic effects of the
endotoxin.
[33,36]
Khan et al.
[37]
tested the hypothesis that Ca(OH)
2
denatures IL-1 alpha, TNF-alpha, and CGRP. Human
IL-1 alpha (0.125 ng/mL), TNF-alpha (0.2 ng/mL),
and CGRP (0.25 ng/mL) were incubated with
Ca(OH)
2
(0.035 mg/mL) for 1-7 days. At the end
of the incubation period, the pH of the samples
was neutralized, and the concentrations of the
mediators were measured by immunoassays. The
analyzed data indicated that Ca(OH)
2
denatures IL-1
alpha, TNF-alpha, and CGRP by 50-100% during
the testing periods (P < 0.001). They concluded that
denaturation of these proinflammatory mediators is
a potential mechanism by which Ca(OH)
2
contributes
to the resolution periradicular periodontitis.
Postoperative pain
Postoperative or intraoperative flare-up and pain are
often the measure of the success or failure of single
visit treatment, although pain during treatment has
been proved to have no effect on long-term outcomes.
Postoperative pain at the mild level is common in
root canal treatment which may be the result of
overinstrumentation, overflling, passage of medicine
or infected debris into the periapical tissues, damage of
the vital neural or pulp tissues or central sensitization.
[14]
The preponderance of the research to date has shown
no signifcant difference in postoperative pain has been
found when one-visit RCT was compared with two-visit
treatment, especially in teeth with vital pulps.
[9,13,38-41]
Healing rate of singleversus multiplevisit endodontic
treatment for infected root canals
The simplest way to compare both treatment options
is to analyze them using a healed or not healed
outcome. The short- or long-term follow-up of the
bone radiographic image and size of the lesion is the
most commonly used technique to evaluate the healing,
usually based on the PAI score developed by Orstavik
et al.
[42]
The number of studies that compare both
techniques for a legitimate and credible follow-up time
are not many compared to the mature evidence base
that supports the using or not of intracanal medicines.
[4]
[Downloadedfreefromhttp://www.saudiendodj.comonFriday,May24,2013,IP:36.73.89.227]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Al-Rahabi and Abdulkhayum: Single visit root canal treatment
81 Saudi Endodontic Journal May-Aug 2012 Vol 2 Issue 2
Numerous studies evaluating the effectiveness of
single-versus multiple-appointment root canal treatment
have been published, which reported no significant
differences in effectiveness (healing rates) between these
two treatment regimens.
[14,43-45]
Unfortunately, endodontic
treatment success is often poorly defned. As mentioned
earlier, postoperative or intraoperative fareup and pain
were the only measure of the success or failure used to
evaluate single visit treatment. According to Spangberg;
[46]
Clinical treatment results can be compared by following a
clearly defned criteria for successful outcome or failure.
CONCLUSION
In dentistry and medicine the standard by which
treatment methods are compared is the long-term
outcome.
[47]
The aim of the endodontic therapy
to achi eve the resol uti on of the di sease means
elimination of the etiology, which means elimination
of bacteria. Therefore every time we can get free
microorganisms canals we can perform single visit
root canal treatment. Based on the reports presented
in this over view, the canals with vital pulps can
in principle be regarded as free of bacteria at the
initiation of treatment. Thus, provided a strict aseptic
technique is utilized and enough time is available for
all treatment steps to be performed optimally, the
permanent flling of the canal may take place on the
frst visit.
In teeth with necrotic pulp and apical periodontitis
and with the complex anatomy of teeth and root
canals creates an environment that is a challenge to
the complete cleansing in single visit therefore the
multiple appointment procedure maybe is more
effectiveness to achieve more bacteria negative
Canals.
[30,48]
In addition to killing bacteria, intracanal
medicaments may have other beneficial functions.
Calcium hydroxide neutralizes the biological activity
of bacterial lipopolysaccharide
[36,49]
and makes necrotic
tissue more susceptible to the solubilizing action of
NaOCl at the next appointment. Regardless of the
number of sessions, an effective bacteriological control
is mandatory. The biologic concerns should always be
a priority.
REFERENCES
1. Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of
surgical exposures of dental pulps in germ-free and conventional
laboratory rats. Oral Surg 1965;20:340-9.
2. Sjogren U, Figdor D, Spangberg L, Sundqvist G. The
antimicrobial effect of calcium hydroxide as a short-term
intracanal dressing. Int Endod J 1991;24:119-25.
3. Law A, Messer H. An evidence-based analysis of the
antibacterial effectiveness of intracanal medicaments. J Endod
2004;30:689-94.
4. Sathorn C, Parashos P, Messer H. Antibacterial efficacy of
calcium hydroxide intracanal dressing: a systematic review and
meta-analysis. Int Endod J 2007;40:2-10.
