Beruflich Dokumente
Kultur Dokumente
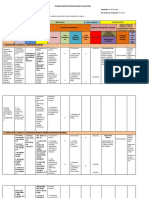
Revenue Cycle
Hochgeladen von
casti134Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Revenue Cycle
Hochgeladen von
casti134Copyright:
Verfügbare Formate
The Health Care
Revenue Cycle
How Money is Generated for the
Business of Health Care Delivery
Robert A. Kaplan BA, DC, MBA, CPAT
Finney Learning Systems, Inc.
205 West 54
th
Street
New York, NY 10019
(212) 757-4788
www.TheRightWay.com
FLS@TheRightWay.com
Copyright 2009, Finney Learning Systems, Inc.
All rights reserved. No part of this publication may be reproduced or distributed in any
form or by any means, electronic, mechanical, photocopying, recording or otherwise, or
stored in a database or retrieval system without the permission in writing of the publisher.
Every effort has been made to supply complete and accurate information. However, Finney
Learning Systems, Inc. does not guarantee the accuracy or completeness of any information
and assumes no responsibility for its use.
ISBN 1-56435-201-3
10 9 8 7 6 5 4 3 2 1
Publisher: Doug Finney
Editor: John Upham
Page Layout: Zach Katagiri
Cover Design: Sandy Krasovec
Book Design: Kevin Cochran, Zachary Aaron
Finney Learning Systems i
Contents
Welcome ..........................................................................................................v
Chapter 1 - Health Care Plans and Legislation
The Health Care Insurance Industry .............................................................................. 2
Health Care Plans .......................................................................................................... 2
Figure 1: Health Care Plans ............................................................................. 2
Indemnity ........................................................................................................ 3
Managed Care Organization (MCO) ............................................................... 3
Important Defnitions .................................................................................................... 5
Physicians Identifcation Numbers .............................................................................. 6
The Major Players .......................................................................................................... 7
Figure 2: The Major Players ............................................................................. 8
The Department of Health and Human Services (DHHS) .............................. 9
The Centers for Medicare and Medicaid Services (CMS) ................................ 9
Medicare ........................................................................................................ 10
Medicaid ........................................................................................................ 11
Civil Monetary Penalties Law (CMP) ........................................................... 12
State Childrens Health Insurance Program (SCHIP) .................................... 12
Balanced Budget Act of 1997 (BBA) ............................................................... 12
Tax Equity and Fiscal Responsibility Act of 1982 (TEFRA) ............................ 12
Defcit Reduction Act of 1984 (DEFRA) ......................................................... 12
Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) ...... 13
Omnibus Budget Reconciliation Act of 1986 (OBRA of 1986) ....................... 13
Omnibus Budget Reconciliation Act of 1989 (OBRA of 1989) ........................ 13
Omnibus Budget Reconciliation Act of 1990 (OBRA of 1990) ........................ 14
Operation Restore Trust of 1995 (ORT) .......................................................... 14
Other Players ............................................................................................................... 14
Health Insurance Portability and Accountability Act of 1996 (HIPAA) ......... 15
National Electronic Data Interchange (EDI) .................................................. 16
Medical Ethics; Fraud and Abuse; Professional Liability............................... 18
False Claims Act (FCA) .................................................................................. 20
Emergency Medical Treatment and Active Labor Act (EMTALA) ................. 21
Patient Bill of Rights ...................................................................................... 22
Quality Improvement Organizations (QIO) .................................................. 22
Understanding Acronyms and Abbreviations ............................................................. 23
Test Taking and Study Strategies ................................................................................. 27
Beware of Pitfalls with Multiple Choice Questions ....................................... 28
Sample Test Questions ................................................................................................. 29
Chapter 2 - Contact with Hospitals and Doctors
Patient Registration, Admission, and Financial Concerns ........................................... 50
Figure 3: Hospital Registration ...................................................................... 50
Registration ................................................................................................... 51
Responsibilities of the Registration Staff ....................................................... 52
Patients Interaction with the Hospital .......................................................... 52
Affliated Health Coverage Protocols ............................................................ 53
Physician Direct Services ............................................................................... 53
The Clean Claim and the Hospital Registration Staff .................................... 53
Financial Counselor ....................................................................................... 55
Summary ....................................................................................................... 55
Effective Patient Scheduling .......................................................................... 57
Advantages of Pre-Admitting Patients .......................................................... 57
Disadvantages of Pre-Admitting Patients ..................................................... 58
The Five Control Points ................................................................................. 59
Pre-Certifcation ............................................................................................ 59
The Health Care Revenue Cycle ii
Medical Case Management/Utilization Review ........................................... 60
Important Criteria for Registering Patients with Managed Care Coverage ... 60
Consent .......................................................................................................... 60
Hospital Admitting Categories .................................................................................... 62
Figure 4: Hospital Admitting Categories ....................................................... 62
Categories of Health Care Charges ................................................................ 63
Categories of Health Care Delivered to the Consumer .................................. 64
Health Care Coverage in the Military .......................................................................... 65
Figure 5: Health Care Coverage in the Military ............................................. 65
CHAMPVA ................................................................................................... 66
TRICARE ....................................................................................................... 66
Defense Enrollment Eligibility Reporting System (DEERS). .......................... 68
Continued Health Care Beneft Program (CHCBP) ....................................... 68
Medicare Determination of Patient Eligibility ............................................................. 69
Medical Spell of Illness .................................................................................. 69
Hospital Inpatient Beneft Days Coverage .................................................... 69
Skilled Nursing Facility Coverage (SNF) ....................................................... 69
Advanced Benefciary Notice (ABN) ............................................................. 70
Medicare Secondary Payer (MSP)/Working Aged Provision ........................ 70
The Medical Staff and Hospital Admitting Protocols................................................... 71
Patient Confdentiality: Privacy Act of 1974 .................................................. 72
The Patients Medical Record and Telephone/Verbal Communication in the
Hospital ..................................................................................................... 72
Patient Self-Determination Act (PSDA) ......................................................... 73
Figure 6: OBRA 1990 ...................................................................................... 74
The Joint Commission on Accreditation of Health Care Organizations ........ 74
Census .......................................................................................................................... 76
Average Daily Census ................................................................................... 77
Percentage of Occupancy ............................................................................... 77
Generally Accepted Accounting Principles (GAAP) .................................................... 78
Understanding Acronyms and Abbreviations ............................................................. 79
More Test Taking Strategies ......................................................................................... 81
Sample Test Questions ................................................................................................ 82
Chapter 3 - Processing Procedures
UB-04 Claim Form ..................................................................................................... 100
Important UB-04 Code/FL Defnitions ........................................................ 101
Completion of the #4 Form Locator in the UB-04 ........................................ 104
Common Working File ............................................................................................... 107
Medicare Processing of the UB-04 Claim Form .......................................................... 108
Claim Form Processing Terminology........................................................... 110
Medicare Secondary Payer .......................................................................... 112
MS-DRGs. ................................................................................................... 114
Medicare DRG Window (The 72-Hour Rule) ............................................... 115
Chargemaster ............................................................................................ 116
Figure 7: Chargemaster ................................................................................ 117
Medicare Deductibles, Co-Payments and Co-Insurances for 2010 ............................. 118
Electronic Billing ........................................................................................................ 119
Types of Financial Statements .................................................................................... 120
Abbreviations and Acronyms .................................................................................... 121
Sample Test Questions ............................................................................................... 123
Chapter 4 - Claim Form for the Doctors Ofce
Medicare .................................................................................................................... 138
Medigap ...................................................................................................... 140
Medical Unlikely Edits (MUE)..................................................................... 140
Finney Learning Systems iii
National Correct Coding Initiative (NCCI) ................................................. 141
Advanced Benefciary Notice (ABN) ........................................................... 142
Comprehensive Error Rate Testing (CERT) ................................................. 143
Recovery Audit Contractors (RAC) ............................................................. 143
Ambulatory Payment Classifcation (APC) ................................................ 143
Medical Necessity ........................................................................................ 145
Medical Standards of Care and Malpractice ................................................ 146
Medical Malpractice .................................................................................... 146
Waiver of Liability ...................................................................................... 146
Clinical Laboratory Improvement Amendment (CLIA) .............................. 148
Health Insurance Claim Number (HICN) ................................................... 148
Medicaid ...................................................................................................... 149
Resource Based Relative Value Scale (RBRVS) ............................................. 149
The CMS-1500 Claim Form ....................................................................................... 151
How to Complete the CMS-1500 Claim Form ............................................ 152
International Classifcation of Diseases ...................................................................... 160
Figure 8: ICD ............................................................................................... 161
Current Procedural Terminology ............................................................................... 165
Figure 9: CPT ............................................................................................... 166
Health Care Common Procedure Coding System (HCPCS) ...................................... 167
Evaluation and Management Services (E/M) .............................................. 167
SOAP Notes and the Patient-Oriented Medical Records (POMR) .............. 169
Defnitions: Types of Third Party Reimbursement and Categories .....................
of Providers .............................................................................................. 170
Abbreviations and Acronyms .................................................................................... 171
Sample Test Questions ............................................................................................... 173
Chapter 5 - Doctor/Hospital Financial Matters
Medical Identity Theft ............................................................................................... 190
Tips for Preventing and Detecting Medical Identity Theft .......................... 190
Responding to Medical Identity Theft ......................................................... 191
Third Party Collection Activity .................................................................................. 192
Bankruptcy ................................................................................................................. 193
Figure 10: Bankruptcy.................................................................................. 193
Involuntary Bankruptcy .............................................................................. 194
The Bankruptcy Abuse Prevention and Consumer Protection Act of 2005 .. 195
Confrming Bankruptcy by the Doctor or Hospital ..................................... 195
Notifcation of Bankruptcy .......................................................................... 195
Discharge of Debtor ..................................................................................... 196
Dismissal of Bankruptcy .............................................................................. 196
Collection Regulations of the Federal Government ................................................... 197
The Truth in Lending Act (TLA) (1969). ...................................................... 197
Fair Debt Collection Practices Act (FDCPA) (1978) ..................................... 197
Fair Credit Billing Act (1975) ....................................................................... 198
Fair Credit Reporting Act (FCRA) (1971) .................................................... 199
Fair and Accurate Credit Transaction Act (includes SKIP) .......................... 199
Equal Credit Opportunity Act (ECOA) ....................................................... 200
Deceased Patient Notifcation ...................................................................... 200
General Accounting Principles Applied to Cashier Functions..................... 201
Effective Collection Policies ......................................................................... 201
Statute of Limitations .................................................................................. 202
Collection Calls to the Patient and Collection Policies ................................ 202
Third Party Collection Agencies .................................................................. 202
Charity Care, Indigent Patient, and Bad Debt ............................................. 203
Judgment, Lien and Tort Liability ................................................................ 203
The Health Care Revenue Cycle iv
Courtesy Discharge ..................................................................................... 203
Abbreviations and Acronyms .................................................................................... 206
Sample Test Questions ............................................................................................... 207
Appendix A: CMS-1500 Form .................................................................................... 221
Appendix B: UB-04 Form ........................................................................................... 222
Appendix C: Superbill ............................................................................................... 223
Appendix D: Medicare Card ...................................................................................... 224
Index........................................................................................................................................ 227
Finney Learning Systems v
Welcome to The Health Care Revenue Cycle. This is a study guide to help the
student or employee acquire an understanding of how the business of health care
in the United States is organized, regulated and reimbursed. By highlighting and
reinforcing important administrative concepts, the student is better prepared to pass
certifcation examinations and work effciently in the health care industry.
This study guide can be used at a multitude of health care facilitiesfrom a doctors
offce to a hospital to an insurance claims offce. It can serve as both a training
manual and a reference guide. In addition to pertinent and extensive information,
each chapter concludes with defnitions of abbreviations and acronyms and an
abundance of sample test questions. The reader will also fnd helpful test-taking
strategies.
Health care in the United States has evolved since the mid-twentieth century into a
complex web of delivery systems, governmental regulations and third party payers.
Therefore, it is crucial that health care organizations have the expertise and resources
to master the inevitable ever changing rules and regulations. Its staff must know how
money is generated for the business of health care delivery.
Welcome
Chapter 1 - Health Care Plans and Legislation 1
Chapter 1 Health Care Plans and Legislation
Chapter Topics
The Health Care Insurance Industry
Health Care Plans
Important Defnitions
Physician Identifcation Numbers
The Major Players (CMS, DHHS, Medicare, etc.)
Other Players (HIPAA, FCA, EMTALA, etc.)
Understanding Acronyms and Abbreviations
Test Taking and Study Strategies
Sample Multiple Choice Test Questions
After studying this chapter you will understand:
Indemnity, MCOs: HMOs, PPOs, POSs
PINs, UPINs, PPINs, EINs, SSNs, NPIs
Department of Health and Human Services (DHHS)
Centers for Medicare and Medicaid (CMS)
Medicare and Medicaid
State Childrens Health Insurance Program (SCHIP)
Balanced Budget Act (BBA)
TEFRA and DEFRA
COBRA and OBRA
MAAC and Limiting Charge
Health Insurance Portability and Accountability Act of 1996 (HIPAA)
EDI
FCA, Department of Justice (DOJ) and Offce of Inspector General (OIG)
Stark Laws, Anti-Kickback Statute, Sarbane-Oxley Act
Fraud and Abuse
Medical Ethics
Professional Liability
CMP or CMPL
EMTALA
Patient Bill of Rights
The Health Care Revenue Cycle 2
The Health Care Insurance Industry
This chapter examines organizations, and the legislation they create, that regulate
how health care is provided to patients in the United States whether in a hospital,
clinic, doctors offce, nursing home, public health clinic, ambulance service or
medical supply company. An examination of the types of insurance plans that pay for
health care, and the coding manuals that are used to get the doctor and hospital paid,
are also examined.
It is crucial for the reader of this study guide to understand that Medicare (operated
by the federal government) is the basis for all health care delivery, processing, and
payment in the United States. Fee schedules, payment protocols, coding manuals and
forms, all infrastructure associated with health care, legal ramifcations concerning
how the patients treatment needs are handled, legal prosecution of health care fraud
and abuse, hospital and nursing home inspection and accreditation, etc., are all based
on Medicare. All health care patients and the public, providers, nurses, hospitals,
nursing homes, suppliers, insurance carriers, governmental agencies, the Department
of Justice and Offce of Inspector General, etc., ultimately follow Medicares rules and
regulations.
Health Care Plans
Figure 1: Health Care Plans
There are basically two types of insurance plans Indemnity and Managed Care.
It is rare today for a patient to pay cash for all his/her health care. Even when the
patient does pay cash, the doctors offce or hospital ultimately submits an insurance
claim, and the patient is reimbursed directly by the carrier or Medicare.
Chapter 1 - Health Care Plans and Legislation 3
Indemnity
This type of insurance plan protects (indemnifes) the patient against a loss of money
as a result of the patient receiving medically necessary health care services. Payment
to the doctor is on a fee-for-service (FFS) basismoney paid for each service provided
the patient and done retroactively (after the services have been provided). The health
care provider or hospital bills the insurance company directly on a claim form and
gets paid according to a payment, fee or benefts schedule. The patient pays a premium
(the cost of buying the insurance) every year to keep the insurance active, and also
pays a deductible every year before the insurance company begins paying for medical
services.
If the provider or hospital is a participating provider, they signed a contract with the
insurance carrier to treat their patients and accept their fee schedule as payment in
full, except for deductibles, co-payments or co-insurances. If the physician is a non-
participating provider, he has not signed a contract with the insurance carrier and the
patient pays the doctor directly when services are rendered. The indemnity plan may
still reimburse the patient, but the patient has to bill the insurance company directly
and will probably receive a fraction of what was paid to the doctor.
The patient also pays a co-insurance (usually 10% or 20%), a percentage of each claim
(i.e., billing for treatment provided the patient), before the insurance company pays
the remainder of the claim. In an 80/20 plan, the most popular, the patient pays
20% of the fee schedule amount to the doctor, and the insurance company pays the
remaining 80% of the fee schedule to the doctor. In a 90/10 plan, the patient pays
10% of the fee schedule to the doctor, and the insurance company pays the remaining
90% of the fee schedule to the doctor.
It is important to understand that the indemnity contract is between the insurance
company and patient only. The consumer can go to any doctor, hospital, therapist,
or medical supplier he chooses and the insurance company pays the bill. The more
services the patient uses, the more money the doctor or hospital makes. Indemnity
insurance is the most expensive form of health care plan as the provider does not
share the fnancial risk of providing medical treatment, procedures, and supplies to
the patient.
Managed Care Organization (MCO)
This type of insurance plan restricts who the consumer can see for health care
treatment. The doctors and hospitals and patient sign a contract with a managed
care plan. The doctors and hospitals who sign an MCO contract are considered to be
in network or participating providers. In return for the patient using only participating
providers and hospitals, there are lower premiums, deductibles, co-insurances and
co-payments compared to indemnity plans.
MCOs are the most common type of health insurance plan in the United States
today. They include Health Maintenance Organizations (HMO), Point-of-Service
plans (POS), and Preferred Provider Organizations (PPO). The main goal of the MCO
The Health Care Revenue Cycle 4
is to ration the use of health care services and reduce the amount of money paid for
those services.
1. Health Maintenance Organizations (HMO). This type of MCO is where
the Primary Care Physician (PCP) acts as the gatekeeper and is given a
capitated rate (a set amount for each member per month known as Per
Member Per Month (PMPM). For the PMPM to be paid prospectively
(in advance), the doctor must provide to the patient certain services such as
screenings, immunizations, well-baby check-ups, mammograms for women,
etc., as well as treatment that is determined to be medically necessary by
the gatekeeper. However, the doctor does not get paid more for additional
services and products, so there is the chance the doctor will lose money on
some patients and make a proft on others. In other words, in this type of
plan, the doctor and hospital share in the risk of providing medical services,
and there is an incentive for the gatekeeper to restrict the patients access to
health care services and products in order to make money.
2. Open Access Plans. Many HMOs have switched from using gatekeepers
to plans in which their members can visit any specialist in the network
without referrals. This is known as HMO Open Access Plan. Even if referrals are
necessary, female HMO members can still see OB-GYN specialists without a
referral.
3. As the gatekeeper, it is the doctor who determines what treatment is to be
provided (if any), and who the patient will be referred to for more specialized
services. Patients cannot simply get whatever services or products they
want. They are not only limited to participating doctors and hospitals, but
the gatekeeper doctor also restricts referrals to other medical specialists and
pre-authorizations are required. Most commonly, the gatekeeper/doctor is
a Primary Care Physician (PCP), but also can be a Gynecologist (GYN) for a
woman or a pediatrician (PED) for a child.
4. Point-of-Service Plans. These are also known as open HMOs. They
operate like HMOs, but allow the consumer to use doctors and hospitals
outside the network of participating providers. There are pre-authorizations
required in a POS plan and utilization of health care services is restricted.
The patient pays higher premiums for a POS than an HMO for the privilege
to go out-of-network. If the patient uses an out-of-network provider or
hospital, the patient is responsible for higher deductibles, co-payments, and
co-insurances. The patient is responsible for the full cost of any health care
services the POS plan considers to be not covered. The out-of-network doctor
or hospital is paid on a FFS basis as determined by the POS, but it is lower
than reimbursement paid to in-network providers. There is no gatekeeper,
which means there is no doctor assigned by the POS plan to restrict the
patients access to other doctors, hospitals, services and products.
5. Preferred Provider Organizations (PPO). This is the most popular type
of health plan. It is provided by employers and there is no gatekeeper.
The doctors and hospitals contract for their medical services with the PPO
directly, at a lower rate than they normally charge, in return for a large pool
Chapter 1 - Health Care Plans and Legislation 5
of patients who pay lower fees. The consumer can choose any health care
provider or facility, even if outside the network. Like the POS, however,
the patient would be responsible for higher deductibles, co-insurances and
co-payments if they go out-of-network. The patient would still require
pre-authorizations, and for health care services not covered by the PPO the
patient would be responsible to cover the full cost.
Important Defnitions
Physician. Defned by Medicare as a Doctor of Medicine (MD), Doctor of Osteopathy
(DO), Doctor of Dental Medicine (DMD), Doctor of Dental Surgery (DDS), Doctor
of Podiatric Medicine (DPM), Doctor of Optometry (OD), or Doctor of Chiropractic
(DC) who are legally licensed to practice (provide medical services and products to
human beings) in the state in which they deliver health care services.
Health Care Practitioner. These are also known as Non-Physician Practitioners
(NPP). Includes Physician Assistant (PA), Certifed Nurse Midwife, Psychologist
(MA, MS, PhD), Nurse Practitioner (NP), Clinical Social Worker (MSW), Physical
Therapist (PT), Occupational Therapist (OT), Respiratory Therapist (RT), Speech
Therapist (ST), Certifed Registered Nurse Anesthetist (CRNA), or Registered Nurse
(RN, MSN, PhD), or other licensed health care professionals.
Good Samaritan Act. Legislation that protects health care professionals from
liability of any civil damages (money) as a result of rendering emergency care. For
example, if a doctor provides emergency medical care to a fellow passenger while on
a plane who suffered a heart attack, and the patient dies or suffers complications, the
doctor would be protected under this act against legal action.
New Patient. One who has not received health care services from the physician, or
another physician of the same specialty in the same group practice, within the past
three years.
Established Patient. One who has received health care services from the physician,
or another physician of the same specialty in the same group practice, within the past
three years.
Inpatient. A person who is admitted to the hospital with the assumption the patient
will stay for 24 hours or more (overnight stay).
Outpatient. A patient who receives treatment in a doctors offce (whether outside
the hospital or in a medical building associated with the hospital), hospital clinic or
outpatient facility (such as a family or dermatology practice), emergency room or
department (E/R), hospital same day surgery center, or ambulatory surgical center
(ASC) where the patient is released within 23 hours, or a hospital admission for
observation purposes only (the doctors and nurses watch the patient and do not treat
the patient; this can occur in the E/R).
Coding. The process of converting diagnoses, symptoms, diseases, procedures,
services, and products into numbers and letters. The ICD-9-CM, HCPCS, CPT-4,
CDT, and NDC manuals are used for this purpose by the medical biller and coder.
The Health Care Revenue Cycle 6
Clearinghouse. A majority of providers and hospitals use a clearinghouse to send
and receive information in correct EDI format (HIPAA approvied electronic) to
third party payers. Under HIPAA, clearinghouses can accept the claim forms in
non-standard formats from the provider, and translate them into standard formats
utilizing ICD-9, CPT, HCPCS, CDT and NDC codes (numbers and letters), before
forwarding them to third party payers. Clearinghouses must receive all required data
elements from providers and hospitals, they cannot create or modify the content of
these claims forms. They review the claim forms to be valid, complete, and HIPAA
compliant, and if they fnd mistakes, they return the claims to the provider or
hospital for corrections, review them again, before sending them out to Medicare,
Medicaid, or commercial (private) third party payers. A medical practice or hospital
may choose to use a clearinghouse to transmit all their claims, or just some of
them. Once the clearinghouse has sent the claims, a verifcation report is sent to the
provider or hospital which summaries what was sent to the payer. Later the receiver,
the third party payer, will send back an electronic response showing the transmission
was received from the clearinghouse and the insurance adjudication process can
proceed for payment.
Pre-certifcation. This is the process of confrming the patients insurance eligibility
and collecting necessary information prior to the patient using the hospital or
health care facility as an inpatient or outpatient. Pre-certifcation may also include
the insurance company issuing an authorization number (through its review
organization) approving the medical necessity of the services, procedures or supplies
that are going to be rendered to the patient.
Maximum Medical Improvement (MMI). This is where the doctor has determined
the patient has reached the best clinical improvement that is possible for the
diagnosis and treatment provided.
Physicians Identifcation Numbers
These are unique numbers (and letters) assigned to each doctor, or group of doctors,
medical supplier, therapist, nurse, health care facility, etc., by insurance companies,
MCOs, Medicare, Medicaid, and IRS so the provider can be easily identifed in all
billing and coding situations and correspondence. Examples include the following:
Provider Identifcation Number (PIN). A number assigned by the insurance carrier
to a physician who renders services to their patients (membership).
State License Number. Every physician, medical supplier, nurse, therapist, etc.,
must obtain this number in order to practice in each state in which they wish to
render health care or provide a service or product.
Unique Provider Identifcation Number (UPIN). A number assigned by Medicare
to each physician.
Performing Provider Identifcation Number (PPIN). Each physician has a separate
PPIN for each group or offce or clinic in which the physician practices. In Medicare,
the group or clinic of practicing doctors gets a Group Provider Number (see below)
Chapter 1 - Health Care Plans and Legislation 7
as well as each doctor receives an individual eight digit (letters and numbers) PPIN
assigned by Medicare.
Group Provider Number. This number is used to identify a group of doctors or
therapists who provide health care services. In addition, the PPIN or PIN may also
be used for each individual provider in the group. However, the Group Provider
Number may be the only number used when the doctor is part of a group practice in
billing and coding the insurance carrier or Medicare.
Social Security Number (SSN): A 9-digit number assigned to all legal United States
citizens. Usually a provider of health care services would not normally use this
number when billing and coding third party payers unless they do not have an EIN
(see below).
Employer Identifcation Number (EIN): This is also known as the Federal Tax
Identifcation Number, and is issued by the Internal Revenue Service (IRS) for anyone
who operates a business and/or who is an employer. This number is usually placed
in the insurance billing and coding forms when the doctor or supplier is the owner
of the medical practice, medical supply company, peer review organization (PRO),
Nursing Referral Service, etc.
National Provider Identifer (NPI). NPI is an important number that each health
care provider (hospital, SNF, doctor, supplier), health plan, and clearinghouse, etc., is given
by HIPAA for all their administrative and fnancial business within the health care
industry or Medicare. The NPI is part of HIPAAs Administrative Simplifcation
Standard and consists of 10 numbers and letters. Simplifcation Standard means
that the goal of HIPAA is to minimize confusion and assign one permanent number,
the NPI, which would replace all the other physician identifcation numbers. This
way, anyone doing business with the medical community will use their NPI as
the sole reliable identifer, and all the other numbers: PIN, PPIN, UPIN, etc., will
gradually be phased out. The CMS-1500 and UB-04 claim forms require the use of the
NPI. The other reason the NPI is so important is that the patient can easily identify all
the providers they come into contact with through the course of their treatment and
through the course of their contact with the health care industry.
The Major Players
The Department of Health and Human Services (DHHS) and the Centers for
Medicare and Medicaid Services (CMS) are the federal governments main
administrative bodies that set standards for health care delivery in the United States.
Everything from fees, manuals, regulations, forms, and health care locations in the
United States, emanate from the DHHS and CMS. Medicare, a division of CMS, is the
gold standard by which all insurance carriers and governmental bodies determine
how to deliver, adjudicate, and reimburse health care.
The major regulatory bodies and laws affecting health care include:
DHHS, CMS, MEDICARE, MEDICAID, SCHIP, BBA, TEFRA, DEFRA, COBRA,
OBRA and MAAC.
The Health Care Revenue Cycle 8
Figure 2: The Major Players
The Department of Health and Human Services (DHHS or HHS) (www.hhs.gov)
and The Centers for Medicare and Medicaid Services (CMS), formerly called the
Health Care Financing Administration (HCFA), are the two main governing bodies
responsible for health care delivery (i.e., providing health care) and reform in the
United States. There are many departments within DHHS, but its principal agency
for administering health care is Medicare. Medicare is the nations largest health
care administrative body and delivery system, handling over one billion claims per
year. Today, health care rules and regulations, fee schedules, payments systems,
and delivery mechanisms, all come from Medicare. It establishes the standards for the
administration of health care for the entire country, both public and private, such as
public health clinics, non-proft insurance companies such as Blue Cross and Blue
Shield, and private for-proft insurance carriers such as State Farm, AllState, Humana
and Aetna.U.S. Healthcare.
Chapter 1 - Health Care Plans and Legislation 9
The Department of Health and Human Services (DHHS)
DHHS supports more than 300 programs, some of which are:
1. Medicare
2. Medicaid
3. Insuring drug and food safety (for example, preventing food poisoning
and adverse drug reactions)
4. Improving the health of mothers and infants (providing pre-natal and
post-natal care, proper nutrition and hygiene)
5. Medical and social science research
6. Prevention of infectious diseases, immunizations
7. Safety and health care for elderly Americans including home-delivered
meals
8. Child-support legal enforcement (make sure that parents fnancially
support their dependent children)
9. Aid to Families with Dependent Children (AFDC)
These numerous DHHS programs are administered through 11 divisions of DHHS
which include:
1. Centers for Medicare and Medicaid Services (CMS)
2. National Institutes of Health (NIH)
3. Food and Drug Administration (FDA)
4. Centers for Disease Control and Prevention (CDC)
5. Agency for Toxic Substances and Disease Registry (ATSDR)
6. Indian Health Services (IHS)
7. Health Resources and Services Administration (HRSA)
8. Substance Abuse & Mental Health Services Administration (SAMHSA)
9. Agency for Health Care Research and Quality (AHRQ)
10. Administration for Children and Families (ACF)
11. Administration for Aging (AOA)
The Centers for Medicare and Medicaid Services (CMS)
CMS, a division of DHHS, acts primarily as the buyer of health care services for
Medicare (Title XVIII) and Medicaid (Title XIX) insuring that programs are properly
administered by its contractors and state agencies). CMS establishes policies
for payment of health care providers, acts as a researcher on the effectiveness of
health care treatment, insures proper management and fnancing, and assesses
The Health Care Revenue Cycle 10
the quality of health care facilities and services such as hospitals, nursing homes,
insurance companies, health maintenance organizations, and federal, state, and local
governmental agencies that deliver health care services to the public. CMS is also
the guarantor of health care security and equal access of health care services and
products to all Americans. In other words, CMS guarantees that all Americans can
get medically necessary treatment regardless of whether they can pay and with no
concern as to race, sex, or ethnic background. Note: See www.cms.hhs.gov to view
the relationship between Medicare and Medicaid.
Medicare
Medicare is a federal program (Title XVIII of the Social Security Act), which was
signed into law in 1965. Medicare Parts A and B are known as the Original Medicare
Plan where services are paid under a Fee-for-Service (FFS) arrangement. It is made
up of four (4) parts:
Part A: Pays for inpatient hospital services, skilled nursing
facilities (SNF), home health services (HHS), hospice
care and psychiatric inpatient care. Also known as
Hospital Insurance (HI). Anyone who receives Social
Security benefts by working for at least 10 years (40
quarters) and paying social security taxes, or having
certain types of disabilities like ESRD, automatically
is enrolled in Part A by the Social Security
Administration (SSA) and does not have to pay
premiums. Those who are over 65 years of age and do
not have Part A benefts can still purchase Medicare
Part A coverage by paying a premium.
Part B: Pays for physician services, medical equipment
and supplies (DME-durable medical equipment),
outpatient hospital services: outpatient physical
therapy, occupational therapy and speech therapy,
outpatient mental health care, clinical laboratory
services (Urinalysis [UA] and Complete Blood Count
[CBC]), home health care, blood, etc. Also known as
Supplementary Medical Insurance (SMI). Those who are
enrolled in Part A are automatically eligible to purchase
Part B coverage (premium for 2009 is $96.40/month).
Those desiring Part B coverage must enroll, coverage
is not automatic. If enrollment in Part B coverage
takes place more than 12 months after a persons
initial enrollment in Part A, there is a permanent 10%
increase in premium for each year the benefciary
Chapter 1 - Health Care Plans and Legislation 11
failed to enroll in Part B. For example, if the
benefciary frst enrolled in Part A in 2008, and does
not choose to purchase Part B coverage until 2009,
there would be a $9.64 penalty (10% X 96.40) added to
each months premium permanently as long as Part B
is purchased during the patients lifetime.
Part C: Originally called Medicare + Choice. Part C is
available to those benefciaries who have Parts A
and B. Part C gives the benefciary the option to get
Medicare Advantage Plans, e.g., Health Maintenance
Organizations (HMOs), Preferred Provider
Organizations (PPOs), Private Fee for Service Plans,
Special Needs Plans, and Medicare Medical Savings
Accounts (MSA), which compete directly with the
Original Medicare Plan.
Part D: Pays for prescription drugs through private insurance
plans. Part D was authorized through the Medicare
Prescription Drug, Improvement and Modernization
Act of 2003 also known as the Medicare
Modernization Act or MMA. Those who have
Medicare Parts A and B are eligible (can purchase)
Part D, if they choose, through monthly premiums.
The Medicare program provides services to those who are over 65 years of age, those
who are disabled of any age, and those with end-stage renal disease (ESRD) who require
kidney transplantation or dialysis of any age. Medicare is administered by the CMS.
In cases where the patient is low income and meets certain income requirements,
dual eligibility can be provided where Medicaid covers some of the costs of
Medicares Part A and Part B deductibles, co-payments, and co-insurances. This
way the patient has little or no out-of-pocket expenses and has medically necessary
treatment covered by both Medicare and Medicaid. Medicare Parts A and B are
known as the Original Medicare Plan.
Medicaid
The Medicaid Program (Title XIX of the Social Security Act) is a funded and
administered state-federal partnership (both the state and federal governments work
together) health insurance program. It is for low-income people with children and
people who are aged, blind, disabled or collecting Supplemental Security Income
(SSI). Also included are low-income pregnant women with children and persons with
very high medical bills. SSI includes money and food stamps from the government.
States set eligibility standards (those who can get Medicaid) and establish payment
rates and benefts and services (what and how much the Medicaid recipient will
The Health Care Revenue Cycle 12
receive and how much the doctor and hospital will be paid for providing health
services).
Civil Monetary Penalties Law (CMP or CMPL)
CMP is also known as Title XI of the Social Security Act. These are money fnes
that are applied to providers and hospitals who are convicted of fraud and abuse
concerning Medicare, Medicaid, any insurance plan or third party payer.
State Childrens Health Insurance Program (SCHIP)
State Childrens Health Insurance Program (SCHIP) (Title XXI of the Social Security
Act) is a program for children whose parents have too much money to be eligible for
Medicaid, but not enough to buy private insurance and are, therefore, uninsured. As
of February 2009, President Obama signed into law the Childrens Health Insurance
Reauthorization Act that expanded coverage for SCHIP-eligible families to include
children of legal immigrants and pregnant women. Funding of the expanded SCHIP
coverage would occur by increasing the federal tobacco tax. The SCHIP program
differs in each state, but all states must provide the following basic services.
1. Inpatient and outpatient hospital service
2. Doctors medical and surgical services
3. Laboratory and x-ray services
4. Well-baby/child care
5. Immunizations (Important!)
Balanced Budget Act of 1997 (BBA)
BBA, signed into law by President Clinton in August 1997, enacted the most
signifcant changes to Medicare and Medicaid since their inception, and expanded
services to SCHIP (Title XXI) through CMS. This act also established the Outpatient
Prospective Payment System (OPPS) known as Ambulatory Payment Classifcations
(APCs).
Tax Equity and Fiscal Responsibility Act of 1982 (TEFRA)
TEFRA is a federal law affecting employers with 20 or more full or part-time
employees. It requires that for employees who are senior citizens, 65 to 69 years old,
the employers group health insurance plans (EGHP) continue to be the primary payer.
Medicare will be the secondary payer. TEFRA, therefore, affords older workers the
same insurance coverage as younger workers.
Defcit Reduction Act of 1984 (DEFRA)
DEFRA, like TEFRA, is applicable to employer groups with 20 or more employees.
DEFRA raised TEFRAs upper age limit beyond 69 years of age for active employees,
making them eligible to enroll in the same group health insurance coverage offered
to younger employees. However, the spouse of an active employee remains restricted
Chapter 1 - Health Care Plans and Legislation 13
to insurance coverage up to age 69 under this plan. DEFRA also froze the amounts
physicians can charge for their services to 1984 rates.
Consolidated Omnibus Budget Reconciliation Act of 1985
(COBRA)
The Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) amended
TEFRA by eliminating the upper age limit of 69 for the spouse of an employee who
has group health insurance working for an employer with 20 or more employees.
Omnibus Budget Reconciliation Act of 1986 (OBRA of 1986)
Do not confuse OBRA of 1986 with OBRA of 1989 or OBRA of 1990. The OBRA of 1986
made employers with 100 or more employees, with large group health plans (LGHP),
the primary coverage for active employees who have Medicare, or dependents of
active employees who have Medicare due to disability other than ESRD. OBRA
set limits for what health care providers can charge Medicare benefciaries, which
was known as MAAC (Maximum Allowable Actual Charge). MAAC is essentially a
Medicare fee schedule stating what Medicare would pay for each health care service
or product. MAAC is important because every payer, whether private or public, pays
for medical services and products based on what Medicare reimburses.
OBRA of 1986 also requires the use of HCPCS coding on the UB-04 claim form for
Medicare claims for outpatient services when rendered in Acute Care or Tertiary
Care or Long-Term Care Hospitals, and Hospital-based Rural Care Clinics. Tertiary
care hospitals provide a full range of medical services, are usually teaching hospitals
associated with medical schools and universities, provide the highest level of trauma
care for the most severe cases, and are associated with research. Examples of tertiary
care hospitals include Massachusetts General Hospital associated with Harvard
University, the University of Pennsylvania Hospital affliated with University
of Pennsylvania, Hershey Medical Center associated with Pennsylvania State
University, etc.
Omnibus Budget Reconciliation Act of 1989 (OBRA of 1989)
OBRA 1989 changed how payment is made to physicians by Medicare, and
established the Resource Based Relative Value Scale (RBRVS). RBRVS is composed
of three elements:
1. Relative Value Unit (RVU) is a fee schedule for every medical procedure
recognized by Medicare. Each medical procedure is assigned a value
based on all of the following:
Work required. (For example, how much effort and time and
expertise is needed by the doctor to perform the surgery.)
Practice expense. (For example, what it costs the doctor to perform
the surgery.)
The Health Care Revenue Cycle 14
Malpractice insurance expense (For example, neurosurgery
costs more to insure against a medical misadventure that an
appendectomy.)
2. Medicare Volume Performance Standard (MVPS) determines how much
every year Medicare will increase payment for services provided by
health care providers and facilities to patients. For example, for 2009, the
Medicare fee for performing an appendectomy was increased 10% (2008=
$1500; 2009= $1650).
3. Limits the amount non-participating physicians can charge Medicare
patients, which is 115% of the Medicare fee schedule, known as the limiting
charge (which replaced the MAAC [OBRA of 1986]). The limiting charge
remains in effect today.
