Beruflich Dokumente
Kultur Dokumente
Superficial Temporal Artery To Middle Cerebral.28
Hochgeladen von
Andreea GiovaniOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Superficial Temporal Artery To Middle Cerebral.28
Hochgeladen von
Andreea GiovaniCopyright:
Verfügbare Formate
OPERATIVE NUANCES
SUPERFICIAL TEMPORAL ARTERY-TO-MIDDLE CEREBRAL ARTERY BYPASS
Fady T. Charbel, M.D.
Department of Neurosurgery, University of Illinois at Chicago, Chicago, Illinois
Guido Meglio, M.D.
Department of Neurosurgery, University of Illinois at Chicago, Chicago, Illinois
THE SUPERFICIAL TEMPORAL artery-to-middle cerebral artery bypass represents the mainstay of bypass operations for cerebral revascularization. The role of this operation in the setting of cerebrovascular occlusive disease, with compromised cerebral hemodynamic reserve, is a topic of current investigation. In this report, we describe technical nuances to avert potential pitfalls in the performance of this procedure. The use of intraoperative quantitative blood flow measurements as a reliable method of assessing the success of the bypass is also described.
KEY WORDS: Blood flow measurement, Cerebrovascular occlusive disease, Extracranial-intracranial bypass, Middle cerebral artery, Superficial temporal artery
Neurosurgery 56[ONS Suppl 1]:ONS-186ONS-190, 2005
DOI: 10.1227/01.NEU.0000144487.85531.FD
Sepideh Amin-Hanjani, M.D.
Department of Neurosurgery, University of Illinois at Chicago, Chicago, Illinois Reprint requests: Sepideh Amin-Hanjani, M.D., Neuropsychiatric Institute (MC 799), Department of Neurosurgery, University of Illinois at Chicago, 912 South Wood Street, Chicago, IL 60612-5970. Email: hanjani@uic.edu Received, March 15, 2004. Accepted, June 9, 2004.
he purpose of this article is to present the technical nuances that have been developed by the senior author (FTC) to avert potential pitfalls in the performance of the superficial temporal artery-to-middle cerebral artery (STAMCA) bypass procedure. In a related article (1) in this issue, the application of intraoperative blood flow measurement as an adjunct in the evaluation of the prognosis for STAMCA bypass is presented in detail. In this article, we focus on the technical maneuvers that enhance the success of this specialized microsurgical procedure. A variety of different bypass options are available depending on clinical circumstances, but the STAMCA bypass can be considered the workhorse of cerebral revascularization and is a technique that must be mastered by surgeons who wish to perform any type of extracranial-intracranial bypass as part of their operative repertoire.
INDICATIONS FOR STAMCA BYPASS
The indications for extracranial-intracranial bypass fall into two major categories: 1) flow replacement in the treatment of complex aneurysms or tumors that require vessel sacrifice; and 2) flow augmentation for the treatment of cerebral ischemia associated with misery perfusion. In this article, we focus on the latter indication; bypass techniques for aneurysms and tumors have been addressed in a
prior article of this type (5). The enthusiasm for use of surgical revascularization, specifically STAMCA bypass, for ischemia was markedly tempered by the results of the extracranial-intracranial bypass trial (2). However, interest in revascularization has been raised again, on the basis of a greater understanding of the importance of assessing cerebral hemodynamic factors. Carefully selected patients with compromised cerebral hemodynamic reserve may benefit from the procedure (4), and a randomized trial is under way to assess the efficacy of bypass with carotid occlusion and misery perfusion documented by positron emission tomography (3). At our institution, the current indications for STAMCA bypass for purposes of flow augmentation are as follows: failure of maximal medical therapy, symptoms concordant with radiographic findings, poor cerebrovascular reserve as demonstrated by xenon computed tomography or single-photon emission computed tomography, and lack of major medical comorbidity. We also use STAMCA bypass in the treatment of symptomatic adult moyamoya disease.
