Beruflich Dokumente
Kultur Dokumente
Blood Typing
Hochgeladen von
Joana Mikee RasayOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Blood Typing
Hochgeladen von
Joana Mikee RasayCopyright:
Verfügbare Formate
1. State the Landteiners principle of the ABO blood groups.
If an antigen (Ag) is present on a patients red blood cells the corresponding antibody (Ab) will not be present in the patients plasma, under normal conditions.Landsteiner, knowing that none of his subjects had been immunized, realized that natural antibodies must develop which are directed against antigens not present on the red cells. Individuals with A antigens on their red cells had sera containing Anti -B antibody. Individuals with B antigens had sera containing Anti-A. AB individuals had sera with no ABO antibodies present and O individuals sera contained Anti -A and Anti-B. Sera from group O individuals may contain a separate antibody, Anti-A,B. Anti-A,B possesses serologic activity not found in mixtures of Anti-A and AntiB. Anti-A,B sera will agglutinate A, B, and AB cells. It is particularly useful in detecting weak A and B antigens. References : http://quizlet.com/19405684/history-of-abo-import-of-karl-landsteiners-rule-flash-cards/ http://www.medialabinc.net/spg117648/the_history_of_the_abo_system_continued.aspx 2. Describe and illustrate the development of the H antigen, A antigen and B antigen. The formation of ABH antigens results from the interaction of genes at three separate loci (ABO, Hh, and Se). These genes do not actually code for the production of antigens but rather produce specific glycosyl transferases that add sugars to a basic precursor substance. A, B, and H antigens are formed from the same basic precursor material (called a paragloboside) to which sugars are attached in response to specific enzyme tranferases elicited by an inherited gene. The precursor substance on erythrocytes is referred to as type 2. This means that the terminal galactose on the precursor substance is attached to the N-acetylglucosamine in a beta 1 4 linkage .A type 1 precursor substance refers to a beta 1 3 linkage between galactose and Nacetylglucosamine. ABH antigens on the RBC are constructed on oligosaccharide chains of type 2 precursor substance. The ABH antigens develop as early as the 37th day of fetal life but do not increase much in strength during the gestational period. The RBCs of the newborn have been estimated to carry anywhere from 25 to 50 percent of the number of antigenic sites found on the adult RBC. As a result, reactions of newborn RBCs with ABO reagent antisera are frequently weaker than reactions with adult cells. The expression of A and B antigens on the RBCs is fully developed by 2 to 4 years of age and remains constant for life. As well as age, the phenotypic expression of ABH antigens may vary with race, genetic interaction, and disease states.
Reference: nd Harmening, D. (1993). Modern Blood Banking and Transfusion practices (2 Edition)
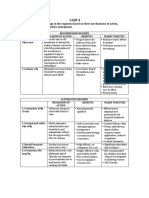
3. Where are the ABO antigens located (distribution) in the body? The ABO (H) antigens are found not only on the red cells, but also on other blood cells (endothelial cells, platelets, lymphocytes, and epithelial cells), in most body fluids (except CSF) and on the cell membranes of tissues such as intestine, urothelium and vascular endothelium. The expression of ABO(H) antigens on the red cell membrane and tissue membranes is controlled by the Hh gene. The expression of ABO(H) antigens into body fluids is controlled by Sese genes. The Sese genes, similar with Hh gene, are located ate chromosome 19q13.3; However, they are not part of the ABO system. The dominate Se gene codes for H transferase type 1 [(1,2) fucosyl-transferase; FUT2]. Without the prior addition of a fucose to the oligosaccharide chains, A and B antigens would not be expressed in the body secretions, irrespective of the presence of A and B transferases. Reference: Greer, J. Wintrobes Clinical Hematology. Volume 1. Page 636 nd Harmening, D. (1993). Modern Blood Banking and Transfusion practices (2 Edition) 4. What is the use of the anti-A, B reagent in ABO typing? Give the reactions of the normal ABO blood types, and variant groups (subgroups) in this reagent. The determination of an ABO blood group is defined by demonstrating the presence or absence of antigens A and/or B on the surface of human red blood cells and by detecting the presence or absence of anti-A and/or anti-B antibodies in the plasma. It is therefore appropriate to identify the erythrocyte antigens using known anti-A and anti-B, then to confirm the results by verifying the presence of the corresponding antibodies in the plasma from the test blood using known red blood cells A1 and B (reverse group). Additional testing of the red blood cells with Anti-A,B reagent facilitates the recognition of certain weak subgroups and is sometimes used as further confirmation of the reactions obtained with Anti-A and Anti-B reagents. Reaction of Cells Tested With Anti-A 0 + 0 + Anti-B 0 0 + + Red Cell ABO Group O A B AB Reaction of Serum Tested Against A1 Cells + 0 + 0 B Cells + + 0 0 Reverse ABO Group O A B AB
