Beruflich Dokumente
Kultur Dokumente
Mineral
Hochgeladen von
Fetria MelaniCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Mineral
Hochgeladen von
Fetria MelaniCopyright:
Verfügbare Formate
Water Electrolytes and Micronutrients
Topic 2
Module 2.3
Metabolism of Minerals and Trace Elements
Alan Shenkin
Learning Objectives
To list the trace elements which need to be supplied to patients receiving artificial nutrition;
To know the effects of deficiency of trace elements;
To understand the reasons why patients receiving artificial nutrition may have increased
requirements;
To understand the value and limitations of methods of assessing trace element status in patients
receiving nutritional support.
Contents
1. Trace Elements- biochemical function, effects of deficiency and methods of assessment
1.1. Zinc
1.2 Copper
1.3 Iron
1.4 Selenium
1.5 Chromium
1.6 Molybdenum
1.7 Manganese
2. Trace elements in clinical nutrition
2.1 Introduction
2.2 Individuals at risk of deficiency
2.3 Clinical deficiency syndromes and sub-clinical deficiency states
2.4 Optimisation of provision of trace elements
2.5 European Union Legislation and Enteral Nutrition
2.6 Trace elements in parenteral and enteral nutrition
2.6.1 Bioavailability of trace elements in enteral nutrition
2.6.2 Overprovision of trace elements
2.6.3 Assessment and monitoring of trace element status
2.7 Pharmaceutical aspects of provision of trace elements in intravenous nutrition
2.8 Assessment and monitoring in clinical practice
Key Messages
Trace elements are an essential part of all diets, both in normal individuals and in those
requiring nutritional support;
Patients requiring intravenous nutrition should receive trace elements from the beginning of
their IV nutrition;
Requirements in disease are often greater than in health, to cope with increased metabolic
requirements and increased losses;
Optimising intake of micronutrients in nutritional support is difficult since laboratory tests are
rarely sufficiently sensitive and specific in patients with an inflammatory response.
Copyright 2008 by ESPEN LLL Programme
1. Trace Elements - biochemical function, effects of deficiency and methods of
assessment
This is a large topic and readers are referred to textbooks of nutrition (1), and to the most recent
Dietary Reference Intakes from the USA (2, 3) for a more detailed discussion.
1.1 Zinc
Zinc has three main types of functions, catalytic, structural and regulatory. Approximately 100
enzymes require zinc for their catalytic activity, especially the enzymes of protein and nucleic acid
synthesis. This accounts for the importance of zinc in growth and tissue repair. Zinc also permits the
folding of other proteins by binding to cysteine and histidine residues, forming zinc fingers. These
have extensive roles in controlling gene transcription, and in facilitating enzyme action, although
not actually catalysing the enzyme e.g. zinc copper superoxide dismutase. Zinc may also directly
affect gene expression e.g. metallothionein synthesis in the liver.
Zinc is absorbed after digestion of macronutrients in the gut. Absorption can be markedly affected
by ingestion of large amounts of other elements such as iron or copper, or by the amount of phytate
or fibre, which reduce the bioavailability. Homeostasis of body zinc is largely controlled by the
amount of zinc absorbed or secreted into the gut. Zinc is mainly transported in plasma bound to
albumin. Urine zinc is usually less than 10% of faecal zinc, unless there is increased muscle protein
catabolism.
Deficiency of zinc is well characterised. Reduced growth in children is an early sign. Severe zinc
deficiency gives rise to alopecia, diarrhoea, delayed sexual maturation, and eczematous skin rash
especially on the face and in body flexures, and impaired appetite. There are also important effects
on immune function.
The most widely used marker of zinc status is plasma zinc concentration which correlates
reasonably well with intake, provided there is no inflammatory response. However, in a hospital
population, surgery, infection, or other inflammatory disease cause an acute fall in plasma zinc.
Changes in plasma zinc concentration must therefore be interpreted together with changes in the
binding protein, albumin, and also changes in the acute phase response, possibly by measuring C-
reactive protein at the same time. Other methods of assessing zinc such as the zinc concentration in
erythrocytes has not proved useful, whereas zinc in hair is too susceptible to methodological
variation. Enzyme activity has also not proved sufficiently specific. Organ failure does not lead to
significant changes in zinc requirement, with the exception of major burns where exudative losses
of zinc can be substantial.
1.2 Copper
Copper has primarily a catalytic role for certain metalloenzymes which act as oxidases. For
example, cytochrome C oxidase is especially important in energy metabolism, lysyl oxidase
produces cross-linkages in collagen and elastin, and ferroxidase oxidises iron to bind to transferrin
for circulation in the plasma and delivery to the tissues.