PREOPERATIVE ASSESSMENT
A more detailed discussion of the preoperative assessment is provided in a related article (1) in this issue. Briefly, symptomatic patients for whom medical therapy has failed are evaluated clinically and undergo a series of
ONS-186 | VOLUME 56 | OPERATIVE NEUROSURGERY 1 | JANUARY 2005
www.neurosurgery-online.com
SUPERFICIAL TEMPORAL ARTERY-TO-MIDDLE CEREBRAL ARTERY BYPASS
preoperative imaging studies, including the following: 1. Angiography to delineate the intracranial lesion, with selective external carotid runs to evaluate the adequacy and course of the STA branches on the affected side 2. Magnetic resonance parenchymal imaging to assess the presence and extent of prior strokes 3. Phase-contrast magnetic resonance angiography quantitative blood flow measurement of intracranial vasculature 4. Single-photon emission computed tomography with and without acetazolamide (Diamox; Wyeth Pharmaceuticals, Collegeville, PA) challenge to assess for loss of cerebrovascular reserve capacity. In addition, preoperative medical and cardiology clearance is obtained. Functional magnetic resonance imaging and neuropsychological testing are also performed as appropriate.
PREOPERATIVE PREPARATION AND ANESTHETIC CONSIDERATIONS
Patients are instructed to take 325 mg of aspirin the night before surgery. An arterial line and central venous access are routinely obtained. Throughout surgery, normovolemia, normocapnia, and normotension are maintained. During temporary vessel occlusion, metabolic burst suppression is induced with barbiturates or inhalational agents and mean arterial blood pressure is raised 25% above baseline.
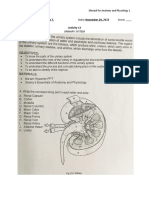
The initial incision through the epidermis and dermis is made with a Colorado microneedle-tip monopolar cautery (Stryker Leibinger, Kalamazoo, MI) at a low setting of 8 along the midpoint of the projected course of the STA branch. Opening the skin in this fashion limits bleeding from the skin edges, whereas the low cautery setting prevents skin edge necrosis or poor wound healing. Once subcutaneous tissue is encountered, a blunt-tip curved snap is used to dissect down the STA. Once the vessel is visualized, the snap is used to dissect proximally in the loose areolar plane above the vessel; the Colorado tip is then used to open the skin to the tip of the snap as sequential dissection is performed until the main trunk of the STA is reached. The same procedure is performed distally, although the tissue is more adherent to the vessel distally and dissection must proceed with caution. The goal is to dissect approximately 8 to 10 cm of STA. Once exposed, a Bovie electrocautery (Bovie Medical Corp., St. Petersburg, FL) with a coated shaft at a setting of 25 to 30 is used to divide the tissue around the STA, allowing it to be lifted from the underlying temporalis muscle fascia (Fig. 1). Once the vessel and its surrounding cuff of tissue have been isolated along their course, they are wrapped in papaverine-soaked cottonoid. The exposure of the STA is performed under loupe magnification with the surgeon and assistant seated.
Craniotomy
Self-retaining fishhook retractors are placed; with the vessel within protective cottonoid, the retractors are reflected to one side or the other. The Bovie electrocautery is used to incise the temporalis fascia and muscle in a T-shaped or cruciate fashion (Fig. 2); each quadrant of muscle is then retracted with hooks. A burr hole is placed with a Midas acorn drill bit (Medtronic Midas Rex, Fort Worth, TX) below the proximal and distal aspects of the course of the vessel, and a circular craniotomy is created with the Midas B1 drill bit (Fig. 3). Thin strips of Gelfoam (Pharmacia & Upjohn, Kalamazoo, MI ) or Surgicel (Johnson & Johnson Products, Chicago, IL) are packed under the bone edges, and the dura is tacked extensively around the margins of the craniotomy to avoid any epidural oozing. The dura is opened initially in a cruciate fashion, and additional cuts are then placed to form multiple triangular flaps that are tacked backward, exposing the cortex (Fig. 4).
