Beruflich Dokumente
Kultur Dokumente
Fluids and Electrolytes
Hochgeladen von
Nano BaddourOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Fluids and Electrolytes
Hochgeladen von
Nano BaddourCopyright:
Verfügbare Formate
Fluids and Electrolytes INTRODUCTION To maintain good health, a balance of fluids and electrolytes, acids and bases must
t be normally regulated for metabolic processes to be in working state. A cell, together with its environment in any part of the body, is primarily composed of FLUI . Thus fluid and electrolyte balance must be maintained to promote normal function. !otential and actual problems of fluid and electrolytes happen in all health care settings, in every disorder and with a variety of changes that affect homeostasis. The nurse therefore needs to FULL" understand the physiology and pathophysiology of fluid and electrolyte alterations so as to identify or anticipate and intervene appropriately. Fluids a solution of solvent and solute Solvent a li#uid substance where particles can be dissolved Solute a substance, either dissolved or suspended in a solution Solution a homogeneous mi$ture of % or more substances of dissimilar molecular structure usually applied to solids in li#uids but applies e#ually to gasses in li#uids Body Fluids A. Function &. Transporter of nutrients , wastes, hormones, proteins and etc %. 'edium or milieu for metabolic processes (. )ody temperature regulation *. Lubricant of musculoskeletal +oints ,. Insulator and shock absorber B. Body Fluid Compartments Intracellular E tracellular Transcellular -ithin .ells /utside cells .ontained in body cavities ,,0 or %1( *%.,0 or &1( T)%.,0 T)Transport system of our body 2ot readily utili3ed by the body !otassium4 5odium4 .5F, !leural fluid, !hosphates )icarbonates 5ynovial Fluid and 'agnesium .hloride peritoneal fluid 5ecreted by epithelial cells Interstitial Intravascular Bound Fluid -ithin the surrounding blood vessels the cells %60T)or &1( of 7.F )one and %1( of 7.F !lasma 8.,0 .artilage 8.,0 9igher protein ense content .onnective tissues 8.,0 C. Body Compartment !olumes 2ormal values !remature Term T)'ale; <60 8,0 Female; 7.F *,0 *60
%, yrs :60 ,60 %60
*, yrs ,,0 *80
:, yrs ,60 *,0
I.F )lood =olume
(,0 >6?&66 ml1kg
(,0 <, ml1kg
*60 86 ml1kg
neonates reach adult values by % yrs and are about half?way by ( months average values @ 86 ml1&66g of lean body mass percentage of water varies with tissue type, A. lean tissues @ :6?<60 ). bone @ %6?%,0 .. fat @ &6?&,0 D. Tonicity o" Body Fluids Tonicity refers to the concentration of particles in a solution The normal tonicity or osmolarity of body fluids is %,6?(66 m/sm1L &.Isotonic 5ame as plasma %.9ypotonic have a lesser or lowers solute concentration than plasma (.9ypertonic higher or greater concentration of solutes .ommon Intravenous 5olutions Solution Na Cl# $% Ca &lu Osm. p' (act )*+l ,, , , , -./ -01 0 , /2, 2a.l 6.>0 30, 30, , , , 1,, 0.. , , 2a.l (.60 031 031 , , , /00 0.. , , *-12a.L 1, 1, , , ---/1.0 4 , 5.6.&<0 0#0 9artmans 3-6 3,6 0 , , -.2 5.. -/ 1../ !lasmalyte 32, 6/ 0 -62 0.0 -. /2 9aemaccel 320 320 0.3 5.-0 , -61 ..1 , , 'annitol%60 , , , , , 3,/ 5., , e$tran 86 302 302 , , , 1,, 2#. , , Osmole the weight in grams of a substance producing an osmotic pressure of %%.* atm. when dissolved in &.6 litre of solution Agram molecular weightB 1 Ano. of freely moving particles per moleculeB Osmolality the number of osmoles of solute per kilogram of solvent Osmolarity the number of osmoles of solute per litre of solution 7ole that number of molecules contained in 6.6&% kg of .&%, or, the molecular weight of a substance in grams C Avogadro's number C :.6%( $ &6%( 7olality the number of moles of solute per kilogram of solvent 7olarity is the number of moles of solute per litre of solution T'E Normal D8NA7ICS OF BOD8 F(UIDS The methods by which electrolytes and other solutes move across biologic membranes are /smosis, iffusion, Filtration and Active Transport. /smosis, diffusion and filtration are passive processes, while Active transport is an active process. 3. OS7OSIS This is the movement of water1li#uid1solvent across a semi?permeable membrane from a lesser concentration to a higher concentration /smotic pressure is the power of a solution to draw water across a semi? permeable membrane .olloid osmotic pressure Aalso called oncotic pressureB is the osmotic pull e$erted by plasma proteins
-. DIFFUSION D)rownian movementE or Ddownhill movementE The movement of particles1solutes1molecules from an area of higher concentration to an area of a lower concentration This process is affected by; a. The si3e of the molecules? larger si3e moves slower than smaller si3e b. The concentration of solution? wide difference in concentration has a faster rate of diffusion c. The temperature? increase in temperature causes increase rate of diffusion Facilitated iffusion is a type of diffusion, which uses a carrier, but no energy is e$pended. /ne e$ample is fructose and amino acid transport process in the intestinal cells. This type of diffusion is saturable. 1. FI(TRATION This is the movement of BOTH solute and solvent together across a membrane from an area of higher pressure to an area of lower pressure 9ydrostatic pressure is the pressure e$erted by the fluids within the closed system in the walls of the container 2. ACTI!E TRANS9ORT !rocess where substances1solutes move from an area of lower concentration to an area of higher concentration with utili3ation of 727FG" It is called an Duphill movementE Usually, a carrier is re#uired. An en3yme is utili3ed also. Types o" Active Transport: a. !rimarily Active Transport 7nergy is obtained directly from the breakdown of AT! /ne e$ample is the 5odium?!otassium pump b. 5econdary Active Transport 7nergy is derived secondarily from stored energy in the form of ionic concentration difference between two sides of the membrane. /ne e$ample is the Glucose?5odium co?transportH also the 5odium?.alcium counter?transport T'E RE&U(ATION OF BOD8 F(UID BA(ANCE To maintain homeostasis, many body systems interact to ensure a balance of fluid intake and output. A balance of body fluids normally occurs when the fluid output is balanced by the fluid input Overvie; o" Fluid Re<ulation =y t>e Body Systems