Copper homeostasis is controlled by modulation of copper absorption from the small intestine and
its excretion in the bile. Urinary losses are very low. Copper is transported in plasma bound to
caeruloplasmin, which participates in tissue iron release.
Deficiency of copper is rare, but it has been observed in TPN and causes normocytic hypochromic
anaemia, neutropenia and skeletal disturbances.
The best markers of copper status are plasma copper or caeruloplasmin, although the acute phase
response will cause an increase due to increased caeruloplasmin synthesis. Concentrations also
increase in pregnancy and with the oral contraceptive pill. Erythrocyte superoxide dismutase may
be helpful, although it can be elevated in situations of oxidative stress.
1.3 Iron
The main function of iron is for oxygen transport within haemoglobin, although a substantial amount
is also required for myoglobin function in skeletal muscle.
Copyright 2008 by ESPEN LLL Programme
Iron status is largely maintained by regulation of absorption in the upper small bowel. Haem iron is
absorbed separately and more efficiently than non-haem iron, which is improved by reducing agents
such as vitamin C, which also form chelates with iron.
Mucosal cells regulate the amount of iron absorbed, which is then carried by transferrin to the
tissues where uptake is controlled by expression of a membrane bound receptor for transferrin. Iron
is stored in the liver and bone marrow in the form of ferritin.
The signs of iron deficiency become progressively severe, with microcytic hypochromic anaemia,
impaired physical activity and endurance in adults and cognitive impairment in children.
There are many laboratory tests for iron status. Serum iron and iron binding capacity (transferrin)
are widely used, but the concentrations of both of these are markedly reduced by the acute phase
response. Serum ferritin is usually the best marker of iron status, but it is increased in the presence
of an acute phase response. Soluble serum transferrin receptor increases in iron deficiency and it
may be the best marker in inflammatory diseases, but it is not yet in widespread use.
Iron status is not directly affected by severe illness. There is however concern that excess iron
provision may exacerbate certain bacterial infections, possibly by providing iron as a substrate for
the microorganisms, and hence iron provision must be very cautious in such patients.
1.4 Selenium
Selenium functions through its presence in selenocysteine, which is incorporated into a number of
proteins, selenoproteins. The functions of these are not fully elucidated but glutathione peroxidases
are essential defence agents against oxidative stress, and iodothyronine deiodinases are central for
thyroid hormone metabolism.
Absorption of selenium from the diet is very efficient much is in the form of selenomethionine, a
plant amino acid, or selenocysteine. Commercial selenium supplements in the form of selenite or
selanate are well absorbed. All selenium species in the diet will eventually all be converted to
selenophosphate, which is the precursor of selenocysteine. Excess selenium is excreted in the urine.
Inadequate selenium intake gives rise to a wide spectrum of diseases. Keshan disease is a
cardiomyopathy of children in China and Kashin-Beck disease of cartilage in adolescents were the
main syndromes from which the deficiency was first identified. In clinical nutrition, skeletal and
cardiomyopathy have both been observed.
It seems likely that selenium deficiency alone does not cause obvious illness unless some other
stimulus, such as a viral infection, is also present.
Assessment of selenium status is most frequently by use of plasma selenium, although plasma or
erythrocyte glutathione peroxidase measurements are also widely used. Plasma selenium is affected
by an acute phase response, but not as markedly as zinc or iron. Organ failure is not considered to
have too much effect on selenium metabolism, although severe burns are associated with marked
losses.
1.5 Chromium
Chromium increases the action of insulin, possibly through amplifying insulin receptor tyrosine
kinase activity. This may lead to an improvement in glucose tolerance in some individuals.
Chromium is absorbed largely in the form of chromium
3+
. Homeostasis is mainly by altering the
excretion in the urine.
A very small number of cases of chromium deficiency have been observed during TPN. They had
weight loss, glucose intolerance, and peripheral neuropathy, which responded to chromium
provision. Sub-clinical deficiency may lead to impaired glucose tolerance in type II diabetes, but
further evidence is still needed regarding the significance of this.
Copyright 2008 by ESPEN LLL Programme
Assessment of chromium status is extremely difficult due to the very low plasma concentrations and
the difficulty in obtaining non-contaminated specimens. However plasma concentration may help in
specialised laboratories. The best assessment may be the response of glucose and insulin to
chromium supplements. Organ failure is not known to cause major effects on metabolism.