SURGICAL TECHNIQUE (see video at web site)
Positioning
The head is fixed in full lateral position with a four-pin Sugita headholder (Mizuho America, Inc., Beverly, MA). A rolled blanket under the ipsilateral shoulder is often required in patients with restriction in lateral rotation to facilitate this. The scalp is shaved, and Doppler sonography is used to map both branches of the STA; this is performed after pinning, which can pull the skin and distort prior markings.
STA Dissection
Generally, the posterior branch of the STA is exposed via a linear incision unless angiography has demonstrated a clearly inadequate posterior branch. In such a circumstance, an incision can be placed directly over the anterior branch, but this may have a tendency to lie on the forehead; alternatively, a semicircular skin flap can be raised behind the hairline, with the anterior branch dissected from the undersurface of the flap. This is the strategy used when a posterior branch is initially exposed but appears to be of poor quality or caliber; the linear incision is merely curved forward and converted into a skin flap, which allows dissection of the anterior branch.
Preparing the Recipient Vessel
The microscope is now brought in for the remainder of the procedure. The cortical surface is examined for a suitable recipient cor-
FIGURE 1. Drawing showing dissection of the STA with its surrounding cuff of tissue.
NEUROSURGERY
VOLUME 56 | OPERATIVE NEUROSURGERY 1 | JANUARY 2005 | ONS-187
CHARBEL
ET AL.
tical MCA branch (Fig. 5). The most important consideration is the size of the recipienta vessel of 1.5 mm or greater is optimal. Other potential considerations are the location (away from the craniotomy edges) and orientation (a tangential orientation of the vessel from 0500 to 2300 h on a clock face is optimal for a righthanded surgeon because it creates the most natural angle for placement of sutures FIGURE 2. Drawing showing the during the anastomosis) of T-shaped incision in temporalis muscle. the vessel. The arachnoids covering potential recipient vessels are opened with a combination of an arachnoid knife, fine forceps, and microscissors. Once a vessel has been selected, a 1-cm region of vessel must be prepared for anastomosis. Small perforators emanating from the vessel in this region must be coagulated with bipolar cautery. This allows mobilization of the vessel from the brain surface for placement of a FIGURE 3. Drawing showing a cirrubber dam underneath the cular craniotomy after placement of burr holes below the proximal and vessel but also prevents distal aspect of the STA. back-bleeding into the anastomosis site during temporary vessel occlusion. Larger perforators can be spared by occlusion with temporary vessel clips during the anastomosis. A small piece of Gelfoam is placed underneath the rubber dam to elevate the vessel out of its sulcus, and a papaverine-soaked cotton ball is applied to the vessel surface.
Preparing the Donor Vessel
At this point, the brain surface is covered with cottonoid and the STA branch is uncovered. A sharp curved snap is used to dissect the artery from the surrounding cuff of tissue proximally to create a site for placement of a temporary clip. The ideal site for temporary clipping is distal to the takeoff of the unused branch of the STA; this allows continued flow through the STA into the nonoccluded branch, reducing stagnant flow and the risk of thrombosis proximal to the temporary clip. If it is necessary to sacrifice the unused branch to mobilize the STA adequately, the branch should be divided with a temporary clip on the proximal stump. This allows the stump to be used for back-bleeding and venting of air after the anastomosis.
