Beruflich Dokumente
Kultur Dokumente
CT Image Quality: Outsource, Inc. (All Rights Reserved)
Hochgeladen von
bbkanilOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
CT Image Quality: Outsource, Inc. (All Rights Reserved)
Hochgeladen von
bbkanilCopyright:
Verfügbare Formate
CT Image Quality
Wil Reddinger, M.Sc., R.T.(R)(CT)
copyright April 1998 OutSource, Inc. (all rights reserved)
CT IMAGE QUALITY Wil Reddinger, M.Sc., R.T.(R)(CT) copyright April 1998 One of the most important functions of a computed tomography (CT) system is to reproduce a threedimensional structure and represent that structure as an accurate two-dimensional cross-section on a television monitor. There are several characteristics that effect how well a CT system performs this task. Spatial resolution, contrast resolution, linearity, noise and artifacts are the primary characteristics that effect image quality in CT. Enhancing or suppressing any of these characteristics depends upon the imaging interests and the region of the body being scanned. It is important that to realize that changing CT parameters such as section thickness, algorithms and field of view have a profound effect on
the overall quality of the CT image. CT image quality is dependant upon balancing these characteristics and parameters to produce the best possible image for the anatomical region being scanned. Image noise and artifacts are the two biggest enemies of CT image quality. CT parameters can be manipulated to either decrease or eliminate the adverse effects of these image quality characteristics. Generally, there is a trade-off when CT parameters are manipulated. For example, if a bone reconstruction algorithm is utilized to increase spatial resolution, image noise increases which degrades contrast or soft tissue resolution. Increasing technical factors such as mAs or kVp decreases image noise but an increase in patient dose occurs. The CT technologist's goal is to manipulate CT parameters according the imaging interest or situation.
Spatial resolution is the CT system's ability to differentiate small objects that are adjacent to one another. The CT scanner's resolving power relies on how well small objects that are close together but have very different attenuation values or CT numbers are imaged. The point between two small objects with very different densities is considered to be a region of high frequency or high contrast. An inherent problem with any CT system is that the edges or boarders of these high frequencies are blurred to a certain degree. Therefore, instead of imaging these two small structures as separate entities, the CT system "sees" them as one structure. A CT system that can image high frequency regions without blur results in smaller objects being resolved. Spatial resolution in conventional radiography is superior compared to the spatial resolution of computed tomography. For example, when evaluating a radiograph
of the facial bones, it is easy to see that blurring does not occur between the maxillae and the maxillary sinus cavity. The area where the edge of the bone meets the sinus is not blurred unless the patient moved during the exposure. A CT section of the same region reveals a "fuzzy" or "hazy" appearance around the edges of the bones. There are parameters that a CT technologist can manipulate to increase the spatial resolution when scanning high frequency regions. Utilizing a bone, sharp, high frequency or high pass algorithm during reconstruction mathematically enhances the edges of structures by diminishing structural blurring. However, the added algorithm produces statistical interference, which results in an increase in image noise. The increase in image noise decreases contrast or soft tissue resolution. Generally, this is an expected outcome because the scan involved visualizing the bone and the
soft tissue demonstrated is sacrificed. Utilizing a bone window, a wide window width and a high window level, is necessary to visually enhance the edges of a structure (Figure 1).
Decreasing section thickness narrows the collimated beam that concentrates the photons on to a smaller area, which increases spatial resolution. Zooming or targeting requires the operator to manipulate the displayed field of view. Zooming or targeting takes a selected region and spreads it over the entire matrix that is used to create and display the CT image. A 512 X 512 matrix yields 262, 144 pixels or "little squares" that the image is displayed upon. If an image an entire abdomen is imaged the matrix contains all of the abdominal structures which fill the 262,144 pixels. If the CT technologist wants to
Figure 1 shows the effect of window width and level on image noise.
increase the spatial resolution of an individual vertebra, the vertebra is "Zoomed" or "Targeted". The result is that the vertebra fills the 262,144 pixels thereby increasing the imaging accuracy of the structure. Primarily, zooming or targeting decreases partial volume averaging of a region which increases the accuracy of the CT numbers in a region of interest measurement. There are 262,144 pixels used to display the image but zooming or targeting decreases their overall size, which decreases the possibility of many tissues occupying a single pixel. Zooming or Targeting is not the same as image magnification. Image magnification is usually achieved by turning a dial or trackball, which results in pixel stretching. Although, this technique may be visually appealing it does not change the amount of tissue occupying a single pixel. The ultimate situation would be to fill each individual pixel with one tissue type.
