Beruflich Dokumente
Kultur Dokumente
Review of The TIG Fellowship Schemes 2013
Hochgeladen von
plastaukOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Review of The TIG Fellowship Schemes 2013
Hochgeladen von
plastaukCopyright:
Verfügbare Formate
Review of The TIG fellowship schemes
2013
JCST Review of the TIG Fellowship Schemes, 2013
Rowena Hitchcock, Andrew Robson, Gareth Griffiths
1|Page
Review of The TIG fellowship schemes
2013
Introduction Surgical practice has changed considerably since the establishment of nine (now 10) surgical specialties within the Royal Colleges of Surgeons. Many specialties have sub specialised both in their clinical practice and training patterns, however some areas of specialised practice have established input from more than one specialty. Over the last five years to facilitate training in these areas the interface training groups have been established in a pattern first used by the Hand Surgery training scheme 20 years ago. These training interface groups (TIG) have been administered by the JCST with group members reporting to the parent SACs and the fellowships managed by a lead Dean and funded by the DH/HEE. The purpose of the fellowship is to create the future leaders of our profession. Our aim is to make these fellowships the best in the world by allowing these selected trainees to witness other specialties caring for patients in their area of interest. They are also given an opportunity to develop their leadership and management skills and understand the role of a consultant in the modern NHS. To this extent they attend Cumberlege Connections Politics, Power and Persuasion course and a residential in common with the other 50+ trainees and faculty. The residential allows networking but also addresses leadership, finance, performance and litigation issues. Currently the underspend from the TIG funds is being utilised to give trainees study leave to the value of 1K and also pay for Cadaveric Courses in Breast Oncoplastic Surgery, Head and Neck Surgery and Cleft Lip and Palate.
Members of the JCST have discussed the scheme with each TIG which must be discussed separately although some themes have emerged.
The Posts
TIGS AND THEIR PARTICIPATING PARENT SPECIALTIES
Breast Cleft Hand Reconstruction cosmetic Head and Neck
Plastic Surgery Orthopaedic Surgery General Surgery ENT Ophthalmic Surgery
* *
* *
* * * *
2|Page
Review of The TIG fellowship schemes
2013
Oral and Maxillofacial Surgery (OMFS) Dermatology Paediatric Surgery
* (*)
The posts are managed by the lead Dean for TIG posts, Davinder Sandhu, and the Bristol PGMDE /HEE supports the governance process including selection. There are 2 to 3 TIG committee meetings per year. Until recently the trainees have been SPRs and appraisal was facilitated by portfolio assessment and trainer assessment forms, recent StR appointments are supported by ISCP during the pre-CCT period. Although nominally pre-CCT many are now in additional training time with a delay in CCT dates. There are curricula for these posts and these are under review in most specialties. The number of posts is adjusted from a funding pool by the Severn PGME to meet needs.
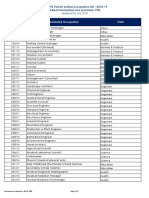
Training Interface Posts Duration Head and Neck Cleft Lip and Palate Reconstructive Cosmetic Breast Hand Appendix A 12 months 12-24 months 4/12
number of posts 7 of 12 funded 3
Number of centres 11 7
TIG committee meetings pa 2 2
On-call with parent specialty No No
15 of 18 funded 9 of 12 funded 10 of 13 funded
18
No
12 months 12 months
12 10
2 2
No Yes
Funding of posts (D Sandhu) In the past these posts had either national funding or local funding. Some units had a number of fellows and it was never clear who was the TIG fellow. Also, although there was a committee for Cosmetic Surgery there was no national funding for any training posts. One of the initiatives I was successfully able to undertake as Lead Dean was to return all local funded monies to the Trusts. Persuade every Strategic Health Authority to give up its TIG funding allocation to the Southwest SHA so that all the monies are centralised. As Lead Dean
3|Page
Review of The TIG fellowship schemes
2013
I and the senior associate director of finance of the SWSHA, became the responsible officer of this funding. In addition, I was able to get 6 WTE funding for Cosmetic Surgery at about 344K. This centralisation gave us the flexibility to use underspends for educational activities as well as support additional posts and absorb other cost pressures such as maternity leave and overlap of fellowships as predicted for 2013/14. Over the last 8 years there have been 4 additional posts funded in Head and Neck, 2 in Breast Oncoplastic, 1 in Hand Surgery and new fellowships have been created within the Cosmetic group in Trauma and Soft Tissue Reconstruction, Skin Cancer and Laser Therapy. The main source of the underspend is due to the fact that cleft numbers are tightly controlled nationally and often they do not appoint to their full allocation. I wish to pay credit to Simon Thompson, Senior Director of Finance for DH and responsible for the almost 5billion education budget for England who supported this initiative. One of the Head and Neck fellowships in Glasgow is funded by Scotland but all the others are funded by DH England even though the devolved nations all benefit. National selection All the TIG posts are appointed by national advertisement and selection, with committee members from each parent specialty represented during selection. This is facilitated by the Severn PGME but the JCST office collates Job Descriptions. To date the posts are appointed a. Longlist +/-shortlist b. Interview centre -national recruitment and person specification. Some TIGs are moving towards recruiting twice a year to be as inclusive as possible with respect to final fellowship exams.
The posts have been sought after with applications of 3-5:1 from NTNs, the application rates show no sign of diminishing, Appendix B. Applications are made in varying numbers from parent and other specialties. Selection figures suggest that appointments are proportional to applications except that applicants from plastics do disproportionally well in Cosmetic but less well in Breast Oncoplastic interviews. Involvement of parent specialties in selection is maintained in all TIGs, however with involvement in so many TIGs Plastic Surgery may have difficulty supplying an equal number of selectors to each group. There has been disquiet in Breast Oncoplastic and to a lesser extent in Head and Neck about disproportionately low number of Plastic Surgery trainees being selected.
