Beruflich Dokumente
Kultur Dokumente
Electrolytes in Pediatrics
Hochgeladen von
Krittin NaravejsakulCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Electrolytes in Pediatrics
Hochgeladen von
Krittin NaravejsakulCopyright:
Verfügbare Formate
Fluid & Electrolytes Fluid & Electrolytes
in in
Pediatric Patients Pediatric Patients
:a.un.eusr nnsoq+u
no.:o:s..:aas
or:annraasass:nrua
. ourru n.a.uee.
Agenda
Body Fluid in Children
Osmolality: Water balance
Intravascular Volume: Sodium balance
Fluid Therapy Fluid Therapy
Body Fluids
TBW (60% wt)
= Intracellular fluid (ICF, 30-40% wt) +
Extracellular fluid (ECF, 20-25% wt)
n+sc:+a e+a 6 .ev v+vvc 8 cc. : total body
water .n+lvslaus::+a
A. 4 Litre
B. 4.8 Litre
Body Fluids
B. 4.8 Litre
C. 6 Litre
Total body water (TBW)
Term infant: 75% wt
Age 1 yr: 60% wt
Male adult: 60% wt
Body Fluids
Male adult: 60% wt
Female adult: 50% wt
Body Fluids
n+sc:+a e+a 6 .ev v+vvc 8 cc. : total body
water .n+lvslaus::+a
A. 4 Litre
B. 4.8 Litre
Body Fluids
B. 4.8 Litre
C. 6 Litre
oeu C ( 8 0.75 )
n+scasc.c.na:+a e+aassn 34 au+v
v+vvc 2.5 cc. : blood volume .n+lvs
laus::+a
A. 150 mL
Body Fluids
A. 150 mL
B. 200 mL
C. 250 mL
ECF (20-25% wt)
= Interstitial fluid (15% wt) + plasma (5% wt)
Intravascular (blood) fluid
8% wt (given Hct 40%)
Body Fluids
8% wt (given Hct 40%)
Preterm NB: 10% wt
n+scasc.c.na:+a e+aassn 34 au+v
v+vvc 2.5 cc. : blood volume .n+lvs
laus::+a
A. 150 mL
Body Fluids
A. 150 mL
B. 200 mL
C. 250 mL
oeu B ( 2500 0.1 )
Intravascular fluid Interstitial fluid
Examples
Heart failure
Hypoalbuminemia
Body Fluids
Hypoalbuminemia
Sepsis
Electrolyte composition
Osmolality
Value 285-295 mOsm/kg
ECF Osm = ICF Osm
Calculated Osm =
2[Na] + [glucose]/18 + [BUN]/2.8 2[Na] + [glucose]/18 + [BUN]/2.8
Effective Osm (tonicity) =
2[Na] + [glucose]/18
Osmolality
Osmolol gap
When Osm
measured
- Osm
calculated
> 10 mOsm/kg
Unmeasured osmoles e.g., methanol, ethylene glycol,
ethanol, mannitol ethanol, mannitol
.c:+ae+a 7 u .uv diabetic ketoacidosis :a
os.+ serum Na 130 mmol/L aa: sugar 300 mg/dL
t+a::oIv serum sugar 100 mg/dL aa. serum
Na a.sus::+a.n+lvs
A. 130.0 mmol/L A. 130.0 mmol/L
B. 133.2 mmol/L
C. 136.4 mmol/L
Osmolality
Hyperglycemia
Shift of H
2
O
Dilution of Na
[Na]
corrected
= [Na]
measured
+ 1.6 ([glucose] 100)/100 [Na]
corrected
= [Na]
measured
+ 1.6 ([glucose] 100)/100
.c:+ae+a 7 u .uv diabetic ketoacidosis :a
os.+ serum Na 130 mmol/L aa: sugar 300 mg/dL
t+a::oIv serum sugar 100 mg/dL aa. serum
Na a.sus::+a.n+lvs
A. 130.0 mmol/L A. 130.0 mmol/L
B. 133.2 mmol/L
C. 136.4 mmol/L
oeu B
Osmolality
Pseudohyponatremia
Na content / serum vol. while high serum lipids or
proteins
Na
Lipids or proteins
Serum
Osmolality
Osm regulation
H
2
O balance
Intake Intake + oxidation = skin + lungs + urine urine + GI loss
Osmoreceptor Osmoreceptor
Osmolality
Antidiuretic Antidiuretic hormone hormone
Osmolality
Thirsty Thirsty
Osmolality
Examples
Nephrotic syndrome (recent onset)
SIADH
Diabetes insipidus Diabetes insipidus
Osmolality
Minimum urine Osm
30-50 mOsm/kg
CH receiving little salt && inadequate protein
Risk for hypo Na Risk for hypo Na
Maximum urine Osm
1200 mOsm/kg
Less urine conc. ability in newborn
Risk for hyper Na dehydration
Intravascular volume
Body content of Na & Cl
Urine Na excretion
Undetectable urine Na
Very high urine Na Very high urine Na
Regulators
Renin-angiotensin system
Atrial natriuretic peptide
Intravascular volume
Sodium
Sodium
Intake
Breast milk: ~ 7 mEq Na /L
Formula: 7-13 mEq Na /L
Excretion Excretion
Increase in diarrhea, cystic fibrosis (sweat Na loss),
some renal diseases
Decrease in hyperaldosteronism, Liddles syndrome
(dysregulation of ENaC)
Hypernatremia
Level > 145-150 mEq/L
Etiology
Excessive Na
: Improperly mixed formula, iatrogenic intake, : Improperly mixed formula, iatrogenic intake,
hyperaldosteronism
Water deficit