However, computer and display matrices are limited in size so it is not likely to happen. Other factors that influence spatial resolution include pixel size, which is influenced by the chosen, scanned field of view and matrix size, width of the detector, spacing between detectors, number of projections or views obtained and focal spot size. Several methods that quantify or measure spatial resolution include the point-spread function (PSF), line spread function (LSF), edge response function (ERF) and the modular transfer function (MTF). The MTF is the most commonly used method to measure the spatial resolution capabilities of a CT system, which is graphically depicted. The MTF demonstrates the frequency components of a structure in line pairs per centimeter (lp/cm). A line pair phantom consists of lead
strips that are placed at different widths apart. The more lines that can be visualized separate from one another, the better the systems spatial resolution. Spatial resolution depends upon imaging high frequency structures located a very small distance apart. In figure ** an MTF value of 1.0 represents a complete, without blurring, transfer of an object through the CT system to a monitor. An MTF value of 1.0 corresponds to imaging large structures that can very easily be imaged accurately by most CT systems. Therefore, the value of 0.1, which represents small, high frequency or density structures, is used to evaluate the spatial resolution capabilities of a CT system. It is known that a CT system does not have problems faithfully imaging large structures such as the liver or brain. Because of the inherent blurring of small, high density structures like IAC's it is important that individual's purchasing CT systems should inquire how
many line pairs per centimeter, at 0.1 on the MTF graph, does the CT system yield. The more lp/cm a CT system produces, the better the spatial resolution. Figure ** consists of three CT systems that have different lp/cm resolution capabilities. At 0.1 MTF it can be visualized that scanner C produces the most lp/cm. This means that scanner C is capable of separating smaller objects from one another than scanner A and B because the structures edges will be less blurred (Figure 2). Contrast Resolution is the ability of a CT scanner to differentiate small attenuation differences on the CT image. Contrast Resolution is also known as LowContrast Resolution and Tissue Resolution. CT can image tissues that vary only slightly in density and atomic number. Most soft tissues have atomic numbers or densities that are nearly the same. The ability of the
Figure 2: Modulation Transfer Function (MTF) Graph
CT scanner to image these slight differences is known as low contrast delectability, which is used to describe contrast resolution in computed tomography. Essentially, contrast resolution describes the CT systems ability to discriminate between two or more anatomical structures that attenuate "nearly" the same amount x-ray photons. CT is superior compared to conventional radiography in discriminating the absorption differences between structures that have similar but slightly different absorption characteristics. The liver, kidneys and psoas muscles are large structures that have different densities and atomic numbers but the absorption characteristics of the structures are not very different. Conventional radiography of the abdomen reveals the image structures as primarily "gray shaded" shadows and are some are superimposed. The position of the structures can be determined but the actual attenuation values cannot be
distinguished from one another. Computed tomography not only eliminates the superimposition of structures but absorption differences can be determined. Absorption properties of any tissue are represented by linear attenuation coefficients, which are numbers that describe the absorption characteristics of the tissues imaged. It is important to remember that the linear attenuation coefficient is an absorption measurement and it is dependant on thickness of a material, density of a material, atomic number and photon energy. A kVp change results in a change of a structures linear attenuation coefficient even if the same structure is being imaged. This is critical because the CT computer eventually assigns each pixel that contains a linear attenuation coefficient a number known as a Hounsfield Unit (HU) or a CT number. A CT operator can utilize a region of interest (ROI) measurement to visually display
CT numbers. Due to partial volume averaging and the inability to shrink the ROI "circle, oval or square" small enough CT numbers are displayed as averages. However, if large structures such as the liver or kidneys are subject to an ROI measurement, it is very likely that when a region is selected to be measured, it is an area that contains the same tissue. CT number ROI measurements should be made with the smallest circle, oval or square and in the center away from boarders and edges of suspected lesions (Figure 3).
Contrast resolution is limited by noise, as noise in an image increases, contrast resolution decreases thereby, inhibiting the ability of the CT scanner to image slight differences in tissue density (Seeram 1994). Tube collimation determines section thickness in CT. When
Figure 3: Region of Interest (ROI) measurements
section thickness is reduced the lead jaws of the collimator aperture closes which reduces the number of photons reaching the detector. The finely collimated beam is also filtered before it goes through the patient. These special filters called bow-tie filters absorb weaker energy photons, which reduce the possibility of scattered photons being detected by the CT detectors. An x-ray beam consists of polychromatic photons or photons having different energies. The bow-tie filters serve to absorb lower energy photons primarily to "lessen" the effects from the polychromatic nature of an x-ray beam. If the x-ray beam was not heavily filtered the accuracy of CT numbers would be sacrificed because less desirable photon energies would probably scatter and be included in the attenuation value of the tissue scanned. The ideal situation would be to have monochromatic x-ray photon energies pass through the patient and into the detectors.
