Beruflich Dokumente
Kultur Dokumente
Pediatricreferencecard 04
Hochgeladen von
yesumovsOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pediatricreferencecard 04
Hochgeladen von
yesumovsCopyright:
Verfügbare Formate
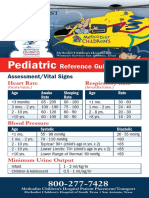
PEDIATRIC ASSESSMENT
General Impression
(First view of patient)
Airway & Appearance (Open/Clear Muscle Tone /Body Position)
Abnormal: Abnormal or absent cry or speech. Decreased response to parents or environmental stimuli. Floppy or rigid muscle tone or not moving. Normal: Normal cry or speech. Responds to parents or to environmental stimuli such as lights, keys, or toys. Good muscle tone. Moves extremities well.
Work of Breathing (Visible movement / Respiratory Effort)
Abnormal: Increased/excessive (nasal flaring, retractions or abdominal muscle use) or decreased/absent respiratory effort or noisy breathing. Normal: Breathing appears regular without excessive respiratory muscle effort or audible respiratory sounds.
Circulation to Skin (Color / Obvious Bleeding)
Abnormal: Cyanosis, mottling, paleness/pallor or obvious significant bleeding. Normal: Color appears normal for racial group of child. No significant bleeding. Decision/Action Points: Any abnormal findings or life-threatening chief complaint such as major trauma/burns, seizures, diabetes, asthma attack, airway obstruction, etc (urgent) proceed to Initial Assessment. Contact ALS if ALS not already on scene/enroute. All findings normal (non-urgent) proceed to Initial Assessment.
Initial Assessment
(Primary Survey)
Airway & Appearance (Open/Clear Mental Status)
Abnormal: Obstruction to airflow. Gurgling, stridor or noisy breathing. Verbal, Pain, or Unresponsive on AVPU scale. Normal: Clear and maintainable. Alert on AVPU scale.
Continue assessment throughout transport
Breathing (Effort / Sounds / Rate / Central Color)
Abnormal: Presence of retractions, nasal flaring, stridor, wheezes, grunting, gasping or gurgling. Respiratory rate outside normal range. Central cyanosis. Normal: Easy, quiet respirations. Respiratory rate within normal range. No central cyanosis.
Circulation (Pulse Rate & Strength / Extremity Color & Temperature / Capillary Refill / Blood Pressure)
Abnormal: Cyanosis, mottling, or pallor. Absent or weak peripheral or central pulses; Pulse or systolic BP outside normal range; Capillary refill > 2 sec with other abnormal findings. Normal: Color normal. Capillary refill at palms, soles, forehead or central body 2 sec. Strong peripheral and central pulses with regular rhythm. Decision/ Action Points: Any abnormal finding (C, U, or P) Immediate transport with ALS. If ALS is not immediately available, meet ALS intercept enroute to hospital or proceed to hospital if closer. Open airway & provide O2. Assist ventilations, start CPR, suction, or control bleeding as appropriate. Check for causes such as diabetes, poisoning, trauma, seizure, etc. Assist patient with prescribed bronchodilators or epinephrine auto-injector, if appropriate. All findings on assessment of child normal (S) Continue assessment, detailed history & treatment at scene or enroute. Normal Respiratory Rate: Infant (<1yr): 30- 60 Toddler (1-3yr): 24 -40 Preschooler(4-5yr): 22- 34 School-age(6-12yr): 18 -30 Adolescent(13-18yr): 12 -20 Normal Pulse Rate: Infant: 100-160 Toddler: 90-150 Preschooler: 80-140 School-age: 70-120 Adolescent: 60-100 Pulses slower in sleeping child / athlete Lower Limit of Normal Systolic BP: Infant: >60 (or strong pulses) Toddler: >70 (or strong pulses) Preschooler: >75 School-age: >80 .Adolescent: >90 Estimated min.SBP >70 + (2 x age in yr)
This reference card should not be considered to replace or supercede regional prehospital medical treatment protocols.
