Beruflich Dokumente
Kultur Dokumente
Comparison of Three Radiographic Methods For Detection of Morphological Temporomandibular Joint Changes - Panoramic, Scanographic and Tomographic Examination PDF
Hochgeladen von
rmontserratOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Comparison of Three Radiographic Methods For Detection of Morphological Temporomandibular Joint Changes - Panoramic, Scanographic and Tomographic Examination PDF
Hochgeladen von
rmontserratCopyright:
Verfügbare Formate
Dentomaxillofacial Radiology (2009) 38, 134140 2009 The British Institute of Radiology http://dmfr.birjournals.
org
RESEARCH
Comparison of three radiographic methods for detection of morphological temporomandibular joint changes: panoramic, scanographic and tomographic examination
H Hintze*,1, M Wiese1,2 and A Wenzel2
1 Department of Oral Radiology, School of Dentistry, University of Aarhus, Denmark; 2Department of Radiology, School of Dentistry, University of Copenhagen, Denmark
Objectives: To compare the diagnostic accuracy of panoramic, scano- and tomographic examination for the detection of morphological temporomandibular joint (TMJ) changes. Methods: TMJs in 80 dry human skulls were radiographed using digital panoramic examination, 46 sagittal (lateral) scanography, and sagittal cross-sectional tomography. All images were examined by three independent observers for the presence or absence of flattening, defects and osteophytes in the various joint components. The true presence of the morphological changes was unanimously decided by consensus of three independent observers using naked-eye inspection. The accuracy for detection of the specific changes in each joint component was expressed as sensitivity and specificity values, whereas the accuracy for detection of morphological changes in general in the condyle and in the TMJ in toto was expressed as the number of matching radiographic and gold standard scores. Results: Up to 23% and 9% of the three joint components were recorded as non-accessible to examination with panoramic examination and sagittal (lateral) scanography, respectively, whereas all components were accessible to examination with sagittal cross-sectional tomography. The difference was significant between panoramic examination and sagittal cross-sectional tomography (P 5 0.018). No significant differences between the three methods for detection of specific morphological changes in the condyles and defects in the articular tubercles and changes in the TMJ in toto were found. Conclusion: No differences in accuracies between the methods were found for the detection of morphological TMJ changes. However, with panoramic examination and sagittal (lateral) scanography markedly more joint components were non-accessible to examination than with sagittal cross-sectional tomography, with which all components were accessible. Dentomaxillofacial Radiology (2009) 38, 134140. doi: 10.1259/dmfr/31066378 Keywords: radiography; temporomandibular joint; digital radiography; panoramic radiography; tomography
Introduction For radiographic examination of the temporomandibular joint (TMJ), several methods are available with conventional extraoral X-ray equipment. A widespread and simple method is a panoramic radiograph requiring a low patient radiation dose and a short productive time for the staff, whereas one of the more sophisticated
*Correspondence to: Hanne Hintze, Department of Oral Radiology, School of Dentistry, Faculty of Health Sciences, University of Aarhus, Vennelyst Boulevard 9, DK-8000 Aarhus C, Denmark; E-mail: hhintze@odont.au.dk Received 11 February 2008; revised 14 April 2008; accepted 14 April 2008
methods is individually corrected, cross-sectional tomography requiring relatively high radiation doses and long working times for the staff.1 Between those two methods various types of TMJ scanography exist.2 Thus, programs for scanography at different anatomical planes are available in more of the modern panoramic X-ray units. Some TMJ scanography programs result in one sagittal and one coronal projection of each of the two joints on the same film, whereas other programs result in two sagittal projections, one in closed- and one in open-mouth position, of
TMJ radiography H Hintze et al
135
both joints on the same film, allowing the observer to view the TMJ in relation to function in the sagittal plan. The last-mentioned scanograms resemble the traditional oblique lateral transcranial projection.3 To select the most accurate examination procedure for a specific patient it is essential to know the efficacy of the procedures available. Seemingly, the accuracy of the above-mentioned methods (panoramic, sagittal scanography in closed and open mouth positions and tomography) undertaken for TMJ diagnostics have not been mutually compared. Therefore, the aim of this study was to compare the diagnostic accuracy of a panoramic examination with sagittal scanography and sagittal cross-sectional tomography for the detection of morphological bone changes in the TMJ in dry human skulls, for which the true presence of changes could be validated by direct visual inspection.