This is a virtually impossible thing to do but heavy filtration and thin collimation of the x-ray beam makes the situation better. When section thickness is reduced the number of photons concentrated on the area of interest is reduced. Decreasing the number of photons results in the image becoming more "grainy". The "grainy" appearance of the section is due to image noise. For example, During a CT scan of the abdomen a technologist may be required to begin the procedure utilizing a 10 millimeter (mm) section thickness. The abdomen protocol may require the technologist to reduce the section thickness to 5mm if the pancreas is a specific area of interest. When comparing the 10 mm and 5 mm sections, note that the 5 mm sections appear to be grainier in appearance than the 10 mm sections. This results from limiting the number of photons used to create the 5 mm sections compared to the 10 mm
sections. Increasing the number of photons to the 5 mm sections may be accomplished by increasing mAs or kVp. However, the increase in technical factors increases patient dose. A soft tissue, standard or smooth algorithm is used during the reconstruction process to enhance soft tissue and contrast resolution. Soft tissue, standard or smooth algorithms are low-frequency or low pass algorithms. Low-frequency or low pass algorithms mathematically accentuate the soft tissues or where there are subtle attenuation differences between the tissues being imaged. The use of these algorithms requires a narrow window width and a low window level to properly be visualize on a television monitor. Detector systems must be sensitive to all the possible interactions between photons and imaged tissues. The number of levels of information that
a detector can detect is called the dynamic range of a detector. The higher the dynamic range the better the detector will be able to see and discriminate between small differences in attenuation. Morgan (1983) defines linearity as " Property of a detector characterized by an output electrical current that is exactly linearly proportional to the input radiation incident on the detector." Linearity is utilized to describe the performance of the CT system. Linearity describes the accuracy between the linear attenuation coefficient and the computer assigned CT number. The CT number scale assigns the linear attenuation coefficient of water the CT number zero. Bushong (1997) describes that the phantom utilized for the quality assurance of linearity of a CT system utilizes several materials placed in different positions throughout a water phantom. These materials
are different in composition and the linear attenuation coefficients and CT numbers are known. Daily checks and calibrations assure the accuracy of the CT numbers of each material and primarily the water contained within the phantom. Although, minor deviations may occur manufacturers have minimums and maximums for operable CT number deviation. The last two characteristics of CT Image quality are noise and artifacts. These two factors degrade CT image quality, scanning parameters and techniques are tailored in an attempt to lessen the adverse effects that appear on the image caused by the two factors. Noise is considered to be the number one limiting factor of CT image quality. Noise is the portion of a signal that
contains no information. Noise is characterized by a grainy appearance of the image. Many authors describe noise as a salt and pepper pattern on the CT image. If a quality assurance phantom is comprised of a known material like water, when the phantom is used to evaluate the quality of the image, it is expected that every portion of that phantom would have the CT number zero. Due to the statistical fluctuation in every scan it is impossible for this to occur. In the case of too little radiation, too few photons reach the detectors. As a result, the variance of CT numbers pixel to pixel is quite large. When a ROI is selected and the average CT number is displayed, the standard deviation is quite large. The level of noise in an image is recorded as the standard deviation in an ROI measurement. The larger the standard deviation, the less accurate the average CT number of the ROI. An analogy would be that of a salary survey. If only 5 people were
interviewed and their annual salary recorded, an average salary could be calculated. The variance, or deviation, between each salary listed would in all likelihood be quite large and the less the average would reflect any one of the five. On the other hand, if 100 people were interviewed, the deviation between each salary listed would not be as great as it was with just 5 people. The average salary calculated would more accurately reflect the salary of the group (Figure 4).
CT system manufacturers have minimum and maximum values for allowable differences in CT numbers of a water phantom. Generally the range of +3 to -3 difference in CT numbers is negligible. Many of the spiral/helical scanners have a +4 to -4 allowable range because of the mathematical process of interpolation is
Figure 4: Noise as a result of low radiation dose
included with the image reconstruction process. The major types of noise include quantum noise, electronic noise and computational noise. Quantum noise is a result of too few photons reaching a detector after being attenuated by the body. Any factor that limits the number of attenuated photons at the detector will increase image noise. Anatomical structure size, reduction of slice thickness without increasing technical factors, decreasing pixel size and scatter radiation are all factors that contribute to image noise. Electronic noise is noise contained within the image that can be caused by vibrations of any of the physical components, especially the rotational components or power fluctuations. Computational noise is primarily caused by all the statistical fluctuations that occur from the reconstruction mathematics that are essential to produce a CT image. A CT image involves millions of mathematical equations