Supported in part by project grant #6 H33 MC 00036 from the Emergency Services for Children program, HRSA, USDHHS in cooperation with NHTSA Rev. 1/04
Pediatric CUPS (with examples)
Critical Absent airway, breathing or circulation (cardiac or respiratory arrest or severe traumatic injury) Compromised airway, breathing or circulation (unresponsive, respiratory distress, active bleeding, shock, active seizure, significant injury, shock, near-drowning, etc.) Normal airway, breathing & circulation but significant mechanism of injury or illness (post-seizure, minor fractures, infant < 3mo with fever, etc.) Normal airway, breathing & circulation No significant mechanism of injury or illness (small lacerations or abrasions, infant 3mo with fever)
Glasgow Coma Score
Infants Children /Adults
Eye Opening
Unstable Spontaneous 4 Spontaneous To speech/sound 3 To speech To pain 2 To pain No response 1 No response Verbal Response Coos or babbles 5 Oriented Irritable crying 4 Confused Cries to pain 3 Inappropriate words Moans to pain 2 Incomprehensible None 1 None Motor Response Spontaneous .6 Obeys commands Withdraws touch 5 Localizes pain Withdraws pain .4 Withdraws pain Abnormal flexion 3 Abnormal flexion Abnormal extension 2 Abnormal extension No response 1 No response
Potentially Unstable
Stable
Neonatal Resuscitation
Dry, Warm, Position, Tactile Stimulation. Suction Mouth then Nose. Call for ALS back-up. Administer O2 as needed. Apnea/Gasping, HR <100 or central cyanosis Ventilate with BVM @ 40-60/min HR<60 after 30 sec BVM Chest Compressions @ 120/min - 3:1 1/3 to 1/2 chest depth 2 thumb encircle chest or 2 fingers ALS available & HR <60 Intubate APGAR Score Epinephrine 0.01-0.03mg/kg 0 pts 1 pt IV/IO/ET Pulse Absent <100 1:10,000 Resp Absent Slow q 3-5 min Irregular Tone Limp Some flexion Reflex None Grimace Color Blue
Respiratory / Cardiac Arrest Treatment
Infant
<1yr
Child
1-8yr
Teen
9-18yr
Ventilation only CPR method 2 pts 100 Good Chest Depth
20/min 2 fingers 1/3-1/2
20/min 12/min 1 hand 1/3-1/2 2 hand 1/3-1/2
Compression Rate 100/min 100/min 100/min Ratio 5:1 5:1 5:1
Active motion Cough Sneeze Pink Body All Blue Limbs Pink
CPR should be started for HR<60. Only AEDs with pediatric capabilities should be used on patients < 8 yrs. of age (approx. 25kg or 55lb).
ALS Guidelines
Asystole or PEA Assess airway & start CPR Intubate & ventilate with oxygen Bradycardia Assess airway & give oxygen VF or pulseless VT Defibrillate up to 3 times as needed 2j /kg 4j /kg 4j /kg Start CPR, intubate, ventilate with O2 Epinephrine: 0.01 mg/kg 1:10,000 IV/ IO 0.1 mg/kg 1:1000 ET Defibrillate 4j / kg Amiodarone 5mg/kg IV/IO or Lidocaine 1mg / kg IV/ IO/ ET or Magnesium 25-50mg/kg IV/ IO (for torsades de pointes or hypomagnesemia) Defibrillate 4j / kg
Intubate if decreased consciousness Epinephrine: 0.01 mg/kg 1:10,000 IV/ IO Start CPR if HR<60. 0.1 mg/kg 1:1000 ET .Continue Epinephrine q 3-5 min, same dose Epinephrine: 0.01 mg/kg 1:10,000 IV/ IO 0.1 mg/kg 1:1000 ET Consider hi dose 0.1 mg/kg 1:1000 IV/IO/ET Continue Epinephrine q 3-5 min, same dose Consider possibility of hypoxia, hypovolemia, hypothermia, hyper/hypokalemia, tamponade, tension .pneumothorax, toxins/poisons/drugs or .thromboembolism & treat if present. Atropine 0.02 mg/kg IV/ IO / ET minimum dose 0.1 mg maximum dose 0.5 mg child; 1.0 mg teen
This reference card should not be considered to replace or supercede regional prehospital medical treatment protocols.
