Beruflich Dokumente
Kultur Dokumente
Psoas Abscess: A Diagnostic Dilemma
Hochgeladen von
Mega MuzdalifahOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Psoas Abscess: A Diagnostic Dilemma
Hochgeladen von
Mega MuzdalifahCopyright:
Verfügbare Formate
A Case Report & Literature Review
Psoas Abscess: A Diagnostic Dilemma
Nabil A. Ebraheim, MD, Jason D. Rabenold, MD, Vishwas Patil, MD, and Christopher G. Sanford, BS
liopsoas muscles are located in the retrofascial space, which lies between the transversalis fascia and the posterior psoas fascia.1 Abscesses of the iliopsoas result most commonly from osseous sources, such as the spine, ileum, and sacroiliac joint. They seldom arise from pyomyositis, trauma, lymphatic spread, or puerperal infections. Immunocompromised patients and drug users are particularly susceptible.
...hip is flexed and has a limited and painful range of motion that diverts attention from the abdominal or pelvic source of the abscess.2
Iliopsoas abscess may initially present with signs and symptoms in the buttock, hip, or thigh. Such signs and symptoms may be obscure, nonspecific, and misleading.1 Diagnosis is often overlooked, as a patient lies supine and refuses to move or resists being turned for examination. With psoas involvement, the hip is flexed and has a limited and painful range of motion that diverts attention from the abdominal or pelvic source of the abscess.2 Pain is referred along the distribution of the gluteal or obturator nerves or along the distribution of the lumbar and sacral nerve roots, thus directing attention elsewhere.2 The abscess may also be overlooked given the deep location of the iliopsoas muscle.3 Iliopsoas abscess is best detected through use of computed tomography (CT), which defines its pathway and allows for appropriate surgical treatment.
AND RESULTS Case 1 A 30-year-old man was admitted after being an inpatient at an outlying facility for several weeks. Hospitalization was for left hip pain caused when the man was struck by
Dr. Ebraheim is Professor and Chair, Dr. Rabenold is Resident, Dr. Patil is Research Associate, and Mr. Sanford is Research Assistant, Department of Orthopaedic Surgery, University of Toledo Medical Center, Toledo, Ohio. Requests for reprints: Vishwas Patil, MD, Department of Orthopaedic Surgery, University of Toledo Medical Center, 3000 Arlington Ave, Toledo, OH 43614 (tel, 419-383-4553; fax, 419383-3526; e-mail, vishwasorth@yahoo.com). Am J Orthop. 2008;37(1):E11-E13. Copyright HealthCom Inc. 2008. All rights reserved. Quadrant
a board in the left groin area 3 months earlier. There was a question of pelvic fracture. On admission, pelvic CT showed large psoas and iliacus muscles extending into the pelvis (Figure 1). CT with contrast injection revealed cystic changes in the acetabulum superiorly. X-rays revealed severe joint space narrowing superiorly. On admission, the patient was taken to the operating room, where he underwent excisional dbridement of a left psoas abscess of the left hip with excisional dbridement of the femoral head (Girdlestone procedure). After 9 days, a pelvic CT scan revealed shrinkage of the psoas. There was also no intraperitoneal, bladder, or prostate involvement. Throughout his hospitalization, the patient received 4 more irrigations and excisional dbridement operations on the left hip and psoas wounds. After 17 days, there was no apparent loculated abscess. The left psoas muscle appeared somewhat larger, as did the left gluteal muscles. The patient was discharged with the left leg nonweightbearing. He was given ampicillin/sulbactam and levofloxacin during the course of his stay. There was no recurrence, and all wounds were healed by secondary wound repair at time of last follow-up (6 months). Case 2 A woman in her late 20s with psoas infection was transferred from an outlying facility. Seven months before admission, she had a laparoscopic cholecystectomy. After CT-guided drainage, which grew methicillin-resistant Staphylococcus aureus, her pain continued. CT scan revealed a large abscess extending to the pelvis, with erosive changes to the ilium and sacroiliac joint. A large flank abscess was seen extending around the iliac wing, mostly subcutaneous and involving the iliopsoas and gluteal muscles (Figure 2). The patient underwent a 2-incision approach for drainage of the abscess and dbridement of destroyed iliac bone. The next day, an abdomen and pelvic CT scan with contrast showed no residual fluid collection. During her hospitalization, the patient had 2 additional irrigation and dbridement operations. The patient was discharged on linezolid with dressing changes and weight-bearing as tolerated. Wounds healed by secondary closure, with no complaints at last follow-up (11 months). Case 3 A man in his late 30s with increasing hip pain was transferred from an outlying facility. He had cardiac catheterization 3 months earlier and shortly after was hospitalized for a few days with right groin pain. At that time, CT scan January 2008 E11
METHODS
Psoas Abscess: A Diagnostic Dilemma
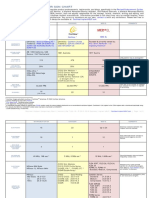
Figure 2. In case 2, (A) computed tomography (CT) scan obtained on admission showed large flank abscess extending around iliac wing, mostly subcutaneous and involving the gluteal muscles. (B) CT scan obtained 1 day after dbridement revealed no residual fluid collection.