Materials and methods The left and right TMJ in 80 dry human skulls was radiographed in a Cranex Tome X-ray unit (Soredex, Helsinki, Finland) using three examination methods: standard panoramic examination (program 001), sagittal scanography in closed and open mandibular position (4 6 lateral TMJ (program 506)), and sagittal (lateral) cross-sectional spiral tomography (program 610694). The tomography was obtained as individually corrected tomograms (based on a lateral four angle pre-examination) oriented perpendicular to the long axis of the condyle and with an image layer thickness of 4 mm. For the majority of joints a series of four cuts was sufficient for imaging the joint from the most lateral to the most medial part. The most frequently used exposure parameters (depending on the size of the skulls) for panoramic examination and sagittal (lateral) scanography were 63 kVp, 10 mA and an exposure time varying from 15 s to 30 s. For sagittal cross-sectional tomography, the tube voltage ranged from 57 kVp to 66 kVp and the tube current from 1.6 mA to 5.0 mA with an exposure time of 46 s. The exposure parameters were determined previously in a pilot study conducted to evaluate which parameters resulted in the subjectively best image quality with each method. Four layers of plastic foils were placed in front of the radiation source (for more details, see Wiese et al4). Digora storage phosphor plates (placed in a cassette without intensifying screens) scanned in a Digora PCT scanner (Soredex, Helsinki, Finland) were used as image receptors in connection with all three examination methods. The skulls were placed on a photostat device to ensure optimal positioning for all radiographic examinations. Panoramic radiographs were obtained with the mandible in a protruded position, tomograms with the mandible in a stable dental occlusion (using a silicone impression in case of tooth loss), and scanograms with the mandible in a stable dental occlusion for
the closed-mouth images and maximum mandibular opening (condyle placed below the articular tubercle) for the open-mouth images. An experienced radiographer performed all examinations. Three pre-calibrated observers (two experienced oral radiologists (observers 1 and 2) and one general dentist under specialist training (observer 3)) examined the radiographs obtained with the three methods individually and in a random order. The condyle was assessed for the presence of flattening, defects and osteophytes; the mandibular fossa and articular tubercle were assessed for the presence of flattening and defects. Flattening was defined as loss of convexity of the bone outlines, defect as a local area of rarefaction in the layer of compact bone and osteophyte as a local outgrowth of bone arising from the exterior surface.5 The left and right joints of each skull were examined independently of each other. Each type of morphological bone change was assessed separately using a binary registration scale: 0 5 no change; 1 5 change. In case the observer could not view each joint component in its entirety, they were asked to record the specific component as non-accessible to examination. All radiographs were assessed in the Digora software on a 19 inch IBM cathode ray tube monitor placed in a room with subdued lighting and the observers were free to use the enhancement facilities in the software as they liked. Radiographs obtained with each of the three methods on 15 randomly selected joints were reexamined 34 weeks after the first examination to evaluate the intraobserver reproducibility. The true presence of morphological changes (flattening, defects and osteophytes) was assessed by three observers independently using naked-eye inspection assisted by a magnifying viewer with built-in light, preceded by an observer calibration session. A binary registration scale for the true presence of changes was used: 0 5 no change; 1 5 change. A change was defined as present if reported by all three observers. The consensus naked-eye inspection served as the gold standard for the radiographic examinations. Figure 1 illustrates radiographs obtained using the three radiographic methods of a TMJ with condylar changes. Data analysis Sensitivity and specificity values were used to express each methods diagnostic accuracy for detection of the defined changes related to each joint component. To express the general diagnostic accuracy for all changes in each joint component and in the TMJ in toto, the number of matching gold standard and radiographic scores was used. The number of matching gold standard and radiographic scores was calculated for each change by counting the number of score differences of 0 (subtracting the radiographic score from the gold standard score). The number of differences resulting in 0 was calculated for each observer with each method. The higher the number of 0 differences,
Dentomaxillofacial Radiology
136
TMJ radiography H Hintze et al
Figure 1 Cropped (a) panoramic examination, (b) sagittal (lateral) scanography in closed and open mandibular position and (c) sagittal crosssectional tomography of (d) a temporomandibular joint with a condyle with flattening and a large bone defect (viewed from the top) and (e), a mandibular fossa and an articular tubercle with no bone changes according to the gold standard. The condylar flattening was recorded with all radiographic methods by all observers, but the condylar defect was not identified by all observers with all methods
Dentomaxillofacial Radiology
TMJ radiography H Hintze et al
137
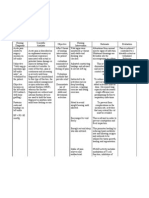
Table 1 Number of joint components in 159 temporomandibular joints recorded as non-accessible to radiographic examination by three observers using three methods Panoramic examination Condyle n (%) Observer 1 Observer 2 Observer 3 1 (1) 2 (1) 3 (2) Mandibular fossa n (%) 2 (1) 30 (19) 37 (23) Articular tubercle n (%) 1 (1) 2 (1) 10 (6) Sagittal (lateral) scanography Condyle n (%) 1 (1) 2 (1) 15 (9) Mandibular fossa n (%) 1 (1) 4 (3) 15 (9) Articular tubercle n (%) 2 (1) 13 (8) 15 (9) Sagittal cross-sectional tomography Condyle n (%) 0 0 0 Mandibular fossa n (%) 0 0 0 Articular tubercle n (%) 0 0 0