Supported in part by project grant #6 H33 MC 00036 from the Emergency Services for Children program, HRSA, USDHHS in cooperation with NHTSA Rev. 1/04
Das könnte Ihnen auch gefallen
- Pediatric Mock Resuscitation ScenariosDokument6 SeitenPediatric Mock Resuscitation ScenariosdinkytinkNoch keine Bewertungen
- Brugada Phenocopy: The Art of Recognizing the Brugada ECG PatternVon EverandBrugada Phenocopy: The Art of Recognizing the Brugada ECG PatternNoch keine Bewertungen
- For & Against by L.G. AlexanderDokument79 SeitenFor & Against by L.G. AlexanderIsmaeil Fazel100% (6)
- PAT - Remick Spring CE 2014Dokument50 SeitenPAT - Remick Spring CE 2014Nadar RizatullahNoch keine Bewertungen
- The Kids Are Alright Pediatric Trauma PearlsDokument21 SeitenThe Kids Are Alright Pediatric Trauma PearlsDaniel Torres CutivaNoch keine Bewertungen
- 23 Mock CodesDokument56 Seiten23 Mock Codesmaguisssa100% (4)
- Advancedpracticenursingprocedures Colyarmargaretsrg 150408034245 Conversion Gate01Dokument589 SeitenAdvancedpracticenursingprocedures Colyarmargaretsrg 150408034245 Conversion Gate01yesumovsNoch keine Bewertungen
- Secondary Growth of PlantsDokument13 SeitenSecondary Growth of PlantsAngie Kong Su Mei50% (2)
- The Ontogenetic Basic of Human AnatomyDokument18 SeitenThe Ontogenetic Basic of Human AnatomymeseniaNoch keine Bewertungen
- PEDIATRIC ASSESSMENT OVERVIEWDokument2 SeitenPEDIATRIC ASSESSMENT OVERVIEWAghnia Nafila100% (1)
- Care of The Normal Newborn: M. Rogers-Walker, MSN/Ed, RNDokument28 SeitenCare of The Normal Newborn: M. Rogers-Walker, MSN/Ed, RNyanetp01Noch keine Bewertungen
- PALS Study GuideDokument12 SeitenPALS Study GuidePrerna SehgalNoch keine Bewertungen
- Pediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesVon EverandPediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesBewertung: 5 von 5 Sternen5/5 (2)
- K7 - Supraventricular Tachycardia (SVT)Dokument44 SeitenK7 - Supraventricular Tachycardia (SVT)Zikri Putra Lan LubisNoch keine Bewertungen
- PALS 2015 Update - Nursing Grand RoundsDokument22 SeitenPALS 2015 Update - Nursing Grand RoundshatsuneNoch keine Bewertungen
- Children's Healthcare of Atlanta PICU Orientation ManualDokument18 SeitenChildren's Healthcare of Atlanta PICU Orientation ManualdmallozziNoch keine Bewertungen
- Acutely Ill ChildDokument50 SeitenAcutely Ill ChildAhmed KhanNoch keine Bewertungen
- ILS Case Studies COMP 2020.ppsxDokument39 SeitenILS Case Studies COMP 2020.ppsxKim Orven KhoNoch keine Bewertungen
- AirCare Pediatric Reference GuideDokument8 SeitenAirCare Pediatric Reference GuideN/ANoch keine Bewertungen
- PICU Common ProblemDokument49 SeitenPICU Common ProblemRawabi rawabi1997Noch keine Bewertungen
- Pocketbook WHO PediatricsDokument398 SeitenPocketbook WHO PediatricsNashria RusdhyNoch keine Bewertungen
- Cardiac MedicationsDokument8 SeitenCardiac Medicationsangeline totaram100% (2)
- Drugs in Cardiac EnmergenciesDokument94 SeitenDrugs in Cardiac EnmergenciesVijayan VelayudhanNoch keine Bewertungen
- Peadiatric Brain Tumour: Wong Ann Cheng MD (Ukm) MRCPCH (Uk)Dokument48 SeitenPeadiatric Brain Tumour: Wong Ann Cheng MD (Ukm) MRCPCH (Uk)An Zheng100% (4)
- Algo StrokeDokument2 SeitenAlgo Strokettrriissnnaa100% (1)
- Picu Ready RecknerDokument2 SeitenPicu Ready RecknerPranitha Reddy0% (1)
- Antrim ED Handbook 2019Dokument238 SeitenAntrim ED Handbook 2019Chris Jardine LiNoch keine Bewertungen
- TraumaBurn ClinicalGuidelines Final PDFDokument34 SeitenTraumaBurn ClinicalGuidelines Final PDFJuan Antonio GarcíaNoch keine Bewertungen
