Beruflich Dokumente
Kultur Dokumente
Obstetric Anesthesia and Ambulatory Anesthesia
Hochgeladen von
Erinne DefrianiOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Obstetric Anesthesia and Ambulatory Anesthesia
Hochgeladen von
Erinne DefrianiCopyright:
Verfügbare Formate
OBSTETRIC ANESTHESIA AND AMBULATORY ANESTHESIA Berrin Gunaydin, MD, PhD Depart ent !" Ane#the#i!$!%y & Di'i#i!
n !" O(#tetri) Ane#the#ia *a)u$ty !" Medi)ine, Ga+i Uni'er#ity, An,ara& Tur,ey Ba),%r!undAmbulatory obstetric surgery enables fast recovery of vital functions, ambulation and a relational life of quality and procedure costs can be significantly reduced when a hospital stay is avoided. Many factors affect ambulatory surgery or procedures. For instance; length of surgery is not a criterion for ambulatory procedures because patients undergoing longer procedures should have their operations earlier in the day. Therefore, improved material and surgical practices broaden potential indications of ambulatory surgery. The choice of the anesthetic techniques or the agents used during the intervention ensures fast recovery of higher functions and limits the risk of postoperative pain which can be controlled with simple analgesic protocols. owever, use of teratogenic drugs before, during and after the procedure particularly for the pregnants and development of nausea and vomiting after returning home and compromise oral drug intake must be prevented. Many parturients might undergo operations !generally nonobstetric" during their pregnancy but most of them can not be performed on ambulatory basis. #rocedures appropriate for obstetric ambulatory surgery are those associated with postoperative care easily managed at home and with low rates of postoperative complications requiring intensive physician or nursing management. $ome of these ambulatory !or outpatient" operations or procedures are evacuation of incomplete miscarriage, surgical treatment of tubal ectopic pregnancy either performed by laparoscopically or open surgery, hysterosalpingography ! $%", hysteroscopy, cervical cerclage and assisted reproductive !A&" surgery. Genera$ )!n#iderati!n#'hatever their age, ambulatory surgery is no longer restricted to patients of A$A physical status ( or ((. #atients whose disease is well)controlled at the anesthesia consultation, even patients of A$A physical status ((( or (* who are medically stable can benefit from ambulatory procedures. #reoperative screening involves complete medical history of the patient and the family, the medications that the patient is taking, and the problems of the patient or the patient+s family may have had with previous anesthetics. This process also provides the staff to remind patient+s arrival time, suitable attire, dietary restrictions !nothing to eat or drink after midnight, no ,ewelry or make up". $taff members can determine whether a responsible person is available to escort the patient to and from the ambulatory unit-hospital and care for the patient at home after surgery. The screening is the ideal time for the anesthesiologist to talk with the patient if possible and to
review the screening record to determine whether additional evaluation by other consultant and if laboratory tests must be obtained. To decrease the risk of aspiration of gastric contents, patients are routinely asked not to eat or drink anything !non per os. /#0 or nothing by mouth" for at least 1 to 2 hours before surgery. According to A$A published practice guidelines for preoperative fasting, patients are allowed to have a light meal up to 1 hours before an elective surgery. The guidelines also support a fasting period for clear fluids of 3 hours for all patients. 4offee is not transparent but is free of particulate matter is accepted as a clear liquid. Therefore, coffee drinkers can be encouraged to drink coffee prior to their procedure because withdrawal symptoms might easily occur. #atients having chronic medications mandatory to continue preoperatively also should be encouraged to take their pills with clear liquids up to 3 hours before surgery. 'hen anesthesia requirement for ambulatory surgery or procedure arises, there are basically two considerations !general or regional". owever, factors related to the alterations in maternal physiologic condition with advancing pregnancy, teratogenic effects of anesthetic drugs, the indirect effects of anesthesia on uteroplacental blood flow, and the potential for abortion or premature delivery should be taken into account. 0f the premedicants; anticholinergics have not been found to be teratogenic, whereas tranquili5ers and sedatives such as phenotia5ines and barbiturates produce anomalies in some species. $everal reports have described a specific relationship between dia5epam and oral clefts. &egarding general anesthesia, intravenous anesthetic agents such as; thiopental, methohe6ital, and ketamine in doses normally used in the operating room have not been associated with birth defects. alogentaed inhalation agents have conflicting results. The teratogenic effect of nitrous o6ide may be related to the inhibitory effect of the agent in both maternal and fetal methionine synthetase activity and vitamine 783. Failure of this en5yme to convert homocystein to the essential amino acid methionine may lead to abnormalities of myelini5ation of nerve fibres. (nhibition of methionine synthesis results in decreased 9/A synthesis and inhibition of cell division. Therefore, it has been recommended not to administer it to pregnant women in the first two trimesters. (t is controversial whether pretreatment with folinic acid, the concentration of which is reduced when methionine synthetase inhibited, affords protection against the effects of nitrous o6ide. :ocal anesthetics have not been shown to be teratogenic in animals or humans. ;vacuation of incomplete miscarriage is a procedure that empties the uterus either by vacuum aspiration or dilatation and curettage. *acuum aspiration is a safer and quicker treatment with less pain than dilatation and curettage which is often done under general anesthesia in an operating room. #ropofol induction and remifentanil infusion have been the popular anesthetic drugs lately for both approaches. ;ctopic pregnancies can occur anywhere along the reproductive tract with the most common side being the fallopian tube. (f an ectopic pregnancy in the fallopian tube is not treated, it can cause tubal rupture and-or intraabdominal bleeding. :aparoscopic surgery under general anesthesia is feasible and less e6pensive than open surgery in the treatment of tubal ectopic pregnancy.