the higher the diagnostic accuracy. Differences between methods were tested by two-way ANOVA with observer and method as the two independent variables. Pairwise comparisons between methods were made by the post hoc t-test (SPSS package, GLM (general linear model) v10.0 for Windows; SPSS Inc., Chicago, IL). The level of statistical significance was P , 0.05. Intraobserver reproducibility was expressed as kappa values. Results Sagittal cross-sectional tomography radiographs of one joint were missing and could not be re-established. This joint was excluded from the study sample, which thereafter was reduced to 159 joints. With each radiographic method the individual observer recorded a number of joint components as being non-accessible to examination (Table 1). With panoramic radiographs up to 23% of the fossae and 6% of the articular tubercles were recorded as non-accessible to examination. The corresponding percentages with scanograms were 9% and 9%, respectively. With tomograms all joint components were accessible to examination. Overall, significantly fewer joint components were accessible to examination with panoramic examination than with sagittal cross-sectional tomography (P 5 0.018); no significant difference existed between panoramic examination and sagittal (lateral) scanography and between the scanography and sagittal cross-sectional tomography. Since only joint components recorded to be accessible to examination with all three methods by all three observers were included in the comparison between methods, the study sample was reduced as shown in Table 2. In this table, the frequency of morphological changes according to the gold standard can also be
seen. In only 97 joints all 3 components (condyle, mandibular fossa and articular tubercle) were accessible to examination by all 3 observers with all 3 methods. Mean sensitivity and specificity values for the detection of flattening, defects and osteophytes in the condyle are shown in Table 3. No significant differences between the three methods were found for sensitivities or specificities. Irrespective of the type of change, the observers were poor in detecting a change, e.g. the mean sensitivity for defects was 0.04 with panoramic examination, 0.18 with sagittal (lateral) scanography and 0.10 with sagittal cross-sectional tomography with true defects in 46% of the 143 examined condyles. Also, flattening was difficult to identify correctly since the mean sensitivities ranged from 0.12 with sagittal cross-sectional tomography to 0.33 with panoramic examination, with true flattening in about 20% of the condyles. Overall, the observers were much better at correctly identifying condyles without morphological changes since the mean specificities ranged from 0.86 to 0.99. These figures indicate that the fraction of false positive registrations was low. The observers performances with the three radiographic methods for detection of changes in the mandibular fossa were not analysed since the true frequency of flattening and defects was 0% and 2%, respectively. The same was the case for flattening in the articular tubercles (frequency less than 1%). For the detection of articular tubercle defects the mean sensitivities for panoramic examination, sagittal (lateral) scanography, and sagittal cross-sectional tomography were 0.00, 0.10 and 0.05, respectively. The mean specificities for the corresponding methods were 1.00, 0.99 and 0.99. Neither sensitivities nor specificities were significantly different for the three methods. Comparison of the three radiographic methods for assessment of all changes in the condyle and the TMJ in toto (n 5 97) is shown in Figure 2. About 77% (332/
Table 2 Number of temporomandibular joint components accessible to radiographic examination with all three methods and their number of morphological changes according to the gold standard Morphological changes Flattening n accessible to exam/ n with changes (%) Condyle Mandibular fossa Articular tubercle 143/28 (19.6) 104/0 (0.0) 131/1 (0.8) Defects n accessible to exam/ n with changes (%) 143/66 (46.2) 103*/2 (1.9) 131/7 (5.3) Osteophytes n accessible to exam/ n with changes (%) 143/2 (1.3) not assessed not assessed
*In one joint one observer missed the recording of defects in the fossa
Dentomaxillofacial Radiology
138
TMJ radiography H Hintze et al
Figure 2 Diagnostic accuracy expressed as the mean number of matching radiographic and gold standard scores for all possible morphological changes in the condyles (maximum n 5 429 (3 variables (flattening, defect, osteophyte) in 143 condyles) and in the temporomandibular joint in toto (maximum n 5 679 (7 variables (3 in the condyle: flattening, defect, osteophyte; 2 in the fossa: flattening, defect; 2 in the tubercle: flattening, defect) in 97 joints)) using panoramic examination (Pan), sagittal (lateral) scanography (Scano) and sagittal cross-sectional tomography (Tomo)
429 6 100%, 330/429 6 100%, 333/429 6 100%) of the radiographic recordings with the three methods were in accordance with the gold standard, whereas this percentage was about 89% (604/679 6 100%, 603/679 6 100%, 604/679 6 100%) for the three methods when the joint was assessed in toto. No significant difference between methods was found. Kappa values for intraobserver reproducibilities for detection of changes in the condyle, fossa and articular tubercle ranged as follows with panoramic examination, sagittal (lateral) scanography and sagittal crosssectional tomography: observer 1: 0.601.00 (95% confidence interval (CI): 0.12, 1.00), 0.461.00 (95% CI: 0.00, 1.00) and 0.441.00 (95% CI: 20.16, 1.00); observer 2: 0.291.00 (95% CI: 20.31, 1.00), 0.821.00 (95% CI: 0.48, 1.00) and 0.821.00 (95% CI: 0.48, 1.00); observer 3: 0.761.00 (95% CI: 0.32, 1.00), 0.761.00 (95% CI: 0.32, 1.00) and 1.00 (no range).