- ECG Changes in myocardial infarctionDokument25 SeitenECG Changes in myocardial infarctionginaulNoch keine Bewertungen
- The Science Behind NRP 7th EditionDokument45 SeitenThe Science Behind NRP 7th Editionviaerea100% (1)
- Stroke Pathway For Acute Care ProvidersDokument5 SeitenStroke Pathway For Acute Care Providersdremad1974100% (1)
- ACLS Primary Survey Guide for Respiratory ArrestDokument34 SeitenACLS Primary Survey Guide for Respiratory Arrest강기연100% (1)
- Persistent Pulmonary Hypertension in Newborn: By: Dr. Abhay Kumar Moderator: Dr. Akhilesh KumarDokument31 SeitenPersistent Pulmonary Hypertension in Newborn: By: Dr. Abhay Kumar Moderator: Dr. Akhilesh KumarAbhay BarnwalNoch keine Bewertungen
- PALS Pulseless Arrest Algorithm: Kleinman, M. E. Et Al. Circulation 2010 122:S876-S908Dokument3 SeitenPALS Pulseless Arrest Algorithm: Kleinman, M. E. Et Al. Circulation 2010 122:S876-S908YONE LENINNoch keine Bewertungen
- Emergency Medical Procedures GuideDokument57 SeitenEmergency Medical Procedures GuideDuane Liloc100% (1)
- ACLS Suspected Stroke AlgorithmDokument8 SeitenACLS Suspected Stroke AlgorithmBirhane GebreegziabiherNoch keine Bewertungen
- Pals CardDokument12 SeitenPals CardSara KhanNoch keine Bewertungen
- ToxidromesDokument1 SeiteToxidromesMayer Rosenberg100% (7)
- UNC ED Pediatric Asthma ProtocolDokument2 SeitenUNC ED Pediatric Asthma ProtocolAhmed BekhetNoch keine Bewertungen
- Neurologic Emergencies: Stroke & TIADokument10 SeitenNeurologic Emergencies: Stroke & TIASamantha Lui100% (2)
- Pharmacology For Paramedics: Jeremy Maddux, NREMTP, I/CDokument215 SeitenPharmacology For Paramedics: Jeremy Maddux, NREMTP, I/CSreejesh RkNoch keine Bewertungen
- Pediatric Cardiac Arrest Algorithm 2020 GuidelinesDokument27 SeitenPediatric Cardiac Arrest Algorithm 2020 GuidelinesLinna AndrianiNoch keine Bewertungen
- A Clinical Approach To SyncopeDokument8 SeitenA Clinical Approach To Syncopepuskesmas tarik100% (1)
- IV PDFDokument63 SeitenIV PDFelbagouryNoch keine Bewertungen
- Best Practice in ShockDokument30 SeitenBest Practice in ShockFoungZanz D. LuffyzNoch keine Bewertungen
- Emergency MedsDokument24 SeitenEmergency MedsNursyNurse100% (1)
- CPR AED Choking Guidelines for Healthcare ProvidersDokument2 SeitenCPR AED Choking Guidelines for Healthcare Providersreyes markNoch keine Bewertungen
- Pediatric Vital Signs MeasurementsDokument3 SeitenPediatric Vital Signs MeasurementsJheDelaPazValenzuelaNoch keine Bewertungen
- Pals HandoutDokument49 SeitenPals HandoutYasir AshfaqNoch keine Bewertungen
- Paeds Handbook Class2021 1568487638Dokument30 SeitenPaeds Handbook Class2021 1568487638kafosidNoch keine Bewertungen
- Pediatric Critical Care, 3rd Edition 2009 DR - NaggarDokument389 SeitenPediatric Critical Care, 3rd Edition 2009 DR - NaggarmariamNoch keine Bewertungen
- Pediatric Assessment TriangleDokument31 SeitenPediatric Assessment TriangleblairNoch keine Bewertungen
- PANCE Prep Pearls Valvular Disease PDFDokument4 SeitenPANCE Prep Pearls Valvular Disease PDFkatNoch keine Bewertungen
- Pediatric Trauma Resuscitation EssentialsDokument16 SeitenPediatric Trauma Resuscitation EssentialsHuseinNoch keine Bewertungen
- Hemodynamics Basic Concepts 1204053445109897 4Dokument115 SeitenHemodynamics Basic Concepts 1204053445109897 4valeriesolidum100% (1)
- Ecg Interpretation: Gel PDokument2 SeitenEcg Interpretation: Gel PjuliperNoch keine Bewertungen