The STA is next dissected at its most distal aspect. Sugita temporary clips (Mizuho America, Inc.) are placed proximally and distally, and the vessel and its cuff are transected distally (Fig. 5). The distal aspect of the STA within the scalp tissue is well coagulated, and the adjacent temporary clip is removed. A blunt-tip needle is then used to flush the STA with heparinized saline FIGURE 4. Drawing of dural open(10 U of heparin/ml) ing in a cruciate fashion with multithrough its cut end. It is im- ple triangular flaps. portant to open the proximal temporary clip briefly and to flush beyond the clip to avert thrombosis. Once flushed, the required length of STA to reach the anastomotic site without tension is gauged, and this length is marked on the vessel with a marking pen. The vessel is then dissected free of its cuff of tissue to a point 1 inch proximal to this. The dissection is performed by holding the vessel taut, creating a plane above the vessel with curved microscissors, and FIGURE 5. Drawing showing a tempodissecting the cuff of tissue rary clip placed on the proximal and disfrom each side of the vessel; tal STA in preparation for cutting of the vessel. The cortical recipient artery is care must be taken to idenidentified. tify and coagulate side branches of the STA as this is performed. It is unnecessary to release the STA from its surrounding cuff along its entire length, because this serves no purpose, is time-consuming, and increases the risk of injury to the vessel. If any oozing is noted from the cuff of tissue, a clip is placed separately across the base of the cuff parallel to the STA temporary clip. At this stage, we routinely check the free flow through the cut end of the STA branch by removing the proximal temporary clip and measuring flow with a quantitative microvascular ultrasonic flow probe (Charbel Micro-Flowprobe; Transonics Systems, Inc., Ithaca, NY) (Fig. 6). This cut flow is documented, and the STA vessel is again flushed with heparinized saline before replacement of the proximal temporary clip.
Performing the Anastomosis
In final preparation for anastomosis, the STA is cut at a 45-degree angle with microscissors and a fish mouth is cre-
ONS-188 | VOLUME 56 | OPERATIVE NEUROSURGERY 1 | JANUARY 2005
www.neurosurgery-online.com
SUPERFICIAL TEMPORAL ARTERY-TO-MIDDLE CEREBRAL ARTERY BYPASS
ated. A marking pen is used to color the outer wall of the vessel, which allows the lumen to be seen more easily by contrast, and the line of incision on the recipient vessel is also marked for the same purpose. It is important to examine the lumen of the STA carefully at this point, because there can be instances of double lumina or vessel dissection that would lead to an unsuccessful bypass. Temporary Sugita clips are placed proximally and then distally on the recipient vessel, which is incised with an ophthalmic blade. The fish-mouthed donor STA is laid next to the recipient to gauge the exact length of the incision necessary (Fig. 7). Anchoring sutures at the apices of the incision are placed with 10-0 nylon suture. Optimally, the suture is passed through the recipient vessel from the inside to the outside to reduce injury to the vessel endothelium (Fig. 7). Once the donor STA has been anchored, interrupted sutures are placed on each side of the anastomosis at close intervals to prevent anastomotic leak. We prefer the interrupted suture technique FIGURE 6. Drawing showing as opposed to running sutures measurement of cut flow secondary to the small size of the through the open end of the STA, vessels, and because of the ten- using the Corsten maneuver dency for intimal disease in the (placement of one end of a cottonoid underneath the vessel, and patient population receiving this the other end against gentle suctype of bypass. Because the walls tion, which avoids bleeding onto of the recipient vessel are thin the field without altering the cut and tend to collapse together, in- flow). The arrow on the flow advertent suturing of the oppo- probe indicates the direction of site wall is a distinct concern. To blood flow. prevent this, a Silastic stent (Dow Corning, Auburn, MI) is placed within the recipient vessel and removed just before the final sutures are placed (Fig. 7). A double-stent technique with an additional stent in the STA can also be used to prevent the same inadvertent back wall suturing of the donor as needed. The sutures are tied with three knots as they are placed, with the exception that the penultimate suture on each side of the anastomosis is left free to allow room for good visualization as the final suture is placed. Sutures are placed at the highest magnification, but tying is often facilitated by briefly zooming out to a lower magnification on the microscope.
The lumen is flushed with heparinized saline before the final suture is tied. Once the anastomosis is complete, the temporary clips on the MCA are released. The STA proximal clip is also released, and gentle pressure is applied to the anastomosis site with cotton balls if there is any oozing. With meticulous attention to suture technique, additional sutures to control anastomotic leak are rarely necessary. Blood flow is again measured, now on the bypassed STA (Fig. 8). We have found that a cut flow index (ratio of the bypass flow to the initial cut flow) is a sensitive predictor of bypass function. The measured blood flow is far superior to mere Doppler sonographic assessment of the presence or absence of flow, and with this information in hand, intraoperative angiography is unnecessary.