Discussion Panoramic radiographs are widely used among general dentists as well as among dental specialists as an overview examination of teeth and jaws since they are easy to perform, economically cheap to produce and provide an image of a large anatomical area from one low-radiation dose exposure.6 For assessment of the TMJ, panoramic radiography is popular too, probably for the same reasons.6 Particularly for the TMJ, panoramic radiography depicts the condyles with large distortion and anatomical overlapping especially in the fossa and tubercle areas, often making these areas difficult or even impossible to examine.711 Compared with lateral tomography it has also been shown that panoramic radiographs obtained with different panoramic units result in large differences in the way that the condyle is depicted depending on its shape.12 These
Dentomaxillofacial Radiology
limitations might well lead to inaccurate diagnoses, and therefore experts recommend that a TMJ radiographic examination is not based solely on panoramic radiography.9,1315 Instead, individually corrected tomography has been recommended as the most accurate technique for TMJ assessment since tomograms are undistorted, anatomically accurate if obtained with individual condyle orientation and depict the joint in its full extent.9 These advantages might be the reason why some studies have reported a higher frequency of TMJ bone changes observed on tomograms than on panoramic radiographs of the same patients.7,16,17 But the higher number of changes reported in tomograms have not always been validated, thus it may be difficult to conclude whether they have been true or false positive recordings. If the latter is the case, tomography might well do more harm than good and all the extra resources needed for tomography compared with the much simpler panoramic examination might be a waste. The diagnostic value of TMJ scanography in open and closed mandibular positions for the detection of morphological bone changes seems not to have been evaluated even though the technique has been available in modern panoramic units for years. In comparison with tomography it is much simpler to produce and should therefore be used if its diagnostic quality equals that of tomography. The present study pertained to answer this question for the identification of a number of common TMJ bone changes, which could be validated rather unambiguously. Overall, the present comparison of panoramic examination, sagittal (lateral) scanography and sagittal cross-sectional tomography showed no significant differences between the three methods irrespective of the morphological change in the condyle or defects in the articular tubercle. For condylar osteophytes this result is in accordance with an in vitro study published
TMJ radiography H Hintze et al
139
Table 3 Diagnostic accuracy for the detection of morphological changes related to the condyle with the three radiographic methods Morphological changes in the condyle Flattening Pan Mean sensitivity Observer 1 Observer 2 Observer 3 Mean specificity Observer 1 Observer 2 Observer 3 0.33 0.39 0.50 0.11 0.91 0.87 0.87 0.99 Scano 0.21 0.21 0.14 0.29 0.86 0.91 0.78 0.90 Tomo 0.12 0.07 0.18 0.11 0.95 0.98 0.89 0.97 Defect Pan 0.04 0.05 0.05 0.02 0.99 0.99 0.97 1.00 Scano 0.18 0.05 0.11 0.38 0.96 1.00 0.90 0.97 Tomo 0.10 0.06 0.18 0.05 0.97 1.00 0.91 1.00 Osteophyte Pan 0.50 0.50 0.50 0.50 0.99 0.98 1.00 1.00 Scano 0.50 0.50 0.50 0.50 0.99 1.00 0.96 1.00 Tomo 0.50 0.50 0.50 0.50 0.99 0.98 0.99 1.00
Pan, panoramic examination; Scano, sagittal (lateral) scanography; Tomo, sagittal cross-sectional tomography
by Tyndall et al,18 who used cementumdentin chips positioned on the surface of a condyle from a dry human skull simulating osteophytes. In this study no significant difference in diagnostic accuracy was found between individually corrected sagittal tomography (3 mm cuts) and two much simpler methods (biplanar (sagittal and coronal) panoramic examination and single-slice arbitrarily corrected sagittal zonography). However, in another study also using attached cementumdentin chips as simulation for condylar osteophytes, the use of a combination of individually corrected sagittal and coronal tomography resulted in a significantly higher diagnostic accuracy than the use of biplanar (sagittal and coronal) panoramic examination.19 The latter finding might primarily be caused by inclusion of coronal tomography as a supplement to the traditional sagittal tomograms, which were used alone in the study by Tyndall et al.18 However, in the present study sample and in patients too, osteophytes usually are located on the anterior surface of the condyle, where they will be superimposed by the condyle head and thereby will be hidden on tomograms obtained in the coronal plane.20 Therefore, we do not believe that the results from the present study would have been different in case tomography in the coronal plane had been included. The present results for condylar bone defects are different from results obtained in a previous study by Honey et al,21 who compared the diagnostic accuracy of panoramic radiography with linear tomography for the detection of physical damage defects on the lateral pole of 37 condyles, and found panoramic radiography significantly more accurate than tomography. However, no explanation for this unexpected finding was given, but a reason could be that the observers were more familiar with panoramic than with tomographic radiographs. In our study all observers were familiar with all methods under evaluation. For all changes it was surprising to see how poorly they were detected by all methods and all observers, e.g. condylar flattening was identified on average in onethird of the joints with this change with panoramic examination, and in one-fifth or less with sagittal (lateral) scanography and sagittal cross-sectional tomography. This was surprising since this morphological