- Procedural Sedation - Audit Information 2017-18Dokument14 SeitenProcedural Sedation - Audit Information 2017-18Anonymous msnwfNd0% (1)
- ACLS Practical Case Scenarios (1 June 2011)Dokument15 SeitenACLS Practical Case Scenarios (1 June 2011)nersNoch keine Bewertungen
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsVon EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNoch keine Bewertungen
- Pediatric Cardiology and Pulmonology: A Practically Painless ReviewVon EverandPediatric Cardiology and Pulmonology: A Practically Painless ReviewNoch keine Bewertungen
- IELTS WritingDokument32 SeitenIELTS WritingNguyễn Bình Nam100% (2)
- Argessay 120614074358 Phpapp02Dokument17 SeitenArgessay 120614074358 Phpapp02yesumovsNoch keine Bewertungen
- Form WritingDokument9 SeitenForm WritingSons YesuNoch keine Bewertungen
- Topics Task 2Dokument2 SeitenTopics Task 2yesumovsNoch keine Bewertungen
- HRR 2014 Final Digital-Uk PDFDokument192 SeitenHRR 2014 Final Digital-Uk PDFThavamNoch keine Bewertungen
- Education Dev Global Era 69Dokument282 SeitenEducation Dev Global Era 69yesumovsNoch keine Bewertungen
- Listofusefulwordsforinterpretingdatain 140723003852 Phpapp01Dokument20 SeitenListofusefulwordsforinterpretingdatain 140723003852 Phpapp01yesumovsNoch keine Bewertungen
- Índice: - Click The Tiles To Access The Respective ChaptersDokument451 SeitenÍndice: - Click The Tiles To Access The Respective ChaptersSons YesuNoch keine Bewertungen
- WCADP MoratoriumReport2010 en 1Dokument47 SeitenWCADP MoratoriumReport2010 en 1yesumovsNoch keine Bewertungen
- Argumentative Essay TodayDokument7 SeitenArgumentative Essay TodaySons YesuNoch keine Bewertungen
- Linking WordsDokument16 SeitenLinking WordsyesumovsNoch keine Bewertungen
- In Many Countries Where Capital Punishment Has Been Abolished There Has Been A Corresponding Rise in Violent Crime RatesDokument264 SeitenIn Many Countries Where Capital Punishment Has Been Abolished There Has Been A Corresponding Rise in Violent Crime RatesSons YesuNoch keine Bewertungen
- Taormina enDokument176 SeitenTaormina enyesumovsNoch keine Bewertungen
- Make Your IELTS Essay Sound More Academic With HEDGINGDokument27 SeitenMake Your IELTS Essay Sound More Academic With HEDGINGBenWorthington100% (2)
- YyDokument2 SeitenYyyesumovsNoch keine Bewertungen
- Workpermitsinireland Abriefguide 091216064028 Phpapp01Dokument12 SeitenWorkpermitsinireland Abriefguide 091216064028 Phpapp01yesumovsNoch keine Bewertungen
- IDokument2 SeitenIyesumovsNoch keine Bewertungen
- JDokument2 SeitenJyesumovsNoch keine Bewertungen
- A Clear Gospel MessageDokument6 SeitenA Clear Gospel MessageMady ChenNoch keine Bewertungen
- Both Sides + Opinion EssayDokument2 SeitenBoth Sides + Opinion Essayandyfarcs21Noch keine Bewertungen
- WPI LogDokument7 SeitenWPI LogyesumovsNoch keine Bewertungen
- HDokument2 SeitenHyesumovsNoch keine Bewertungen
- CH 11Dokument20 SeitenCH 11yesumovsNoch keine Bewertungen
- Writing Practice ActivityDokument5 SeitenWriting Practice ActivityyesumovsNoch keine Bewertungen
- Untitled 1Dokument9 SeitenUntitled 1yesumovsNoch keine Bewertungen
- CDokument2 SeitenCyesumovsNoch keine Bewertungen
- Ad/Disadvantages of Factory: Object 2Dokument3 SeitenAd/Disadvantages of Factory: Object 2yesumovsNoch keine Bewertungen
- Generations ChartDokument3 SeitenGenerations ChartBhopal SinghNoch keine Bewertungen
- HEMOLYTIC ANEMIAS AND ACUTE BLOOD LOSS: CAUSES, SIGNS, DIAGNOSIS AND TREATMENTDokument4 SeitenHEMOLYTIC ANEMIAS AND ACUTE BLOOD LOSS: CAUSES, SIGNS, DIAGNOSIS AND TREATMENTAjay Pal NattNoch keine Bewertungen
