Beruflich Dokumente
Kultur Dokumente
Blood Type RBCs
Hochgeladen von
Prashant Madhukar KambleCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Blood Type RBCs
Hochgeladen von
Prashant Madhukar KambleCopyright:
Verfügbare Formate
Blood type
A blood type (also called a blood group) is a classification of blood based on the presence or absence of inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates, glycoproteins, orglycolipids, depending on the blood group system. Some of these antigens are also present on the surface of other types of cells of various tissues. Several of these red blood cell surface antigens can stem from one allele (or very closely linked genes) and collectively form a blood group system.[1] Blood types are inherited and represent contributions from both parents. A total of 32 human blood group systemsare now recognized by the International Society of Blood Transfusion (ISBT).[2] The two most important ones are ABO and the RhD antigen; they determine someone's blood type (A, B, AB and O, with + and - denoting RhD status). Many pregnant women carry a fetus with a blood type different from their own, and the mother can form antibodies against fetal RBCs. Sometimes these maternal antibodies are IgG, a small immunoglobulin, which can cross the placenta and causehemolysis of fetal RBCs, which in turn can lead to hemolytic disease of the newborncalled erythroblastosis fetalis, an illness of low fetal blood counts that ranges from mild to severe. Sometimes this is lethal for the fetus; in these cases it is called hydrops fetalis. [3]
Blood group systems[edit]
A complete blood type would describe a full set of 30 substances on the surface of RBCs, and an individual's blood type is one of many possible combinations of blood-group antigens.[2] Across the 30 blood groups, over 600 different blood-group antigens have been found,[4] but many of these are very rare, some being found mainly in certain ethnic groups. Almost always, an individual has the same blood group for life, but very rarely an individual's blood type changes through addition or suppression of an antigen ininfection, malignancy, or autoimmune disease.[5][6][7][8] Another more common cause in blood type change is a bone marrow transplant. Bone-marrow transplants are performed for many leukemias and lymphomas, among other diseases. If a person receives bone marrow from someone who is a different ABO type (e.g., a type A patient receives a type O bone marrow), the patient's blood type will eventually convert to the donor's type. Some blood types are associated with inheritance of other diseases; for example, the Kell antigen is sometimes associated with McLeod syndrome.[9] Certain blood types may affect susceptibility to infections, an example being the resistance to specific malaria species seen in individuals lacking the Duffy antigen.[10]The Duffy antigen, presumably as a result of natural selection, is less common in ethnic groups from areas with a high incidence of malaria.[11]
ABO blood group system[edit]
The ABO system is the most important blood-group system in human-blood transfusion. The associated anti-A and anti-B antibodies are usually immunoglobulin M, abbreviated IgM, antibodies. ABO IgM antibodies are produced in the first years of life by sensitization to environmental substances such as food, bacteria, [12] and viruses. The O in ABO is often called 0(zero, or null) in other languages.
Other blood group systems[edit]
Main article: Human blood group systems
32 blood-group systems have been identified, including the ABO and Rh systems.[16] Thus, in addition to the ABO antigens and Rh antigens, many other antigens are expressed on the RBC surface membrane. For example, an individual can be AB, D positive, and at the same time M and N positive (MNS system), K positive (Kell system), Lea or Leb negative (Lewis system), and so on, being positive or negative for each blood group system antigen. Many of the blood group systems were named after the patients in whom the corresponding antibodies were initially encountered.