1.6 Molybdenum
Molybdenum is a co-factor for several oxidiser enzymes, especially sulphite oxidase and xanthine
oxidase. These are of special importance in disposal of sulphite which otherwise causes neurological
damage, and in catabolism of purines.
Deficiency of molybdenum is generally a genetic disorder. Nutritional deficiency has only been
reported in one patient who developed tachycardia, headache and night blindness, which were
corrected by molybdenum supplements.
Assessment is rarely done. Plasma concentration is very low and difficult to measure. The best
markers are metabolic, molybdenum deficiency being linked to low serum urate, low urine sulphate
and elevated urine xanthine and hypoxanthine. Since the primary route of excretion is the urine,
renal failure will be associated with molybdenum retention and the risk of toxicity.
1.7 Manganese
Manganese metalloenzymes are involved in amino acid, cholesterol and carbohydrate metabolism.
Glycosyl and xylosyl transferases are important in proteoglycan synthesis, which is required for bone
formation.
Dietary manganese is poorly absorbed (less than 5%). It is transported in the blood bound to
transferrin and albumin. Excretion is via the bile to the faeces, with little excretion in urine.
Manganese deficiency is extremely rare, and only under experimental conditions have signs of a
scaly rash and low plasma cholesterol been observed.
The best estimates of manganese status are from whole blood manganese since this is less affected
by haemolysis or contamination during collection. Plasma manganese may be helpful but collection
of suitable specimens is critically important. Cholestatic liver damage leads to manganese
accumulation, and this may reach toxic levels with subsequent accumulation in central nervous
tissue and extrapyramideal syndrome. Many preparations of trace elements for TPN have contained
excessive amounts of manganese, leading to toxicity, so monitoring is important, especially in long-
term provision.
Trace elements are essential inorganic micronutrients, which are required in the diet in very small
amounts but nonetheless they are critical both for maintenance of health and treatment of disease.
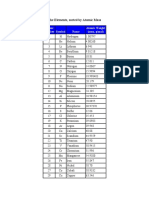
The function of trace elements and effect of their deficiencies are summarised in Table 1. A more
complete account can be found in various textbooks of nutrition (1, 4).
Table 1 Trace elements - Functions, biochemical model of action, effects of
deficiency and methods of assessment (6)
Function(s)
Biochemical modes
of action
Effects of
deficiency
Assessment of
status
Comments
Z
i
n
c
Protein
synthesis
Control of diffe-
rentiation
Enzyme cofactor
"Zinc
fingers" in DNA
Growth
Hair loss
Skin rash
Immune function.
Plasma zinc
- with albumin
and C-reactive
protein
Plasma Zn falls
in acute phase
reaction
I
r
o
n
O
2
transport
Electron
transport
Haem/myoglobin
Cytochromes
Hypochromic
anaemia Possibly
increased resistance
to infection
Serum iron/ IBC
Serum ferritin
with CRP
Blood Hb
and film
Serum Fe falls
and ferritin
increases in
APR
- care needed
not to exceed
IBC
Copyright 2008 by ESPEN LLL Programme
C
o
p
p
e
r
Collagen/elastin
synthesis
Antioxidant
Lysyl oxidase
Zn/Cu superoxide
dismutase
Caeruloplasmin
Subperiosteal
bleeding Cardiac
arrhythmia Anaemia
Neutropenia
Plasma copper
or
caeruloplasmin
with CRP
Plasma Cu
increases in
acute phase
reaction
S
e
l
e
n
i
u
m
Antioxidant
Thyroid function
Immune
function
Glutathione
peroxidase
Tyrosine deiodinase
T lymphocyte
receptor expression
Cardiomyopathy
Skeletal myopathy
Nail abnormalities
Macrocytosis
Neoplastic risk
Plasma Se
RBC glutathione
peroxidase
Urine Se
Whole blood Se
Platelet
glutathione
peroxidase
Se depletion
may be
asymptomatic
M
a
n
g
a
n
e
s
e
Not clear
Some
antioxidant
Enzyme cofactor
Mitochondrial
superoxide
dismutase
Cholesterol
Red blood cells
Possibly
mucopolysaccha-
ride abnormalities
Whole blood Mn Deficiency
state not
confirmed in
man
C
h
r
o
m
i
u
m
Carbohydrate
metabolism
Insulin activity
Lipoprotein
metabolism
Gene expression
Glucose intolerance
Weight loss
Peripheral
neuropathy
Plasma Cr Contamination
free blood
sampling
required
Cr is present as
a contaminant
of most TPN
solutions
M
o
l
y
b
d
e
n
u
m
Amino acid
metabolism
Purine
metabolism
Sulphite oxidase
Xanthine oxidase
Intolerance to
S amino acids:
- tachycardia
- visual upset
Urinary
hypoxanthine
sulphite
Rarely
measured
I
o
d
i
n
e
Energy
metabolism
Thyroid hormones Hypothyroidism Serum T
4
T
3
TSH
F
l
u
o
r
i
d
e
Bone/tooth
mineralization
Calcium fluorapatite Dental caries Urine excretion Provision in
nutritional
support is
controversial
2. Trace elements in clinical nutrition
2.1 Introduction
The provision of an adequate amount of trace elements is an integral part of all nutrition support
regimens by both parenteral and enteral routes.