$% is a test frequently undertaken to find out whether fallopian tubes are open in the investigation of infertility. (t involves a dye being in,ected via the cervi6 and uterus into the fallopian tubes which enables them to be visuali5ed using an <)ray which can be painful procedure requiring analgesia. Additionally, minimal invasive operative hysteroscopy can replace laparotomic surgery in many intrauterine lesions which can be satisfactorily done under loco)regional anesthesia with paracervical block !#47" and periorificial infiltration as an alternative to general anesthesia. Transvaginal ultrasound guided oocyte retrieval !T=%0&" and laparoscopic A& procedures require anesthesia as well. 4onscious sedation or monitored anesthesia care !MA4", total intravenous anesthesia, #47, neura6ial blocks and general anesthesia have all been used successfully for T=%0&, whereas general anesthesia has been the most commonly used technique for laparoscopic A& procedure particularly because of the necessity of Trendelenburg position. For T=%0&, ben5odia5epins, ketamin and opioids !fentanyl, alfentanil, remifentanil, or meperidine" does not appear to interfere with either fertili5ation or embryo development in animals and humans. Although propofol accumulates in the follicular fluid, there have been no differences in fertili5ation, embryo cleavage or implantation rates when compared to volatile agents or #47. Thiopental is detected in follicular fluid but no adverse reproductive effects have been found compared to propofol. *olatile agents have been observed to depress 9/A synthesis and mitosis in cell cultures; regarding sevoflurane and desflurane, compound A and fluorine have been noted to have adverse effects on rapidly dividing cells. 9opaminergic antiemetic agents like droperidol and metoclopramide induce hyperprolactinemia leading to potential impairment of ovarian follicle maturation and corpus luteum function. Additional analgesia is often required when #47 is used alone. &emifentanil with its short elimination half)life and increased metabolism by blood and tissue esterases makes it a suitable agent to provide analgesia with #47 as a part of MA4. More ambulatory obstetric procedures can be e6pected in the near future, pointing out the importance of developing more adapted medical structures. RE*ERENCES 8. 7arash #%, 4ullen 7F, $toelting &>. 4linical Anesthesia, ?th ed, :ippincott 'illiams and 'ilikins, #hiladelphia, 3@@1, 88?3)882@ 3. Forna F, %ulme5oglu A. $urgical procedures to evacuate incomplete miscarriage. 4ochrane database of $ystematic &eviews 3@@A;B C. Marinangeli F, 4icco55i A, Antonucci $, (ovinelli %, 4olangeli A, *arrassi %. =se of remifenatnil in ambulatory obstetric surgery. A dose effect study. Minerva Anestesiol 8DDD; 1?!A)2". BD8)A. B. a,enius #E, Mol F, Mol 7'E, 7ossuyt #MM, Ankum 'M, *an der *een F. (nterventions for tubal ectopic pregnancy. 4ochrane database of $ystematic &eviews 3@@A;B
?. Ahmad %, 9uffy E, 'atson AE$. #ain relief in hysterosalpingography. 4ochrane database of $ystematic &eviews 3@@A;B
1. 4anni M, %allia :, Fan5ago ;, 7occi F, 7ertini =, 7arbero M. 9ay)surgery operative hysteroscopy with loco)regional anesthesia. Minerva %inecol 3@@8; ?C !?". C@A)88. A. /eilson E#. (nterventions for suspected placenta praevia. 4ochrane database of $ystematic &eviews 3@@A;B 2. Tsen :4. Anesthesia for assisted reproductive technologies. (nt Anaesthesiol 4lin 3@@A; B?. DD)88C D. %unaydin 7, >FvFlcFm 05ulgen (, 05turk ;, Tekgul G, >aya >. &emifenatnil versus remifentanil with paracervical block on plasma remifentanil concentrations and pulmonary function tests for transvaginal ultrasound guided oocyte retrieval. E 0pioid Management 3@@A; C. 31A)3A3
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Use of One-Lung Ventilation For Thoracic SurgeryDokument26 SeitenUse of One-Lung Ventilation For Thoracic SurgeryErinne DefrianiNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Perioperative Cardiovascular Evaluation For Noncardiac SurgeryDokument46 SeitenPerioperative Cardiovascular Evaluation For Noncardiac SurgeryErinne DefrianiNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Autoregulation of The Cardiovascular SystemDokument15 SeitenAutoregulation of The Cardiovascular SystemErinne DefrianiNoch keine Bewertungen