being solved at approximately the same time. Spiral/helical CT data uses a mathematical technique called interpolation along with a reconstruction algorithm to produce axial image data from a volume of data. The process of adding a mathematical technique makes the computer work harder, which results in the CT image suffering by becoming grainier in appearance. It may be very difficult to actually distinguish which characteristic is responsible for the grainy appearance of an image but noise is always there. "An Artifact is any distortion or error in the image that is unrelated to the subject being studied (Morgan 1983)." Wolbarst (1993) describes artifacts as aberrations that arise at the interfaces of materials significantly different from the radiologic properties of the structures being scanned. There are many causes of artifacts that degrade
image quality as well as hide areas of pathology. Artifacts can appear as geometrical inconsistencies, blurring, streaks or inaccurate CT numbers. Streak artifacts are the most common distortions or errors that affect the quality of CT images. Motion, metallic objects, out-of-field, edge gradient effects, high-low frequency interfaces, equipment malfunctions and sampling errors are all causes of streak artifacts. Motion artifacts occur primarily because during reconstruction the mathematical algorithm is unable to solve for the inconsistencies in attenuation. Image reconstruction relies on the computer's ability to place attenuation values onto a matrix, which is nothing more than grid that has rows and columns of little blocks or pixels. If motion occurs during the scan the computer is unable to place an attenuation value at the proper
corresponding "address" so it can only manipulate the data it is given. The result usually appears as blurring or streaking of the object being scanned. Metallic objects such as dental fillings or prosthesis cause a streaking effect on an image. The appearance may mimic a "splashing" effect from the middle of the structure towards the edges of the object scanned. The primary reason that streaks occur from metal objects is because the objects exceed the attenuation values that CT system can faithfully image (Figure 5). Many older CT number scales assign the number 1000 as the top of the number scale. The number 1000 coincides with the attenuation value of cortical bone, which is primarily the densest structure in the human body. Many
Figure 5: Streaking artifact due to dental fillings
alloys used to make dental fillings or prosthesis have attenuation values greater than cortical bone. Therefore, the computer can only assign the highest value it knows. These metallic type objects exceed the dynamic range of the detectors in the detector array. The result is the metallic object is unable to be faithfully image resulting in streak artifacts. Many newer CT systems include attenuation values higher than bone. CT number scales have been expanded to include objects that have a CT number as high as 4,000. Out of field artifacts are caused by anatomy that is out side of the selected scan field of view. For example, if a persons chest measures 54 centimeters (cm) and the maximum scan field of view is 48cm, the CT system can only image 48 of the 54 cm. Unfortunately, The "extra" tissues are blocking detectors and attenuating photons.
The CT system can only account for the 48 cm scan circle and is unable to avoid the blocked detectors. Streak artifacts occur throughout the entire image, which degrades diagnostic accuracy and the overall quality of the CT image (Figure 6). Edge gradient and high-low frequency interface are similar causes of streak artifacts present on an image. Edge gradient streak artifacts generally occur when the edges of a "sharp" high-density object interface with a smooth surface. A streak artifact originates from the edges of the high frequency structure. Edge gradient artifacts frequently occur from the edges between bone and soft tissue. For example, on a CT image of the pelvis the ischial spines are sharp high frequency structure that interface with adjacent muscle tissue, which is a low frequency structure. A thin black streak artifact arises
Figure 6: Streaking caused by tissue being outside the scan circle (scan FOV).
from the edge of the bone. The streak emanating from a thin biopsy needle is an example of edge gradient streak artifacts. Streak artifacts arise from materials or structures when a high-density material such as barium interfaces with a low-density material such as air. This type of streak artifact commonly occurs in the gastrointestinal tract is filled with barium and air. The artifact arises due to the inability of the CT system to "transfer" the information accurately. In the previous discussion of spatial resolution, it was explained that CT systems inherently have problems with imaging structures that rapidly change from high to low densities (Figure 7). Equipment malfunctions such as tube arching, electrical malfunctions and detector malfunctions produce streak artifacts on a CT image. Tube arching artifacts give rise
Figure 7: Steaks due to dense contrast material in the bowel.