Omnibus Budget Reconciliation Act of 1990 (OBRA of 1990)
As a result of OBRA of 1990, hospitals who wish to participate in Medicare and
Medicaid must develop and implement programs and policies assisting the patient
to make their own medical decisions, appoint a Health Care Surrogate or Durable
Power of Attorney, and execute an AMD. The Patient Self Determination Act
(PSDA) is also known as the Advanced Medical Directive (AMD). The PSDA gave
the patient the right (in a legally binding document) to determine, in advance, what
health care measures they want if they become incapacitated including a Do Not
Resuscitate (DNR) directive, and appoint a Health Care Surrogate and a Power of
Attorney to carry out their directives. The DNR allows the patient to state, in a legally
binding document, what health care measures they want, or do not want, to maintain
their life in case of becoming terminally ill or injured.
Operation Restore Trust of 1995 (ORT)
The Operation Restore Trust of 1995 (ORT) was designed to combat fraud, waste and
abuse in the fve states with the highest Medicare expenses, e.g., California, Florida,
New York, Texas and Illinois. These fve states have received particular attention
by the federal government because they have the highest rates of health care fraud,
abuse and waste in the United States.
Other Players
These organizations and laws complement the DHHS and CMS, as they play an
integral role in the delivery of health care and establish standards for the elimination
of health care fraud, abuse and waste and prosecution of offenders.
They include: HIPAA, NPI, EDI, FCA, DOJ, OIG, Fraud and Abuse, Medical Ethics,
Professional Liability, CMP, EMTALA, Patient Bill of Rights.
Chapter 1 - Health Care Plans and Legislation 15
Health Insurance Portability and Accountability Act of 1996
(HIPAA)
HIPAA, a.k.a Kennedy-Kassenbaum Act, insures the portability of health insurance
when employees change jobs (makes the employee capable of taking their insurance
from employer to employer). In addition, it increases accountability of the health
care contracts that insurance companies write for the patient, increases accountability
of the health insurance carrier itself (makes them more transparent), contains broad
new health care anti-fraud and anti-abuse provisions so the government can fght fraud and
abuse and protect the patient from having their Personal Health Information (PHI) stolen,
and improves availability of health insurance to working families and their children.
HIPAA also establishes three administrative simplifcation provisions which are: (1)
HIPAA Privacy Rule, (2) HIPAA Security Rule, and (3) HIPAA ElectronicTransaction
and Code Sets Standards. Managed Care Organizations (MCOs) are affected under
HIPAA for ALL their health care related business, not just Medicare.
For further information contact: http://www.cms.hhs.gov/hipaa/hipaa2.
HIPAAs key provisions include the following:
1. Guaranteed ability to get health insurance for employers with 50 or less
employees. This means these employees will have the ability to purchase
health care insurance regardless of their health status, age, or medical history.
2. Guaranteed renewal of insurance regardless of health status of any member
of a group of insured people. This means the employee can continue to have
health insurance year after year regardless of health status, age, or medical
history.
3. Guaranteed access for those who lose their group health insurance due to
loss of employment, or change of job to an employer without insurance.
4. If an employee had a medical condition that existed prior to getting new
health insurance with a current or new employer, this medical condition
cannot be used to deny coverage to employees who already had coverage.
HIPAA also applies this rule to limited medical conditions treated and
diagnosed within six (6) months prior to enrollment in a new insurance
health plan, whether it is a current or new employer. This means the new
insurance company cannot deny coverage to the employee because they had
recently been diagnosed and treated for certain diseases or illnesses.
5. For self-employed individuals (people who own and operate their own
businesses), tax deductions for insurance costs will increase from 30% to
80%.
6. Health Savings Accounts (HSAs), is the new name for Medical Savings
Accounts (MSAs), and remain in effect.
7. Administrative Simplifcation. All providers and health care plans
involved in electronic health care transactions must utilize a single set of
national standards and identifers. This means those doctors and hospitals
and medical suppliers who transmit their bills for payment through the
The Health Care Revenue Cycle 16
computer, must use standardized codes (numbers and letters) and forms and
language that everyone understands.
8. Covered Entities: Under HIPAA there are 3 types of health care
organizations that are affected: (1) Health Plans, (2) Health Care
Clearinghouses, and (3) Health Care Providers.
9. Health care fraud and abuse are investigated and prosecuted by the
Department of Justice (DOJ) and the Offce of Inspector General (OIG).
10. HIPAA regulations are enforced by the Offce for Civil Rights (OCR).
National Electronic Data Interchange (EDI)
EDI produced rules that made all HIPAA paperwork and fnancial transactions the
same and understandable by everyone involved in the health care industry (just like
HIPAA assigns an NPI). Manuals that have codes describing all aspects of providing
and billing health care, such as ICD-9-CM, CPT-4, HCPCS, CDT, NDC, Unique Health
Identifer, Security and Privacy of Health Information, Electronic Signature, and information
transfer between health plans, are now the only materials used so that everyone
involved in the business of health care understands what everyone else is doing.
Remember, one of the major goals of HIPAA is to standardize all criteria within the
entire health care industry
1. The International Classifcation of Diseases, 9th Revision, Clinical Modifcation
(ICD-9-CM), is a three volume numeric and alphanumeric coding manual
established by the World Health Organization (WHO) for all outpatient and
inpatient conditions, symptoms, pathologies and diagnoses. The ICD-9-
CM is updated every year. The CMS also sponsored the production of the
ICD-10-PCS, International Classifcation of Diseases, 10th Revision, Procedure
Classifcation system, which will replace the ICD-9-CM, for reporting a
more detailed description of health care procedures and technologies for
the inpatient. The ICD-10-CM will replace the ICD-9-CM for inpatient and
outpatient diagnoses and clinical conditions.
2. The ICD-9-CM consists of Volume 1, Tabular List, which is a numeric
(numbers) and alphanumeric (letters and numbers) listing of all the
diagnosis/pathology/condition codes, and Volume 2, The Alphabetic Index, is
an alphabetic listing of everything found in Volume 1. Volume 1 also includes
V codes, which are supplementary alphanumeric codes for non-pathological
medical situations the patient may encounter such as innoculations, tissue
transplantation, dialysis, family and patient medical history, rehabilitation,
chemotherapy and radiation therapy, etc. Volume 1 also includes E codes,
which are supplementary alphanumeric codes for external causes of trauma
such as motor vehicle accidents (MVAs), poisoning, terrorism, railroad/bus/
aircraft injuries, water-related trauma, sports injuries, etc.
3. The Current Procedural Terminology, 4th edition (CPT-4), is a manual of numeric
and alphanumeric codes for all physician, hospital, Ambulatory Surgical
Center (ASC), Skilled Nursing Facility (SNF), inpatient and outpatient
medical procedures and services, and is owned by the American Medical
Chapter 1 - Health Care Plans and Legislation 17
Association (AMA). Place of Services code sets (POS) are also part of this
manual, which specifes locations that medical services and procedures are
delivered to the patient such as the doctors offce or hospital. The CPT is
also composed of modifers and add-on codes which are coupled to the main
CPT code, that further describe particular physician services in more detail,
as well as P codes which describe the patients physical status (how
healthy or sick they are) when a medical procedure such as anesthesia or
surgery is performed.
4. The CPT is divided into three 3 categories of codes:
Category I codes (5-digit numeric) are found in six chapters: Evaluation
and Management (E/M), Anesthesiology, Surgery, Radiology, Pathology
and Laboratory, and Medicine, and are for inpatient and outpatient
physician procedures and services. Category I codes are the only ones
that are reimbursed by the insurance companies and Medicare.
Category II codes (5 digit alphanumeric ending in the letter F) are for
performance measurement and statistical analysis (counting things).
Category III codes (5 digit alphanumeric ending in the letter T) are
for new and experimental medical procedures and services. In some
instances when the Category III code becomes proven through research
and generally accepted by the medical community, they become
Category I codes.
HCPCS, which stands for the Health Care Common Procedure Coding
System, was developed by the CMS (HCFA) as a 2-part or level coding
system. This manual consists of a collection of codes for procedures,
supplies, products and services that are rendered to Medicare and
Medicaid benefciaries, and patients with other private insurance plans.
These codes are divided into two levels: Level I, which are the same
codes as the CPT-4 Category I codes, and Level II codes, which are
national codes that cover ambulance services, medical supplies and
products, durable medical equipment (DME), prosthetics and orthotics
and some physician services not found in Level I. Although Level II
codes are called national codes, in reality, all the ICD, CPT, HCPCS,
CDT, and NDC codes are national codes as they are used throughout the
United States.
5. The National Drug Code manual (NDC) is made up of codes for retail
pharmacies and pharmaceuticals, and is maintained by the Food and Drug
Administration (FDA).
6. The Current Dental Terminology manual (CDT) is made up of codes for dental
services.
Additional information and further clarifcation to assist with your understanding
and test preparation can be accessed at the following websites:
http://www.cms.hhs.gov/healthplans/
http://answers.hhs.gov
The Health Care Revenue Cycle 18
http://www.wedi.org
http://www.wpc-edi.com
Medical Ethics; Fraud and Abuse; Professional Liability
Medical Ethics are standards of conduct based on moral principles. They are
generally accepted as a guide for behavior towards patients, physicians, co-workers,
the government, insurance companies and anyone within the health care industry.
Acting within ethical behavior boundaries means carrying out ones responsibilities
with integrity, decency, respect, honesty, competence, fairness and trust, like a Boy or
Girl Scout!
Professional Liability refers to the legal concept that the physician and hospital are
liable for their own conduct and conduct of their employees. Respondent Superior
is the legal term meaning Let the master answer. In other words, the doctor and
hospital are liable for the actions of their employees whether it involves billing and
coding, adherence to HIPAA, treatment of the patient, fraud, abuse, etc.
Fraud is defned as a deliberate deception perpetuated for unlawful or unfair gain. In
other words, lying to the patient or falsifying paperwork to the insurance company to
get money or assets that do not belong to the provider.
Health Care Fraud includes the incorrect reporting of a diagnosis or procedure or
service in order to maximize payments. It also pertains to billing for services not
rendered, altering claims (changing the diagnosis and treatment) to receive payment,
or unbundling and accepting kickbacks (monetary or otherwise). Fraud and abuse
are investigated and prosecuted by the Offce of Inspector General (OIG) and the
Department of Justice (DOJ).
Abuse is defned as the misuse of a person, substance, service, procedure, or fnancial
matter so that harm is caused. Health care abuse includes the following:
1. Medically insuffcient, excessive or unwarranted use of technology
(surgical, diagnostic, laboratory, etc.); medically inappropriate utilization of
pharmaceuticals, services, procedures and products (such as durable medical
equipment [DME]). In other words, giving the patient too much (over-
utilization) or too little (under-utilization) surgery or medicine, or giving
medical supplies to the patient that are not needed.
2. Abuse of authority or compromising patient privacy or patient
confdentiality matters (violating HIPAA). In other words, not keeping
the patients medical information from public view, purposely divulging
information publicly to harm the patient or selling it to make money.
3. Improper billing and coding practices (e.g., upcoding, which is coding for a
more expensive service than what was actually provided), billing Medicare
instead of the primary insurer, increasing charges to Medicare benefciaries
but not other patients, or unbundling of services and procedures. Unbundling
is defned as using more procedural codes (CPT and HCPCS) than is
normally warranted in order to bill for medical treatment to get additional
Chapter 1 - Health Care Plans and Legislation 19
reimbursement from the insurance company. Bundling is defned as taking
several procedural codes and combining them into one for the treatment
rendered. This usually results in less money being paid to the health care
provider.
4. Medically unnecessary or AMA (against medical advice) treatment of the
patient. This refers to the illegal and clinically unsubstantiated transferring of
the patient out of the hospital. The provider or health care facilitys duty of
care to the patient has been violated. For example, a doctor or hospital might
dump the patient on the street or at home before the patient is medically
stable or because the patient cannot pay. AMA also includes the patient
voluntarily leaving the hospital before treatment is completed or MMI has
not been achieved, or against the doctors advice.
Reporting Fraud and Abuse may be directed to the Medicare contractors (the
insurance company that Medicare hired to service its customers such as Blue Cross/
Blue Shield) customer service line or fraud department by calling the contractors
fraud hotline, or calling the OIG fraud hotline number: 1-800-HHS-TIPS, with the
following information:
1. Patients Name
2. Date of Service (DOS)
3. Name of Provider
4. Providers Medicare Number
5. Explanation of alleged fraudulent or abusive activities
6. Patients Health Insurance Claim Number
7. Description of Service, Procedure, or Product
8. Address of Provider, and any other pertinent information
Civil Monetary Penalties (Law) (CMPs or CMPLs) is legal punishment (monetary
fnes) imposed by the court when Medicare has determined that a provider or
hospital has violated Medicare, Medicaid, or any health care rules and regulations,
such as fraud or abuse, violation of HIPAA laws, or other administrative infractions.
Title XI of the Social Security Act authorizes the imposition of CMPs.
The Offce of Inspector General (OIG) has seven (7) components in its compliance
plans for doctors and hospitals to avoid fraud and abuse in billing, coding and
delivery of health care services, in the health care workplace. They include the
following:
1. Establish written policies and procedures to check for fraud and abuse in the
health care workplace.
2. Have a Compliance Offcer. This is someone who is in charge of enforcing
policies and procedures to check for fraud and abuse in the workplace.
3. Have effective training and education in the workplace to avoid fraud and
abuse.
The Health Care Revenue Cycle 20
4. Stress effective communication between all employees so that fraud and
abuse can be detected and eliminated.
5. Make sure standards and disciplinary sanctions are clearly written, posted
and known so that all employees are aware of how to avoid fraud and abuse.
6. Promote constant auditing and monitoring in the health care workplace to
avoid fraud and abuse.
7. When fraud and abuse are detected, timely response to offenses occurs as
well as corrective actions are taken.
False Claims Act (FCA)
The False Claims Act (FCA), also known as the Lincoln Act, Qui Tam Statute
or the Informer Act, imposes civil and criminal liability on any doctor or hospital
or supplier that submits an abusive or fraudulent claim for payment to the United
States government or to any third party payer. A health care provider that is found
guilty of fraud and abuse can also be excluded from Medicare and Medicaid.
Examples of fraud and abuse include kickbacks, billing for services not provided,
infating invoices, over-utilization or under-utilization, misrepresenting services
and supplies and procedures provided to patients, providing services not medically
necessary for fnancial gain, and denying patients access to quality health care.
National anti-fraud and anti-abuse laws under HIPAA, and other federal regulations,
are enforced by the OIG and the DOJ. The frst person who brings a Qui Tam suit, is
known as the relater (or whistle-blower). The National Health Care Anti-Fraud
Association has estimated that of the $3+ trillion spent on health care in 2009, from 3
to 5 percent were lost to fraud.
Additional laws relating to health care fraud and abuse control include:
1. Stark Laws, which are self-referral prohibitions, are guidelines that make
it illegal for the physician, or members of their immediate family, to have
fnancial relationships (ownership) with health care facilities which they
refer their patients. For example, a doctor refers patients to a laboratory,
x-ray clinic, or DME company for services or supplies that the doctor (or
their family) owns or has a fnancial interest. Therefore, the provider (or
their family) is making money every time a referral is made. There are
many exceptions to the Stark legislation which allows self-referral through a
variety of legally created business structures, known as safe harbors.
2. Anti-Kickback Statute makes it illegal for any health care provider or facility
to knowingly offer or accept any gifts or money for referring patients to
receive services or products paid by any government health care program
like Medicare, Medicaid, SCHIP, etc. This statute includes the provider
routinely not collecting co-insurances and co-payments the patient is liable.
Accepting money or other forms of reward, such as vacations, property,
tickets to a football game or Broadway show, dinner, gifts, etc., for referring
patients to other providers is also prohibited. The doctor accepting kickbacks
for sending patients to a medical supplier for DME, taking kickbacks for
sending patients for x-rays, taking kickbacks for sending patients to an
Chapter 1 - Health Care Plans and Legislation 21
orthopedic surgeon for treatment, or giving money or gifts to lawyers for
sending patients to the doctors offce for treatment due to an mva, worker-
related injury or a slip-and-fall accident, are all prohibited.
3. The Sarbanes-Oxley Act of 2002 requires publicly traded companies, ones
that are listed on the New York Stock Exchange or Nasdaq and offer stock
to the public, to prove they are fnancially sound and their record keeping
accurately refects the activities of the company (there is no fraud or abuse).
This act is important as related to the health care revenue cycle because the
Sarbanes-Oxley Act applies to for-proft health care corporations such as
insurance companies (State Farm, AllState, Farmers), medical equipment
and device companies (Medtronic, Johnson & Johnson), MCOs (Aetna U.S.
Healthcare, Humana), pharmaceutical companies (Smith Kline, Merck,
Schering-Plough, Johnson & Johnson), etc. Since these companies furnish
services and supplies worth billions of dollars to the public, they must be
operating legally, follow generally accepted accounting principles (GAAP),
and be fnancially liquid, otherwise they could have a devastating fnancial
effect on Medicare and other government funded health care programs. This
act also includes whistle-blower protection so that employees in these
corporations can report fraud and abuse and other wrongdoing without fear
of retaliation.
Emergency Medical Treatment and Active Labor Act (EMTALA)
EMTALA involves:
1. Medical Screening Examination is provided to anyone who goes to a
hospitals emergency room (ER) requesting examination and treatment
for the purpose of determining whether emergency medical treatment is
required.
2. Necessary Stabilizing Treatment is rendered to the patient if the hospital
has determined that urgent medical treatment is needed because it is an
emergency.
3. Restricting Transfers Until Stabilization. The hospital may not transfer
the patient until the patient is notifed of the hospitals obligation to provide
further examination and treatment, and of the risks of transfer. A physician,
or qualifed medical personnel, at the hospital certifes in writing that
transferring the patient (or unborn child) is in the patients best interests as
the treatment provided at another facility outweighs the risk of transfer.
4. The transfer is a Medically Appropriate Transfer. A medically appropriate
transfer means that the transferring facility provides necessary medical
treatment minimizing risks to the patient and/or unborn child and that the
receiving hospital has available space and qualifed medical personnel to
treat the patient and has agreed to accept the transfer.
5. The Transferring Hospital sends all medical records, informed consent and
certifcations provided under EMTALA and any other requirements imposed
by the DHHS; and the name(s) and address(es) of any on-call physician
The Health Care Revenue Cycle 22
or medical personnel who have refused or failed to appear at the hospital
within a reasonable time period to provide necessary emergency stabilizing
treatment.
6. Transfer is executed within a safe and timely fashion through the use of:
qualifed medical personnel, appropriate medical transportation equipment
and vehicles (ambulance), and appropriate life support measures.
Patient Bill of Rights
Patient Bill of Rights was developed by the American Medical Association (AMA)
guaranteeing the patient the following basic rights:
1. To receive courteous, considerate, respectful treatment in a clean and safe
environment.
2. To receive appropriate medical care that the patient understands.
3. Patient receives easily understood information about their medical treatment
plan and the consequences related to care. The right to get a second medical
opinion. The right to get an itemized statement and explanation of charges
and what fnancial obligations may result for the patient. What fnancial
assistance may exist for the patient; if the facility accepts Medicare or
Medicaid.
4. Continuity of care. What patient support services are available (welfare and
social services)..
5. Confdentiality and Privacy.
6. Participation of the patient in their own planning of health care and
execution of treatment.
7. Rights of refusal of care and the consequences of these decisions.
8. Use of grievance mechanisms.
Quality Improvement Organizations (QIO)
Quality Improvement Organizations (QIO) are a network throughout the United
States of multi-disciplinary experts responsible for each state, territory, and the
District of Columbia, whose mission is to insure the quality, effectiveness, effciency
and cost effectiveness of health care provided to Medicare benefciaries. The QIO
reports its results to the CMS.
Chapter 1 - Health Care Plans and Legislation 23
Understanding Acronyms and Abbreviations
The remainder of this chapter consists of acronyms, defnitions, and sample questions
that you might encounter if taking a test or a certifcation exam of the material
covered in this chapter. It is recommended that the student prepare fashcards to
help memorize these important concepts. There is more about fashcards in the next
section.
The health care industry operates using acronyms (letters that represent a treatment,
organization, disease, person, etc.) or abbreviations (a shortened form of a medical
term generally using letters). Sometimes a disease or medical procedure is named
after a person, such as Reynauds Syndrome, which is the name of a vascular disease
known as paroxysmal digital cyanosis; Harrington Rods, which describes a type of
orthopedic surgical instrumentation; Bennetts Fracture, which is the name of type of
bone fracture; Osgood-Schlatters Disease, which is the name of a metabolic disease;
or Bence-Jones Albuminuria, which describes a type of blood disorder.
AMA American Medical Association; Against Medical Advice
APCs Ambulatory Payment Classifcations
AOA Administration on Aging
ACF Administration for Children and Families
AFDC Aid to Families with Dependent Children
AHRQ Agency for Health Care Research and Quality
ATSDR Agency for Toxic Substances and Disease Registry
BBA Balanced Budget Act of 1997
CAH Critical Access Hospital
COBRA Consolidated Omnibus Budget Reconciliation Act of 1985
CDC Centers for Disease Control
CDT Current Dental Terminology
CMP Civil Monetary Penalties
CMPL Civil Monetary Penalty Laws
CMS Centers for Medicare and Medicaid Services
CMS-1500 Centers for Medicare and Medicaid Services 1500 billing and coding
form
CPT-4 Current Procedural Terminology, 4th edition
DC Doctor of Chiropractic
DDS or DMD Doctor of Dental Surgery or Doctor of Dental Medicine
DEFRA Defcit Reduction Act of 1984
DHHS Department of Health and Human Services
The Health Care Revenue Cycle 24
DNR Do Not Resuscitate
DO Doctor of Osteopathy (medicine)
DOJ Department of Justice
DOS Date of Service
DNR Do Not Resuscitate
DPM Doctor of Podiatric Medicine (foot doctor)
EDI Electronic Data Interchange
EGHP Employer Group Health Plan
EIN Employer Identifcation Number
EMTALA Emergency Medical Treatment and Active Labor Act
FCA False Claims Act or Lincoln Act or Qui Tam Statute or Informer Act
FDA Food and Drug Administration
FFS Fee for Service
HI Hospital Insurance (Medicare Part A)
HIPAA Health Insurance Portability and Accountability Act of 1996; aka-
Kennedy-Kassenbaum Act.
HCFA Health Care Financing Administration (old name for the CMS)
HCPCS Health Care Common Procedure Coding System
HHS Home Health Services
HMO Health Maintenance Organization
HRSA Health Resources and Services Administration
HSA Health Savings Account (formerly known as Medical Savings Accounts
or MSAs)
ICD-9-CM International Classifcation of Diseases, 9th Revision, Clinical
Modifcation
ICD-10-PCS International Classifcation of Diseases, 10th Revision, Procedure
Classifcation System
IHS Indian Health Services
IRS Internal Revenue Service
LGHP Large Group Health Plan
MAAC Maximum Allowable Actual Charge, now known as the Limiting
Charge
MCO Managed Care Organization
MHI Medicare Hospital Insurance
Chapter 1 - Health Care Plans and Legislation 25
MMA Medicare Modernization Act (aka-Medicare Prescription Drug,
Improvement and Modernization Act of 2003)
MMI Maximum Medical Improvement
MVPS Medicare Volume Performance Standard
NDC National Drug Code
NIH National Institutes of Health
NP Nurse Practioner
NPI National Provider Identifer
NPP Non-Physician Practitioner
OBRA Omnibus Budget Reconciliation Act of 1986/1989/1990
OCR Offce for Civil Rights
OD Doctor of Optometry (eye doctor)
OIG Offce of Inspector General
OPPS Outpatient Prospective Payment System
ORT Operation Restore Trust of 1995
OT Occupational Therapist
PA Physician Assistant
PCP Primary Care Physician
PHI Protected Health Information
PIN Provider Identifcation Number
POS Point-of-Service or Place of Service
PPIN Performing Provider Identifcation Number
PPO Preferred Provider Organization
PT Physical Therapist
RBRVS Resource Based Relative Value Scale
RN Registered Nurse
RRB Railroad Retirement Board
RVU Relative Value Unit
SAMHSA Substance Abuse and Mental Health Services Administration
SMI Supplementary Medical Insurance (Part B Medicare)
SSA Social Security Administration
SSI Social Security Income
ST Speech Therapist
The Health Care Revenue Cycle 26
TEFRA Tax Equity and Fiscal Responsibility Act of 1982
Title XI Civil Monetary Penalties Law (CMPL)
Title XVIII Medicare
Title XIX Medicaid
Title XXI SCHIP: State Childrens Health Insurance Program
UPIN Unique Provider Identifcation Number (Medicare)
UB-04 Hospital Inpatient (and Hospital Affliated Outpatient) billing and
coding form
QIO Quality Improvement Organization
Chapter 1 - Health Care Plans and Legislation 27
Test Taking and Study Strategies
To learn this information to a degree that you feel secure enough to be tested on it can
seem to be a daunting task, so let us suggest a few common sense and time-honored
study techniques for material of this nature.
1. First of all, do not try to memorize anything until you thoroughly
understand it. For example, if you do not understand and grasp the primary
purpose of SCHIP, it is doubtful you will be able to respond intelligently
to a question related to it. Therefore, review the material as many times as
necessary until youre comfortable with the topic. Then, whatever has to be
memorized will come naturally and effortlessly.
2. Once you feel that you have a strong grip on the major topics and the data
that relates to it, use fash cards as a review technique. Put a major topic such
as HIPAA on one side of a 3 x 5 card and on the other side place important
facts such as the date it was enacted into law, the President who signed it
into law, the defnition of the related acronym, if one is used, and a few
pertinent defning words or phrases. You will fnd it an easy and convenient
mechanism to review what you have learned. You can even carry these cards
with you anywhere and review them whenever you have the opportunity.
3. Examinations, especially those with principally multiple choice questions,
usually have time constraints (often one or two hours). In this case, it is
usually wise to spend not more that one minute on each questionmove
quickly through the questions.
4. It is imperative for you that all questions are answered. Its better to
intelligently guess than leave a question blank, since blank answers count
the same as incorrect ones. Do not make this a test taking strategy, however.
Well-designed computer programs often detect fagrant guessing and
invalidate the entire test. Of course, using good common sense is always an
excellent way to attack any multiple choice question to arrive at the correct
answer.
5. Multiple choice tests today are usually administered on a computer screen
through the testing organizations internet or intranet. Individual questions
are fashed on the screen in sequence. We strongly recommend answering
each question in sequence, re-checking your response for accuracy, and then
moving on to the next question. Skipping questions with the intent to return
later is a poor strategy because you probably will not have time to revisit it.
Concentrate on completing the test as a whole in the order the questions are
presented.
6. It is also important that you enter all data on the proper screens and use the
computer program as instructed. Avoid right clicking the mouse, striking
keys on the keyboard, and any unnecessary motion with the computer
equipment or monitor. Actions such as this sometimes result in shutting
down the examination.
The Health Care Revenue Cycle 28
Beware of Pitfalls with Multiple Choice Questions
1. It is crucial to be aware of the phrasing of questions. Details in the way
questions are expressed can cause you to choose wrong answers. For
example, in question #15, you are asked an easy questionthe defnition of
MAAC, which is an acronym for the Medicare Allowable Actual Charge.
The correct answer, therefore, is C. If youre not careful, however, you
might choose A, which switches Allowable and Actual in the defnition. Be
careful of such tricky variations.
2. The next type of question is where the test taker quickly picks out the most
important terms in the question, then focuses in on the correct answer
(questions #7, 11, 12, 13, or 14 below are examples). In question #12, the term
Resource Based Relative Value Scale is the important term in the question
that defnes the federal governments legislation known as OBRA of 1989.
The correct response B. However, the examinee has to be careful in his
or her reading and interpretation to not answer A. This is a distracter
choice: OBRA of 1986. (Answers C, D and E should be quickly
eliminated as they have no relationship to the question at all.)
3. The next type of multiple choice question, which is more diffcult, is where
the examinee concentrates on a chart or graph in order to answer the
question. The student reads the question, quickly picks out the important
terms, discerns from the graph or chart what the correct response is, and then
locates the correct answer.
4. For a question that you may not be exactly sure of the correct answer, try
removing all the answers you know are not correct. By this process of
elimination, you can often arrive at the correct one.
Chapter 1 - Health Care Plans and Legislation 29
Sample Test Questions
Here are 90 sample questions that should prepare you for taking an exam on this
chapter. They should be answered in about 90 minutes or less.
1. The two main governing bodies effecting health care change are:
A. DHHS
B. OIG
C. Medicare
D. CMS
E. A and D
Answer: E
2. Medicare, Medicaid, AFDC, Improving maternal/infant health, and assuring
drug and food safety are some of the more than 300 programs provided by:
A. CMS
B. DHHS
C. SCHIP
D. BBA of 1997
E. TEFRA
Answer: B
3. ___________ describes a program run by the CMS and other organizations for
children whose parents have too much money to be eligible for Medicaid, but
not enough money to buy private insurance.
A. Title XIX
B. BBA of 1997
C. TEFRA of 1982
D. SCHIP
E. OBRAS of 1989
Answer: D
4. _____________ is a unique 10-digit number for health care providers that will
identify the doctor or hospital making the paperwork easier to bill Medicare.
A. ICD-9-CM
B. NPI
C. OIG
D. CMP
E. EMTALA
Answer: B
The Health Care Revenue Cycle 30
5. The _____________ was developed by the AMA and guarantees the patients
courteous, considerate, and respectful treatment; appropriate health care,
continuity of care, confdentiality and privacy, refusal of care, use of grievance
mechanisms, etc.
A. EMTALA
B. QIO
C. Patient Bill of Rights
D. National Institutes of Health
E. Food and Drug Administration
Answer: C
6. _______________ establishes that the patient and unborn child receives a
medical screening examination, necessary stabilizing treatment, restricting
transfers until medically stabilized, and appropriate transfer to another
medical facility.
A. EMTALA
B. DHHS
C. Patient Bill of Rights
D. Fraud and Abuse
E. Qui Tam Statute
Answer: A
7. ___________ acts primarily as the purchaser of health care services for
Medicare and Medicaid benefciaries, establishes protocols and policies for
reimbursement of health care providers, assures that Medicare and Medicaid
are properly administered by third parties, and conducts research and assesses
the quality of health care facilities and services.
A. DHHS
B. EMTALA
C. CMS
D. Title XVIII
E. Title XXI
Answer: C
8. ______________ reimburses for the cost of physician services, outpatient
hospital services, and medical equipment and supplies.
A. Medicare Part A
B. Medicare Part B
C. Medicare Part C
D. Medicare Part D
E. SCHIP
Answer: B
Chapter 1 - Health Care Plans and Legislation 31
9. Anyone with Medicare Parts A and B is eligible to join this plan called
_____________, AKA-Medicare drug plan.
A. Medicare Part C
B. Medicare Part D
C. Title XIX
D. Title XXI
E. HIPAA
Answer: B
10. Title XVIII of the Social Security Act provides insurance coverage for:
A. people who are 65 years or older.
B. people who are disabled.
C. people with ESRD, requiring dialysis or kidney transplantation.
D. A, B, and C
Answer: D
11. _____________ eliminated the age limit previously imposed on a spouse for
health plan coverage where any active employee, age 65 or older, is eligible
for insurance coverage under their employers group health plan where the
employer has 20 or more employees.
A. OBRA of 1986
B. OBRA of 1989
C. COBRA of 1985
D. RBRVS
E. DEFRA of 1984
Answer: C
12. __________ established the Resource Based Relative Value Scale.
A. OBRA of 1986
B. OBRA of 1989
C. COBRA of 1985
D. OBRA of 1990
E. DEFRA of 1984
F. HIPAA
Answer: B
13. The __________ is comprised of three major elements: (1) fee schedule for
payment of physician services known as the RVU, (2) the MVPS, and (3) the
limiting charge.
A. OBRA of 1986
B. HIPAA
C. COBRA of 1985
D. RBRVS
E. BBA of 1997
Answer: D
The Health Care Revenue Cycle 32
14. ________ is federal legislation to make large group health plans with 100
or more employees the primary coverage for active employees who have
Medicare, or for dependents of active employees who have Medicare due to a
disability other than ESRD. This legislation also established the MAAC.
A. OBRA of 1986
B. HIPAA
C. COBRA of 1985
D. BBA of 1997
E. OBRA of 1990
F. None of the above
Answer: A
15. MAAC is an acronym that represents _____________.
A. Maximum Actual Allowable Charge
B. Maximum Attainable Allowable Charge
C. Maximum Allowable Actual Charge
D. Minimum Actuated Allowable Charge
Answer: C
16. The _____________ is the heart of the fee schedule whereby every medical
procedure recognized by Title XVIII has been assigned units of value for
resources used to provide medical services.
A. RBRVS
B. NPI
C. RVU
D. OIG
E. CMP
Answer: C
17. The Relative Value Unit is made up of _________________.
A. Work required.
B. Practice expense.
C. Continuing education expense.
D. Malpractice insurance expense.
E. A, B, and D.
F. B, C, and D.
Answer: E
18. Medicare is also known as ___________ of the Social Security Act.
A. Title XVIII
B. Title XIX
C. Title XXI
D. CMP
E. DEFRA of 1984
Answer: A
Chapter 1 - Health Care Plans and Legislation 33
19. Medicaid is also known as ___________ of the Social Security Act.
A. Title XVIII
B. Medicare Part C
C. Title XXI
D. DEFRA of 1984
E. Title XIX
Answer: E
20. The State Childrens Health Insurance Program is also known as ____________
and in __________ was extended to include children of legal immigrants and
pregnant women.
A. Title XIX; February, 2008
B. Medicare Part D; February, 2007
C. DEFRA of 1984; February, 2009
D. Title XXI; February, 2009
E. MAAC; January, 2009
Answer: D
21. Under the RBRVS, limits on what non-participating physicians can charge
Medicare benefciaries, is known as the MAAC or the __________________,
which is ___________ of the fee schedule amount.
A. Limiting Charge, 100%
B. Limiting Charge, 200%
C. Limiting Charge, 115%
D. OBRA of 1986, 115%
E. OBRA of 1989, 110%
Answer: C
22. The Kennedy-Kassenbaum Act of 1996 is also known as __________________.
A. CMP
B. OBRA of 1986
C. Medicare Part A
D. HIPAA
E. Qui Tam Statue
Answer: D
23. _______________ legislation enacted the most signifcant changes to Medicare
and Medicaid programs since they were begun and expanded the services
provided to SCHIP recipients.
A. TEFRA of 1982
B. BBA of 1997
C. Health Insurance Portability and Accountability Act of 1996
D. COBRA of 1985
E. DEFRA of 1984
Answer: B
The Health Care Revenue Cycle 34
24. The ___________ is also called the Lincoln Act, Informer Act, or the Qui
Tam Statute.
A. False Claims Act
B. CMPs
C. EMTALA
D. Patient Bill of Rights
E. QIO
Answer: A
25. The ______________ was developed by the American Medical Association
in 1975 which guarantees the patient courteous, considerate and respectful
treatment in a clean and safe environment, appropriate health care, continuity
and confdentiality of care, privacy, refusal of care, use of grievance
mechanisms, etc.
A. EMTALA
B. Civil Monetary Penalties
C. Medicare Parts A, B, C, and D
D. Title XXI
E. Patient Bill of Rights
Answer: E
26. The CMS administers the ______________ program which is designed
to monitor and improve utilization and quality of care for Medicare
benefciaries._____________ is the process of confrming the patients insurance
eligibility, collecting necessary information prior to the the patient using the
hospital or health care facility as an inpatient or outpatient, and the issuance of
an authorization number.
A. CMP; ABN
B. Medicare Parts A, B, C, and D; Pre-certifcation
C. QIO; Pre-certifcation
D. OIG; Stark Laws
E. EMTALA; Sarbanes-Oxley Act
Answer: C
27. __________ includes the incorrect coding of diagnoses or procedures and
services to maximize reimbursement, billing for services not rendered, altering
claims to receive payment, or accepting kickbacks.
A. Abuse
B. OIGs Compliance Plans
C. Fraud
D. DHHS
E. CMS
Answer: C
Chapter 1 - Health Care Plans and Legislation 35
28. ____________ includes excessive or medically unwarranted use of technology,
pharmaceuticals, equipment, and supplies; abuse of patient privacy and/or
confdentiality or duty of care to the patient.
A. Abuse
B. OIGs Compliance Plans
C. Fraud
D. DHHS
E. CMP
Answer: A
29. When Medicare has determined a provider or facility has violated Medicare
rules and regulations, for example the repeated unbundling of outpatient
surgery charges or Medicare assignment provisions, the application of
_______________ may occur.
A. Abuse
B. OIG
C. Fraud
D. DOJ
E. CMPs
Answer: E
30. Suspected health care fraud and abuse in Title XVIII programs can be reported
to ________________:
A. Medicare contractors customer service line
B. Medicares fraud department
C. 1-800-HHS-TIPS
D. OIGs fraud hotline number
E. All of the above
Answer: E
31. CMS guarantees health care security which includes:
A. Benefciaries access to affordable and quality health care services and
products.
B. Protection of the rights and dignity of its benefciaries.
C. Benefciaries receive clear and useful information; providers assist
benefciaries in making sound medical decisions.
D. All of the above.
Answer: D
32. ___________ provides coverage for inpatient hospital services, SNF, HHS, and
hospice care. ___________ was originally called the Medicare + Choice plan.
A. Medicare Part D; Medicare Part C
B. Medicare Part C; Medicare Part B
C. Medicare Part B; Medicare Part D
D. Medicare Part A; Medicare Part C
E. EMTALA; HIPAA
Answer: D
The Health Care Revenue Cycle 36
33. ______________ is also known as Medicare Advantage Plans which include
HMOs, PPOs, private FFS plans, and Special Needs plans.
A. Medicare Part D
B. Medicare Part C
C. Medicare Part B
D. Medicare Part A
E. Title XXI
Answer: B
34. Written policies and procedures, designated compliance offcer, effective
training and education, effective lines of communication, enforced standards
and well-publicized disciplinary procedures, auditing and monitoring
protocols, and responding to offenses and developing corrective action plans
constitute the _______________.