C
Figure 1. In case 1, computed tomography (CT) scans obtained on admission revealed (A) large inflamed psoas muscle extending into pelvis and (B) very large inflamed iliacus muscle extending into pelvis. (C) CT scan obtained 17 days later revealed no obvious loculated fluid collection. Left psoas and gluteal muscles appeared somewhat larger.
A of the abdomen and pelvis with contrast revealed no retroperitoneal or intramuscular hematoma. The patient had previously had lumbar spine laminectomy with hardware fusion as well. Duration of the left hip pain was approximately 2.5 months. The patient could not bear weight on the left leg because of severe pain. CT scans from an outside facility on admission indicated enlargement of the iliopsoas muscles as well as soft-tissue enlargement extending to the hip and proximal femur (Figure 3). During hospitalization, the patient was taken to the operating room, where he underwent excisional dbridement of the left psoas as well as left hip arthrotomy with excisional dbridement. Cultures revealed left hip osteomyelitis with methicillin-sensitive S aureus. Five days later, he underwent irrigation and excisional dbridement of the femoral head (Girdlestone procedure) with insertion of antibiotic-loaded cement spacer and closure of the hip wound over drains with packing of the iliac wound. CT scan 10 days after initial drainage and 5 days after excisional dbridement of the femoral head showed a large iliopsoas muscle. Two additional irrigation and dbridement operations of the left iliac wound were performed during hospitalization. The patient was discharged on cefotaxime, weight-bearing as tolerated, and wound vacuum-assisted closure. He underwent total hip arthroplasty and had no complications at time of last follow-up (29 months).
Figure 3. In case 3, (A) computed tomography (CT) scan obtained on admission showed enlarged inflamed iliopsoas muscles. (B) Coronal CT scan obtained on admission showed soft-tissue enlargement of the iliopsoas extending to the hip and proximal femur. (C) CT scan obtained on admission revealed enlarged inflamed iliopsoas muscle. (D) CT scan obtained 10 days after initial drainage (5 days after excisional dbridement of femoral head) showed large iliopsoas muscle.
DISCUSSION The iliopsoas muscle complex extends from the edges of the 12th thoracic vertebra to the 5th lumbar vertebra and the lesser trochanter of the femur and is a direct posterior relation of many of the abdominal and retroperitoneal viscera.4 The psoas muscle has a rich vascular supply that
E12 The American Journal of Orthopedics
is believed to predispose it to hematogenous spread from sites of occult infection. In 70% of people, it is a single structure (psoas major), but 30% also have a psoas minor muscle, which lies anterior to the psoas major along the same course.5 Symptoms are often nonspecific. Patients may present with fever, flank pain, abdominal pain, or limp. Other symptoms are nausea, malaise, and weight loss.5 Because psoas abscesses are difficult to diagnose, a through medical history of the patient and a good physical examination are critical for prompt diagnosis of psoas abscess. Abscess formation promptly requires surgical drainage before antibiotic therapy.3 For orthopedic surgeons, iliac-crest apophyseal-splitting incision is an easy, direct, and familiar procedure. This approach allows excellent drainage of psoas and iliacus abscesses and drainage of ilium, sacrum, and sacroiliac joint. Drainage of the abscess is not sufficient, and radi-
N. A. Ebraheim et al
THE ROLE
OF ImAGING IN DIAGNOSIS AND TrEATmENT
CT is the method of choice for abscess detection, though ultrasonography and magnetic resonance imaging are also useful. Ultrasonography is diagnostic in only 60% of cases of psoas abscess, compared with 80% to 100% for CT.6,7 Ultrasonography is influenced by body habitus and gaseous bowel distension and is operator-dependent. Magnetic resonance imaging, radionuclide imaging, and positron emission tomographic imaging have all been used in evaluating psoas abscess, though the negative cost implications and lack of ready availability make it difficult to identify any advantage over CT scanning.4 Both CT and ultrasonography allow for guided percutaneous needle aspiration and drainage.8 CT defines the extrapelvic pathway of spread and allows for appropriate surgical excision drainage at the gluteal area and/or about the proximal femur and hip joint.1 The most common