- Infinity Urea Liquid Reagent ENDokument2 SeitenInfinity Urea Liquid Reagent ENKouame FrancisNoch keine Bewertungen
- Vitality Fitness Assessment Form: 1. DetailsDokument2 SeitenVitality Fitness Assessment Form: 1. DetailsmusturNoch keine Bewertungen
- Worksheet Central DogmaDokument3 SeitenWorksheet Central DogmaRein Jhonnaley Dioso100% (1)
- Drug 1Dokument2 SeitenDrug 1Nicholas TagleNoch keine Bewertungen
- Surya NamaskarDokument2 SeitenSurya NamaskarDipkumar Patel100% (2)
- The Importance of Anaerobic ExerciseDokument13 SeitenThe Importance of Anaerobic Exerciseapi-357421918Noch keine Bewertungen
- The Motor System and Its Disorders LectureDokument51 SeitenThe Motor System and Its Disorders LectureKaito Noburu ShinNoch keine Bewertungen
- Excerpt From "Presence" by Amy CuddyDokument10 SeitenExcerpt From "Presence" by Amy CuddyOnPointRadioNoch keine Bewertungen
- Lesson 1 Forensic 5Dokument7 SeitenLesson 1 Forensic 5Marcos DmitriNoch keine Bewertungen
- Selection of Artificial TeethDokument44 SeitenSelection of Artificial TeethMohamed VandettaNoch keine Bewertungen
- CJR Biology UmumDokument15 SeitenCJR Biology UmumGresia FalentinaNoch keine Bewertungen
- Pharmaceutics 09 00041 v2Dokument14 SeitenPharmaceutics 09 00041 v2thasyaNoch keine Bewertungen
- DNA/RNA Extraction Guide - Isolate Nucleic Acids From CellsDokument27 SeitenDNA/RNA Extraction Guide - Isolate Nucleic Acids From CellsSahilKulkarniNoch keine Bewertungen
- Arab Board Orthopedic Exam June 2013Dokument35 SeitenArab Board Orthopedic Exam June 2013Nasser AlbaddaiNoch keine Bewertungen
- Alaryngeal SpeechDokument1 SeiteAlaryngeal Speechvee propagandaNoch keine Bewertungen
- Respiratory Muscle Ultrasonography: Methodology, Basic and Advanced Principles and Clinical Applications in ICU and ED Patients-A Narrative ReviewDokument12 SeitenRespiratory Muscle Ultrasonography: Methodology, Basic and Advanced Principles and Clinical Applications in ICU and ED Patients-A Narrative Reviewalejandro RodriguezNoch keine Bewertungen
- Reduce sodium guide for food industryDokument82 SeitenReduce sodium guide for food industryperunikicaNoch keine Bewertungen
- 3 - Physiology of The Stomach and Regulation of Gastric SecretionsDokument31 Seiten3 - Physiology of The Stomach and Regulation of Gastric SecretionsMaleeha YasminNoch keine Bewertungen
- Removable Partial Denture ComponentsDokument128 SeitenRemovable Partial Denture ComponentsVikas Aggarwal50% (2)
- Lesson 1 - Gen Bot LecDokument3 SeitenLesson 1 - Gen Bot LecYoko DeangNoch keine Bewertungen
- EMG in Weightlifting Performance During The SnatchDokument5 SeitenEMG in Weightlifting Performance During The SnatchsafaaismaeelNoch keine Bewertungen
- FTND - Harmful Effects of Pornography - s-10915 PDFDokument100 SeitenFTND - Harmful Effects of Pornography - s-10915 PDFponderatulNoch keine Bewertungen
- Bag-Valve-Mask Ventilation (BVM)Dokument1 SeiteBag-Valve-Mask Ventilation (BVM)Aidan RajkumarNoch keine Bewertungen
- Interval Training For PerformanceDokument20 SeitenInterval Training For PerformancePaulo Tsuneta100% (1)
- Nontoxic Nodular GoiterDokument7 SeitenNontoxic Nodular GoiterKayshey Christine ChuaNoch keine Bewertungen
- Hypertension ControlDokument7 SeitenHypertension ControlXyla CullenNoch keine Bewertungen
- Porges-2003-The Polyvagal Theory-Phylogenetic Contributions To Social BehaviorDokument11 SeitenPorges-2003-The Polyvagal Theory-Phylogenetic Contributions To Social BehaviorJohn Bakalis100% (1)