A. Title XVIII
B. Omnibus Budget Reconciliation Act of 1986
C. 7 Components of OIGs Compliance Plans
D. Civil Monetary Penalties
E. Quality Improvement Organization
Answer: C
35 ___________ establishes the following three (3) general requirements: medical
screening examinations, necessary stabilizing treatment for the patient, and
restricting transfers until patient is medically stabilized.
A. EMTALA
B. CMP
C. Title XIX
D. ICD-9-CM
E. DEFRA of 1984
Answer: A
36. The ______________ is a coding manual utilized by retail pharmacies to code
for pharmaceuticals and is maintained by the FDA.
A. ICD-9-CM
B. CDT
C. CPT-4
D. NDC
E. OIG
Answer: D
37. The ___________ is a coding manual for physician inpatient and outpatient
services and procedures, add-on codes, modifers and patient status codes.
A. ICD-9-CM
B. CDT
C. CPT-4
D. NDC
E. OIG
Answer: C
Chapter 1 - Health Care Plans and Legislation 37
38. _____________ is the manual made up numeric and alphanumeric code sets for
diagnoses, conditions, and pathologies.
A. ICD-9-CM
B. CDT
C. CPT-4
D. NDC
E. OIG
Answer: A
39. ____________ is the coding manual for dental services.
A. OIG
B. EMTALA
C. CDT
D. NPI
E. CPT-4
Answer: C
40. Fraud and abuse control are coordinated by the ____________ and
_____________.
A. OIG
B. NPI
C. CPT
D. DOJ
E. OBRA of 1986
F. A and D
G. B and C
H. HIPAA
Answer: F
41. HIPAA legislation:
A. Insures portability of health insurance when employees change jobs
B. Increases accountability of health care providers, insurers and facilities
C. Also known as Kennedy-Kassenbaum Act
D. Attempts to decrease fraud and abuse
E. Improves availability of health insurance to working families and their
children
F. All of the above
Answer: F
42. DEFRA of 1984 amended the ______________ upper age limit for active
employees who wish to enroll in the employers group insurance coverage.
A. OBRA of 1989
B. TEFRA of 1982
C. OBRA of 1986
D. RBRVS
E. BBA of 1997
Answer: B (Important)
The Health Care Revenue Cycle 38
43. ____________ is a coding manual consisting of three volumes.
A. HIPAA
B. CPT-4
C. ICD-9-CM
D. NDC
E. CDT
Answer: C
44. The ______________ is known as the heart of the fee schedule.
A. RBRVS
B. CDT
C. HIPAA
D. RVU
E. NPI
Answer: D
45. Those eligible for the Title XIX program include all of the following except:
A. Certain low income families with children
B. Aged, blind, or disabled people on SSI
C. Certain low income pregnant women and children
D. People who have very high medical bills
E. People who have COPD
Answer: E
46. The ___________ program expands health care coverage for the nations
uninsured children.
A. Title XVIII
B. Title XIX
C. Title XXI
D. HIPAA
E. OBRA of 1990
Answer: C
47. The _________________ prohibits making a false claim to get paid by the
federal government, withholding property with the intention to defraud or
willingly conceal it from the government, or making a fraudulent receipt for
government property.
A. OIG
B. FCA
C. DOJ
D. Abuse
E. HIPAA
Answer: B
Chapter 1 - Health Care Plans and Legislation 39
48. ____________ consists of three categories of numeric and alphanumeric code
sets.
A. ICD-9-CM
B. FCA
C. HIPAA
D. CPT-4
E. CDT
Answer: D
49. _____________ legislates signifcant changes to Title XVIII and Title XIX
programs, and expands services through CMS to Title XXI programs.
A. TEFRA of 1982
B. HIPAA of 1996
C. BBA of 1997
D. OBRA of 1989
E. COBRA of 1985
Answer: C
50. ____________ requires hospitals, as a condition of participation in the Medicare
and Medicaid programs, to develop and implement plans and procedures to
insure the patients right to make their own health care decisions, appoint a
Health Care Surrogate or Durable Power of Attorney, and execute their own
AMDs.
A. OBRA of 1986
B. OBRA of 1989
C. OBRA of 1990
D. TEFRA of 1982
E. HIPAA of 1996
Answer: C
51. The _____________ is a legal document where the patient determines, in
advance, what health care measures they want or do not want, if they become
incapacitated due to a terminal illness or injury.
A. DNR
B. HIPAA of 1996
C. RBRVS
D. EMTALA
E. NPI
Answer: A
52. ____________ is legislation that provided for RBRVS, RVU, MVPS, and
limiting charge.
A. DEFRA of 1984
B. OBRA of 1986
C. TEFRA of 1982
D. HIPAA of 1996
E. OBRA of 1989
F. OBRA of 1990
Answer: E
The Health Care Revenue Cycle 40
53. ___________ health insurance plan requires a gatekeeper.
A. PPO
B. POS
C. HMO
D. Indemnity
E. FFS
Answer: C
54. ___________ is the most restrictive type of health care plan.
A. PPO
B. POS
C. HMO
D. Indemnity
E. FFS
Answer: C
55. ____________ is the least restrictive type of health care plan and allows
the patient to go to any doctor or hospital they want; there are no pre-
authorizations required.
A. PPO
B. POS
C. HMO
D. Indemnity
E. FFS
F. D and E
G. A and B
Answer: F
56. _________ plan has the doctor sharing in the cost of providing care to the
patient by receiving a PMPM, also known as ____________.
A. HMO; Capitation
B. POS; FFS
C. PPO; Capitation
D. Indemnity; Deductible
E. FFS; Co-payment
Answer: A
57. The two essential types of health care plans are ___________ and
_____________.
A. FFS and HMO
B. HMO and PPO
C. POS and PPO
D. Indemnity and Managed Care
E. Indemnity and FFS
Answer: D
Chapter 1 - Health Care Plans and Legislation 41
58. The Health Care Surrogate and Power of Attorney are legally appointed by
the patient to oversee their medical decisions, if they become incapacitated, as
outlined in the _______________.
A. Indemnity insurance plan
B. EMTALA
C. PSDA
D. CMP
E. QIO
Answer: C
59. _____________ type(s) of insurance has the health care provider not share the
risk with the insurance company of the cost of providing treatment to the
patient.
A. FFS
B. Indemnity
C. PPO
D. HMO
E. POS
F. B and D
G. A, B, C, E
Answer: G
60. ____________ are the types of insurance plans that require the patient get pre-
authorizations prior to receiving certain medical services.
A. FFS
B. Indemnity
C. PPO
D. HMO
E. POS
F. C, D and E
G. A and B
Answer: F
61. ______________ defnes standards of conduct based on moral principles.
A. HIPAA
B. Fraud
C. Abuse
D. Medical Ethics
E. EMTALA
Answer: D
The Health Care Revenue Cycle 42
62. ____________ was developed by the CMS to promote correct coding of health
care services and diagnoses, and to control incorrect coding, that could lead to
inappropriate payment of Medicare Part B health care claims.
A. HIPAA
B. NCCI
C. Medical Ethics
D. EMTALA
E. Professional Liability
Answer: B
63. ___________ is when the doctor or hospital are legally responsible for the
action of their employees when it comes to billing and coding, fraud, abuse,
HIPAA, and other matters pertaining to the business of health care.
A. HIPAA
B. NCCI
C. Medical Ethics
D. EMTALA
E. Professional Liability
Answer: E
64. _____________ is defned as using more procedural codes (CPT and HCPCS)
than is normally warranted when billing for medical treatment, in order to
receive additional insurance reimbursement.
A. Unbundling
B. Professional Liability
C. Bundling
D. EMTALA
E. Professional Liability
Answer: A
65. _____________ is defned as taking several procedural codes (CPT and HCPCS)
and combining them into one code when billing for medical treatment. This
usually results in less money being paid to the doctor or hospital by the
insurance carrier.
A. Unbundling
B. Professional Liability
C. Bundling
D. EMTALA
E. Professional Liability
Answer: C
Chapter 1 - Health Care Plans and Legislation 43
66. Each physician has a separate __________ for each group or offce or clinic
in which the physician practices. ___________ is a number assigned by the
insurance carrier to a physician who renders services to their patients.
A. PPIN; PIN
B. PIN; PPIN
C. UPIN; PPIN
D. EIN: State License Number
E. SSN: PIN
Answer: A
67. The ___________ is a number the physician is assigned by Medicare.
The ___________ is a number that is assigned by HIPAA as part of its
administrative simplifcation plan.
A. State License Number; SSN
B. PIN; PPIN
C. UPIN; NPI
D. EIN; NPI
E. SSN; UPIN
F. PPIN; EIN
Answer: C
68. The ___________ is a number assigned by the IRS; is also known as the Federal
Tax Identifcation Number.
A. PPIN
B. PIN
C. UPIN
D. EIN
E. NPI
F. State License Number
Answer: D
69. Most commonly in an HMO the gatekeeper(s) is usually a:
A. Gynecologist
B. PCP
C. Oncologist
D. Pediatrician
E. A, B, D
F. All of the above
Answer: E
70. _______________ is a number the health care provider must obtain from the
state where they would like to practice.
A. SSN
B. EIN
C. PPIN
D. State License Number
E. PIN
F. UPIN
Answer: D
The Health Care Revenue Cycle 44
71. The organization that developed the ICD-9-CM coding manual is____________
and is used to code________________.
A. HCFA; diagnoses, medical screenings, causes of trauma
B. WHO; non-pathological medical situations, external causes of trauma
C. AMA; medical procedures, services and products
D. UPIN; medical procedures, services and products
Answer: B
72. The Centers for Medicare and Medicaid was formerly known as
_______________. MMI stands for _______________.
A. DHHS; Maximum Modifed Importance
B. ICD; Minimum Medical Imporatance
C. WHO; Maximum Modifed Improvement
D. HCFA; Maximum Medical Improvement
E. EMTALA; Maximum Medical Improvement
Answer: D
73. DME, orthotics and prosthetics, ambulance services and various medical
supplies and products are coded in the __________.
A. CPT
B. ICD
C. HCPCS
D. DHHS
E. EIN
F. FCA
Answer: C
74. A patient who has not been seen by their physician, or a physician of a similar
medical specialty in the same group practice, within 3 years, is known for
insurance purposes as a ____________.
A. Established Patient
B. Deceased Patient
C. Inpatient
D. New Patient
E. Discharged Patient
Answer: D
75. ____________ is defned as an MD, DO, DDS, DMD, DPM, OD, or DC that is
legally licensed to practice health care in their state. ____________ is defned as
PA, Psychologist, Clinical Social Worker, PT, OT, ST, RT, or RN.
A. Physician; Health Practitioner
B. Therapist; Nurse
C. Health Practitioner; Physician
D. State License Number; Physician
E. Inpatient; Outpatient
Answer: A
Chapter 1 - Health Care Plans and Legislation 45
76. The OIG has listed seven components in their compliance plan to avoid fraud
and abuse. They include:
A. Monitoring and auditing
B. Name a compliance offcer
C. Have written policies and protocols
D. Effective education and training
E. Enforce disciplinary procedures
F. A, B, C
G. All of the above
Answer: G
77. SCHIP covers all of the following except:
A. Inpatient and outpatient hospital services
B. Laboratory and x-ray services
C. Well-baby/child care
D. Immunizations
E. Doctors medical and surgical services
F. All of the above
G. E, D and E
Answer: F
78. Those who are deemed eligible for Title XIX benefts are referred to as:
A. Benefciary
B. Recipient
C. Relater
D. Debtor
E. Creditor
Answer: B
79. Federal law levies which of the following punishments for fling false claims
against the United States government?
A. Civil penalties
B. Criminal penalties such as jail time
C. Monetary fnes
D. Removal of the provider or hospital from participation in Medicare or
Medicaid
E. All of the above
Answer: E
80. Health care abuse includes all of the following except:
A. Insuffcient, excessive or unwarranted use of medical treatment and products
B. Abuse of authority by doctors and hospitals related to the patients privacy
C. Improper billing and coding practices
D. Billing for medical services that were not performed
E. Medically unnecessary or AMA transferring the patient to another facility
Answer: D
The Health Care Revenue Cycle 46
81. The ___________ required HCPCS coding on the UB-04 claim form for
Medicare patients for outpatient services rendered in Acute Care, Tertiary
Care, or Long Term Care Hospitals.
A. BBA of 1997
B. COBRA of 1985
C. OBRA of 1986
D. OBRA of 1989
E. PSDA
Answer: C
82. Which of following legislation expanded the services provided by the CMS
through SCHIP and established APCs?
A. BBA of 1997
B. COBRA of 1985
C. OBRA of 1986
D. OBRA of 1989
E. TEFRA of 1982
Answer: A
83. Which of the following acts provided for the RBRVS, RVU and MAAC?
A. DEFRA of 1984
B. TEFRA of 1982
C. OBRA of 1986
D. OBRA of 1989
E. HIPAA of 1996
Answer: D
84. Which of the following acts provided for employees over age 65 who are
receiving health insurance through a LGHP?
A. DEFRA of 1984
B. TEFRA of 1982
C. OBRA of 1986
D. OBRA of 1989
E. HIPAA of 1996
Answer: C
85. The _____________ raised the age limit above 69 years of age for an employee
to be eligible for EGHP (primary payer). The _____________ raised the age
limit above 69 years of age for the spouse of an employee to be eligible for
EGHP (primary payer).
A. DEFRA of 1984; COBRA of 1985
B. COBRA of 1985; TEFRA of 1982
C. DEFRA of 1984; HIPAA of 1996
D. BBA of 1997; COBRA of 1985
E. TEFRA of 1982; OBRA of 1990
Answer: A
Chapter 1 - Health Care Plans and Legislation 47
86. RBRVS is the acronym for:
A. Relative Based Resource Value Scale
B. Resource Based Relative Value Scale
C. Reporting Based Resource Value Scale
D. Resource Based Reporting Valuation Scale
Answer: B
87. MVPS is the acronym for:
A. Median Value Performance Scale
B. Medicare Value Performance Scale
C. Medicaid Value Performance Standard
D. Medicare Volume Performance Standard
Answer: D
88. HIPAA stands for:
A. Health Information Portability and Accountability Administration
B. Home Information Portability and Accountability Administration
C. Health Insured Portability and Accountability Act
D. Health Insurance Portability and Accountancy Act
E. Health Insurance Portability and Accountability Act
Answer: E
89. HCPCS:
A. Health Care Common Procedure Classifcation Standard
B. Health Care Common Procedure Coding System
C. Health Care Coding Procedure Common
D. Health Care CPT Procedure Coding
Answer: B
90. PMPM is the acronym for ______________ and is found with ___________.
A. Per Member Per Month; PPOs
B. Per Month Per Member; POSs
C. Per Membership Per Month, MCOs
D. Per Member Per Month; Indemnity Insurance
E. Per Member Per Month; HMOs
Answer: E
End of Chapter 1
Chapter 2 - Contact with Hospitals and the Doctors 49
Chapter 2 Contact with Hospitals and Doctors
Chapter Topics
Patient Registration, Admission, and Financial Concerns
Health Care Coverage in the Military
Medicare Determination of Patient Eligibility
The Medical Staff and Hospital Admitting Protocols
Census
Generally Accepted Accounting Principles (GAAP)
Understanding Acronyms and Abbreviations
More Test Taking Strategies
Sample Test Questions
After studying this chapter you will understand:
Emergency Medical Treatment and Active Labor Act (EMTALA)
Clean Claim; Registration Department Control Points
Functions of the Registrar; Pre-Admission Testing (PAT)
Primary Care Physician (PCP); Effective Patient Scheduling
Categories of Health Care Delivered to the Consumer
Explanation of Benefts (EOB); Remittance Advice (RA)
Pre-certifcation; Hospital Charges
Medical Case Management; Utilization Review
Consent; Census
Hospital Admitting Categories: Inpatients and Outpatients
TRICARE; CHAMPVA; Non-Availability Statement (NAS)
Defense Enrollment Eligibility Reporting System (DEERS)
Medicare Spell of Illness; Advanced Benefciary Notice (ABN
Coordination of Benefts (COB); Average Length of Stay (ALOS)
Medicare Secondary Payer (MSP)
Privacy Act of 1974; Skilled Nursing Facility (SNF)
Patient Self Determination Act (PSDA)
Advanced Medical Directives (AMD)
Joint Committee on Accreditation of Health Care Organizations (JCAHO)
Generally Accepted Accounting Principles (GAAP)
Joint Committee on Accreditation of Health Care Organizations (JCAHO)
The Health Care Revenue Cycle 50
Patient Registration, Admission, and Financial
Concerns
Figure 3: Hospital Registration
In the business of health care, the consumer (the patient), the spouse and family
members come into contact with many consequential people at the hospital, the
doctors offce and the insurance company. Because of the nature and complexity
of treatment and products provided to the patient, there are often other people
associated with the patient who must be kept informed.
Therefore, having effective lines of communication between the health care
providers, the hospital, the patient and their families, is essential. Furthermore,
because of the potentially large bills generated when receiving medical services
and the long periods of time the consumer may be in contact with all the providers
(hospital, doctors, medical suppliers, therapists and rehabilitation specialists), the
need for communication is crucial to the competent management of the patients
fnancial obligations.
More important, health care services and products cannot be abruptly interrupted
if payment is not made by the consumer or insurance carrier, because it could
adversely affect the patients health. Therefore, it is essential for health care providers
to maintain a successful long term relationship with the patient and the signifcant
people in their lives, to maximize a positive clinical outcome and to insure that
Chapter 2 - Contact with Hospitals and the Doctors 51
monies owed are paid in a timely fashion. The insurance company, in particular,
must be made aware of what is going on with its customer so that it can pay its part
of the medical expenses. The insurance carrier usually pays the largest percentage, so
effective dialogue with them is one of the most important aspects of the consumers
contact with the health care industry.
Registration
At the time of registration to a hospital, clinic, doctors offce, SNF or public health
facility, the following information is compiled for the patient. The information
is not always supplied by the patient, but sometimes by a family member or
guarantor. A guarantor is the person who assumes the fnancial responsibility to
pay the medical bill, but is not always the patient. The person who collects this
information is known as the registrar and may be part of the hospital or doctors
offce working in the admissions offce or registration department. The registration
or admission department has multiple duties. First of all, it collects demographic and
socioeconomic information, clinical data, fnancial/legal data, and handles clerical
matters. It also administers affliated health coverage protocols and direct physician
services (discussed shortly). The following is a representative list of the registrars
duties:
1. Collection of demographic data includes: name, address, home and work
phone numbers, age, sex, social security number, proof of identifcation like a
drivers license, etc.
2. Collection of socioeconomic data includes: names of spouse and relatives,
religion, place of worship, important contacts, etc.
3. Preparation of the medical record by collection of clinical data includes:
Chief Complaint (CC), Diagnosis (Dx), date and mechanism of injury (for
example, mva 2/7/09), diagnostic imaging studies (x-ray, MRI, CAT scan,
etc.), previous medical and non-medical providers, physical examination
results, laboratory and biopsy results, health care history, etc.
4. Collection of fnancial/legal data includes: medical insurance information,
credit card data, deductibles and co-payments, deposits, names/addresses/
phone numbers of insurance carriers (and adjusters) and person who is
responsible for the injury, etc.
5. Get the name/address/phone numbers of lawyer, date of accident (D/A),
etc.
6. Complete clerical matters such as securing patients personal property,
transportation to and from hospital, who will responsible for the patient once
discharged from hospital, etc.
Note: Demographic, socioeconomic, clinical, fnancial/legal and
clerical information are considered basic acceptable data collection by
the registrar at the time of hospital registration and admission for
the patient.
The Health Care Revenue Cycle 52
Responsibilities of the Registration Staf
As the health care industry becomes more complicated due in part to governmental
regulations for admissions, in-house procedures, discharges and fnancial matters,
the responsibilities of the registration/admission staff (known as the registrar)
have evolved into handling the following items:
1. Federal, state, and institutional rules, regulations, and specialized
paperwork.
2. EMTALA, Advanced Medical Directives, Patient Bill of Rights, An
Important Message from Medicare.
3. Medicares Advanced Benefciary Notice (ABN), HIPAA, BBA, MSP, and
other rules and regulations that affect how the patients information and
insurance are handled.
4. Managed care pre-authorizations/pre-certifcations, and second opinion for
surgery and treatment requirements.
5. Determining Average Length of Stay (ALOS) criteria. The general thrust of
the health care industry is not only to provide medically necessary treatment,
but reduce the amount of time the patient is in the hospital. The more care
that can be provided on an outpatient basis, either in the doctors offce or
patients home, the better.
6. Financial matters.
7. Facilitation of the hospital registration process: emphasize customer service
with easy patient pre-registration, selling a positive patient experience,
decrease wait times for admission/registration, timely patient contact with
a well-informed staff.
8. General Admitting Responsibilities for the Hospital Registration Staff
Public relations and education for the patient, physician and community.
Community liaison with patients case management and all pertinent
medical personnel. Get the patient in contact with a social worker, law
enforcement, welfare, housing services, etc. after the patient leaves the
hospital.
Collection of demographic, insurance, and fnancial data.
Pre-certifcation, pre-approval, and verifcation of insurance coverage.
Communication to the patient of all fnancial matters related to their
health care.
Patients Interaction with the Hospital
1. Scheduling for medical treatment.
2. Pre-registration and pre-certifcation, pre-deposit activities, inpatient
admitting.
3. Outpatient activities, discharge responsibilities, physician direct services.
4. Affliated health coverage protocols (see below).
Chapter 2 - Contact with Hospitals and the Doctors 53
Afliated Health Coverage Protocols
The registrar acts as liaison between the patient, hospital, doctor, therapists,
medical suppliers, regulatory agencies, etc. Standard responsibilities encompass the
following:
1. 24-hour access to appropriate medical personnel (doctor, Registered Nurse
[RN] or Physician Assistant [PA], etc. are kept informed of the patients
needs).
2. Telephone triage (the registrars ability to contact all the health care
providers and family members in a timely fashion and in the correct order of
necessity).
3. Referral services for other physicians, therapists, treatment or durable
medical equipment (DME) so the patient gets the health care they need in a
timely fashion.
4. Customer Service, including medical education of the public, so the patient
and their families understand what health care they are receiving and the
ramifcations of this care, as well as the costs of treatment.
5. Compliance of monitoring protocols. In other words, the registrar makes
sure the hospital and doctor meet state and federal rules when handling
the patient. HIPAA compliance is of utmost importance. It all must be
documented in writing. For example, the registrar makes sure the patient
does not become an outlier. An outlier is a patient whose treatment and
time in the hospital exceeds what is normally expected for the diagnosis,
prognosis, age, sex and history.
Physician Direct Services
These are services that help the medical staff do their job. The registration
department many times is instrumental in providing these services, and they include:
1. Community and hospital physician referrals (telling the patient what doctors
to go to for their needs) and marketing to the public.
2. Primary Care Physician (PCP) notifcation of their patients who are admitted
for hospital emergency services (ER).
3. Hospital physician outbound call services (making sure the doctors at the
hospital can contact the patient and their families once out of the hospital).
The Clean Claim and the Hospital Registration Staf
1. Adequate and accurate collection of all patient data so that a Clean Claim
can be produced is most important! A clean claim is created on a CMS-1500
(for non-hospital outpatient, laboratory, DME, orthotics, prostheses) or a UB-
04 (for hospital inpatients and outpatients) coding and billing forms, that are
sent to the insurance carrier for payment (either electronically or paper) with
no delays in reimbursement. The data on these forms can be reviewed by the
insurance carrier or a peer review organization (PRO). No additional contact
with the provider or hospital is necessary and a clean claim should pass all
The Health Care Revenue Cycle 54
edits with no delays in reimbursement. A PRO is a panel of doctors who
work for the insurance company, a state licensing board, or a clearinghouse
that reviews the CMS-1500 and UB-04 and the patients treatment record to
determine medical necessity, errors in billing and coding, fraud and abuse,
utilization issues in providing medical care, malpractice, etc. The PRO may
be called in to review why the patient has become an outlier and was not
discharged earlier from the hospital.
2. Creation of the permanent patient medical fle (electronically and paper) is
an essential function of the registrar so a legal record is produced.
3. Generating the permanent patient identifcation process for the hospital
computer system is important so the patient can be accurately identifed for
billing purposes and the correct provision of medical services, medical record
storage is accomplished, and treatment mistakes are reduced.
4. A clean claim has the following characteristics:
It is valid all information is accurate and spelled correctly.
It is complete all required information is provided.
It can successfully pass inspection for payment by a third-party
(insurance company, PRO, clearinghouse, or auditor) without further
intervention by the health care provider or treatment facility.
According to HIPAA Privacy Rule, providers and hospitals may legally
use the patients information they collect for treatment and payment
purposes, staff training, compliance issues, and quality improvement.
The information collected is known as TPO: T = Treatment, primarily
for the purpose of the doctor discussing the patients case with other
providers; P = Payment, so the provider can submit insurance claims
on behalf of the patient to get paid; O = Operations, for the purpose
of staff training (the attending physician training medical students
and residents, for example) and quality improvement at the hospital.
The information taken from the patient is known as Protected Health
Information (PHI).
5. Accurate and complete collection of insurance and billing data during the
registration process is essential for the generation of a Clean Claim so that
insurance reimbursement is not delayed. In all cases of insurance coverage,
the registrar should collect the following:
Copy of the insurance card(s), front and back, Medicare card, and any
other third party information.
Patients drivers license and SSN (Social Security Number).
All the pertinent demographics.
Complete fnancial data.
Billing information; Occurrence, Value, Revenue, Condition, ICD and
CPT codes; and other required data for the UB-04 or CMS-1500 forms.
Chapter 2 - Contact with Hospitals and the Doctors 55
Financial Counselor
The role of the registrar as fnancial counselor in the registration and admission process
has changed over the years to include the following:
1. Verify patient demographics, insurance (third party payers), and basic
fnancial information so that a determination of the patients ability to pay
can be made.
2. Explain to the patient the hospitals collection policy. It must be stressed to
the patient the importance of paying medical bills on time.
3. Determine the patients estimated fnancial responsibility and request payment in
full at the time of admission to the hospital.
4. Establish payment arrangements if the patient cannot pay in full.
5. Obtain all information regarding third party payers so that insurance
verifcation and pre-certifcations can be made in a timely fashion.
6. Complete all pre-admission paperwork to minimize patient dissatisfaction
and maximize the patients positive experience with the doctor and hospital.
7. A good pre-registration process will emphasize the selling of a positive
experience with the hospital or doctors offce, decrease the amount of
dissatisfaction by both the patient and health care staff, and reduce the
number of complaints. In todays competitive business environment, the
hospital or doctors offce must sell themselves like any retail operation
to the public, patient and their families. Not only does this increase repeat
business and referrals, but it also reduces potential malpractice lawsuits.
Summary
To summarize thus far, a consistent and well-executed pre-registration (which
includes the pre-admission) system will:
1. Firmly establish all fnancial matters with the patient and guarantor in
advance of the provision of health care services.
2. Clearly identify all insurance beneft limitations before health care services
are provided. The patient should know how his/her health care will be paid
and by whom.
3. Clearly identify all deductibles, copayments, co-insurances and deposits to
be collected prior to health care services being provided.
4. Accurately and completely collect all fnancial, insurance, demographic and
socioeconomic data, and satisfy all clerical issues, so that a CLEAN CLAIM
is generated!
5. Be completed at least 24 hours prior to admission, also known as the pre-
admission.
6. A patient is more inclined to pay the deposit, copayments, co-insurances and
satisfy their deductibles, at the time of admission (when there is a sense of
urgency!), than after the insurance carrier has paid the claim and the patient
The Health Care Revenue Cycle 56
has been discharged from the hospital. The patient will be made aware of all
payments, charges, and balances due to the hospital and physician because
the insurance carrier will issue an Explanation of Benefts (EOB) to the patient
and a Remittance Advice (RA) to the health care facility and provider.
7. Outline all health care treatment, services, and products that are planned
and exact dates when they are to be scheduled and performed by the doctor
and medical staff. Make sure the patient knows exactly who will provide what
services, how the patient and family can contact the doctor(s), and how long
the patient will be in the hospital, if possible. This will help in establishing a
good rapport with the patient and their family, and maximize the selling of
a positive health care experience.
8. It is recommended that 70% to 90% of all scheduled admissions to the
hospital be pre-registered within 24 hours of the date of treatment. If the pre-
registration, collection, and pre-verifcation system are consistent and
thorough, fnancial risk to the hospital and provider, and patient anxiety and
confusion, are reduced.
9. The Deposit is the estimated portion of the hospital bill not covered by patients
insurance coverage. Payment can be made prior to admission, at admission, or
at time of discharge. The deposit can be paid by the patient in full or fnanced
over time. However, paying the deposit in-full at the time of pre-admission
is to the hospitals and patients advantage. Because there is a sense of urgency
on the part of the patient to handle all fnancial criteria prior to treatment,
the patients anxiety level is reduced. The hospital, of course, reduces its
collection expenses and improves its cash fow position.
10. Collecting the Deposit:
Advantages
Increases cash fow for hospital.
Reduces amounts due at discharge for the patient.
Reduces the accounts receivable (A/R) for hospital.
Reduces bad (uncollectable) debt for hospital.
Disadvantages
Creates possible public relations problems between hospital, doctor, and
patient.
Damages the selling of a good hospital experience to the patient
and family. The public generally has a distorted view of doctors and
hospitals. They believe that health care services are grossly expensive,
and that medical bills and the methods insurance companies use to pay
for them are incomprehensible. Furthermore, the public generally holds
the misconception that the doctor and hospital are affuent and should
not be so insistent in collecting their money; that they are in health care
to primarily help the patient (altruistic) with no regard to the expenses
involved. Patients and their families often think that money should not
even be a consideration for the doctor and hospital. The public fails to
Chapter 2 - Contact with Hospitals and the Doctors 57
understand that health care is a business, and runs on funds like any
other business. Therefore, handling the patient and money when it
comes to health care requires sensitivity and common sense.
11. Before the hospitals registrar can calculate the patients fnancial obligations,
particularly the deposit at pre-admission, the following must be taken into
consideration:
Most important: third party insurance plan reimbursement for medical
services provided.
The average length of stay (ALOS) per the diagnosis and the admitting
physicians estimate.
The average cost of the hospital stay by medical or surgical specialty.
For example, the costs for neurosurgery can easily run tens of thousands
of dollars compared to an appendectomy or setting a simple fracture.
The average cost of outpatient procedures being conducted, such as
CBC, urinalysis (UA), x-rays, CAT scan, biopsy, etc.
Third party payer fee schedule hospitals DRG, fat rate, contractual
payer allowances (these terms means how much the hospital and doctor
will be paid according to pre-determined insurance and Medicare
payment schedules).
Intensive care unit (ICU), Critical care unit (CCU), Progressive care unit
(PCU), private, semi-private per diem room charges.
Other than urgent care or emergency room treatment, collection of the patients
portion of health care services is highly desirable for both fnancial and public
relations reasons during pre-admission.
EMTALA, however, forbids the registrar from addressing the consumers
fnancial obligations, collection of any monies, or contact with the
insurance company for coverage verifcation or pre-certifcation
numbers, until the patient is stabilized in emergency situations.
Efective Patient Scheduling
Effective Patient Scheduling insures maximum productivity in the hospital or
doctors offce. The effcient administration of medical services is essential, to keep
dissatisfaction to a minimum by physician, clinical staff, patient, and administrative
personnel. A balance between collecting the necessary demographic, clinical,
fnancial, legal, and insurance information from the patient, and providing medically
necessary clinical services to the patient in a timely fashion, is the goal of optimal
patient scheduling. Patient scheduling is usually performed by the registrar.
Advantages of Pre-Admitting Patients
There are major advantages for pre-admitting patients:
1. Maximizing patient familiarity with admissions process.
2. Minimizing admission time.
The Health Care Revenue Cycle 58
3. Hospital room, facility needs, and pre-admission diagnostic services (EKG,
laboratory, imaging, biopsy) can be anticipated and provided in a timely fashion
by reducing any surprises for the patient. Pre-admission testing (PAT) is
particularly important, as diagnostic medical testing in advance of providing
treatment, are critical for the patient and doctor and facility so that surgical/
hospitalization suitability can be determined for the patient prior to being
admitted. PAT helps the doctor determine what treatment is to be provided
before the patient is admitted to the hospital and takes into account any
medical history (such as diabetes, cancer, or hemophilia), which would have
negative consequences if surgery is to be performed due to retarded healing
and bleeding problems.
4. Insurance resources, forms, and requirements (for example, pre-
certifcation) can be completed and validated prior to the delivery of treatment.
It is important the patient sign and date the Assignment of Benefts
allowing the hospital or doctor to release medical information to the
insurance company so the claim can be processed and paid (Block #12 in the
CMS-1500 claim form). It is also imperative the patient sign the I authorize
payment of medical benefts (to the hospital or doctor or supplier) so they
can be paid directly by the insurance carrier (Block #13 in the CMS-1500
claim form). If block #13 is not signed, the check would be sent to the patient
and the provider would have to seek out the patient for payment.
5. Financial counseling can be provided prior to the delivery of hospital
services. Therefore un-reimbursable care can be determined early. This is
important for the hospitals accounting department and cash fow. The
hospital should know in advance if they should pursue obtaining welfare
reimbursement for the patient to help pay the bill.
6. Copayments, deductibles, and deposits can be determined and collected
prior to services being delivered.
7. Second opinions for surgery and other procedures or tests can be conducted
prior to treatment being rendered.
8. Patient anxiety is reduced, as the patient is more fully aware of all fnancial
obligations and health care procedures and tests are explained in advance of
treatment being delivered. This helps in the selling of a positive health care
experience to the consumer (good public relations).
Disadvantages of Pre-Admitting Patients
Disadvantages of pre-admitting patients include:
1. Actual dates of hospital admission are not always known in advance. The
practice of medicine is not exact and cannot always be predicted.
2. Insurance forms, consent forms, and other paperwork are forgotten by the
patient, or are delayed, invalid, or incomplete.
3. Insurance pre-certifcation and pre-verifcation cannot always be
satisfactorily completed in a timely fashion.
Chapter 2 - Contact with Hospitals and the Doctors 59
4. Patient forgets to bring valid and current insurance information,
identifcation data, social security information, or does not adequately
complete demographic information; patients and/or guarantors writing is
illegible.
The Five Control Points
There are fve control points during which the registrar has an opportunity to
complete the registration and fnancial requirements of a patients hospital stay. They
are as follows:
1. Pre-admission
2. Admission
3. While the patient is in the hospital receiving treatment
4. At discharge
5. Post-discharge (at home, while recuperating)
Pre-Certifcation
Pre-certifcation is the mechanism of verifying insurance coverage, authorizing
medical necessity for treatment, and data collection prior to the patients admission
to the hospital.
1. Pre-certifcation does not insure that the claim will be paid under the
insurance policys provisions.
2. Ultimately, it is the policyholders (patient) obligation to get the necessary pre-
certifcations and pre-authorizations from the insurance company. However, as
a courtesy and good public relations, the hospital usually provides this
customer service.
3. The end result is elimination of payment delays, reduction of fnancial risk and bad
debt, and to make the pre-admission and registration process an agreeable
experience for the consumer.
4. The purpose of insurance verifcation is as follows:
Calculation of pre-certifcation and pre-authorization benefts (most
insurance plans limit how much treatment they will pay for and how
long they will pay for it).
Surgical second opinion determinations are on fle. Especially for
expensive surgeries or cancer therapies, the insurance company many
times wants to make sure the treatment is verifed by another doctor.
Deductibles, co-payments, deposits, and any other out-of-pocket
expenses collected
Name of the third party administrator (TPA) handling the claim for the
employer is confrmed. A TPA is sometimes used as an intermediary
between the patient and employer (who is self-insured) that handles
collecting premiums, processing, and paying claims.
The Health Care Revenue Cycle 60
Names, addresses and phone numbers of insurance adjusters, lawyers,
employers and claims offces are confrmed.
5. An employer that is self-insured creates healthcare coverage for its
employees that does not use an outside insurance company, but funds their
own healthcare coverage for their own employees.
Medical Case Management/Utilization Review
As the health care industry becomes more complex, the role of the utilization
review nurse (a member of the nursing staff, PRO or insurance company), and the
registration and fnancial services and admissions staff, has become increasingly
more interdependent. Examples of some of these mutual obligations include:
1. Liaison with the PCP and specialty physicians; liaison with the hospital and
insurance carriers utilization department.
2. Reduction of unnecessary admissions and effcient management of the
ALOS.
3. Assist the patient with discharge matters and insurance appeals process
when treatment is denied.
4. Pre-certifcation and re-authorization approvals.
Important Criteria for Registering Patients with Managed Care
Coverage
1. Check carefully consumers with insurance coverage endorsed by Health
Maintenance Organizations (HMOs), Preferred Provider Organizations
(PPOs) and Point of Service plans (POS)
2. Information that must be collected to process payment for hospital and
provider services include:
Pre-certifcation and pre-authorization requirements, numbers,
signatures, and forms.
Utilization of only in-network or participating health care facilities,
hospitals, and providers. Name and address and phone number of the
gatekeeper.
Collection of co-payments.
Consent
Consent is the hospitals legal way to get the patients permission to be admitted to
the hospital (inpatient or outpatient) to receive treatment. Signed release forms are
essential to legally obtain the patients consent for care. It is usually the registrars
responsibility to get the patients consent at pre-admission or admission to the
hospital or doctors offce. Normally parents or guardians of a minor, married or
divorced, regardless of any divorce judgments, are legally responsible for giving
consent for health care and are fnancially responsible for the health care costs of their
child.
Chapter 2 - Contact with Hospitals and the Doctors 61
Emancipated Minor, for health care purposes, is a patient who has not reached the
age of majority, has been liberated from their parents, and has been granted the same
responsibilities and fnancial obligations as an adult. Therefore, an emancipated
minor would make their own medical decisions. The age of majority is 18 to 21 years
(varies from state to state).
An emancipated minor is where a court of law has liberated the child (declared an
adult) on the basis of the following:
1. The child no longer requires parental guidance or fnancial assistance.
2. The child fathered or gave birth to a child.
3. The child has reached the age of majority.
Six Types of Consent
1. General Consent involves getting permission from the patient to receive
routine laboratory testing such as a complete blood count (CBC) or urinalysis
(UA), diagnostic imaging (x-rays, MRIs, CAT scans) and general medical
screening and treatment.
