Beruflich Dokumente
Kultur Dokumente
Anaesthesia MC Kh32 C PDF
Hochgeladen von
Sandeep RayarothOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Anaesthesia MC Kh32 C PDF
Hochgeladen von
Sandeep RayarothCopyright:
Verfügbare Formate
Anaesthesia Machine
II >32. 1 NEED FOR ANAESTHESIA
Surgical methods of treatment consists mainl y of operations whi ch are normally carried out under
some form of anaesthesia. Anaesthesia serves the following two functions:
1. It ensures that the patient does not feel pain and minimizes patient discomfort; and
2. It provides the surgeon with favourable conditions for the work.
When anaesthesia is given so that the patient loses consciousness, it is called' general anaes-
thesia' . In general anaesthesia, the anaes theti c agent is administered to the body so that it reaches
the brain via the blood stream. The usual method is ' inhalation anaesthes ia' in which gaseous
anaesthetic agents are introduced via the lungs. Examples of such agents are diethyl ether,
chloroform, hal othane, cyclopropane and nitrous oxide (N
2
0, laughing gas). During anaesthesia,
not only is the anaesthetic administered in the required amount but also oxygen. Any excess
carbon dioxide is also eliminated. In the superficial stages of anaesthesia, the patient can breathe
for himself-spontaneous ventilation. At a greater depth of anaesthesia, it may be necessary to
support the patient with artificial ventilation known as controlled ventilation.
32. 1.1 Del ivery of Ana est hes ia
The anaes thetic delivery system consists of an anaesthesia machine, a patient breathing circuit, a
venti lator and airway equipment. .
The machinecomprises a gas supply--;-delivery unit and an anaesthetic vapourizer.
The breathing circuitconsists of a closed loop of breathing tubing, containing two uni -directional
breathing valves and an Adjustable Pressure Limiting (APL) valve, a CO
2
absorber, a means for
venting excess gases (scavenging), a h\lII\idifu;'r, and a collapsible reservoir bag.
. A mechanical ventilatoris used for positive pressure ventilation.
. The airway management equipment includes the mask and endotracheal tube, which interface the
patient with the breathing circuit.
826 Handbook of Biomedical lnstrummtation
.> 32.2 A AESTHESIA MACHI E
An anaesthesia machine is a device which is used to deliver a precisely known but variable gas
mixture incl uding anaesthetic and Iife-sustaining gases to the system.
Generally. a variable concent ration gas mixture of oxygen. nitrous oxide and anaesthetic vapour
like ether or halothane is obtained from the machine and is made to flow through the breathing
circuit to the patient. It is composed of two subsystems (Fig. 32.1): (i) The gas supply-delivery unit.
which cons ists of tubing and flowmetres interconnected in parallel; and (ii) The anaesthetic
vapourizer, which is used to produce an anaesthetic vapour from a volatile liquid.
32.2. 1 Gas Supply System
Gases are provided to the anaesthesia machine from either a pressurized hospi tal central supply
or small storage cylinders attached to the machine.
Centralized Supply:Centralised supply systems consist of bulk or cylinder storage for main and
rese rve supply. control equipment including valves and pressure regulators. a distribution
pipeline, and numerous supply outlets. The system is so designed and operated that the necessary
supply of gases (oxygen and nitrous oxide) is always available. The gas supplied by the hos pital
is regulated and maintained aI 275-345 kPa (40-50 psi) at the wa ll outl et.
Gases are supplied to the anaesthesia machine inlet from the central system via a flexible hose
connected to the operating room wall outlet. In order to prevent interchanging the gas supply wall
outlet with the incorrect anaesthesia machine inl et. for example, nitrous oxide for oxygen. non-
interchangeable connectors are used at each end of the hose. The two types of non-interchangeable
connections most commonly used are the Diameter Index Safety System (DISS) and non-inter-
changeable qu ick couplers. Each type of connection incorporates a male and female end that is
specially designed for each type of gas. In addition to the connector design, colour-coded hoses for
each speci fic gas are utilized.
Gas Cylinders: A second gas supply source is the cylinders located in yokes attached 10 the
anaesthes ia machine. This supply can be utilized as either the main source when a central gas
supply does not exist , or a reserve when central gas supply is available.