: DI, insensible loss in NB, inadequate intake
Water & Na deficit
: GI, cutaneous, or renal losses
Hypernatremia
Manifestations
If dehydrated, less symptoms at initial
If Na largely or rapidly increase, CNS symptom
Hyperglycemia & mild hypo Ca (occasional) Hyperglycemia & mild hypo Ca (occasional)
Brain hemorrhage
Central pontine myelinolysis (occasional)
Brain edema in chronic case (due to rapid Na
correction)
HYPERNATRAEMIA
H
2
O
Losses
Na
+
+H
2
O
Deficits
Na
+
Addition
Excess
Hypovolemia
TBW
Body Na
+
Renal Losses Extrarenal losses
U
Na
Variable
U
Na
>20 mEq/l
Euvolemia
TBW
Normal body Na
+
Hypervolemia
TBW
Body Na
+
U
Na
>20 mEq/l
U
Na
<20 mEq/l
Renal Losses
Osmotic or Loop
Diuretics,
Postobstruction,
Intrinsic Renal
Disease
Extrarenal losses
Sweating, Burns,
Diarrhea, Fistulae
Hypotonic Saline
Renal Losses
Central DI
Nephrogenic DI
Extrarenal losses
Respiratory and Dermal
Insensible losses
Primary
Hyperaldosteronism,
Cushings syndrome,
Conns syndrome,
Hypertonic Dialysis
Hypertonic NaHCO
3
,
NaCl Tablets,
Saline enemas
Water Replacement
Diuretics & Water
Replacement
Hypernatremia
Treatment of hyper Na dehydration
Restore intravascular vol.
NS 20 mL/kg over 20 min (repeat till vol. stored)
Determine time for correction
Reduce Na < 12 mEq/L q 24 hr Reduce Na < 12 mEq/L q 24 hr
Administer fluid at constant rate
D5 NS - 20 mEq/L KCl at rate 1.25-1.5 time maintenance
Follow serum Na
Adjust fluid based on status & serum Na
Replace ongoing losses as they occur
n+sce+a 2 .ev v+vvc 4.7 cc .uv
nephrogenic DI :uqv+l e+.+av v+vvca.uv
4.0 cc :aos.+ serum Na 170 mmol/L n+sc:
free water deficit .n+lvs laus::+a
A. 320 mL A. 320 mL
B. 360 mL
C. 400 mL
Free Water Deficit
Current total Na = Previous total Na
C
1
V
1
= C
2
V
2
Na
actual
TBW = Na
desired
(TBW + H
2
O
Def
)
H
2
O
Def
= TBW [(Na
actual
/ Na
desired
) 1]
( if TBW = 0.6 wt, Na
desired
= 145 mEq/L )
H
2
O
Def
= 0.6 wt* [(Na
actual
/ 145) 1] 1000 mL
= [ 600 wt / 145 ] [ Na
actual
145 ] mL
4 wt [ Na
actual
145 ] mL
* actual weight
Fluid** Sodium Potassium
1. Total
= wt %deficit
= 4.7 kg 15%
= 0.7 kg (700 mL)
2. Free water (FWD)
= 4 wt [Na
actual
145]
[Na]
ECF
SFD %deficit
ECF
= 140 (300/1000) 60%
~ 25 mEq
[K]
ICF
SFD %deficit
ICF
= 150 (300/1000) 40%
= 18 mEq
Deficit Therapy
= 4 wt [Na
actual
145]
= 4 4 [170 145]
= 400 mL
3. Solute (SFD)
= total free water
= 700 400
= 300 mL
Avoid increasing the sodium by more than 12 mEq/L each 24 hr
Hyponatremia
Level < 130-135 mEq/L
Etiology
1 Pseudohyponatremia
2 Hyperosmolality 2 Hyperosmolality
3 Hypovolemia: Extrarenal or renal loss
4 Euvolemia: SIADH, glucocorticoid def,
hypothyroidism, H
2
O intoxication
5 Hypervolemia: CHF, hypoalbuminemia,
renal failure, capillary leak
Total body water
Total body Na
+
Total body water
Total body Na
+
HYPONATRAEMIA (<135 mEq/L)
PSEUDO-
HYPONATRAEMIA
Normal Plasma osmolality High FACTITOUS
HYPONATRAEMIA
Low
TRUE HYPONATRAEMIA
ECF volume Decreased Increased
Normal
Extrarenal
Renal
Total body water
Normal total body Na
+
Extrarenal
GI loss
Skin loss
Third
space
loss
UNa
<10 mmol/l
Renal
Osmotic diuresis/diuretic
therapy
Vomiting and bicarbonaturia
Post-obstructive diuresis
Recovery phase of ATN
Salt-losing CRF
Fanconi syndrome
Mineralocorticoid deficiency/
resistance
Cerebral salt wasting
UNa
>20 mmol/l
Non-oedematous states
SIADH
Excessive water intake
Antidiuretic drugs
Reset osmostate
Glucocorticoid deficiency
Hypothyroidism
Oedematous states
Nephrotic syndrome
Hepatic failure
Cardiac failure
Capillary leak
syndrome
Acute and chronic
renal failure
UNa
>20 mmol/l
UNa
<10 mmol/l
UNa
>20 mmol/l
Hyponatremia
Manifestations
If dehydrated, more symptoms
If Na largely or rapidly decrease, CNS symptom
(brain edema) (brain edema)
Central pontine myelinolysis in chronic case (due to
rapid Na correction, >12 mEq/L in 24 hr)
Hyponatremia
Treatment of dehydration
Restore intravascular vol.