2.2 Individuals at risk of deficiency
By the time a patient commences nutritional support, he/she may already have developed a whole
body depletion of one or more essential nutrients. The extent of this will depend on a number of
factors:
The nutritional state of the patient on admission to hospital. The pre-existing illness may have
caused a period of anorexia, or inadequate digestion or absorption of nutrients;
The duration and severity of inadequate nutritional intake whilst in hospital, as a result of
surgery or other treatment;
Copyright 2008 by ESPEN LLL Programme
Any increased losses through small bowel fistula/aspirate (rich in zinc), biliary fluid (rich in
copper) burn exudate fluid (rich in zinc/copper/selenium), or dialysate (rich in water soluble
nutrients);
Moreover, some individuals will have an increased daily requirement, partly to keep up with
increased losses, and partly to meet metabolic requirements these are particularly important
when patients become anabolic after a period of catabolism or when normal growth resumes in
a child.
Identification of potential micronutrient deficiencies should be part of the nutritional assessment of
every patient, since conditions such as alcoholism, coeliac disease, inflammatory bowel disease,
etc., predispose to such deficiencies. Students should make themselves familiar with the more
common associations found in medical and surgical practice and be alert to their occurrence.
2.3 Clinical deficiency syndromes and sub-clinical deficiency states
Classical nutritional deficiency usually results in a complex syndrome of typical signs and
symptoms, and these have now been fully characterized for each of the vitamins and trace
elements. These syndromes were the basis on which the essential micronutrients were initially
identified, and there is now a reasonable understanding of the nutritional consequences of severe
deficiency, and the intake necessary to prevent clinically obvious deficiency from developing.
It is, however, now clear that as an individual develops progressively more severe depletion of one
or more micronutrients, he/she will pass through a series of stages with biochemical or physiological
consequences. The metabolic or physiological penalty of such a sub-optimal nutritional status is
usually not clear, but the assumption remains that this impaired metabolism is likely to result in
detrimental effects. Similarly, specific and localized tissue deficiencies can occur which can lead to
pathological changes. Such situations can be defined as sub-clinical deficiency. The time course for
development of a sub-clinical deficiency state varies for each individual micronutrient, and depends
upon the nature and amount of tissue or body stores. The consequences of an inadequate intake are
more clearly delineated in Figure 1.
Figure 1 Consequences of inadequate micronutrient intake
A sub-clinical deficiency state can be either absolute or relative. Thus an intake less than the
requirement in normal health will lead to sub-clinical deficiency, or to a typical clinical deficiency
state. However, certain patients have significantly increased requirements as a result of their
Copyright 2008 by ESPEN LLL Programme
disease process, and hence an intake normally regarded as adequate may be relatively insufficient
and lead to a sub-clinical deficiency state. Most of the recommendations for vitamin and trace
element supplements in TPN, and the content in enteral feeds, include an allowance for an
increased requirement in disease.
2.4 Optimisation of provision of trace elements
Defining the optimal intake of micronutrients is far from ideal. It is possible to make a reasonable
assessment of the requirements of an individual, based upon the requirements in health, the likely
underlying nutritional state of the patient at the time of presentation, and the ongoing effects of
the disease process. Such a level of provision using the enteral feeds and intravenous additives,
which are currently commercially available, has been proved to be adequate in most cases to
prevent the development of a deficiency state. However, provision of micronutrients to ensure the
best possible tissue function remains poorly defined. Possible methods of trying to optimise
provision in relation to function can be considered with respect to the antioxidant system, and also
to the immune system.
It is to be expected that in the next few years, well controlled clinical trials will help to clarify the
situations where increased provision of these micronutrients is or is not helpful, both in reducing
the biochemical effects of reactive oxidant species (ROS), and also in altering complication rates
and outcome in serious illness. Many of the disease states thought to be associated with ROS are
chronic degenerative conditions, such as atherosclerosis and neoplastic disease. The increasing
number of patients dependent on life-long TPN makes the long-term provision of adequate amounts
of micronutrients an important part of nutritional therapy.
