Beruflich Dokumente
Kultur Dokumente
7 8 Infection
Hochgeladen von
Prince AhmedOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
7 8 Infection
Hochgeladen von
Prince AhmedCopyright:
Verfügbare Formate
13/11/2012
1
Infection of The Jaws and Periosteal
Reactions
Dr. Mustafa Alkhader
Assistant Professor of Oral Radiology
White & Pharoah, Oral Radiology Principles and Interpretation 6
th
.
Ed.
Ch. 20
I nflammatory Lesions
Most common pathologic conditions of the
jaws
Teeth create a direct pathway for
inflammatory agents and pathogens to
invade the bone when caries and
periodontal disease are present
General clinical features
Cardinal signs of
inflammation: Swelling,
redness, heat, pain, and loss
of function.
Acute lesions: recent and rapid onset, pronounced pain,
fever and swelling.
Chronic lesions: prolonged gradual course, mild pain,
intermittent fever, slow swelling. Symptoms may be entirely
sub-symptomatic.
General Radiographic features
Location:
Periapical: epicenter at apex of a tooth.
Periodontal lesions: at alveolar crest, furcation or even up to root
apex.
Osteomyelitis: posterior mandible, rare in maxilla.
Periphery:
ill defined.
Internal structure:
Bone resorption, formation or combination of both.
Sequestra: a radiopaque island of non-vital bone surrounded by
ill-defined radiolucency.
General Radiographic features
Effect on surrounding structures:
Bone resorption, formation or combination of
both.
Widening of PDLS.
Root resorption.
Cortical bone resorption.
Periosteal elevation and new bone formation.
13/11/2012
2
Rarefying Osteitis
A radiographic interpretation, not a diagnosis.
It refers to a localized inflammatory
response. The diagnosis of rarefying osteitis
will be abscess, cyst, or granuloma.
Infection of The Jaws and Periosteal Reactions Infection of The Jaws and Periosteal Reactions
Infection of The Jaws and Periosteal Reactions Infection of The Jaws and Periosteal Reactions
Sclerosing Osteitis
May be present around the periphery of
rarefying osteitis or by itself
Infection of The Jaws and Periosteal Reactions Infection of The Jaws and Periosteal Reactions
13/11/2012
3
Infection of The Jaws and Periosteal Reactions
Periapical Inflammatory Lesions
Caries
Periodontitis
Trauma
Necrotic Pulp Apical periodontitis
Periapical
Abscess
Periapical
Granuloma
Osteomyelitis
Periapical
cyst
Size
Epicenter
Sequestra
Infection of The Jaws and Periosteal Reactions
Periapical Inflammatory
Lesions
At least 60% demineralization must occur
before the lesion can be seen on a
radiograph. Therefore, it is inappropriate to
use a radiograph as a vitality test
Histologically, the lesion is apical
periodontitis, which is defined as
aperiapical abscess or periapical granuloma
Periapical Inflammatory
Lesions
Clinically, the symptoms may include pain,
swelling, fever, lymphadenopathy, or may
be asymptomatic
It is important to note that the clinical
presentation may not correspond with the
histopathological or radiographic findings
Radiographic features
Location:
Periphery:
Internal structure:
Effect on surrounding structures:
Periapical Inflammatory Lesions
13/11/2012
4
Halo Effect
Infection of The Jaws and Periosteal Reactions Infection of The Jaws and Periosteal Reactions
Mucositis
(Localized Mucositis)
Infection of The Jaws and Periosteal Reactions Infection of The Jaws and Periosteal Reactions
Periapical Inflammatory Lesions
Differential Diagnosis:
PCD
Enostosis
Granuloma.
Cyst.
Healing scar
Malignancies (leukemia)
Metastatic lesions.
Management:
Elimination of cause: Endo Tx / Extraction.
Antibiotics
Pericoronitis
Definition: inflammation of
tissue surrounding a partially
erupted tooth which extends to
the bone.
Clinically:
Pain and swelling
Trismus
Ulcerated oberculum.