A. Systemic Re<ulators o" Body Fluids 1. Renal Re<ulation ?RAS@ This system regulates sodium and water balance in the 7.F The formation of urine is the main mechanism 5ubstance released to regulate water balance is F72I2. Fenin activates Angiotensinogen to Angiotensin?I, A?I is en3ymatically converted to Angiotensin?II A a powerful vasoconstrictorB 2. Endocrine Re<ulation The primary regulator of water intake is the thirst mechanism, controlled by the thirst center in the hypothalamus Aanterolateral wall of the third ventricleB Anti?diuretic hormone AA 9B is synthesi3ed by the hypothalamus and acts on the collecting ducts of the nephron A 9 increases rate of water reabsorption The adrenal gland helps control FI7 through the secretion of AL/5T7F/27? a hormone that promotes sodium retention and water retention in the distal nephron ATFIAL 2ATFIUF7TI. factor AA2FB is released by the atrial cells of the heart in response to e$cess blood volume and increased wall stretching. A2F promotes sodium e$cretion and inhibits thirst mechanism 3. &astro#intestinal re<ulation The GIT digests food and absorbs water The hormonal and en3ymatic activities involved in digestion, combined with the passive and active transport of electrolyte, water and solutions, maintain the fluid balance in the body. B. Fluid Inta)e 9ealthy adult ingests fluid as part of the dietary intake. >60 of intake is from the ingested food and water &60 of intake results from the products of cellular metabolism Usual intake of adult is about %, ,66 ml per day The other sources of fluid intake are; I=F, T!2, )lood products, and colloids C. Fluid Output The average fluid losses amounts to %, ,66 ml per day, counterbalancing the input. The routes of fluid output are the following; 5725I)L7 L/55? Urine, feces or GI losses, sweat I25725I)L7 L/55? though the skin and lungs as water vapor UFI27? is an ultra?filtrate of blood. The normal output is &,,66 ml1day or (6? ,6 ml per hour or 6.,?& ml per kilogram per hour. Urine is formed from the filtration process in the nephron F7.AL loss? usually amounts to about %66 ml in the stool Insensible loss? occurs in the skin and lungs, which are not noticeable and cannot be accurately measured. -ater vapor goes out of the lungs and skin. Aater 7eta=olism aily )alance; turnover @ %,66 ml a. Intake i. drink @ &,66 ml ii. food @ 866 ml iii. metabolism @ (66 ml b. Losses i. urine @ &,66 ml ii. skin @ ,66 ml insensible losses @ *66 ml sweat @ &66 ml iii. lungs @ *66 ml iv. faeces @ &66 ml 'inimum daily intake @ ,66 ml with a JnormalJ diet 'inimum losses @ &,66 ml1d Losses are increased withH
a. increased ambient T b. hyperthermia @ &(0 per K. c. decreased relative humidity d. increased minute ventilation e. increased 'F/% Fluid Im=alances F(UID !O(U7E DEFICIT or '89O!O(E7IA efinition; This is the loss of e$tra cellular fluid volume that e$ceeds the intake of fluid. The loss of water and electrolyte is in e#ual proportion. It can be called in various terms? vascular, cellular or intracellular dehydration. )ut the preferred term is hypovolemia. ehydration refers to loss of -AT7F alone, with increased solutes concentration and sodium concentration !athophysiology of Fluid =olume eficit 7tiologic conditions include; a. =omiting b. iarrhea c. !rolonged GI suctioning d. Increased sweating e. Inability to gain access to fluids f. Inade#uate fluid intake g. 'assive third spacing Fisk factors are the following; a. iabetes Insipidus b. Adrenal insufficiency c. /smotic diuresis d. 9emorrhage e. .oma f. Third?spacing conditions like ascites, pancreatitis and burns !AT9/!9"5I/L/G"; Factors inade#uate fluids in the body decreased blood volume decreased cellular hydration cellular shrinkage weight loss, decreased turgor, oliguria, hypotension, weak pulse, etc. The 2ursing !rocess in Fluid =olume eficit A55755'72T; 9>ysical e amination -eight loss, tented skin turgor, dry mucus membrane 9ypotension Tachycardia .ool skin, acute weight loss Flat neck veins ecreased .=! Su=Bective cues Thirst 2ausea, anore$ia 'uscle weakness and cramps .hange in mental state
(a=oratory "indin<s &. 7levated )U2 due to depletion of fluids or decreased renal perfusion %. 9emoconcentration (. !ossible 7lectrolyte imbalances; 9ypokalemia, 9yperkalemia, 9yponatremia, hypernatremia *. Urine specific gravity is increased Aconcentrated urineB above &.6%6 NURSIN& DIA&NOSIS Fluid =olume deficit
9(ANNIN& To restore body fluids I79(E7ENTATION A55I5T I2 '7 I.AL I2T7F=72TI/2 !rovide intravenous fluid as ordered !rovide fluid challenge test as ordered NURSIN& 7ANA&E7ENT &. Assess the ongoing status of the patient by doing an accurate input and output monitoring %. 'onitor daily weights. Appro$imate weight loss & kilogram C &literL (. 'onitor =ital signs, skin and tongue turgor, urinary concentration, mental function and peripheral circulation *. !revent Fluid =olume eficit from occurring by identifying risk patients and implement fluid replacement therapy as needed promptly ,. .orrect fluid =olume eficit by offering fluids orally if tolerated, anti? emetics if with vomiting, and foods with ade#uate electrolytes :. 'aintain skin integrity 8. !rovide fre#uent oral care <. Teach patient to change position slowly to avoid sudden postural hypotension F(UID !O(U7E ECCESS: '89ER!O(E7IA Fefers to the isotonic e$pansion of the 7.F caused by the abnormal retention of water and sodium There is e$cessive retention of water and electrolytes in e#ual proportion. 5erum sodium concentration remains 2/F'AL !athophysiology of Fluid =olume 7$cess 7tiologic conditions and Fisks factors .ongestive heart failure Fenal failure 7$cessive fluid intake Impaired ability to e$crete fluid as in renal disease .irrhosis of the liver .onsumption of e$cessive table salts Administration of e$cessive I=F Abnormal fluid retention !AT9/!9"5I/L/G" 7$cessive fluid e$pansion of blood volume edema, increased neck vein distention, tachycardia, hypertension. T>e Nursin< 9rocess in Fluid !olume E cess A55755'72T !hysical 7$amination &. Increased weight gain %. Increased urine output (. 'oist crackles in the lungs *. Increased .=! ,. istended neck veins :. -hee3ing 8. ependent edema 5ub+ective cue1s &. 5hortness of breath %. .hange in mental state Laboratory findings &. )U2 and .reatinine levels are L/- because of dilution %. Urine sodium and osmolality decreased Aurine becomes dilutedB (. .MF may show pulmonary congestion 2UF5I2G IAG2/5I5 o Fluid =olume e$cess I'!L7'72TATI/2
A55I5T I2 '7 I.AL I2T7F=72TI/2 Administer diuretics as prescribed Assist in hemodialysis !rovide dietary restriction of sodium and water 2UF5I2G 'A2AG7'72T &. .ontinually assess the patientNs condition by measuring intake and output, daily weight monitoring, edema assessment and breath sounds %. !revent Fluid =olume 7$cess by adhering to diet prescription of low salt? foods. (. etect and .ontrol Fluid =olume 7$cess by closely monitoring I=F therapy, administering medications, providing rest periods, placing in semi?fowlerNs position for lung e$pansion and providing fre#uent skin care for the edema *. Teach patient about edema, ascites, and fluid therapy. Advise elevation of the e$tremities, restriction of fluids, necessity of paracentesis, dialysis and diuretic therapy. ,. Instruct patient to avoid over?the?counter medications without first checking with the health care provider because they may contain sodium E(ECTRO(8TES 7lectrolytes are charged ions capable of conducting electricity and are solutes found in all body compartments. 3. Sources o" electrolytes Foods and ingested fluids, medicationsH I=F and T!2 solutions -. Functions o" Electrolytes 'aintains fluid balance Fegulates acid?base balance 2eeded for en3ymatic secretion and activation 2eeded for proper metabolism and effective contraction, nerve transmission
processes
of
muscular