Yoke:Each anaes thesia machine has at least one yoke for an oxygencylinder but most are provided
with two. In addition to oxygen, most machine designs include a nit rous oxide yoke. In order to
prevent incorrect placement of a tank into the wrong yoke. two pins located in the yoke must fit
into corresponding holes drilled into the tank neck. The placement of these pins and corresponding
holes is unique for each gas. This identification system, which is referred to as the ' Pin Index Safety
System' , has been standardized to prevent the accidental fitting of a wrong cylinder to the yoke.
Pressure Regula tor. Machine pressure regulators red uce cylinder gas pressures to 275kPa (40psi)
before the gas flows through the machine. The regul ator has one high-pressure inlet. one high-
pressure outlet and two-low pressure outlets. The high pressure inlet"is connected with the
cylinder through a non-return valve. The non-return valve prevents the flow into an emptycylinder
or back into the central piping system and also enables its removal and replacement when the
reserve cylinder is turned on without interrupting the supply of gas.
;,..
"
[
s
[
Reservlor
bag
- To patient
Expiratory
valve
CO
2
absorber
115 --..::t--lJ' valve
Exhaust
valve .
rr
By-pass
valve '
Direct reading
vapourizer
Rotameter
I
Needle
valve
N
20
serviceInlet
Pressure
regulator
Cheek
valve
Pressure
gauge
N
20
'-
2
t
t
2
Service Inlet
-
2
Flush valve
Bubble-through
vapourlzer
>Fig . 32.1 ScI,emtl/i c diagram of all allaestlresia machine ami patient breatlri"g circuit
"
828 Handbook of Biomedical Instrumentation
Pressure Gauge: Pressure gauges are attached to the cylinders to indicate the contents of the gases
in the cylinders. For oxygen, the operating range of the gauge isO to 150 kg /cm
2
. Whenever the
newoxygen cylinder is hooked up and taken in line, the indi cator should be above this mark. With (
the gradual usage of the gas, the reading would drop gradually, when the indicator shows that the
pressure has fallen below the minimum level of acceptance, the 'llinder should be refilled. If for
any reason, the pressure gauge shows a reading above ISO kg/ em during use, the cylinder should
be disconnected immediately and repl aced .
Fail Safe System: From the supply, the gas flows into the inlet of the anaesthesia machine and is
directed through the pressure safety system (fail-safe system) towards the flow delivery unit. The
pressure safety system will not allow nitrous oxide to flow unl ess an oxygen supply pressure
exists in the machine. The fail-safe system consis ts of a master pressure regulator valve located in
the oxygen supply line. From the master regulator, a reference pressure is provided to the slave
regulator valve controlling the pressure and flow of the nitrous oxide line. When sufficient oxygen
pressure of 275 kPa (40 psi) is present in the master regulator , the reference pressure enables the
slave regulator valve to open and for nitrous oxide to flow. Unfortunately, pure nitrous oxide can
be delivered with only oxygen supply pressure present; oxygen flow is not requined.
Regulations now require oxygen-ni trous oxide ratio safeguards, which need a minimum
continuous low flow of oxygen varying from 200 to 300 mL/min, as indicated by the low-flow
rotameter. In newl y designed machines, ingenious mechanical devices prevent the delivery of gas
mi xtures with an oxygen concentration below a low limit. Oxygen-nitrous oxide rati os vary from
25:75 to 30:70, depending on the manufacturer .
Gas Deli very Units: From the fail-safe system, the gas is directed to the flow delivery unit. Two
methods have been used to accomplish delivery and control of the gas mixture: gas proportioning
and gas mixing.
In a gas proportioning system, the delivered concentration of each gas constituent is the
function of a pre-determined, precisely controlled ratio of proportionality which is independent of
the total gas flow. For example, for a desired mi xture of 70%nitrous oxide and 30%oxygen, the
metered ratio of mass delivery wi ll always be 7:3,regardless of the total flow rate. Concentration is
only a fun ction of the proportional relationship between constituents. It does not rely on setting
individual gas flows. An oxygen-nitrous oxide bleeder used in a manner similar to the oxygen-
air blenders commonly used wi th mechanical ventilators performs this function.