13/11/2012
5
Pericoronitis
Radiographic features
Either no changes or
Localized rarifaction or sclerosis
Mandibular wisdom is the most commonly
affected.
Area of rarifaction that causes increase in the
width of folicular space.
Pericoronitis
Radiographic features
Normal
Pericoronitis
Enlarged follicular space
Sclerotic bone
Osteomyelitis
Inflammation of the bone
May spread to involve:
Marrow
Cortex Periosteum
Cancellous portion
Caused by pyogenic organisms from abscessed
teeth, trauma, or surgery
Source of infection can not always be identified
Bacteria and by-products stimulate an
inflammatory reaction in bone
In young patients, the periosteum is lifted by
inflammatory exudates. New bone is laid down.
This is called Garres Osteomyelitis
Presence of sequestra is a hallmark of
osteomyelitis. These can be seen in both plain
films and CT
Acute and chronic forms exist
Acute form demonstrates purulent drainage
Paresthesia of the lip may be present,
suggesting a malignancy
Location
The most common location of
osteomyelitis of the jaws is the posterior
body of the mandible
Involvement of the maxilla is rare, perhaps
due to its excellent vascularity
13/11/2012
6
Borders
The borders of these lesions are illdefined,
gradually blending into the normal
trabecular pattern
Internal architecture
Initially, there is a slight decrease in the
radiodensity of the bone, with the trabeculae
becoming less well defined
There may be scattered areas of lucency in the
area
Later, areas of sclerotic bone are seen
Sequestra are most apparent in the chronic forms
Chronic osteomyelitis may arise from the acute
form or de novo
In the chronic form, the balance tips in favor of
osteoclastic activity
Trabeculae may be completely obscured, yielding
a uniformly opaque appearance to the bone
Sequestra are generally larger in the chronic form
Effects on adjacent structures
Surrounding bone may be resorbed or laid down
May cause resorption of the cortex
In Garres osteomyelitis, the cortex is expanded
through deposition of new bone. The radiographic
appearance of these new layers of bone is termed
onion skin or proliferative periostitis
Chronic suppurative Osteomyelitis
Axial CT showing multiple
sequestra
Coronal CT showing extension
to TMJ
13/11/2012
7
DD?
Osteoradionecrosis
High radiation dose (50 Gy) lowers the bone
blood supply and reparative power of osteocytes.
A minor infection or trauma may lead to
osteoradionecrosis.
More in posterior mandible.
More in male (susceptibility of carcinomas).
Osteoradionecrosis
Clinically:
It resembles ch.supp.osteo. But it shows :
More spread
Late sequestration.
Radiographically:
Areas of RL,RO.
More spread.
No actual difference except with history of
radiation to head and neck.
Das könnte Ihnen auch gefallen
- Salivary Gland Radiology PresentationDokument40 SeitenSalivary Gland Radiology PresentationPrince AhmedNoch keine Bewertungen
- Craniofacial Anomalies Part 3Dokument17 SeitenCraniofacial Anomalies Part 3Prince AhmedNoch keine Bewertungen
- Salivary Gland - Part3Dokument27 SeitenSalivary Gland - Part3Prince AhmedNoch keine Bewertungen
- 6,8,9Dokument1 Seite6,8,9Prince AhmedNoch keine Bewertungen
- Thorax Lab... ZezoDokument104 SeitenThorax Lab... ZezoPrince AhmedNoch keine Bewertungen