2. Special Consent involves getting permission from the patient to receive
HIV testing; major/minor surgery; anesthesia; non-surgical procedures with
more than a minimal risk of body structure alteration; Cobalt, chemotherapy
or radiation therapy; Psychiatric or electroshock therapy; experimental
procedures; and treatment for drug and alcohol abuse/disorders.
3. Expressed Consent can be written or oral with the patient allowing the
treatment recommend by the medical staff.
4. Implied Consent in Fact is agreement for treatment by the patients silence,
by the patient not objecting.
5. Implied Consent by Law is legal agreement for treatment because the
patient is unconscious, includes transportation to the emergency room, and
the law allows health care treatment to proceed.
6. Informed Consent is where the patient understands why he or she is
receiving treatment and what health care services are being performed and
agrees to the treatment to be provided.
The Health Care Revenue Cycle 62
Hospital Admitting Categories
Figure 4: Hospital Admitting Categories
1. Inpatient: Patient is formally admitted to the hospital overnight and
occupies a bed (upon the doctors order) for more specialized and intensive
diagnostic, laboratory, medical and surgical services. It is the hospitals
obligation for continued care after discharge of the patient.
2. Outpatient: The patient in this case is not admitted to the hospital overnight
and usually is treated and discharged within the same day. An outpatient can
become an inpatient if it is medically warranted.
Emergency: Patient receives immediate medical screening, diagnosis and
treatment on an unscheduled basis in the hospitals emergency or urgent
care facilities, but not admitted for inpatient or observation services. The
hospital is responsible for the emergency outpatient while under care
and until discharge. Frequently the hospital will recommend the patient
see their personal doctor once discharged from the E/R and return if any
complications occur.
Clinic: Patient receives diagnosis and treatment in the hospitals
medical or surgical facilities on an ambulatory basis. It is the hospitals
obligation for continued care until the diagnosis is resolved, and it is
the hospitals responsibility to discharge the patient from treatment. In
this case the patient may go back and forth from the clinic over a period
of days or weeks until the diagnosis is resolved.
Chapter 2 - Contact with Hospitals and the Doctors 63
Private or Referred: Patient is referred by patients private physician
for diagnosis and treatment on an ambulatory basis at the hospital. The
outpatient will return to his/her private physician, and it is the private
physicians obligation for continued care and discharge from care. The private
physician, if on the hospitals staff, can also admit the patient to the
hospital if medically warranted.
Ambulatory: Broader and less specialized diagnostic, medical and
surgical care provided to the outpatient in this setting. Examples would
include podiatric (foot) surgery, plastic surgery, or other minor surgery
for cuts or abrasions. The ambulatory surgical center (ASC) would
handle this type of outpatient.
Same Day Surgery: The patient receives surgical services on an
ambulatory basis and does not require hospital admission. The hospital
is responsible for the patients condition only while under care. This
designation could include the clinic or private outpatient, or ambulatory
surgical center (ASC).
Categories of Health Care Charges (also known as Rates)
1. Actual: The true dollar amount the provider or supplier or hospital bills
Medicare or other third party payers for services rendered. For example,
although the appendectomy was billed by the surgeon for $3,000 (the actual
charge), Medicares approved charge or approved amount is $2,200. If the
surgeon is a participating provider with Medicare, she must accept the
$2,200 as payment in full, plus collecting any co-payments, co-insurances or
deductibles.
2. Approved: What Medicare will reimburse the hospital or provider for
each service, which is dependent on what part of the country treatment
is provided. This is Medicares fee schedule, the highest amount of money
Medicare will pay, no matter what the hospital or doctor bills Medicare.
$2,200 would be the approved charge (see Actual charge above).
3. Prevailing: Market determined or going rate for the cost of medical
services and products in a particular geographic area, for example New
York City metropolitan area. The fees charged by doctors in New York may
exceed or be less than the payment Medicare approves in its fee schedule.
If the doctor is a participating provider with Medicare, they must accept
what Medicare pays and cannot charge the patient more money to collect
the balance (balance billing). For New York City, for example, the prevailing
rate (what Medicare will pay) is $2,200 for an appendectomy. However, for
Oklahoma City the prevailing rate for an appendectomy would be $1,500. It
costs a lot more to perform this surgery in New York City than in Oklahoma
City. Even if the doctor bills Medicare $5,000 for an appendectomy, Medicare
will only pay the doctor $2,200 if performed in New York City.
4. Usual, Customary and Reasonable (UCR): What most health care providers
or facilities charge for a particular procedure or service within a geographic
region. For example, a New York hospitals fee for a service would be
The Health Care Revenue Cycle 64
considered UCR if it fell within what most other hospitals charge within
the New York City metropolitan area for that particular treatment.
5. Global: Total amount paid by Medicare, which consists of the professional
fee (what the doctor charges for performing surgery, making a diagnosis,
interpreting x-rays or laboratory studies) and the technical fee (the cost of
producing the x-ray or laboratory analysis or surgical procedure; fee for
use of hospitals surgical suite, anesthesia, supplies, equipment). When this
charge is for surgery, it is known as a Global Surgery charge or Surgical Package.
Categories of Health Care Delivered to the Consumer
1. Acute Inpatient Care is a level of short-term urgent health care that is
delivered to a patient suffering from acute disease or trauma, which may
be life-threatening. It is generally administered in the hospitals emergency
room (ER) or urgent care facility. This type of care is short-term (days) rather than
long-term (weeks or months) or chronic (years) in nature.
2. Observation Care is health care administered in a hospital where the patient
occupies a bed and is monitored by the nursing staff, to ascertain the need for
possible hospital admission. Observation services usually do not exceed 24
hours, and CMS has established guidelines that insurance claims submitted
for observation care exceeding 48 hours will be reviewed for medical
necessity. Important: Outpatient observation services cannot be substituted
for medically appropriate inpatient hospitalization. The hospital must decide
quickly whether to treat the patient in the ER and discharge them, or admit
as an inpatient.
3. Outpatient Care pertains to the patient receiving treatment at a hospital,
clinic, ambulatory surgical center (ASC), outpatient center, laboratory or
radiologic facilities, but is not hospitalized as an inpatient.
4. Long-term Care (LTC) is reserved for patients who are chronically ill,
permanently or temporarily disabled or those afficted with Alzheimers
disease. Services include 24-hour nursing care; rehabilitation such as
physical, speech, and occupational therapy; help and training with Activities
of Daily Living (ADLs) such as eating, toileting, dressing, bathing; and
rehabilitation directed to assist those transitioning from hospital to home.
Coverage for LTC and Skilled Nursing Facility (SNF) services is provided
through Medicare (Title XVIII) for up to 100 days per calendar year, and
Medicaid (Title XIX) for those who have limited fnancial resources.
5. Hospice Care is made available to terminally ill patients and support for their
families through not-for-proft hospice organizations. This type of care is
covered under Medicare and Medicaid.
6. Respite Care is short term custodial supervision that provides the family
member or other unpaid caregiver relief from caring for an elderly, frail, ill,
disabled, or dependent person at home. Respite care is covered under Medicare
and Medicaid. In other words, someone else replaces the full-time caregiver
for a short time to give them a break.
Chapter 2 - Contact with Hospitals and the Doctors 65
7. Custodial Care provides assistance to the individual to meet personal needs
such as shopping, dressing, cleaning the house, personal hygiene, paying
bills, companionship, etc. This type of service may be provided by those
persons who do not have professional health care training and are not covered by
Medicare.
8. Home Health Care provides the individual at their residence rehabilitative
care, supportive care, physical or occupational therapy, or other therapeutic
care. In order to be reimbursed by Medicare, the physician must certify
that the patient is home-bound and in need of intermittent skilled nursing
services and therapy, with an established plan of treatment and care.
9. Gatekeeper is the role of the Primary Care Provider (PCP) in closed panel
managed care organizations. The PCP is the initial contact for the consumer
with the managed care organization (MCO). The gatekeeper controls the
patients access to all medical care and hospitals. The patient must go
through the gatekeeper for all medical referrals, treatment, diagnostic
and laboratory work. A closed panel is defned as a limited number of health
care providers and facilities the MCO contracts with to provide services to
its membership, who sign an agreement to provide services to the MCOs
benefciaries at a pre-agreed fee. MCOs include HMOs, PPOs and POSs.
Health Care Coverage in the Military
Figure 5: Health Care Coverage in the Military
The Health Care Revenue Cycle 66
CHAMPVA (Civilian Health and Medical Program of the Veterans Administration)
This is a Veterans Administration (VA) program for veterans (and their spouses and
children) with total or permanent service-connected disabilities, or the spouses and
children of veterans who died as a result of military related disabilities. Veterans
are those men and women who have served in the Army, Navy, Marines, Air Force,
Coast Guard and reserves and have been discharged.
TRICARE
Is a regionally administered health care plan for active duty and retired members of the
uniformed services (those who are serving or did serve in the Army, Navy, Air Force,
Marines, Coast Guard, etc.) TRICARE is the new name for CHAMPUS. For any
member of the military, or their spouse or family, to be enrolled in a military health
care plan, they must be listed in the Defense Enrollment Eligibility Reporting System
(DEERS).
Note: Be careful not to confuse CHAMPUS with CHAMPVA.
1. The three types of TRICARE coverage are:
TRICARE Prime is where Military Treatment Facilities (MTF) are the
principal source of health care delivery for active duty personnel. They
pay no fees for any medical service they receive. A MTF is a health care facility
operated by one of the branches of the Army, Navy, Marines, Coast
Guard, Air Force, etc., such as Veterans Administration hospitals or
clinics, feld hospitals (places that provide health care on the battlefeld)
or facilities located in militarily active areas, or any other health care
facilities operated in active or non-active areas anywhere in the world.
TRICARE Extra is a preferred provider organization (PPO) that operates
just like those offered to the general public. A Non-Availability Statement
(NAS) is required before any non-emergency hospital inpatient services
are provided by a non-MTF, such as a civilian hospital or civilian doctors
offce. Civilian means not affliated with the military.
TRICARE Standard is a fee-for-service (FFS) health plan that operates
just like those offered to the general public. This type of health plan uses
a Diagnosis Related Group (DRG) payment system (which is a fee schedule
listing how much will be paid for different types of treatment) for acute
care in hospitals in 49 states, District of Columbia, and Puerto Rico.
Maryland is exempt from the DRG payment system. A NAS is required
before any non-emergency hospital inpatient services are provided by a non-
MTF.
Important: TRICARE Extra and TRICARE Standard both require an NAS
before non-emergency treatment is provided at civilian hospitals and civilian
doctors. See #5 below for further discussion of the NAS
2. Federal law mandates that any civilian hospital participating in Medicare also
participate in TRICARE Standard for in-patient hospital services, so members
of the military can get treatment in a civilian hospital or non-MTF.
Chapter 2 - Contact with Hospitals and the Doctors 67
3. Those who are not eligible for TRICARE include:
Most people who are eligible for Medicare and are over 65 years of
age, are not eligible for TRICARE, unless they are a family member of
someone on active duty in the military.
Someone who is Medicare eligible due to a disability or end stage renal
disease (ESRD), and less than 65 years of age, can have TRICARE until
age 65, but also must be enrolled in Medicare Part B.
After age 65, these individuals lose their TRICARE health plan and must
enroll in Medicare.
4. TRICARE for Life is an expanded TRICARE program for Medicare-eligible
military retirees who are 65 or older, their eligible family members and
survivors, and certain former spouses. In order to qualify for TRICARE
for Life benefts, the member must also be enrolled in Medicare Parts A and B.
There are no premiums for TRICARE for Life and Medicare Part A, except
for Medicare Part B coverage which requires the payment of a premium.
TRICARE for Life is the secondary payer to Medicare. TRICARE for Life
pays for any out-of-pocket expenses for treatment after Medicare has paid
frst.
5. The Non-Availability Statement (NAS) is required before any non-
emergency hospital inpatient services are provided to a TRICARE Extra or
Standard benefciary by a non-MTF. The NAS is valid for 30 days after it is
issued and only for pre-approved treatment. It can be used from the date of
the hospital admission until 15 days after discharge (for any follow-up care).
Note: Understanding the NAS is not easy, so its recommended that you
read this section several times. You may also want to research the NAS on the
internet.
Exclusions to NAS requirements include:
If the benefciary has health insurance coverage that is primary to
TRICARE.
Any outpatient emergency medical or psychiatric treatment.
Skilled Nursing Facility (SNF) or Residential Treatment Center (RTC)
admissions; treatment in a student infrmary (found at a trade school,
college or university).
Any health benefts mandated under the Program for Persons with
Disabilities.
Medical care received outside the catchment area (a geographical area
made up of so many square miles) of an MTF, which consists of an area
of 40 miles. For example, if the VA hospital is located in Philadelphia,
PA, then the catchment area would include a geographical area 40 miles
in any direction from the Philadelphia VA. The area 40 miles north
to Allentown, PA, 40 miles east to Atlantic City, NJ, 40 miles south to
Wilmington, DE,. and 40 miles west to Lancaster, PA, would be the
catchment area for the Philadelphia VA.
The Health Care Revenue Cycle 68
When the patient has other health insurance THAT IS NOT TRICARE Standard,
such as Blue Cross/Blue Shield, this other health insurance is primary. Tricare
Standard will share the cost of non-emergency inpatient hospital care, without a
NAS, in this case. Providers should be aware that even if the MTF issues a NAS,
this neither guarantees payment nor authorizes that TRICARE Standard will pay at
all.
TRICARE is primary coverage when the patient also has Medicaid, Indian
Health Service (IHS) obtaining non-IHS care, or other insurance coverage for
out-of-pocket medical expenses. TRICARE pays second when the patient has
medical coverage under workers compensation, personal injury protection,
no-fault, uninsured motorist insurance under the patients automobile policy,
student health care insurance, Health Maintenance Organization insurance
(HMO), or Preferred Provider Organization insurance (PPO).
6. With maternity care, the date when the pregnant patient starts with prenatal
care with a civilian doctor, this is determined to be the Date of Admission, as
far as TRICARE is concerned. Moreover, since maternity care is considered not
an emergency, an NAS is required if the mother chooses to use civilian doctors and
hospitals. The NAS is valid for 42 days following the end of the pregnancy.
7. Submission of TRICARE claims must be within one (1) year of the date
when treatment was rendered; otherwise late, invalid, and/or incomplete
claims will not be processed or paid.
8. Information necessary for the timely payment of TRICARE claims include:
Patients name, date of birth (DOB), social security number (SSN),
sponsor or patient (as listed on the Military Identifcation Card)
Other pertinent health insurance information
CPT, HCPCS and ICD codes; dates of service (DOS)
Treatment Authorization Number (TAN)
Providers and/or hospitals tax identifcation number or SSN
Defense Enrollment Eligibility Reporting System (DEERS).
This is a computerized database, operated by the Department of Defense (DOD), and
utilized by TRICARE contractors (providers of health care services to the military)
to substantiate what military health care plans are available for the benefciary (and their
families). DEERS also lists exactly what persons can get health care.
Continued Health Care Beneft Program (CHCBP)
1. Provides health care benefts to former members of the military and their
families for 18 to 36 months after separation from active duty or loss of
eligibility for military health benefts.
2. The member of the military must enroll in CHCBP within 60 days from leaving
the military, or loss of eligibility, in order to continue coverage under the
CHCBP program.
3. CHCBP provides the same coverage as the TRICARE Standard program.
Chapter 2 - Contact with Hospitals and the Doctors 69
Medicare Determination of Patient
Eligibility
Medical Spell of Illness
Defnition: Medical Spell of Illness, also referred to as the Beneft Period, commences
when the patient is admitted to the hospital or SNF, and terminates sixty (60)
consecutive days after the fnal discharge. A benefciary can be moved from the
hospital to a SNF and back again an unlimited number of times, provided no more
than 60 consecutive (continuous) days have elapsed between each discharge and
readmission. All these transfers from the hospital to the SNF and home and then back
again to the hospital and SNF, etc., would be considered the same Spell of Illness.
Once a Spell of Illness has ended, the patients next admission to a hospital or SNF
will constitute a new Beneft Period. There is no limit on the number of Beneft
Periods. Each new Spell of Illness, however, will generate a new inpatient deductible
that has to be paid by the patient. For year 2009, the deductible for Medicare Part
A which covers hospitalization and SNF, for each Spell of Illness, is $1,068.00. For
example, if the patient has fve Spells of Illness in 2009, the patient would pay (5 X
$1,068=) $5,340.
See www.medicare.gov for more information on Medicare deductibles, copayments,
and premiums.
Hospital Inpatient Beneft Days Coverage (see also p. 118-119)
Medicare Part A pays for 150 days of inpatient hospitalization per calendar year,
with coverage arranged into 60 day, 30 day, and 60 day reimbursement periods (60-
30-60). The initial 60 days are called full days or covered days and are paid in full
by Medicare except for the annual deductible, which is paid by the patient (for 2009:
$1,068.00 for each Spell of Illness). The next 30 days are known as the co-insurance
days, as Medicare will pay for these days less the daily co-insurance amount (for
2009: $267.00 per day of hospitalization). These frst 90 days of the total of 150 days,
full/covered days and co-insurance days, are known as renewable as they can be
used repeatedly with each new beneft period or Spell of Illness.
The last 60 days of the 150 days are referred to as Non-Renewable, or Lifetime
Reserve Days (LTR). The Medicare patient has these 60 LTR days available once in
a lifetime. Once they are utilized, they are gone forever. LTR co-insurance for 2009 is
$534.00 per day of hospitalization. If the patient elects not to use these LTR days, then
the patient is responsible for all inpatient costs incurred during this time period.
Skilled Nursing Facility Coverage (SNF) (see also p. 118-119)
For Medicare to pay for treatment in a SNF, the benefciary must frst be an inpatient
in a hospital for at least three consecutive days, not including the day of discharge,
before being admitted to a SNF for skilled and/or special medical services. SNF care
does not cover custodial care. Medicare pays for 100 days of care per calendar year.
The frst 20 days are paid entirely by Medicare. The benefciarys responsibility for
The Health Care Revenue Cycle 70
days 21 through 100 is $133.50 per day for 2009. Beyond these 100 days per year, the
patient is responsible for all costs incurred in the SNF.
Advanced Benefciary Notice (ABN)
For those consumers that have Medicare Part B, an Advanced Benefciary Notice
of Non-Coverage (ABN) can be used. An ABN must be completed by the patient
BEFORE any Medicare Part B services are rendered by the doctor that may be
determined not medically reasonable and necessary (Medicare denies payment). Medicare
medical necessity criteria should be carefully examined by the provider and patient
to establish whether it is reasonable to assume the treatment for the diagnosis will
not be paid by Medicare.
The purpose of the ABN is to notify the patient, in a timely manner, that in case of
Medicare denial they will be responsible for all costs if they still get the medical
care; the patient has the right to refuse treatment; and the patient is informed of the
consequences of their health care decisions. The patient must read and sign and date
the ABN so that it is legally in effect.
When it is an emergency situation, EMTALA stipulates that an ABN not be given to
the patient until the patient is medically screened and clinically stabilized.
See www.cms.hhs.gov/BNI/Downloads/CMSR131G.pdf for more information
concerning the ABN.
Medicare Secondary Payer (MSP) and the Working Aged
Provision
The employer, or two or more employers, must have at least 20 employees combined
and provide an employer group health plan (EGHP), to be eligible for the Working
Aged Provision to make the MSP effective. This means that when there are 20
or more employees, the employers must offer the same health insurance plans
(EGHP) to its employees that are over 65 years of age as those who are younger
than 65. If those employees that are over 65 elect to join the EGHP, then the Working
Aged provision applies and the EGHP becomes the primary payer and Medicare becomes
the secondary payer for health care services. In other words, MSP operates by using
coordination of benefts (COB) with the patients other insurances to determine who
is the primary or secondary payer.
More information can be accessed at: www.cms.hhs.gov/medicare/cob/msp/msp_home.asp.
Medicare is the secondary payer for those who are the following:
1. Aged 65 or older, employed, and has coverage under an employer-sponsored
group health plan (EGHP) or an employee group health plan (plan offered
through a union).
2. Aged 65 or older and covered by working spouses EGHP or an employee
group health plan.
Chapter 2 - Contact with Hospitals and the Doctors 71
3. Those under 65, disabled, and covered by a large group health plan (LGHP)
provided by their employer, or the EGHP offered by another family
members employment (spouse).
4. Those afficted with End Stage Renal Disease (ESRD) and have their own
or spouses EGHP or union plan, or other family members EGHP or union
plan. A thirty (30) month Coordination of Benefts (COB) period is in effect
whereby the EGHP starts as the primary coverage, and pays for the frst
30 MONTHS of medical treatment for ESRD, before Medicare pays ESRD
expenses as the primary payer after these 30 months have passed.
5. Those covered by Workers Compensation, Federal Black Lung, automobile,
no-fault, or liability insurance plans.
6. Those who health care needs are covered under Veterans Administration
(VA).
The Medical Staf and Hospital Admitting
Protocols
The most important privilege a member of the hospitals medical staff is granted is the right to
admit patients to the hospital for health care services. The admission of the patient to the
hospital is a critical decision impacting on the consumers health, requiring decisions
by the admitting physician and hospital administrator. The admitting staff or registrar
cannot admit patients.
1. It is not permissible for the registrar to refuse to admit a patient the doctor
has ordered to admit, even if the consumer is unable to pay for treatment. Any
delays the registrar causes the patient in getting treatment may result in
adverse legal action such as a malpractice suit.
2. EMTALA does not allow interference with the admitting process for any
reason whatsoever if it is an emergency situation. The hospital is obligated to
admit the patient to the ER when it is medically urgent.
3. If it is strictly an elective procedure, which means not an urgent or
emergency clinical condition directly affecting the patients health, only
the admitting physician can cancel or delay the admission until the hospitals
fnancial criteria are satisfed by the patient.
4. Admitting the patient to the hospital presents the registrar with
clinical, legal, and time-sensitive issues that could expose the hospital,
administrator, and physician to adverse legal action. In addition, the refusal
or delayed admission of the consumer denies the hospital of potential
revenue and generates negative publicity.
5. Only a member of the hospitals medical staff can admit a patient.
6. If a patient is refused admission for any reason, it is imperative the
admitting physician and hospital administrator are contacted immediately.
The admitting physician must have the right to appeal the refusal of their
patients admission to the hospital in a timely manner.
The Health Care Revenue Cycle 72
Patient Confdentiality: Privacy Act of 1974
1. Patient privacy is a serious legal matter and cannot be violated whatsoever by
any member of the hospitals Registration, Admission, Financial, Administration,
Medical staff, employee, volunteer or anyone connected with the hospital.
2. The legislation that governs protection of the patients confdentiality related
to all hospital service areas is called the Privacy Act of 1974. Related to health
care, anyone who has contact with the patient, all records, all treatment
provided, etc., must be kept confdential. Practically speaking, the patients
medical records need to be out of public view and doctors and nurses and
therapists should not be discussing private health information (PHI) in
public. This act established protection for the patient against invasion of
privacy by the abuse of their records by the executive branch of the federal
government (The White House), and those governmental agencies subject to
the Freedom of Information Act (FOIA). This act does not apply to records
maintained by state and local governments, or private organizations and
companies.
3. The Privacy Act of 1974 is legally applicable to United States citizens and
aliens legally admitted for permanent residence.
The Patients Medical Record and Telephone/Verbal Communica-
tion in the Hospital
1. The Patients medical record is a legal document (important) and cannot be
released without the patients written consent. It may, however, be released
by legal subpoena for any civil or criminal proceedings (unless prohibited
by law). It must be stored in areas free from theft, destruction, unauthorized
access, water damage, and insect infestation.
2. All medical documentation must be valid, complete, suffciently detailed and
accurate, and legible.
3. Incorrect entries into the medical record will be corrected with a single
line drawn through the incorrect information, initialed and dated by the
member of the medical staff performing the correction, with the correct data
written adjacent to the incorrect data. (Note: This is very important for anyone
working in the health care feld)
Medical personnel legally authorized to make corrections include:
Attending physician, physician assistant (PA), licensed registered nurse
(RN), or nurse practitioner (NA).
Student, under supervision from a properly licensed supervisor or
teacher, from an accredited health professions program.
4. Verbal and telephone orders from the referring physician can only
be accepted by a licensed physician, nurse, physician assistant, nurse
practitioner or other duly licensed Health Care practitioner. The referring
physician is the doctor who sends the patient to the hospital for further
specialized treatment. The admitting physician is the one who places the
patient in the hospital and assumes all responsibility for care, administers
Chapter 2 - Contact with Hospitals and the Doctors 73
and documents the treatment, and discharges the patient back to the
referring physician. Sometimes the referring physician and admitting
physician are the same.
5. All telephone and verbal orders will contain the following information:
Date and time the order was received by the physician, PA, RN, NA, etc.
(with full name and designation).
Name of the ordering physician and patient involved (patient status and
all identifying data included).
The exact medical order transcribed word for word (verbatim).
6. It is mandatory that permanent copies of the patients Advanced Medical
Directive (AMD), Living Will, Health Care Surrogate, and Health Care Power
of Attorney are included and continually updated in the medical record.
7. There is a direct connection between completion of the insurance claim form
and the patients medical record. All information pertinent to successfully
flling out the insurance claim form (producing a clean claim) so the doctor
and hospital get paid, will be found in the medical record.
Patient Self-Determination Act (PSDA)
1. PSDA is also known as the Advanced Medical Directive (AMD), which is a
legal instrument that includes the following:
A Living Will, which is legal documentation prepared while the patient
is still alive and coherent, addressing what health care is desired or
not desired (e.g. Do Not Resuscitate or DNR) if the patient becomes
incoherent due to a terminal disease or other debilitating condition.
The Living Will or AMD will be activated when the patient becomes
incapacitated, and the Health Care Surrogate can then legally make
treatment decisions. Out-of-state approval of a Living Will may be problematic
as laws governing PSDAs vary from state to state.
Selection of a Health Care Surrogate or Health Care (Durable) Power
of Attorney. This is a legal document that designates someone else, also
known as a proxy or agent, the right to make medical care decisions if the
patient becomes incapacitated. Having an AMD on fle does not mean
that it will ever have to be implemented.
2. The PSDA or AMD is defned as a legal document such as a Living Will or
Durable Power of Attorney and is recognized by state law. The PSDA: (1)
gives the patient the right to make directives about their future medical care
when they are incapable of making these decisions on their own; (2) allows
the patient to accept or refuse any health care; and (3) gives the patient the
right to execute a living will or grant a durable power of attorney for health
care to a designated individual. The Durable Power of Attorney means
that someone is legally appointed by the patient to act with the powers of a
lawyer specifcally related to executing the patients wishes for their future
health care when they become unable to do this on their own.
The Health Care Revenue Cycle 74
3. Omnibus Budget Reconciliation Act of 1990 (OBRA) states that in order
for hospitals to participate in Medicare (Title XVIII) and Medicaid (Title
XIX) programs, they must develop ways to implement Advanced Medical
Directives so their patients can be enabled to make their own health care
decisions. Most hospitals are promoting the importance of the AMD before
the consumer becomes sick and needs the hospital for treatment. This act
established the PSDA.
4. Important: An AMD is activated when the patient becomes incapacitated. The
patient can revoke the AMD anytime by destroying ALL copies.
Figure 6: OBRA 1990
The Joint Commission on Accreditation of Health Care Organiza-
tions (JCAHO)
In the United States, JCAHO is the leading organization establishing health care
standards and an accrediting body in the health care industry. JCAHOs main focus
is to promote state-of-the-art protocols that emphasize improving the quality, safety,
and optimal delivery of treatment administered by health care organizations such as
hospitals. JCAHO is the pre-eminent surveyor of hospitals, and audits and accredits
them every three (3) years. JCAHO inspects, certifes, and establishes the standards
of just about every aspect of the functioning of a hospital, which includes the
registration and admissions departments. Remember, JCAHO used Medicare as the
gold standard.
Chapter 2 - Contact with Hospitals and the Doctors 75
JCAHO emphasizes the following areas in the registration and admission areas of the
hospital:
1. Patient Confdentiality and Privacy (HIPAA)
2. Advanced Medical Directives
3. Patient Rights and Responsibilities
4. Hospitals Organizational Ethics and Protocols (ways of doing things)
5. Continuum of Health Care (how treatment is provided in a timely manner
and a smooth medically necessary fashion)
6. Management of the Health Care Environment and the Delivery of Health
Care
7. Patient Security (medical record privacy and patients physical security in
the hospital)
8. Communication between Doctors, Allied Medical Staff, Hospital Staff,
Patient, and Public
Contingency Plans for Disasters in the Registration and Admissions Departments
1. JCAHO requires registration and admissions departments in every hospital
to have in place plans in case of disruptions of hospital services, or disasters.
Disasters include: fres, foods, storms such as hurricanes, and earthquakes.
Also included are civil disorders such as riots, power failures, massive
injuries (terrorism or outbreaks of disease affecting many people [epidemics])
that would tax the hospitals resources, bomb threats, or explosions.
2. JCAHOs requirements demand that each hospital have institution-wide
plans in place, and operational, in case of emergencies for the registration
and admissions departments, particularly affecting inpatient admissions and
discharge operations.
3. Planning for disaster and emergency contingencies encompasses three
areas for the admitting/registration departments:
Emergency Response involves the handling of the disaster so that as it
is happening the extent of damage is limited, sensitive data is protected,
and operational impact is minimized.
Back-up plans involve the time period immediately after the disaster.
Categorizing time-sensitive operations, identifying operating resources
and facilities critical to the maintenance of admission/registration
hospital functions in temporary facilities (if necessary), and preparing
permanent facilities to be made functional again.
Recovery plans are coordinated with back-up directions to insure the
transition from emergency response, to a resumption of permanent
functioning of the admission and registration departments is smooth,
and conficts are resolved.
The Health Care Revenue Cycle 76
A comprehensive emergency contingency plan involves: personnel, security,
data, software, hardware, supplies, communications, IT, storage, operational
space, and documentation.
Census
Census refers to the number of inpatients in the hospital at any particular point in
time.
1. The most common census is the Midnight Census.
2. Every health care institution has fxed and variable expenses that are
affected by the population of patients admitted to the hospital, as well
as those utilizing inpatient and outpatient services such as radiology,
laboratory, ASC, PT, OT, ST, etc.
3. A low census for a period of time (weeks, for example) will have a negative
effect on the hospitals cash fow, accounts receivable (A/R) and accounts
payable (A/P), due to hospital beds that are not flled and hospital services
not being utilized. A low census means the hospital and doctors are not
selling their services to enough customers to make enough money to pay
their expenses and make a proft.
4. Lost revenues during periods of low census may result in cash generation
that is insuffcient to cover the hospitals fxed expenses (many of which are
24 hours per day, 7 days per week) such as salaries, utilities (heat, electricity),
building maintenance, operation of the emergency room and surgical suites
and laboratories, etc., which remain the same over the short term (weeks)
regardless of the number of patients in the hospital.
5. Over the long term (months) with a low census, variable expenses will be
lowered because less medical supplies are used and fewer employees are
working (they are laid off). However, the hospital may still experience cash
fow problems negatively impacting the hospitals capital reserves, because
there are fxed expenses that need to be paid and other obligations that need
to be handled. Hospitals simply cannot shut down their services because of
future uncertainties of the medical needs of the public; ongoing training of
medical and allied health students, residents, and nurses; ongoing research
operations; and contractual obligations with permanent medical staff and
use of specialized medical equipment (CAT scan, MRI, electron microscope,
surgical equipment and laboratories, etc.)
6. Therefore, a high census for a suffciently long period of time will
compensate for a low census by the hospital making more and more money
during times of a high census.
Chapter 2 - Contact with Hospitals and the Doctors 77
Average Daily Census
This is the average number of inpatients physically in the hospital each day for a
specifc period of time.
Formula:
Sum of Total Patient Days (patients in the hospial)
Number of Days Within a Time Period (i.e, one month)
= Average Daily
Census
For example, for the month of January, 2009, the daily census is:
January 1: 167 patient days = daily census
January 2: 177 patient days = daily census
January 3 180 patient days = daily census
January 4 190 patient days = daily census
January 5 159 patient days = daily census
through to January 31: 209 patient days = daily census
7120 = Sum of Total Patient Days (Total Number of Patients in the Hospital)
for the Entire Month of January, 2009
Total Number of Days in January, 2009 = 31 Days
Sum of Total Patient Days
Days in January
7120
31
= = 229 = Average Daily Census
On Average, for the month of January, 2009, there were 229 patients in the
hospital each day.
Percentage of Occupancy
Formula is the ratio of actual number of patient days (hospital beds flled with
people) divided by the maximum number of patient days (hospital beds that can be
flled) the hospital can handle during a specifc period of time. If the hospital can hold a
maximum of 200 patients per day (it has 200 beds available), and for January 1, 2009
the hospital had a daily census of 167 patients (167 beds were actually flled with
patients), the percentage of occupancy would be as follows:
Actual Patient Days
Maximum Patient Days
167
200
= = 84%
84% indicates that for January 1, 2009, the Hospital is 84% Full =
PERCENTAGE OF OCCUPANCY
The Health Care Revenue Cycle 78
Generally Accepted Accounting Principles
(GAAP)
Defnition: The accounting principles used in the handling of cash, credit card
receipts, checks, and other fnancial instruments the registrar in the registration
or admissions offce must follow to insure fnancial safety and accuracy, and to
minimize shortages (losses). This is another one of the many duties of the registrar
that of a cashier.
The cashier must:
1. Maintain a payment log (who paid what to whom).
2. Maintain a locked cash drawer that is secured and out of public view.
3. Maintain duplicate numbered receipt logs of all fnancial transactions, so
that the hospital, doctor and patient all have a written record of all fnancial
activity. For example, the patient can prove they actually did pay their co-
payments, co-insurances, deposits, etc.
4. Issue receipts for all cash payments and all fnancial transactions in a timely
fashion.
5. Store fnancial deposits, that have not been deposited in the hospitals bank
accounts, in a theft-proof and fre-proof safe
6. Checks should be immediately endorsed with For Deposit Only to the
hospital or doctors offce.
Chapter 2 - Contact with Hospitals and the Doctors 79
Understanding Acronyms and Abbreviations
It is recommended the student prepare fashcards to facilitate memorizing these
concepts.
ABN Advanced Benefciary Notice
ADL Activities of Daily Living
ALOS Average Length of Stay
AMD Advanced Medical Directive
A/P Account Payable (bills waiting to be paid to vendors that have
provided services and products to the hospital)
A/R Accounts Receivable (revenues waiting to be received by the hospital
from patients or insurance companies that have been billed for
health care services provided by the hospital)
CC Chief Complaint
CAT scan Computerized Axial Tomography scan
CCU Critical Care Unit
CHAMPVA Civilian Health and Medical Program of the Veterans Administration
CHCBP Continued Health Care Beneft Program
CMS-1500 Centers for Medicare and Medicaid services billing and coding form
(outpatient)
COB Coordination of Benefts
DEERS Defense Enrollment Eligibility Reporting System
DOB Date of Birth
DOD Department of Defense
DOS Date of Service
DNR Do Not Resuscitate
DRG Diagnosis Related Group
Dx Diagnosis
EGHP Employer Group Health Plan
EOB Explanation of Benefts
EKG Electrocardiogram
ESRD End Stage Renal Disease (kidney failure)
FOIA Freedom of Information Act
GAAP Generally Accepted Accounting Principles
HMO Health Maintenance Organization
The Health Care Revenue Cycle 80
IHS Indian Health Service
ICU Intensive Care Unit
JCAHO Joint Commission on Accreditation of Health Care Organizations
LTC Long Term Care
LTR Lifetime Reserve Days
MSP Medicare Secondary Payer
MCO Managed Care Organization
MRI Magnetic Resonance Imaging
MTF Military Treatment Facility
NP Nurse Practitioner
NAS Non-Availability Statement
OBRA (1990) Omnibus Budget Reconciliation Act of 1990
PA Physician Assistant
PAT Pre-Admission Testing
PCU Progressive Care Unit
PPO Preferred Provider Organization
PSDA Patient Self Determination Act
RA Remittance Advice
RN Registered Nurse
RTC Residential Treatment Center
SNF Skilled Nursing Facility
SSN Social Security Number
TAN Treatment Authorization Number
TPA Third Party Administrator
UB-04 Billing and coding form for hospital use (inpatient)
VA Veterans Administration
Chapter 2 - Contact with Hospitals and the Doctors 81
More Test Taking Strategies
In this chapter, much of the information is presented in an outline or laundry list
format, where multiple lines of data are related to a main concept. When answering
multiple choice questions for this kind of information, be sure to remain focused
on the main concept as you consider each answer. Those that pertain to the main
concept are correct, those that do not are incorrect. To use a simple example, in
question #3 belowThe responsibilities of the hospital registrations staffthe main
concept is registrar. As you read each possible answer ask whether it relates to a
registrars responsibilities. Because, in this case, they all do, the correct answer is E
all of the above. (Look also at questions #6, 9, 12 and 13.)
Sometimes you are asked to choose the one response that is not applicable. Again,
a simple example is question #2 All of the following are included in the Physicians
Direct Services except. The main concept is, of course, Physicians Direct Services.
There is only one answer that does not relate to the main conceptanswer C,
changing the patients prescription for pharmaceuticals. Often the choice that is not
applicable (the correct answer) either is so absurd as to not make any sense (the
registrar would never alter the patients prescription) or is not consistent with the
listed responsibilities that you have learned. (Questions #7, 8 and 10 are similar kinds
of questions.)
The Health Care Revenue Cycle 82
Sample Test Questions
These 80 questions should be answered in 80 minutes or less (one minute per
question).
1. Advantages of pre-admitting a patient to the hospital include all of the
following except:
A. Hospital room, facility needs, and PAT can be anticipated in a timely fashion.
B. Insurance pre-certifcation, pre-verifcation, and collection of copayments,
deductibles, and deposits can be handled prior to the medical service being
rendered.
C. 70% to 90% of all patients should be pre-registered at least 48 hours prior to
admission.
D. Second opinions for surgery and other procedures can be obtained prior to
provision of health care services.
Answer: C
2. All of the following are included in Physician Direct Services except:
A. Hospital staff physician outbound call services
B. PCP notifcation of their patients who experience an emergency department
admission
C. Changing the patients prescription for pharmaceuticals
D. Community and staff physician referrals and marketing to the public
E. Effective Patient Scheduling
Answer: C
3. The responsibilities of the hospital registration staff, the registrar, include
handling:
A. ABN, EMTALA, Patient Bill of Rights.
B. Adequate collection of all necessary data so that a clean claim can be
produced.