FIGURE 7. Drawing showing placement of the first stitch at the apex of the anastomosis. A stent is in place inside the recipient vessel to prevent the walls of the vessel from collapsing together.
Closure of the Craniotomy
The dura is not closed, and the dural opening is covered with a piece of Gelfoam. The bone is replaced, but the burr hole is enlarged to accommodate the STA vessel, avoiding any kinking or pressure on the vessel. The muscle is reapproximated loosely, and the skin is closed with care to avoid injury to the proximal STA trunk. The unused branch of the STA is generally ligated to optimize flow through the bypass.
FIGURE 8. Drawing showing measurement of bypass flow after completion of the anastomosis (also see Ref. 1).
POSTOPERATIVE CARE
Patients are placed on a regimen of 325 mg of aspirin daily, starting immediately after surgery. Patients are observed in the intensive care unit after surgery; they are kept well hydrated, and hypotension is avoided. Baseline angiography and quantification of flow through the bypass by phase-contrast magnetic resonance angiography are performed after surgery. Patients are discharged on daily aspirin and undergo follow-up noninvasive testing with phase-contrast magnetic resonance angiography to monitor the status of the bypass. Potential postoperative complications include epidural hematoma and wound infection. Postoperative graft occlusion is
NEUROSURGERY
VOLUME 56 | OPERATIVE NEUROSURGERY 1 | JANUARY 2005 | ONS-189
CHARBEL
ET AL.
rare, given that bypass function can be well assessed during surgery with flow measurement, and graft revision can be performed at that time if necessary.
the sylvian fissure, which may provide a larger volume of blood flow immediately. Laligam N. Sekhar Great Neck, New York
1. Diaz FG, Umansky F, Mehta B, Montoya S, Dujovny M, Ausman JI, Cabezudo J: Cerebral revascularization to a main limb of the middle cerebral artery in the Sylvian fissure: An alternative approach to conventional anastomosis. J Neurosurg 63:2129, 1985.
CONCLUSION
The success of the STAMCA bypass is highly dependent on careful attention to technique at every stage of the operation, from STA dissection to skin closure. Adherence to a stereotyped step-by-step approach to this operation, with recognition of the importance of every step, can result in consistent technical success.
DISCLOSURE
FTC is a consultant for Transonics Systems, Inc. (Ithaca, NY).
REFERENCES
1. Amin-Hanjani S, Du X, Mlinarevich N, Meglio G, Zhao M, Charbel FT: The cut flow index: An intraoperative predictor of the success of extracranialintracranial bypass for occlusive cerebrovascular disease. Neurosurgery 56[Suppl 1]:7585, 2005. 2. EC/IC Bypass Study Group: Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke: Results of an international randomized trial EC/IC Bypass Study Group. N Engl J Med 313:11911200, 1985. 3. Grubb RL Jr, Powers WJ, Derdeyn CP, Adams HP, Clarke WR: The Carotid Occlusion Surgery Study. Neurosurg Focus 14:Article 9, 2003. 4. Nussbaum ES, Erickson DL: Extracranial-intracranial bypass for ischemic cerebrovascular disease refractory to maximal medical therapy. Neurosurgery 46:3743, 2000. 5. Sekhar LN, Kalavakonda C: Cerebral revascularization for aneurysms and tumors. Neurosurgery 50:321331, 2002.