1. Types o" Electrolytes .ATI/25? positively charged ionsH e$amples are sodium, potassium, calcium A2I/25? negatively charged ionsH e$amples are chloride and phosphatesO The ma+or I.F cation is potassium APQBH the ma+or I.F anion is !hosphates The ma+or 7.F cation is 5odium A2aQBH the ma+or 7.F anion is .hloride A.l?B D8NA7ICS OF E(ECTRO(8TE BA(ANCE 3. Electrolyte Distri=ution 7.F and I.F vary in their electrolyte distribution and concentration I.F has PQ, !/*?, proteins, 'gQ, .aQQ and 5/*? 7.F has 2aQ, .l?, 9./(? -. Electrolyte E cretion These electrolytes are e$cessively eliminated by abnormal fluid losses Foutes can be thru urine, feces, vomiting, surgical drainage, wound drainage and skin e$cretion 1. Re<ulation o" Electrolytes a@ Renal Re<ulation occurs by the process of glomerular filtration, tubular reabsorption and tubular secretion =@ Endocrine Re<ulation hormones play a role in this type of regulation; Aldosterone# promotes 2a retention and P e$cretion ANF# promotes 2a e$cretion 9T'# promotes .a retention and !/* e$cretion Calcitonin# promotes .a and !/* e$cretion c@ &IT Re<ulation electrolytes are absorbed and secreted some are e$creted thru the stool T'E CATIONS SODIU7 The most abundant cation in the 7.F 2ormal range in the blood is &(,?&*, m7#1L A loss or gain of sodium is usually accompanied by a loss or gain of water. 'a+or contributor of the plasma /smolality
5ources; iet, medications, I=F. The minimum daily re#uirement is % grams Imbalances? 9yponatremiaC R&(, m7#1LH 9ypernatremiaC S&*, m7#1L Functions; !articipates in the 2a?P pump Assists in maintaining blood volume Assists in nerve transmission and muscle contraction !rimary determinant of 7.F concentration. .ontrols water distribution throughout the body. !rimary regulator of 7.F volume. 5odium also functions in the establishment of the electrochemical state necessary for muscle contraction and the transmission of nerve impulses. <. Fegulations; skin, GIT, GUT, Aldosterone increases 2a retention in the kidney &. %. (. *. ,. :. 8. SODIU7 DEFICIT: '89ONATRE7IA Fefers to a 5odium serum level of less than &(, m7#1L. This may result from e$cessive sodium loss or e$cessive water gain. !athophysiology 7tiologic Factors &. Fluid loss such as from =omiting and nasogastric suctioning %. iarrhea (. 5weating *. Use of diuretics ,. Fistula /ther factors &. ilutional hyponatremia -ater into$ication, compulsive water drinking where sodium level is diluted with increased water intake %. 5IA 9 7$cessive secretion of A 9 causing water retention and dilutional hyponatremia 9yponatremia hypotonicity of plasma water from the intravascular space will move out and go to the intracellular compartment with a higher concentration cell swelling -ater is pulled I2T/ the cell because of decreased e$tracellular sodium level and increased intracellular concentration T>e Nursin< 9rocess in '89ONATRE7IA A55755'72T Sodium De"icit ?'yponatremia@ .linical 'anifestations .linical manifestations of hyponatremia depend on the cause, magnitude, and rapidity of onset. Although nausea and abdominal cramping occur, most of the symptoms are neuropsychiatric and are probably related to the cellular swelling and cerebral edema associated with hyponatremia. As the e$tracellular sodium level decreases, the cellular fluid becomes relatively more concentrated and TpullsE water into the cells. In general, those patients having acute decline in serum sodium levels have more severe symptoms and higher mortality rates than do those with more slowly developing hyponatremia. Features of hyponatremia associated with sodium loss and water gain include anore$ia, muscle cramps, and a feeling of e$haustion. -hen the serum sodium level drops below &&, m7#1L A5I; &&, mmol1LB, thee ff signs of increasing intracranial pressure occurs; o lethargy o .onfusion o muscular twitching o focal weakness o hemiparesis o papilledema o convulsions
In summary; !hysical 7$amination &. Altered mental status %. =omiting (. Lethargy *. 'uscle twitching and convulsions Aif sodium level is below &&, m7#1LB ,. Focal weakness 5ub+ective .ues &. 2ausea %. .ramps (. Anore$ia *. 9eadache Laboratory findings &. 5erum sodium level is less than &(, m7#1L %. ecreased serum osmolality (. Urine specific gravity is L/- if caused by sodium loss *. In 5IA 9, urine sodium is high and specific gravity is 9IG9 2UF5I2G IAG2/5I5 Altered cerebral perfusion Fluid volume 7$cess I'!L7'72TATI/2 A55I5T I2 '7 I.AL I2T7F=72TI/2 !rovide sodium replacement as ordered. Isotonic saline is usually ordered.. Infuse the solution very cautiously. The serum sodium must 2/T be increased by greater than &% m7#1L because of the danger of pontine osmotic demyelination Administer lithium and demeclocycline in 5IA 9 !rovide water restriction if with e$cess volume 2UF5I2G 'A2AG7'72T &. !rovide continuous assessment by doing an accurate intake and output, daily weights, mental status e$amination, urinary sodium levels and GI manifestations. 'aintain sei3ure precaution %. etect and control 9yponatremia by encouraging food intake with high sodium content, monitoring patients on lithium therapy, monitoring input of fluids like I=F, parenteral medication and feedings. (. Feturn the 5odium level to 2ormal by restricting water intake if the primary problem is water retention. Administer sodium to normovolemic patient and elevate the sodium slowly by using sodium chloride solution SODIU7 ECCESS: '89ERNATRE7IA 5erum 5odium level is higher than &*, m7#1L There is a gain of sodium in e$cess of water or a loss of water in e$cess of sodium. !athophysiology; 7tiologic factors &. Fluid deprivation %. -ater loss from -atery diarrhea, fever, and hyperventilation (. Administration of hypertonic solution *. Increased insensible water loss ,. Inade#uate water replacement, inability to swallow :. 5eawater ingestion or e$cessive oral ingestion of salts /ther factors &. iabetes insipidus %. 9eat stroke (. 2ear drowning in ocean *. 'alfunction of dialysis Increased sodium concentration hypertonic plasma water will move out form the cell outside to the interstitial space .7LLULAF 59FI2PAG7 then to the blood -ater pulled from cells because of increased e$tracellular sodium level and decreased cellular fluid concentration T>e Nursin< 9rocess in '89ERNATRE7IA A. Sodium E cess ?'ypernatremia@