There has been a thorough investigation into Breast Oncoplastic national selection appendix C.
4|Page
Review of The TIG fellowship schemes
2013
To date there has been no evidence of bias and the way forward may be to have a portfolio station with an agreed weighting. Plastic Surgery feel this would give due recognition of the achievements of their trainees. There has been concern expressed that a Plastic Head and Neck trainee who was successful in all other stations was not appointed because in one station his attitude was felt not to be consistent with someone holding a TIG fellowship. This trainee was also spending a year at a top institute in Taiwan and it was felt that there would be little gain for him to repeat this type of fellowship.(D Sandhu) Interview with the patient representative, Ursula Van Mann, to the recent national selection episodes in General Surgery and Plastic Surgery suggest that she was not aware of any issues between the general and plastic surgical consultants present and did not see any evidence of bias based on specialty. Curriculum and Assessment There is a defined curriculum either within the take or host specialty curriculum developed by the committee and approved by the GMC. The curricula are being actively reviewed in several specialties. The trainee representatives however report lack of clarity of expected curriculum and outcome measures. This may be improved as StRs replace SpRs as they have better working knowledge of curricula and use workplace based assessments against them. Apart from Cosmetic Surgery which are only 4 months duration the rest of the fellowships are for one year and Cleft often goes onto a second year. For most fellowships the host Deanery normally carries out the ARCP process and the TPD from the parent/donor PGME is invited to attend. There is the option for the ARCP process to be carried out by the parent PGME rather than the host Deanery, particularly in the rare case of an unsatisfactory outcome. In Cosmetic Surgery there is an end of placement report. All these fellowships (except Cosmetic Surgery) are out of programme and normally the CCT date is extended. Governance and Outcomes of Training The TIG STC committees are drawn from parent specialists within the TIG recognised centres and contribute enormously to the running of these fellowships and have built a close liaison with Severn Postgraduate Medical Education. Breast Oncoplastic have a patient member on the committee, the others do not. The overall responsibility for governance however lies with the Severn PGME and appears to be managed with great expertise and enthusiasm by Davinder Sandhu. The SAC chairs or other members should act as liaison and members of the committee but attendance from some specialties in some TIGs has been poor, appendix E. There are different Terms of Reference for all TIGs.
5|Page
Review of The TIG fellowship schemes
2013
The donor deanery is responsible for management of unsatisfactory annual assessment outcomes but these are rare given the highly selected group involved. Certificates of completion of a fellowship are under review but are given at the end of some fellowships either by SAC or TIG committee- they currently reflect solely a completed period of training rather than competence.
6|Page
Review of The TIG fellowship schemes
2013
Discussion of Individual Fellowship Programmes
Each Author led discussions with stakeholders but interviews often crossed several TIGs and so contributions were made by all authors.
Breast Onco-Plastic Reconstruction
Rowena Hitchcock Sept 2013, Discussions with trainee representatives, patient representative, Mark Henley, Anne Tansley, Chris Caddy, Kieran Horgan , Davinder Sandhu, Aiden Fitzgerald, Megan Warde
These posts were set up to improve breast surgery and training in the face of 400 vacancies 12 years ago. There are 9-12 Breast Oncoplastic fellowships in originally 18 centres (now largely 12) these are managed by the TIG STC which meets twice a year, attendance at these meetings has been variable. Recently Plastic Surgery representatives have been largely unable to attend. Plastic Surgery and General Surgery have equal representation and posts are open to both specialties trainees. The trainees are given extra training time to complete the fellowship with delayed CCT and are assessed by the local trainer with reference to the trainees donor STC supported by the Severn Deanery. Recent changes to the CCT requirements of General Surgery include 6 years on call and may require a whole year extension of CCT date. Some feel that there is a Nottingham London centric axis raising the possibility of reassigning training centres. There are 3 sought after international fellowships running parallel to the TIGs
AIMS The aim of training and expected range of outcome skills is not clear to all the
interviewed contributors. Whilst the TIG chair expects a training period to develop the oncology and MDT skills of Plastic Surgery trainees and the reconstructive skills of General Surgery trainees others have of an expectation of homogenous training based on comparable starting skills. Some expect to develop an all- round breast surgeon with universal skills whilst others expect trainees to enter and leave with a specialty specific sub set of skills to match niche needs in the workforce. The General Surgery trainees can expect to complete a repertoire of reconstructive skills but not free flap microvascular work. Whilst the Plastic Surgery trainees with these skills learn a greater knowledge of oncology, ablative surgery and MDT working but not enough to be perceived to have homogenous ablative and oncology skills of the majority of breast unit consultants, indeed a Trust recently refused to consider the application of a Plastic Surgery Breast Oncology fellow for a consultant post.
7|Page
Review of The TIG fellowship schemes
2013
It should be recognised that some Plastic Surgical trainees are aiming at general Plastic Surgery consultant posts but with support to a breast unit or private breast aesthetic roles. Microvascular skills require high through put to maintain and represent a small percentage of breast unit activity and whilst the additional reconstructive skills of a Plastic Surgerytrained breast surgeon are useful, only a small number of microvascular work posts can be expected within regional reconstructive. It has been suggested that if Plastic Surgical trainees are to gain better access to TIG selection and subsequent consultant roles then there would need to be a development of Plastic Surgery oncology modular training so that pre-fellowship training better matches permitting similar outcome objectives. The alternative is to set aside a subset of posts requiring established reconstructive skills to develop a workforce matched number of microvascular skilled reconstructive surgeons.