NS 20 mL/kg over 20 min (repeat till vol. stored)
Rapid vol. repletion
20 mL/kg NS or Ringer lactate (max 1 L) over 2 hr 20 mL/kg NS or Ringer lactate (max 1 L) over 2 hr
Calculate 24-hr fluid needs (subtract isotonic fluid already
administered)
Administer remaining vol.
D5 NS - 20 mEq/L KCl over 24 hr
Follow serum Na
Replace ongoing losses as they occur
If active symptoms, give 3% NaCl (0.5 mEq/ mL) to
raise serum Na 125 mEq/L
Volume = Na space wt (125 [Na]
actual
)
Hyponatremia
or = 4 - 6 mL/kg
Potassium Potassium Potassium Potassium
The majority of body K is contained in muscle
The majority of extracellular K is in bone
< 1% of total body K is in plasma
Na Na
Na Na
150 150 mEq K mEq K
++
/L /L
K movement into cells K movement into cells
by effect of by effect of
Insulin Insulin
--Adrenergic agonists Adrenergic agonists
pH pH
K movement out of cells K movement out of cells
by effect of by effect of
--Adrenergic agonists Adrenergic agonists
pH pH
plasma osmolality plasma osmolality
Hyper K Hyper K stimulates stimulates
ATP ATP
ATP ATP
Na Na
K
K
K channel K channel
K channel K channel
K
K
Hyper K Hyper K stimulates stimulates
adrenal release of adrenal release of
catecholamines catecholamines
insulin secretion insulin secretion
Effect of intracellular potassium
K gradient generate action potential & rate of
cellular repolarization
Low conc raises intra-pH while high conc lowers
intra-pH.
Maintaining cell volume because of its important Maintaining cell volume because of its important
contribution to intracellular osmolality.
Most K absorption occurs in small intestine,
whereas colon exchanges body K for luminal
Na.
Renal failure, aldosterone, and glucocorticoids Renal failure, aldosterone, and glucocorticoids
colonic K secretion.
Urine K excretion by Urine K excretion by
aldosterone aldosterone
glucocorticoids glucocorticoids
ADH ADH
high urinary flow rate high urinary flow rate
high sodium delivery to high sodium delivery to
the distal nephron the distal nephron
Urine K excretion by Urine K excretion by
insulin
catecholamines
urinary ammonia
+
+
+
+
Hyperkalemia Hyperkalemia Hyperkalemia Hyperkalemia
SPURIOUS LABORATORY VALUE
Hemolysis Hemolysis
Tissue ischemia during blood drawing Tissue ischemia during blood drawing
Thrombocytosis or leukocytosis Thrombocytosis or leukocytosis
INCREASED INTAKE
Intravenous or oral Intravenous or oral
Blood transfusions Blood transfusions
TRANSCELLULAR SHIFTS
Acidemia Acidemia
Hyperosmolality Hyperosmolality
Insulin deficiency Insulin deficiency
DECREASED EXCRETION
Renal failure or renal disease Renal failure or renal disease
eg,. renal tubular disease, urinary tract eg,. renal tubular disease, urinary tract
obstruction, sickle cell disease, kidney obstruction, sickle cell disease, kidney
transplant, lupus nephritis transplant, lupus nephritis
Mineralocorticoid disorders Mineralocorticoid disorders
- - Acquired Addison disease Acquired Addison disease
- - 21 21- -OH def OH def
- - 3 3- -OH dehydrogenase def OH dehydrogenase def
- - Lipoid cong adrenal hyperplasia Lipoid cong adrenal hyperplasia
- - Adrenal hypoplasia congenita Adrenal hypoplasia congenita
Etiologies Etiologies
Hyperosmolality Hyperosmolality
Insulin deficiency Insulin deficiency
Cellular damage (eg,. Cellular damage (eg,.