.linical 'anifestations primarily neurologic !resumably the conse#uence of cellular dehydration. 9ypernatremia results in a relatively concentrated 7.F, causing water to be pulled from the cells. .linically, these changes may be manifested by; o restlessness and weakness in moderate hypernatremia o disorientation, delusions, and hallucinations in severe hypernatremia. ehydration AhypernatremiaB is often overlooked as the primary reason for behavioral changes in the elderly. If hypernatremia is severe, permanent brain damage can occur Aespecially in childrenB. )rain damage is apparently due to subarachnoid hemorrhages that result from brain contraction. A primary characteristic of hypernatremia is thirst. Thirst is so strong a defender of serum sodium levels in normal people that hypernatremia never occurs unless the person is unconscious or is denied access to waterH unfortunately, ill people may have an impaired thirst mechanism. /ther signs include dry, swollen tongue and sticky mucous membranes. A mild elevation in body temperature may occur, but on correction of the hypernatremia the body temperature should return to normal. A55755'72T !hysical 7$amination &. Festlessness, elevated body temperature %. isorientation (. ry, swollen tongue and sticky mucous membrane, tented skin turgor *. Flushed skin, postural hypotension ,. Increased muscle tone and deep refle$es :. !eripheral and pulmonary edema 5ub+ective .ues &. elusions and hallucinations %. 7$treme thirst (. )ehavioral changes Laboratory findings &. 5erum sodium level e$ceeds &*, m7#1L %. 5erum osmolality e$ceeds %>, m/sm1kg (. Urine specific gravity and osmolality I2.F7A57 or elevated I'!L7'72TATI/2 A55I5T I2 T97 '7 I.AL I2T7F=72TI/2 &. Administer hypotonic electrolyte solution slowly as ordered %. Administer diuretics as ordered (. esmopressin is prescribed for diabetes insipidus 2UF5I2G 'A2AG7'72T &. .ontinuously monitor the patient by assessing abnormal loses of water, noting for the thirst and elevated body temperature and behavioral changes %. !revent hypernatremia by offering fluids regularly and plan with the physician alternative routes if oral route is not possible. 7nsure ade#uate water for patients with I. Administer I=F therapy cautiously (. .orrect the 9ypernatremia by monitoring the patientNs response to the I=F replacement. Administer the hypotonic solution very slowly to prevent sudden cerebral edema. *. 'onitor serum sodium level. ,. Feposition client regularly, keep side?rails up, the bed in low position and the call bell1light within reach. :. !rovide teaching to avoid over?the counter medications without consultation as they may contain sodium 9OTASSIU7 The most abundant cation in the I.F !otassium is the ma+or intracellular electrolyteH in fact, ><0 of the bodyNs potassium is inside the cells. The remaining %0 is in the 7.FH it is this %0 that is all?important in neuromuscular function. !otassium is constantly moving in and out of cells according to the bodyNs needs, under the influence of the sodium?potassium pump.
2ormal range in the blood is (.,?, m7#1L 2ormal renal function is necessary for maintenance of potassium balance, because <6?>60 of the potassium is e$creted daily from the body by way of the kidneys. The other less than %60 is lost through the bowel and sweat glands. 'a+or electrolyte maintaining I.F balance 5ources? iet, vegetables, fruits, I=F, medications Functions; &. 'aintains I.F /smolality %. Important for nerve conduction and muscle contraction (. 'aintains acid?base balance *. 2eeded for metabolism of carbohydrates, fats and proteins ,. !otassium influences both skeletal and cardiac muscle activity. a. For e$ample, alterations in its concentration change myocardial irritability and rhythm. Fegulations; renal secretion and e$cretion, Aldosterone promotes renal e$cretion acidosis promotes P e$change for hydrogen Imbalances; 9ypokalemiaC R(., m7#1L 9yperkalemiaCS ,.6 m7#1L 9OTASSIU7 DEFICIT: '89O$A(E7IA .ondition when the serum concentration of potassium is less than (., m7#1L !athophysiology 7tiology &. Gastro?intestinal loss of potassium such as diarrhea and fistula %. =omiting and gastric suctioning (. 'etabolic alkalosis *. iaphoresis and renal disorders ,. Ileostomy /ther factor1s &. 9yperaldosteronism %. 9eart failure (. 2ephrotic syndrome *. Use of potassium?losing diuretics ,. Insulin therapy :. 5tarvation 8. Alcoholics and elderly ecreased potassium in the body impaired nerve e$citation and transmission signs1symptoms such as weakness, cardiac dysrhythmias etc.. T>e Nursin< 9rocess in 'ypo)alemia 9otassium De"icit ?'ypo)alemia@ .linical 'anifestations !otassium deficiency can result in widespread derangements in physiologic functions and especially nerve conduction. 'ost important, severe hypokalemia can result in death through cardiac or respiratory arrest. .linical signs rarely develop before the serum potassium level has fallen below ( m7#1L A,&; ( mmol1LB unless the rate of fall has been rapid. 'anifestations of hypokalemia include fatigue, anore$ia, nausea, vomiting, muscle weakness, decreased bowel motility, paresthesias, dysrhythmias, and increased sensitivity to digitalis. If prolonged, hypokalemia can lead to impaired renal concentrating ability, causing dilute urine, polyuria, nocturia, and polydipsia ASSESS7ENT !hysical e$amination &. 'uscle weakness %. ecreased bowel motility and abdominal distention (. !aresthesias *. ysrhythmias ,. Increased sensitivity to digitalis 5ub+ective cues &. 2ausea , anore$ia and vomiting
%. Fatigue, muscles cramps (. 7$cessive thirst, if severe Laboratory findings &. 5erum potassium is less than (., m7#1L %. 7.G; FLAT DTE waves, or inverted T waves, depressed 5T segment and presence of the DUE wave and prolonged !F interval. (. 'etabolic alkalosis I79(E7ENTATION ASSIST IN T'E 7EDICA( INTER!ENTION &. !rovide oral or I= replacement of potassium %. Infuse parenteral potassium supplement. Always dilute the P in the I=F solution and administer with a pump. I=F with potassium should be given no faster than &6?%6?m7#1 hourL (. 27=7F administer P by I= bolus or I' NURSIN& 7ANA&E7ENT &. .ontinuously monitor the patient by assessing the cardiac status, 7.G monitoring, and digitalis precaution %. !revent hypokalemia by encouraging the patient to eat potassium rich foods like orange +uice, bananas, cantaloupe, peaches, potatoes, dates and apricots. (. .orrect hypokalemia by administering prescribed I= potassium replacement. The nurse must ensure that the kidney is functioning properlyL *. Administer I= potassium no faster than %6 m7#1hour and hook the patient on a cardiac monitor. To 7'!9A5IU7; !otassium should 27=7F be given I= bolus or I'LL ,. A concentration greater than :6 m7#1L is not advisable for peripheral veins. 9OTASSIU7 ECCESS: '89ER$A(E7IA 5erum potassium greater than ,., m7#1L !athophysiology 7tiologic factors &. Iatrogenic, e$cessive intake of potassium %. Fenal failure? decreased renal e$cretion of potassium (. 9ypoaldosteronism and AddisonNs disease *. Improper use of potassium supplements /ther factors &. !seudohyperkalemia? tight tourni#uet and hemolysis of blood sample, marked leukocytosis %. Transfusion of DoldE banked blood (. Acidosis *. 5evere tissue trauma Increased potassium in the body .ausing irritability of the cardiac cells !ossible arrhythmiasLL The 2ursing !rocess in 9yperkalemia 9otassium E cess ?'yper)alemia@ .linical 'anifestations )y far the most clinically important effect of hyperkalemia is its effect on the myocardium. .ardiac effects of an elevated serum potassium level are usually not significant below a concentration of 8 m7#1L A5I; 8 mmol1LB, but they are almost always present when the level is < m7#1L A5I; < mmol1LB or greater. As the plasma potassium concentration is increased, disturbances in cardiac conduction occur. The earliest changes, often occurring at a serum potassium level greater than : m7#1 L A5I; : mmol1LB, are peaked narrow T waves and a shortened VT interval. If the serum potassium level continues to rise, the !F interval becomes prolonged and is followed by disappearance of the ! waves.