5. Peters LB, Wesselink PR, Moorer WR. The fate and the role of
bacteria left in root dentinal tubules. Int Endod J 1995;28:95-9.
6. Shuping G, rstavik D, Sigurdsson A, Trope M. Reduction of
intracanal bacteria using Nickel-titanium rotary instrumentation
and various medications. J Endod 2000;26:751-5.
7. Dalton BC, Orstavik D, Phillips C, Pettiette M, Trope M.
Bacterial reduction with nickel-titanium rotary instrumentation.
J Endod 1998;24:763-7.
8. Oliet S. Single-visit endodontics: a clinical study. J Endod
1983;9:147-52.
9. Soltanoff W. A comparative study of the single-visit and the
multiple visit endodontic procedure. J Endod 1978;4:278-81.
10. Weiger R, Rosendahl R, Lost C. Influence of calcium
hydroxide intracanal dressings on the prognosis of teeth
with endodontically induced periapical lesions. Int Endod J
2000;33:219-26.
11. Moorer WR, Genet JM. Evidence for antibacterial activity of
endodontic gutta-percha cones. Oral Surg 1982;53:503-7.
12. Siqueira JF, Favieri A, Gahyva SM, Moraes SR, Lima KC,
Lopes HP. Antimicrobial activity and flow rate of newer and
established root canal sealers. J Endod 2000;26:274-7.
13. El Mubarak AH, Abu-bakr NH, Ibrahim YE.
Postoperative Pain in Multiple-visit and Single-visit Root
Canal Treatment. J Endod 2010;36:36-9.
14. Figini L, Lodi G, Gorni F, Gagliani M. Single versus multiple
visits for endodontic treatment of permanent teeth: A Cochrane
systematic review. J Endod 2008;34:1041-7.
15. Nair PN. Light and electron microscopic studies of root canal
flora and periapical lesions. J Endod 1987;13:29-39.
16. Molven O, Olson I, Kerekes K. Scanning electron microscopy
of bacteria in the apical part of root canals in permanent teeth
with periapical leisons. Endod Dent Traumatol 1991;7:226-9.
17. Sjgren U, Figdor D, Persson S, Sundqvist G. Influence of
infection at the time of root filling on the outcome of endodontic
treatment of teeth with apical periodontitis. Int Endod J
1997;30:297-306.
18. Tronstad L, Barnett T, Riso K, Slots J. Extraradicular
endodontic infections. Endod Dent Traumatol 1987;3:86-90.
19. Sunde PT, Olsen I, Eribe ER, Moter A, Tronstad L. Bacteria
of asymptomatic periapical endodontic lesions identified by
anaerobic cultivation and genetic methods. Int Endod J
2002;35:79.
20. Schein B, Schilder H. Endotoxin content in endodontically
involved teeth. J Endod 1975;1:19-21.
21. Yamasaki M, Kumazawa M, Kohsaka T, Nakamura H,
Kameyama Y. Pulpal and periapical tissue reactions after
experimental pulpal exposure in rats. J Endod 1994;20:13-7.
22. Mller AJ, Fabricius L, Dahle' n G, Heyden G. Influence
on periradicular tissues of indigenous oral bacteria and
necrotic pulp tissue in monkeys. Scand J Dent Res 1981;89:
475-84.
23. Chugal NM, Clive JM, Spangberg LS. A prognostic model for
assessment of the outcome of endodontic treatment: Effect of
biologic and diagnostic variables. Oral Surg Oral Med Oral Pat
Oral Radiol Endod 2001;91:342-52.
24. Bystrm A, Sundqvist G. Bacteriologic evaluation of the effect
of 0.5 percent sodium hypochlorite in endodontic therapy. Oral
Surg Oral Med Oral Pathol 1983;55:307-12.
[Downloadedfreefromhttp://www.saudiendodj.comonFriday,May24,2013,IP:36.73.89.227]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Al-Rahabi and Abdulkhayum: Single visit root canal treatment
84 Saudi Endodontic Journal May-Aug 2012 Vol 2 Issue 2
25. Nair PN, Henry S, Cano V, Vera J. Microbial status of
apical root canal system of human mandibular first molars
with primary apical periodontitis after one-visit endodontic
treatment. Oral Surg Oral Med Oral Pat Oral Radiol Endod
2005;99:231-52.
26. Jorge V, Siqueira JF, Ricucci D, Loghin S, Fernez N, Flores B,
et al. One- versus Two-visit Endodontic Treatment of Teeth
with Apical Periodontitis: A Histobacteriologic Study. J Endod
2012;38:1040-52.
27. Reit C, Molander A, Dahle' n G. The diagnostic accuracy
of microbiolgic root canal sampling and the influence of
antimicrobial dressings. Endod Dent Traumatol 1988;15:278-83.