change as well as the other changes must be suspected to be rather manifest since it was observed by the visual inspection method by all three observers. In case of miniature or dubious flattenings they would probably have been identified by one or two of the observers only, not all three. The present sensitivity and specificity values for sagittal cross-sectional tomography are somewhat different from the corresponding values in a previous study based on the same skulls.22 The main reason is that the previous study used a less strict gold standard. The reason for the rather poor detection of condylar flattening with all methods could be the projection plane. From a previous study it has been found that the sensitivity for the identification of flattening is higher with coronal tomograms than with sagittal tomograms.22 That no significant difference in diagnostic accuracy was found between panoramic examination, sagittal (lateral) scanography, and sagittal cross-sectional tomography for the detection of morphological bone changes speaks in favour of using panoramic examination or sagittal (lateral) scanography, which are much simpler to undertake and result in a much smaller radiation burden than sagittal cross-sectional tomography.1 The production time for e.g. a panoramic radiograph is only a minor fraction of the production time for a bilateral tomographic examination, and the same is true for the radiation doses for the two methods.1 However, it should be remembered that up to 23% of the fossae and 9% of the condyles and tubercles were recorded as non-accessible to examination with panoramic examination and sagittal (lateral) scanography, respectively, in contrast with sagittal cross-sectional tomography, with which all three components in all joints were accessible to examination. In the clinical situation the advantages and disadvantages of the various radiographic methods need to be considered before ordering the specific TMJ examination method. The poor diagnostic accuracy with the present radiographic methods should lead to considerations about the general use of conventional TMJ radiographic examinations in patients since the TMJ findings must be interpreted with large reservations especially negative findings in the condyles, which might well be
Dentomaxillofacial Radiology
140
TMJ radiography H Hintze et al
false. The high specificity values for all changes with all methods may be explained by the fact that all methods under evaluation were effective for the identification of joint components without changes. However, the high specificities could also indicate method limitations. If the radiographic methods under evaluation are unable to depict truly present TMJ bone changes then the observers would not be able to perceive them, and therefore they recorded the joint component as having no change the same as being sound. This in combination with a low disease frequency would lead to high specificity values. The intraobserver reproducibility ranged from fair to almost perfect according to the terminology suggested by Landis and Koch23 with panoramic examination and from moderate to almost perfect with sagittal
References
1. Ludlow JB, Davies-Ludlow LE, Brooks SL. Dosimetry of two extraoral direct digital imaging devices: NewTom cone beam CT and Orthophos Plus DS panoramic unit. Dentomaxillofac Radiol 2003; 32: 229234. 2. White SC, Pharoah MJ (eds). Oral radiology. Principles and interpretation (5th edn). St Louis: Mosby, 2004. 3. Westesson P-L, Katzberg RW (eds). Imaging of the temporomandibular joint. Baltimore: Williams & Wilkins, 1991. 4. Wiese M, Hintze H, Svensson P, Wenzel A. Comparison of diagnostic accuracy of film and digital tomograms for assessment of morphological changes in the TMJ. Dentomaxillofac Radiol 2007; 36: 1217. , Petersson A. Radiography of the temporomandib5. Omnell K-A ular joint utilizing oblique lateral transcranial projections. Comparison of information obtained with standardized technique and individualized technique. Odont Revy 1976; 26: 7792. 6. Pendlebury ME, Horner K, Eaton KA. Selection criteria for dental radiography (2nd edn). London: Faculty of General Dental Practitioners (UK), The Royal College of Surgeons of England, 2004. 7. Habets LL, Bezuur JN, Jimenez Lopez V, Hansson TL. The OPG: an aid in TMJ diagnostics. III. A comparison between lateral tomography and dental rotational panoramic radiography (Orthopantomography). J Oral Rehabil 1989; 6: 401406. 8. Ruf S, Pancherz H. Is orthopantomography reliable for TMJ diagnosis? An experimental study on a dry skull. J Orofacial Pain 1995; 9: 365374. 9. Brooks SL, Brand JW, Gibbs SJ, Hollender L, Lurie AG, Omnell , et al. Imaging of the temporomandibular joint. A position K-A paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 83: 609618. 10. Epstein JB, Caldwell J, Black G. The utility of panoramic imaging of the temporomandibular joint in patients with temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92: 236239. 11. Fallon SD, Fritz GW, Laskin DM. Panoramic imaging of the temporomandibular joint: an experimental study using cadaveric skulls. J Oral Maxillofac Surg 2006; 64: 223229.
(lateral) scanography and sagittal cross-sectional tomography. Corresponding values have been found in other TMJ studies using different radiographic techniques and modalities.4,17,21,22 However, in cases with fair and moderate reproducibility the diagnostic value of the method is further reduced and it becomes more difficult for the clinician to trust the diagnostic outcome. In conclusion, no significant differences in diagnostic accuracies between panoramic examination, sagittal (lateral) scanography, and sagittal cross-sectional tomography were found for the detection of morphological TMJ changes primarily condylar changes. This supports the use of the simplest method (panoramic examination) which, however, was poorer than sagittal cross-sectional tomography at depicting the condyle, the fossa and the tubercle in each joint.