Blood transfusion[edit]
Transfusion medicine is a specialized branch of hematology that is concerned with the study of blood groups, along with the work of a blood bank to provide atransfusion service for blood and other blood products. Across the world, blood products must be prescribed by a medical doctor (licensed physician or surgeon) in a similar way as medicines. Much of the routine work of a blood bank involves testing blood from both donors and recipients to ensure that every individual recipient is given blood that is compatible and is as safe as possible. If a unit of incompatible blood istransfused between a donor and recipient, a severe acute hemolytic reaction with hemolysis (RBC destruction), renal failure and shock is likely to occur, and death is a possibility. Antibodies can be highly active and can attack RBCs and bind components of the complement system to cause massive hemolysis of the transfused blood. Patients should ideally receive their own blood or type-specific blood products to minimize the chance of a transfusion reaction. Risks can be further reduced by cross-matching blood, but this may be skipped when blood is required for an emergency. Cross-matching involves mixing a sample of the recipient's serum with a sample of the donor's red blood cells and checking if the mixture agglutinates, or forms clumps. If agglutination is not obvious by direct vision, blood bank technicians usually check for agglutination with a microscope. If agglutination occurs, that particular donor's blood cannot be transfused to that particular recipient. In a blood bank it is vital that all blood specimens are correctly identified, so labelling has been standardized using a barcode system known as ISBT 128. The blood group may be included on identification tags or on tattoos worn by military personnel, in case they should need an emergency blood transfusion. Frontline German Waffen-SS had blood group tattoos during World War II. Rare blood types can cause supply problems for blood banks and hospitals. For example Duffy-negative blood occurs much more frequently in people of African origin,[19] and the rarity of this blood type in the rest of the population can result in a shortage of Duffy-negative blood for these patients. Similarly for RhD negative people, there is a risk associated with travelling to parts of the world where supplies of RhD negative blood are rare, particularly East Asia, where blood services may endeavor to encourage Westerners to donate blood.[20]
Red blood cell compatibility[edit]
Blood group AB individuals have both A and B antigens on the surface of their RBCs, and their blood plasma does not contain any antibodies against either A or B antigen. Therefore, an individual with type AB blood can receive blood from any group (with AB being preferable), but cannot donate blood to any group other than AB. They are known as universal recipients.
Blood group A individuals have the A antigen on the surface of their RBCs, and blood serum containing IgM antibodies against the B antigen. Therefore, a group A individual can receive blood only
from individuals of groups A or O (with A being preferable), and can donate blood to individuals with type A or AB.
Blood group B individuals have the B antigen on the surface of their RBCs, and blood serum containing IgM antibodies against the A antigen. Therefore, a group B individual can receive blood only from individuals of groups B or O (with B being preferable), and can donate blood to individuals with type B or AB.
Blood group O (or blood group zero in some countries) individuals do not have either A or B antigens on the surface of their RBCs, and their blood serum contains IgM anti-A and anti-B antibodies against the A and B blood group antigens. Therefore, a group O individual can receive blood only from a group O individual, but can donate blood to individuals of any ABO blood group (i.e., A, B, O or AB). If a patient in a hospital situation were to need a blood transfusion in an emergency, and if the time taken to process the recipient's blood would cause a detrimental delay, O Negative blood can be issued. They are known as universal donors.