CT feature of an abscess is usually a focal hypodense lesion within a larger muscle.9 Lenchik and colleagues10 reported low attenuation in 100% of their abscesses, but this sign also can be seen in neoplasms and hematomas. Margination of the abscesses can be variable. Rounded, smooth collections conforming to the configuration of the involved muscles with enhancement of the rim of the abscess wallthe so called rind signcan be present.4,11 Less frequently, infiltration of the surrounding fat and irregular margins of the lesion are found. When CT findings are assessed, the clinical setting can differentiate inflammatory, neoplastic, and hemorrhagic conditions of the iliopsoas muscle.9 Presence of gas bubbles or airfluid level is regarded as more specific for an abscess, though gas has been reported in neoplasms.12 Multiloculated lesions can also be found. cal excision of all necrotic tissue should be performed. Eradication of the bone and soft-tissue infection requires several operations. Postoperative antibiotics are obligatory and are adapted individually. Most patients experience full recovery with no continuing sequelae.3 However, there is the possibility of residual effects, such as osteomyelitis of adjacent bones, scarring of muscle, weakness, functional impairment, and a depression at the infection site.3 Summary of the 3 Cases All 3 of the patients described here were referred to us from outside institutions. In each case, pretreatment CT scans revealed substantial abscess collection formations. Three months earlier, 1 patient underwent heart catheterization
through the groin, with concern shortly thereafter of retroperitoneal or intramuscular hematoma. At the time, this was investigated with CT scan and was shown to be negative. This patient also had previous lumbar spine laminectomy with hardware fusion. A different patient underwent laparoscopic cholecystectomy 7 months earlier, and the third had recent trauma about the groin, with questionable pelvic fracture. All 3 patients had a 2-incision excisional drainage approach (1 iliac-crest apophyseal-splitting incision, 1 gluteal/hip incision). In 2 patients, excisional dbridement of the femoral head was necessary. One patient had previous CT-guided abscess drainage that failed to control the problem.
CONCLUSIONS Although iliopsoas abscess presents unclear signs and symptoms, often in the lower extremities, CT can aid in evaluating and diagnosing the abscess. Once the abscess is detected, successful treatment should include surgical drainage as well as excision of all existing necrotic tissue. Determinants of success include early diagnosis, complete drainage, and proper antibiotic use. AUTHOrS DISCLOSUrE STATEmENT REFErENCES
The authors report no actual or potential conflict of interest in relation to this article.
1. Ebraheim NA, Havel PE, Jackson WT. CT detection of intrapelvic origin of lower extremity infections in traumatized limbs. J Orthop Trauma. 1988;1(4):306-311. 2. Simons GW, Sty JR, Starshak RJ. Retroperitoneal and retrofascial abscesses. A review. J Bone Joint Surg Am. 1983;65(8):1041-1058. 3. Bickels J, Ben-Sira L, Kessler A, Wientroub S. Primary pyomyositis. Current concepts review. J Bone Joint Surg Am. 2002;84(12):22772286. 4. Garner JP, Meiring PD, Ravi K, Gupta R. Psoas abscessnot as rare as we think? Colorectal Dis. 2007;9(3):269-274. 5. Taiwo B. Psoas abscess: a primer for the internist. South Med J. 2001;94(1):2-5. 6. Ricci MA, Meyer KK. Psoas abscess complicating Crohns disease. Am J Gastroenterol. 1985;80(12):970-977. 7. Desandre A, Cottone F, Evers M. Iliopsoas abscess: etiology, diagnosis and treatment. Am Surg. 1995;61(12):1087-1091. 8. Cantasdemir M, Kara B, Cebi D, Selcuk ND, Numan F. Computed tomographyguided percutaneous catheter drainage of primary and secondary iliopsoas abscesses. Clin Radiol. 2003;58(10):811-815. 9. Zissin R, Gayer G, Kots E, Werner M, Shapiro-Feinberg M, Hertz M. Iliopsoas abscess: a report of 24 patients diagnosed by CT. Abdom Imaging. 2001;26(5):533-539. 10. Lenchik L, Dovgan DJ, Kier R. CT of the iliopsoas compartment: value in differentiating tumor, abscess, and hematoma. AJR Am J Roentgenol. 1994;162(1):83-86. 11. Ralls PW, Boswell W, Henderson R, Rogers W, Boger D, Halls J. CT of inflammatory disease of the psoas muscle. AJR Am J Roentgenol. 1980;134(4):767-770. 12. Feldberg MA, Koehler PR, van Waes PF. Psoas compartment disease studied by computed tomography. Radiology. 1983;148(2):505-512.