2.5 European Union Legislation and Enteral Nutrition
The European Union has issued a directive on Dietary Foods for Special Medical Purposes (FSMPS).
This includes guidelines on vitamin and trace element content. In many cases, the minimum intake
suggested for an individual with an energy intake of 2000 kcals is in excess of the reference intake
in a normal population. This allows for the increased requirement of most individuals receiving
enteral nutrition. The directive defines FSMPs as:
nutritionally complete standard formula which can be used as a sole source of nutrition
these must comply with the guidelines for micronutrient composition, as shown in Table 3 and
Table 4;
nutritionally complete, nutrient adapted disease specific formula which also must be
suitable as a sole source of nutrition;
nutritionally incomplete formulas which are not suitable as a sole source of nutrition.
Selection of the most appropriate tube feed often requires assistance from an experienced
dietician. Students should be aware that although the micronutrient composition must lie within the
ranges quoted, these are wide and they have been designed for a 2000 Kcal intake, which is rarely
achieved enterally. Different commercial products can have quite different amounts of
micronutrients. 1500 kcals of feed is an intake, which is more widely met in clinical practice. The
range of amounts present in this amount of feeds, which are currently available in Europe, is
therefore also shown as a guide in Table 2.
2.6 Trace elements in parenteral and enteral nutrition
Many of the trace elements now recognized as being essential for human nutrition have been better
characterized as a result of studies in patients who were depending totally upon their intravenous
intake during total parenteral nutrition (TPN), especially for prolonged periods.
The key features of an essential trace element are that its removal or inadequate supply in the diet
is associated with reproducible structural or biochemical changes, and that these are reversible on
provision of the element. This has been convincingly demonstrated in TPN for zinc, copper,
selenium, iron, molybdenum, and chromium. In addition, there is good evidence of biochemical
essentiality of iodine and of manganese, and the nutritional benefits of fluoride on bones and teeth.
Cobalt is also recognized as being essential, although all requirements seem to be met by supply of
vitamin B
12
alone.
Copyright 2008 by ESPEN LLL Programme
A summary of suggested intravenous and enteral intakes of trace elements in nutritional support is
provided in Table 2 It is important to note the significant difference between intakes by the
intravenous and enteral routes, which are largely due to the efficiency of absorption from the gut.
Table 2 Trace Elements in parenteral and enteral nutrition
- Fresenius-Kabi
- Baxter Health Care
- Various commercially available standard feeds
IV Supplement Enteral Nutrition
EC Directive
Units Additrace (1) Decan (2)
Minimum Maximum
Approximate
amount (3) in
feed providing
1500 kcal
mg 6.5 10.0 10 30 15-23
Zinc
mmol 100 153 153 459 230-353
mg 1.3 0.48 1.2 10 2-3
Copper
mmol 20 7.6 19 157 31-46
mg 1.2 1.0 10 40 20-30
Iron
mmol 20 17.9 179 714 358-537
mg 0.3 0.2 1 10 3-6
Manganese
mmol 5 3.6 18 180 54-108
mg 30 70 50 200 70-112
Selenium
mmol 0.4 0.89 0.63 2.5 0.89-1.4
mg 10 15 25 300 100-150
Chromium
mmol 0.2 0.29 0.48 5.8 1.9-2.8
mg 19 25 70 360 150-225
Molybdenum
mmol 0.2 0.26 0.73 3.75 1.6-2.4
mg 131 1.5 130 700 150-300
Iodide
mmol 1 0.012 1 5.3 1.2-2.4
mg 0.95 1.45 0 4 0-3
Fluoride
mmol 50 76 0 210 0-156
2.6.1 Bioavailability of trace elements in enteral nutrition
The bioavailability of micronutrients is the efficiency with which each micronutrient is used in the
body. It depends on absorption from the gut and utilization by the tissues. Gut factors are
considered to be of most importance and depend on:
Dietary composition e.g. the chemical form of a nutrient (iron in heme, selenium in
selenomethionine); the presence of antagonistic ligands (e.g. phytate, fibre); and competitive
interactions (e.g. iron, zinc and copper can compete for absorption);
Luminal /mucosal factors;
Redox state, dietary hydrolysis, and binding to amino acids or carrier proteins may all modify
absorption.