Selection is largely from final year trainees who have passed at least the first part and
recently the second part of the exam. There are matching long and shortlisting criteria for both specialties and attempts have been made to make the interviews generic. Although initially few plastic surgeons applied this has increased lately but few have been successful. It seems likely that late specialisation within Plastic Surgical training leaves trainees unable to match up to general surgeons who elect early for a Breast Surgery career with tailored training posts, research audit etc. Attempts have been made to adjust criteria to value Plastic Surgery skills but this has less effect at interview where interview skills come to fore: General Surgery trainees help each other, seek advice practice mammary fold trainee group A detailed review of the selection process has demonstrated no significant issues with the process- appendix C. Opinions vary as to whether there should be specific posts for those with Plastic Surgical skills or whether Plastic Surgery trainees should prepare longer and better for selection using matching entry criteria.
Quality of Posts
All interviewees agreed that the fellowship posts represented excellent training and should continue to be supported. The trainee representative suggested that the fellowships were well appreciated and thought to be excellent training although she suggested that the educational supervisors were not clear as to the curriculum and outcomes of the training period.
Assessment & credentialing : This would appear to be a generic area for discussion amongst the TIGs but is marked in Breast Oncology given the lack of homogeneity of outcome skills. The University of East Anglia offers a distance learning MS in Breast Oncology which many trainees have taken during or before selection.
8|Page
Review of The TIG fellowship schemes
2013
Conclusion
It becomes clear that the training needs and expectations of the General Surgery and Plastic Surgery trainees are not the same and that the roles of a Plastic and General surgeon within a breast unit are different. The detailed investigation performed by Davinder Sandhu suggests that the appointment process was transparent and fair. However, it may be that there is indirect discrimination against the plastic surgical trainees since the selection process and TIG post would seem to better fit with the aspirations of the general surgeon than the plastic surgical trainee. It is also possible that Breast Surgery may be significantly more popular for women in General Surgery whilst in Plastic Surgery other options are more popular. Focussed post CCT microsurgery breast fellowships are an option. Discussion with TIG committee members and trainees suggest that the pre- selection support given to general surgical trainees is greater than that given to plastic surgical trainees and that this contributes to the differential application and success rate of trainees. Hearsay would suggest that the general surgical trainees are well organised and support each other in the process of preparing for the fellowship applications such applicants are therefore motivated knowledgeable and prepared whilst the plastic surgical trainees are less supported. Action points 1. The Breast Oncoplastic TIG should consider a. Composition of the TIG committee, b. Review/ expansion of training centres whether the post design, duration, curriculum, person specification, and selection processes should be the same for both parent specialties. c. Developing pre-application support for interested surgical trainees should be organised, particularly for the plastic surgical trainees to develop interest early in training d. Clear outcomes should be defined for all posts and certification of competences or meritorious completion considered.
2. The JCST should a. Consider the appointment of a neutral TIG chairman. b. Set up a working group including representatives from the TIG committee, British Plastic and Reconstructive Aesthetic surgeons and Association of Breast Surgeons i. consider workforce needs
ii. review the aims of the TIGs and single/modular curricula iii. support the TIG on the post design, duration, curriculum , person specification, and selection processes iv. Decide whether selection should: be based on ability not previous breast experience eg all papers , audits etc not breast related which clearly favours General Surgery trainees who would apply with 2 years breast training,
9|Page
Review of The TIG fellowship schemes
2013
or allow workforce need equated sub-allocation of the fellowship posts should be instigated ie 1:4 posts allocated to Plastic Surgery trainees.
10 | P a g e
Review of The TIG fellowship schemes
2013
Head and Neck TIG
Gareth Griffiths August 2013 Summary of discussion with Bob Woodwards, Chair of the Head and Neck TIG
The fellowships are aimed at giving trainees a good understanding of what all specialties involved in H&N work can offer.. The aim is not to create a single unified H&N surgeon, but to give H&N surgeons based in each of the parent specialties of ENT, OMFS and Plastic Surgery an awareness of what the other specialties can offer so that all can work effectively within an MDT. The TIG aims to expose trainees to the other disciplines to learn and to appreciate what is possible. 11 units have approved posts and 7-9 fellows are funded centrally from Severn Deanery. Fellowships last for one year. : (4 interface training centres Central Manchester, North Manchester, Liverpool and Birmingham have no plastic representation in the local clinical training group. Not all the trainers at these centres (OMFS and ENT) fully accept role of Plastic Surgery within the sub specialty and fellowships. These trainers sit on the TIG STC and partake in selection. 4 centres have had TIG visits: appendix D. Attempts to incorporate Plastic Surgery input have failed to date. There are several other potentially accreditable units including Newcastle, Hull, Oxford and East Grinstead. Addendum by Rowena Hitchcock) A curriculum written by ENT surgeons has accepted by the GMC but it needs to be updated. It is based on the OMFS curriculum but there is a separate H&N section in the Plastic Surgery curriculum. All three contributing specialties are now reviewing the curriculum. The changes are expected to be largely in emphasis rather than substance. Applicants are longlisted against the essential criteria and all eligible applicants are interviewed. Selection centre is run by Severn Deanery. The posts are competitively sought after 17 good applicants for 7 posts most recently. Appointments reflect the proportion of applicants approximately 80% of appointees are from ENT or OMFS and only 20% from Plastic Surgery. The TIG has tried hard to foster interest in Plastic Surgery trainees but with limited success. There have been no formally raised issues over the fairness of the appointment system. However, there are two anecdotal examples of Plastic Surgery trainees not being appointed which caused concern amongst BAPRAS members.,Appendix E. Trainee assessment is by annual RITA or ARCP carried out by the Deanery in which the fellowship is taking place with representation from the fellows home Deanery. Trainers send 6 monthly reports to the TIG.