to many streaks and may appear to look like a "lightening storm". Streak artifacts that arise from malfunctioning detectors generally appear as straight line streaks. Edge gradient streak artifacts are contained within the anatomical part and are not always straight line streak artifacts. A malfunctioning detector causes a straight black line streak artifact on a scout image. Streak artifacts may also arise if too few views or projections of an object are obtained. These types of streak artifacts have been virtually eliminated because CT scanners are capable of producing hundreds of thousands of views or projections. The more views, or projections, "taken" of an object, the more accurate the image reconstruction. Beam hardening artifacts occur when the low energy photons are absorbed leaving the high-energy photons to strike the detectors. When x-ray photons strike a high-
density structure such as bone, lower energy photons are absorbed which results in further hardening of the beam. Hardening the beam results in a more penetrating beam. If the photons then traverse over a region that consists of low densities structures such as the brain, the resultant effect is a thick streak artifact that appears across the region. This occurs because the effective energy of the x-ray beam is increased when it passes through the tissues being scanned. When the energy of the beam is changed during the scanning process, the linear attenuation coefficients of the tissue that the "harder" beam travels across are changed. If an ROI measurement were taken in the area of the dark streak one would find that the CT numbers would be lower in that region. For example, when imaging the posterior fossa, beamhardening artifacts are found in the area between the bone and soft tissue. If an ROI measurement were
obtained without the beam hardening effect, soft tissue may have a CT number between 50 and 60. If an ROI measurement were obtained in the area of the beamhardening artifact, the CT numbers would be lower than the "real" or actual CT numbers of the soft tissue being scanned. The brain tissue that has a CT number between 40-60 might have a CT number value as low as -30. This is referred to as a "cupping" artifact. Methods of reducing this artifact include heavy beam filtration prior to entering the patient, higher kVp techniques and software programs that compensate for the "void" left by beam hardening (Figure 8). Ring artifacts appear on a CT image as a ring or a number of rings superimposed on the structures being scanned. The artifact is commonly associated with third generation or rotate-rotate CT systems. This artifact
Figure 8: Examples of beam-hardening artifact
occurs due to one or several misaligned or miscalibrated detectors in the detector array of the rotate-rotate CT system. The tube and detector array rotate at the same time. The tube and detectors are physically connected to one another. If the tube shifts slightly it can cause misalignment of the CT system. Therefore, a "bad" view is created for every photon that the misaligned or miscalibrated detector or detectors "sees". The result is non-uniform information becoming a part of the image that manifests as a series of rings. The detector or detectors must be re-aligned or re-calibrated to eliminate ring artifacts (Figure 9). The partial volume effect or volume averaging is when two or more different tissue types occupy the same pixel and are averaged together. The ultimate scenario for CT would be for one tissue type to occupy one pixel. Due to
Figure 9: Ring artifact(s)
the limitations of CT matrices, which determine how many pixels, makes up a CT image this is virtually impossible to accomplish. For example, if one pixel contained three separate tissues that had CT numbers of 60, 80 and 200, the ROI measurement of that pixel would be approximately 113. The tissues are averaged which produces a number that is inconsistent with the three tissues that were evaluated. Partial volume averaging is always present and can never be entirely eliminated. Utilizing smaller section thicknesses or smaller displayed field of views may increase the accuracy of CT numbers. CT image quality is dependant upon the balancing of parameters relative to image resolution. Balancing image quality by manipulating and altering CT parameters depends upon the region or the condition being scanned with respect for patient dose. Image quality is also
dependant upon limiting or eliminating the image degrading effects of noise and artifacts.
Reference List
Berland, Lincoln L. (1987). Practical CT Technology and Techniques. New York: Raven Press. Bushberg, Jerrold T., Seibert, J. Anthony, Leidholdt, Edwin M., and Boone, John M. (1994). The Essential Physics of Medical Imaging. St. Baltimore: Williams & Wilkins. Bushong, Stewart. (1993). Radiologic Science for Technologists. 5th edition. St. Louis: CV Mosby Publishers. Behrman, Richard H. Editor. (1994) Study Guide to Computed Tomography Advanced Applications. Greenwich, Connecticut: Clinical Communications Inc. Curry, Thomas S, Dowdey, James E., and Murry, Robert C. (1990). Christensen's Physics of Diagnostic Radiology. 4th edition. Philadelphia: Lea & Febiger. Morgan, Carlisle L. (1983). Basic Principles of Computed Tomography. Baltimore: University Park Pres
Scroggins,D. , Reddinger,W. , Carlton,R., & Shappell,A. (1995). Computed Tomography Review. Philadelphia: J.B. Lippincott Seeram, Euclid. (1994). Computed Tomography: Physical Principles, Clinical Applications and Quality Assurance. Philadelphia: W.B. Saunders Company. Wolbarst, Anthony B. (1993). Physics of Radiology. St. Norwalk, CT: Appleton & Lange.