Finally, there is decomposition and prolongation of the VF5 comple$. =entricular dysrhythmias and cardiac arrest may occur at any point in this progression. 2ote that in 5evere hyperkalemia causes muscle weakness and even paralysis, related to a depolari3ation block in muscle. 5imilarly, ventricular conduction is slowed. Although hyperkalemia has marked effects on the peripheral neuromuscular system, it has little effect on the central nervous system. Fapidly ascending muscular weakness leading to flaccid #uadriplegia has been reported in patients with very high serum potassium levels. !aralysis of respiratory muscles and those re#uired for phonation can also occur. Gastrointestinal manifestations, such as nausea, intermit tent intestinal colic, and diarrhea, may occur in hyperkalemic patients. A55755'72T !hysical 7$amination &. iarrhea %. 5keletal muscle weakness (. Abnormal cardiac rate 5ub+ective .ues &. 2ausea %. Intestinal pain1colic (. !alpitations Laboratory Findings &. !eaked and narrow T waves %. 5T segment depression and shortened VT interval (. !rolonged !F interval *. !rolonged VF5 comple$ ,. isappearance of ! wave :. 5erum potassium is higher than ,., m7#1L 8. Acidosis I'!L7'72TATI/2 A55I5T I2 '7 I.AL I2T7F=72TI/2 &. 'onitor the patientNs cardiac status with cardiac machine %. Institute emergency therapy to lower potassium level by; a. Administering I= calcium gluconate? antagoni3es action of P on cardiac conduction b. Administering Insulin with de$trose?causes temporary shift of P into cells c. Administering sodium bicarbonate?alkalini3es plasma to cause temporary shift d. Administering )eta?agonists e. Administering Paye$alate Acation?e$change resinB?draws PQ into the bowel 2UF5I2G 'A2AG7'72T &. !rovide continuous monitoring of cardiac status, dysrhythmias, and potassium levels. %. Assess for signs of muscular weakness, paresthesias, nausea (. 7valuate and verify all 9IG9 serum P levels *. !revent hyperkalemia by encouraging high risk patient to adhere to proper potassium restriction ,. .orrect hyperkalemia by administering carefully prescribed drugs. 2urses must ensure that clients receiving I=F with potassium must be always monitored and that the potassium supplement is given correctly :. Assist in hemodialysis if hyperkalemia cannot be corrected. 8. !rovide client teaching. Advise patients at risk to avoid eating potassium rich foods, and to use potassium salts sparingly. <. 'onitor patients for hypokalemia who are receiving potassium?sparing diuretic CA(CIU7
'a+ority of calcium is in the bones and teeth 5mall amount may be found in the 7.F and I.F 2ormal serum range is <., W &6., mg1dL 5ources; milk and milk productsH dietH I=F and medications Functions; &. 2eeded for formation of bones and teeth %. For muscular contraction and rela$ation (. For neuronal and cardiac function *. For en3ymatic activation ,. For normal blood clotting Fegulations; &. GIT? absorbs .aQ in the intestineH =itamin helps to increase absorption %. Fenal regulation? .aQ is filtered in the glomerulus and reabsorbed in the tubules; (. 7ndocrine regulation; !arathyroid hormone from the parathyroid glands is released when .aQ level is low. !T9 causes release of calcium from bones and increased retention of calcium by the kidney but !/* is e$creted .alcitonin from the thyroid gland is released when the calcium level is high. This causes e$cretion of both calcium and !/* in the kidney and promoted deposition of calcium in the bones. Imbalances? 9ypocalcemiaC R<., mg1dLH 9ypercalcemiaC S&6., mg1dL T'E ANIONS C'(ORIDE The ma+or Anion of the 7.F 2ormal range is >,?&6< m7#1L 5ources; iet, especially high salt foods, I=F Alike 255B, 9.l Ain the stomachB Functions; &. 'a+or component of gastric +uice %. Fegulates serum /smolality and blood volume (. !articipates in the chloride shift *. Acts as chemical buffer Fegulations; Fenal regulation by absorption and e$cretionH GIT absorption Imbalances; 9ypochloremiaC R >, m7#1LH 9yperchloremiaC S&6< m7#1L 9'OS9'ATES The ma+or Anion of the I.F 2ormal range is %., to *., mg1dL 5ources; iet, T!2, )one reserves Functions; &. .omponent of bones, muscles and nerve tissues %. 2eeded by the cells to generate AT! (. 2eeded for the metabolism of carbohydrates, fats and proteins *. .omponent of 2A and F2A Fegulations; Fenal glomerular filtration, endocrinal regulation by !T9? decreases !/* in the blood by kidney e$cretion Imbalances? 9ypophosphatemiaC R%., mg1dLH 9yperphosphatemia S*., mg1dL BICARBONATES !resent in both I.F and 7.F Fegulates acid?base balance together with hydrogen 2ormal range is %%?%: m7#1L 5ources; ietH medications and metabolic by?products of the cells. Function; .omponent of the bicarbonate?carbonic acid buffer system Fegulation; Pidney production, absorption and secretion Imbalances; 'etabolic acidosisC R%% m7#1LH 'etabolic alkalosisC S%: m7#1
ACID BASE BA(ANCE Acids substances that can donate or release protons or hydrogen ions A9QBH e$amples are 9.l, carbonic acid, acetic acid. )ases or alkalis substances that can accept protons or hydrogen ions because they have low 9Q concentration. The ma+or base in the body is )I.AF)/2AT7 A9./(B .arbon dio$ide is considered to be acid or base depending on its chemical association -hen assessing acid?base balance, carbon dio$ide is considered A.I because of its relationship with carbonic acid. )ecause carbonic acid cannot be routinely measured, carbon dio$ide is used. p9? is the measurement of the degree of acidity or alkalinity of a solution. This reflects the relationship of hydrogen ion concentration in the solution. The higher the hydrogen ion concentration, the acidic is the solution and p9 is L/ The lower the hydrogen concentration, the alkaline is the solution and the p9 is 9IG9 2ormal p9 in the blood is between 8.(, to 8.*, SU99(8 AND SOURCES OF ACIDS AND BASES 5ources of acids and bases are from; &. 7.F, I.F and body tissues %. Foodstuff (. 