Most current anaesthesia machines use gas mi xing. In this technique, the flow rate of each
constituent is independently controlled and measured by a deli very unit consisting of a needle
valve and a rotameter. The needle valve functions as a flow controller and a means of turning the
gas on and off. The rotameter is a vari able orifice flowrnetre and consists of a transparent tube with
a tapered internal diameter and a floating bobbin flow indicator.
During the administration of anaesthesia, it may be necessary to fill the patient breathing
circuit with oxygen at a rat e higher than what the gas delivery unit can supply. For ~ x m p l e such
a situation exists any time the patient is disconnected to the breathing circuit. This hi gher flow of
oxygen is supplied via the oxygen flush valve and line. The oxygen flush system provides a high
flow ranging from 35 to 75 L/min at a high pressure (20-45 psi, 270-590 kPa) directly into the
patient breathing circui t.
AnaesthesiaMachine 829
Each gas hasa specific delivery unit. These units are connected in pa rallel and exhaus t into a
common manifold prior to leaving the machine. The final concentration and total flow determined
by mixing the component flows are dependent functions and subject to the accuracy of the control
and measurement equipment.
32.2. 2 Vapour Delivery
The various liquids that possess anaesthetic properties are too potent (strong) to be used as pure
vapours. They are thus diluted in a carrier gas such as air and/or oxygen, or ni trous oxide and
oxygen. The device that allows vapourization of the liquid ana esthetic agent and its subsequent
admixtu re with a carrier gas for administration to a patient is called a 'vapourizer'. Vapourizers
thus produce an accurate gaseous concentration from a volatile liquid anaesthetic. The anaesthetic
vapo ur can then be safely added to the previousl y metered oxygen and nitrous oxide as the
mixture leaves the mixing manifold.
Vapourizers are available in one of the two basic designs: the flowmetre controll ed or the
concentration-ealibrated. In either device, the anaesthetic vapours are picked up from the
vapo urizer by a carri er gas consis ting either of pure oxygen or an oxygen-ni trous oxide mixture
that bubbles through or passes over the liqui d. The liquid surface area to gas interface is designed
to ensure the most efficient vapourization process.
As a resul t of vapourization, a drop in liquid temperature is produced. As the liquid tempera-
ture decreases, a thermal gradi ent is established between the liquid and the surroundings. This
results in a decrease in the quantity of the vapour produced. Inorder to maintain the performance
of the vapourizer, the temperatu re drop is minimized or prevented by the incorporati on of a
thermal sour ce. This is achieved by using a water bath or surrounding the vapo urizing liquid
with a heating element. These devices may also control the temperature of the carrier gas entering
the vapourizer.
The ma terials selected for vapourizer construction require both a hi gh specific heat and high
thermal conductivity. Materials with high specific hea ts will change temperature more slowly
and maintain an appropriate thermal inertia. The higher the thermal conductivity, the higher the
conduction of heat from the surroundings. Because of its availability and lower cost, copper has
been one of the most common materials used. Although not ideal, copper has a moderate specific
heat and a high thermal conductivity. Early vapourizers were accordingl y called "copper kettles".
In order to provide a stable and predictable concentra tion of anaesthetic vapour, the
vapourizers include a suitable method of ob taining calibrated dil ution of va pour to avoid
administration of too powerful volatile anaesthetic agents to the patient. This can be done by
several means and the vapourizers are accor dingly classified into various categories discussed
below.
VariableBypass the carr ier gas flow from the flowmeter is split into two streams
in a known rati o: one streamwhich is called 'chamber flow' , flows over the liquid agent while the
other streamgoes through the bypass path and does not enter the vapo urizing chamber. The fina)
concentration can be controlled by varying the splitting ratio between the vapourizer gas and the
bypass gas using an adjustabl e valve (Fig. 32.2).
830 Handbook of Biomedical Inst rumentation
,
,
,
t
,
,
.... _-- ...
c
1
C= vapourizer
chamber
L = Liquid
> Fig. 32. 2 A schematic diagram ofa variable bypass vapourizer. A flo w spli tting
valve that can be rotated to alter the relative diameters ofthe vapourizer
and bypass channels
> Fig. 32.3 Schematic diagram of a
measuredflo w vapourizer
-
L
J---'l!'w"lv--{ v, E
.------- - -----,
The splitting ratio of the two flows depends on the ratio of resist ances to their flow, which is
controlled by the concentra tion control di al and the automatic tempera tu re compensation valve.