- Edition CH #23 Other Bone Diseases: Stuart C. White & Michael J. PharoahDokument21 SeitenEdition CH #23 Other Bone Diseases: Stuart C. White & Michael J. PharoahPrince AhmedNoch keine Bewertungen
- Abdomen LabDokument140 SeitenAbdomen LabPrince AhmedNoch keine Bewertungen
- Chapter 3,4Dokument1 SeiteChapter 3,4Prince AhmedNoch keine Bewertungen
- 1 PrognosisDokument13 Seiten1 PrognosisPrince AhmedNoch keine Bewertungen
- Cons VII Script 1 Bleaching Discolored TeethDokument19 SeitenCons VII Script 1 Bleaching Discolored TeethPrince AhmedNoch keine Bewertungen
- Chapter 2Dokument1 SeiteChapter 2Prince AhmedNoch keine Bewertungen
- Pedo V Script 1management of Developing OcclusionDokument12 SeitenPedo V Script 1management of Developing OcclusionPrince AhmedNoch keine Bewertungen
- Implant Script 1implants History DefinitionDokument10 SeitenImplant Script 1implants History DefinitionPrince AhmedNoch keine Bewertungen
- Oral Surgery Script 1 Facial TraumaDokument13 SeitenOral Surgery Script 1 Facial TraumaPrince AhmedNoch keine Bewertungen
- O.M II Script 1 PigmentationsDokument16 SeitenO.M II Script 1 PigmentationsPrince AhmedNoch keine Bewertungen
- 1 PrognosisDokument13 Seiten1 PrognosisPrince AhmedNoch keine Bewertungen
- Ortho 1Dokument9 SeitenOrtho 1Prince AhmedNoch keine Bewertungen
- 1 Occlusal SplintsDokument17 Seiten1 Occlusal SplintsPrince AhmedNoch keine Bewertungen
- Oral Surgery Script 1 Facial TraumaDokument13 SeitenOral Surgery Script 1 Facial TraumaPrince AhmedNoch keine Bewertungen
- Developmental Disturbances of The Face and Jaws (Part 1) : By: Nasuha MaarifDokument33 SeitenDevelopmental Disturbances of The Face and Jaws (Part 1) : By: Nasuha MaarifPrince AhmedNoch keine Bewertungen
- Developmental Disturbances of The Face and Jaws (Part 1) : By: Nasuha MaarifDokument33 SeitenDevelopmental Disturbances of The Face and Jaws (Part 1) : By: Nasuha MaarifPrince AhmedNoch keine Bewertungen
- Prosthodontics Laboratory 8 (Corrected)Dokument38 SeitenProsthodontics Laboratory 8 (Corrected)Prince AhmedNoch keine Bewertungen
- O.M II Script 1 PigmentationsDokument16 SeitenO.M II Script 1 PigmentationsPrince AhmedNoch keine Bewertungen
- 1 Occlusal SplintsDokument17 Seiten1 Occlusal SplintsPrince AhmedNoch keine Bewertungen
- Pedo V Script 1management of Developing OcclusionDokument12 SeitenPedo V Script 1management of Developing OcclusionPrince AhmedNoch keine Bewertungen
- Ortho 1Dokument9 SeitenOrtho 1Prince AhmedNoch keine Bewertungen
- Implant Script 1implants History DefinitionDokument10 SeitenImplant Script 1implants History DefinitionPrince AhmedNoch keine Bewertungen
- Prostho II LAB 2Dokument27 SeitenProstho II LAB 2Prince AhmedNoch keine Bewertungen
- Cons VII Script 1 Bleaching Discolored TeethDokument19 SeitenCons VII Script 1 Bleaching Discolored TeethPrince AhmedNoch keine Bewertungen
- Lab Prostho 10Dokument13 SeitenLab Prostho 10Prince AhmedNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Chapter Four: Water Conveyance Structures: CanalDokument11 SeitenChapter Four: Water Conveyance Structures: Canaljebril yusufNoch keine Bewertungen
- Kelley Bollen All About DogsDokument141 SeitenKelley Bollen All About DogsRoxanaAndreeaNoch keine Bewertungen
- New Zealand CompaniesDokument3 SeitenNew Zealand CompaniesSukanth KaushalNoch keine Bewertungen