C. Creating the permanent patient medical fle.
D. Adherence to HIPAA rules and regulations.
E. All of the above.
Answer: E
4. The estimated portion of the hospital bill, not covered by insurance and paid
by the patient at pre-admission, is known as the:
A. EOB
B. RA
C. Deposit
D. Clean claim
E. PCP
Answer: C
Chapter 2 - Contact with Hospitals and the Doctors 83
5. Excellence in patient scheduling involves a balance between patient
satisfaction and collecting the necessary ___________ information.
A. Demographic
B. Financial/Legal
C. Clinical
D. Insurance
E. All of the above
Answer: E
6. The most important responsibility of the hospital registration staff is:
A. Production of a clean claim
B. Creating the permanent patient medical fle
C. Creating the permanent patient identifcation process
D. Accurate collection of patient information
Answer: A
7. A clean claim submitted to the insurance carrier involves all the following,
except:
A. It is Valid and Complete
B. TPO information collected is PHI and covered under HIPAAs Privacy Rule
C. Will result in no delays in reimbursement to the doctor or hospital
D. It is fraudulent and abusive
E. Can be audited by a third party with no further intervention by the health
care provider or facility
Answer: D
8. As the health care industry becomes more complicated, the role of the hospital
registrar has evolved to include all of the following except:
A. Implementation of federal and state rules, regulations; completion of
paperwork.
B. Handling the hospitals legal matters.
C. Compliance of HIPAA, ABN, MSP.
D. Adherence to ALOS criteria.
E. All of the above.
Answer: B
9. Disadvantages of pre-admitting a patient to the hospital includes:
A. Paperwork is incomplete, invalid, delayed or forgotten by the patient.
B. Pre-certifcation and pre-verifcation processes are not always completed in a
timely fashion.
C. Dates of actual hospital admission, procedures and surgical services are not
always known in advance.
D. All of the above.
Answer: D
The Health Care Revenue Cycle 84
10. The fve collection control points the registrar has with the patient to complete
the registration process include all of the following except:
A. In-house
B. After discharge
C. HIPAA
D. Pre-Admission
E. Admission
F. At discharge
Answer: C
11. The process of conducting all laboratory work, diagnostic imaging, EKGs,
biopsies, etc., prior to the patient being admitted to the hospital, is called
___________.
A. PAT
B. ALOS
C. ABN
D. EOB
E. PCP
F. CHCBP
Answer: A
12. A consistent and well-executed hospital registration system will ___________
before health care services are provided to the patient.
A. Identify all patients copayments, deductibles, deposits, and fnancial
obligations
B. Be completed at least 24 hours
C. Identify all insurance limitations, pre-certifcations, pre-verifcations, and
other requirements
D. Collect all demographic, socioeconomic, and clerical information
E. All of the above
Answer: E
13. Advantages of pre-admitting a patient to the hospital include all of the
following:
A. Insurance pre-certifcation and pre-verifcation criteria, collection of
copayments, deductibles, and deposits are handled prior to medical service
being rendered.
B. 70% to 90% of all patients should be pre-registered at least 24 hours prior to
admission.
C. Second opinions for surgery and other procedures can be obtained prior to
provision of health care services.
D. Hospital room, facility needs, and PAT can be anticipated in a timely fashion.
E. Takes advantage of the patients sense of urgency.
F. All of the above
Answer: F
Chapter 2 - Contact with Hospitals and the Doctors 85
14. The three types of TRICARE are:
A. Special
B. Prime
C. Standard
D. Extra
E. B, C, D
F. A, B, C
Answer: E
15. Active military duty personnel are enrolled in ______________ and pay no fees.
A. TRICARE Prime
B. TRICARE Standard
C. TRICARE Extra
D. CHAMPVA
E. None of the above
Answer: A
16. Federal law requires hospitals participating in Medicare to also participate in
__________________ for inpatient services.
A. TRICARE Prime
B. TRICARE Standard
C. TRICARE Extra
D. CHAMPVA
E. B and E
F. A and C
Answer: B
17. _______________ describes a computerized database administered by the DOD
and used by TRICARE to confrm who is eligible for treatment and what plan
they have.
A HIPAA
B. Department of Defense
C. OIG
D. DEERS
E. PCP
F. CHCBP
Answer: D
18. ______________ is defned as a health care program for veterans, their spouses
and children, with permanent or total service-connected disabilities, and
surviving spouses and children of veterans who died as a result of a service
connected disability.
A. CHAMPUS
B. TRICARE
C. CHAMPVA
D. MEDICARE
E. DEERS
Answer: C
The Health Care Revenue Cycle 86
19. _____________ utilizes a DRG payment system for most admissions to acute-
care, short-term hospitals in 49 states, the District of Columbia, and Puerto
Rico for those in the military or their families. _________________ is exempt
from DRGs.
A. TRICARE Prime; Maryland
B. TRICARE Extra; Virginia
C. TRICARE Standard; Maryland
D. CHAMPVA; Virginia
E. None of the above
Answer: C
20. Which of the following require a NAS to be issued to the benefciary before
any non-emergency civilian hospital inpatient services may be provided?
A. TRICARE Prime
B. TRICARE Standard
C. TRICARE Extra
D. CHAMPVA
E. CHCBP
F. A and B
G. B and C
H. D and E
Answer: G
21. Which of the following criteria are not related to the NAS?
A. Required for TRICARE Standard and Extra
B. Valid for 30 days after the date of issuance of the NAS
C. Remains valid from the benefciarys date of admission to the hospital until
15 days after discharge
D. It is not issued at the discretion of the MTF Commander.
E. All of the above
Answer: D
22. TRICARE for Life is a(n):
A. Expanded program for Medicare-eligible military who are 65+ years,
families, survivors, some spouses.
B. Must be enrolled in Medicare Parts A, B and C.
C. There are no fees except for Part B premiums.
D. Secondary payer to Medicare.
E. A, C and D
F. B, C and D
Answer: E
23. TRICARE claims must be submitted within _______________.
A. One (1) year of the DOS, regardless whether the claim is invalid or
incomplete.
B. Two (2) years of the DOS.
C. One (1) year of the DOS, and claim must be valid and complete.
D. Three (3) years of the DOS, and claim must be valid and complete.
Answer: C
Chapter 2 - Contact with Hospitals and the Doctors 87
24. TRICARE is the primary payer for all of the following when the benefciary
also has:
A. Medicaid.
B. IHS coverage for non-IHS medical services.
C. Other insurance coverage for out-of-pocket expenses.
D. All of the above.
Answer: D
25. Medicares Spell of Illness is defned as:
A. Having no deductible to be paid.
B. Beneft Period.
C. Begins when the patient is admitted to the hospital or SNF.
D. Ceases 60 days after the benefciary has been discharged from the hospital or
SNF.
E. Is considered the same Spell of Illness as long as each admission and
readmission to the hospital or SNF are consectuve and not longer than 60
days each.
F. B, C, D, E
G. A, B, C
Answer: F
26. TRICARE is considered the secondary payer when the benefciary also has
______________ coverage:
A. Workers Compensation
B. PIP coverage
C. No Fault
D. Uninsured motorists (under auto policy)
E. Student health
F. HMO, PPO
G. All of the above
Answer: G
27. Before the registrar can accurately estimate the patients fnancial obligation to
the hospital, the following are applicable:
A. Preferably will occur at discharge.
B. ALOS and the admitting physicians estimated length of hospital stay have
to
be determined.
C. Average cost per diem by type of medical/surgical service, inpatient and/or
outpatient, have to be estimated.
D. EMTALA does not have to be considered.
E. Daily ICU, CCU, private or semi-private room charges determined.
F. B, C, E
G. A, B, C.
Answer: F
The Health Care Revenue Cycle 88
28. When the consumer enters the hospital for emergency care or an urgent care
clinic before being medically screened, the registrar can:
A. Call the insurance company for authorization and certifcation numbers.
B. Ask the patient for deposit or co-payments.
C. Ignore EMTALA requirements.
D. None of the above.
E. All of the above.
Answer: D
29. Medicare Part A pays for all or part of ____________ of hospitalization.
A. 60 days.
B. 150 days.
C. 30 days.
D. 100 days.
E. None of the above.
Answer: B
30. The inpatient hospital beneft days that Medicare will pay for are defned as:
A. First 60 days: Full or Covered Days.
B. First 30 days: LTR Days
C. Third 60 days: Lifetime Reserve Days
D. Second 30 days: Coinsurance Days
E. Third 60 days: SNF beneft
F. A, C and D
G. B, D and E
Answer: F
31. The frst 90 inpatient hospital beneft days that Medicare Part A will pay for
are known as _______________ ; the last 60 inpatient hospital beneft days are
known as _____________.
A. Renewable days; Non-Renewable days.
B. Renewable days; LTR.
C. Non-renewable days; Renewable days.
D. Spell of Illness; Beneft Period.
E. A and B
Answer: E
32. The following are applicable for Medicare to reimburse SNF care except:
A. The patient is receiving custodial care.
B. The patient was frst admitted to the hospital for at least three consecutive
days, not including the day of discharge, prior to entering the SNF.
C. The patient was receiving skilled or special services.
D. There is a 100 day SNF beneft.
Answer: A
Chapter 2 - Contact with Hospitals and the Doctors 89
33. TRICARE will never pay for health care services when the patient also has
______________.
A. Medicaid
B. Workers compensation
C. CHAMPVA
D. Student health insurance
E. PIP and no-fault coverage under patients own automobile policy
Answer: C
34. The ABN encompasses the following:
A. In an emergency situation, should not be given to a benefciary until
medically screened and stabilized.
B. Applicable for patients with Medicare Part B benefts.
C. Benefciary should not be given an ABN unless there is a genuine likelihood
the medical services will be denied.
D. All of the above.
E. B and C
Answer: D
35. Pre-certifcation:
A. Insures that the claim will be paid under the provisions of the health
insurance policy.
B. Is the hospitals obligation to get from the patients insurance carrier.
C. Does not affect payment delays, fnancial risk, and bad debt for the
hospital.
D. Does not affect the pre-admission process or patients experience with the
hospital.
E. None of the above.
Answer: E
36. In consideration of the physician admitting the patient to the hospital:
A. In case of an emergency, cannot be denied because of the patients inability to
pay for services.
B. Only a member of the hospitals medical staff can admit patients for health
care services.
C. It is acceptable for a member of the hospitals registration staff to deny or
delay admission.
D. It is an important privilege the hospital grants only to the medical staff.
E. B, C and D
F. A, B and D
Answer: F
The Health Care Revenue Cycle 90
37. The Privacy Act of 1974:
A. Is applicable only to United States citizens and aliens lawfully admitted for
permanent residence.
B. Provides protection against invasion of privacy due to abuse of personal
records by the executive branch of the federal govt.
C. Applies to governmental agencies subject to the FOIA.
D. Applies to records maintained by state and local governments.
E. All of the above.
F. A, B and C.
G. B, C and D.
Answer: F
38. The patients medical record includes all of the following:
A. Optional to be complete, valid, legible, accurate and suffciently detailed.
B. Is not a legal document.
C. Not necessary to be stored to be free from water and insect damage.
D. Not necessary to be protected from theft, abuse, destruction, or unauthorized
use.
E. Incorrect entries can be erased.
F. Anyone in the hospital can make corrections into the medical record.
G. None of the above.
Answer: G
39. All verbal and telephone orders concerning the patients hospital care include:
A. Full name and designation of authorized staff member documenting the
order
B. Date and time the order was received.
C. The name of the ordering physician.
D. Not necessary to write down the order verbatim.
E. Can be accepted by anyone employed by the hospital.
F. A, B, D, and E.
G. A, B, C.
Answer: G
40. The AMDs are written legal instruments that include:
A. The Living Will
B. HMO
C. Assignment of a health care surrogate.
D. Assignment of a health care power of attorney.
E. NAS
F. A, C and D
G. C, D and E
Answer: F
Chapter 2 - Contact with Hospitals and the Doctors 91
41. _____________ is a written legal document providing direction about what
health care the consumer wants or does not want when there is a terminal
illness or other debilitating condition.
A. MCO
B. Living Will
C. OBRA of 1990
D. FOIA
E. Privacy Act of 1974
Answer: B
42. The key elements of HMOs, MCOs, or PPOs the registrar must confrm prior
to medical care being rendered are:
A. Pre-certifcation and pre-authorization data.
B. Refuse to admit the patient to the hospital until HMO data is verifed, even if
it is an emergency.
C. Insure the hospital accepts the patients managed care health insurance.
D. Insure the medical staff doctors accept the patients managed care health
insurance.
E. A, C and D
F. B and D
Answer: E
43. The AMD is also known as the:
A. PSDA
B. CHAMPVA
C. HIPAA
D. DEERS
E. PROXY
Answer: A
44. The AMD is activated when the patient becomes ________________ and can be
revoked by the patient ______________.
A. Coherent, Calling the attorney.
B. Incapacitated, destroying some copies of the AMD.
C. Incapacitated, destroying all copies of the AMD.
D. MSP; accepting OBRA of 1990.
E. None of the above.
Answer: C
45. Medicare is the secondary payer for all of the following except:
A. 65 or older, employed with an EGHP.
B. Spouse, who is 65 years or older, of someone who is employed with an
EGHP.
C. Those who receive coverage under Workers Compensation, Federal Black
Lung, automobile insurance.
D. Those with ESRD and for the COB period of 15 months.
E. Those who receive services covered under the VA.
Answer: D
The Health Care Revenue Cycle 92
46. ___________________ is consent that can be written or oral and the patient
agrees to the treatment described to him or her.
A. Informed consent
B. Implied consent in fact
C. Special consent
D. Implied consent by law
E. General consent
F. Actual or expressed consent
Answer: F
47. __________________ occurs when the patient is unconscious and admitted to
the ER for treatment allowed by law.
A. Informed consent
B. Implied consent in fact
C. Special consent
D. Implied consent by law
E. General consent
F. Actual consent
Answer: D
48. _________________ is consent by silence as the patient implies permission for
the treatment by not objecting.
A. Informed consent
B. Implied consent in fact
C. Special consent
D. Implied consent by law
E. General consent
F. Actual consent
Answer: B
49. ____________ type of consent is used to get permission for the patient to receive
HIV testing, major/minor surgery, anesthesia, chemotherapy or radiation
therapy, or psychiatric therapy.
A. Informed consent
B. Implied consent in fact
C. Special consent
D. Implied consent by law
E. General consent
F. Actual consent
Answer: C
Chapter 2 - Contact with Hospitals and the Doctors 93
50. _____________ describes a type of consent where the patient understands what
treatment is being provided and what procedures are to be performed.
A. Informed consent
B. Implied consent in fact
C. Special consent
D. Implied consent by law
E. General consent
F. Actual consent
Answer: A
51. The following are related to the PSDA except:
A. AMD
B. Health Care Surrogate
C. Living Will
D. Privacy Act of 1974
E. OBRA of 1990
Answer: D
52. _________________ describes a consumer who suddenly enters the hospital for
immediate screening, diagnosis and treatment but not admitted to the hospital
for inpatient or observation services.
A. Clinic
B. Inpatient
C. Emergency
D. Ambulatory
E. Same Day Surgery
Answer: C
53. _____________ describes a consumer who has been admitted to the hospital
upon the orders of a physician who is expected to stay overnight.
A. Clinic
B. Inpatient
C. Emergency
D. Ambulatory
E. Same Day Surgery
Answer: B
54. ________________ describes an outpatient who receives surgical services with
no admission to the hospital.
A. Clinic
B. Inpatient
C. Emergency
D. Ambulatory
E. Same Day Surgery
F. D and E
Answer: F
The Health Care Revenue Cycle 94
55. _____________ is the charge consisting of the professional fee and technical
fee.
A. Global
B. Actual
C. UCR
D. Prevailing
E. Approved
Answer: A
56. ____________ charge is the monies paid to the provider or hospital per the
Medicare fee schedule.
A. Global
B. Actual
C. UCR
D. Prevailing
E. Approved
Answer: E
57. ____________ charge is the average fee billed by most of the providers or
hospitals for a particular service in a geographic area.
A. Global
B. Actual
C. UCR
D. Prevailing
E. Approved
Answer: C
58. _______________ defnes broader and less specialized diagnostic, medical, and
surgical care provided to the consumer on an outpatient basis.
A. Clinic
B. Inpatient
C. Emergency
D. Ambulatory
E. Same Day Surgery
Answer: D
59. Observation care involves:
A. Usually does not exceed 24 hours.
B. Those services provided in a hospital.
C. Those services provided in an ASC.
D. Claims submitted for more than 48 hours of observation care will be
reviewed for medical necessity by CMS.
E. A, B, and C
F. A, B, and D
G. A, B, C and D
Answer: F
Chapter 2 - Contact with Hospitals and the Doctors 95
60. _______________ is generally made available to patients who are terminal,
chronically ill or disabled in a nursing facility or rest home.
A. Outpatient care
B. Respite care
C. Long Term care
D. Hospice care
E. Custodial care
F. Home Health care
G. Gatekeeper
Answer: C
61. _______________ is not covered by Medicare and can be administered by those
who are not professionally trained.
A. Outpatient care
B. Respite care
C. Long Term care
D. Hospice care
E. Custodial care
F. Home Health care
G. Gatekeeper
Answer: E
62. ______________ is the role of the PCP in managed care plans that controls
access to specialized medical treatment and facilities.
A. Outpatient care
B. Respite care
C. Long Term care
D. Hospice care
E. Custodial care
F. Home Health care
G. Gatekeeper
Answer: G
63. _____________ care that is provided to terminally ill individuals and their
families by non-profts.
A. Outpatient care
B. Respite care
C. Long Term care
D. Hospice care
E. Custodial care
F. Home Health care
G. Gatekeeper
Answer: D
The Health Care Revenue Cycle 96
64. Checks immediately endorsed with For Deposit Only, cashier maintains a
locked cash drawer and payment log, cashier stores un-deposited cash and
checks and other fnancial instruments in a theft-proof and fre-proof safe, are
required of:
A. HIPAA
B. GAAP
C. Privacy Act of 1974
D. JCAHO
E. Durable Power of Attorney
Answer: B
65.
Sum of Total Patient Days in a Month
Total Number of Days in a Month
= .
A. GAAP
B. Percentage of Occupancy
C. HIPAA
D. Average Daily Census
E. Informed Consent
F. Revenue
Answer: D
66
.
Actual Patient Days (Census)
Maximum Patient Days (Total Beds)
= .
A. GAAP
B. Percentage of Occupancy
C. HIPAA
D. Average Daily Census
E. Informed Consent
F. Revenue
Answer: B
67. Planning for emergency and disaster events includes the following except:
A. GAAP
B. Response
C. Back-up
D. Recovery
E. Privacy Act of 1974
F. A and E
G. B and C
Answer: F
68. ___________ requires hospital-wide disaster and emergency plans.
A. GAAP
B. ABN
C. JCAHO
D. ALOS
E. PSDA
Answer: C
Chapter 2 - Contact with Hospitals and the Doctors 97
69. The most important privilege a member of the hospitals medical staff is to:
A. Admit patients for health care services.
B. Follow GAAP.
C. Enforce HIPAA.
D. Follow PSDA directives.
E. Insure the JCAHO is followed in the hospital.
Answer: A
70. _______________ refers to the number of patients occupying beds in the
hospital at a particular point in time, for example, January 5, 2009.
A. JCAHO
B. Census
C. Percentage of Occupancy
D. ALOS
E. Medicare Part A
Answer: B
71. Assignment of Benefts must be obtained from the patient _____________.
A. At discharge
B. When the patient is home
C. At time or service
D. At Registration
E. None of the above
Answer: D
72. If Medicare considers an item or service as medically necessary, it must meet
all of the following criteria except:
A. Provided at the convenience of the patient or doctor or hospital
B. Be consistent with generally accepted medical standards
C. Consistent with the patients diagnosis, illness or symptoms
D. Established as safe and effective
Answer: A
73. Verbal telephone orders must contain all of the following except:
A. The order must be written verbatim as taken over the telephone
B. SSN of the patient
C. Name of referring physician
D. The date the order was received
E. The time the order was received
Answer: B
74. MSP utilizes the ____________ when determining who is the primary or
secondary payer.
A. Deductibles
B. HIPAA
C. Birthday Rule
D. COB
E. ABN
Answer: D
The Health Care Revenue Cycle 98
75. Which of the following is not a type of consent?
A. Implied Consent in Fact
B. Implied Consent by Law
C. Special Consent
D. Emergency Consent
E. Informed Consent
Answer: D
76. DEERS:
A. Defense Enrollment Eligibility Reporting System
B. Defense Eligibility Enrollment Reporting System
C. Defense Enrollment Eligibility Recording System
D. Defense Enrollment Elastic Reporting System
Answer: A
77. ALOS:
A. Audited Length of Stay
B. Average Length of Stay
C. Average Line of Stay
D. Audited Leave of Stay
Answer: B
78. JCAHO:
A. Joint Committee on the Accreditation of Home Organizations
B. Joint Commission on the Accreditation of Health Care Organizations
C. Joint Committee on the Accreditation of Health Care Organizations
D. Joint Commission on the Average of Health Care Organizations
Answer: B
79. CHAMPVA:
A. Congressional Health and Medical Program of the Veterans Administration
B. Civilian Home and Medical Program for the Veterans Administration
C. Civilian Health and Military Program for the Veterans Administration
D. Civilian Health and Medical Program of the Veterans Administration
Answer: D
80. CHCBP:
A. Continued Health Continuum Beneft Program
B. Continued Health Care Beneft Premiere
C. Continued Health Care Beneft Program
D. Care Health Continued Beneft Program
Answer: C
End of Chapter 2
Chapter 3 - Processes and Procedures 99
Chapter 3 Processing Procedures
Chapter Topics
UB-04 Claim Form
Common Working File
Medicare Processing of the UB-04 Claim Form
Medicare Deductibles, Co-Payments and Co-Insurances for 2009
Electronic Billing
Financial Statements
Abbreviations & Acronyms
Sample Test Questions
After studying this chapter you will understand:
UB-04 Claim Form
UB-04 Field Locators and Data Elements
Insurance Policy and Coordination of Benefts (COB)
Common Working File
What does returning a Medicare claim as unprocessable mean?
Claim Form Processing Terminology
Medicare; MS-DRGs; 72-Hour Rule
Medicare Deductibles, Co-payments, Co-insurances
Clean Claim
Financial Statements: Superbill, Itemized Statement, and Data Mailer
Birthday Rule
Medicare Secondary Payer (MSP)
Electronic Billing: Electronic Data Interchange (EDI)
Chargemaster
The Health Care Revenue Cycle 100
UB-04 Claim Form
Patients rarely pay health care providers directly. The only payments they make to
the health care system is for insurance coverage (through premiums) or through co-
payments, co-insurances and deductibles. This, of course, represents only a small
fraction of what is actually paid for health care services and products.
The insurance policy is a legal contract between the policyholder (the consumer
who buys the contract) and the insurance carrier (the company or government
agency that agrees to pay for most of the approved health care services and treatments
provided the patient). Keep in mind that the insurance carrier (per the contract with
the patient) only pays for what it is legally liable to pay for as well as what it decides
is medically warranted. For example, if the patient has diabetes, the insurance
policy will not necessarily pay for everything associated with the treatment of
that disease. For example, there may be limitations on the amounts of insulin that
will be reimbursed, whether the insurance carrier will pay for a brand name or a
generic version of insulin, how many syringes will be paid for, how many glucose
(laboratory ) tolerance tests (GTT) will be paid for, how many offce visits and what
types of medical specialists will be allowed per month or year, how much will be
paid for medically proven complications related to the patients diabetes, etc. The
diabetic patient may very well require treatment and supplies that are medically
warranted and necessary, but this does not mean that the insurance company will
pay for everything. The patient may still be responsible for thousands of dollars of
uncompensated medically warranted and necessary treatment and supplies.
Generally, whether the patient is aware of it of not, there is more than one insurance
company responsible for payments. There is the primary insurance company that
pays frst. Insurance carriers that pay the remainder of the health care bill after the
primary insurance company has paid its share are known as the secondary (number
2 in line) and tertiary payers (number 3 in line). Therefore, if Medicare is the primary
payer, it pays the medical bill frst, then whatever treatment and products remain
unpaid, Medigap (for example, through Aetna) pays second and Blue Cross/Blue
Shield pays third. This process of determining in what order the insurance companies
pay is called coordination of benefts (COB). This does not mean the patient has
nothing remaining to pay after these three insurance companies are fnished
there are deductibles, co-payments and co-insurances, for which the patient is
contractually liable. Furthermore, not all medical treatments and products will be
approved for payment by these insurance carriers, so the patient may also have
additional bills to pay.
Information collected from the patient, doctor and hospital needs to be placed
on claim forms so the insurance carrier and Medicare can process them and issue
payment for health care services. There are two standard claim formsthe CMS-
1500 for treatment, services and products given to the patient outside the hospital,
and the UB-04 for services given the patient inside the hospital or affliated with the
hospital. The UB-04 is used for services rendered to the patient while admitted to
the hospital (inpatient), as well as for services provided the patient while using the
Chapter 3 - Processes and Procedures 101
emergency room, outpatient clinic, and other facilities affliated with the hospital but
on an outpatient basis.
The National Uniform Billing Committee (NUBC), Centers for Medicare and
Medicaid (CMS) and the American Hospital Association (AHA) are responsible for
the creation and revisions of the UB-04 (aka-CMS 1450) claim form (see example
p. 222,) that replaced the UB-92 as of February, 2005, which until then was the
form used for all hospital inpatient and outpatient services and procedures. As of
May 23, 2007, skilled nursing facilities (SNF), home health practitioners (such as
nurses, physical and occupational therapists, home health aides, etc.), outpatient
rehabilitation facilities, and community mental health centers were also required to
begin using this claim form for their invoicing and coding of health care services.
The electronic version of the UB-04, known as the X12N837 Institutional Health
Care Claim Transaction (837I), was created as a result of HIPAA. The X12N837 is
considered an Electronic Data Interchange transaction set (EDI), which is software
for this claim form, utilized on the computer. One of the major improvements of this
electronic version of the UB-04 is that secondary and tertiary payers can be billed
simultaneously with the primary insurance carrier, because this electronic version
incorporates a feature named Coordination of Benefts data (COB). COB determines
the fnancial responsibility for each insurance payerprimary, secondary, and
tertiary. In other words, the insurance carriers talk to each other and agree who
should pay the medical bills frst, then second and third.
The UB-04 or CMS 1450 claim form contains 81 Form Locators or Field Locators
(FL), which hold Data Elements. Data Elements are bits of information critical to
the payment of the claim by the insurance company. The information is inserted by
a medical coder and pertains to the medical treatment of the patient and the nature
of the invoice itself along with billing, coding, patient, hospital, department, clinic,
identifcation numbers, and other provider, patient and facility information. Note:
Form locators and data elements are crucial elements in the process of medical
billing.
There are 81 Field or Form Locators (FL), which are 81 numbered spaces (listed
from #1 to #81) on the UB-04 form, which delineate names, revenue/occurrence/
value codes, addresses, numbers, charges, third party payers, hospital and provider
identifcation, social security numbers, name of guarantor, credit card numbers,
fnancial information, ICD/CPT codes, hospital department information, and other
statistics necessary for the payment, analysis, storage, and adjudication of hospital-
related health care administered to the patient by a commercial insurance company,
third party administrator (TPA), TRICARE/CHAMPVA, Medicare or Medicaid, etc.
Important UB-04 Code/FL Defnitions
Each of the Field (Form) Locators on the UB-04 have specifc information that
is placed into them. It is important to know exactly what codes, numbers, and
information goes into the Form (Field) Locatorsthere are 81 of themfor
employment or test purposes.
The Health Care Revenue Cycle 102
Field Locators (FL) #1 to #17: Provider and Patient Information is placed here in the
UB-04. FL #4 is particularly important as it describes the Type of Bill (TOB) the
insurance company will receive from the hospital (see Completion of the #4
Form Locator in the UB-04 below).
Condition Codes
1. Are placed in Form Locators (FL) #18 to #28.
2. Are UB-04 claim form codes which defne circumstances relating to the
invoice that affects how the insurance company or third party payer
processes the health care bill. In other words, the Condition Code: 02
would tell the insurance company the bill for hospital services is because the
patient was injured while working on-the-job.
3. Examples:
02 Condition is Employment Related. This code is for medical services
provided due to the patient being injured while working on the job.
21 Billing for Denial. Code for billing for medical services that will not be
paid (not medically necessary or not covered by insurance).
40 Same Day Transfer. Code indicates the patient is being transferred from
one health care facility to another.
Occurrence Codes
1. Are placed in Form Locators (FL) #31 to #34.
2. Are UB-04 claim form codes used to identify a specifc date defning a
signifcant event that affects how the insurance company processes the health
care bill. In other words, the Condition Code: 01 would tell the insurance
company the bill for hospital services is because the patient was injured on
1/1/09 because of an mva. The specifc date is 1/1/09.
3. Examples:
01 Auto Accident. The date the auto accident or MVA (motor vehicle
accident) occurred.
11 Date of Onset of Symptoms/Disease.
18 Date of Patient or Benefciary Retirement.
Value Codes
1. Are placed in Form Locators (FL) #39 to #41.
2. Are UB-04 claim form codes used to specify a value of monetary nature such
as the cost of a specifc medical provision (hospital room), type of insurance
coverage that pays the hospital bill, or a type of insurance that will pay for a
specifc disease.
3. Examples:
01 Most common dollar amount (UCR) for the cost of a semi-private (2 beds
and 2 patients ) room in the hospital.
Chapter 3 - Processes and Procedures 103
12 Working Aged Patient (over 65 years), or spouse, with an Employer
Group Health Plan (EGHP).
13 End Stage Renal Disease (ESRD) Benefciary with Medicare Coordination
of Benefts (COB) of 30 months with an EGHP.
Revenue Codes
1. Revenue codes are descriptions and dollar amounts charged for hospital
services provided to the inpatient or outpatient.
2. Are placed in Form Locators (FL) #42 to #49
3. Are UB-04 claim form codes used to identify a specifc accommodation,
ancillary service or invoicing calculation for a particular service in the
hospital.
4. Examples:
250 Pharmacy: a dollar amount indicating the costs of the patient receiving
drugs while an inpatient in the hospital.
300 Lab: a particular dollar amount indicating the costs of the patient
receiving laboratory services such as a complete blood count [CBC] or
urinalysis [UA] while an inpatient or outpatient in the hospital.
351 Outpatient Procedures: a particular dollar amount associated with
surgical procedures done on an ambulatory basis not requiring
admission to the hospital as an inpatient.
450 Emergency Room: a particular dollar amount associated with health care
administered on an urgent basis in the hospitals ER.
Field Locator #56: This is where the National Provider Identifcation number (NPI) of
the doctor who is billing for medical services given to the patient in the hospital
is placed.
ICD-9-CM Codes
1. Are placed in Form Locators (FL) #66 to #71.
2. Are codes taken from the International Classifcation of Diseases, 9th
Revision, Clinical Modifcation coding manual (ICD-9-CM) and put into the
UB-04 claim form to describe diagnoses, trauma, medical conditions, medical
history, and V and E codes of the patient while in the hospital as an inpatient
or outpatient.
Field Locator #67: The main diagnosis (ICD) code that brought the patient to the
hospital in the frst place. After the patient initially comes to the hospital, this
is the preliminary major diagnosis presented to the medical staff or the major
diagnosis the referring doctor sent the patient to the hospital with for further
examination and treatment.
Field Locators #67A through #67Q: Other diagnosis (ICD) codes that are pertinent to
describing the patients medical condition.
The Health Care Revenue Cycle 104
Field Locator #69: Admitting Diagnosis (ICD). This is the diagnosis the admitting
physician at the hospital initially determined was the cause of the patients chief
complain (CC) when the patient frst came to the hospital. This diagnosiis may
be the same as that found in FL #67, or it may have been changed to refect what
additional examination and testing revealed.
Field Locator #70A to #70C: Patients reason for the hospital visit. Why the patient
came to the hospital in the frst place.
Field Locator #71: The Prospective Payment System (PPS) code is placed here. The
PPS is described later in this chapter.
Field Locator #72A to #72C: The External Cause of Injury code is placed here. These
are known as E codes and found in the ICD coding manual that describe what
trauma the patient suffered. Examples are car accident (MVA), fall, poisoning,
sports accident, act of terrorism, etc.
Field Locator #74: Main Procedure (CPT-4) codes and dates that the medical services
were provided are placed here. These are codes that describe what medical
services or treatment or supplies were provided at the hospital to the patient.
These CPT codes are found in the coding manual called the Current Procedural
Terminology, 4th edition (CPT-4).
Field Locators #74A to 74E: Other Procedural Terminology Codes {CPT} and dates
are placed here. These codes complement the codes entered in FL #74 (principal
treatment), which describe additional procedures and services rendered to the
patient at the hospital.
Completion of the #4 Form Locator in the UB-04
The chart on the next page is to be used for Form Locator #4 on the UB-04. It is
very important the FL #4 three-digit codes are understood because they inform the
insurance carrier of the shape of the invoice. Such as does the bill come from the
hospital, SNF, or a clinic (digit 1 called the Type of Facility); are services being
provided to an inpatient or outpatient, or is the patient at a rural or mental health
facility (digit 2 called the Bill Classifcation); and what type of bill is it: a no-pay
or hospital admission (digit 3 called the Frequency). Use the UB-04 coding form
in this study guide to help you understand how to complete this part of the form.
The following example illustrates how Form Locator #4 and the data elements are
connected (aka-linkage):
Chapter 3 - Processes and Procedures 105
Form Data Element Description
4
Type of Bill
(TOB)
The kind of claim form (TOB) the hospital is
submitting to the insurance company for payment.
Contains three (3) numbers with each digit
representing: (1) the type of health care facility
providing treatment, (2) status of the patient and/
or type of insurance, and (3) what type of payment
situation exists (how the hospital bill will be paid).
The TOB is used on all claims sent to Medicare,
Medicaid, Blue Cross/Blue Shield, commercial
insurance companies, TRICARE and workers
compensation insurance.
For this example, 110 is the data element which is placed into form locator (FL) #4
on the UB-04. It is often an important test question. See the UB-04 claim form, p. 222, for
the location of the FL #4 (right upper corner).
UB-04 Claim Form Type of Bill (TOB) Code 110 is known as a No Pay
Claim. For Medicare recipients, a hospital must submit a no-pay bill (utilizing
110) when the Utilization Review (UR) nurse that works for the hospital has
determined the Medicare patient should not have been admitted as an inpatient
because the admission is considered not medically necessary. However, the admitting
physician has determined the hospital admission is medically warranted and the patient
has been admitted anyway. Because Medicare is not going to pay for treatment, it
is mandatory that the hospitals registration, admissions, or fnancial departments
discuss monetary obligations with the patient, patients family, guarantor, or health
care surrogate at this time so that payment arrangements can be made. Regardless of
whether the hospital will be paid or not, Medicare must be notifed of all interactions of its
benefciaries with hospitals and doctors.
Identifying and Defning TOB 110
The chart below is to be used to determine the correct code to be placed in Form
Locator #4 in the UB-04. The following example illustrates how Form Locator #4
and the data element are connected (a.k.a.-linkage). Note: This is a commonly asked
question on coding tests and understanding this concept is crucial for the medical
coder because all UB-04 claim forms require FL #4 to be flled so payment can be
issued from Medicare or third party payers.
1. The frst digit is categorized as TYPE OF FACILITY. For example, the 1st
digit of 1 1 0 is 1 and defnes hospital for Place of Service (POS). This is
where the medical services are rendered to the patient.
2. The second digit is categorized as BILL CLASSIFICATION. For example,
the 2nd digit of 1 1 0 is 1 and defnes the type of patient who has been
admitted to the hospital, in this case an inpatient, who is utilizing Medicare
Part A benefts to pay their hospital bill.
The Health Care Revenue Cycle 106
3. The third digit is categorized as FREQUENCY. For example, the 3rd digit
of 1 1 0 is 0 which defnes a type of claim where payment from Medicare
to the hospital for medical services rendered to the patient will probably
not occur. This third digit tells the insurance company how the bills will be
coming in for payment from the hospital and providers.
Important This chart is to be used for flling out FL #4 for the TOB. The medical coder
has one set of choices for the frst digit, three sets of choices for the second digit, and
one set for the third digit.
First Digit: Type of Facility (Place of Service-POS)
1 Hospital
2 Skilled Nursing
3 Home Health
4 Religious Non-medical Healthcare Facility (Hospital)
5 Religious Non-medical Healthcare Facility (Extended Care)
7 Clinic (see special coding for second digit below)
8 Special Facility, Hospital ASC Surgery (requires special information
for second digit below)
Second Digit: Bill Classifcation (and/or type of patient or care level)
Use if frst digit is 1, 2, 3, 4 or 5.
1 Inpatient (Medicare Part A)
2 Inpatient (Medicare Part B)
3 Outpatient
4 Other (Medicare Part B)
5 Intermediate Care-Level I
or Second Digit: Classifcation for (type of ) Clinic
Use if frst digit is 7.
1 Rural Health Clinic (RHC)
2 Hospital Based or Independent Renal Dialysis Facility
3 Free Standing Provider-Based Federally Qualifed Health Center
(FQHC)
4 Other Rehabilitation Facility (ORF)
5 Comprehensive Outpatient Rehabilitation Facility (CORF)
6 Community Mental Health Center (CMHC)
Chapter 3 - Processes and Procedures 107
or Second Digit: Classifcation for (type of ) Special Facilities
Use if frst digit is 8.
1 Hospice (Non-hospital based)
2 Hospice (Hospital Based)
3 Ambulatory Surgical Center Services to Hospital Outpatients
4 Free Standing Birthing Center
5 Critical Access Hospital
Third Digit Classifcation: This is known as FREQUENCY, or how often the patient
is utilizing medical services and how many or types of bills are being generated.
A Hospice
Admission Notice
Used when hospice is submitting UB-04 as an admission
notice (Medicare is informed the patient has entered this
facility).
B Hospice
Termination or
Revocation Notice
Used when UB-04 is notice of termination or revocation
(patient will not be coming to this place for treatment).