Usua lly, less than 20%of the gas becomes enriched-satu rated with va pour and more than 80% is
bypassed, to rejoin at the vapouri zer outlet. The output of curr ent variable bypass va pourizers is
relatively constant over the range of fresh gas flows from approxima tely 250 mL/min to 15 L/ min.
The output of va pourizers is linear at the ambient temperature (2-35C) due to automatic
temperature compensati ng devices that increase
carri er gas flow as the liquid vol at ile agent tempe-
rature decreases. Also, they are composed of metals
with high specific heat and thermal conductivi ty. t
Check valves are provided to prevent back pressure
effect on the va pourizer from the breathing circuit
due to positive pressure ventilation.
Measured-flow Vapourizers: In these devices, the
anaestheti c agent is heated to a temperature above t
the boiling point (so that it behaves as a gas) and is
then met red into the fresh gas flow (Fig. 32.3).
Var ious anaesthetic agents have Widely di ffe-
rent pot encies and physical properties and hence
require vapourizers constructed specifically for v
2
each agent. They are thus ' agent-specific'. They are
only calibrated for a single gas, usuall y with keyed
filters that decrease the likelihood of fill ing the
vapourizer with the wrong agent.
Anaesthesia Machine 831
Vapourizers are provided with various safety related inter-locks which ensure that:
- Only one vapourizer is turned on;
- Gas enters only the one which is on;
- Trace vap our output is minimized when the vapo urizer is off;
- Vapourizers are locked into the gas circui t, thus ensuring that they are seated correctly; and
- Other important safety featu res are followed including keyed filters and secured mounting
to minimi ze tipping (tilting) which may obstruc t the working of the valves.
32.2.3 Delivery System
Patient Breathing System:The function of a patient breathing system is to deliver anaesthetic and
respiratory gases to and from the patient. It describes both the mode of operation and the apparatus
by which inhalation agents are delivered to the patient. The breathi ng system may be
1. Rebreathing Type: This refers to re-breathing of some or all of the previously exhaled
gases, including carbon di oxide and wa ter vapour.
2. Non-rebreathing Type: In this a fresh gas supply is delivered to the patient and re-breath-
ing of previously exhaled gases is prevented . Usua lly, non-rebreathing type systems are
applied in practice. This is achieved by using:
- Non-rebreathing uni-directional valve;
- Carbon dioxide absorption system; involving;
Uni-di rectional (circle) system; and
Hi-directional (to-and-fro) system. .
Figure 32.4 shows the principle of a non-rebreathing system which uses uni-directional
non-brea thing valve. Fresh gas entering the inspiratory part is either sucked in by the patient's
Inspiratorylimb
Expiratorylimb
.---_A'--_---,
FGF-
I
(Fresh gas
flow)
/y
Patient
(a) Inspiration
Inspiratorylimb
_ _ A'-_ _ -,
Expiratorylimb
,---_ _ A'- _
'\
Patient
(b) Exhalat ion
> Fig. 32.4 Non-breathingvalve
Handbook of Biomedical Instrument ation 832
~
inspiratory effort or blown in during controlled ventilation. The non-rebreathin g valve is so
designed that when it is open to admit inspiratory gas, it does not permit the flow from the
expiratory part to get through it. When the patient exhales, the reverse happens, as the inspiratory
valve is occluded and the expiratory valve is opened to allow expi ratory.,gases to escape. The
inspi ratory system usually includes a rubber bag of two-litre capacity which acts as a reservoir for
fresh gas . The reservoir bag is refilled wi th fresh gas during the expiratory phase. It can also be
compressed normally to provide assisted or controlled ventilation. The fresh gas supply is
linked to a length of corrugated breathing hose (minimum length -lDem with an internal volume
of 550 ml). This represents slightly more than the average tidal volume in an anaesthetized adult
breathing spontaneously. This is, in turn, connected to a variable tension, spring-loaded flap
value for venting off exhaled gases. This valve is located as close to the patient as possible, and is
called an APL (adj us table pressure limiting) valve. The APL valve works as a pep-off valve to
ens ure that the pa tient is not subjected to the surges in the gas supply. When the gas encounters
resistance from the patient, the excess gas pop. out. The arrangement is shown in Fig. 32.5. In this
case, carbon dioxide elimination is achieved by the flushing action of the fresh gas introduced
with the breathing system, rather than by separation. Obviously, this syste m retains the potential
for re-breathing of carbon dioxide when the fresh gas flow rates are reduced.