- Anesthesia For Termination of Pregnancy in Patient With Eisenmenger's SyndromeDokument26 SeitenAnesthesia For Termination of Pregnancy in Patient With Eisenmenger's SyndromeErinne Defriani100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Advanced Cardiovascular Life Support (Acls)Dokument45 SeitenAdvanced Cardiovascular Life Support (Acls)Erinne DefrianiNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- MPERSDokument1 SeiteMPERSKen ChiaNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Adult Module 1 - Five Healthy Habits Handout (English) PDFDokument2 SeitenAdult Module 1 - Five Healthy Habits Handout (English) PDFKennedy FadriquelanNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Vital Statistics: Presented by Mrs - Arockia Mary Associate ProfDokument17 SeitenVital Statistics: Presented by Mrs - Arockia Mary Associate ProfraghumscnNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- 2021 Life Skills ATP Grade 5Dokument10 Seiten2021 Life Skills ATP Grade 5Koketso SekwenyaneNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- 3 Ways To Take Isabgol - WikiHowDokument6 Seiten3 Ways To Take Isabgol - WikiHownasirNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Form 28 Attendence RegisterDokument1 SeiteForm 28 Attendence RegisterSanjeet SinghNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Form - Pelaporan B3Dokument16 SeitenForm - Pelaporan B3sukma nugraNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Online Games and Academic AchievementDokument25 SeitenOnline Games and Academic AchievementJasmine GamoraNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- AERO241 Example 10Dokument4 SeitenAERO241 Example 10Eunice CameroNoch keine Bewertungen
- Proposed Child Right's Policy FrameworkDokument2 SeitenProposed Child Right's Policy FrameworkCrisDBNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Catalogue CV. Traka Abadi UniversalDokument15 SeitenCatalogue CV. Traka Abadi UniversalHackers StevenNoch keine Bewertungen
- Chi - Square Test: PG Students: DR Amit Gujarathi DR Naresh GillDokument32 SeitenChi - Square Test: PG Students: DR Amit Gujarathi DR Naresh GillNaresh GillNoch keine Bewertungen
- AA-036322-001 - Anchor Bolt DetailsDokument1 SeiteAA-036322-001 - Anchor Bolt DetailsGaurav BedseNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- CASE DIGEST GAISANO CAGAYAN vs. INSURANCE COMPANY OF NORTH AMERICADokument3 SeitenCASE DIGEST GAISANO CAGAYAN vs. INSURANCE COMPANY OF NORTH AMERICAclaireNoch keine Bewertungen
- Manual of GardeningDokument812 SeitenManual of GardeningPrakash PatelNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- PulpectomyDokument3 SeitenPulpectomyWafa Nabilah Kamal100% (1)
- Grand Hyatt Manila In-Room Dining MenuDokument14 SeitenGrand Hyatt Manila In-Room Dining MenuMetroStaycation100% (1)
- SSP 465 12l 3 Cylinder Tdi Engine With Common Rail Fuel Injection SystemDokument56 SeitenSSP 465 12l 3 Cylinder Tdi Engine With Common Rail Fuel Injection SystemJose Ramón Orenes ClementeNoch keine Bewertungen
- Fundamental Molecular Biology: GenomesDokument45 SeitenFundamental Molecular Biology: GenomesMoonHoLeeNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- STR Mpa-MpmDokument8 SeitenSTR Mpa-MpmBANGGANoch keine Bewertungen
- Schindler 3100: Cost-Effective MRL Traction Elevator For Two-And Three-Story BuildingsDokument20 SeitenSchindler 3100: Cost-Effective MRL Traction Elevator For Two-And Three-Story BuildingsHakim BgNoch keine Bewertungen
- Frequency Inverter: User's ManualDokument117 SeitenFrequency Inverter: User's ManualCristiano SilvaNoch keine Bewertungen
- 24.2 The Core Assumptions of MindfulnessDokument9 Seiten24.2 The Core Assumptions of Mindfulnessale alvarezNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Tri-Partite Agreement AssociationDokument9 SeitenTri-Partite Agreement AssociationThiyagarjanNoch keine Bewertungen
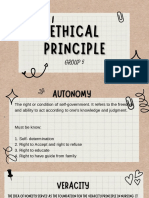
- Group 5 - Ethical PrinciplesDokument11 SeitenGroup 5 - Ethical Principlesvirgo paigeNoch keine Bewertungen
- Metallurgical Test Report: NAS Mexico SA de CV Privada Andres Guajardo No. 360 Apodaca, N.L., C.P. 66600 MexicoDokument1 SeiteMetallurgical Test Report: NAS Mexico SA de CV Privada Andres Guajardo No. 360 Apodaca, N.L., C.P. 66600 MexicoEmigdio MartinezNoch keine Bewertungen
- Biology 1st Term PaperDokument2 SeitenBiology 1st Term PapershrirahulambadkarNoch keine Bewertungen
- Astm B633Dokument5 SeitenAstm B633nisha_khan100% (1)
- Mobrey CLT PDFDokument18 SeitenMobrey CLT PDFAnonymous Oydnu9Noch keine Bewertungen
- Sol. Mock Test CBSE BiologyDokument3 SeitenSol. Mock Test CBSE BiologysbarathiNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)