0 Non-payment or
Zero Claim
Provider uses this code when payment is not anticipated
from the insurance company. Medicare requires this third
digit only for Spell of Illness for hospital inpatient
cases.
2 Interim-First
Claim
Used for frst of an expected series of bills for which
medical care is invoiced or for updating inpatient
deductibles.
Common Working File
The Common Working File (CWF) was developed by the CMS in 1989 to manage all
of the records for each Medicare patient. It is an information gathering device that
is decentralized into nine regional sites across the United States. The CWF is also
offcially known as Medicares master patient and procedural data base.
The Health Care Revenue Cycle 108
The CWF contains the following:
1. Medicare Patient Eligibility and Utilization data: claim history, MSP, ESRD
patient, benefts and effective dates of insurance coverages, LTRs, etc.
2. Beneft periods and days remaining in the current beneft period
3. Entitlement of Medicare Parts A and B
4. Medicare Parts A and B deductible information
5. Date of Birth (DOB)
6. Date of Death
Medicare Processing of the UB-04 Claim Form
What does returning a Medicare claim as unprocessable mean?
It means the Medicare Fiscal Intermediary (FI) or Medicare carrier (the insurance
company like Blue Cross/Blue Shield that actually signs a contract with Medicare
to provide health care services) uses many different review processes to check
submitted claims, and will notify the hospital or provider that their Medicare claim
cannot be processed and that it must be corrected and/or re-submitted. The claim
can be returned to the hospital or provider by Medicare either electronically or by
paper copy, with a checklist of items that need attention and directions on how to
make corrections.
1. The main reason that a Medicare claim is unprocessable is that it contains
incomplete or invalid data. An incomplete claim has required information
that is missing, such as DOB or NPI. An invalid claim has all the necessary
information, but some part of the required information is incorrect or illogical,
such as a wrong DOB or the NPI is missing some numbers and letters.
2. Corrections by the hospital or provider must be submitted to the Medicare
FI or carrier so the corrected claim can be processed. If it is not returned
within 45 days, that portion of the claim that is not corrected is considered
suspended and is returned as unprocessable, and the hospital or provider
is notifed by Remittance Advice (RA) or Explanation of Medicare Benefts
(EOMB).
3. When the Medicare FI or carrier returns a claim for correction, it will provide
the following:
The benefciarys (patient) name.
HICN (Health Information Claim Number) or Social Security Number
(SSN).
Dates that health care services were given to the patient.
Patient account number assigned by the hospital or doctors offce.
A list of the corrections to be made on the claim form, either by
description or by code.
Chapter 3 - Processes and Procedures 109
If the Medicare carrier or FI normally keeps certain required UB-04 data
elements on the patient (such as condition codes), then if that particular
feld locator is submitted incomplete, the FI or carrier will not return the
claim as unprocessable, since it is already on fle.
4. Medicare Claim Editor (MCE) is computer software that edits (reviews)
UB-04 and CMS-1500 claim forms for valid and complete data submitted
by hospitals, providers, and suppliers to insurance carriers. There are three
types of MCEs:
Code Edits examine the claim form for the correct use of ICD codes.
Coverage Edits examine the type of patient and the procedures
(CPT) performed on the patient to determine if the medical services
administered are covered by the insurance company.
Clinical Edits examine the clinical necessity of CPT and ICD information
for linkage. Linkage is where the patients diagnoses (ICD), and the
medical services provided (CPT) to the patient by the hospital and
doctor, are reasonable. For example, if the patient is diagnosed with
appendicitis, is the patient receiving the appropriate examinations, lab
tests, diagnostic imaging studies (x-rays, MRIs, CAT scans, etc.) and
surgical care to correct the appendicitis?
5. Medicare Administrative Contractor (MAC). By 2011, Medicare will amend
its contracts so that Medicare Parts A and B will be administered (the health
care paperwork will be handled) by 15 MACs. The provider or hospital or
supplier will be assigned to the MAC that covers the geographic location
where they are located. Until 2011, Medicare Parts A and B are being handled
by 25 FIs (Fiscal Intermediary) and 18 insurance carriers.
6. Billing Compliance programs must be established by the hospital or
physician practice, third party billing company, or collection agency to meet
legal requirements for Medicare best practices (the most effcient and correct
way to handle things). These compliance programs cover billing and coding
protocols and to prevent fraud and abuse. These programs include:
Employee training and competency assessments.
Internal and external audits of department operations.
Clinical issues as they relate to improved patient services through more
effcient billing.
How to Develop the Billing Compliance Program.
Making sure employees follow all billing laws and regulations
Providing compliance orientation and training to employees.
Making sure employees are compliant with all billing rules and
regulations.
Establishing a way to make sure employees know what they are doing.
Monitor their work on a regular basis.
Performing background checks on employees and vendors providing
Medicare contracted services.
The Health Care Revenue Cycle 110
Providing for non-retaliatory confdential reporting of suspected fraud
and abuse.
Establishing disciplinary policies for non-compliance by employees and
vendors.
Claim Form Processing Terminology
1. Incomplete: Any claim that has missing required information such as DOB,
HCIN, patients name, address, ICD or CPT codes, signatures, etc.
2. Invalid: Any claim that has all the required information, but some of
it is inaccurate such as wrong DOB or HCIN, patients name is spelled
incorrectly, address of hospital is wrong, ICD or CPT codes are wrong or not
linked properly, etc.
3. Required: Any data element or piece of information that is essential for the
claim to be processed by the Medicare FI or carrier.
4. Conditional: Any data element that must be completed if other conditions
or situations exist in the provision of health care services to the patient.
A perfect example is when the guarantor (the person who actually has
purchased the insurance, the insured) is different than the person who is
receiving medical attention in the hospital (the patient).
5. If the claim is Returned as Unprocessable: This does not mean the claim
will be physically returned to the hospital, doctor or supplier. It refers to the
fact that the FI or carrier, through any of a number of editing processes, will
notify the doctor or hospital or supplier of invalid and/or incomplete data
and request correction and re-submission of the claim within 45 days.
6. Charge Capture: The process by which all monies billed for health care
treatment, services, procedures and products are accurately and completely
collected and placed in the correct Field (Form) Locators on the UB-04, CMS-
1500 or other claim forms such as a superbill.
7. A Clean Claim is a claim that will pass all front-end claim editing by the
Medicare FI or carrier. This means the insurance carrier will send all claims
frst through a computer scanner (remember UB-04 and CMS-1500 paper
claim forms are printed with red optical scanning ink or in electronic form
for computers to read them) to quickly ascertain invalid and/or incomplete
information.
a. A claim that is processed electronically.
b. A claim, if investigated for further review, does not require additional
contact with the hospital, provider or supplier, insurance benefciary or
guarantor, or Social Security Administration (SSA).
c. A claim, if chosen for medical necessity review, has all supporting
medical evidence complete and valid (progress notes, laboratory results,
surgical reports, rehabilitation notes, etc.) and included with the original
UB-04 or CMS-1500 claim, as instructed by the Medicare FI or carrier.
Chapter 3 - Processes and Procedures 111
d. A claim that will not be reviewed on a retrospective or post-payment
basis. This means the Medicare FI or carrier cannot review a claim after it
has been paid to the hospital, doctor or supplier.
e. A claim that correctly identifes Conditional Payments. This is a
payment made by Medicare because another insurance company is
responsible for the bill. The claim is not expected to be paid within 120
days from the date of receipt by the primary insurance carrier, so this
conditional (temporary) payment is made by Medicare to prevent the
Medicare benefciary from using their own money to pay their medical
bills. Medicare reserves the right to collect the monies they paid out to
the primary insurance payer such as workers compensation, liability,
automobile insurance, etc.
f. A claim that correctly captures the Assignment of Benefts. The
Assignment of Benefts should be completed at the time of patient
registration, pre-admission, or admission, and never later than the patient
being discharged from the hospital. It is a written authorization signed
by the policyholder (owner of the insurance policy or covered patient
such as spouse or child) to the insurance company stating the insurance
company should pay the hospital, doctor or medical supplier directly.
If the provider or hospital accept assignment of Medicare benefts, they
agree to be paid by Medicare directly, accept only what the Medicare fee
schedule pays for medical services rendered, and only charge the patient
the Medicare deductibles, co-insurances and co-payments. If the hospital
or provider do not accept Medicare assignment, they can charge more
than what Medicare allows for a medical service, and they can demand
the patient pay the entire charge for medical treatment before they
are rendered. If the provider or hospital do not accept the Assignment
of Benefts, they are restricted to charging no more than 115% of the
Medicare fee schedule.
g. A claim that follows the provisions of the Working Aged Rule. This
rule is for someone who is at least 65 years old, currently employed and
covered by an EGHP, or is covered by an EGHP of a working spouse of
any age. Equal Beneft Rule: Federal law mandates that any employer,
with twenty (20) or more employees (full time or part time), must
offer the same health care coverage under the same conditions to their
employees over age 65, as that offered to employees and their spouses
who are under 65 years of age.
EGHP = Employer Group Health Plan.
The Health Care Revenue Cycle 112
h. A claim that follows the regulations of the Birthday Rule. The Birthday
Rule relates to coordination of benefts (COB) when the responsible
parents insurance is determined to pay the childs health care bills frst,
where both parents have health insurance. COB means the insurance
companies determine who is responsible to pay the childs medical bills.
Gender Rule: The male head of household (father) who has insurance is
determined to pay the childs health costs frst.
i. The Birthday Rule states that the birthday of the parent born frst in the
calendar year, regardless of the year he/she was born, is responsible to
have his/her health insurance pay the childs medical bills frst. If the
fathers DOB is January 31, 1960, and the mothers DOB is July 1, 1959,
although the mother is older, since the father was born in January, and
the mother was born in July, and January comes before July in the calendar,
it is the fathers insurance that is responsible to pay for his childs health
care bills frst.
j. Exceptions to the Birthday Rule:
If both parents have the same birthday, the parent with the health
insurance plan for the longer period of time covers the child frst.
If the parents are divorced or separated, and both have health
insurance plans, it is the parent who has legal custody of the child
whose health insurance pays the childs medical bills frst. If the
parent who has custody remarries, and if the new spouse has health
care insurance, then the new spouses insurance policy pays second.
Finally, the health care insurance plan of the parent that does not have
custody pays the childs medical bills last.
Exception: If the court has issued a divorce decree indicating that
one parent is responsible for paying their childs medical bills, then
that parent pays frst, but the health care insurance carrier has to be
made aware of this legal arrangement.
Medicare Secondary Payer (MSP)
Federal regulations require all health care providers, hospitals, and medical
suppliers to know when they can bill Medicare as the primary payer (frst insurance
company to pay the patients bill) or when they can bill Medicare as the secondary
payer (second insurance company to pay the patients bill). Medicare requires that
providers and hospitals accurately identify the primary payer and bill them frst.
Repeatedly billing Medicare frst when Medicare is the secondary payer, constitutes
fraud and abuse.
About three (3) months before a potential benefciary becomes eligible for coverage
by Medicare, an Initial Enrollment Questionnaire (IEQ) is completed by the patient,
which documents other health care insurance coverage they have that may be
Chapter 3 - Processes and Procedures 113
primary to Medicare. This information is entered into the Common Working File
(CWF).
Since 1980, costs have been shifted from Medicare to other sources of payment. In
essence, Medicare has moved its responsibility from primary payer to secondary
payer. Medicare is determined to be the secondary payer when:
1. The benefciary is injured on the job and whose treatment is covered frst by
Workers Compensation insurance the employer has purchased (required in
most states).
2. The benefciary has black lung disease documented by the federal
governmentusually those who have worked in coal mines-- and other
insurance is the primary payer.
3. The benefciary is injured due to a car accident as the driver, pedestrian,
or passenger, where the benefciarys no-fault automobile insurance is the
primary payer. Homeowners or commercial insurance is primary when the
benefciary is injured as the result of someone elses fault, e.g. falling on their
property, an accident due to their negligence, or falling on a slippery foor in
a store or being assaulted by an employee, etc.
4. Liability insurance that covers injuries as a result of someone elses fault
where subrogation is involved, is the primary payer. Subrogation mean the
injured persons own insurance pays frst, then the responsible partys insurance
becomes legally obligated to reimburse the injured partys insurance who has
already paid frst.
5. The benefciary is entitled to Medicare coverage due to end stage renal disease
(ESRD). However, Medicare has a 30 month coordination of benefts (COB)
period that begins when a patient is frst diagnosed with ESRD, regardless if
the benefciary is enrolled with Medicare or not. The 30 month COB means that
regardless if the person is enrolled with Medicare, no matter what their age, 30
months after the day they are diagnosed with ESRD, Medicare will become
the primary payer for ESRD. During the initial 30 months, the benefciary
would be required to fnd another primary payer until Medicare coverage
kicks in and pays frst.
If ESRD is the only reason the patient is receiving Medicare coverage, then
after another insurance plan covers the frst 30 months as the primary payer:
Medicare coverage will end 12 months after the patient no longer
requires kidney dialysis maintenance care. Patients other insurance will
then be responsible again to pay for ESRD.
Medicare coverage will end 36 months after the patient has a successful
kidney transplant. Patients other insuarance will then be responsible
again to pay for ESRD.
After Medicare has terminated coverage in #1 or #2 above, EGHP
provided for employees aged 65 or older or spouse (of any age) of
employee with EGHP, will again resume payment for care related to
ESRD.
The Health Care Revenue Cycle 114
Where Veterans Administration (VA) health care coverage is available for
ESRD care, the patient can choose either Medicare or VA coverage, but
not both. In this case, if the VA health care coverage is chosen, it handles
all ESRD treatment from the date it is diagnosed, whereas Medicare
begins coverage only after the 30 month COB.
Medicare coverage will end when disabled patients with ESRD under 65
years of age are covered by LGHP (more than 100 employees). In this case,
the LGHP covers all ESRD treatment. For example, if the patient under
65 years of age had LGHP coverage when frst diagnosed with ESRD,
the LGHP would cover all treatment related to the ESRD. If the patient
had received Medicare coverage after the 30 month COB, and then was
eligible for LGHP coverage, the LGHP would assume being the primary
payer for ESRD instead of Medicare. LGHP=Large Group Health Plan,
which means employers with more than 100 employees provide coverage with
major insurance carriers such as AllState, State Farm, Humana, Aetna U.S.
Healthcare, United Health, Blue Cross/Blue Shield, etc.
MS-DRGs are also known as Medicare Severity-Diagnosis Re-
lated Groups.
The CMS created 745 MS-DRGs which are based on how much service or product
a patient consumes or utilizes in the hospital, or how long the patient stays in the
hospital.
These MS-DRGs are based on 25 major diagnostic categories (MDCs), which are
25 groupings of associated diagnoses of illnesses, pathologies, or conditions. An
example of an MS-DRG would be diabetes and the associated complications affliated
with this disease such as retinopathy, neuropathy, poor wound healing, etc. or
comorbidities such as obesity and poor physical status of the patient.
MS-DRGs allow the hospital to defne and measure what kinds of diseases and
what types of patients the hospital treats. CMS allows the hospital to adjust the claim
forms sent to the Medicare FI or carrier up to 60 days after submission, by sending
in subsequent (additional corrected) claim forms, from the date the hospital receives
the Remittance Advice (RA) from Medicare. The CMS uses the UB-04 claim forms to
determine which of the 745 MS-DRGs are applicable to the hospital.
MS-DRGs are created based on three (3) levels of payments to the hospital by the
Medicare FI or carrier:
1. Major complication (infection) or comorbidity (pre-existing condition such as
obesity, advanced age or diabetes). MCC= major complication or comorbidity.
2. Complication or comorbidity = CC.
3. No complication or comorbidity.
MS-DRGs do not produce any money savings to Medicare, but will increase
payments to hospitals treating patients that are more severely sick or have more
complicated diseases, and decrease payments to hospitals that treat patients who
Chapter 3 - Processes and Procedures 115
are less sick or have fewer complicated diseases. From a practical point of view, a
hospital that treats more severely sick people (heart disease and cancer, for example)
will use more medical services and supplies, and should be paid more by Medicare,
than a hospital that treats patients whose diagnoses are less complicated and more
routine (uncomplicated diabetes, foot care, simple fractures, etc.) Therefore, major
medical centers (such as University of Pennsylvania, Harvard, Stanford, Mayo
Clinic, Columbia University, University of Chicago, etc.) that have medical schools
and teaching hospitals will attract the more complicated diseases and will have the
personnel and equipment and expertise. Therefore, Medicare, through the MS-DRG,
will recognize this and pay them more.
MS-DRGs are defned by the following criteria:
1. Diagnosis: Primary and secondary diagnoses (ICD).
2. Procedures: medical and surgical procedures (CPT and HCPCS).
3. Complications
4. Comorbidities
5. Signs and symptoms
6. Gender (male or female)
7. Discharge status from care or the hospital
Medicare DRG Window (The 72-Hour Rule)
1. Applies to Inpatient Prospective Payment System (IPPS) hospitals and
providers paid by the DRG payment system. The IPPS is a method of
payment and DRG is a fee schedule, which describe the mechanism by which
Medicare pays for services. Medicare designates certain types of hospitals
either as participating with IPPS or not participating with IPPS. The Medicare
DRG window, 72-Hour Rule, does not apply to non-IPPS hospitals (see #2
below). The 72-Hour Rule means that if the consumer gets treatment and
services and products related to their illness or injury outside of the hospital
as an outpatient for up to three days, then has to be admitted to a hospital for
the same illness or injury, according to Medicare, all the outpatient services
received outside the hospital for up to 3 days prior to being admitted to
the hospital, PLUS all the care received while admitted to the hospital as an
inpatient, would be ALL bundled (combined) together and coded and billed
on the claim forms as one incident.
2. For example, a patient has chest pain and weakness and shortness of breath
for three days (for example, Monday-Tuesday-Wednesday), then goes to his
family doctor for an examination, diagnostic testing (EKG), and treatment
for a heart condition, gets medicine from the local pharmacy for his heart
condition, then is admitted to the hospital for a week (Thursday through the
following Wednesday), and is treated for this same heart condition. Medicare
states that the 3 days of outpatient treatment and the 7 days of inpatient
treatment, all for the same heart condition (principal diagnosis), should be
billed as if it were one episode of illness on the claim forms. In other words,
The Health Care Revenue Cycle 116
only the 3 days of outpatient treatment, no matter how much outpatient
treatment the patient actually received, and all the 7 days of inpatient
treatment for the same diagnosis, will be consideration as one (bundled) and
billed as one. Non-diagnostic treatment and outpatient services not related to
the principal diagnosis provided within 3 days of admission to the hospital,
are not covered by the 72-hour Rule and must be billed separately (cannot be
bundled) on different claim forms.
3. Non-IPPS hospitals are subject to the 24-Hour Rule (which acts just like the
72-Hour Rule but for 24 hours instead) and exempt from the 72-Hour Rule.
Non-IPPS hospitals that are covered by the 24-Hour Rule include:
Psychiatric Hospitals.
Rehabilitation Hospitals (those that provide PT, OT, ST to patients that
have suffered stroke, cancer, severe trauma, etc.)
Childrens Hospitals.
Long-term Care Hospitals (LTC)
Cancer Hospitals.
ANY hospital located outside the 50 states, District of Columbia, or
Puerto Rico.
Resource Utilization Groups (RUGs)
There are 53 RUGs, representing a mix of different types of inpatients, diagnoses,
conditions and pathologies, that are found in a Skilled Nursing Facility (SNF).
By determining the variety of patients and their health status in an SNF, Medicare
can ascertain what payment to make for each type of patient and medical services
required under the SNF Prospective Payment System (PPS). In other words,
Medicare can examine the kinds of diseases patients are being treated for at nursing
homes all over the country and decide how much money to pay the SNF for their
services in consideration of the funds Medicare has available.
Critical Access Hospital Program:. The CAH program assures Medicare benefciaries
the ability to get medical care in rural areas where there is a lack of doctors,
emergency rooms, maternity facilities, cancer treatment facilities etc. Medicare can
allocate suffcient funds so that enough doctors and hospitals and equipment are
available to serve the needs of the population in areas distant from cities all over the
United States.
Chargemaster
The chargemaster is also known as the Charge Description Master (CDM). The
CDM contains a variety of numbers and letters that include department numbers,
revenue codes, chargemaster numbers, descriptions of charges, dollar amounts of the
charges, CPT/HCPCS codes, modifers, and general ledger numbers (numbers in a
list describing some aspect of service or product supplied to the hospital inpatient
or outpatient). The chargemaster is a master pricing list, the main compilation of all
charges (amount of money billed) for services, drugs, medical equipment, supplies,
Chapter 3 - Processes and Procedures 117
or anything provided in the delivery of health care to the hospital inpatient or
outpatient.
Data elements of the chargemaster are placed in the UB-04 claim form in feld
locators (FL) 42 to 49, some of which are known as revenue codes, are numbers that
defne specifc accommodations, ancillary services, or billing calculations such as
370 for anesthesia or 490 for Ambulatory Surgical Center (ASC). 490 describes
the use of the surgical suite by the doctor in the ASC, and 370 describes the use
of the anesthesia equipment the hospital provides the doctor. Revenue codes were
developed by the National Uniform Billing Committee (NUBC). Another type
of data element of the chargemaster is known as the Department Number. This
is a three digit number, for example 335 for radiology department or 770 for
the medical supplies department, that defnes which department in the hospital is
charging the patient for a specifed health care service or product.
Figure 7: Chargemaster
Chargemaster Numbers are a combination of numbers the hospital assigns
to describe supplies, procedures, or use of facilities. In the following example,
the chargemaster number includes both the item (or product) number and the
department number which goes into FL 42 to 49. For example:
Department Number = 325 for the medical supplies department
of the hospital that has the sutures in its
inventory
Item or Product Number = 6767 for sutures (which is a product
the doctor uses to sew up a surgical
incision).
The Health Care Revenue Cycle 118
THEREFORE, the Chargemaster Number = 3256767 (325 + 6767).
goes in the UB-04 in FL 42 to 49. This number tells Medicare what
hospital department and what product is being billed.
Charges, created by a series of numbers (270, 325, 6767 and 1), refect what the
patient and the insurance company or Medicare are being billed for a specifc
medical item. All these numbers, and the charge of $60.00, is placed in the UB-04
in FL 42 to 49. This way the UB-04 shows numbers for each service, procedure or
product that is billed.
The following example for sutures is as follows:
Revenue Code = 270 (Surgery) This is the department where the
sutures will be used.
Department Number = 325 (Medical Supplies) This is where the inventory
(sutures) are stored and will be billed to.
Item Number = 6767 (Sutures)
Description of Item = Sutures
Units (how many?) = 1 (Package of Sutures)
Charge = $60.00 (Per package of Sutures)
Medicare Deductibles, Co-Payments and Co-
Insurances for 2010
These fgures change every year. For more information contact: www.medicare.gov.
The following chart displays the fees the patient pays for the health care services
and products he/she receive when Medicare is used to pay for the treatment. These
fgures should be memorized as their use is routine for health care employees (It is
also wise that students commit them to memory.)
Medicare
Calculation per Beneft
Period
2010 Beneft Period
(What the Patient Pays)
Part A: Hospital Inpatient
1. Part A Deductible for Days 1
through 60
2. Part A Co-Insurance for Days
61-90
3. Part A Lifetime Reserve Days
(LTR) or Non-Renewable
days. Days 91-150.
This satisfes the 2010
Inpatient Deductible
Rate is 25% of 2010
Inpatient Deductible
Rate is 50% of 2010
Inpatient Deductible
Amount
= $1,100.00 for 2010 per
each Illness
= $275.00 per day
(1100/4 = $275.00)
= $550.00 per day
(1100/2 = $550.00)
Chapter 3 - Processes and Procedures 119
Part A: Skilled Nursing Facility
(SNF)
Inpatient in the SNF for Days
1-20
Inpatient in the SNF for Days
21-100
No Deductibles or Co-
Insurance or Co-payments
Rate is 1/8 of 2010
Inpatient Deductible
Amount
= $0
= $137.50 per day
(1100/8 = $137.50)
Part A: Blood Deductible for
2010
Patient pays for frst 3
pints
= 3 pints of blood for
2010
Part B Outpatient Annual
Deductible
This satisfes the
Medicare Part B
Outpatient Deductible
$155.00 for 2010. The
patient pays this once/
year for all services
and products provided
under Medicare Pt. B
Electronic Billing
Under HIPAA, the use of electronic billing of health care services (Electronic
Data Interchange: EDI) has been strongly promoted and the use of paper claims
discouraged. As of October 16, 2003, HIPAA has prohibited most Medicare
participating hospitals, providers and medical suppliers from submitting paper
claims to Medicare. Also, electronic submission has to be HIPAA compliant before
payment is made.
Examples of electronic billing (non-paper) transactions to the insurance carrier for
payment include:
1. Entry of medical information by hand (manual, typing on the keyboard) into
the computer.
2. Personal Computer (PC) downloading of data.
3. Use of tape, compact disc (CD), or fash drive to electronically transfer
information to the computer.
4. Use of a Central Processing Unit (CPU), a large main-frame computer, to
another CPU.
Advantages of Electronic Billing for the hospital, provider, and insurance carrier
include:
1. Faster payment (no delays due to mailing and re-mailing claim forms)
2. Less paper needed and less clerical involvement by fewer people; more
automation of billing process.
The Health Care Revenue Cycle 120
3. Speeds up moving information of the health care claim to the insurance
carrier.
4. An electronic receipt (proof) that the medical information was sent to the
insurance carrier is created.
5. Faster follow-up and communication between the hospital, provider, and
medical supplier and insurance carrier.
Disadvantages of Electronic Billing for the hospital, provider, and insurance
carrier include:
1. Not every insurance carrier handles electronic billing transactions effectively;
there still may be problems.
2. Computer attachments, formats, software, etc., may not be compatible
between hospital and provider and insurance carrier; uploading and
downloading information problems and incompatibilities.
3. Retrieval of information and communication issues between parties is
compromised.
4. Security issues; hacking.
Types of Financial Statements
(see example of the Superbill on page 223.)
Itemized Statement. Shows a detailed accounting of every hospital service included
on the patients bill including date of service (DOS), description of service, all codes,
amounts of monies charged, what the insurance company will pay, what the patient
has paid and will owe, and totals. Also known as an I-Bill. An itemized statement is
generated after a UB-04 has been established; the UB-04 summarizes all the charges
listed on the I-bill.
Superbill. Is an invoice that documents the most common ICD/CPT/HCPCS codes
and charges for medical services and products used in an outpatient hospital facility,
clinic, or offce, including routine examination, treatment, laboratory and diagnostic
services. A superbill will be customized to refect the services and products provided
for each medical specialty, and it is designed to eliminate the medical coder from
transcribing to a claim form all the necessary information from the medical record or
patient chart. The superbill becomes the claim form, as the physician simply flls out
the superbill, which is then sent directly to the insurance payer. The superbill is also
known as a Face Sheet or an Encounter Form or Charge Slip.
Data Mailer. A statement used to tell the patient how much the patient owes the
hospital or doctor on an account with a balance. It also tells the patient how old the
amount owed is (e.g.-30 days, 60 days, 90 days) or if it has been sent to a collection
agency.
Chapter 3 - Processes and Procedures 121
Abbreviations and Acronyms
AHA American Hospital Association
CBC Complete Blood Count
CC Complication or Comorbidity
CD Compact Disc
CDM Charge Description Master
CORF Comprehensive Outpatient Rehabilitation Facility
CMHC Community Mental Health Center
CMS-1500 A universal claim form used by doctors, medical supply companies,
ambulatory surgical centers, orthotic and prosthetic suppliers, etc.,
for patients on an outpatient basis for billing dollar amounts and
coding medical diagnoses and procedures. This claim form is used
for non-hospital services.
COB Coordination of Benefts
CPU Central Processing Unit
CWF Common Working File
CPT Current Procedure Terminology
DOB Date of Birth of the patient
EDI Electronic Data Interchange
EGHP Employee Group Health Plan (more than 20 employees)
EOMB Explanation of Medicare Benefts, also known as Remittance Advice.
FI Fiscal Intermediary, also known as carrier, is an insurance company
that contracts with Medicare to provide health care services and
products to its benefciaries.
FL Form Locator or Field Locator which is found on the UB-04
FQHC Federally Qualifed Health Center
HICN Health Information Claim Number found on the Medicare card, or
Social Security Number for the patient
ICD/ICD-9-CM International Classifcation of Diseases, 9th Revision, Clinical
Modifcation
IEQ Initial Enrollment Questionnaire
LGHP Large Group Health Plan (more than 100 employees)
LTC Long Term Care
MAC Medicare Administrative Contractor
MCC Major Complication or Comorbidity
The Health Care Revenue Cycle 122
MCE Medical Claim Editor
MDC Major Diagnostic Categories
MS-DRG Medicare Severity-Diagnosis Related Groups
MSP Medicare Secondary Payer
NUBC National Uniform Billing Committee
ORF Other Rehabilitation Facility
PC Personal Computer
PPS Prospective Payment System, or IPPS (Inpatient Prospective Payment
System), or OPPS (Outpatient Prospective Payment System)
RHC Rural Health Clinic
RUG Resource Utilization Groups for Skilled Nursing Facility (SNF)
SNF Skilled Nursing Facility
TOB Type of Bill. Placed in feld locator #4 in the UB-04 claim form.
UA Urinalysis
UB-04 A universal claim form used by a hospital for billing dollar amounts
and coding medical diagnoses and procedures (ICD, CPT, HCPCS)
for inpatients/outpatients. Also known as CMS 1450; used to be
called the UB-92.
UR Utilization Review
Chapter 3 - Processes and Procedures 123
Sample Test Questions
These questions in multiple choice format require particular attention to the details
concerning the UB-04 and CMS-1500 claim forms, all aspects concerning types of
bills, and what is included in each form locator or block of each insurance form.
These questions are detailed and require the student or employee to differentiate
minutiae. These 65 questions should be answered in 65 minutes or less.
1. The UB-04 claim form is also known as the __________ which replaced the
_____________.
A. CMS-1500;UB-92.
B. CMS-1450;UB-92.
C. UB-92; CMS-1450.
D. X12N837; CMS-1500.
Answer: B
2. The UB-04 has ________________ or _______________.
A. 33 Blocks, 81 Data Elements.
B. 81 Form Locators, 33 Blocks.
C. 81 Form Locators, 81 Field Locators.
D. None of the above.
Answer: C
3. The UB-04 must be used by all of the following when it involves hospital
inpatient or outpatient care:
A. Medicare, Medicaid
B. Workers Compensation Insurance
C. TRICARE
D. Commercial Insurance Companies, Blue Cross
E. All of the above
Answer: E
4. Conditions Codes are:
A. Found in FL #18 to #28.
B. Defnes circumstances relating to the invoice that affects how the insurance
company processes the invoice.
C. Examples are 02, 21, and 40.
D. All of the above.
Answer: D
5. ____________ are found in FL #42 to #49.
A. Condition Codes
B. ICD Codes
C. Occurrence Codes
D. Revenue Codes
E. Value Codes
Answer: D
The Health Care Revenue Cycle 124
6. ___________ are used to identify a specifc accommodation, ancillary service,
or invoicing calculation for a particular service provided in the hospital in the
CMS 1450.
A. Condition Codes
B. Revenue Codes
C. Value Codes
D. ICD Codes
E. Occurrence Codes
Answer: B
7. Form Locator #4 is very important as it describes in the UB-04 the
_____________.
A. Admitting Diagnosis
B. Provider and Patient Information
C. Type of Bill
D. External Cause of Injury
E. E Code
Answer: C
8. Form Locators #1 to #17 in the CMS-1450 describe ________________.
A. Admitting Diagnosis
B. Provider and Patient Information
C. Type of Bill
D. Main Diagnosis Code
E. NPI
Answer: B
9. ____________ describes the TOB the hospital is submitting to the insurance
company for payment in the CMS-1450.
A. FL# 69
B. FL# 71
C. FL# 18 to #28.
D. FL# 4
E. None of the above.
Answer: D
10. ______________ codes in the UB-04 the external cause of injury such as car
accident, sports injury, poisoning, or terrorism.
A. FL #72A to C
B. FL #70A to C
C. FL #71
D. FL #42 to #49
E. FL #31 to #34
Answer: A
Chapter 3 - Processes and Procedures 125
11. ____________ claim is one that has missing required information.
A. Incomplete
B. Clean
C Invalid
D. Required
E. Complete
Answer: A
12. ___________ claim is one that has all the necessary information but the data is
inaccurate or illogical.
A. Incomplete
B. Clean
C. Invalid
D. Valid
E. Complete
Answer: C
13. A clean claim involves the following except:
A. Will pass all front-end claim editing by a Medicare FI or carrier.
B. It is processed electronically.
C. Will be reviewed on a retrospective or post-payment basis.
D. If investigated for further review, does not require further contact with
the hospital, provider or supplier, SSA, or insurance company.
E. If chosen for medical necessity review, all supporting medical evidence and a
valid/complete UB-04 have already been included.
Answer C
14. When a Medicare FI or carrier returns the hospitals UB-04 claim form as un-
processable, the hospital has __________ to correct it and re-submit it.
A. 88 days
B. 45 days
C. 90 days
D. 100 days
E. None of the above
Answer: B
15. ____________ was developed by the CMS in 1989 to manage all of the records
of each Medicare benefciary. It is an information gathering device that is
decentralized into 9 regional sites across the United States.
A. Fiscal Intermediary
B. HICN
C. MSP
D. CWF
E. RHC
F. TOB
Answer: D
The Health Care Revenue Cycle 126
16. The main procedural code (CPT) is placed in _____________ in the UB-04.
A. FL #69
B. FL #67A to Q
C. FL #74
D. FL #4
E. FL #56
Answer: C
17. ___________ is a UB-04 claim form code used to identify a specifc date defning
a signifcant event that affects how the insurance company processes the
invoice.
A. Occurrence Code: FL #31 to #34
B. Value Code: FL#39 to #41
C. Revenue Code: FL #42 to #49
D. ICD Code: FL #66 to #71
Answer: A
18. The name of the pieces of information (or bits of data) placed in the 81 feld or
form locators in the UB-04 claim form is known as _______________.
A. CWF
B. Data Elements
C. CPT
D. Clean Claim
E. TOB
Answer: B
19. The UB-04 TOB code is a 3-digit code whereby each digit is determined by
____________ and entered in FL# _____.
A. First Digit-Type of Facility (POS)
B. Second Digit-Bill Classifcation for the frst digit being 1 to 5
C. Second Digit-Bill Classifcation for the frst digit being 7
D. Second Digit-Bill Classifcation for the frst digit being 8
E. Third Digit-Frequency
F. 4
G. 69
H. 71
I. A, B, C, D, E, F
J. A, B, D, G
K. C, D, E, H
Answer: I
20. The CWF contains the following:
A. Those benefciaries who have Medicare Parts A and B
B. Medicare Parts A and B deductible information
C. DOB, Date of Death
D. Beneft periods and days remaining in the current beneft period
E. All of the above
Answer: E
Chapter 3 - Processes and Procedures 127
21. The blood deductible for 2009 for Medicare is ______________.
A. 1 Pint
B. 2 Pints
C. 3 Pints
D. 4 Pints
E. 5 Pints
Answer: C
22. The frst 20 days of inpatient treatment in a SNF for Medicare will cost the
patient:
A. $1068.00 per year
B. $ 267.00 per day
C. $ 133.50 per day
D. $0
Answer: D
23. Days 21 through 100 for inpatient treatment in a SNF for Medicare will cost the
patient:
A. $1068.00 per year
B. $ 267.00 per day
C. $ 133.50 per day
D. $0
Answer: C
24. The patient will have to pay ____________ deductible for 2009 for Medicare
Part A Hospital inpatient care.
A. $1068.00
B. $ 256.00
C. $ 133.50
D. $0
Answer: A
25. Medicare will pay for the frst ___________ days of inpatient care at a SNF per
year.
A. 60 days
B. 90 days
C. 100 days
D. 150 days
E. None of the above
Answer: C
26. The Chargemaster includes all of the following except:
A. Department Numbers
B. Revenue Codes
C. Refunds
D. CPT/HCPCS codes
E. Charges
Answer: C
The Health Care Revenue Cycle 128
27. LTRs are ______________ and pay for _________________ days of Medicare
Part A inpatient hospital care.
A. Renewable; 91 to 150
B. Non-renewable; 91 to 150
C. Non-renewable; 61 to 90
D. Renewable; 61 to 90
Answer: B
28. $267.00 per day is what the patient pays for _______________________ for
Medicare Part A inpatient hospital care.
A. Deductible
B. Co-insurance
C. LTR
D. SNF
E. None of the above
Answer: B
29. A No-Pay Claim is defned as:
A. For Medicare patients.
B. Hospital must submit this TOB when the UR nurse has determined the
Medicare patients admission is not medically necessary.
C. The admitting physician, however, feels the Medicare patients hospital
admission is medically warranted.
D. It will be necessary for the registration and/or fnancial department to
discuss
with the patient, their family, guarantor, or health care surrogate monetary
obligations.
E. A hospital invoice that will probably not be paid by Medicare.
F. None of the above.
G. All of the above.
Answer: G
30. ________________ must be established by the hospital or physician practice,
third party billing company, or collection agencies to meet Medicare best
practices billing and coding protocols and to prevent fraud and abuse.
A. No-Pay claims
B. LTRs
C. Billing Compliance programs
D. MCEs
E. MACs
Answer: C
Chapter 3 - Processes and Procedures 129
31. An _______________ provides a complete detailed accounting of every hospital
service posted to the patients account including DOS, description of services
and products, all codes, dollar amounts, estimated insurance payment, and
patients fnancial obligations and what the patient already paid by leaving a
deposit.
A. Itemized Statement
B. Superbill
C. No-pay claim
D. Data Mailer
E. UB-04
F. Face Sheet
Answer:A
32. A _______________ is an invoice to document the most common ICD/CPT/
HCPCS codes and charges for medical services and products, is customized
for each medical specialty, and be sent directly to the insurance carrier for
payment, and eliminates the need for transcription from the medical record.
A. Superbill
B. Face Sheet
C. Encounter Form
D. Data Mailer
E. B, C and D
F. A, B, and C
Answer: F
33. Medicare is determined to be the secondary payer when _______________.
A. The employee is injured on the job and workers compensation insurance
will cover the health care costs frst.