APt.
> Fig. 32.5 Mapleson breath ing system used with spontaneous breathing FGF
(Fresh Gas Flow ), APL (Adj ustable Pressure Limiting) valve, RB
(Reservoir Bag)
Circle System: The circle is the most popular breathing circui t and is a closed loop of large-bore,
low-pressure tubing divided into an inspiratory and an expiratory limb. Contained within this
loop are two uni-directional valves, a CO
2
absorber, circuit gas venting (scavenging), an adjustable
pressure-limiting valve, reservoir bag, and airway management equipment including masks
and endotracheal tubes. The patient is connected to the absorber by two corrugated hoses, one
inspiratory and the other expiratory.
Fresh gas is introduced proximal to a uni-directional inspiratory breathing valve. During
inspiration, gas moves through the absorber from either the reservoir bag or ventilator bellows and
inspiratory valve into the inspiratory limb of the circuit. The pressure difference between the
inspiratory and expir atory limbs keeps the uni-directional expiratory valve closed. During exhala-
tion, the pressure differential reverses. The inspiratory valve closes and the expiratory valve opens,
allowing the exhaled gas to flow into the reservoir bag or ventilator bellows and absorber. The
APLor the pep-off valve enables the anaesthetist to control the circuit volume and pressure by the
reguIation of gas venting from the circuit. Circuit exhaust is either carried into the room or collected
by a gas scavenging system.
Anaesthesia Machine 833
Uni-directional breathing valves are available in several designs. The disk valve is the most
common in modem systems. This valve consists of onl y one movable part, a flat disk. The disk is
made of either plastic or metal and is held against the valve seat by ei ther gravity or a mechanical
spring. The valves are placed in trans parent devices so that their action may be observed.
The APL is designed to regulate circuit pressures by manuall y adjus ting the spring tensi on
against a disk. When circuit pressure overcomes the valve resistance, the disk is lifted from its seat
and gas is allowed to exhaust from the circuit. The circuit volume and pressures throughout the
delivery of anaesthesia are continuously observed so that the APL valve can be appropriately
adjusted .
The absorber contains a carbon dioxide absor bent (soda lime) in a closed container. Soda lime
is used in the form of granules so that they ha ve a large volume and large surface area. Thus, the
expired air remains in contact with the soda lime for a relat ively long period of time, increasing the
efficiency of absorption. Granules of an optimumsize are selected as, too large a size leads to poor
contact and poor absorption, while too small a size clogs the soda lime bed and causes resistance
to the gas flow. The exhaled gas is made to flow through the absorber where the is removed.
The remaining gas is mi xed with fresh gas flowing from the machine and re-breathed via the
inspiratory limb. When the soda lime gets consumed, its colour changes from pink to yellowish.
The reservoir or breathing bag is highly compliant, with an easily expanded volume. The bag
allows the accumulation of gas during exhalation so that a reservoir is available for the next
inspiration. It provides a means for visually monitoring the spontaneous brea thing patt ern of
the pa tient and buffers increases in breathing circuit pressure. The bag also provides a means
that can be used to manually ventilate the patient. Either passive or acti ve scavenging sys tems
are utilized in removing the circuit exha ust. In passive scavenging, anaesthetic waste gases are
vented directly int o the existing room ventil ation systems. The tubing connects either the ventilator
or the APL valve exhaus t port of the breathing circuit to the hospital ventilation system. In
active methods, the anesthetic circuit connects directly to a high-flow vacuum system via an
appropriate int erface.
32.2.4 Humidification
Dry gases supplied by the anaesthesia machine may cause clinica lly significant desiccation of
mucus. This may contribute to retention of secretion and the mucus flow may cease. Lung compli-
ance will consequently fall . Therefore, air or anaesthetic gases need to be humidified.
Absolute Humidity: This isthe maximum mass of water vapour which can becarried by a given
volume of air (mg / L). This quantity is pre-dominantly determined by temperature. Warm air can
carry much more moisture:
Relative Humidity (RH} This is the percentage of the amount of humidity present in a sample, as
compared to the absolute humidity possible at the sample temperature.