his article focuses on the technical aspects of STAMCA bypass used to help augment blood flow in symptomatic patients documented to have poor cerebrovascular reserve. The preoperative preparation, followed by the surgical technique, is outlined in detail, and the steps necessary for the preparation of the STA and recipient MCA are well described. As this article mentions, attention to detail at every step of the operation is key to the success of the procedure. The authors use 10-0 nylon suture in an interrupted manner for anastomosis. At this institution, a running suture is routinely used. However, either technique is effective and should be left to the surgeons discretion. After the anastomosis, the authors leave the dural edges in their anatomic position. Here, however, the dural flaps are routinely inverted, as performed in encephalodurosynangiosis, to allow additional stimuli for neovascularization. Peyman Tabrizi Robert F. Spetzler Phoenix, Arizona TAMCA bypass surgery is used for the treatment of complex aneurysms or tumors that require vessel sacrifice or cerebral ischemia in those demonstrating misery perfusion. As for indication, preoperative cerebral blood flow study is the most important issue. At our institute, a balloon occlusion test is essential for the treatment of aneurysms or tumors. In the case of hemodynamic compromise, extracranial-to-intracranial bypass is performed. In the case of ischemia, STAMCA bypass is performed for the patients who present with less than 80% regional cerebral blood flow and less than 10% cerebrovascular reserve after acetazolamide challenge. As for the technical aspects, the surgeon should place careful interrupted sutures, confirming the intimal layer. I also suggest that the success of STAMCA bypass is highly dependent on careful attention to technique at every stage of the operation. Yasushi Takagi Nobuo Hashimoto Kyoto, Japan
Acknowledgment
We acknowledge the contributions of Luke Corsten, M.D., to the technique of cut flow measurement.
COMMENTS
n this article, Charbel et al. have presented a nice step-bystep review of the superficial temporal artery-to-middle cerebral artery (STAMCA) bypass technique, which is still useful in many surgical situations. I do not open the skin with a Colorado needle and do not divide the cuff around the STA with a monopolar current. Also, before the anastomosis, I take the sleeve around the STA down for only approximately 1 cm. A variant of this technique, first reported by Diaz et al. (1), that I find useful is the anastomosis of the STA to an M3 branch in
Customer Service Contact Information CNS Members: Call Sue Souders at: 301/223-2325. Non-CNS Members: Call either 301/223-2300 or 1-800/638-3030. Customer Service fax: 301/223-2400. Customer Service email: customerservice@lww.com
ONS-190 | VOLUME 56 | OPERATIVE NEUROSURGERY 1 | JANUARY 2005
www.neurosurgery-online.com
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Barthel IndexDokument1 SeiteBarthel IndexChu Ai Reen50% (2)
- Neuroanatomy Draw It To Know ItDokument477 SeitenNeuroanatomy Draw It To Know ItLiangrid Nunes Barroso RodriguesNoch keine Bewertungen
- Scotchcast PDFDokument311 SeitenScotchcast PDFSaadNoch keine Bewertungen
- Policies and Procedures For Ambulance ServiceDokument3 SeitenPolicies and Procedures For Ambulance ServiceLymberth Benalla100% (1)
- Double Reimplantation Technique To Reconstruct.20Dokument8 SeitenDouble Reimplantation Technique To Reconstruct.20Andreea GiovaniNoch keine Bewertungen
- A Novel Minimally Occlusive Microvascular.33Dokument8 SeitenA Novel Minimally Occlusive Microvascular.33Andreea GiovaniNoch keine Bewertungen