Das könnte Ihnen auch gefallen
- Online BankingDokument5 SeitenOnline BankingPrashant Madhukar KambleNoch keine Bewertungen
- Prakash Amte: Early LifeDokument4 SeitenPrakash Amte: Early LifePrashant Madhukar Kamble50% (2)
- Chandra Ya AnDokument2 SeitenChandra Ya AnPrashant Madhukar KambleNoch keine Bewertungen
- Demat AccountDokument6 SeitenDemat AccountPrashant Madhukar KambleNoch keine Bewertungen
- Campus: Bharati Vidyapeeth Is A Group of Higher Educational Institutions, Established inDokument6 SeitenCampus: Bharati Vidyapeeth Is A Group of Higher Educational Institutions, Established inPrashant Madhukar KambleNoch keine Bewertungen
- Packaging and LabelingDokument7 SeitenPackaging and LabelingPrashant Madhukar KambleNoch keine Bewertungen
- Growing Cases of Crimes Among The YouthDokument26 SeitenGrowing Cases of Crimes Among The YouthPrashant Madhukar KambleNoch keine Bewertungen
- Demat AccountDokument6 SeitenDemat AccountPrashant Madhukar KambleNoch keine Bewertungen
- Creating New Jobs Is A Crucial Task and Plays An Important Role in The EconomyDokument2 SeitenCreating New Jobs Is A Crucial Task and Plays An Important Role in The EconomyPrashant Madhukar KambleNoch keine Bewertungen
- Environments Natural Resource Biodiversity Geodiversity EcosystemsDokument1 SeiteEnvironments Natural Resource Biodiversity Geodiversity EcosystemsPrashant Madhukar KambleNoch keine Bewertungen
- Mother TeresaDokument3 SeitenMother TeresaPrashant Madhukar KambleNoch keine Bewertungen
- A New Vision For HumanityDokument1 SeiteA New Vision For HumanityPrashant Madhukar KambleNoch keine Bewertungen
- Pratap GadDokument3 SeitenPratap GadPrashant Madhukar KambleNoch keine Bewertungen
- John Logie BairdDokument3 SeitenJohn Logie BairdPrashant Madhukar KambleNoch keine Bewertungen
- Growing Cases of Crimes Among The YouthDokument8 SeitenGrowing Cases of Crimes Among The YouthPrashant Madhukar KambleNoch keine Bewertungen
- Corruption in IndiaDokument11 SeitenCorruption in IndiaPrashant Madhukar KambleNoch keine Bewertungen
- Curriculum Vitae: Dhundppa Machindra Bansode AddressDokument1 SeiteCurriculum Vitae: Dhundppa Machindra Bansode AddressPrashant Madhukar KambleNoch keine Bewertungen
- Main Problems and Future Prospects of Small Scale Industries in IndiaDokument7 SeitenMain Problems and Future Prospects of Small Scale Industries in IndiaPrashant Madhukar KambleNoch keine Bewertungen
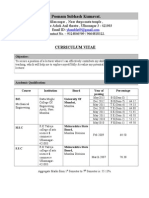
- Curriculum Vitae: Name Contact No Email ID AddressDokument2 SeitenCurriculum Vitae: Name Contact No Email ID AddressPrashant Madhukar KambleNoch keine Bewertungen
- Sneha SG TeachingDokument2 SeitenSneha SG TeachingPrashant Madhukar KambleNoch keine Bewertungen
- Campus: Bharati Vidyapeeth Is A Group of Higher Educational Institutions, Established inDokument6 SeitenCampus: Bharati Vidyapeeth Is A Group of Higher Educational Institutions, Established inPrashant Madhukar KambleNoch keine Bewertungen
- Curriculum Vitae: B-306 LAXMIRAJ, Pandurangwadi, Manpada Road, Dombivali - East Mumbai PHONE NO: 09967354531,09969799771Dokument2 SeitenCurriculum Vitae: B-306 LAXMIRAJ, Pandurangwadi, Manpada Road, Dombivali - East Mumbai PHONE NO: 09967354531,09969799771Prashant Madhukar KambleNoch keine Bewertungen
- Poonam Subhash Kuma VatDokument2 SeitenPoonam Subhash Kuma VatPrashant Madhukar KambleNoch keine Bewertungen
- Albin Abraham Fresher Be MechDokument2 SeitenAlbin Abraham Fresher Be MechPrashant Madhukar KambleNoch keine Bewertungen