11 | P a g e
Review of The TIG fellowship schemes
2013
A Certificate of Completion is awarded at the end of the TIG, subject to SAC approval (addendum by JCST secretariat). Failure to complete the fellowship satisfactorily is very unusual. Training units are visited by the TIG for governance purposes. All posts are considered suitable for training, but some do have smaller operative numbers than others. Overall, the TIG works well, achieves its aims as stated above and the applicants are of high quality.
Plastic Surgery used to play a significant role but OMFS are now doing more reconstructions. Reasons are probably multifactorial, but include wide variety of other work required from plastic surgeons, ability of OMFS to do the reconstructions and possibly closer monitoring of oncological treatment deterring some plastic surgeons. The H&N TIG have worked hard to maintain Plastic Surgery involvement, but interest in H&N across the broader Plastic Surgery community is decreasing.
There are changes in surgical practice affecting training for example treatment is moving away from major ablation with reconstruction to transoral/ robotic surgery and Chemotherapy resulting in less involvement from Plastic Surgery. These seem to be moving more quickly in some regions than in others and this is putting strain on the current design of the TIG (my interpretation).
Gareth Griffiths August 2013
12 | P a g e
Review of The TIG fellowship schemes
2013
HAND
Andrew Robson This appears to be a very well established fellowship with few if any problems. This fellowship seems to encourage cross fertilisation of ideas between the two specialties. Plastic Surgery and T&O seem to enjoy cordial relations and work well with each other. Appointments tend to be approximately 50:50 between the two specialties. There is strong evidence of feminization of the workforce with balanced male-female applicants. Plastic Surgery trainees seem to be perceived as the stronger applicants. There are several good points to highlight: New modular syllabus Hard work of chairman in marketing fellowships to stakeholders System of visits by chairman in place Further useful points; Trainees tend to stay in or near parent deanery, not encouraged but it happens Geographically remoter posts less popular No system for formal certification but sign off by TIG chair (a bit like approval of OOP) (Trainees can request certificates addendum by JCST secretariat) TIG works well, SAC chairs (unlike some other TIGs) sit on TIG but also with representatives from speciality associations. A suggestion of regular planned rotation of the chair through the Specialities has been made
13 | P a g e
Review of The TIG fellowship schemes
2013
Cleft Lip and Palate TIG
Gareth Griffiths
Summary of discussion with David Drake, Chair of the Cleft TIG Small sub specialty 24 cleft surgeons who operate on babies in 11 UK units Was the first TIG to be established following a national review of cleft surgery in the 1990s. At that time there was perceived to be a deficiency in service provision in cleft surgery and there was disagreement between OMFS and Plastic Surgery over who should be carrying out the surgery. The review recommended the establishment of a national training programme, hence the Cleft TIG. Because of the difficulties between OMFS and Plastic Surgery at the start of the TIG, it was decided the Chair should be from a neutral specialty. The 4 specialties originally involved were OMFS, Plastic Surgery, ENT and Paediatrics. The Chairs initially were from ENT and Paediatric Surgery as these specialties are only peripherally involved in cleft surgery. Paediatric Surgery withdrew from the TIG quite early on as they had so little involvement in the surgery. The TIG has worked well and has achieved a convergence of views between those involved to the extent that it is now felt appropriate that the Chairs should be appointed from the parent specialties. The current Chair, David Drake, is an OMFS surgeon and the first non-neutral Chair. Some major centres are multiply represented on the committee whilst others are not currently represented. The aims of the TIG are to train surgeons from the parent specialties to be able to carry out all aspects of cleft surgery (except some adult jaw surgery). It is expected that all graduates of the TIG programme will focus their careers on cleft surgery, largely to the exclusion of their parent specialty. Because of this and because the TIG fellowship focuses entirely on cleft, applicants must have achieved all the requirements of their parent specialty before applying for a TIG. Fellowships last for between 1-2 years and most trainees leave the fellowship to enter a consultant post in a cleft unit. Fellows follow a defined curriculum with targets at 6 months and at the end of the post. Post numbers are planned around the expected vacancies and there are 1-2 vacancies per year with about 2 people in post at any one time.