'etabolic products of cells like ./%, lactic acids, and ammonia D8NA7ICS OF ACID#BASE BA(ANCE Acids are constantly produced in the body )ecause cellular processes need normal p9, acids and bases must be balanced continuously ./% and 9./( are crucial in maintaining the balance A ratio of 9./( and .arbonic acid is maintained at %6;& 5everal body systems Alike the respiratory, renal and GITB together with the chemical buffers are actively involved in the normal p9 balance The ma+or ways in which balance is maintained are the process of acid1base secretion, production, e$cretion and neutrali3ation 3. RE&U(ATION OF ACID#BASE BA(ANCE B8 T'E C'E7ICA( BUFFER )uffers are present in all body fluids functioning mainly to prevent e$cessive changes in the p9. )uffers either remove1accept 9Q or release1donate 9Q The ma+or chemical buffers are; &. .arbonic acid?)icarbonate )uffer Ain the 7.FB %. !hosphate buffer Ain the 7.F and I.FB (. !rotein buffer Ain the I.FB The action of the chemical buffer is immediate but limited -. RE&U(ATION OF ACID#BASE BA(ANCE B8 RES9IRATOR8 S8STE7 The respiratory center in the medulla is involved .arbon dio$ide is the powerful stimulator of the respiratory center The lungs use ./% to regulate 9Q ion concentration Through the changes in the breathing pattern, acid?base balance is achieved within minutes Functions of the respiratory system in acid?base balance; &. ./% Q 9%/ 9%./( %. ./%activates medullaFF./% is e$haled p9 rises to normal (. 9./(depresses FF./% is retained)icarbonate is neutrali3ed p9 drops to normal 1. RE&U(ATION OF ACID#BASE BA(ANCE B8 T'E $IDNE8 Long term regulator of the acid?base balance
5lower to respond but more permanent Achieved by ( interrelated processes &. )icarbonate reabsorption in the nephron %. )icarbonate formation (. 9ydrogen ion e$cretion -hen e$cess 9Q is present AacidicB, p9 fallskidney reabsorbs and generates )icarbonate and e$cretes 9Q -hen 9Q is low and 9./( is high AalkaloticB. p9 rises kidney e$cretes 9./( and 9Q is retained. Normal Arterial Blood &as !alues &. p9 W 8.(,?8.*, %. p/% W <6?&66 mm9g (. p./% W (,?*, mm9g *. 9co( W %%?%: m7#1L ,. )ase deficit17$cess W AQ1?B% :. /% saturation W ><?&660 FACTORS AFFECTIN& BOD8 F(UIDSD E(ECTRO(8TES AND ACID#BASE BA(ANCE 3. A&E Infants have higher proportion of body water than adults -ater content of the body decreases with age Infants have higher fluid turn?over due to immature kidney and rapid respiratory rate 3. &ENDER AND BOD8 SIEE -omen have higher body fat content but lesser water content Lean body has higher water content -. EN!IRON7ENT AND TE79ERATURE .limate and heat and humidity affect fluid balance 1. DIET AND (IFEST8(E Anore$ia nervosa will lead to nutritional depletion 5tressful situations will increase metabolism, increase A 9 causing water retention and increased blood volume .hronic Alcohol consumption causes malnutrition 2. I((NESS Trauma and burns release PQ in the blood .ardiac dysfunction will lead to edema and congestion 0. 7EDICA( TREAT7ENTD 7EDICATIONS AND SUR&ER8 5uctioning, diuretics and la$atives may cause imbalances Acid Base Im=alances 7eta=olic Al)alosis A base bicarbonate e$cess A result of a loss of acid and the accumulation of bases 515 ? serum p9 S 8.*,, increased serum 9./(, serum P level less than *, tetany, confusion and convulsions 2ursing Interventions ? watch for s1s of hypokalemia, L/. and sei3ure precautions 7eta=olic Acidosis A base bicarbonate deficit .omes from too much acid from metabolism and loss of bicarbonate 515 ? 5erum p9 R8.(,, Increased PQ level, PA APussmaulNs FespirationsB, 5hock, stupor, coma 2ursing Intervention ? Give 9./(1'onitor PQ levels
Respiratory Al)alosis A deficit of carbonic acid caused by hyperventilation 515 ? decreased levels of ./% and increased levels of p9, 9./( near normal 2ursing Interventions ? monitor for an$iety and observe for signs and symptoms of tetany Respiratory Al)alosis A carbonic acid e$cess .aused by an condition that interferes with the release of ./% from the lungs Asedatives, ./! , narcotics etc.B 515 ? serum p9 R 8.(,, increased serum ./% levelsS *, mm 9g, serum P increased, cyanosis 2ursing Interventions ? !rovide /%, 5emifowlers position, sei3ure precautions Interpretation Arterial Blood &ases If acidosis the p9 is down If alkalosis the p9 is up The respiratory function indicator is the !./% The metabolic function indicator is the 9./( 5tep & Look at the p9 Is it up or downX If it is up ? it reflects alkalosis If it is down ? it reflects acidosis 5tep % Look at the !./% Is it up or downX If it reflects an opposite response as the p9, then you know that the condition is a respiratory imbalance If it does not reflect an opposite response as the p9 ? move to step III 5tep ( Look at the 9./( oes the 9./( reflect a corresponding response with the p9 If it does then the condition is a metabolic imbalance
Das könnte Ihnen auch gefallen
- Gastrointestinal Anatomy and Physiology: The EssentialsVon EverandGastrointestinal Anatomy and Physiology: The EssentialsJohn F. ReinusNoch keine Bewertungen
- Basic Concept of OxygenationDokument50 SeitenBasic Concept of OxygenationWiradianto PutroNoch keine Bewertungen
- Acute Kidney Injury (AKI) :: FeaturesDokument3 SeitenAcute Kidney Injury (AKI) :: FeaturesDavid PerezNoch keine Bewertungen
- Cardiovascular FunctionDokument157 SeitenCardiovascular FunctionJonnabelle PadillaNoch keine Bewertungen
- Cesarean Section PrimaryDokument33 SeitenCesarean Section PrimaryKazvin Carl PeraltaNoch keine Bewertungen
- Complications of LaborDokument54 SeitenComplications of Laborallie-jones-6489100% (2)
- BODY Weight 100%: Balance/Imbalances & TherapyDokument11 SeitenBODY Weight 100%: Balance/Imbalances & TherapyVictoria Castillo TamayoNoch keine Bewertungen
- Midterm Quiz - NCM 106.2016Dokument4 SeitenMidterm Quiz - NCM 106.2016Andrea BroccoliNoch keine Bewertungen
- Nursing Care During Labor and Pain Management2015Dokument51 SeitenNursing Care During Labor and Pain Management2015christopher ebarbNoch keine Bewertungen