Rhabdomyolysis, tumor lysis Rhabdomyolysis, tumor lysis
syndrome, tissue necrosis, syndrome, tissue necrosis,
hemolysis/hematomas/GI bleeding) hemolysis/hematomas/GI bleeding)
Medications (succinylcholine, digitalis Medications (succinylcholine, digitalis
intoxication, fluoride intoxication, Beta intoxication, fluoride intoxication, Beta--
adrenergic blockers) adrenergic blockers)
Exercise Exercise
Malignant hyperthermia Malignant hyperthermia
Hyperkalemic periodic paralysis Hyperkalemic periodic paralysis
- - Adrenal hypoplasia congenita Adrenal hypoplasia congenita
- - Aldosterone synthase def Aldosterone synthase def
- - Adrenoleukodystrophy Adrenoleukodystrophy
- - Hyporeninemic hypoaldosteronism Hyporeninemic hypoaldosteronism
- - Pseudohypoaldosteronism type I & II Pseudohypoaldosteronism type I & II
Medications (eg,. ACEIs, ARBs, K Medications (eg,. ACEIs, ARBs, K- -
sparing diuretics, cyclosporin, NSAIDs, sparing diuretics, cyclosporin, NSAIDs,
trimethoprim) trimethoprim)
Serum K is 0.4 mEq/L higher than plasma K
For platelet 100,000/L, serum K 0.15 mEq/L
WBCs > 200,000/L can cause dramatic serum K
If significant WBCs or platelets, sample should be from
plasma that is evaluated promptly. plasma that is evaluated promptly.
Excessive K intake, by itself, not usually cause
hyper K.
To evaluate renal response to hyper K
Transtubular potassium gradient (TTKG)
Remark: urine osmolality must be greater than the serum osmolality
TTKG < 8 during hyper K
= Defect in renal K excretion due to either lack of
aldosterone or inability to respond to aldosterone
In adrenal disorders causing decreased production of
aldosterone
Hyper K, metabolic acidosis and salt wasting with hypo Na
A deficiency in renin, a result of kidney damage, can
lead to decreased aldosterone production.
Impaired renal function in some patients partially
accounts for hyper K accounts for hyper K
Pseudohypoaldosteronism type 1
In autosomal recessive variant,
- defect in renal Na channel
- severe symptoms, beginning in infancy
In autosomal dominant form, In autosomal dominant form,
- defect in aldosterone receptor
- milder, often remitting in adulthood
Pseudohypoaldosteronism type 2
Gordon syndrome
Autosomal dominant
Activating mutations in either WNK1 or WNK4
Hypertension due to salt retention and impaired Hypertension due to salt retention and impaired
excretion of K and H
+
Cardiac Manifestations
ECG changes begin with peaking T waves followed,
as K level increases, by
PR interval,
flattening P wave, flattening P wave,
widening QRS complex and
eventually ventricular fibrillation
If K level > 6.06.5 mEq/L, ECG should be obtained.
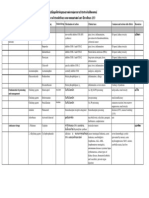
Agent Dose Onset
(Duration)
Comments/side effects
NaHCO
3
(1 mEq/mL)
1 mEq/kg IV over 10-30 min 15-30 min
(1-4 hr)
Assure adequate ventilation; do
not give simultaneously with
Ca
Ca gluconate
(10%)
0.5-1 mL/kg IV over 5-15 min Immediate
(30-60 min)
Monitor ECG for bradycardia; stop
infusion if pulse <100/min
-agonist
(albuterol)
<25 kg: 2.5 mg
>25 kg: 5-10 mg via nebulizer
30 min Tachycardia
Hypertension
Medication for Hyperkalemia
(albuterol) >25 kg: 5-10 mg via nebulizer Hypertension
Kalimate 1 g/kg PO in H
2
O or
PR in 5%glucose or
2%methylcellulose
50-60 min (PR)
2-3 hr (PO)
Constipation
Kayexalate 1 g/kg PR in 30% sorbitol
or PO in 70% sorbitol
50-60 min (PR)
2-3 hr (PO)
Na, P, Ca
Constipation
Glucose and
insulin
Glucose 1 g/kg and insulin
0.2 u/kg IV over 1-2 hr
15-30 min
(3-6 hr)
Monitor blood sugar
Algorithm for Hyperkalemia
Normal ECG
(~K
+
= 6-7 mEq/L)
- Elimination K+ from all intake
- Polystyrene resin (kalimate,
kayexalate)
Abnormal ECG
(~K
+
>7 mEq/L)
- 10% Ca gluconate 1 mL/kg IV
in 5 min
- NaHCO3 1-2 mL/kg IV in 10 min
K
+
> 6 mEq/L
kayexalate)
po q 6 hr or enema over
4-6 hr
- NaHCO3 1-2 mL/kg IV in 10 min
- Regular insulin 0.1 U/kg IV with
D25W 2 mL/kg in 30 min
- Dialysis if above unsuccessful
In patients not anuric, loop diuretic renal K excretion.