- Microvascular Retractor A New Concept Of.34Dokument4 SeitenMicrovascular Retractor A New Concept Of.34Andreea GiovaniNoch keine Bewertungen
- Bilateral Internal Carotid To Anterior Cerebral.26Dokument5 SeitenBilateral Internal Carotid To Anterior Cerebral.26Andreea GiovaniNoch keine Bewertungen
- Revascularization of The Anterior Cerebral Artery.38Dokument4 SeitenRevascularization of The Anterior Cerebral Artery.38Andreea GiovaniNoch keine Bewertungen
- In Situ Bypass in The Management of Complex.23Dokument6 SeitenIn Situ Bypass in The Management of Complex.23Andreea GiovaniNoch keine Bewertungen
- Abortion: Refers To The Expulsion of Human Fetus Before The Period of ViabilityDokument50 SeitenAbortion: Refers To The Expulsion of Human Fetus Before The Period of ViabilityEzekiel ReyesNoch keine Bewertungen
- Urinary SystemDokument5 SeitenUrinary SystemJushelle Anne Tigoy Pilare100% (1)
- OB2 RLE SAS 6 Versions SAS 7 Caesarian Section SAS 8 Uterine AtonyDokument26 SeitenOB2 RLE SAS 6 Versions SAS 7 Caesarian Section SAS 8 Uterine AtonyHana LandinginNoch keine Bewertungen
- Clinical Presentation of Varicose VeinsDokument8 SeitenClinical Presentation of Varicose VeinslucyishakNoch keine Bewertungen
- BloodCollectionTechniques e Rev07 0116 LowresDokument15 SeitenBloodCollectionTechniques e Rev07 0116 LowresBilly Samame YarascaNoch keine Bewertungen
- CH 071 Acute Kidney Injury in ChildrenDokument9 SeitenCH 071 Acute Kidney Injury in Childrenarun babuNoch keine Bewertungen
- Actions To Prevent Wrong Person Site Procedure EventsDokument4 SeitenActions To Prevent Wrong Person Site Procedure EventsAlfie YannurNoch keine Bewertungen
- Kuliah EmergensiDokument66 SeitenKuliah EmergensiRifqi RamdhaniNoch keine Bewertungen
- Obstetric HemorrhageDokument104 SeitenObstetric HemorrhageRanjit SharmaNoch keine Bewertungen
- Perfusionist Job DescriptionDokument3 SeitenPerfusionist Job DescriptionNouman IshaqNoch keine Bewertungen
- HerniasDokument64 SeitenHerniasKalpana SubediNoch keine Bewertungen
- HemorrhoidsDokument26 SeitenHemorrhoidsWaqar ZahirNoch keine Bewertungen
- 13Nutritional-Support LatestDokument76 Seiten13Nutritional-Support LatestKryzza LeizellNoch keine Bewertungen
- XRAYDokument2 SeitenXRAYCharm Arroyo100% (1)
- ESC Guideline NSTEMI PDFDokument59 SeitenESC Guideline NSTEMI PDFsisrinovritaNoch keine Bewertungen
- Intraoperative Management of Shock in Adults - UpToDateDokument36 SeitenIntraoperative Management of Shock in Adults - UpToDateYessica RivasNoch keine Bewertungen
- OptiLube Active Brochure 2012 Second EditionDokument4 SeitenOptiLube Active Brochure 2012 Second EditionOptimum Medical SolutionsNoch keine Bewertungen
- Ophtha Imp MCQ FmgeDokument54 SeitenOphtha Imp MCQ Fmgevikas prajapatNoch keine Bewertungen
- Hollis V Dow Corning CorporationDokument2 SeitenHollis V Dow Corning CorporationAlice Jiang100% (1)
- EmbryologyDokument1 SeiteEmbryologyprasannaipad324Noch keine Bewertungen
- ElectrocardiographyDokument21 SeitenElectrocardiographyTol Man ShresthaNoch keine Bewertungen
- Sentinel Lymph Node (SLN) Biopsy PDFDokument5 SeitenSentinel Lymph Node (SLN) Biopsy PDFMDNoch keine Bewertungen
- HybaseDokument6 SeitenHybaseSreejith SwaminathanNoch keine Bewertungen
- Learning To Perform Ear Reconstruction: Gordon H. Wilkes, M.D., F.R.C.S.CDokument6 SeitenLearning To Perform Ear Reconstruction: Gordon H. Wilkes, M.D., F.R.C.S.Cbob sumadi lubisNoch keine Bewertungen
- CystosDokument1 SeiteCystosgeorgeloto12Noch keine Bewertungen
- Massive Hemorrhage ProtocolDokument19 SeitenMassive Hemorrhage ProtocolYeseniaNoch keine Bewertungen