- Group 5 - Hemodialysis - Chronic Kidney FailureDokument31 SeitenGroup 5 - Hemodialysis - Chronic Kidney FailureKimberly Abella CabreraNoch keine Bewertungen
- LasixDokument1 SeiteLasixKatie McPeek100% (2)
- Pediatric Nursing (Nomral) : Psychiatric (Sigmund Freud) Nursing Concept Range Extends To The 18 MonthDokument6 SeitenPediatric Nursing (Nomral) : Psychiatric (Sigmund Freud) Nursing Concept Range Extends To The 18 MonthVon R SemillaNoch keine Bewertungen
- Common Medical AbbreviationsDokument3 SeitenCommon Medical AbbreviationsBráian Tzéims άλμπαNoch keine Bewertungen
- A-T-I Endocrine NotesDokument3 SeitenA-T-I Endocrine NotesKelseyAnnBarnesNoch keine Bewertungen
- Endocrine: Common Lab Tests For Endocrine and Hormonal DisordersDokument19 SeitenEndocrine: Common Lab Tests For Endocrine and Hormonal DisordersPhilip SimanganNoch keine Bewertungen
- Hyperemesis Gravidarum: Bleeding Complications of PregnancyDokument6 SeitenHyperemesis Gravidarum: Bleeding Complications of PregnancykirbsNoch keine Bewertungen
- UrinalysisDokument9 SeitenUrinalysisyuppierajNoch keine Bewertungen
- Pharmacokinetics For Test 1Dokument3 SeitenPharmacokinetics For Test 1KaitlynNoch keine Bewertungen
- Completed Concept MapDokument4 SeitenCompleted Concept Mapapi-607361848Noch keine Bewertungen
- Antipsychotic Drugs: Conventional AntipsychoticsDokument16 SeitenAntipsychotic Drugs: Conventional AntipsychoticsApple MaeNoch keine Bewertungen
- Drugs in The Neonatal Unit: 1 Julia PettyDokument5 SeitenDrugs in The Neonatal Unit: 1 Julia PettyMarjoNoch keine Bewertungen
- Week 11 - Ch. 36 - UrinaryDokument27 SeitenWeek 11 - Ch. 36 - UrinaryMary SingletonNoch keine Bewertungen
- Umbilical Cord Prolapse: Green-Top Guideline No. 50Dokument13 SeitenUmbilical Cord Prolapse: Green-Top Guideline No. 50Nurul Aimi Abdul RahmanNoch keine Bewertungen
- 4 Urinary and Bowel EliminationDokument59 Seiten4 Urinary and Bowel Eliminationsechzhen100% (1)
- Labor DeliveryDokument10 SeitenLabor Deliverydhodejun lizhaldeNoch keine Bewertungen
- Insulin AdministrationDokument15 SeitenInsulin Administrationmec17Noch keine Bewertungen
- Endocrine System 2Dokument7 SeitenEndocrine System 2Lhaura Joy ArsenioNoch keine Bewertungen
- Quizlet EndoDokument17 SeitenQuizlet EndoemmaNoch keine Bewertungen
- Antepartum 1Dokument3 SeitenAntepartum 1Emily DavisNoch keine Bewertungen
- Nclex ReviewDokument113 SeitenNclex Reviewk johnstonNoch keine Bewertungen
- ST ND RDDokument12 SeitenST ND RDwaterbuglilyNoch keine Bewertungen
- Alteration in OxygenationDokument8 SeitenAlteration in Oxygenationraquel maniegoNoch keine Bewertungen
- Fluidsandelectrolytes 090224074347 Phpapp02Dokument102 SeitenFluidsandelectrolytes 090224074347 Phpapp02IsaacJ22Noch keine Bewertungen
- NURS 3337 Day1 WorkbookDokument18 SeitenNURS 3337 Day1 WorkbookEmerald Holly TagoNoch keine Bewertungen
- Antepartum PeriodDokument3 SeitenAntepartum PeriodjisooNoch keine Bewertungen
- The Process of OxygenationDokument7 SeitenThe Process of OxygenationMich CercadoNoch keine Bewertungen
- Pharmacology: General Anaesthetic AgentsDokument65 SeitenPharmacology: General Anaesthetic AgentsSharifa DarayanNoch keine Bewertungen
- Pneumonia and BronchiolitisDokument48 SeitenPneumonia and Bronchiolitisshashank panwarNoch keine Bewertungen
- Pharmacology Test 3 ReviewDokument6 SeitenPharmacology Test 3 ReviewNatalia BortellNoch keine Bewertungen
- SimulationDokument5 SeitenSimulationJessFriend100% (1)
- Celiac DiseaseDokument37 SeitenCeliac DiseaseTaj lamajed100% (1)
- Pregnancy Induced Hypertension PihDokument17 SeitenPregnancy Induced Hypertension PihRose DeymNoch keine Bewertungen
- OB Study GuideDokument43 SeitenOB Study Guidelilchibaby3161100% (1)
- Fluids and Electrolytes: Irene L. Gardiner, MDDokument48 SeitenFluids and Electrolytes: Irene L. Gardiner, MDGabriel Carlo FranciscoNoch keine Bewertungen
- IV FluidsDokument17 SeitenIV FluidsTiffany NicolèNoch keine Bewertungen
- Drugs Affecting Blood PressureDokument54 SeitenDrugs Affecting Blood PressureJeremy VivitNoch keine Bewertungen
- Hepatobiliary Disorders: Katrina Saludar Jimenez, R. NDokument42 SeitenHepatobiliary Disorders: Katrina Saludar Jimenez, R. NKatrinaJimenezNoch keine Bewertungen
- Management of Patients With Neurologic Infections, Autoimmune Disorders & NeuropathiesDokument92 SeitenManagement of Patients With Neurologic Infections, Autoimmune Disorders & NeuropathiesejarnmdNoch keine Bewertungen
- Immunity 1Dokument6 SeitenImmunity 1Tori RolandNoch keine Bewertungen
- NclexDokument4 SeitenNclexihatetouNoch keine Bewertungen
- PHARMACOLOGYDokument19 SeitenPHARMACOLOGYIligan, JamaicahNoch keine Bewertungen
- Set Ea505092Dokument3 SeitenSet Ea505092davidvpnNoch keine Bewertungen
- Nursing Care of Client With Endocrine DisorderDokument93 SeitenNursing Care of Client With Endocrine DisorderApril_Anne_Vel_343Noch keine Bewertungen
- 2017 Fluid and Electrolytes LECTURE NOTESDokument34 Seiten2017 Fluid and Electrolytes LECTURE NOTESHarley Justiniani Dela CruzNoch keine Bewertungen
- POSTPARTUM-scenario2 bsn2dDokument4 SeitenPOSTPARTUM-scenario2 bsn2dHannah VillavicencioNoch keine Bewertungen
- Mod Family Planning Final PDFDokument124 SeitenMod Family Planning Final PDFPatricia Anne EsmedillaNoch keine Bewertungen
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideVon EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNoch keine Bewertungen
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- BioKids Parent HandbookDokument11 SeitenBioKids Parent HandbookNano BaddourNoch keine Bewertungen
- 2009 Student Code of ConductDokument11 Seiten2009 Student Code of ConductNano BaddourNoch keine Bewertungen
- Neurology ICM-Seizures and Epilepsy Learning ObjectivesDokument3 SeitenNeurology ICM-Seizures and Epilepsy Learning ObjectivesNano BaddourNoch keine Bewertungen
- 6638 Neonnatal Assessement and Examination Term NewbornDokument8 Seiten6638 Neonnatal Assessement and Examination Term NewbornNano BaddourNoch keine Bewertungen