14 | P a g e
Review of The TIG fellowship schemes
2013
Selection is organised centrally via Severn PGME with a multi station interview portfolio, audit and research, clinical. The panel decides the questions the night before the interviews. The interview is a deep examination of the applicants knowledge, commitment and experience of cleft surgery. Successful applicants will show all these attributes by having worked on cleft units and by having carried out audits and research in cleft. An understanding of protocols, MDT working and the contributions of individuals to the development of cleft surgery is expected. With such a selection process, the applicants are essentially pre-selected and are already known to be committed cleft surgeons. Generally, 1 or 2 applicants stand out and up to 6 others are also interviewed for 1 or 2 posts. Truly committed trainees are generally eventually successful, although it may take a couple of applications to be appointed. Appointees overall are equally shared between Plastic Surgery and OMFS. There has only ever been 1 ENT applicant. One truly committed trainee was not appointed in the past because of a weak academic record. This was the only non-appointment known to cause concern. As a result, only academic work carried out during specialty training is now considered. This trainee was successful the following year. Assessment has been by RITA up to now. The first ARCP trainee is now in post and will be assessed by ISCP and WBAs. In addition, the previous TIG Chair and some TIG members review all aspects of fellows performance during visits to their units. When curriculum requirements have been met a Certificate of Completion is awarded. Only one fellow has failed to complete the TIG successfully. Post review is carried out by the TIG visits. All cleft units are considered suitable for TIG training, but at times there may be too many other fellows or newly appointed consultants to make having a TIG fellow appropriate on specific units. The committee might be strengthened by reducing double representation of some centres and ensuring that a wider range of centre and consultant seniority are represented
15 | P a g e
Review of The TIG fellowship schemes
2013
Reconstructive Cosmetic (skin cancer, laser, trauma)
Andrew Robson
This TIG is different from all others in that it is offering short 4month posts, with the aim of giving trainees a taster in reconstructive/cosmetic rather than make them experts. There is significant exposure to private work. The posts are very individualised posts which makes design of a curriculum difficult. There is no specific curriculum although it is based on the cosmetic model in the Plastic Surgery curriculum. This TIG is responsible for reconstructive cosmetics, skin cancer (pilot), laser and trauma fellowships. There is wide representation from specialities including Dermatology. Approximately 70% of posts go to Plastic Surgery trainees. There is a vibrant TIG, with representation from all the SACs and speciality associations and interested groups eg Healing Foundation. No issues have been raised with selection and the posts are very competitively sought. It is noted that trainees tend to stay in or near parent deanery. There are concerns that with the decrease in LATs that it may become more difficult for trainees to be granted OOP; more difficult to get cover for 4/12 than 1 year. Certification: the TIG chair signs off but some trainees dont request or apply for certificates. TIG chair is very concerned about the effect of dissatisfaction that plastic surgeons have with other TIGS may spill over to Reconstructive with possible serious consequences upon this fellowship.
16 | P a g e
Review of The TIG fellowship schemes
2013
Areas for further discussion
The primary function of these posts is to provide world class specialist training and to fulfil the workforce need for the subspecialties represented. However, a side effect has been to potentially improve the national and local interactions between the parent specialties, via the TIG committees, local consultant trainer relationships, improved multidisciplinary clinical meetings and the understanding of the specialty consultants as a whole. This appears to be particularly the case for the Cleft and Hand TIGs. It is recognised that the TIGS continue to contribute to these aims and the fellowships are highly competitive and are universally felt to be worthwhile. The TIGs are functioning within a supportive structure offered by the Severn PGME and Davinder Sandhu. A theme has emerged that in many TIGs meetings are poorly attended and some specialities are heavily underrepresented at meetings and interviews. It is important that all units with TIG fellowships subscribe fully to the principles of interface working and have all specialities integrated. A debate is in progress about whether units that do not have all specialities represented should be involved in training TIG fellows. This is most relevant in Head and Neck where there are excellent teams providing a good service and H&N training but for a variety of reasons do not involve plastic surgeons in the service. These centres could offer local OOP or post CCT Fellowships instead. Transparency of the selection process is clearly key to the success of the TIGs. It is clear that, despite unease about the apparent unfairness of selection in some specialties, the process has been diligently applied and comprehensively and fairly overseen and managed. Adjustment of the process may however better meet the needs of different parent specialties and thus address apparent unfairness and the Severn PGME has initiated a series of TIG meeting to review recruitment strategies. There is a theme of concern about back filling of posts vacated, especially with the reduction of LATS and a recent Dean who declined any trainee to have any pre CCT fellowships based on funding and training time required for CCT. Whilst most specialties are working to refine their curricula, all specialties would benefit from a clarification of the curriculum and outcome with preparation of a selection of ISCP global objectives defining what is expected of each individual trainee during a TIG post. This and educational supervisor training would facilitate governance of both the post and the trainee.
17 | P a g e
Review of The TIG fellowship schemes
2013
All the trainees come with different training and exposure to the fellowship subject, different interests within the training offered by the posts and many have differential expectations of their roles after completion of the posts. However, where these differences are more marked between the parent specialties for example Plastic Surgery and General Surgery or Plastic Surgery and ENT, OMFS a TIG committee and specialty organisation group should explore the effects on trainees of the issues raised in each TIG section. Some method of individual assessment and certification of the extent of training competencies gained during the post would both support the successful trainee and NHS employer reducing the expectation of either party of universal skills. Clarification by each STC and specialty organisation should be given to whether completion of a fellowship alone qualifies a CCT holder to be a sub specialist in that area or whether it is the starting point for skill maturation within a supportive consultant setting. There is room for improvement in the JCST /TIG relationship, with better reporting of TIG activity to the JCST - perhaps with a joint TIG representative to the JCST or SAC reporting as a fixed agenda item. SAC involvement and attendance at TIG meetings, selection and ARCPs has been patchy, particularly where a parent specialty is perceived to be disillusioned with the process. Deanery governance of the TIGs would be facilitated by unification of the TIG terms of reference with particular reference to SAC roles in TIG committees. The hard work of the SACs, TIG committees, parent training program directors, host deaneries/PGME and trust hospitals is delivering a structured, accountable, integrated training designed to meet the service and workforce needs of the subspecialty. There is room for revision in some areas but the fellowships are universally recognised as high quality training and valuable for future career and development.