12. Mawani F, Lam EWN, Hoe G, McKee I, Raboud DW, Major PW. Condylar shape analysis using panoramic radiography units and conventional tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 99: 341348. 13. Hollender L. Standards of radiological care. Am Acad Oral and Maxillofac Radiol Newsl 1998; 25: 112. 14. Pharoah MJ. The prescription of diagnostic images for temporomandibular joint disorders. J Orofacial Pain 1999; 13: 251254. 15. Leon SD. The use of panoramic radiography for evaluating temporomandibular disorders. Gen Dent 2004; 52: 339341. 16. Larheim TA. Comparison between three radiographic techniques for examination of the temporomandibular joints in juvenile rheumatoid arthritis. Acta Radiol Diagn 1981; 22: 195201. 17. Dahlstro m L, Lindvall A-M. Assessment of temporomandibular joint disease by panoramic radiography: reliability and validity in relation to tomography. Dentomaxillofac Radiol 1996; 25: 197201. 18. Tyndall DA, Davies KL, Ludlow JB. A comparison of zonography, multidirectional tomography, and biplanar panoramic images for detection of simulated condylar arthropathy of the temporomandibular joint. Int J Adult Orthod Orthognath Surg 1995; 10: 277284. 19. Ludlow JB, Davies KL, Tyndall DA. Temporomandibular joint imaging. A comparative study of diagnostic accuracy for the detection of bone change with biplanar multidirectional tomography and panoramic images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 80: 735743. 20. Isberg A. Temporomandibular joint dysfunction. A practitioners guide (1st edn). Oxford: Isis Medical Media Ltd, 2001. 21. Honey OB, Scarfe WC, Hilgers MJ, Klueber K, Silveira AM, Haskell BS, et al. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparison with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop 2007; 132: 429438. 22. Hintze H, Wiese M, Wenzel A. Cone beam CT and conventional tomography for the detection of morphological temporomandibular joint changes. Dentomaxillofac Radiol 2007; 36: 192197. 23. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159174.
Dentomaxillofacial Radiology
Das könnte Ihnen auch gefallen
- Evaluation of The Severity of Temporomandibular Joint Osteoarthritic Changes Related To Age Using Cone Beam Computed Tomography PDFDokument7 SeitenEvaluation of The Severity of Temporomandibular Joint Osteoarthritic Changes Related To Age Using Cone Beam Computed Tomography PDFrmontserratNoch keine Bewertungen
- Evaluacion de Cambios Oseos en ATM Usando CBCT PDFDokument6 SeitenEvaluacion de Cambios Oseos en ATM Usando CBCT PDFrmontserratNoch keine Bewertungen
- Comparison of Diagnostic Accuracy of LM and Digital Tomograms For Assessment of Morphological Changes in The TMJ PDFDokument6 SeitenComparison of Diagnostic Accuracy of LM and Digital Tomograms For Assessment of Morphological Changes in The TMJ PDFrmontserratNoch keine Bewertungen
- 381 Full PDFDokument9 Seiten381 Full PDFrmontserratNoch keine Bewertungen
- Diagnostic Accuracy of Microcomputed Tomography For Osseous Abnormalities in The Rat Temporomandibular Joint Condyle PDFDokument5 SeitenDiagnostic Accuracy of Microcomputed Tomography For Osseous Abnormalities in The Rat Temporomandibular Joint Condyle PDFrmontserratNoch keine Bewertungen
- 286 Full PDFDokument5 Seiten286 Full PDFrmontserratNoch keine Bewertungen
- Correlating Cone Beam CT Results With Temporomandibular Joint Pain of Osteoarthritic Origin PDFDokument5 SeitenCorrelating Cone Beam CT Results With Temporomandibular Joint Pain of Osteoarthritic Origin PDFrmontserratNoch keine Bewertungen
- Diagnostic Performance of Magnetic Resonance Imaging For Detecting Osseous Abnormalities of The Temporomandibular Joint and Its Correlation With Cone Beam Computed Tomography PDFDokument7 SeitenDiagnostic Performance of Magnetic Resonance Imaging For Detecting Osseous Abnormalities of The Temporomandibular Joint and Its Correlation With Cone Beam Computed Tomography PDFrmontserratNoch keine Bewertungen
- Correlation Between Disc Displacements and Locations of Disc Perforation in The Temporomandibular Joint PDFDokument8 SeitenCorrelation Between Disc Displacements and Locations of Disc Perforation in The Temporomandibular Joint PDFrmontserratNoch keine Bewertungen
- Cone Beam CT and Conventional Tomography For The Detection of Morphological Temporomandibular Joint Changes PDFDokument6 SeitenCone Beam CT and Conventional Tomography For The Detection of Morphological Temporomandibular Joint Changes PDFrmontserratNoch keine Bewertungen