Hypokalemia Hypokalemia
Etiologies Etiologies
SPURIOUS
High white blood cell count
TRANSCELLULAR SHIFTS
Alkalemia
Insulin, -adrenergic agonists, drugs/toxins
(theophylline, barium, toluene)
Hypokalemic periodic paralysis
DECREASED INTAKE
EXTRARENAL LOSSES
Diarrhea
Laxative abuse
Sweating
RENAL LOSSES
With metabolic acidosis
Distal renal tubular acidosis (RTA)
Proximal RTA
RENAL LOSSES (cont)
With metabolic alkalosis
- Low urine chloride
Emesis nasogastric suction
Chloride losing diarrhea
Cystic fibrosis
Low chloride formula
Posthypercapnia
Previous loop or thiazide diuretic use
- High urine chloride and normal blood
pressure
Gitelman syndrome
Distal renal tubular acidosis (RTA)
Proximal RTA
Ureterosigmoidostomy
Diabetic ketoacidosis
Without specific acid-base disturbance
Tubular toxins: amphotericin, cisplatin,
aminoglycosides
Interstitial nephritis
Diuretic phase of acute tubular necrosis
Postobstructive diuresis
Hypomagnesemia
High urine anions (e.g., penicillin or penicillin
derivatives)
pressure
Gitelman syndrome
Bartter syndrome
Loop and thiazide diuretics
- High urine chloride and high blood pressure
Adrenal adenoma or hyperplasia
Glucocorticoid-remedial aldosteronism
Renovascular disease
Renin-secreting tumor
17-hydroxylase def
11-hydroxylase def
Hypokalemia is common in children, with most
cases related to gastroenteritis.
Clinical manifestration
Muscle weakness, cramps or paralysis with the legs,
followed by the arms (when K < 2.5 mEq/L)
Urinary retention, constipation or ileus
(when K < 2.5 mEq/L)
Primary polydipsia, impaired urinary concentrating ability, Primary polydipsia, impaired urinary concentrating ability,
interstitial nephritis and renal cysts
Hypo K may worsen hepatic encephalopathy because
hypo K stimulates renal ammonia production
To evaluate renal response to hypo K
Transtubular potassium gradient (TTKG)
Remark: urine osmolality must be greater than the serum osmolality
TTKG > 4 in the presence of hypo K
= Excessive urinary losses of potassium
Management
Type of therapy depends on K level, clinical symptoms,
renal function, presence of K transcellular shifts, ongoing
losses, and the patient's ability to tolerate oral K.
Oral K is safer, albeit not as rapid in urgent situations. Oral K is safer, albeit not as rapid in urgent situations.
Choice for supplementation depends on concurrent
electrolyte abnormalities
Fluid Therapy Fluid Therapy
Maintenance Therapy
Body Surface Area Method 1500 mL/BSA (m
2
)/day
100/50/20 Method
Weight
0-10 kg
11-20 kg
> 20 kg
Fluid
100 mL/kg/day
100 mL + 50 mL/kg/day for every kg > 10 kg
1500 mL + 20 mL/kg/day for every lg > 20 kg
4/2/1 Method 4/2/1 Method
Weight
0-10 kg
11-20 kg
> 20 kg
Fluid
4 mL/kg/h
40 mL + 2 mL/kg/h for every kg > 10 kg
60 mL + 1 mL/kg/h for every kg > 20 kg
Insensible + Measured Losses Method
400-600 mL/BSA (m2)/day + urine output (mL/mL) + L
other measured losses (mL/mL)
High water needs of smaller, less mature patients
Upper limit of 2.4 L/ 24 hr in adult-sized patients
Maximum fluid rate 100 mL/hr
Maintenance Therapy
Maximum fluid rate 100 mL/hr
Composition of Intravenous Solutions
Fluid [Na
+
] [Cl
-
] [K
+
] [Ca
2+
] [Lactate
-
]
Normal saline (0.9% NaCl) 154 154
Normal saline (0.45% NaCl) 77 77
Normal saline (0.225% NaCl) 38.5 38.5
Maintenance Therapy
Normal saline (0.225% NaCl) 38.5 38.5
Ringer lactate 130 109 4 3 28
In all children,
carefully monitor wt, urine output, and elytes.