Reference: http://faculty.madisoncollege.edu/mljensen/BloodBank/lectures/abo_blood_group_system.htm http://www.fda.gov/downloads/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/LicensedPro ductsBLAs/BloodDonorScreening/BloodGroupingReagent/ucm081307.pdf 5. What is the anti-A reagent? Differentiate the reactions of A1 and A2, A1b and A2b with this reagent. Differences Reaction in anti-A Reaction in anti-A1 Cells Enzyme A1 + + 80 % of all group A (or AB) A1 gene elicits production of high concentrations of the enzyme _-3A2 + 20% of all group A (or AB)
N-acetylgalactosaminyltransferase, which converts almost all of the H precursor structure to A1 antigens on the RBCs. Number of antigen sites 810,000 to 1,170,000 sites on the 240,000 to 290,000 antigen adult RBC sites on the adult A2 RBC Immunodominant sugar N-acetyl-D-galactosamine N-acetyl-D-galactosamine Qualitative differences also exist, inasmuch as 1 to 8 percent of A2 individuals produce anti-A1 in their serum, and 22 to 35 percent of A2B individuals produce anti-A1. This antibody can cause discrepancies in ABO testing and incompatibilities in crossmatches with A1 or A1B cells. Because anti-A1 is a naturally occurring IgM cold antibody, it is unlikely to cause a transfusion reaction because it usually reacts better or only at temperatures well below 37_ C. It is to be considered clinically significant if it is reactive at 37_C. There must be some difference between the antigenic structure of A1 and A2 because, even though the same immunodominant sugar (N-acetyl-D-galactosamine) is attached by the same transferase (_-3-N-acetylgalactosaminyltransferase), A2 and A2B individuals cannot recognize the A1 antigen as being part of their own RBC makeup and are immunologically stimulated to produce a specific A1 antibody that does not cross-react with A2 RBCs. The antigens present on the RBCs of A1 and A2 individuals can be represented in two ways. It is generally presented that A1 has both the A and A1 antigen on the RBC, whereas A2 has only A antigen on its. However, to simplify the concept, one can think of A1 as having only A1 antigen sites and A2 as having only A antigen sites. Serum from group B individuals contains two antibodies, anti-A and anti-A1; therefore, this antibody mixture reacts with both A1 and A2 RBCs because both cells have the A antigen. If serum from a group B individual (which contains anti-A and anti-A1) is adsorbed with A2 cells (which contain only the A antigen), anti-A will bind to the RBC. The serum left after the cells and attached anti-A are removed by centrifugation is referred to as absorbed serum and contains anti -A1. This absorbed serum will react only with A1 antigen sites. The seed of the plant Dolichos biflorus, which serve as another source of anti-A1, is known as anti-A1 lectin. Lectins are seed extracts that agglutinate human cells with some degree of specificity. This reagent agglutinates A1 (or A1B) cells but does not agglutinate A2 (or A2B cells). Reference: nd Harmening, D. (1993). Modern Blood Banking and Transfusion practices (2 Edition)
Das könnte Ihnen auch gefallen
- Sworn Statement of Assets, Liabilities and Net WorthDokument2 SeitenSworn Statement of Assets, Liabilities and Net WorthJoana Mikee RasayNoch keine Bewertungen
- Nerve Sparing Surgery in Cervical CarcinomaDokument8 SeitenNerve Sparing Surgery in Cervical CarcinomaJoana Mikee RasayNoch keine Bewertungen
- Impetigo, Erysipela S, Cellulitis: Rasay, Joana Mikee DDokument48 SeitenImpetigo, Erysipela S, Cellulitis: Rasay, Joana Mikee DJoana Mikee RasayNoch keine Bewertungen
- DERMA2Dokument48 SeitenDERMA2Joana Mikee RasayNoch keine Bewertungen
- Major Depressive Disorder: Presented By: Justin Darrell A. SALACUPDokument15 SeitenMajor Depressive Disorder: Presented By: Justin Darrell A. SALACUPJoana Mikee Rasay100% (1)
- Basic Hematologic Tests and Erythrocytic Disorders AnemiaDokument4 SeitenBasic Hematologic Tests and Erythrocytic Disorders AnemiaJoana Mikee RasayNoch keine Bewertungen
- 2017 AHA Kawasaki DiseaseDokument74 Seiten2017 AHA Kawasaki DiseaseEdwin WijayaNoch keine Bewertungen