- It is ideal to provide gases at body temperature and 100%RH to the patient's airway. The humi-
dification measures tha t are commonly employed include heated airway humidifiers, nebulizers
and heat and moisture exchangers.
(i) In the heated humidifiers, the ai r passes over the surface of the heated wa ter and
vapourization takes place. The temperature of the water is thermostaticall y controlled.
Handbook of Biomedical Inst rumentation 834 --"- . .__
1"
(a)
(b)
Principle ofthe nebuli zer
Employing the benwulIi effect,
a j et of air may be used to draw
a Iiquid up a small tubefr om a
reservoir and to entrain it as
droplets
(b) TIle droplets may be made to
impinge on an 'anuil', so caus-
ing them to be brokell up into
st ill smaller droplets
> Fig. 32.6
(a)
Preferably, two thermostats in series are
used, S<' that if one thermostat fails, the
other would still cut off the electric supply
before a dangerous temperature is reached.
The temperature sensor is usually placed
near the patient -end of the delivery tube so
as to ens ure the maximumefficiency.
(ii) Nebulizers are used to supply moisture in
the form of dropl ets. A jet of air or gases
may be used to entrain water drawn from a
reservoir (Fig. 32.6). As the water enters the
jet, it is broken up into a large number of
droplets, i .e. it is nebulized. Nebulizers
based on this principl e are also used in
some ventilators. In ultrasonic nebulizers,
water is broken int o droplets by continu-
ous bombardment of ultrasound energy
which vigorously vibrates the water.
(iii) Heat and moisture exchangers are based on
the pri nciple of conserving the patient's
own heat and moisture without external
energy or water supply. The fibre-packed
cartridges conta in a moisture-absorbent
materi al that absorbs the patient's exhaled
water and heal. During inspiration, the
dry, inspired circuit gas flows thr ough the
wa rm, moisturized absorbent where it is
warmed and humidified. Fibre cartridges
are not as efficient at warming as humidi-
fiers. However, they do signi ficantly retard
patient heat loss.
For protection of pati ents from infection, clean or sterile disposable breathing circuits and bacterial
filters have been advocated and widely used to red uce post-operative respiratory infections.
Although simple in design, breathing circuits can be sources of many problems. The most
common and serious problem is the potenti al for disconnection at any of several locat ions.
Numerous invest igat ors have shown that 10-15% of preventable mi shaps result directly from
airway leaks and disconnects. The causes for leaks and disconnects include poor fit due to
incorrect size, incorrect shape taper connections, inappropriate fabri cati on of materials, thermal
expa ns ion, broken fit tings and the absence of a locking de vice.
32 .2.5 Ventilators
An integral component of the anaesthetic delivery system is the ventilator. The ventilator provides
a positive force for transpor ting respirat ory and anaesthetic gases into an apneic patienl. The
Anaesthesia Macltine
ventilators provide positive pressure venti lati on at a controlled minute vol ume (Tidal vol ume,
Rate). They operate either electronicallyor mechani cally with pneumatic or electric power source.
Most of the currentl y used ventilators consist of a bellows contained within another housing.
The bellows communicate direc tly with the brea thing circuit and causes a pre-selected volume of
gas to flow into the patient. The flow of gas into the circuit resul ts from collapsing the ventilator
bellows by pressurizing the surrounding gas volume contained within the bellows housing.
The ventilator is either located wi thin the mainframe of the anaesthesia machine or is attached
as an accessory unit. The outlet of the ventilator connects directl y to the patient breathing circuit of
the anaes thetic delivery sys tem at the location and in place of the breathing reservoir bag. The
ventil ator thus functions as a controller for both ventilat ion and circuit gas supply by repl acing
the functions of the reservoir bag and APLvalve.
32.2.6 Pat ient Circuit
The patient circuit consists of black corrugated anti-static rubber tube, a chrome plated tube fitting
(Tjoint), a two litre re-breathing bag, a Heidbrink valve and a face mask with an elbow fitting. The
face mask is designed to fit the pati ent' s face perfect ly wit hout any leaks and yet to exert the
minimum of pressure which might depress the jaws and cause respiratory obstruction.