Maintenance Therapy
Sources of Water loss
Urine 60%
Insensible loss (ISL) ~35% (skin & lungs)
Stool 5%
Maintenance Therapy
ISL, 40% in infants; 25% in adolescents
Fever - Increase maintenance fluids by 10-15%
for each degree > 38
o
C
Tachypnea
(nonhumidified environment)
- Increase maintenance fluids by 5-10%
Maintenance Therapy
AVERAGE COMPOSITION OF DIARRHEA
- Sodium : 55 mEq/L
- Potassium : 25 mEq/L
- Bicarbonate: 15 mEq/L
Replacement Therapy
APPROACH TO REPLACEMENT OF ONGOING LOSSES
- Solution: D5 0.2 NS + 20 mEq/L NaHCO
3
+ 20 mEq/L KCl
- Replace stool mL/mL q 16 hr
AVERAGE COMPOSITION OF GASTRIC FLUID
- Sodium: 60 mEq/L
- Potassium: 10 mEq/L
- Chloride: 90 mEq/L
Replacement Therapy
APPROACH TO REPLACEMENT OF ONGOING LOSSES
- Solution: NS + 10 mEq/L KCl
- Replace output mL/mL q 16 hr
1. Mild dehydration
<5% in infant; <3% in older child or adult
2. Moderate dehydration
510% in infant; 36% in older child or adult
3. Severe dehydration
Deficit Therapy
3. Severe dehydration
>10% in infant; >6% in older child or adult
Body weight loss
a
<5% (3%) 10% (6%) >15% (9%)
Symptoms
interstitial fluid
- Colour
- Mucous membranes
- Eyes
- Skin turgor
Thirst
Pale
Dry
Restless
Grey
Parched
Deep set
Tenting
Lethargic/obtunded
Mottled
Cracked
sunken
Loss - Skin turgor
- Fontanelle
intra-vascular vol
- Pulse
- CRT
b
- BP
- Urine output
Flat
Tenting
Soft
rate, weak
~ 2 sec
Normal/low
Oliguria
Loss
Sunken
rate, feeble
> 3 sec
Low/unrecordable
Anuria
a, Percentage outwith parentheses indicate estimates for infancy and those within are estimates beyond infancy.
b, capillary refill time
Treatment of dehydration
Restore intravascular vol.
NS 20 mL/kg over 20 min (repeat till vol. stored)
Rapid vol. repletion
20 mL/kg NS or Ringer lactate (max 1 L) over 2 hr
Dehydration Therapy
20 mL/kg NS or Ringer lactate (max 1 L) over 2 hr
Calculate 24-hr fluid needs (subtract isotonic fluid already
administered)
Administer remaining vol.
D5 NS 20 mEq/L KCl over 24 hr
Follow serum Na
Replace ongoing losses as they occur
Monitoring Therapy
VITAL SIGNS
Pulse
Blood pressure
INTAKE AND OUTPUT
Fluid balance
Dehydration Therapy
Fluid balance
Urine output and specific gravity
PHYSICAL EXAMINATION
Weight
Clinical signs of depletion or overload
ELECTROLYTES
Acute diarrhea
Intravenous therapy may be required in
severe dehydration
uncontrollable vomiting
extreme fatigue, stupor, or coma
Dehydration Therapy
extreme fatigue, stupor, or coma
gastric or intestinal distention
Acute diarrhea
Deficit
Mild dehydration: ORS 50 mL/kg within 4 hr
Moderate dehydration: ORS 100 mL/kg over 4 hr
Additional ORS 10 mL/kg for each stool
Dehydration Therapy
Additional ORS 10 mL/kg for each stool
Maintenance (after rehydration)
Mild diarrhea: ORS 100 mL/kg/24 hr until the diarrhea
stops.
severe diarrhea: ORS 1015 mL/kg/hr under close
supervision
Dehydration Therapy
A risk of hypernatremia with the WHO ORS
if maintenance solution is used without supplemental water or formula
...anurnaa+ran:oa.u.:u :.rn.+u.:u. u.:u
Inzun+.u.:uaanaa aou.:uaa.+..+n.anra..
nnan+nona+n.un+.aau nan+non:nnna.nn
ar+.nnaruo.nan a nur... ar+.nnaruo.nan a nur...