Das könnte Ihnen auch gefallen
- Nugzar LipartelianiDokument78 SeitenNugzar LipartelianiTarun SinghNoch keine Bewertungen
- CT 1stDokument60 SeitenCT 1stDrHassan Ahmed ShaikhNoch keine Bewertungen
- CT1 Part 9 Image QualityDokument29 SeitenCT1 Part 9 Image Qualityrazan abdalrhmanNoch keine Bewertungen
- Pertanyaan ACS TicagrelorDokument5 SeitenPertanyaan ACS TicagrelorwhitecoatNoch keine Bewertungen
- Image EnhancementDokument14 SeitenImage EnhancementsanyamtimeNoch keine Bewertungen
- Lecture 20d CT Image RecontructionDokument40 SeitenLecture 20d CT Image RecontructionLajja Parikh PatelNoch keine Bewertungen
- Tweet TemplateDokument3 SeitenTweet TemplateEutychus2ndNoch keine Bewertungen
- CT Basics - Part 1Dokument27 SeitenCT Basics - Part 1bahadirerNoch keine Bewertungen
- Dynamic Controlled Atmosphere Storage A New Technology For The New York Storage IndustryDokument4 SeitenDynamic Controlled Atmosphere Storage A New Technology For The New York Storage IndustryYogesh KathrechaNoch keine Bewertungen
- Lecture3 Contrast Enhancement PDFDokument46 SeitenLecture3 Contrast Enhancement PDFSahil GandhiNoch keine Bewertungen
- (John C Russ) The Image Processing Cookbook (B-Ok - Xyz)Dokument108 Seiten(John C Russ) The Image Processing Cookbook (B-Ok - Xyz)getinetNoch keine Bewertungen
- 3.RS Image Enhancement 2014Dokument14 Seiten3.RS Image Enhancement 2014Thiwanka Chameera JayasiriNoch keine Bewertungen
- Slide Product Brilinta Crestor AsmihaDokument3 SeitenSlide Product Brilinta Crestor AsmihaMaretha Dyah AnggrainiNoch keine Bewertungen
- Epilepsi PDFDokument11 SeitenEpilepsi PDFJonathan SinartaNoch keine Bewertungen
- Principles of Computer Tomography ImagingDokument331 SeitenPrinciples of Computer Tomography ImagingomarbenhagiNoch keine Bewertungen
- CT Image QualityDokument13 SeitenCT Image QualityRAVI RANJAN- RIMTNoch keine Bewertungen
- CT Image QualityDokument25 SeitenCT Image QualityRa'eel Khan100% (2)
- Imaging of Normal SpineDokument32 SeitenImaging of Normal SpineDestia AnandaNoch keine Bewertungen
- Spinal TuberculosisDokument18 SeitenSpinal TuberculosisKevin KusumanNoch keine Bewertungen
- Pengayaan Koass Ortho - Update 5 VersionDokument122 SeitenPengayaan Koass Ortho - Update 5 Versionanon_967171484Noch keine Bewertungen
- Aktivitas Fisik Pada Dewasa Dan GeriatriDokument20 SeitenAktivitas Fisik Pada Dewasa Dan GeriatriAdinda Suci MaghfiraNoch keine Bewertungen
- Lecture 2// 8.4 CT Numbers, Hounsfield Unit, Gray Scale and Image QualityDokument7 SeitenLecture 2// 8.4 CT Numbers, Hounsfield Unit, Gray Scale and Image QualityThome JerkNoch keine Bewertungen
- Lesson 5 IMAGE QUALITYDokument6 SeitenLesson 5 IMAGE QUALITYWayne De Vergara PalaypayonNoch keine Bewertungen
- Cone Beam Technology: A Brief Technical: History of CAT and CBCTDokument9 SeitenCone Beam Technology: A Brief Technical: History of CAT and CBCTHugo MoralesNoch keine Bewertungen
- Module 1 Computed Tomography and Principles of OperationsDokument6 SeitenModule 1 Computed Tomography and Principles of OperationsWayne De Vergara PalaypayonNoch keine Bewertungen
- Document 39Dokument31 SeitenDocument 392022819384Noch keine Bewertungen
- CT Quality AssuranceDokument9 SeitenCT Quality AssuranceuatilakarathnaNoch keine Bewertungen
- Medical ImagingDokument9 SeitenMedical ImagingRajes WariNoch keine Bewertungen
- Trigger 40 - CTDokument14 SeitenTrigger 40 - CTBriann Louis PaderangaNoch keine Bewertungen
- DI Chap1Dokument9 SeitenDI Chap1HuntingparxxNoch keine Bewertungen
- Ultrasound Image Optimization ("Knobology") - B-ModeDokument12 SeitenUltrasound Image Optimization ("Knobology") - B-ModeSami MoqbelNoch keine Bewertungen
- Currently Available Maxillofacial CBCT EquipmentDokument4 SeitenCurrently Available Maxillofacial CBCT EquipmentzilniNoch keine Bewertungen
- Computed Tomography III: Reconstruction Image Quality ArtifactsDokument33 SeitenComputed Tomography III: Reconstruction Image Quality Artifactsgameplay84Noch keine Bewertungen
- NahidaDokument7 SeitenNahidaانجاز مشاريعNoch keine Bewertungen