18 | P a g e
Das könnte Ihnen auch gefallen
- Cuspid Volume 2: Clinically Useful Safety Procedures in DentistryVon EverandCuspid Volume 2: Clinically Useful Safety Procedures in DentistryBewertung: 3 von 5 Sternen3/5 (1)
- Fellowship Accreditation in Pediatric Otolaryngology: A Review of The IssuesDokument5 SeitenFellowship Accreditation in Pediatric Otolaryngology: A Review of The IssuesDeepBhattacharyyaNoch keine Bewertungen
- Professionalism and Ethics: A guide for dental care professionalsVon EverandProfessionalism and Ethics: A guide for dental care professionalsNoch keine Bewertungen
- National Oncoplastic Breast FellowshipDokument3 SeitenNational Oncoplastic Breast Fellowshipplastauk100% (1)
- A Handbook for Student Nurses, 201819 edition: Introducing key issues relevant for practiceVon EverandA Handbook for Student Nurses, 201819 edition: Introducing key issues relevant for practiceNoch keine Bewertungen
- Summer 2012Dokument4 SeitenSummer 2012wmogtNoch keine Bewertungen
- The Impact of General Dental CDokument16 SeitenThe Impact of General Dental CSinta WuLandariNoch keine Bewertungen
- 2017 Psgs Surgical CurriculumDokument117 Seiten2017 Psgs Surgical CurriculumJorge De VeraNoch keine Bewertungen
- Issue 1: No Evidence To Justify Lengthening TrainingDokument4 SeitenIssue 1: No Evidence To Justify Lengthening TrainingAnonymous ZVKnOlNoch keine Bewertungen
- Oral MaxilloFacialSurgery Overview August09Dokument2 SeitenOral MaxilloFacialSurgery Overview August09sarahhNoch keine Bewertungen
- GM Skills Intelligence Pack Education Jan 2022Dokument59 SeitenGM Skills Intelligence Pack Education Jan 2022Mathew PanickerNoch keine Bewertungen
- SWOT AnalysisDokument2 SeitenSWOT AnalysisSaiKaung Htet WaiYanNoch keine Bewertungen
- RANZCOG Annual Report 2013Dokument43 SeitenRANZCOG Annual Report 2013fruittinglesNoch keine Bewertungen
- Assessment of Student Financial Assistance Programs (Stufap) Policies, Procedures, and Control MechanismsDokument18 SeitenAssessment of Student Financial Assistance Programs (Stufap) Policies, Procedures, and Control Mechanismsemerita molosNoch keine Bewertungen
- Improving Future of Surgical Training Education Consensus Recommendations From Association of Surgeons in TrainingDokument4 SeitenImproving Future of Surgical Training Education Consensus Recommendations From Association of Surgeons in TrainingsarahisthedonNoch keine Bewertungen
- ASiT Response - CST-HST Bulge Response - FinalDokument11 SeitenASiT Response - CST-HST Bulge Response - FinalAssociation of Surgeons in TrainingNoch keine Bewertungen
- Good Practice For Good Jobs in Early Childhood Education and Care (Oecd) (Z-Library)Dokument54 SeitenGood Practice For Good Jobs in Early Childhood Education and Care (Oecd) (Z-Library)Norazura Abd HamidNoch keine Bewertungen
- Medical Training Initiative Guide: July 2017Dokument22 SeitenMedical Training Initiative Guide: July 2017Sanjeev SrivastavNoch keine Bewertungen
- Coursework For Dental AssistantDokument4 SeitenCoursework For Dental Assistantnub0vomygun2100% (2)
- Pinoy MDDokument24 SeitenPinoy MDJay MartinezNoch keine Bewertungen
- Postgraduate Medical Training in The UK: For Nepalese Doctors Association Meeting 2016Dokument14 SeitenPostgraduate Medical Training in The UK: For Nepalese Doctors Association Meeting 2016ethemNoch keine Bewertungen
- Non Clinical Careers1Dokument6 SeitenNon Clinical Careers1Mohamed AbdulrazaqNoch keine Bewertungen
- FeeeeeeeeeeeDokument24 SeitenFeeeeeeeeeeeBianca ElenaNoch keine Bewertungen
- CSQ Bulletin75Dokument72 SeitenCSQ Bulletin75Alaina LongNoch keine Bewertungen
- Candidate Guide FGDPDokument47 SeitenCandidate Guide FGDPToni MaddoxNoch keine Bewertungen
- Quarterly Elixir Vol I (2) Feb03-12Dokument6 SeitenQuarterly Elixir Vol I (2) Feb03-12tepps7789Noch keine Bewertungen
- 302 November 2016Dokument12 Seiten302 November 2016Cornwall and Isles of Scilly LMCNoch keine Bewertungen
- WTD-0910-006 - MTI Booklet FINAL (Web-Email v2)Dokument20 SeitenWTD-0910-006 - MTI Booklet FINAL (Web-Email v2)Sumit BatraNoch keine Bewertungen
- ASiT Yearbook 2011Dokument126 SeitenASiT Yearbook 2011Association of Surgeons in TrainingNoch keine Bewertungen
- CHEDDokument93 SeitenCHEDPing RojoNoch keine Bewertungen
- Final Report - Draft - Feasibility RPLDokument76 SeitenFinal Report - Draft - Feasibility RPLmajaliwaally100% (1)
- NZQA Minutes June 4 GG 5 v2Dokument8 SeitenNZQA Minutes June 4 GG 5 v2Amit BaruahNoch keine Bewertungen
- Dental Foundation Programme Year 2Dokument74 SeitenDental Foundation Programme Year 2Toni MaddoxNoch keine Bewertungen