B. The person has black lung disease as determined by the federal government.
C. The person has suffered an injury covered by auto no-fault, liability,
commercial, or homeowners insurance which will pay the health care costs
frst.
D. The person has ESRD, however, Medicare will be the primary payer after a
15 month COB period.
E. All of the above.
F. A, B, and C
G. B, C, and D
Answer: F
34. When the provider, hospital or medical supplier repeatedly bills Medicare as
the primary insurer when they know Medicare should be billed secondarily,
and they do not identify the primary payer, this constitutes _____________.
A. Violation of MSP provisions
B. Fraud
C. Abuse
D. All of the above
E. None of the above
Answer: D
The Health Care Revenue Cycle 130
35. __________ is software that edits UB-04 and CMS-1500 claim forms for validity
and completeness.
A. MCE
B. MSP
C. EOMB
D. PPS
E. FQHC
Answer: A
36. The electronic version of the UB-04 is known as:
A. Explanation of Medicare Benefts
B. X12N837 Institutional Health Care Claim Transaction
C. FQHC
D. MCE
E. Common Working File
Answer: B
37. The ______________ relates to the COB for health care insurance to determine
which parents insurance coverage pays their childs medical bills frst, when
both parents have health care insurance.
A. Chargemaster
B. MCE
C. Birthday Rule
D. EOMB
E. Assignment of Benefts
Answer: C
38. ______________ is a written authorization, signed by the insurance
policyholder or patient, given to the insurance carrier indicating payment for
medical services should be sent to the hospital or provider directly.
A. Birthday Rule
B. EOMB
C. FQHC
D. MCE
E. Assignment of Benefts
F. Chargemaster
Answer: E
Chapter 3 - Processes and Procedures 131
39. Advantages of Electronic billing of health care claims to the insurance carrier
include:
A. Faster payment to the hospital.
B. Less paper required; fewer people involved in the billing process; more
automation.
C. Receipt of all communication and transactions between the hospital and
insurance company is made.
D. Faster follow-up and communication between the hospital and insurance
carrier.
E. All of the above.
F. B, C and D
Answer: E
40. Concerning EDI, HIPAA:
A. Encourages the use of electronic transactions (EDI) for the hospital to bill
Medicare.
B. Discourages the use of paper claims for billing purposes.
C. Since 10/16/2003, only allows Medicare participating hospitals to bill
electronically.
D. Electronic submission of claim forms must be HIPAA compliant before
payment is made to the hospital.
E. All of the above
F. A, B and D
Answer: E
41. ________________ describes the main pricing list for hospital services,
products, supplies or drug prices for inpatients and outpatients.
A. EDI
B. Chargemaster
C. MS-DRG
D. COB
E. Data Mailer
Answer: B
42. _____________ defne and measures what kinds of diseases and what types of
patients are using the hospital.
A. EDI
B. Chargemaster
C. MS-DRGs
D. COB
E. Data Mailer
Answer: C
The Health Care Revenue Cycle 132
43. CMS allows a hospital to fle subsequent inpatient DRG adjustments up to
_______________ from the date the hospital receives the RA.
A. 60 days
B. 30 months
C. 100 days
D. 45 days
E. 90 days
Answer: A
44. MS-DRGs are determined based on three levels of payments from the
Medicare FI or carrier, which are:
A. MCC
B. CC
C. No complication or comorbidity
D. All of the above
E. A and C
Answer: D
45. _____________ applies to IPPS hospitals where all outpatient medical and
diagnostic services provided up to three days prior to admission to the
hospital, that are related to the primary diagnosis, and all care provided while
the consumer is an inpatient, all for the same principal diagnosis, are bundled
together and billed together.
A. 24-hour Rule
B. 48-hour Rule
C. 72-hour Rule
D. MS-DRG
E. RUG
Answer: C
46. The 72-hour Rule does not apply to all of the following except:
A. Psychiatric Hospitals
B. Ambulance Services
C. IPPS Hospitals and Providers
D. Childrens Hospitals
E. Cancer Hospitals
F. Any hospital outside the 50 states, Washington DC, and Puerto Rico
Answer: C
47. __________________ program assures that patients with Medicare access to
health care services in rural areas.
A. 24-hour Rule
B. 72-hour Rule
C. MS-DRG
D. Critical Access Hospital
E. Chargemaster
Answer: D
Chapter 3 - Processes and Procedures 133
48. The _____________ applies to Psychiatric, Rehabilitation, Cancer, and Non-
IPPS hospitals.
A. 24-hour Rule
B. 72-hour Rule
C. Critical Access Hospital
D. MS-DRG
E. 48-hour Rule
Answer: A
49. ____________ are used by Medicare to determine payment to SNF patients
based on the patients health status and amount of care they require.
A. RUGs
B. MS-DRGs
C. IPPS
D. Chargemaster
E. 72-hour Rule
Answer: A
50. There are 53 RUGs which represent the mix of different types of inpatients,
diagnoses, conditions and pathologies, that are found in a:
A. CAH
B. ASC
C. SNF
D. E/R
E. None of the above
Answer: C
51. ______________ are a combination of numbers (such as 3256767) the hospital
assigns to describe supplies, procedures, or use of facilities.
A. Global Charges
B. UCRs
C. No Pays
D. Chargemaster Numbers
E. Professional Components
Answer: D
52. ____________ is computer software that edits UB-04 and CMS-1500 claim forms
for valid and complete data submitted by hospitals, providers, and suppliers
to insurance carriers.
A. CAH
B. UCR
C. EDI
D. RUG
E. MCE
Answer: E
The Health Care Revenue Cycle 134
53. The _______ is also offcially known as Medicares master patient and
procedural data base.
A. MAC
B. MCE
C. CWF
D. RUG
E. FQHC
Answer: C
54. 02 Condition is Employment Related. This code is for medical services
provided due to the patient being injured while working on the job is a
_____________ found in FL #18 to #28 on the UB-04.
A. Revenue Code
B. TOB Code
C. Value Code
D. Condition Code
E. Occurrence Code
Answer: D
55. 01 Auto Accident (the date the auto accident or mva [motor vehicle accident]
occurred) is a ______________ found in FL #31 to #34 on the UB-04.
A. Revenue Code
B. TOB Code
C. Value Code
D. Condition Code
E. Occurrence Code
Answer: E
56. 01 Most common dollar amount (UCR) for the cost of a semi-private (2 beds
and 2 patients ) room in the hospital is a _______________ found in FL #39 to
#41 on the UB-04.
A. Revenue Code
B. MSP
C. Value Code
D. Condition Code
E. Occurrence Code
Answer: C
57. 250 Pharmacy: a dollar amount indicating the costs of the patient receiving
drugs while an inpatient in the hospital is a ________________ found in FL
#42 to #49 on the UB-04.
A. Revenue Code
B. MSP
C. Value Code
D. Condition Code
E. Occurrence Code
Answer: A
Chapter 3 - Processes and Procedures 135
58. ____________ is for Provider and Patient Information to be placed here in the
UB-04.
A. FL #18 to #28
B. FL #42 to #49
C. FL #66 to #71
D. FL #67A to #67Q
E. FL #1 to #17
Answer: E
59. About three (3) months before a potential benefciary becomes eligible
for coverage by Medicare, an ________ is completed by the patient which
documents other health care insurance coverage they have that may be
PRIMARY to Medicare. This information is entered into the _______.
A. CWF; IEQ
B. IEQ; CWF
C. CWF; ABN
D. MSP; CWF
E. RHC; IEQ
Answer: B
60. _____________ in the UB-04 represents the ADMITTING DIAGNOSIS
(ICD). This is the diagnosis the admitting physician at the hospital initially
determined was the cause of the patients chief complaint (CC) when the
patient frst came to the hospital.
A. FL #1 to #17
B. FL #71
C. FL #69
D. FL #74
E. FL #56
Answer: C
61. IPPS is the acronym for:
A. Inpatient Payment Prospective System
B. Involuntary Prospective Payment System
C. Inpatient Prospective Provider System
D. Inpatient Prospective Payment System
Answer: D
62. HICN is the acronym for ___________ and is issued by ______________:
A. Health Insurance Claim Number; Medicare
B. Healthcare Information Claim Number; Medicare
C. Health Information Classifcation Number; Medicaid
D. Home-Based Insurance Classifcation Number; Medicaid
Answer: A
The Health Care Revenue Cycle 136
63. MS-DRG represents:
A. Medicaid Severity-Diagnosis Related Group
B. Medicare Severity-Diagnosis Related Group
C. Medicare Special-Diagnostic Related Group
D. Medicaid Several-Diagnosis Related Group
Answer: B
64. EOMB stands for:
A. Explanation of Medicaid Benefts
B. Exploration of Medicare Benefts
C. Examination of Medicare Benefts
D. Explanation of Medicare Benefts
Answer: D
65. EGHP represents ____________ and is for employers with ___________
employees.
A. Employee Group Health Plan; 20 or more
B. Employer Group Healthcare Provisions; 25 or more
C. Explanation of Group Health Plan; 30 or more
D. Employer Group Health Plan; 20 or more
Answer: D
End of Chapter 3
Chapter 4 - Claim Form for the Doctors Ofce 137
Chapter 4 Claim Form for the Doctors Ofce
Chapter Topics
Medicare
The CMS-1500 Claim Form
The International Classifcation of Diseases, 9th Revision, Clinical
Modifcation (ICD-9-CM)
Current Procedural Terminology, 4
th
Edition (CPT-4)
Health Care Common Procedure Coding System (HCPCS)
Abbreviations and Acronyms
Sample Test Questions
After studying this chapter you will understand:
Medicare: Timely Filing of Claims; Parts A, B, C and D; Medigap
CMS-1500 Claim Form
Medigap
Medical Unlikely Edits (MUE)
ICD: Diagnosis codes, V and E codes
CPT: Category I, II and III codes
HCPCS: Level I and II codes
Resource Based Relative Value Scale (RBRVS)
Evaluation and Management Services (E/M)
SOAP notes; Problem-Oriented Medical Record (POMR)
National Correct Coding Initiative (NCCI)
Advanced Benefciary Notice (ABN)
Comprehensive Error Rate Testing (CERT)
Recovery Audit Contractors (RAC)
Ambulatory Payment Classifcation (APC)
Clinical Laboratory Improvement Amendment (CLIA)
Medical Necessity
Waiver of Liability
Third Party Reimbursement: Capitation, Fee-for-Service (FFS), Per Diem
Health Insurance Claim Number (HICN or HIC)
Medicaid
Medical Standards of Care; Malpractice
Neoplasms and Cancers
The Health Care Revenue Cycle 138
Medicare
Medicare, of course, has been covered in previous chapters, but because almost every
administrative procedure in the health care industry derives from it, it is always wise
to begin with a short review and further discussion of this very large and infuential
government program. As you know, Medicare benefciaries select from two main
types of coverage plans: traditional fee-for-service (payment per each service,
procedure or supply rendered) or Managed Care.
Timely Filing of Claims (UB-04/CMS-1500) Requirements for Medicare Parts A
and B
1. For Medicare Part B: When medical services are rendered January 1st
through September 30th in one calendar year, the provider or hospital has
until December 31st of the next calendar year to fle a claim to Medicare. For
example, if the services were provided June 30, 2009, the provider or hospital
has until December 31, 2010 to fle the claim.
2. For Medicare Part B: When medical services are rendered October 1st
through December 31st in one calendar year, the provider or hospital
has until December 31st two years later to fle the claim to Medicare. For
example, if the services were provided November 30, 2009, the provider or
hospital has until December 31, 2011 to fle the claim.
3. If these time requirements are not met for Medicare Part B, Medicare will not
pay the claim.
4. Providers of services to Medicare benefciaries cannot charge the patient for
preparing and fling any claim sent to Medicare.
5. Medicare Part A claims must be fled within one (1) year of the date of service
(DOS) or Medicare reimbursement will be reduced by 10%.
Ancillary Services (Important)
1. These are services provided to the patient other than usual and customary
room and board (the bed and food the hospital provides the patient).
2. These ancillary services include:
Operating Room Charges
Anesthesia
Pharmacy and Blood and its Administration
Radiology
Laboratory
Medical and Surgical Supplies
Physical Therapy (PT), Occupational Therapy (OT), Speech Therapy (ST)
Inhalation Therapy (specialized equipment and medication that helps
the patient breath better)
Medicare is available to the following categories of people:
1. Persons who are 65 years or older, retired on Social Security benefts.
2. Spouse of a person paying into the Social Security System with payroll taxes.
Chapter 4 - Claim Form for the Doctors Ofce 139
3. Those who received Social Security disability benefts for 24 months.
4. Those diagnosed with ESRD.
5. Kidney donors to ESRD patients; all expenses related to the kidney
transplantation are covered.
6. Retired Federal employees of the Civil Service Retirement System (CSRS).
Medicare is made up of 4 parts: A, B, C and D
Medicare Part A:
Pays for the following: care in a hospital as an inpatient, CAH, skilled
nursing facilities, hospice care, and home health care. Most people get Part
A automatically at age 65, and do not have to pay premiums because they
or their spouse worked for at least 10 years and paid into Medicare Part A
through their Social Security taxes.
Medicare Part B:
Part B is also known as Supplementary Medical Insurance (SMI). It pays for
doctors services, outpatient care in a hospital setting, PT, OT, ST, diagnostic
services, surgical services, ambulatory surgical care, DME, outpatient
mental health care, laboratory services, blood, ambulance, emergency care,
chiropractic care, orthotics and prosthetics, and home health care. Enrolling
in Part B is optional and requires the patient to pay a separate monthly
premium, which is usually deducted from the consumers monthly social
security check. For 2009, the premium is $96.40. (Note: It can be useful to
know this number.)
Certain Preventative Screening Services are also covered under Medicare
Part B, some of which are:
1. Bone Mass Measurements
2. Pap Smears and Pelvic Examinations
3. Prostate Cancer Screenings (Digital Rectal Examinations [DRE]: one
DRE every 12 months)
4. Vaccinations (One Flu shot per year in the fall or winter; Pneumonia
shot; Hepatitis shot).
What is not covered by Medicare Parts A and B:
1. Acupuncture
2. Dental Care and Dentures
3. Cosmetic Surgery
4. Custodial Care
5. Healthcare received outside the United States
6. Hearing Aids
7. Orthopedic Shoes
The Health Care Revenue Cycle 140
8. Outpatient Prescription Drugs (that would be covered by Medicare
Part D)
9. Routine Foot Care
10. Routine Eye Care and Prescription Glasses
11. Routine Physical Examinations
Medicare Part C: Managed Care Plans (formerly known as Medicare + Choice)
Medicare Part D: Prescription Drug Plan
Medigap
Medigap is a supplemental insurance policy sold by a private insurance carrier
(AARP or Humana, for example) that pays for some of the gaps (unpaid amounts),
in Medicare coverage such as the annual deductibles, co-payments, and co-
insurances the patient would have to normally pay. Medigap works only with the
Original Medicare Plan, Parts A & B (fee-for-service). Patients covered by Medicare
managed care plan (Part C), Part D (drug plan), and Medicaid do not need Medigap policies.
Note: This concept is important for the employee working in the doctors offce or
hospital because the consumer usually does not understand the intricacies between
their Medicare coverage, Medigap, and any other insurances they have!
After a Medicare carrier or FI processes a claim for a patient with Medigap coverage,
the carrier automatically forwards the claim to the Medigap payer, indicating the
amount Medicare approved and paid for the procedures, services and supplies. This
process of Medicare automatically forwarding the processed claim to Medigap is
known as Coordination of Benefts (COB). Once the Medigap carrier adjudicates
the claim, the provider is paid directly, eliminating the need for the practice or
hospital to fle a separate Medigap claim. This is one of the advantages of electronic
submissionnot only does Medicare send the processed claim to Medigap
automatically, but the amount of paperwork is signifcantly reduced and the doctor
and hospital are paid in a much shorter period of time. This is why the CMS-1500
form needs to be properly completed for Medicare and Medigap. The benefciary
receives copies of the Medicare Summary Notices (MSN) that explain the charges
paid and what is due.
Medical Unlikely Edits (MUE)
MUE is where HCPCS and CPT codes are reviewed due to anatomical considerations to
reduce incorrect coding errors. By anatomical, this type of pre-payment review makes
sure the diagnosis codes (ICD) are consistent (linked) with the part of the body being
treated by the doctor. For example, if the ICD code for bunion of the right big toe
is used on the claim form, the MUE process makes sure that it is consistent with the
CPT code for the appropriate surgical procedure (bunionectomy), and that both the
ICD and CPT codes are appropriate for the correct part of the bodythe foot.
Chapter 4 - Claim Form for the Doctors Ofce 141
National Correct Coding Initiative (NCCI or CCI)
The NCCI was established by Medicare to help the physician and hospital code (CPT
and HCPCS) services, procedures and products correctly, reduce wrong coding (such
as unbundling), and eliminate codes that should not be used together under certain
clinical situations (also known as mutually exclusive codes [MEC]). NCCI controls
incorrect coding that would lead to inappropriate payment of Medicare claims.
For the most part, all other insurance companies and third party payers follow
Medicares lead in correcting improper coding and reviewing their claims. The NCCI
checks for improper coding by applying CCI edits, which is a computer program that
electronically scans the claim forms. CCI edits apply to claims that bill and code for
more than one procedure performed on the same Medicare patient, on the same date
of service, by the same provider. Claims are denied when codes reported together do
not pass an edit.
An example of unbundling involves CPT codes for spinal manipulative therapy
(SMT) (98941) a chiropractor would use, and the CPT code for the use of moist heat
or cold (97010). If the doctor manipulates the cervical vertebrae and applies heat to
the neck on the same visit (2 procedures in the same encounter), they would never be
billed and coded separately (unbundled) for the same date of service, because most
third party payers and Medicare normally bundle these two codes under the one
main SMT code (for example, 98941). If the provider does unbundle when billing and
coding, Medicare would apply the NCCI edits and only pay one fee under the one
SMT CPT code (for example, 98941) for both the SMT and heat. If 98941 is billed
at $50.00 and 97010 is billed at $30.00, Medicare would bundle these codes into
98941 and pay the provider only $50.00. If the chiropractor continues to unbundle
these codes and bills them separately encounter after patient encounter, even after
being informed of Medicare bundling these codes on the RA, Medicare would
consider this abuse.
Another case of unbundling involves surgery that is billed as global surgery
or surgical package. Normally all pre-surgical preparation of the patient, the
surgery itself, and all the normal post-surgical and recovery services, are bundled
and paid one fee under the one main CPT surgical code. Therefore, the CPT code
for an oophorectomy (surgical removal of the ovary) is 58940. 58940 pays for
all the services (with one fee to the doctor) associated with this surgical procedure.
This spans the time beginning with the pre-operative evaluation and management
services, to the admission of the patient to the hospital, the surgery, all the post-
surgical recovery, and concluding with the discharge. Under the NCCI, all the
separate CPT codes for the oophorectomy are bundled under one code (58940), and
would not be billed a la carte with many different CPT codes. The doctor, therefore,
is paid one fee for 58940.
Mutually Exclusive Code edits (MEC) apply, for example, when the doctor bills
50021 for an open percutaneous drainage of renal or perirenal abscess. Codes
50020 (open drainage of renal or perirenal abscess) and 49061 (open percutaneous
drainage of retroperitoneal abscess) could not also have been reasonably (clinically)
performed during a single patient encounter or date of service. Therefore, 50020
and 49061 cannot be billed concurrently with 50021. If the provider reports
The Health Care Revenue Cycle 142
both codes to the insurance company on the claim form, either 50021/50020 or
50021/49061, only the 50021 will be paid but at the lower fee of the two reported
CPT codes. This means the medical biller cannot report 49061 or 50020 when
billing 50021. Medicare will reject the claim until the provider corrects the claim
and removes the 50020 or 49061.
If 50021 and 49061 are reported together, for example, Medicare will use MEC
edits and will pay the lower of the two fees. In this case, 50020 is reimbursed
at $1500 and 49061 is reimbursed at $750, Medicare will pay the $750 only. The
provider at this point cannot appeal the payment of $750 retroactively after Medicare
adjudicated the claim, nor can the provider balance bill the patient because the
reduced fee was due to the doctors incorrect coding of the drainage of the kidney
abscess. Medicare considers repeated inappropriate use of these codes as abuse.
The NCCI establishes standards for medical billing, identifes codes that are
prone to fraud and abuse and identifes codes that are susceptible to unbundling
or should not be billed together. NCCI reviews claims before they are paid, known
as pre-payment review, analyzing codes to make sure they comply with NCCI editing
standards particularly to insure that certain pairs of codes are compatible. When
codes are rejected due to NCCI edits, those charges related to those denied codes
cannot be billed to the patient, since Medicare not paying those denied codes is due
to incorrect coding rather than a lack of medical necessity. Therefore, the provider
cannot use the Advanced Benefciary Notice (ABN) for denied services and cannot
collect from the patient. The doctor or hospital would have to correct the coding
errors and re-bill Medicare within 45 days after receiving the Remittance Advice (RA)
from Medicare (remember this from Chapter 3?).
Guidelines for the use of CPT-4 and HCPCS codes, as well as ways to identify
fraud and abuse in the use of these codes, are handled under the NCCI. For further
information see: http://www.cms.hhs.gov/manuals/iom and http://www.cms.hhs.
gov/physicians/cciedits/
Advanced Benefciary Notice (ABN)
The ABN is a signed document which notifes the patient that certain procedures,
products or services Medicare will probably not pay the doctor or service provider
(such as a laboratory) before they are administered. If rejected by Medicare (as all
procedures, products or services must be billed to Medicare whether payment is
expected or not), the ABN makes the patient legally responsible for payment for
all the Medicare denied services. This means the ABN can be used in court to force
the patient to pay his/her debt for medical services. It is imperative the doctor
include diagnoses and conditions (ICD codes) on the ABN along with the anticipated
procedures (CPT codes) that will be conducted, so that Medicare can edit these and
make a determination of medical necessity.
If the provider fails to get a signed ABN prior to services being rendered, and is
denied by Medicare, the patient is not liable to pay for the denied services and the
doctor cannot ask the patient for payment. The Balance Budget Act (BBA) places
limitations on certain laboratory, radiology, and cardiovascular tests provided to
Chapter 4 - Claim Form for the Doctors Ofce 143
Medicare patients. Therefore, it is imperative that prior to services being provided,
an ABN is signed by the patient. If medical necessity and the diagnosis codes and
procedural codes do not satisfy Medicare standards, it is the responsibility of the
service provider, doctor, medical supplier or laboratory to notify the Medicare patient
that these services will be denied and that the patient is therefore responsible for
payment of these denied services.
Comprehensive Error Rate Testing (CERT)
This produces a report showing error rates found on claim forms submitted by
providers and hospitals. It tells Medicare how well the insurance companies and
fscal intermediaries (FI) that adjudicate (process the paperwork) and pay Medicare
services are instructing the hospitals and doctors to code correctly. It also reports
the current number of mistakes being made in coding. Obviously, if the FI has CERT
results that are substantially higher than other comparable third party payers, this
informs Medicare that something is wrong with the insurance carrier regarding how
it handles its claims or how it is instructing its doctors and hospitals and suppliers.
Recovery Audit Contractors (RAC)
The purpose of the RAC is to reduce wrong payments by Medicare to doctors and
hospitals. It does this by detecting and correcting overpayments and underpayments
made by Medicare.
Ambulatory Payment Classifcation (APC)
This is an important and sometimes diffcult concept. The Balanced Budget Act of
1997 (BBA), the Balanced Budget Refnement Act of 1999 (BBRA) and the CMS,
developed a Medicare Outpatient Prospective Payment System (OPPS) and APC.
The OPPS describes a mechanism (paperwork and regulations) in which Medicare
pays its bills. Diseases that are clinically similar (such as diabetes, retinopathy
[disease of the eye] and neuropathy [nerve pain]) are grouped under an Ambulatory
Patient Classifcation system (APC) by Medicare, which is a fee schedule that bundles
all the charges into payment based on the value of treating the diabetes, neuropathy
and retinopathy, for outpatients. Therefore, when the doctor treats diabetes and eye
disease and nerve pain on an outpatient basis, reimbursement to the provider and
hospital is made by Medicare (using the OPPS paperwork and regulations) according
to the preset fees (monies to be paid by Medicare) based on the APC classifcation. In
the case of diabetes, all associated medical treatment is assigned to an APC, which
are fees for the treatment for diabetes, nerve pain and eye disease.
Conversely, for services provided in the hospital for inpatients, an Inpatient
Prospective Payment System (IPPS ) is used instead of the OPPS, and the fee
schedule used is called a DRG (Diagnosis Related Group) instead of an APC. So
if this same patient gets his diabetes, nerve pain and eye disease treated while
admitted to the hospital, the billing department would use the IPPS (paperwork and
regulations) as the way to bill Medicare, and use the DRG to fgure out what they can
charge Medicare for services rendered to the patient. I hope this is clear!
The Health Care Revenue Cycle 144
The DRGs and APCs are used to help control costs. Previously, the use of DRGs
(and APCs beginning in 2000) had services, procedures and products paid on a
much more expensive FFS basis. In other words, a separate fee would be charged
to treat the diabetes, another fee to treat the eye disease, and another fee to treat the
nerve pain, known as unbundling. The FFS fee schedule is more expensive than
using the APC or DRG, which consist of assigning one less expensive bundled fee for
treating everything related to the treatment of the diabetes.
In other words, the APC is a schedule of fees applied using the OPPS mechanism,
so that Medicare can pay for certain medical services provided for patients who are
outpatients. Included in the defnition of outpatient are: (1) outpatient services
provided in a hospital setting, (2) outpatient hospitalization services at community
mental health centers and (3) Medicare Part B services for inpatients at hospitals who
have no Medicare Part A coverage. In the case of this last point (#3), there are patients
who do not have Medicare insurance coverage when they are admitted to a hospital
(Part A), so any medical service or product provided on an outpatient basis while
they are in the hospital would be paid under the APC. For example, if the patient is
in the hospital for repair of a fractured femur (a broken thigh bone), the APC would
be the fee schedule used for outpatient services and products like post-surgical
bandages, wound care, cast maintenance, crutches, physical and occupational
therapy, etc., associated with the healing of the repaired femur. The hospital and
doctor would have to fnd another way to get the actual surgical repair of the
fractured femur paid, probably through public assistance or simply absorb the cost.
All paid services that have clinical similarities are classifed into groups known as
APCs. In other words, each APC represents medical services that are for the same
type of diagnoses, such as all services used in the treatment of diabetes have prices
for these services listed under one APC. There may also be more than one APC
utilized for each patient encounter (the patient may be treated for more than one type
of diagnosis or clinical situation per visit, for example, diabetes and skin cancer). The
APC is for outpatient services that are affliated with the hospital, but not inpatient.
The DRG is similar to the APC in that the DRG is utilized for services affliated with
the hospital but are inpatient. It is important to understand the subtle differences
between the APC and DRG!
1. An APC is determined by utilizing HCPCS/CPT-4 Codes, Evaluation and
Management Codes (E/M), ICD-9-CM codes for reason of the visit (V or E
codes), and Place of Service Codes (POS). When utilizing HCPCS/CPT-4
codes, services in the hospital must be listed by the amount provided (or by
units of service provided). They include the following:
Ambulatory Surgery
Diagnostic Imaging
Radiology
Emergency Department (E/R)
Pharmacy
Clinic
Note: These services are all outpatient hospital services.
Chapter 4 - Claim Form for the Doctors Ofce 145
2. Hospitals and health care facilities that are exempt (not affected) by the
APCs (Outpatient PPS) include:
1. Critical Access Hospitals (CAH)
2. Certain Hospitals in Maryland
3. Cancer Hospitals
4. Indian Health Services Facilities (IHS)
3. Hospitals and health care facilities that are affected by the APCs
(outpatient PPS) include:
1. Acute Care Hospital Outpatient Services (your typical full service
hospital)
2. Hospitals exempt from Inpatient Prospective Payment System (IPPS)
such as psychiatric hospitals, rehabilitation hospitals, childrens
hospitals, LTC hospitals, cancer hospitals, etc.
3. Hospitalization associated with Community Mental Health Centers
Medical Necessity
This is defned as follows:
Health care services that are safe and effective, reasonable
and necessary for the treatment of the illness or injury,
consistent with the diagnosis, generally accepted medical
procedures and services (not experimental), not provided for
the convenience of the patient or doctor, and administered
at the appropriate level of care (no over-utilization or under-
utilization).
A part of medical necessity would presume that medical personnel who treat the
patient are appropriately trained and licensed for the diagnosis and treatment
provided. For example, a periodontist (a dentist who specializes in the treatment of
the gums) must be licensed in the state where the patient is receiving the care. This
would be necessary for the insurance carrier to pay the claim. The third party payer
would also demand that all appropriate documentation (surgical reports, pathology
reports, x-ray and MRI reports, laboratory results, PT and OT reports, medical
supplies and equipment, etc.) be included with the CMS-1500 claim forms, and
proper pre-authorizations and second surgical opinions are secured before payment
is made. It is imperative that the medical coder/biller and front offce personnel be
vigilant and detail oriented so that payment is made in a timely fashion and delays
are minimized.
The Health Care Revenue Cycle 146
Medical Standards of Care and Malpractice
Medical standards of care are state and federal specifc performance measures for the
delivery of health care for medical professionals. This can include doctors, nurses,
therapists, medical suppliers, and anyone else licensed to provide any health care
service or product to the public. Medical malpractice (malpractice = bad practice)
results when the provider or hospital injures the patient, or is responsible for their
death or disability or medical complications, due to failure to follow generally
accepted treatment protocols, neglect, or abandonment of the patient.
Medical malpractice can involve the following:
1. The health care professional or hospital not performing necessary surgical
procedures in a timely manner (for example, waiting too long to perform
cardio-pulmonary resuscitation [CPR] resulting in brain damage).
2. Performing the wrong surgery (for example, amputating the wrong leg).
3. Medically unnecessary delays in treatment (for example, delaying
chemotherapy to shrink a tumor).
4. Administering the wrong treatment for the diagnosis.
5. Prescribing the wrong drugs or the incorrect amounts of drugs.
6. Abandoning the patient.
7. Not responding to the patients medical needs in a timely fashion.
8. Misdiagnosing or failing to diagnose (for example, the doctor completely
missing a cancerous growth).
9. Intentionally or unintentionally harming the patient.
10. Over-treating or under-treating the patient.
11. Assault and battery.
12. Inappropriate contact with the patient, sexual or otherwise.
13. Violating HIPAA, or any other medical or non-medical violations of the
doctor-patient relationship.
Waiver of Liability
This is applicable to all health care providers. It is defned as Medicare patients
who did not know, nor could reasonably be expected to know, that certain medical
services were not covered by Medicare, are protected from the obligation to pay for
health care services. Medicare also considers over-utilization or under-utilization
of care, or custodial care, as medically unnecessary and will deny payment and the
Waiver of Liability will relieve the patient of the responsibility to pay. If Medicare
determines that the patient should have been aware that the service would not be
covered by Medicare, then the patient would be liable to pay for the services that
Medicare denied.
1. The Waiver of Liability rule states that when the patient and/or doctor is frst
notifed that a medical service is not covered by Medicare, this is called the
Notifcation of Non-coverage. When the patient receives the Notifcation of
Chapter 4 - Claim Form for the Doctors Ofce 147
Non-Coverage, but still receives the service, the patient cannot expect Medicare
to pay for the denied services and the patient is liable for payment. Second
and third notices do not remove the patients liability to pay for denied
services, and the patient cannot claim he/she was not aware of the denial
of coverage nor received the frst Notifcation of Non-Coverage. Medicare
encourages the provider and hospital to know the latest regulations and
insurance coverage rules by reading the Medicare Summary Notice (MSN)
and its bulletins.
2. When the Waiver of Liability rule would or would not be applicable include:
When a partial denial is made by the insurance carrier for a particular
medical service because it is determined to be medically unnecessary or
unreasonable (for example, the medical treatment is not consistent with
the diagnosis). A partial denial means that only part of all the services
billed for a diagnosis will not be paid, and an insurance appeal (review)
of the entire claim has not been made, then the Waiver of Liability
applies. For example, when the ophthalmologist performs a complete
eye exam, the doctor can reasonably assume that an eye refraction
would also be paid as an eye refraction is normally a part of a complete
eye exam. If Medicare pays for the entire eye exam, except for the eye
refraction, the Waiver of Liability applies and the patient would not have
to pay for the eye refraction.
The doctor may have also had previous experience with Medicare
that they do pay for complete eye exams including the eye refraction,
and would not have expected that suddenly Medicare would not
pay for part of the complete eye exam, the refraction. At this point,
the ophthamologist could appeal Medicares non-payment of the eye
refraction and attempt to get payment. Whether the doctor gets paid or
not for the eye refraction, the Waiver of Liability protects the patient from
paying for the eye refraction. The doctor may ultimately have to absorb
the cost of the eye refraction because, after all, the patient could not have
reasonably been expected to know that the eye refraction would not have
been reimbursed as part of a complete eye examination.
When a third party payer (insurance carrier or Medicare, for example)
denies coverage of a specifc medical service, such as performing a
fasting blood glucose test (FBG) as part of a complete exam for diabetes,
and the third party payer has clearly excluded the FBG in its health care
insurance contract (policy) with the patient, the Waiver of Liability
does not apply. The provider can still attempt to seek reimbursement
by appealing the claim (asking the insurance carrier to look at the claim
again) to the third party payer. However, if ultimately the doctor cannot
get payment for the FBG from the insurance carrier, the patient would be
liable for payment of the FBG because the FBG is contractually excluded
from payment in the patients insurance policy.
The Health Care Revenue Cycle 148
Clinical Laboratory Improvement Amendment (CLIA)
1. All clinical laboratory services (CBC, UA, liver panel, thyroid, biopsy, FBG,
etc.) that a Medicare patient receives must be performed by a laboratory that
is certifed by one of the following CLIA accrediting bodies and is issued a
certifcate known as a:
Certifcate of Waiver
Certifcate for Provider-Performed Microscopy Procedures
Certifcate of Registration
Certifcate of Compliance
Certifcate of Accreditation
2. All approved laboratory facilities and providers are issued a CLIA number,
which consists of ten letters or numbers with a "D" in the third position of the
CLIA number (for example: 12D3456789). Only New York and Washington
do not require a CLIA number. The CLIA number is placed in block 23 of
the CMS-1500 claim form. Only one CLIA number can be reported per claim form
submitted to Medicare.
3. The CLIA number must be placed in Block #23 in the CMS-1500 claim form
so that the third party payer will issue payment. For further information on
CLIA consult www.cms.hhs.gov/clia/
4. Managed Care Organizations (HMO, PPO, POS) require that their members
use their approved laboratory facilities. The provider, hospital, and patient
should be aware of the approved facilities, and if the patient insists upon
using a non-approved lab, this will result in the MCO patient being
fnancially responsible for all costs. Ultimately, the patient is responsible to
know what facilities and services are approved.
Health Insurance Claim Number (HICN or HIC)
1. Each Medicare benefciary receives a red, white and blue card (see example,
p. 224) listing his/her name, Medicare claim number, sex, and what coverage
exists (Medicare Parts A, B, C or D). This card has the Health Insurance
Claim Number (HICN or HIC) and permits the patient to access health
coverage under the Medicare program. It is important the medical coder see
this card, as well as the Medigap card, and any other insurance identifcation
cards, and copy them and place them in the patients fle for future reference.
2. The HICN is made up of the patients 9 digit numerical social security
number plus a suffx.
Example: 123-45-6789A is the HICN. A is the suffx representing this
benefciary as the wage earner and the person who worked for at least 10
years (40 quarters) and paid into the social security system.
Examples of Suffxes used in the HCIN:
A Wage Earner, 65 years or older
B Wife (spouse), 65 years or older
Chapter 4 - Claim Form for the Doctors Ofce 149
C Child
D Widow
HAD Disabled Adult
M Part B benefts only
T Uninsured and entitled only to health insurance benefts
F5 Adopting Father
W Disabled Widow
Medicaid (MCD)
Medicaid (MCD) is state-federal partnership that provides monetary assistance, food
stamps, health care, and other types of assistance to those who are low income.
Medicaid is the payer of last resort, meaning that all other health insurance
plans pay frst, including Medicare, before Medicaid will pay. In some
instances, the patient may have both Medicare and Medicaid coverage,
known as Dual Eligibility, where Medicaid pays for some of Medicares
premiums, deductibles, co-payments and co-insurance.
Resource Based Relative Value Scale (RBRVS)
1. This was made into law by the Omnibus Reconciliation Act of 1989 (OBRA-
89) and changed the way doctors and hospitals were paid. The RBRVS
contains three features:
Fee schedule for paying doctor's services
A schedule that determines the rate of increase for doctor's services
known as the Medicare Volume Performance Standard (MVPS). This
indicates how much the price of certain health care services and products
are increased each year. For example, the MVPS is 10%. The payment is
$10.00 for 2008, therefore the MVPS would increase the $10.00 by 10% so
the new price for 2009 would be $10.00, plus the $1.00 increase = $11.00
for 2009.
What physicians can charge for their services who do not participate in
Medicare is known as the Limiting Charge. The limiting charge is 115%
of the Medicare fee schedule. The limiting charge used to be known as the
MAAC.
2. The Relative Value Unit (RVU) is the BASIS (or heart) of the Medicare
fee schedule
The RVU is made up of three (3) components that determine what Medicare
will pay the doctor for providing services to the patient and include:
The amount of work required to perform the medical service (for
example, effort the doctor has to provide to do the surgery).
What it costs the doctor to perform the medical service (overhead).
What it costs the doctor in malpractice insurance premiums to practice
his specialty. More highly complex surgery like brain neurosurgery is not
The Health Care Revenue Cycle 150
only far more complicated and takes many hours to perform, but is far
more risky and the patient has a higher chance of death, complications
or disability. It will therefore cost the neurosurgeon much more in
malpractice premiums. Compared to less complex surgery such as a
bunionectomy performed by a podiatrist, which costs much less in
malpractice premiums, these expenses are refected in the RVU.
Medicare Participation by the Doctor
Advantages
Higher payments to the doctor from the Medicare fee schedule (in
some cases, the doctor is paid more by Medicare than what they would
normally charge a non-Medicare patient)
RBRVS payments are 5% higher than the Medicare fee schedule
Less collection effort required since Medicare is a reliable payer
Medicare pays 80% of the fee schedule directly to the provider or
hospital. The other 20% is paid through co-insurances and co-payments
directly to the provider or hospital.