- An Investigation of Magnetic Resonance Imaging Features in 14 Patients With Synovial Chondromatosis of The Temporomandibular Joint PDFDokument7 SeitenAn Investigation of Magnetic Resonance Imaging Features in 14 Patients With Synovial Chondromatosis of The Temporomandibular Joint PDFrmontserratNoch keine Bewertungen
- Baseline Clinical and Radiographic Features Are Associated With Long-Term (8 Years) Signs:symptoms For Subjects With Diseased Temporomandibular Joint PDFDokument5 SeitenBaseline Clinical and Radiographic Features Are Associated With Long-Term (8 Years) Signs:symptoms For Subjects With Diseased Temporomandibular Joint PDFrmontserratNoch keine Bewertungen
- The Relationship Between Temporomandibular Joint Disk Displacement and Mandibular Asymmetry in Skeletal Class III Patients PDFDokument8 SeitenThe Relationship Between Temporomandibular Joint Disk Displacement and Mandibular Asymmetry in Skeletal Class III Patients PDFrmontserratNoch keine Bewertungen
- 55 Full PDFDokument4 Seiten55 Full PDFrmontserratNoch keine Bewertungen
- Relationship Between Temporomandibular Joint Internal Derangement and Facial Asymmetry in Women PDFDokument9 SeitenRelationship Between Temporomandibular Joint Internal Derangement and Facial Asymmetry in Women PDFrmontserratNoch keine Bewertungen
- Reliability of Two Techniques For Measuring Condylar Asymmetry With X-Rays PDFDokument8 SeitenReliability of Two Techniques For Measuring Condylar Asymmetry With X-Rays PDFrmontserratNoch keine Bewertungen
- Relationship Between Internal Derangement of The Temporomandibular Joint and Dentofacial Morphology in Women With Anterior Open Bite PDFDokument9 SeitenRelationship Between Internal Derangement of The Temporomandibular Joint and Dentofacial Morphology in Women With Anterior Open Bite PDFrmontserratNoch keine Bewertungen
- Synovial Chondromatosis in The Temporomandibular Joint Complicated by Displacement and Calci Cation of The Articular Disk - Report of Two Cases PDFDokument4 SeitenSynovial Chondromatosis in The Temporomandibular Joint Complicated by Displacement and Calci Cation of The Articular Disk - Report of Two Cases PDFrmontserratNoch keine Bewertungen
- Quantification of Condylar Resorption in Temporomandibular Joint Osteoarthritis PDFDokument15 SeitenQuantification of Condylar Resorption in Temporomandibular Joint Osteoarthritis PDFrmontserratNoch keine Bewertungen
- Prevalence of TMJ Disorders Among Students and Its Relation To Malocclusion PDFDokument7 SeitenPrevalence of TMJ Disorders Among Students and Its Relation To Malocclusion PDFrmontserratNoch keine Bewertungen
- Diagnostic of Craniofacial Asymmetry. Literature Review PDFDokument5 SeitenDiagnostic of Craniofacial Asymmetry. Literature Review PDFrmontserratNoch keine Bewertungen
- Prevalence of Vertical Condilar Asymmetry of The Temporomandibular Joint in Patients With Signs and Symptoms of Temporomandibular Disorders PDFDokument7 SeitenPrevalence of Vertical Condilar Asymmetry of The Temporomandibular Joint in Patients With Signs and Symptoms of Temporomandibular Disorders PDFrmontserratNoch keine Bewertungen
- Association Between Condylar Asymmetry and Temporomandibular Disorders Using 3D-CT PDFDokument7 SeitenAssociation Between Condylar Asymmetry and Temporomandibular Disorders Using 3D-CT PDFrmontserratNoch keine Bewertungen
- Idiopathic Condylar Resorption of The Temporomandibular Joint in Teenage Girls (Cheerleaders Syndrome) PDFDokument7 SeitenIdiopathic Condylar Resorption of The Temporomandibular Joint in Teenage Girls (Cheerleaders Syndrome) PDFrmontserratNoch keine Bewertungen
- Correlation Between The Condyle Position and IntraExtraarticular Clinical Findings of Temporomandibular Dysfunction PDFDokument7 SeitenCorrelation Between The Condyle Position and IntraExtraarticular Clinical Findings of Temporomandibular Dysfunction PDFrmontserratNoch keine Bewertungen
- Analisis de La Curvatura de Los Condilos Mandibulares Ueda PDFDokument6 SeitenAnalisis de La Curvatura de Los Condilos Mandibulares Ueda PDFrmontserratNoch keine Bewertungen
- Gender Diffrences TMJ Disorders PDFDokument0 SeitenGender Diffrences TMJ Disorders PDFrmontserratNoch keine Bewertungen
- Association Between Disk Position and Degenerative Bone Changes of The Temporomandibular Joints - An Imaging Study in Subjects With TMDDokument1 SeiteAssociation Between Disk Position and Degenerative Bone Changes of The Temporomandibular Joints - An Imaging Study in Subjects With TMDrmontserratNoch keine Bewertungen