2.6.2 Overprovision of trace elements
Excess trace elements may be provided inadvertently as contaminants of other nutrients - in TPN
e.g. Al in Ca/P supplements, Cr in amino acids. Some older commercial trace element supplements
contain excess manganese (> 5 mol/d), which has been shown to be related to a toxicity condition
in some patients after long-term use.
2.6.3 Assessment and monitoring of trace element status
An accurate assessment of trace element status during nutritional support is difficult, especially in
seriously ill patients (5). Some guidelines are:
Tests of plasma concentration are a poor reflection of tissue status;
Plasma concentration of Zn, Fe, Se all falls during an acute phase response (APR), whereas Cu
increases (see Fig. 2);
Plasma concentration may be of value in stable patients without an active APR;
For some elements, measurement of enzyme activity may be helpful e.g. red blood cell or
plasma glutathione peroxidase as a marker of selenium status;
Copyright 2008 by ESPEN LLL Programme
Plasma concentration may be helpful in identifying over-provision.
2.7 Pharmaceutical aspects of provision of trace elements in intravenous
nutrition
Care must be taken to minimize interactions between nutrients, or between individual
micronutrients and the infusion bags or giving sets. Instability caused by trace elements is unusual,
although thee are limitations to the amount of inorganic iron which is stable in infusion mixtures.
Chemical interaction with trace elements, especially the oxidative effect of copper on vitamin C is
minimized by addition immediately before infusion.
2.8 Assessment and monitoring in clinical practice
Some tests commonly used to assess trace elements are included in Table 1. The acute phase
reaction associated with trauma and infection markedly affects plasma concentration of many trace
elements (Fig. 2).
Variation in Plasma Trace Elements after Surgery
0. 0
4. 0
8. 0
12. 0
16. 0
20. 0
24. 0
0 12 24 36 48 6 0 72 84 9 6
Ti me (hrs )
C
o
n
c
(
u
m
o
l
/
l
)
Copper
Iron
Zinc
Figure 2 Changes in plasma iron, zinc and copper after elective surgery.
Similar changes occur after any acute trauma, infection or inflammation
Because of the limitations in interpretation of these data, it is common practice, especially in
patients receiving TPN, only to assess on a regular basis the status of zinc, copper, selenium (mainly
in long-term nutritional problems) and iron. The other laboratory tests which are available to assess
micronutrients are usually only used when there is a particular clinical problem where confirmation
of micronutrient deficiency or excess is necessary. If such tests are not available, and a deficiency
is suspected, a therapeutic trial of increased intake can usually be safely given if renal function and
liver function are satisfactory. In patients receiving enteral nutrition or TPN where some intestinal
absorptive capacity may still be present, an oral or enteral multi-mineral supplement may also be
provided.
A two-week course of a well balanced micronutrient supplement is unlikely to cause any harm, and
may occasionally be beneficial. Alternatively, an increase in intravenous supply can be given for a
limited period, with careful clinical monitoring. In such cases a blood/plasma sample at the
beginning of supplementation should be stored for possible analysis at a later date.
Copyright 2008 by ESPEN LLL Programme
3. Summary
Trace elements are an essential part of all diets and should be given in full daily amounts with all
forms of artificial nutrition. Requirements in disease, although difficult to quantify, are often
greater than those in health. In some conditions, e.g. burns or small bowel fistulae, losses may be
greatly in excess of normal and, in those who are likely to be already depleted an initial catch up
replacement dose may be required. Although major deficiencies give rise to characteristic
syndromes, it is possible that subclinical deficiencies, single or multiple, may affect clinical
outcome adversely although more evidence is needed before this is established. Optimising intake
of trace elements and minerals in patients undergoing nutritional support is difficult since
laboratory tests often lack sensitivity and specificity in the presence of inflammation e.g. effects on
Zn, Fe, and Cu blood levels. As a practical policy, therefore, it is wise to give at least the RDI, with
additions to counteract any prior deficit, to meet continuing losses, and to meet the metabolic
demands of the response to disease and injury.
References
1. Shils ME, Olson JA, Shike M, Ross AC. Modern Nutrition in Health and Disease. 9th ed. Baltimore:
Williams and Wilkins; 1999.
2. Food and Nutrition Board IoM. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium,
and Carotenoids. Washington, DC: National Academy Press; 2000.
3. Food and Nutrition Board IoM. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic,
Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium,
and Zinc. Washington, DC: National Academy Press; 2002.
4. O'Dell BL, Sunde RA. Handbook of Nutritionally Essential Mineral Elements. New York, Basel,
Hong Kong: Marcel Dekker; 1997.