- Babasaheb Gawde Institute of Management Studies (Bgims) : Shende Chetan SharadDokument2 SeitenBabasaheb Gawde Institute of Management Studies (Bgims) : Shende Chetan SharadPrashant Madhukar KambleNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- LMGT Trans 1Dokument1 SeiteLMGT Trans 1Christian L. TolentinoNoch keine Bewertungen
- Brosur LabkesdaDokument1 SeiteBrosur Labkesdael_karimahNoch keine Bewertungen
- Blood LecturesDokument128 SeitenBlood LecturessrhrenaissanceNoch keine Bewertungen
- Blood Typing and GeneticsDokument22 SeitenBlood Typing and GeneticsJalajarani Aridass0% (1)
- Patho Physiology Lecture13Dokument10 SeitenPatho Physiology Lecture13Manar AlzobiNoch keine Bewertungen
- Production of Platelet CountsDokument9 SeitenProduction of Platelet CountsJack KayatNoch keine Bewertungen
- Red Blood Cells Lecture 4Dokument33 SeitenRed Blood Cells Lecture 4Panashe MawaroNoch keine Bewertungen
- 15 - Toronto Notes 2011 - HematologyDokument58 Seiten15 - Toronto Notes 2011 - HematologyWaiwit Chotchawjaru100% (1)
- BIOL 102 - Group Activity #2Dokument8 SeitenBIOL 102 - Group Activity #2Abhi RajNoch keine Bewertungen
- Operator Loadout for Arid EnvironmentsDokument11 SeitenOperator Loadout for Arid EnvironmentsJustus WeißeNoch keine Bewertungen
- PHYSIOLOGY OF BLOOD: FUNCTIONS, COMPOSITION AND RED BLOOD CELLSDokument23 SeitenPHYSIOLOGY OF BLOOD: FUNCTIONS, COMPOSITION AND RED BLOOD CELLSmiknayrb galdianoNoch keine Bewertungen
- Blood BiochemistryDokument124 SeitenBlood BiochemistrySohail AhamdNoch keine Bewertungen
- Practical HaematologyDokument70 SeitenPractical HaematologyMustafa Khandgawi100% (1)
- Seminar: Faizan Khan, Tobias Tritschler, Susan R Kahn, Marc A RodgerDokument14 SeitenSeminar: Faizan Khan, Tobias Tritschler, Susan R Kahn, Marc A RodgerJuan Camilo Morales TabordaNoch keine Bewertungen
- Immunohematology ASCPi Review Booklet (Part 1)Dokument22 SeitenImmunohematology ASCPi Review Booklet (Part 1)Mark Justin OcampoNoch keine Bewertungen
- RBC and WBC Identification Under MicroscopeDokument7 SeitenRBC and WBC Identification Under MicroscopeHriday jyoti DekaNoch keine Bewertungen
- Grafik QC Hematologi 2023 BaruDokument125 SeitenGrafik QC Hematologi 2023 BaruSyifa nurfitriNoch keine Bewertungen
- 01 - Blood-Function and CompositionDokument45 Seiten01 - Blood-Function and Compositionsylvester GelacNoch keine Bewertungen
- Hematology Analyzers, Coagulation Systems Product GuideDokument4 SeitenHematology Analyzers, Coagulation Systems Product GuideElvan Dwi WidyadiNoch keine Bewertungen
- Composition and Function of BloodDokument4 SeitenComposition and Function of BloodDevendra RawatNoch keine Bewertungen
- Blood: MR Marudhar Associate Professor Nims UniversityDokument67 SeitenBlood: MR Marudhar Associate Professor Nims UniversityDr-Marudhar MarudharNoch keine Bewertungen
- Ins Thrombotimer2Dokument32 SeitenIns Thrombotimer2Med Rachid ZianiNoch keine Bewertungen
- CTK-USA (Aria) : End User Price List-Rapid TestDokument2 SeitenCTK-USA (Aria) : End User Price List-Rapid TestAbdalazeez AlsayedNoch keine Bewertungen
- Coagulation DisordersDokument40 SeitenCoagulation DisordersDr. Shatdal Chaudhary100% (6)
- Management of Hypovolemic Shock FinalDokument13 SeitenManagement of Hypovolemic Shock FinalDrGarikipati Krishna VenuNoch keine Bewertungen
- Rules of 3 Jeri Walters Knoxville 2015Dokument26 SeitenRules of 3 Jeri Walters Knoxville 2015pieterinpretoria391Noch keine Bewertungen
- Complete Blood Count ReportDokument5 SeitenComplete Blood Count ReportVikas VermaNoch keine Bewertungen
- Innovative Teaching Manual Innovative Teaching Manual Innovative Teaching Manual Innovative Teaching Manual Innovative Teaching ManualDokument8 SeitenInnovative Teaching Manual Innovative Teaching Manual Innovative Teaching Manual Innovative Teaching Manual Innovative Teaching ManualgeethaNoch keine Bewertungen
- Clinical Guidelines For The Use of Granulocyte TransfusionsDokument13 SeitenClinical Guidelines For The Use of Granulocyte Transfusionssm19790% (1)
- A PTTDokument15 SeitenA PTTHendra SshNoch keine Bewertungen