n::L:u:11t:1vn:::1tv1v
n::L1vnutnan::ta1auv:nunnannutntuv1:1t
Das könnte Ihnen auch gefallen
- 160 2.hepatolithiasis PDFDokument19 Seiten160 2.hepatolithiasis PDFKrittin NaravejsakulNoch keine Bewertungen
- 160 2.hepatolithiasis PDFDokument19 Seiten160 2.hepatolithiasis PDFKrittin NaravejsakulNoch keine Bewertungen
- 160 - 3.HP and NSAID Negative Peptic PDFDokument12 Seiten160 - 3.HP and NSAID Negative Peptic PDFKrittin NaravejsakulNoch keine Bewertungen
- 160 - 4.probiotics and Irritable Bowel PDFDokument15 Seiten160 - 4.probiotics and Irritable Bowel PDFKrittin NaravejsakulNoch keine Bewertungen
- 160 2.hepatolithiasis PDFDokument19 Seiten160 2.hepatolithiasis PDFKrittin NaravejsakulNoch keine Bewertungen
- 165 - 5.constipation in Patients With Spinal Cord InjuryDokument13 Seiten165 - 5.constipation in Patients With Spinal Cord InjuryKrittin NaravejsakulNoch keine Bewertungen
- 160 - 4.probiotics and Irritable Bowel PDFDokument15 Seiten160 - 4.probiotics and Irritable Bowel PDFKrittin NaravejsakulNoch keine Bewertungen
- 160 2.hepatolithiasis PDFDokument19 Seiten160 2.hepatolithiasis PDFKrittin NaravejsakulNoch keine Bewertungen
- 165 - 5.constipation in Patients With Spinal Cord InjuryDokument13 Seiten165 - 5.constipation in Patients With Spinal Cord InjuryKrittin NaravejsakulNoch keine Bewertungen
- 160 - 4.probiotics and Irritable Bowel PDFDokument15 Seiten160 - 4.probiotics and Irritable Bowel PDFKrittin NaravejsakulNoch keine Bewertungen
- 165 - 5.constipation in Patients With Spinal Cord InjuryDokument13 Seiten165 - 5.constipation in Patients With Spinal Cord InjuryKrittin NaravejsakulNoch keine Bewertungen
- 160 - 3.HP and NSAID Negative Peptic PDFDokument12 Seiten160 - 3.HP and NSAID Negative Peptic PDFKrittin NaravejsakulNoch keine Bewertungen
- Pediatriccardiovascularproblemsinemergencysetting15 Feb 2011 110216224036 Phpapp02Dokument75 SeitenPediatriccardiovascularproblemsinemergencysetting15 Feb 2011 110216224036 Phpapp02Krittin NaravejsakulNoch keine Bewertungen
- Definition of Terms2013Dokument80 SeitenDefinition of Terms2013Krittin NaravejsakulNoch keine Bewertungen
- Use of Vasopressors in Sepsis Resuscitation PDFDokument11 SeitenUse of Vasopressors in Sepsis Resuscitation PDFKrittin Naravejsakul100% (1)
- 191-Pitfalls in Management of Bleeding Disorders-20111117163513Dokument81 Seiten191-Pitfalls in Management of Bleeding Disorders-20111117163513Krittin NaravejsakulNoch keine Bewertungen
- Lecture Diarrhea and ConstipationDokument63 SeitenLecture Diarrhea and ConstipationKrittin NaravejsakulNoch keine Bewertungen
- Dementia and NeuropsychiatryDokument133 SeitenDementia and NeuropsychiatryKrittin Naravejsakul100% (1)
- EYE EXAMSDokument42 SeitenEYE EXAMSKrittin NaravejsakulNoch keine Bewertungen
- °Âõπ∑Ÿ¡∫√‘‡«≥™Àõß∑Âõß °"√Æ‘‡§√"-Àåªí≠À"°Âõπ∑Ÿ¡∫√‘‡«≥™Àõß∑Âõß„Π‡¥Á° ·Π«∑"ß°"√´-°ª√-«-Μ‘·≈-Μ√«®√À"ß°"¬ ‡§√◊Ëõß¡◊Õ ◊∫§Âπ∑"ß√-ß '«‘∑¬"·≈-‡«™»" Μ√Å𑫇§≈'¬√Å Tumor Markers °"√¬◊Π¬-Π°"√«‘Π‘®©-¬¢-Èπ Ÿ¥∑Â"¬Dokument40 Seiten°Âõπ∑Ÿ¡∫√‘‡«≥™Àõß∑Âõß °"√Æ‘‡§√"-Àåªí≠À"°Âõπ∑Ÿ¡∫√‘‡«≥™Àõß∑Âõß„Π‡¥Á° ·Π«∑"ß°"√´-°ª√-«-Μ‘·≈-Μ√«®√À"ß°"¬ ‡§√◊Ëõß¡◊Õ ◊∫§Âπ∑"ß√-ß '«‘∑¬"·≈-‡«™»" Μ√Å𑫇§≈'¬√Å Tumor Markers °"√¬◊Π¬-Π°"√«‘Π‘®©-¬¢-Èπ Ÿ¥∑Â"¬priscillaNoch keine Bewertungen
- Drug List-53 STDDokument24 SeitenDrug List-53 STDKrittin NaravejsakulNoch keine Bewertungen
- PE Spine2010Dokument38 SeitenPE Spine2010Krittin NaravejsakulNoch keine Bewertungen
- ReA SittichaiDokument22 SeitenReA SittichaiKrittin NaravejsakulNoch keine Bewertungen
- Ent Instruments 100503041754 Phpapp02Dokument59 SeitenEnt Instruments 100503041754 Phpapp02Krittin NaravejsakulNoch keine Bewertungen
- Common Ent Emergencies 24126Dokument64 SeitenCommon Ent Emergencies 24126Krittin NaravejsakulNoch keine Bewertungen
- Anticoagulants in AcsDokument66 SeitenAnticoagulants in AcsKrittin NaravejsakulNoch keine Bewertungen
- EYE EXAMSDokument42 SeitenEYE EXAMSKrittin NaravejsakulNoch keine Bewertungen
- Osce Ecg 110401044906 Phpapp01Dokument28 SeitenOsce Ecg 110401044906 Phpapp01Krittin NaravejsakulNoch keine Bewertungen