- Master of Public Health Thesis ExamplesDokument5 SeitenMaster of Public Health Thesis Examplesp0kasov1syd2100% (2)
- Anthony Tricoli-Reflections From A College President-When Access Is Not Enough or The Significance of Academic AdvisingDokument5 SeitenAnthony Tricoli-Reflections From A College President-When Access Is Not Enough or The Significance of Academic AdvisingRotanda ThomasNoch keine Bewertungen
- Otolaryngology Residency Selection: Are We Doing It Right?: ReviewDokument9 SeitenOtolaryngology Residency Selection: Are We Doing It Right?: ReviewcaromoradNoch keine Bewertungen
- Health Careers - Training and Development (Plastic Surgery) - 2015-07-10Dokument3 SeitenHealth Careers - Training and Development (Plastic Surgery) - 2015-07-10James DaviesNoch keine Bewertungen
- Mds Periodontics Thesis TopicsDokument7 SeitenMds Periodontics Thesis Topicsamyholmesmanchester100% (2)
- Up MSC 05-06 Tofi StatementDokument11 SeitenUp MSC 05-06 Tofi StatementJace AlacapaNoch keine Bewertungen
- Eye Care ReportDokument20 SeitenEye Care ReportJoeven HilarioNoch keine Bewertungen
- Thesis UctDokument7 SeitenThesis Ucttkxajlhld100% (2)
- Endo Don Tics CurriculumDokument44 SeitenEndo Don Tics Curriculumgaurav patilNoch keine Bewertungen
- GDC Safe Practitioner ConsultationDokument16 SeitenGDC Safe Practitioner ConsultationMugdha FrancisNoch keine Bewertungen
- Message From TYRC Chair: Joseph Gilhooly, MDDokument6 SeitenMessage From TYRC Chair: Joseph Gilhooly, MDSilvy AmaliaNoch keine Bewertungen
- Caldicott Guardians Training Needs Analysis and Survey ReportDokument22 SeitenCaldicott Guardians Training Needs Analysis and Survey Reportpayah5646Noch keine Bewertungen
- CPD Psychiatry BookletDokument25 SeitenCPD Psychiatry BooklettonyjesudasNoch keine Bewertungen
- Dftcurriculum Finaldraft 2015Dokument33 SeitenDftcurriculum Finaldraft 2015emchen11Noch keine Bewertungen
- Ceng Et Al (2021, Training Effectiveness)Dokument8 SeitenCeng Et Al (2021, Training Effectiveness)Nabila RizkikaNoch keine Bewertungen
- Phlebotomy CourseworkDokument5 SeitenPhlebotomy Courseworkf5ddpge2100% (2)
- Long-Term Objectives, Strategic Analysis and ChoiceDokument10 SeitenLong-Term Objectives, Strategic Analysis and ChoiceatifpfizerNoch keine Bewertungen
- 360 PathwaysDokument3 Seiten360 PathwaysHung TranNoch keine Bewertungen
- The Benefits of Postgraduate StudyDokument3 SeitenThe Benefits of Postgraduate StudyRatnam SankarNoch keine Bewertungen
- Diploma of Membership in Restorative DentistryDokument3 SeitenDiploma of Membership in Restorative DentistryomeerulrafieNoch keine Bewertungen
- Who Is Succeeding at ENT ST3Dokument5 SeitenWho Is Succeeding at ENT ST3dpac108Noch keine Bewertungen
- Specialist Recognition Pathway For IMGsDokument6 SeitenSpecialist Recognition Pathway For IMGs197088Noch keine Bewertungen
- PDS University Institute of Dentistry Clinical Course CatalogDokument40 SeitenPDS University Institute of Dentistry Clinical Course CatalogjentotheskyNoch keine Bewertungen
- CapitalNurse Preceptorship FrameworkDokument23 SeitenCapitalNurse Preceptorship FrameworkRijantono Franciscus Maria100% (1)
- Guidelines For STR Training Orthodontics July 2012Dokument10 SeitenGuidelines For STR Training Orthodontics July 2012Hussain alhelalNoch keine Bewertungen
- GDL 2010-04-14 SET Recruitment Booklet V9Dokument23 SeitenGDL 2010-04-14 SET Recruitment Booklet V9juweriy100% (1)
- Trend Analysis of The Nursing Shortage in CanadaDokument11 SeitenTrend Analysis of The Nursing Shortage in Canadaelliott.allmanNoch keine Bewertungen
- Chieving Linical Xcellence: The Combined Management of Open Tibial Fractures (Wet Lab Training)Dokument2 SeitenChieving Linical Xcellence: The Combined Management of Open Tibial Fractures (Wet Lab Training)plastaukNoch keine Bewertungen
- Hand Course Flyer 2015Dokument1 SeiteHand Course Flyer 2015plastaukNoch keine Bewertungen
- Dallas Rhinoplasty SymposiumDokument8 SeitenDallas Rhinoplasty SymposiumplastaukNoch keine Bewertungen
- Plastics Careers Event Final Agreed With MDPDokument1 SeitePlastics Careers Event Final Agreed With MDPplastaukNoch keine Bewertungen
- MXF02 PosterDokument1 SeiteMXF02 PosterplastaukNoch keine Bewertungen
- AdvertDokument1 SeiteAdvertplastaukNoch keine Bewertungen
- Euraps Flyer2pg-A5-05-10-2014Dokument2 SeitenEuraps Flyer2pg-A5-05-10-2014plastaukNoch keine Bewertungen
- ChristieDokument3 SeitenChristieplastaukNoch keine Bewertungen
- Education Day Programme Flyer - 6.11.14Dokument1 SeiteEducation Day Programme Flyer - 6.11.14plastaukNoch keine Bewertungen