- Regimen Options for Scabies CaseDokument2 SeitenRegimen Options for Scabies CaseJoana Mikee RasayNoch keine Bewertungen
- Syspath 1Dokument2 SeitenSyspath 1Joana Mikee RasayNoch keine Bewertungen
- m.19 Blood Flukes - Schistosoma (Part 2) Dr. Asuncion 10-24-17Dokument2 Seitenm.19 Blood Flukes - Schistosoma (Part 2) Dr. Asuncion 10-24-17Joana Mikee RasayNoch keine Bewertungen
- HemaDokument2 SeitenHemaJoana Mikee RasayNoch keine Bewertungen
- HemaDokument2 SeitenHemaJoana Mikee RasayNoch keine Bewertungen
- Differences of Blood Service FacilityDokument2 SeitenDifferences of Blood Service FacilityJoana Mikee RasayNoch keine Bewertungen
- Histology PicturesDokument2 SeitenHistology PicturesJoana Mikee RasayNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Analysis of VariancesDokument40 SeitenAnalysis of VariancesSameer MalhotraNoch keine Bewertungen
- Hotel Design Planning and DevelopmentDokument30 SeitenHotel Design Planning and DevelopmentTio Yogatma Yudha14% (7)
- PM - Network Analysis CasesDokument20 SeitenPM - Network Analysis CasesImransk401Noch keine Bewertungen
- Malaysia Year 2011 Calendar: Translate This PageDokument3 SeitenMalaysia Year 2011 Calendar: Translate This PageStorgas FendiNoch keine Bewertungen
- Levels of Attainment.Dokument6 SeitenLevels of Attainment.rajeshbarasaraNoch keine Bewertungen
- Voltaire's Candide and the Role of Free WillDokument3 SeitenVoltaire's Candide and the Role of Free WillAngy ShoogzNoch keine Bewertungen
- R4 User GuideDokument48 SeitenR4 User GuideAaron SmithNoch keine Bewertungen
- Hydrotest CalculationDokument1 SeiteHydrotest CalculationkiranNoch keine Bewertungen
- Shimano Brakes ManualDokument36 SeitenShimano Brakes ManualKon Arva100% (1)
- Medical filter performance specificationsDokument1 SeiteMedical filter performance specificationsPT.Intidaya Dinamika SejatiNoch keine Bewertungen
- Joyful Living: (Based On Chapter 13: Advaitananda Prakaranam of Panchadashi of Sri Vidyaranya Swami)Dokument11 SeitenJoyful Living: (Based On Chapter 13: Advaitananda Prakaranam of Panchadashi of Sri Vidyaranya Swami)Raja Subramaniyan100% (1)
- January 2013 Igcse Timetable 22-06-2012Dokument2 SeitenJanuary 2013 Igcse Timetable 22-06-2012Rizwanur RahmanNoch keine Bewertungen
- Genre Worksheet 03 PDFDokument2 SeitenGenre Worksheet 03 PDFmelissaNoch keine Bewertungen
- HU675FE ManualDokument44 SeitenHU675FE ManualMar VeroNoch keine Bewertungen
- Impact of Recruitment & Selection on Employee RetentionDokument39 SeitenImpact of Recruitment & Selection on Employee RetentiongizawNoch keine Bewertungen
- ThesisDokument250 SeitenThesislax mediaNoch keine Bewertungen
- IEC-60721-3-3-2019 (Enviromental Conditions)Dokument12 SeitenIEC-60721-3-3-2019 (Enviromental Conditions)Electrical DistributionNoch keine Bewertungen
- Raychem Price ListDokument48 SeitenRaychem Price ListramshivvermaNoch keine Bewertungen
- 99 181471 - Sailor System 6000b 150w Gmdss MFHF - Ec Type Examination Module B - Uk TuvsudDokument6 Seiten99 181471 - Sailor System 6000b 150w Gmdss MFHF - Ec Type Examination Module B - Uk TuvsudPavankumar PuvvalaNoch keine Bewertungen
- Research Paper Theory of Mind 2Dokument15 SeitenResearch Paper Theory of Mind 2api-529331295Noch keine Bewertungen
- Java MCQ QuestionsDokument11 SeitenJava MCQ QuestionsPineappleNoch keine Bewertungen
- SQL 1: Basic Statements: Yufei TaoDokument24 SeitenSQL 1: Basic Statements: Yufei TaoHui Ka HoNoch keine Bewertungen
- Brooks Cole Empowerment Series Becoming An Effective Policy Advocate 7Th Edition Jansson Solutions Manual Full Chapter PDFDokument36 SeitenBrooks Cole Empowerment Series Becoming An Effective Policy Advocate 7Th Edition Jansson Solutions Manual Full Chapter PDFlois.guzman538100% (12)
- Moderntheater 170210003221 PDFDokument80 SeitenModerntheater 170210003221 PDFDycan MikeNoch keine Bewertungen
- Digital Citizenship Initiative To Better Support The 21 Century Needs of StudentsDokument3 SeitenDigital Citizenship Initiative To Better Support The 21 Century Needs of StudentsElewanya UnoguNoch keine Bewertungen
- Mechanical Questions & AnswersDokument161 SeitenMechanical Questions & AnswersTobaNoch keine Bewertungen
- EG-45-105 Material Information Sheet (Textura) V2Dokument4 SeitenEG-45-105 Material Information Sheet (Textura) V2GPRNoch keine Bewertungen
- Done by Akansha Bharti Harshitha K.N. Ishika Sunil Rajput Rashmi NaikDokument12 SeitenDone by Akansha Bharti Harshitha K.N. Ishika Sunil Rajput Rashmi NaikRamya BalanNoch keine Bewertungen
- Mama Leone's Profitability AnalysisDokument6 SeitenMama Leone's Profitability AnalysisLuc TranNoch keine Bewertungen