- Immune Reconstitution Inflammatory Syndrome (IRIS) : V. LuviraDokument32 SeitenImmune Reconstitution Inflammatory Syndrome (IRIS) : V. LuviraKrittin NaravejsakulNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Preauricular SineDokument5 SeitenPreauricular SineAldy BimaNoch keine Bewertungen
- 2001 Pathology MCQDokument11 Seiten2001 Pathology MCQOsama Bakheet100% (1)
- Norton Healthcare News: February 2010Dokument12 SeitenNorton Healthcare News: February 2010Norton HealthcareNoch keine Bewertungen
- Kreozan PoisoningDokument9 SeitenKreozan Poisoningdr Alex stanNoch keine Bewertungen
- Effect of Cervical Cancer Prevention Education in Middle-School Girl in KoreaDokument6 SeitenEffect of Cervical Cancer Prevention Education in Middle-School Girl in KoreaTrysna Ayu SukardiNoch keine Bewertungen
- Maintenance Fluid TherapyDokument22 SeitenMaintenance Fluid TherapyJonathan IngramNoch keine Bewertungen
- 1st Aid CPR & ERSDokument159 Seiten1st Aid CPR & ERSAhmad FaizNoch keine Bewertungen
- NHSN Manual OverviewDokument445 SeitenNHSN Manual OverviewDayana RodriguezNoch keine Bewertungen
- Infeksi parasit di saluran cerna: Diagnosis dan pengobatan protozoa dan helminta penyebab diareDokument69 SeitenInfeksi parasit di saluran cerna: Diagnosis dan pengobatan protozoa dan helminta penyebab diareRangga DarmawanNoch keine Bewertungen
- Perioperative Nurses Role Anterior THADokument20 SeitenPerioperative Nurses Role Anterior THACrystal Thomas-VollstaedtNoch keine Bewertungen
- Legalization of Marijuana in IndiaDokument40 SeitenLegalization of Marijuana in IndiaSiddharth GargNoch keine Bewertungen
- Berglundh Et Al-2018-Journal of PeriodontologyDokument6 SeitenBerglundh Et Al-2018-Journal of PeriodontologyestefyNoch keine Bewertungen
- Dental Implants History and DefinitionDokument6 SeitenDental Implants History and DefinitionRmz StudyNoch keine Bewertungen
- VSR-411 Veterinary Surgery & Anaesthesiology Question BankDokument7 SeitenVSR-411 Veterinary Surgery & Anaesthesiology Question Bankvishnu dathNoch keine Bewertungen
- IntroductionDokument5 SeitenIntroductionDivyansh GolyanNoch keine Bewertungen
- Recording of Fluid Balance Intake-Output PolicyDokument7 SeitenRecording of Fluid Balance Intake-Output PolicyRao Rizwan ShakoorNoch keine Bewertungen
- Spa Kaki Diabetik Efektif Memperbaiki Sensasi Kaki Pada DiabetesiDokument8 SeitenSpa Kaki Diabetik Efektif Memperbaiki Sensasi Kaki Pada DiabetesiDETA INDRAYANTINoch keine Bewertungen
- TYROSINEMIADokument9 SeitenTYROSINEMIAMaria ClaraNoch keine Bewertungen
- Drug EruptionsDokument11 SeitenDrug EruptionsAchmad Hariyanto100% (1)
- Cancer Metastasis LymphDokument785 SeitenCancer Metastasis LymphAlfred NgNoch keine Bewertungen
- Ukuran Hepar Lien Pada AnakDokument6 SeitenUkuran Hepar Lien Pada Anakivan ekoNoch keine Bewertungen
- Total Nasal Symptom ScoreDokument1 SeiteTotal Nasal Symptom ScoreLidia Shafiatul Umami100% (1)
- Lower Leg Anatomy: Volume 0%Dokument14 SeitenLower Leg Anatomy: Volume 0%zenik kusrini100% (1)
- Bad Habits That Can Hurt Your BrainDokument9 SeitenBad Habits That Can Hurt Your BrainTina MonroyNoch keine Bewertungen
- Conversation of Nurse With PatientDokument2 SeitenConversation of Nurse With PatientYola NoviyanaNoch keine Bewertungen
- Oral Rehabilitation Patient InjuriesDokument7 SeitenOral Rehabilitation Patient InjuriesAlexandru Codrin-IonutNoch keine Bewertungen
- Growth Hormone DeficiencyDokument11 SeitenGrowth Hormone DeficiencyIgor VasićNoch keine Bewertungen
- Inotropes and Vasopressors - Circulation. 2008Dokument11 SeitenInotropes and Vasopressors - Circulation. 2008Dani AguirreNoch keine Bewertungen
- Piezosurgery: By, Prathusha.U CRI Department of Public Health Dentistry Chettinad Dental CollegeDokument36 SeitenPiezosurgery: By, Prathusha.U CRI Department of Public Health Dentistry Chettinad Dental CollegePrathusha Umakhanth100% (1)
- Bhasa InggrisDokument23 SeitenBhasa InggrisrinaNoch keine Bewertungen