5. Shenkin A. Micronutrients in the severely-injured patient. Proc Nutr Soc 2000; 59(3):451-456.
6. Shenkin A. Adult micronutrient requirements. In: Payne-James J, Grimble G, Silk D, editors.
Artificial Nutrition Support in Clinical Practice. 2nd ed. London: GMM; 2001. 193-212.
Copyright 2008 by ESPEN LLL Programme
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Duplex & Super Duplex InformationDokument7 SeitenDuplex & Super Duplex InformationrajeshNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Asme Section IxDokument260 SeitenAsme Section IxHassan Aziz100% (3)
- Creusabro 4800Dokument8 SeitenCreusabro 4800ravigurajapuNoch keine Bewertungen
- Material Identification NumbersDokument2 SeitenMaterial Identification Numbersrajatapc12007Noch keine Bewertungen
- Duplex Stainless SteelDokument24 SeitenDuplex Stainless SteeljeffreymacaseroNoch keine Bewertungen
- 0803134592Dokument278 Seiten0803134592bebopbee100% (2)
- Design Guidelines For The Selection and Use of Stainless SteelDokument15 SeitenDesign Guidelines For The Selection and Use of Stainless Steelnarasimha2140% (1)
- Steel Heat Treatment Handboook-Metalluurgy and TechnologiesDokument850 SeitenSteel Heat Treatment Handboook-Metalluurgy and Technologiesmusiomi200596% (23)
- SSC 6MO Steel Spec SheetDokument2 SeitenSSC 6MO Steel Spec SheetDouglas BooyensNoch keine Bewertungen
- Inconel 718 Alloy 718 Uns n07718 Din 2.4668Dokument3 SeitenInconel 718 Alloy 718 Uns n07718 Din 2.4668SamkitNoch keine Bewertungen
- Malnutrition in Stroke PatientDokument8 SeitenMalnutrition in Stroke PatientFetria MelaniNoch keine Bewertungen
- 2 Semestre Acid TodayDokument44 Seiten2 Semestre Acid Todayrubens_marcos0% (1)
- Screening Damage Mechanism - 581 & 571Dokument28 SeitenScreening Damage Mechanism - 581 & 571Febri Ramdani NugrahaNoch keine Bewertungen
- Nutrition For AdultDokument60 SeitenNutrition For AdultFetria MelaniNoch keine Bewertungen
- SP-2041 2014Dokument19 SeitenSP-2041 2014wawanNoch keine Bewertungen
- Olahraga Kekuatan OtotDokument8 SeitenOlahraga Kekuatan OtotFetria MelaniNoch keine Bewertungen
- StrokeDokument2 SeitenStrokeFetria MelaniNoch keine Bewertungen
- Kolesterol 123Dokument7 SeitenKolesterol 123Fetria MelaniNoch keine Bewertungen
- AntioxidantDokument22 SeitenAntioxidantFetria MelaniNoch keine Bewertungen
- Cerebral Blood FlowDokument37 SeitenCerebral Blood FlowFetria MelaniNoch keine Bewertungen
- Dash Diet PamphletDokument64 SeitenDash Diet PamphletbohnjucurNoch keine Bewertungen
- Antioxidants and Stress Tolerance 2010Dokument22 SeitenAntioxidants and Stress Tolerance 2010AKICA023Noch keine Bewertungen
- Stroke Imaging AlgorithmDokument8 SeitenStroke Imaging AlgorithmFetria MelaniNoch keine Bewertungen
- Stroke PatofDokument22 SeitenStroke PatofderiNoch keine Bewertungen
- Dysphagia Nutrition Hydration in Stroke 2012Dokument8 SeitenDysphagia Nutrition Hydration in Stroke 2012Fetria MelaniNoch keine Bewertungen
- Muscle Atrophy DialysisDokument8 SeitenMuscle Atrophy DialysisFetria MelaniNoch keine Bewertungen
- Fisiologi Kulit MenuaDokument1 SeiteFisiologi Kulit MenuaFetria MelaniNoch keine Bewertungen
- Living With Uc Brochure FinalDokument19 SeitenLiving With Uc Brochure FinalJon Wafa AzwarNoch keine Bewertungen
- Mna Short FormDokument1 SeiteMna Short FormFetria MelaniNoch keine Bewertungen
- DehydrationDokument10 SeitenDehydrationEko SetiawanNoch keine Bewertungen
- Patient EducationDokument18 SeitenPatient EducationFetria MelaniNoch keine Bewertungen