- Image Quality and Image ArtifactsDokument22 SeitenImage Quality and Image Artifactslavanyarangaswamy31Noch keine Bewertungen
- BME 404 - Lab08Dokument10 SeitenBME 404 - Lab08abdullah al MamunNoch keine Bewertungen
- Basic Principles of CTDokument77 SeitenBasic Principles of CTcroydubsNoch keine Bewertungen
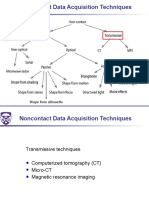
- 08 No Contact Data Asquisition Misc 2019 09 19Dokument47 Seiten08 No Contact Data Asquisition Misc 2019 09 19TimNoch keine Bewertungen
- Characteristics of Multislice CT: Recent TopicsDokument5 SeitenCharacteristics of Multislice CT: Recent TopicsAngelina ProtikNoch keine Bewertungen
- Edited CT Pres GRP 3Dokument37 SeitenEdited CT Pres GRP 3sanyengereNoch keine Bewertungen
- Computed Tomography and Magnetic Resonance ImagingDokument14 SeitenComputed Tomography and Magnetic Resonance ImagingChecko LatteNoch keine Bewertungen
- Welcome To International Journal of Engineering Research and Development (IJERD)Dokument6 SeitenWelcome To International Journal of Engineering Research and Development (IJERD)IJERDNoch keine Bewertungen
- ScanDokument3 SeitenScanLyka SantosNoch keine Bewertungen
- Module 3Dokument7 SeitenModule 3Wayne De Vergara PalaypayonNoch keine Bewertungen
- Geometrik Kedokteran2Dokument5 SeitenGeometrik Kedokteran2tasyaNoch keine Bewertungen
- CT Made ECasyDokument47 SeitenCT Made ECasyAnonymous ceYk4p4Noch keine Bewertungen
- Medical Imaging Systems Example QuestionsDokument2 SeitenMedical Imaging Systems Example QuestionsPika17Noch keine Bewertungen
- Computed Tomography MachineDokument24 SeitenComputed Tomography MachineGaurav Molankar100% (1)
- Cone Beamed Computerized Dental Tomography in DentistryDokument5 SeitenCone Beamed Computerized Dental Tomography in DentistryMeris JugadorNoch keine Bewertungen
- Waldo Tobler 1987Dokument5 SeitenWaldo Tobler 1987jp8c64f9ggNoch keine Bewertungen
- Section 2.3 Spatial Resolution, Pixel Size, and ScaleDokument6 SeitenSection 2.3 Spatial Resolution, Pixel Size, and ScaleShahid AmirNoch keine Bewertungen
- Evaluasi Ketebalan Irisan (Slice Thickness) Pada Pesawat CT-Scan Single SliceDokument7 SeitenEvaluasi Ketebalan Irisan (Slice Thickness) Pada Pesawat CT-Scan Single SliceKyun GazeboNoch keine Bewertungen
- E 1441 - 97 Rte0ndetukveDokument37 SeitenE 1441 - 97 Rte0ndetukveMarceloNoch keine Bewertungen
- Points, Pixels, and Gray Levels: Digitizing Image Data: James B. PawleyDokument22 SeitenPoints, Pixels, and Gray Levels: Digitizing Image Data: James B. PawleyÖner AyhanNoch keine Bewertungen
- Volumetric 3D Display For Radiation Therapy PlanningDokument28 SeitenVolumetric 3D Display For Radiation Therapy PlanningNewberryNoch keine Bewertungen
- Computed TomographyDokument4 SeitenComputed TomographyemilyNoch keine Bewertungen
- Module 1 Computed Tomography and Principles of OperationsDokument6 SeitenModule 1 Computed Tomography and Principles of OperationsWayne De Vergara PalaypayonNoch keine Bewertungen
- Segmentation and Feature Extraction LolDokument2 SeitenSegmentation and Feature Extraction LolMansi KasarNoch keine Bewertungen
- CT ScanningDokument24 SeitenCT ScanningMurary S PottyNoch keine Bewertungen
- Intramuscular Injection GuidelinesDokument2 SeitenIntramuscular Injection GuidelinesMehabooba Mehataf100% (1)
- Penguin Restaurant Infront of Cancer HospitalDokument2 SeitenPenguin Restaurant Infront of Cancer HospitalbbkanilNoch keine Bewertungen
- Kei10344 FMDokument4 SeitenKei10344 FMbbkanilNoch keine Bewertungen
- FS41 p34 Aptip Body OncologyDokument5 SeitenFS41 p34 Aptip Body OncologybbkanilNoch keine Bewertungen
- Important Information About Your StatementDokument1 SeiteImportant Information About Your StatementbbkanilNoch keine Bewertungen
- Chapter 4 Scintillation Detectors: 4.1. Basic Principle of The ScintillatorDokument10 SeitenChapter 4 Scintillation Detectors: 4.1. Basic Principle of The ScintillatorbbkanilNoch keine Bewertungen
- Bushong ReviewDokument10 SeitenBushong ReviewbbkanilNoch keine Bewertungen