January 2008 E13
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- CraniotomyDokument10 SeitenCraniotomyUzma KhanNoch keine Bewertungen
- 40th Annual Percivall Pott Scientific MeetingDokument26 Seiten40th Annual Percivall Pott Scientific MeetingAlex Mulligan100% (1)
- Soal Tes PpdsDokument14 SeitenSoal Tes PpdsDuas Jourgie100% (1)
- Introduction To IT ITeS Industry Class 9 Questions and Answers - CBSE Skill EducationDokument11 SeitenIntroduction To IT ITeS Industry Class 9 Questions and Answers - CBSE Skill EducationAarav SakpalNoch keine Bewertungen
- Magnetic Resonance Spectroscopy and Its Clinical Applications: A ReviewDokument21 SeitenMagnetic Resonance Spectroscopy and Its Clinical Applications: A Reviewale saenzNoch keine Bewertungen
- Mastermind: WorksheetDokument25 SeitenMastermind: WorksheetMilka RahmanNoch keine Bewertungen
- LCP Extra-Articular Distal Humerus PlateDokument24 SeitenLCP Extra-Articular Distal Humerus PlateLuka DamjanovicNoch keine Bewertungen
- Carte RMN PDFDokument14 SeitenCarte RMN PDFLilianaGiogîrdacNoch keine Bewertungen
- SCHIZAS Qualitative GradingDokument6 SeitenSCHIZAS Qualitative GradingDitaAnggaraKusumaNoch keine Bewertungen
- QuestionsDokument21 SeitenQuestionsashaaman0325Noch keine Bewertungen
- Langerhans Cell Histiocytosis (LCH) : Guidelines For Diagnosis, Clinical Work-Up, and Treatment For Patients Till The Age of 18 YearsDokument10 SeitenLangerhans Cell Histiocytosis (LCH) : Guidelines For Diagnosis, Clinical Work-Up, and Treatment For Patients Till The Age of 18 Yearsadrian Morales PeraltaNoch keine Bewertungen
- Imaging MethodsDokument63 SeitenImaging MethodsYlrebmik ArrabiNoch keine Bewertungen
- Equipments of Modern Imaging ModalitiesDokument4 SeitenEquipments of Modern Imaging Modalitiescoordinator.dargaiNoch keine Bewertungen
- Imaging in Avascular Necrosis of The Femoral HeadDokument44 SeitenImaging in Avascular Necrosis of The Femoral Headmichaelhtun100% (1)
- Informed Consent For Mri: PATIENT NAMEDokument1 SeiteInformed Consent For Mri: PATIENT NAMEyulia anggreniNoch keine Bewertungen
- Update On Neuroimaging For Categorization of Parkinson's Disease and Atypical ParkinsonismDokument11 SeitenUpdate On Neuroimaging For Categorization of Parkinson's Disease and Atypical ParkinsonismYo MismoNoch keine Bewertungen
- MS Rle ExamssDokument69 SeitenMS Rle ExamssSSA CommissionNoch keine Bewertungen
- Master Thesis MriDokument8 SeitenMaster Thesis Mriafknoaabc100% (2)
- The Joint Commission - Proposed Standards Changes For Diagnostic Imaging ServicesDokument14 SeitenThe Joint Commission - Proposed Standards Changes For Diagnostic Imaging ServicesaegysabetterwayNoch keine Bewertungen
- Excite1 5TDokument43 SeitenExcite1 5TTihomir DrenovskiNoch keine Bewertungen
- 2022 - Bedside Ultrasound For Ventricular Size Monitoring in Patients With PEEK Cranioplasty - A Preliminary Experience of Technical Feasibility in Neurotrauma SettingDokument9 Seiten2022 - Bedside Ultrasound For Ventricular Size Monitoring in Patients With PEEK Cranioplasty - A Preliminary Experience of Technical Feasibility in Neurotrauma SettingRosi MontesNoch keine Bewertungen
- QRG - Mri AbdomenDokument2 SeitenQRG - Mri AbdomenKhairunNisaNoch keine Bewertungen
- Entero SequencesDokument12 SeitenEntero SequencesKelvin SueyzyNoch keine Bewertungen
- Cochlear Implant Comparison Chart: 16 CFR Part 255 Revised Endorsement GuidesDokument9 SeitenCochlear Implant Comparison Chart: 16 CFR Part 255 Revised Endorsement GuidesLong An DoNoch keine Bewertungen
- European MP and E Conference - ProceedingsDokument377 SeitenEuropean MP and E Conference - ProceedingsEduardoHernandezNoch keine Bewertungen
- Specs OnI 0.36T Open MRI (China)Dokument10 SeitenSpecs OnI 0.36T Open MRI (China)Юрий ФоминNoch keine Bewertungen
- ProKnow CAP Hippocampus 20181113 PDFDokument16 SeitenProKnow CAP Hippocampus 20181113 PDFAna Paula IoostNoch keine Bewertungen
- SWOT Analysis Applied To Hybrid PDFDokument318 SeitenSWOT Analysis Applied To Hybrid PDFCarlos Alberto de MendonçaNoch keine Bewertungen
- Articulo EpitimpanoDokument8 SeitenArticulo EpitimpanoFabian Camelo OtorrinoNoch keine Bewertungen
- Ashutosh VermaDokument114 SeitenAshutosh VermaMaster PrintersNoch keine Bewertungen