- Basic English Grammar Lesson 2Dokument28 SeitenBasic English Grammar Lesson 2Fuad HasanNoch keine Bewertungen
- MeasurementDokument4 SeitenMeasurementreemobeidaNoch keine Bewertungen
- Basic Nursing NotesDokument4 SeitenBasic Nursing Notesbonggoi100% (1)
- Costing of Service SectorDokument42 SeitenCosting of Service SectorSaumya AllapartiNoch keine Bewertungen
- New Wool2Yarn Global 2021LRDokument87 SeitenNew Wool2Yarn Global 2021LR周星Noch keine Bewertungen
- Critical Analysis of The Great Belt East Bridge PDFDokument10 SeitenCritical Analysis of The Great Belt East Bridge PDFMahmoud Moustafa ElnegihiNoch keine Bewertungen
- JQ 1530AP Fiber Laser Sheet Cutting Machine QuotationDokument7 SeitenJQ 1530AP Fiber Laser Sheet Cutting Machine Quotationcons vesNoch keine Bewertungen
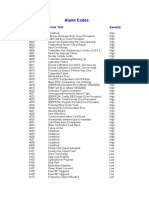
- Alarm Codes: Alarm Code Alarm Text SeverityDokument2 SeitenAlarm Codes: Alarm Code Alarm Text SeverityЕТМNoch keine Bewertungen
- Thermal Overload Motor Relay ProtectionDokument4 SeitenThermal Overload Motor Relay ProtectionBhavik PrajapatiNoch keine Bewertungen
- Tekla Structural Designer 2015i User GuideDokument696 SeitenTekla Structural Designer 2015i User GuideYasonsky Captain100% (3)
- Full Download Introduction To Statistical Methods and Data Analysis 6th Edition Ott Solutions ManualDokument36 SeitenFull Download Introduction To Statistical Methods and Data Analysis 6th Edition Ott Solutions Manualrucaizatax98% (45)
- Plant Systematics ActivityDokument10 SeitenPlant Systematics ActivityJan ReiNoch keine Bewertungen
- Design of Rocker-Bogie MechanismDokument27 SeitenDesign of Rocker-Bogie MechanismInternational Journal of Innovative Science and Research Technology86% (7)
- SoloveyDokument15 SeitenSoloveyMihai Robert100% (3)
- Bentley BrochureDokument9 SeitenBentley BrochureSebastian HickeyNoch keine Bewertungen
- Lesson Plan AcDokument3 SeitenLesson Plan Acjaycee68Noch keine Bewertungen
- Gregory. Aristotle On The Timaeus Receptacle PDFDokument20 SeitenGregory. Aristotle On The Timaeus Receptacle PDFFrncscCnsnllNoch keine Bewertungen
- Level N - Fiction TeacherDokument1 SeiteLevel N - Fiction Teacherapi-64933074Noch keine Bewertungen
- The Rainbow Scada: Internet Enabled Genset ControllerDokument42 SeitenThe Rainbow Scada: Internet Enabled Genset ControllerBimMarius100% (1)
- Fe Standard: English System Information AssayDokument1 SeiteFe Standard: English System Information Assayadvanced techNoch keine Bewertungen
- Heyday of European ImperialismDokument3 SeitenHeyday of European ImperialismHassanor Hadjizaman ImamNoch keine Bewertungen
- Chirality (mathematics) : (enantíos), meaning "opposite", and μέρος (méros), meaning "part"), also known asDokument2 SeitenChirality (mathematics) : (enantíos), meaning "opposite", and μέρος (méros), meaning "part"), also known asHyperionNoch keine Bewertungen
- 011CMEDDokument13 Seiten011CMEDphilip xeroNoch keine Bewertungen
- Kmeuk - Kinflex LeafletDokument4 SeitenKmeuk - Kinflex LeafletShafivuddin KamaluddinNoch keine Bewertungen
- Contoh ResumeDokument3 SeitenContoh ResumePutri AisyahNoch keine Bewertungen
- The One and Only by Emily GiffinDokument12 SeitenThe One and Only by Emily GiffinRandom House of Canada50% (2)
- Aoac Fatty Acid CerealsDokument2 SeitenAoac Fatty Acid CerealsRoxana CalderonNoch keine Bewertungen