- Immunity and Aging1742-4933!5!15Dokument10 SeitenImmunity and Aging1742-4933!5!15Fetria MelaniNoch keine Bewertungen
- BUN Creatinin RatioDokument5 SeitenBUN Creatinin RatioFetria MelaniNoch keine Bewertungen
- The Anatomy of A Great Poster: Richard Gerkin, M.D. Bridget Stiegler, D.ODokument31 SeitenThe Anatomy of A Great Poster: Richard Gerkin, M.D. Bridget Stiegler, D.OFetria MelaniNoch keine Bewertungen
- Clinical NutritionDokument7 SeitenClinical NutritionFetria MelaniNoch keine Bewertungen
- Clinical Ass Unstable HemidynamicDokument9 SeitenClinical Ass Unstable HemidynamicFetria MelaniNoch keine Bewertungen
- Algorithm Pyloric StenosisDokument15 SeitenAlgorithm Pyloric StenosisFetria MelaniNoch keine Bewertungen
- Full Liquid DietDokument1 SeiteFull Liquid DietFetria MelaniNoch keine Bewertungen
- Nutrisi Ulseratif KolitisDokument1 SeiteNutrisi Ulseratif KolitisFetria MelaniNoch keine Bewertungen
- FitokimiaDokument0 SeitenFitokimiaFetria MelaniNoch keine Bewertungen
- Klasifikasi WagnerDokument8 SeitenKlasifikasi WagnerNina AmeliaNoch keine Bewertungen
- Modul 0 Introduction To Clinical Nutrition PDFDokument7 SeitenModul 0 Introduction To Clinical Nutrition PDFEko SetiawanNoch keine Bewertungen
- Clear Liquid DietDokument3 SeitenClear Liquid DietFetria Melani100% (1)
- MTJ FabricationDokument1 SeiteMTJ FabricationRobertNoch keine Bewertungen
- High Temperature SteelDokument5 SeitenHigh Temperature Steelsathyadevi konnurNoch keine Bewertungen
- SmawDokument56 SeitenSmawFakhar WindratamaNoch keine Bewertungen
- Li!IllDokument11 SeitenLi!IllHira FiazNoch keine Bewertungen
- Equivalent Valve Forged Cast PDFDokument2 SeitenEquivalent Valve Forged Cast PDFAlessandro Marcio LiraNoch keine Bewertungen
- The ElementsDokument4 SeitenThe ElementsHaider AliNoch keine Bewertungen
- Atboic VII III CR PDFDokument416 SeitenAtboic VII III CR PDFKashilal IndraNoch keine Bewertungen
- Precipitation of Molybdenum (V) As The Hydroxide AND Its Separation From RheniumDokument3 SeitenPrecipitation of Molybdenum (V) As The Hydroxide AND Its Separation From RheniumBrent WoottonNoch keine Bewertungen
- Wire BrochureandBulletinsDokument204 SeitenWire BrochureandBulletinsarturoNoch keine Bewertungen
- Feasibility Study Part - II Fission Mo-99 Production by The Irradiation of A LEU Metallic Uranium Foil at Tajoura Research ReactorDokument5 SeitenFeasibility Study Part - II Fission Mo-99 Production by The Irradiation of A LEU Metallic Uranium Foil at Tajoura Research Reactorbsebsu7901Noch keine Bewertungen
- Thermowell CatalogDokument24 SeitenThermowell CatalogMANTCRUZNoch keine Bewertungen
- Understanding Internal Defects in Mo Fabricated by Wire Arc Additive Manufacturing Through 3D Computed TomographyDokument10 SeitenUnderstanding Internal Defects in Mo Fabricated by Wire Arc Additive Manufacturing Through 3D Computed TomographySaketh BachuNoch keine Bewertungen
- A270 - Sanitary Stainless Steel TubingDokument2 SeitenA270 - Sanitary Stainless Steel TubingfitiranNoch keine Bewertungen
- Lehr Belt Catalogue PDFDokument7 SeitenLehr Belt Catalogue PDFshivam_dubey4004Noch keine Bewertungen
- ACT词汇与长难句 新Dokument313 SeitenACT词汇与长难句 新jessicalvgiahmisNoch keine Bewertungen
- 7 - MSP REFRAM Molybdenum Production SotA - G. Ye PDFDokument19 Seiten7 - MSP REFRAM Molybdenum Production SotA - G. Ye PDFJo An MeMeNoch keine Bewertungen
- Is 228 - 20Dokument6 SeitenIs 228 - 20Nav TalukdarNoch keine Bewertungen