28. Barbosa CA, Goncalves RB, Siquera Jr JF, DeUzeda M.
Evaluation of the antimicrobial activities of calcium hydroxide,
chlorhexidine, and camphorated paramonochlorophenol as an
intracanal medicament. A clinical and laboratory study. J Endod
1997;23:297-300.
29. rstavik D, Kerekes K, Molven O. Effects of extensive apical
reaming and calcium hydroxide dressing on bacterial infection
during treatment of apical periodontitis: A pilot study. Int
Endod J 1991;24:1-7.
30. Molander A, Reit C, Dahlen G. The antimicrobial effect of
calcium hydroxide in root canals pretreated with 5% iodine
potassium iodide. Endod Dent Traumatol 1999;15:205-9.
31. Engstrm B, Hard AF, Segerstad L, Ramstrm G, Frostell G.
Correlation of positive cultures with the prognosis for root canal
treatment. Odontol Revy 1964;15:257-70.
32. Safavi KE, Nichols FC. Alteration of biological properties of
bacterial lipopolysaccharides by calcium hydroxide treatment.
J Endod 1994;20:127-9.
33. Martinho FC, Gomes B. Quantification of endotoxins and
cultivable bacteria in root canal infection before and after
chemomechanical preparation with 2.5% sodium hypochlorite.
J Endod 2008;34:268-72.
34. Tanomaru JM, Leonardo MR, Tanomaru Filho M, Bonetti
Filho I, Silva LA. Effect of different irrigation solutions and
calcium hydroxide on LPS. Int Endod J 2003;36:733-9.
35. Lim GC, Torabinejad M, Kettering J, Linkhardt TA,
Finkelman RD. Interleukin 1 b in symptomatic and asymptomatic
human perirradicular lesions. J Endod 1994;20:225-7.
36. Hong CY, Lin SK, Kok SH, Cheng SJ, Lee MS, Wang TM,
et al. The role of lipopolysaccharide in infectious bone resorption
of periapical lesion. J Oral Pathol Med 2004;33:162-9.
37. Khan AA, Sun X, Hargreaves KM. Effect of calcium hydroxide
on proinflamatory cytokines and neuropeptides. J Endod
2008;34:1360-3.
38. Roane JB, Dryden JA, Grimes EW. Incidence of postoperative
pain after single- and multiple-visit endodontic procedures. Oral
Surg 1983;55:68-72.
39. Al-Negrish AR, Habahbeh R. Flare up rate related to root
canal treatment of asymptomatic pulpally necrotic central
incisor teeth in patients attending a military hospital. J Dent
2006;34:635-40.
40. Albashaireh ZS, Alnegrish AS. Postobturation pain after
single- and multiple-visit endodontic therapy. A prospective
study. J Dent 1998;26:227-32.
41. Eleazer PD, Eleazer KR. Flare-up rate in pulpally necrotic
molars in one-visit versus two-visit endodontic treatment.
J Endod 1998;24:614-6.
42. Orstavik D, Kerekes K, Eriksen HM. The periapical index:
A scoring system for radiographic assessment of apical
periodontitis. Endod Dent Traumatol. 1986;2:20-34.
43. Sathorn C, Parashos P, Messer H. The prevalence of postoperative
pain and flare-up in single- and multiple-visit endodontic
treatment: A systematic review. Int Endod J 2008;41:91-9.
44. Vince A. Penesis, Outcome of One-visit and Two-visit endodontic
treatment of necrotic teeth with apical periodontitis: A randomized
controlled trial with one-year Evaluation. J Endod 2008;34:251-7
45. Su Y, Wang C, Ye L. Healing rate and post-obturation pain of
single- versus multiple-visit endodontic treatment for infected
Rootcanals: A systematic review. J Endod 2011;37:125-32.
46. Spangberg L. Evidence-based endodontics: The one-visit
treatment idea. Oral Surg Oral Med Oral Pat Oral Radiol
Endod 2001;91:617-8.
47. Trope M, Bergenholtz G. Microbiological basis for endodontic
treatment: can a maximal outcome be achieved in one visit?
Endod Top 2002;1:40-53.
48. Sjgren U, Figdor D, Spangberg L, Sundqvist G. The
antimicrobial effect of calcium hydroxide as a short-term
intracanal dressing. Int Endod J 1991;24:119-25.
49. Safavi KE, Nichols FC. Effect of calcium hydroxide on bacterial
lipopolysaccharide. J Endod 1993;19:76-8.
How to cite this article: Al-Rahabi M, Abdulkhayum AM. Single visit
root canal treatment: Review. Saudi Endod J 2012;2:80-4.
Source of Support: Nil. Confict of Interest: None.