- Bushong: Radiologic Science For Technologists, 10th EditionDokument6 SeitenBushong: Radiologic Science For Technologists, 10th EditionbbkanilNoch keine Bewertungen
- Bushong Rad ProtectionDokument7 SeitenBushong Rad ProtectionbbkanilNoch keine Bewertungen
- X-Ray Tube DiagramDokument1 SeiteX-Ray Tube DiagrambbkanilNoch keine Bewertungen
- Bipolar Disorder or ManicDokument16 SeitenBipolar Disorder or Manicbbkanil100% (1)
- AAPM Report 39 - CT Acceptance Testing (1993)Dokument101 SeitenAAPM Report 39 - CT Acceptance Testing (1993)DethsorNoch keine Bewertungen
- Prosthetics Lower Limb Catalogue 2012Dokument292 SeitenProsthetics Lower Limb Catalogue 2012mihaela_moldova9128Noch keine Bewertungen
- Multimode Optical Fiber Based SpectrometersDokument16 SeitenMultimode Optical Fiber Based Spectrometersebn123Noch keine Bewertungen
- Strategies For Film Replacement in RadiographyDokument15 SeitenStrategies For Film Replacement in Radiographysaleemut3100% (1)
- En c1316 Sarix Ti Ip ps041311Dokument4 SeitenEn c1316 Sarix Ti Ip ps041311Antonio ChipanaNoch keine Bewertungen
- Week 7 B Chapter 29, 30 Computed Tomography 45Dokument45 SeitenWeek 7 B Chapter 29, 30 Computed Tomography 45freedy freedyNoch keine Bewertungen
- 5.basic SensitometryDokument14 Seiten5.basic SensitometryankamgudeNoch keine Bewertungen
- Full Download Digital Radiography and Pacs 2nd Edition Carter Test BankDokument35 SeitenFull Download Digital Radiography and Pacs 2nd Edition Carter Test Bankbridieditch100% (27)
- Inside ProlithDokument179 SeitenInside ProlithgoucloudNoch keine Bewertungen
- SilverFast Resolution Target (USAF 1951) PDFDokument10 SeitenSilverFast Resolution Target (USAF 1951) PDFsage.electconNoch keine Bewertungen
- Radiamatic II Spec enDokument6 SeitenRadiamatic II Spec enAndrey ClavijoNoch keine Bewertungen
- 2022 @dentolib Antigoni Delantoni, Kaan Orhan Atlas of DentomaxillofacialDokument229 Seiten2022 @dentolib Antigoni Delantoni, Kaan Orhan Atlas of Dentomaxillofacialc8dqt289hfNoch keine Bewertungen
- 04main Measure Insp SensorsDokument66 Seiten04main Measure Insp SensorsJoao RobertoNoch keine Bewertungen
- 2018 OceanOptics InnovationBrochureDokument16 Seiten2018 OceanOptics InnovationBrochureDicky ArintaNoch keine Bewertungen
- RPT 29Dokument79 SeitenRPT 29Vidya NaikNoch keine Bewertungen
- Nano 5Dokument18 SeitenNano 5caralbmarbat_3207679Noch keine Bewertungen
- RDT 112 Prelim SummaryDokument26 SeitenRDT 112 Prelim SummaryJian SolimanNoch keine Bewertungen
- Paper 37472 Manuscript 12431 0 Final UpdatedDokument9 SeitenPaper 37472 Manuscript 12431 0 Final UpdatedAli ArdeshiriNoch keine Bewertungen
- A Beginner's Guide To Ultrasound BiomicrosDokument9 SeitenA Beginner's Guide To Ultrasound BiomicrosSALAH YOUNISNoch keine Bewertungen
- A Low-Cost High-Performance Digital Radar Test BedDokument9 SeitenA Low-Cost High-Performance Digital Radar Test BedWesley ChenNoch keine Bewertungen
- Bangladesh University of Engineering and Technology (Buet), DhakaDokument46 SeitenBangladesh University of Engineering and Technology (Buet), DhakaRashedKhanNoch keine Bewertungen
- Talysurf Cci 6000Dokument3 SeitenTalysurf Cci 6000Parveen SwamiNoch keine Bewertungen
- VersaDoc MP 4000 Sole Source SpecificationsDokument3 SeitenVersaDoc MP 4000 Sole Source SpecificationsdnajenNoch keine Bewertungen
- Checker 4G7C DatasheetDokument3 SeitenChecker 4G7C DatasheetGregg JamesNoch keine Bewertungen
- PikselDokument11 SeitenPikselNur RahmaNoch keine Bewertungen
- Tem PrimerDokument31 SeitenTem Primerjackactforever4Noch keine Bewertungen
- Physics PDFDokument47 SeitenPhysics PDFstoicea_katalinNoch keine Bewertungen
- Diopter Focus of ANVIS EyepiecesDokument39 SeitenDiopter Focus of ANVIS Eyepieceswildan mullerNoch keine Bewertungen
- Missile Approach Warning Systems - The Infrared vs. Ultraviolet Debate Geoff Van HeesDokument14 SeitenMissile Approach Warning Systems - The Infrared vs. Ultraviolet Debate Geoff Van Heessreeramk1350% (2)
- Basic Principles of UltrasoundDokument38 SeitenBasic Principles of UltrasoundredaradeNoch keine Bewertungen