- Association Between Condylar Asymmetry and Temporomandibular Disorders Using 3D-CT PDFDokument7 SeitenAssociation Between Condylar Asymmetry and Temporomandibular Disorders Using 3D-CT PDFrmontserratNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Octopi RoxDokument29 SeitenOctopi Roxlam2289Noch keine Bewertungen
- A Medical Outreach Elective CourseDokument11 SeitenA Medical Outreach Elective CourseRobert SmithNoch keine Bewertungen
- Anatomy of Writing For Publication For Nurses PDFDokument369 SeitenAnatomy of Writing For Publication For Nurses PDFfernlover3901100% (1)
- Risk Assessment For Balustrade Glass InstallationDokument3 SeitenRisk Assessment For Balustrade Glass InstallationNicos PapadopoulosNoch keine Bewertungen
- Factors Affecting Social Science Teachers' Burnout in Selected State Universities in The PhilippinesDokument41 SeitenFactors Affecting Social Science Teachers' Burnout in Selected State Universities in The PhilippinesAmadeus Fernando M. Pagente100% (1)
- Methodological Literature Review 1 1Dokument8 SeitenMethodological Literature Review 1 1api-584018105Noch keine Bewertungen
- Food Safety 3Dokument22 SeitenFood Safety 3Syarahdita Fransiska RaniNoch keine Bewertungen
- Psychoeducational and Family Therapy in Relapse PreventionDokument4 SeitenPsychoeducational and Family Therapy in Relapse PreventionEdson HilárioNoch keine Bewertungen
- Tushar FinalDokument29 SeitenTushar FinalRaj Prixit RathoreNoch keine Bewertungen
- Prepositions of Time ExplainedDokument18 SeitenPrepositions of Time ExplainedyuèNoch keine Bewertungen
- Laboratory Hygiene and SafetyDokument34 SeitenLaboratory Hygiene and SafetyResmiNoch keine Bewertungen
- 380 Final PaperDokument46 Seiten380 Final Paperapi-538048965Noch keine Bewertungen
- Journal Homepage: - : IntroductionDokument3 SeitenJournal Homepage: - : IntroductionIJAR JOURNALNoch keine Bewertungen
- Effect of Ointment Base Type on Percutaneous Drug AbsorptionDokument4 SeitenEffect of Ointment Base Type on Percutaneous Drug AbsorptionINDAHNoch keine Bewertungen
- IWA Publishing - Anaerobic Reactors For Sewage Treatment - Design, Construction and Operation - 2020-01-10Dokument1 SeiteIWA Publishing - Anaerobic Reactors For Sewage Treatment - Design, Construction and Operation - 2020-01-10JOHNY ALEJANDRO GARCIA SEPULVEDANoch keine Bewertungen
- PIDSR Other DiseasesDokument45 SeitenPIDSR Other DiseasesMichelle TuraNoch keine Bewertungen
- GoalSettingWorkbookFinal PDFDokument21 SeitenGoalSettingWorkbookFinal PDFDato KhutsishviliNoch keine Bewertungen
- NCP - Acute Pain - FractureDokument1 SeiteNCP - Acute Pain - Fracturemawel73% (22)
- Sysman Safety-Integrated-5ed en PDFDokument345 SeitenSysman Safety-Integrated-5ed en PDFErdincNoch keine Bewertungen
- The Costly Business of DiscriminationDokument46 SeitenThe Costly Business of DiscriminationCenter for American Progress100% (1)
- Thesis-Android-Based Health-Care Management System: July 2016Dokument66 SeitenThesis-Android-Based Health-Care Management System: July 2016Noor Md GolamNoch keine Bewertungen
- E136Dokument4 SeitenE136Subramanya RaoNoch keine Bewertungen
- GENETIC DISORDERS AND CYTOGENETICSDokument7 SeitenGENETIC DISORDERS AND CYTOGENETICSsmilechance8Noch keine Bewertungen
- الورقة الثالثة- القبالة-2Dokument4 Seitenالورقة الثالثة- القبالة-2Habebt MusabNoch keine Bewertungen
- Stetler Model EBP PosterDokument1 SeiteStetler Model EBP PosterEmily MNoch keine Bewertungen
- Being A Medical DoctorDokument14 SeitenBeing A Medical DoctorMichael Bill GihonNoch keine Bewertungen
- Stefan White, Andrew Sinclair (Auth.), John M. Hutson, Garry L. Warne, Sonia R. Grover (Eds.) - Disorders of Sex Development_ an Integrated Approach to Management-Springer-Verlag Berlin Heidelberg (20Dokument327 SeitenStefan White, Andrew Sinclair (Auth.), John M. Hutson, Garry L. Warne, Sonia R. Grover (Eds.) - Disorders of Sex Development_ an Integrated Approach to Management-Springer-Verlag Berlin Heidelberg (20Aakanksha MehtaNoch keine Bewertungen
- Emotional Dysregulation in Adult ADHD What Is The Empirical EvidenceDokument12 SeitenEmotional Dysregulation in Adult ADHD What Is The Empirical EvidenceVo PeaceNoch keine Bewertungen
- Psychological Impact of COVID-19 Pandemic in The Philippines PDFDokument13 SeitenPsychological Impact of COVID-19 Pandemic in The Philippines PDFAndrea KamilleNoch keine Bewertungen