1111> 32.3 ELEORONICS I THE ANAESTHETIC MACHI NE
Any delivery system is expected to meet accurately and safely, the patient's varying requirements
for respiratory and anaesthetic gases. The system must be able to monitor the function of the
delivery system itself and the effect of the anaesthesia on the patient. Also, dur ing the entire
procedure the machine performance should not only be monitored and controlled, but its
status should be continually assessed and recorded. In order to meet these requ irements, the
impact of electronics on the design and functioning of the anaesthetic machine has been
phenomenal.
The totally pneumatic anaes thetic machine still has many meri ts, which include its being easy
to understand and easy 'to maintain, as also its cheaper cost and reliability. However, certain
problems are encountered whi ch directly affect the performance and safety of a pneumatic anaes-
theti c machine. This is ove rcome through the utiliza tion of newer technologies and automation
of instrumentation and anaesthetic delivery. Microprocessor-based anaesthetic equipment
facilitat es improvements in:
Gas supply and proportioning syst ems;
Breathing circui ts;
Gas scavenging and humidification devices; and
Ventilators.
The use of microprocessor technology allows us to fully integrate control and safety functions
and protects the patient from: gas suppl y failure, electri cal supply failure, hypoxic mixtures,
disconnections, vapourizer function, excessive airway pressure exhaled minute vol ume outside
pre-set limits, oxygep or volatile agents outside the pre-set limit , end-tidal CO
2
outside present
limits and technical failure. All abnormal conditions cause an alarm to appea r on the monitor
panel, which also displays the nature of the fault.
836 Handbook of Biomedical Instrumentation
Computer application with appropriate data processing inputs and outputs, automation
and integration of machine func tions and record-keeping are increasingly becoming possible.
Ergonomically designed machines with easy to read and interpret display systems are also being
commonly used.
Anaesthesia has a profound effect upon all physiological systems. Most of these effects are
deleterious, and therefore, it is import ant to know how the human body is affected by anesthesias.
With a view to increasing patient safety and achieving a good degr ee of risk management, all
systems affected by anaesthetic drugs must be monitored. This is done by using moni toring
equipment wi th visible and audible alarms as illustrated in Chapter 6.
> Fig. 32.7 AEP (Audit ory Evoked Potentialrmonit or to measure individual's level
of consciousness during general anaesthesia. (Courtesy: Alars Medical
Systems, U.K)
Since individual responses to a particular dose of anaesthetic vary considerably, it is advisable
to measure the effect of the anaesthetic on a patient' s level of consciousness. One method to do so
is to measure Auditory Evoked Pot enti als (AEP), which is a neuro-physiological indicator of the
changes in the level of consciousness during anaesthesia. This is an electrical signal contained
within the EEG, which is obtained by delivering an auditory stimulus to the patient' s acoustic
nerve. The fast extraction of the complex AEPsignal, the brain' s response to the auditory stimulus
of the acoust ic nerve is obtained by mapping the signal and establishing an index which
is developed as a gr aphic curve and a single number on the monitor screen (Fig. 32.7). This
index which is calculated from a proprietary ma thematical modelling method, quantifies the
level of anaest hesia. For example, typically, if this index is higher than 60, the patient is
awake, and decreases in line wi th decreasing level of consciousness (loss of conscious typically
occurring below 30). Re-usable apply stimula tion to the acoustic nerve to obtain
AEP, which is then measured by a set of three disposable electrodes; two electrodes are applied