- Curry Night Invite 2Dokument1 SeiteCurry Night Invite 2plastaukNoch keine Bewertungen
- Bsrs Poster (TZ) Nov 2014Dokument1 SeiteBsrs Poster (TZ) Nov 2014plastaukNoch keine Bewertungen
- Canniesburn Flap Course Advert Sept 2014Dokument5 SeitenCanniesburn Flap Course Advert Sept 2014plastaukNoch keine Bewertungen
- GU Symposium RCDM Jul 14Dokument1 SeiteGU Symposium RCDM Jul 14plastaukNoch keine Bewertungen
- ProgramDokument1 SeiteProgramplastaukNoch keine Bewertungen
- Announcement 2Dokument1 SeiteAnnouncement 2plastaukNoch keine Bewertungen
- 14th June Scar OutcomesDokument2 Seiten14th June Scar OutcomesplastaukNoch keine Bewertungen
- Interventional Neuroradiology - A Neuroscience Sub-SpecialtyDokument8 SeitenInterventional Neuroradiology - A Neuroscience Sub-Specialtysatyagraha84Noch keine Bewertungen
- Current Techniques in Small Animal Surgery, 5th Edition (VetBooks - Ir)Dokument1.156 SeitenCurrent Techniques in Small Animal Surgery, 5th Edition (VetBooks - Ir)Cryzta Privit Senorin100% (13)
- Disability Support Pension Claim FormsDokument11 SeitenDisability Support Pension Claim Formscurtisbrown89Noch keine Bewertungen
- Saudi Board of Physical Medicine and Rehabilitation (SBPMR)Dokument16 SeitenSaudi Board of Physical Medicine and Rehabilitation (SBPMR)Meenakshiputraeashwarprasad MacherlaNoch keine Bewertungen
- News On AMOSUP HospitalDokument16 SeitenNews On AMOSUP HospitalAMOSUPWeb100% (1)
- CHSI Company Profile & ServicesDokument10 SeitenCHSI Company Profile & ServicesPhilip P. SinghNoch keine Bewertungen
- Hahn - Internist Medical AutobioDokument32 SeitenHahn - Internist Medical AutobiozipoliteNoch keine Bewertungen
- Sufixe Si PrefixeDokument14 SeitenSufixe Si Prefixeseaofdreams6Noch keine Bewertungen
- Consultant General SurgeryDokument2 SeitenConsultant General SurgeryMohamed AbbasNoch keine Bewertungen
- PIL Paliganj PatnaDokument8 SeitenPIL Paliganj PatnaVishal Kumar SinghNoch keine Bewertungen
- The Intricacies of Fourth Year Planning 2018 PDFDokument75 SeitenThe Intricacies of Fourth Year Planning 2018 PDFAnonymous Qo8TfNNoch keine Bewertungen
- Defense of Joel WallachDokument7 SeitenDefense of Joel WallachBen SteigmannNoch keine Bewertungen
- EAUN15 Guideline Intravesical InstillationDokument90 SeitenEAUN15 Guideline Intravesical InstillationRafael RojasNoch keine Bewertungen
- Section of Physical and Rehabilitation MedicineDokument219 SeitenSection of Physical and Rehabilitation MedicineNatalia Loredana100% (4)
- Nuclear Medicine Resources ManualDokument544 SeitenNuclear Medicine Resources ManualHend Ayman Azazy100% (2)
- Adjusted ContractDokument19 SeitenAdjusted Contractmarsen100% (1)
- NSW Priority Skilled Occupation List 2018 19Dokument3 SeitenNSW Priority Skilled Occupation List 2018 19Vasif SholaNoch keine Bewertungen
- The Coming of The New OrganizationDokument16 SeitenThe Coming of The New Organizationshoaib_ulhaq100% (1)
- The Promise Perils Problems and Progress of Competency Based Medical EducationDokument8 SeitenThe Promise Perils Problems and Progress of Competency Based Medical EducationJasmik SinghNoch keine Bewertungen
- Medical, Dental Retainership ProposalDokument3 SeitenMedical, Dental Retainership ProposalJoseph Gayod100% (1)
- Jagannadha Rao PeelaDokument2 SeitenJagannadha Rao PeelaJagannadha Rao PeelaNoch keine Bewertungen
- Puzzles SetDokument87 SeitenPuzzles SetShubham ShuklaNoch keine Bewertungen
- Chapter IDokument50 SeitenChapter Isutarmisaja15Noch keine Bewertungen
- Ccrisp Administrator Handbook 20Dokument1 SeiteCcrisp Administrator Handbook 20balasepuriNoch keine Bewertungen
- TN Primary Care Physicians COMPLAINT (Exhibits Attached)Dokument89 SeitenTN Primary Care Physicians COMPLAINT (Exhibits Attached)HLMeditNoch keine Bewertungen
- Forensic NursingDokument8 SeitenForensic NursingAssignmentLab.comNoch keine Bewertungen
- Guidelines and Levels of Care For Pediatric Intensive Care UnitsDokument16 SeitenGuidelines and Levels of Care For Pediatric Intensive Care Unitssridhar_physioNoch keine Bewertungen
- What Is The Bonded Medical Places (BMP) Scheme? What Is A District of Workforce Shortage?Dokument2 SeitenWhat Is The Bonded Medical Places (BMP) Scheme? What Is A District of Workforce Shortage?honeyjoy76Noch keine Bewertungen
- Code of Ethics Medical ProfessionDokument8 SeitenCode of Ethics Medical ProfessionAustin CharlesNoch keine Bewertungen
- Pediatrics: A Resource GuideDokument35 SeitenPediatrics: A Resource GuideKarl Martin PinedaNoch keine Bewertungen