[Downloadedfreefromhttp://www.saudiendodj.comonFriday,May24,2013,IP:36.73.89.227]||ClickheretodownloadfreeAndroidapplicationforthisjournal
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Summer Internship ReportDokument103 SeitenSummer Internship ReportChandan Srivastava100% (4)
- Med Surge 2 - RESP SYSTEM NOTESDokument26 SeitenMed Surge 2 - RESP SYSTEM NOTESlorrainenxumalo75% (4)
- S1 Hippocratic Oath Seminar and Reading NotesDokument7 SeitenS1 Hippocratic Oath Seminar and Reading NotesTaraSubba1995Noch keine Bewertungen
- Product CatalogDokument13 SeitenProduct Catalogkleos70Noch keine Bewertungen
- Development and Validation of The Theistic Spiritual Outcome SurveyDokument14 SeitenDevelopment and Validation of The Theistic Spiritual Outcome SurveyMircea PocolNoch keine Bewertungen
- NewDokument58 SeitenNewAkhil SoodNoch keine Bewertungen
- Wintobootic2mockboard Exam - Social Work CounselingDokument4 SeitenWintobootic2mockboard Exam - Social Work CounselingATLASNoch keine Bewertungen
- Castlegar/Slocan Valley Pennywise November 21, 2017Dokument42 SeitenCastlegar/Slocan Valley Pennywise November 21, 2017Pennywise PublishingNoch keine Bewertungen
- Pulse OximetryDokument16 SeitenPulse OximetryDineshkumarNoch keine Bewertungen
- Physical Education Class 12 Short Answers Chapter 3Dokument7 SeitenPhysical Education Class 12 Short Answers Chapter 3Anushka TomarNoch keine Bewertungen
- Eyelid Surgery Los AngelesDokument2 SeitenEyelid Surgery Los AngelesVeronica HinmanNoch keine Bewertungen
- The Dangers of CrammingDokument2 SeitenThe Dangers of CrammingIntan Shafira RachmadhiniNoch keine Bewertungen
- EGYPT Registered Products Update 22-10-09 1Dokument103 SeitenEGYPT Registered Products Update 22-10-09 1Anuj MairhNoch keine Bewertungen
- Models of SupervisionDokument10 SeitenModels of SupervisionFarhan KhalidNoch keine Bewertungen
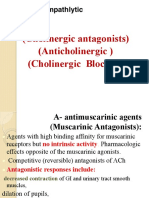
- AnticholinergicsDokument34 SeitenAnticholinergicskityamuwesiNoch keine Bewertungen
- Tips of Operations - VAC TherapyDokument32 SeitenTips of Operations - VAC TherapyRandika PereraNoch keine Bewertungen
- Therapeutic Gases 9.3.17 and CoughDokument29 SeitenTherapeutic Gases 9.3.17 and CoughThor O100% (1)
- 2005 - Stavridakis - Immediate Dentin Sealing of Onlay Preparations - Thickness of Pre-Cured Dentin Bonding Agent and Effect of Surface CleaningDokument11 Seiten2005 - Stavridakis - Immediate Dentin Sealing of Onlay Preparations - Thickness of Pre-Cured Dentin Bonding Agent and Effect of Surface CleaningAndreea BorislavschiNoch keine Bewertungen
- Insulin IndexDokument13 SeitenInsulin IndexbookbookpdfNoch keine Bewertungen
- Mental Health Disorders Nclex Nursing ResourcesDokument79 SeitenMental Health Disorders Nclex Nursing ResourcesSadako100% (1)
- CPG - Whiplash Associated DisordersDokument74 SeitenCPG - Whiplash Associated DisordersGumDropNoch keine Bewertungen
- Ancient Mesopotamia Medicine HistoryDokument4 SeitenAncient Mesopotamia Medicine HistoryJhhhcfNoch keine Bewertungen
- Calcium HoaxDokument40 SeitenCalcium HoaxpuravNoch keine Bewertungen
- Discipline of CounsellingDokument16 SeitenDiscipline of CounsellingJeffrey de LeonNoch keine Bewertungen
- Mnemonic DeviceDokument12 SeitenMnemonic DeviceJonathan ObañaNoch keine Bewertungen
- Garcinia Cambogia MonographDokument5 SeitenGarcinia Cambogia Monographeddee90Noch keine Bewertungen
- Coagulation DisordersDokument26 SeitenCoagulation DisordersLia pramita0% (1)
- Direct Anterior Total Hip ArthroplastyDokument13 SeitenDirect Anterior Total Hip Arthroplasty21701101006 Rosita SariNoch keine Bewertungen
- SpinalinjuryDokument29 SeitenSpinalinjurymustikaNoch keine Bewertungen
- Primary ImmunodeficienciesDokument4 SeitenPrimary Immunodeficienciesnayd dsNoch keine Bewertungen