- UW History Examination Important PointsDokument41 SeitenUW History Examination Important PointsNano Baddour100% (1)
- Vac Care Handbook V1Dokument14 SeitenVac Care Handbook V1Nano BaddourNoch keine Bewertungen
- Hands:, Tablets, Wheelchair, WarfarinDokument16 SeitenHands:, Tablets, Wheelchair, WarfarinRhythm VasudevaNoch keine Bewertungen
- Ent RevisionDokument104 SeitenEnt RevisionNano BaddourNoch keine Bewertungen
- Fluid and ElectrolytesDokument137 SeitenFluid and ElectrolytesNano Baddour100% (1)
- FluidDokument2 SeitenFluidXoul IsmailNoch keine Bewertungen
- Hyponat HypernatremiaDokument14 SeitenHyponat HypernatremiaNano BaddourNoch keine Bewertungen
- Fluids and ElectrolytesDokument66 SeitenFluids and ElectrolytesJhedNuquiNoch keine Bewertungen
- Doctor S GuideDokument900 SeitenDoctor S GuidedrvijeypsgNoch keine Bewertungen
- JAUNDICE Internal Medicine PresentationDokument34 SeitenJAUNDICE Internal Medicine PresentationNano BaddourNoch keine Bewertungen
- ENTDokument4 SeitenENTNano BaddourNoch keine Bewertungen
- NZ Doctors BookletDokument49 SeitenNZ Doctors BookletNano BaddourNoch keine Bewertungen
- Dust Mites and Bed BugsDokument2 SeitenDust Mites and Bed BugsNano BaddourNoch keine Bewertungen
- Symptoms Differential ChartsDokument52 SeitenSymptoms Differential ChartsXiaxin Liu100% (2)
- MuskuloskeletalDokument41 SeitenMuskuloskeletalNano BaddourNoch keine Bewertungen
- CNSinfections 4Dokument1 SeiteCNSinfections 4Nano BaddourNoch keine Bewertungen
- Volar Wrist LacerationsDokument4 SeitenVolar Wrist LacerationsNano BaddourNoch keine Bewertungen
- Research Example Chapter 1Dokument8 SeitenResearch Example Chapter 1C Augustina S Fellazar100% (1)
- Systemic Complications of Iv Therapy Complications Assessment Nursing Management Fluid OverloadDokument4 SeitenSystemic Complications of Iv Therapy Complications Assessment Nursing Management Fluid OverloadMakagago And BruskoNoch keine Bewertungen
- Acid Base PhysiologyDokument1 SeiteAcid Base PhysiologyHAMMYER ALROKHAMINoch keine Bewertungen
- Why Jaggery? Is Jaggery Healthy? What Is Better: Jaggery or Sugar? Can Jaggery Cure Ailments?Dokument5 SeitenWhy Jaggery? Is Jaggery Healthy? What Is Better: Jaggery or Sugar? Can Jaggery Cure Ailments?satheb319429Noch keine Bewertungen
- Environmental Studies-FIRST UNIT-vkmDokument59 SeitenEnvironmental Studies-FIRST UNIT-vkmRandomNoch keine Bewertungen
- Adr Enaline (Epinephrine) 1mg/ml (1:1000) : Paediatric Cardiac Arrest AlgorhytmDokument13 SeitenAdr Enaline (Epinephrine) 1mg/ml (1:1000) : Paediatric Cardiac Arrest AlgorhytmwawaNoch keine Bewertungen
- Protokol KemoterapiDokument147 SeitenProtokol KemoterapiDala VW100% (1)
- Tap Presentation - Google SlidesDokument12 SeitenTap Presentation - Google Slidesapi-208317298Noch keine Bewertungen
- China Animal Healthcare: The Healing TouchDokument19 SeitenChina Animal Healthcare: The Healing TouchBin WeiNoch keine Bewertungen
- Menstrual Blood Derived Stem Cells and Their Scope in Regenerative Medicine A Review ArticleDokument6 SeitenMenstrual Blood Derived Stem Cells and Their Scope in Regenerative Medicine A Review ArticleInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Extended Spectrum BetalactamasesDokument63 SeitenExtended Spectrum Betalactamasestummalapalli venkateswara raoNoch keine Bewertungen
- Complications of DiabetesDokument3 SeitenComplications of Diabetesa7wfNoch keine Bewertungen
- Expression of Interest - Elective Placement For Medical StudentsDokument2 SeitenExpression of Interest - Elective Placement For Medical Studentsfsdfs100% (1)
- Growth Comparison in Children With and Without Food Allergies in 2 Different Demographic PopulationsDokument7 SeitenGrowth Comparison in Children With and Without Food Allergies in 2 Different Demographic PopulationsMaria Agustina Sulistyo WulandariNoch keine Bewertungen
- U.S. Fund For UNICEF Annual Report 2010Dokument44 SeitenU.S. Fund For UNICEF Annual Report 2010U.S. Fund for UNICEF100% (1)
- 10a General Pest Control Study GuideDokument128 Seiten10a General Pest Control Study GuideRomeo Baoson100% (1)
- Nur Writing - Marilyn JohnsonDokument4 SeitenNur Writing - Marilyn Johnsonyinghua guo0% (1)
- Annex I Summary of Product CharacteristicsDokument29 SeitenAnnex I Summary of Product CharacteristicslisnerisNoch keine Bewertungen
- ScenarioDokument1 SeiteScenarioAngel Lynn YlayaNoch keine Bewertungen
- Punjab Municipal Corporation Act, 1976 PDFDokument180 SeitenPunjab Municipal Corporation Act, 1976 PDFSci UpscNoch keine Bewertungen
- NURSING CARE PLAN - Decreased Cardiac OutputDokument2 SeitenNURSING CARE PLAN - Decreased Cardiac OutputRy Pablo83% (41)
- 3E - Agustin, Anne Julia - Group 1 - Case 7,8Dokument5 Seiten3E - Agustin, Anne Julia - Group 1 - Case 7,8Anne Julia AgustinNoch keine Bewertungen
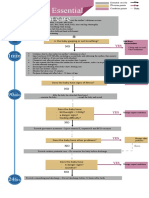
- Algorithm: Essential Newborn Care: Is The Baby Gasping or Not Breathing?Dokument1 SeiteAlgorithm: Essential Newborn Care: Is The Baby Gasping or Not Breathing?Dela cruz KimberlyNoch keine Bewertungen
- Beauty Care 1st Summative TestDokument4 SeitenBeauty Care 1st Summative TestLlemor Soled SeyerNoch keine Bewertungen
- Formulation and Evaluation of Herbal Lip Rouge.: Research ArticleDokument5 SeitenFormulation and Evaluation of Herbal Lip Rouge.: Research ArticleTynNoch keine Bewertungen
- Subjective: Diarrhea Related To Watery Short Term: IndependentDokument4 SeitenSubjective: Diarrhea Related To Watery Short Term: IndependentEmma Lyn SantosNoch keine Bewertungen
- Msds ChloroformDokument9 SeitenMsds ChloroformAhmad ArisandiNoch keine Bewertungen
- Guidelines EuromyastheniaDokument4 SeitenGuidelines Euromyastheniadokter mudaNoch keine Bewertungen
- Mood Disorders - Psychology ProjectDokument16 SeitenMood Disorders - Psychology ProjectKanika Mathew100% (1)
- NUR091 - Session 8Dokument6 SeitenNUR091 - Session 8aquinoemjay27Noch keine Bewertungen