in the forehead and one behind the ear to estimate the level of consciousness in a fast and
non-invasive manner.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- High Frequency Oscillatory Ventilation (HFOV) تغريدDokument16 SeitenHigh Frequency Oscillatory Ventilation (HFOV) تغريدtaghreednurseNoch keine Bewertungen
- PulmoVista 500 - APPLICATION - Identify Onset of Derecruitment - 032018Dokument2 SeitenPulmoVista 500 - APPLICATION - Identify Onset of Derecruitment - 032018tomNoch keine Bewertungen
- Monitoring and Troubleshooting in Mechanical VentilatorDokument77 SeitenMonitoring and Troubleshooting in Mechanical VentilatorRashma Little RobinNoch keine Bewertungen
- Newport E360Dokument188 SeitenNewport E360Bắc Trần XuânNoch keine Bewertungen
- Respiratory Disorders NCLEX ReviewDokument22 SeitenRespiratory Disorders NCLEX ReviewPotchiee Pfizer50% (2)
- Concept Map Complex Care 2017Dokument7 SeitenConcept Map Complex Care 2017api-401537905Noch keine Bewertungen
- Effectiveness of b-CPAP for infant respiratory distressDokument17 SeitenEffectiveness of b-CPAP for infant respiratory distressWaltas KariukiNoch keine Bewertungen
- Smiths Pneupac Ventipac OperatorDokument66 SeitenSmiths Pneupac Ventipac Operatorzebubu1Noch keine Bewertungen
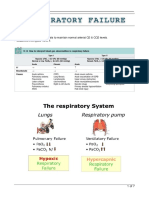
- Respiratory FailureDokument7 SeitenRespiratory FailureLulu100% (1)
- Mechanical VentilationDokument108 SeitenMechanical Ventilationrizal aljufri100% (1)
- 1505-1018a VentiladorDokument202 Seiten1505-1018a VentiladorFranklin Hernàn Avila PachecoNoch keine Bewertungen
- Status AsthmaticusDokument22 SeitenStatus AsthmaticusGali Kesuma100% (1)
- Penlon AV-S - Technical Training Course PDFDokument174 SeitenPenlon AV-S - Technical Training Course PDFluisNoch keine Bewertungen
- Basic Nursing Fundamentals EliminationDokument35 SeitenBasic Nursing Fundamentals Eliminationlisa100% (1)
- CRT Exam Review Guide Chapter 12Dokument29 SeitenCRT Exam Review Guide Chapter 12Dharlyn MungcalNoch keine Bewertungen
- ASV GalileoDokument43 SeitenASV GalileoalvyandaniNoch keine Bewertungen
- Case Study An Older COVID-19 Patient in A Turkish IntensiveDokument7 SeitenCase Study An Older COVID-19 Patient in A Turkish IntensiveAJENGNoch keine Bewertungen
- Respiratorymuscle Assessmentinclinical Practice: Michael I. PolkeyDokument9 SeitenRespiratorymuscle Assessmentinclinical Practice: Michael I. PolkeyanaNoch keine Bewertungen
- Airway Assessment & Management of Primary Trauma SurveyDokument91 SeitenAirway Assessment & Management of Primary Trauma SurveyNabighah ZukriNoch keine Bewertungen
- SV300 Service Training-Basic - V2.0 - ENDokument83 SeitenSV300 Service Training-Basic - V2.0 - ENFrancisco BaezNoch keine Bewertungen
- 13managing The Critically Ill Child-Freemedicalbooks2014Dokument360 Seiten13managing The Critically Ill Child-Freemedicalbooks2014avi_1388100% (1)
- 241 TracheostomyDokument12 Seiten241 Tracheostomyalbert hutagalungNoch keine Bewertungen
- Clinical Intensive Care Medicine PDFDokument980 SeitenClinical Intensive Care Medicine PDFYysitaa Gar Rey100% (8)
- Chest TraumaDokument23 SeitenChest TraumaMutaz DredeiNoch keine Bewertungen
- Concept Map Critical CareDokument6 SeitenConcept Map Critical Careapi-508559825Noch keine Bewertungen
- Gas monitoring with ultrasound sensorsDokument77 SeitenGas monitoring with ultrasound sensorsnabila quasimahNoch keine Bewertungen
- Sle 5000 EnglishDokument8 SeitenSle 5000 EnglisheliyantiarozaNoch keine Bewertungen
- ICU Ventilator Dyssynchrony DiagnosisDokument12 SeitenICU Ventilator Dyssynchrony DiagnosisBrenda Serrano LaraNoch keine Bewertungen
- FDA Guidance - Reviewer Guidance For Ventilators (Draft) PDFDokument31 SeitenFDA Guidance - Reviewer Guidance For Ventilators (Draft) PDFwingNoch keine Bewertungen
- PREDICTIVE ASSOCIATIONS of Music, Anxiety and Sedaative 2017Dokument12 SeitenPREDICTIVE ASSOCIATIONS of Music, Anxiety and Sedaative 2017Jorge Muñoz AyalaNoch keine Bewertungen