Medicare advertises to the public the doctor is participating, potentially
increasing the pool of patients available to the doctor.
Easier for the doctor to collect deductibles, co-payments and co-
insurances directly from the patient.
Disadvantages
Doctor is limited to how much money can be charged the Medicare
patient
Doctor can only collect up to what the Medicare fee schedule allows
Medicare Non-Participation by the Doctor
Advantages
Revenue collections are increased for the doctor (Doctor gets paid
directly from the patient and does not have to wait for Medicare to pay).
Doctor can collect up to 115% of the Medicare fee schedule.
Doctor can choose to participate or not to participate for each patient;
fexibility for the doctor.
Medicare patients must be charged the exact same fees for the same
services as any other patient.
Disadvantages
May cost the doctor more to collect fees by having to chase the patient
for payment.
Doctor's fees must be collected entirely from the patient; doctor therefore
may lose some patients who do not want to pay cash.
Doctor must still submit claims to Medicare even if the patient pays the
provider directly; patient gets reimbursed through Medicare
Chapter 4 - Claim Form for the Doctors Ofce 151
The CMS-1500 Claim Form
(see p. 221)
1. The CMS-1500 claim form is generally used by the doctor, DME company,
laboratory, PT, OT, ST, orthotics and prosthetics, and other outpatient
services to bill the insurance carrier or Medicare. Although electronic
submission is the preferred method of submission, paper claims are still
acceptable in some instances. Ambulance companies are still required to use
the CMS-1491 claim form.
2. The CMS-1500 claim form is printed in red drop out ink so that it can be
read optically by computer such as image processing technology known as
image character recognition (ICR). This kind of electronic processing allows
easier facsimile transmission (fax) and image storage by Medicare and other
third party payers. Photocopies of the CMS-1500 will not be accepted for
processing by any third party payer.
3. Medicare will not accept non-standard claim forms, such as superbills, face
sheets, or encounter forms or other extraneous documentation in place of
the CMS-1500. However, other third-party payers may accept the superbill
in place of the CMS-1500. Documentation that is necessary for processing
the CMS-1500, such as medical records, certifcates of medical necessity,
certifcations required by law, surgical reports and second opinions, lab
reports, diagnostic imaging studies, etc., will be accepted in addition to the
CMS-1500 form.
4. For the CMS-1500 to generate payment, it must be submitted clean, that
means complete and valid. All required or mandatory felds or blocks must be
flled out complete and valid, and those felds that are known as conditional
must be completed for specifc situations depending on each case. A good
example of conditional felds that need to be completed would be blocks
#1a, 4, 7, 11a-d, where the insured (or guarantor) is different than the patient.
Therefore these blocks in this particular case would need to be completed so
the claim would be considered valid and complete and therefore clean, and
would be paid.
5. Completion of the CMS-1500 Claim Form (related to Medicare) is discussed
block by block and listed whether each block must be flled out for every
patient (required) or may be flled out depending if certain situations exist
(conditional). Blocks that are considered optional are suggested by Medicare
to be completed for statistical analysis. The right upper margin of the claim
form should not be used at all by the medical coder, doctor or hospital, and
should be left blank.
6. Blocks #1 to #13 are flled out with data related to the patient. Blocks #14 to
#33 are flled out with data related to the health care provider. Important!
The Health Care Revenue Cycle 152
How to Complete the CMS-1500 Claim Form
Note: Some information is specifc for Medicare claims only.
CMS-1500 Block or Field
#1: This is where the type of health care insurance carrier is placed (Medicare,
Blue Cross/Blue Shield, TRICARE, etc.) and is REQUIRED.
#1a: This is where the HICN is placed, and whether Medicare is the primary or
secondary payer. This is REQUIRED.
#2: Enter the Patients Name (last name [including Jr., Sr., II, III, etc], frst name
and middle initial). However, leave out titles and degrees (such as MD, PhD,
Esq., Sister, Captain, etc.) This is REQUIRED. Example: Smith Jr. Stanley A.
or Hancock III, Frederick H.
#3: Enter the Patients Birth date in MM/DD/YY format only and sex (M or
F). This is REQUIRED. Example: 11/10/49.
#4: Enter the Insureds Name here. When insured and patient are the same, enter
SAME in this block. If there is no insurance primary to Medicare, leave
blank. This is CONDITIONAL.
#5: Enter the Patients Mailing Address and telephone number. If there is no
telephone number, enter 000-000-0000. This is REQUIRED
#6: Patients relationship to the person who has the insurance, such as self,
spouse or child, is the information entered in this block. Filling out this block
is CONDITIONAL and dependent on whose insurance plan it is and who is
receiving treatment under this insurance plan.
#7: Insureds address and telephone number is entered in this block. When the
insureds address is the same as the one who is receiving treatment, write
SAME. Filling out this block is CONDITIONAL when blocks #4 and #11
are completed.
#8: The status of the patient: married or single, employed, or a student, is placed
here. This information is REQUIRED and used to determine COB eligibility
(helps the insurance carriers determine who pays frst, second, third, etc.)
#9, 9a, 9b, 9c, 9d: Other insureds name, insurance policy number, DOB, sex,
employer or school name, name of insurance carrier is placed in blocks #9A,
#9B, #9C and #9D. This data is CONDITIONAL depending on whether there is
Medigap insurance.
Block #9: Other insureds Last Name, First Name and Middle Initial are
placed here.
Chapter 4 - Claim Form for the Doctors Ofce 153
Block #9a: Other insureds insurance policy or group number. This is where
information for Medigap is placed.
Block #9b: Other insureds date of birth in MM/DD/YY format and sex.
Block #9c: DO NOT enter the Employers name or School name (of Other
Insureds) and instead put in this block the address of where the
Medigap claims are adjudicated by the carrier.
Block #9d: Enter the name of the insurance carrier that is providing the
Medigap insurance.
#10, 10a, 10b, 10c: Patients condition (how the patient was injured or developed an
illness or disease) related to employment, auto accident or other accident is
placed here. This information is REQUIRED.
#10d: Medicaid (MCD) number of the patient is placed in this block.
CONDITIONAL if the patient has Medicaid.
#11, 11a, 11b, 11c, 11d: If there is no insurance primary to Medicare, enter NONE in
#11, ignore 11a, b, c and go to block #12.
Block #11: This feld is REQUIRED if there is insurance PRIMARY to
Medicare. Put in Medigaps insurance number (or other insurance
carrier) here if applicable. When there is insurance primary to Medicare,
it is REQUIRED to fll out 11a, b, and c. If there is no insurance PRIMARY
to Medicare, put NONE in #11.
Block#11a: Put in Insureds (Medigap or other insurance carrier) DOB (MM/
DD/YY) and sex. CONDITIONAL.
Block#11b: Put the name of the insureds employer (or date of retirement
[MM/DD/YY]) or the name of the school where the insured is enrolled.
CONDITIONAL.
Block#11c: Put in the name of the insurance carrier that provides Medigap,
or other insurance carrier that is primary to Medicare. CONDITIONAL.
Block#11d: Leave BLANK, not required by Medicare. If Medicare is not
involved in this claim, check YES or NO.
#12: Patients or Authorized Persons Signature (guarantor or guardian if child)
plus date (MM/DD/YY) is entered in this feld. The purpose of this block is
to give permission for the doctor or hospital to release the patients protected
health information (PHI) that is on the claim form to the insurance carrier or
Medicare so that it can be processed and payment can be made. Signature
The Health Care Revenue Cycle 154
on File (SOF) may be placed in the signed line instead of the patients
actual signature. Many times the SOF authorization is created by the patient
signing a separate piece of paper legally authorizing the doctor or hospital
to release the patients PHI as needed for as many CMS-1500 or UB-04 claim
forms as is necessary. This SOF authorization is effective indefnitely unless
revoked by the patient. The completion of Block #12 is REQUIRED.
#13: Insureds or Authorized Persons Signature is placed in this block. This
is also known as the Assignment of Benefts. This block must be flled
out so the insurance carrier pays the doctor or hospital directly. An SOF
authorization, just like that done in Block #12 above, can be used instead of
the patients actual signature. Completion of this block is REQUIRED.
#14: Date of current illness, injury or pregnancy (MM/DD/YY) is put in this
block. More specifcally, the frst date when the illness or injury began, or the
pregnancy began, is the date that must be entered here and is REQUIRED.
For chiropractic services, the frst date when treatment began is the date put
in this block and is REQUIRED. In addition, when treatment is chiropractic
care, the date when x-rays were taken (for the parts of the spine treated), in
MM/DD/YY format, is placed in feld #19 as well.
#15: If the patient has had the same or similar illness as the one being coded and
billed on the current CMS-1500 form, that date (MM/DD/YY) is normally
put in this block. However, for Medicare claims this feld would be left blank.
Therefore, for all insurance claims other than Medicare, this block should be
flled out, but it is OPTIONAL.
#16: The dates (from: MM/DD/YY; to: MM/DD/YY)) the employed patient
is unable to work is put in here. Used for disability insurance information
purposes and is CONDITIONAL.
#17: Name of Referring Physician, if there is one, who sent the patient or ordered
a service (such as laboratory or medical supplier), is placed in this block.
Completion of this block is CONDITIONAL. Referring Physician means
an MD, DO, DDS, DMD, DPM, OD, or DC who refers the patient to another
doctor in the hospital for more specialized services. An Ordering Physician
prescribes non-physician services such as PT/OT/ST therapy, laboratory
(CLIA) services, or durable medical equipment (DME) such as a neck or back
brace, wheelchair, etc.
#17a: An identifying number (other than NPI) of the referring or ordering
physician is placed in this block. Filling out this block is CONDITIONAL on
whether there is a referring or ordering physician.
Chapter 4 - Claim Form for the Doctors Ofce 155
#17b: The NPI (HIPAA National Provider Identifer Number) is placed in this
block, CONDITIONAL on whether there is a referring or ordering physician
for a service or product.
#18: This feld holds the dates the patient was in the hospital (from: MM/DD/YY;
to: MM/DD/YY) and is CONDITIONAL on the patient being hospitalized.
#19: This feld is known as Reserved for Local Use. This includes chiropractic
care, and other Not Otherwise Classifed (NOC) codes such as: unlisted
drug codes, unlisted procedure codes, CPT modifer -99 code, hearing
aid, homebound status of the patient, dental, hospice, and information
related to respiratory (lung) measurements, etc. Filling out this block is
CONDITIONAL if any of these situations are pertinent for this patient.
#20: This block is flled out when an Outside Laboratory is used (also known as
purchased diagnostic services). Fill in this block by checking YES for Outside
Lab?, and the price the doctor paid for buying the services of a laboratory
outside of the doctors offce. For example, when the doctor sends the patient
to an outside lab whose staff takes the blood and urine samples (technical
portion), and the doctor at the lab interprets the results (professional
component), and a dollar amount is reported, this would constitute the
CONDITIONAL situation when Block #20 would need to be completed. This
dollar amount tells the insurance carrier or Medicare that this is the price
the referring doctor paid to a laboratory, outside of his offce, to perform
requested laboratory tests.
#21: This is where up to four ICD-9-CM diagnosis codes are placed in order of
severity; coded to the HIGHEST LEVEL OF SPECIFICITY. This must be flled
out for every claim and is REQUIRED!
#22: Medicaid re-submission. When a Medicaid claim is sent again to the carrier
for re-consideration for payment. NOT REQUIRED BY MEDICARE.
OPTIONAL.
#23: Prior Authorization Number. Enter the Prior Authorization Number,
assigned by the Professional Review Organization (PRO) of an MCO, that
is given to the health care provider before a medical service is rendered to
the patient. This number tells the MCO that the service was pre-approved
and it can now be paid upon submission of the CMS-1500. This block is also
where the CLIA number is placed for outside lab services. Completing this
feld is CONDITIONAL on whether the insurance carrier requires a Prior
Authorization Number or an outside lab was used. Only one CLIA number
can be used per claim and only for paper claims.
The Health Care Revenue Cycle 156
#24A, B, C, D, E, F, G, H, I , J. Successfully completing this block is very important
Block #24A: Dates when health care services were provided (from:
MM/DD/YY; to: MM/DD/YY) and is REQUIRED information for every
claim.
Block #24B: Where the service was provided (POS-Place of Service) and is
REQUIRED information for every claim. Is it important to know these POS
codes! The POS codes are located on the frst page of the CPT-4 coding manual.
POS CODES:
11 Offce
21 Inpatient in the hospital
22 Outpatient services provided in hospital setting
23 Emergency Room in a hospital
24 Ambulatory Surgical Center (ASC) that may be affliated with a
hospital or is a free-standing facility
31 Skilled Nursing Facility (SNF)
Block #24C: EMG. This block is completed if the medical treatment is
emergency related. CONDITIONAL, dependent on insurance or
governmental requirements.
Block #24D: Codes for Medical Procedures, Services, or Supplies are entered
here. This is where the HCPCS and CPT codes are placed and are
REQUIRED for all claims submissions.
Block #24E: Diagnosis Pointer. This is where the ICD diagnoses are matched
(linked) to the HCPCS/CPT procedural codes. For example, in Block
#21 if the diagnosis was listed under #1 as appendicitis, and in Block
#24D on line #1 the medical service was an appendectomy, then in
Block #24E (on line #1) appendicitis would be linked to appendectomy
with the number 1. In other words, the diagnosis and medical surgical
procedure would be clinically connected (making sense to the insurance
carrier), and the claim then could be successfully processed and payment
would be made. REQUIRED.
Block #24F: Charges. This is where the actual dollar amounts (for example:
$1500.00 for the appendectomy) are placed for the medical services
rendered to the patient by the surgeon. REQUIRED.
Block #24G: Days or Units. Place in this block the numbers of services
provided, minutes of anesthesia administered, amount of medication
provided, numbers of medical supplies given to the patient, etc.
REQUIRED for every claim.
Chapter 4 - Claim Form for the Doctors Ofce 157
Block #24H: EPSDT Family Planning. For early and periodic screening
of certain medical conditions (for example, mammograms for breast
cancer [CA] or prostate PSA testing for prostatic cancer [CA]), diagnoses
(cancer), and treatment related medical services. Family Planning
(birth control) would also be listed here. Completion of this block is not
required by Medicare. Filling out this feld is OPTIONAL. PSA=PROSTATE
SPECIFIC ANTIGEN
Block #24I: ID (identifcation) Qualifer. An additional identifcation number
(non-NPI) for the doctor is placed here if the doctor does not have an
NPI number. CONDITIONAL.
Block #24J: Rendering Provider ID number. The number of the doctor, CLIA
laboratory, medical supplier or therapist who actually administered the
service or product to the patient is entered in this block. Completion of
this block is REQUIRED for every claim.
Block #25: Federal Tax Identifcation Number, Employer Identifcation
Number (EIN), or Social Security Number (SSN) is placed here for the
doctor or supplier of health care services or products. If Medigap was
reported, flling out this block is CONDITIONAL for Medicare claims.
Block #26: Patients Account Number, assigned by the doctors offce or
laboratory or medical suppliers accounting system, is used to help the
provider keep track of the patient and is not related to Medicare or the
insurance carrier. CONDITIONAL on whether any number is assigned
by the provider of medical services.
Block #27: Accepts Assignment. Check this block YES or NO to indicate
whether the doctor accepts assignment of Medicare benefts (takes what
Medicare will pay according to the fee schedule), will bill Medicare
directly, and will wait for payment from Medicare. REQUIRED for all
Medigap and Medicare participating providers.
Block #28: Total Charge. Add up all the individual charges listed in 24F and
place that number in this block. REQUIRED for all claims.
Block #29: Amount Paid. This block refects the total amount of money
the patient paid for services that are covered by Medicare or other
insurances. This number represents the co-payments or co-insurances
the patient is contractually required to pay according to their health care
policy. REQUIRED for all claims.
Block #30: Balance Due. This number refects how much remains to be
paid on the claim. It is calculated by taking the total charges (#28)
The Health Care Revenue Cycle 158
and subtracting what the patient paid (#29). NOT REQUIRED FOR
MEDICARE. It is OPTIONAL for all other insurances.
Block #31: This block is for the signature of the provider or supplier, plus
academic degrees or credentials, and date signed (MM/DD/YY). For
example: John Smith, MD. REQUIRED for all claims.
Block #32: Name of the physical location where the actual medical services
were provided (Main Street Podiatry Services, 1234 Walnut Street, Phila.,
PA 19111). No Post Offce addresses allowed. This applies to all providers
(hospitals, laboratories, clinics, doctors offce). If the location where
the actual services were administered to the patient is also the billing
address, the word SAME would go into block #32. REQUIRED of all
claims.
Block #32a: Put the National Provider Identifcation (NPI) number of the
provider in this feld. CONDITIONAL if there is an NPI. If the provider
does not have an NPI, see block #32b below.
Block #32b: Other identifcation numbers go into this block. CONDITIONAL
for the provider with a non-NPI number. The non-NPI number goes into
this block, plus two more digits (listed in a special chart) are added to
the non-NPI number as a prefx. All this sounds very confusing, but these
numbers would be provided by the doctor or hospital and you would be aware
what to do with them.
Block #33: The physical location where the claim form is being billed from,
where the insurance check is to be mailed to, and where the insurance
carrier should make contact with the provider or facility for any
additional information related to the claim. No Post Box Offce numbers.
When block #32 is the same as block #33, enter SAME in block #32.
This is REQUIRED of all claims.
Block #33a: The providers NPI is placed in this block (just like #32a).
CONDITIONAL.
Block #33b: Other identifcation numbers go into this block (just like #33a).
CONDITIONAL
Important
Rejected claims that are incomplete or invalid must be corrected and re-
submitted to Medicare. The provider or supplier or hospital cannot bill the
Medicare benefciary (patient) for rejected claims, attempting to collect
monies owed, due to the fact the insurance company or Medicare is denying
the claim because of an incorrectly prepared CMS-1500 claim.
Chapter 4 - Claim Form for the Doctors Ofce 159
Physicians or suppliers that do not accept Medicare assignment can request
payment in full from the patient when services are rendered to the patient.
Medicare requires that even though the provider does not participate with
Medicare, the provider can still submit claims to Medicare so the patient can
be reimbursed, avoiding a fnancial hardship.
Additional information concerning completion of the CMS-1500 claim form
can be accessed at: http://www.nucc.org/images/stories/PDF/claim_
form_manual_v3-0_7-07.pdf
Important Provider Identifcation Numbers for completion of the CMS-1500.
Other than the NPI, the doctor, supplier, group practice (a collection of doctors),
or hospital are assigned other numbers by the insurance carrier or Medicare. They
include:
1. UPIN: Unique Provider Identifying Number is the number assigned to each
doctor providing services to Medicare patients.
2. PPIN: Performing Provider Identifcation Number is a special number
assigned to each doctor in a group of doctors practicing together (group
practice).
3. PIN: Provider Identifcation Number is the number an insurance company
assigns to each participating doctor.
Review of important terms that are related to the processing of the insurance claim
and the patients Protected Health Information (PHI):
1. MSP: Medicare as the secondary payer. This is where another insurance
carrier is the frst one to pay the claim before Medicare. This is determined
through COB (coordination of benefts) where the insurance carriers and
Medicare determine who pays the claim frst, second, third, etc. It is the
doctor or hospital or suppliers responsibility to determine if Medicare is
primary or secondary payer before submitting the claim forms!
2. Bundled Services: This is where multiple medical services are coded with
one CPT code, and billed and paid with one fee, aka Global Surgical Fee
or Surgical Package. The one CPT code covers uncomplicated (normal,
no infections or complications) pre-operative, surgical, and post-operative
services for the diagnosis, regardless of the amount of procedures or services
rendered. For example, there would be one CPT code, one charge, and one
payment for all the services the doctor and hospital provides the patient for
an appendectomy for the diagnosis of appendicitis.
3. Unbundled Services: This is where multiple medical services are CPT coded,
billed and paid separately, a la carte. An insurance carrier may choose not
to pay for unbundled services and may bundle them for payment purposes.
4. Release of the PHI Under Court Order happens if required to be used
as evidence by a court of law. The provider may release the PHI without
the patients written approval if a judicial order is served upon the doctor or
hospital. If the court issues a subpoena, this is a court order demanding
The Health Care Revenue Cycle 160
the doctor or a member of the medical staff to appear in person and testify.
Usually in this case the doctor will bring all the necessary paperwork and
records to court to help their testimony. If the court requires the witness
to bring specifc evidence, such as a patients medical record, it issues a
subpoena duces tecum, which demands the doctor or member of the staff to
appear, testify, and to bring the requested documentation. Testify means
the doctor is ordered to speak the truth publicly in court about a specifc
matter or patient.
5. The HIPAA Security Rule requires covered entities (doctors, hospitals, SNFs,
governmental bodies, public health clinics, etc.) to establish and enforce
safeguards to protect the patients Protected Health Information (PHI). The
security rule delineates how to secure and protect the PHI on computer
networks, the Internet, storage discs (CDs), paper fles, anywhere in the
doctors offce, hospital, SNF, insurance company, any health care facility,
third party payer, clearinghouse, in transit, etc.
6. The Security Rule includes:
Encryption. The process of coding information in such a way that only
authorized individuals on a computer with the password and username
can decipher the PHI.
Access Control. Limits who can handle the PHI and a record of who
has seen what information when is preserved. The doctor should have
complete access to the PHI, however, the secretary or medical biller may
only need permission to see certain parts of the PHI.
Back-up protocols. Critical so that lost or damaged PHI can be quickly
replaced. Hopefully, back-up will be off-site away from the doctors
offce or hospital.
International Classifcation of Diseases, 9th
Revision, Clinical Modifcations
Also known as the ICD-9-CM, the International Classifcation of Diseases, 9th Revision,
Clinical Modifcations, was developed by the World Health Organization (WHO). It is
utilized by hospitals, providers, medical suppliers, and any other health care delivery
system in the United States to report to third party payers such as health care
insurance companies, Medicare and fscal intermediaries, the patients diagnoses,
conditions, symptoms, complaints, problems, injuries, trauma, medical histories,
screenings or clinical situations. The ICD is used all over the worldin Europe,
Canada, Japan, Australia, etc.
The ICD is updated every year to refect new disease processes, new technologies, greater
specifcity in coding, and codes that are expanded, changed, added or deleted. The
National Center for Health Statistics and CMS publish these changes to the ICD every
fscal year beginning October 1, with implementation of these changes by January 1 of the
following year (for example, changes made on October 1, 2009 must be utilized by health
care providers and hospitals no later than January 1, 2010).
Chapter 4 - Claim Form for the Doctors Ofce 161
1. Diagnoses, conditions, pathologies, symptoms, complaints, problems,
medical histories or injuries are reported in codes consisting of numbers
and/or letters the patient is experiencing, as determined by the health
care provider. The CMS provides guidelines on how to properly apply
standardized coding practices to the UB-04 and CMS-1500 throughout the
United States. In other words, how to correctly place all the CPT and ICD
codes on these forms. See Chapter 3 for appropriate placement of ICD codes
in the UB-04 form for hospital inpatients and outpatients. The CMS-1500 is
generally utilized for coding non-hospital outpatient treatment, OT/PT/ST,
prosthetics, orthotics, and durable medical goods (DME) where ICD codes
are placed in block 21. See examples of the UB-04 and CMS-1500 on pages
221 of this study guide. (For further information concerning the ICD, see
www.ama.org)!
2. It is imperative the medical coder provide complete, valid, and precise ICD
codes so that every pertinent aspect of the patients diagnostic condition
and medical situation are captured in the UB-04 and CMS-1500 on page 221.
By properly coding with the ICD and CPT/HCPCS manuals, the hospital
or provider can get fully reimbursed for every service or product provided.
Figure 8: ICD
The Health Care Revenue Cycle 162
When coding is complete and valid, linkage is accomplished. Linkage
is when procedures such as surgeries, examinations, administration of
therapies and drugs and medical supplies are consistent with the diagnosis and
medical situation the patient is experiencing, and may be experiencing on an acute or
chronic basis.
3. Accurate and appropriate coding will maximize the hospitals and doctors
cash fow, improve the fnancial bottom line, reduce insurance denials,
reduce lost charges for medical services billed, reduce lost revenues,
and reduce the accounts receivable (A/R). A/R represents all the money
outstanding that is owed to the hospital or doctor by the patient and/
or insurance carrier or FI. Medicares National Coverage Determinations
(NCD) and/or Local Medical Review Policies (LMRPs) are instrumental
in providing coding initiatives and coverage criteria to the hospital and
provider.
4. Therapies can include physical therapy (PT), occupational therapy (OT),
speech therapy (ST), cardiac and respiratory rehabilitation, radiation therapy
and chemotherapy, nursing care, orthotist (who fts neck and back braces, for
example), prosthetist (who fts artifcial legs and breasts, for example), and
other types of treatment administered by a physician, therapist, nurse, or
other licensed health care provider. The ICD codes would be for diagnoses
and conditions, the CPT or HCPCS codes would be for the actual services
these health care providers would administer. The HCPCS manual would
also code for medical supplies and ambulance services these health care
providers would prescribe for the patient.
5. The ICD coding manual consists of a Table of Contents, Introduction, then
three volumes and the appendices. However, Volume 3 is reserved for
procedures, hospitals, and special uses. Volumes 1 and 2 are primarily for
the medical coder for assigning ICD codes. After volumes 1 and 2 are the
Offcial ICD-9-CM Government Appendices A through E.
6. APPENDIX A is known as the Morphology of Neoplasms, which are special
ICD codes that begin with the letter M followed by 4 numbers, a slash
and another number, for example M8640/1. This number is used solely
by pathologists, who are medical doctors that specialize at looking at tissue
samples under the microscope, to determine whether the tissue sample is
cancerous, neoplastic, malignant or benign.
7. Volume 2 is positioned frst in the ICD book, known as the Alphabetic
Index, and lists every diagnosis, symptom, condition, complaint, pathology
or problem, alphabetically (A to Z). V and E Codes are also listed in
Volume 2. However, the actual sections where V and E codes are positioned is at
the end of Volume 1, the Tabular List. Volume 2 matches the actual words of the
diagnosis to an ICD number, this number is then found in Volume 1 by the
coder, and the ICD code can then be expanded upon further and verifed to
the highest level of specifcity.
8. The Highest Level of Specifcity means that ICD codes have been
established to the greatest degree of defnition and accuracy. Optimally, the
ICD code should be coded up to 5 numbers, for example 123.45, and are
Chapter 4 - Claim Form for the Doctors Ofce 163
found in the ICD coding manual for each diagnosis the patient is determined
to have by the health care provider. Sometimes the highest level of specifcity may
have only 4 numbers, such as 123.4, and rarely only 3 digits, such as 123. The
following represents three ways the ICD codes are presented:
123 = This ICD number is coded to the category level (3 numbers)
123.4 = This ICD number is coded to the sub-category level (4 numbers).
123.45 = This ICD number is coded to the sub-classifcation level (5
numbers). This ICD number is considered coded to the Highest Level of
Specifcity.
9. Also in Volume 2, when the coder proceeds alphabetically to the letter N,
the Table of Neoplasms is found, which lists all cancers and neoplasms by
Anatomical Body Location according to six (6) categories of malignancies
and non-malignancies.
10. These six categories include:
Three listings for Malignant Cancers. Malignant cancers are aggressive,
rapidly growing, can invade other tissues, and can be lethal.
1 Primary Malignancy. The original malignant cancer site, for
example, prostate.
2 Secondary Malignancy. This is a cancer that has spread from the
primary malignancys original cancer site, for example the prostate,
to a second location, the lumbar spine. When a cancer has spread, it
is known to have metastasized.
3 Carcinoma In Situ. This is a malignant cancer that never moves to
other parts of the body. In other words, the cancer stays in place [in
situ]. It is stationary.
Three listings for Non-Malignant Cancers. These cancers are not aggressive.
They are slow growing, rarely invade other tissues, and are generally not
lethal.
1 Benign (Think of early skin cancers like basal cell carcinoma or
squamous cell carcinoma, generally as a result of too much sun
exposure)
2 Uncertain Behavior (The pathologist cannot determine if it is benign
or malignant cancer; aka-borderline malignancy)
3 Unspecifed Nature (The pathologist determines it is a growth of
cells [neoplasm], but cannot determine if it abnormal, cancerous or
not)
11. Volume 1 is positioned second in the ICD manual, and is known as the
Tabular List. The Tabular List has the exact same ICD numbers as found
in Volume 2, but presented in numerical order, corresponding to every
diagnosis, pathology or problem the coder found frst in Volume 2. These
The Health Care Revenue Cycle 164
ICD codes in both Volumes 1 and 2 can be up to 5 numbers (e.g.-123.45) in
length.
12. ICD codes in Volumes 1 and 2 begin with the number 001 and go up to
999.9. The Tabular List consists of 17 Chapters (for example, numbers
running from 100 to 150), with each chapter broken up into Sections (for
example, 100 to 110), each Section broken up into Categories (for example,
103), each category subdivided into Sub-categories (for example, 103.4), and
each sub-category is fnally subdivided into Sub-classifcations (for example,
103.45). The sub-classifcation code of the ICD, for example: 103.45, is coded
to the Highest Level of Specifcity.
13. The last portion of Volume 1, Tabular List, are sections for V codes and E
codes. The V codes are all alphanumeric, running from V01 through V89.09,
with all codes beginning with the letter V plus up to 4 numbers.
V CODES include medical services or health care situations other than
disease or pathologies such as the following:
1 Vaccinations (Flu, Hepatitis or Small Pox)
2 Tissue Transplantation (Kidney, Bone or Skin)
3 Medical screenings for diseases or conditions (HIV, Mammography,
Prostate, Scoliosis, Meningitis or Hepatitis)
4 Medical History (woman with a history having caesarian births,
exposure to poisons or black lung disease, family history of cancer)
5 Psychological Counseling
6 Use of Medical Devices, Orthotics, Prosthetics
7 Kidney dialysis
E CODES follow the V codes at the end of the Tabular List (Volume 1) in
the ICD manual. E codes are all alphanumeric and begin with the letter E
followed by up to four digits and range from E800 to E999.1.
E codes document EXTERNAL causes of disease, injury or trauma such as:
1 Automobile, bus, truck, subway, train, motorcycle, bicycle accidents,
etc., involving driver, passenger, and pedestrians
2 Boats, wave runners, waterskiing accidents, etc.
3 Sports related accidents such as skiing, football, swimming, etc.
4 Terrorism related injuries
5 Poisoning
6 Aircraft and spacecraft accidents
7 Work related injuries
14. Sequencing the ICD Codes on the UB-04 and CMS -1500 Claim Forms
includes the following:
The ICD Code representing the most severe diagnosis, pathology or injury is
placed frst in the coding form (primary or principal), followed by the next
most severe which is secondary, followed by the third diagnosis (tertiary),
Chapter 4 - Claim Form for the Doctors Ofce 165
and so on. Co-existing medical conditions are also ICD coded in this way,
as long as they have a direct clinical signifcance on the Primary Diagnosis.
Do not code diagnoses that are probable, suspected, questionable, no longer
applicable (cured or resolved), or ones that have been ruled out by the
physician prior to the Primary Diagnosis being established.
In surgical cases, when the pre-operative diagnosis (aka working or qualifed
diagnosis) is different than the post-operative diagnosis, code the post-
operative diagnosis only on the UB-04 as the actual diagnosis. For example,
if the patient enters the emergency room with subjective signs and symptoms
of chest pain, nausea and left arm pain, the pre-operative diagnosis would
tentatively be myocardial infarction (heart attack!). Once the patient
was admitted to the hospital, a thorough examination conducted, cardiac
catheterization was performed, laboratory tests (EKG) were run, the primary
diagnosis would be changed to dyspepsia (indigestion). Both diagnoses
have very similar signs and symptoms. The post-operative diagnosis of
dyspepsia is the one that is coded on the UB-04.
The doctors may even document several working diagnoses in the course
of the patients hospitalization such as myocardial infarction, dyspepsia,
ventricular fbrillation, etc., in attempt to establish the one clinically accurate
diagnosis and rule out the diagnoses that are not correct. This process
substantiates to Medicare or the insurance carriers all the tests, biopsies,
examinations, and procedures that had to be performed on the patient to
fnally rule out all the incorrect diagnoses, and establish the one diagnosis
that is objectively proven and needs to be treated. This ruling out process is
called establishing a differential diagnosis.
Current Procedural Terminology, 4
th
Edition
(CPT-4)
The CPT is a uniform coding system that defnes and lists in numerical order medical
services and procedures such as surgery, medicine, laboratory tests, x-rays and
MRIs, biopsies, anesthesia, medical evaluation and management, optometry and
podiatry services, etc., covering all the medical and allied health specialties that
are provided by doctors, nurses, therapists, allied health practitioners, and anyone
licensed to deliver health care treatment.
The CPT manual is made up of a Table of Contents, Introduction, three Categories
of 5-digit codes (made up of numbers and/or letters) known as Category I,
Category II, and Category III, Appendices A through M, and the Index. Category
I codes constitute the majority of the CPT manual, which consists of codes with
fve numbers, covering services in six sections labeled: Evaluation and Management,
Anesthesia, Surgery, Radiology, Pathology and Laboratory, and Medicine. Category I codes
run from 00100 through 99607. Category II codes cover health care performance and
statistical measurements, and Category III codes are for health care experimental
procedures.
The Health Care Revenue Cycle 166
Figure 9: CPT
CPT category I codes (which are also found in HCPCS Level 1) may also have
modifers attached to them. Modifers are made up of two numbers (22 to 99), and
indicate that a performed service or procedure has been altered in some way, but not
changed the defnition or the assigned HCPCS/CPT code.
Example: 27590-62. 27590 is the Category I code for Amputation, thigh,
through femur, any level, and modifer -62 indicates Two Surgeons.
Therefore, this CPT procedural code indicates to the insurance carrier (that is
going to pay the bill) that two surgeons were involved in the surgical procedure
of cutting off the patients thigh. The modifer -62 has altered the CPT code
25790 to indicate that two surgeons are involved in this surgical procedure
instead of just one surgeon.
Modifers are found in Appendix A of the CPT manual and can indicate the
following:
1 A service or procedure has both a technical and professional component,
or at more than one location, or has been increased or decreased in
amount of service provided, was performed by more than one doctor
(for example, the surgery involved the operation of the cardio-
pulmonary bypass machine by one doctor and the open heart surgery
was performed by another doctor)
2 Only part of a service or procedure was performed on the patient.
Chapter 4 - Claim Form for the Doctors Ofce 167
3 An adjunctive service (another additional service) to the main service or
procedure was performed.
4 A service or procedure was performed on more than one area of the body
(bilateral). For example, both eyes.
5 A service or procedure was performed more than once or unusual
circumstances were involved in the administration of the service or
procedure For example, repeated surgeries were performed for the
removal of a cancer.
Health Care Common Procedure Coding
System (HCPCS)
HCPCS is a coding manual that is composed of two levels:
1 Level I consists of CPT category I codes, which consist of fve numbers
running from 00100 through 99607. CPT Category I codes are found in
Level I of HCPCS.
2 Level II consists of 5-digit alphanumeric codes beginning with letters
A through V and followed by four numbers (for example, L1134)
that identify health care products, supplies or services. Examples would
be Durable Medical Equipment (DME) such as walkers, commodes,
oxygen tanks, low back supports, etc; ambulance services; prosthetics;
orthotics; and other supplies (syringes, bandages, drainage tubes,
catheters, etc.) when used outside the doctors offce or hospital.
The Omnibus Reconciliation Act of 1986 (OBRA-86)) is legislation that requires
that the HCPCS coding be utilized on the UB-O4 claim forms for all Medicare
outpatient services provided in Acute Care Hospitals, Tertiary Care Hospitals,
Long Term Care Hospitals, Hospital Based Rural Health Clinics (RHCs), and
Federally Qualifed Health Clinics (FQHCs).
HCPCS Level I codes are the federal governments equivalent of the CPT-
4 Category I codes, and are mandatory for billing (utilizing the UB-04 claim
form) for procedures and services and products for Medicare inpatients and
outpatients. HCPCS Level I is used for assigning codes for procedures and
services in the hospital. In other words, CPT Category I codes = HCPCS Level I
codes.
Evaluation and Management Services (E/M)
1. Evaluation and Management Service codes are found in the CPT-4
Category I codes, and HCPCS Level I codes, and refect the health care
providers determination of the patients status, counseling of the patient
and coordination of medical care. In other words, these codes represent
all the cognitive (thinking) activities (such as analysis of examination
fndings, diagnostic imaging studies, laboratory tests, medical history,
previous treatment, and referrals) the doctor goes through at arriving at a
determination of what the diagnoses are and what treatment to give the
The Health Care Revenue Cycle 168
patient. The E/M section is divided into broad categories such as offce visits,
hospital visits, and consultations.
The E/M codes are created by considering seven key components which are:
History (Important)
Examination (Important)
Medical decision making by the doctor (Most Important)
Counseling
Coordination of Care
Nature of Presenting Problem
Time involved
2. E/M services are for offce visits, outpatient services, hospital observation
services, hospital inpatient services, consultations, emergency department
services, nursing facility services, case management services, rest home and
custodial care, delivery/newborn/pediatric care, critical care services and
home-based health services. E/M codes are meant to cover all health care
providers evaluation and management of procedures, services, treatments and
products administered in all the medical specialties such as Dermatology,
Obstetrics and Gynecology, Urology, Radiology, Orthopedics, Cardiology,
Ophthamology, Internal Medicine, Gastroenterology, Colorectal Medicine,
Otorhinolaryngology, Psychiatry, and all the subspecialties such as
Hematology, Immunology, Parisitology, Hepatology, Oncology, Trauma
Medicine, Nephrology, Physiatry, Pneumonology, Podiatry, etc.
3. Dentistry has its own CPT-type manual called the Common Dental
Terminology manual (CDT). Allied health care is also covered in the
CPT/HCPCS manual such as OT, PT, ST, radiology technician, respiratory
technician, nursing, home health aide, Chiropractic, Psychology, etc.
4. Other procedures, services and products found in the CPT and HCPCS
manuals include:
Ambulatory surgical services
Diagnostic imaging services such as x-rays, MRIs, CAT scans, etc.
Laboratory services (UA, CBC, biopsies, etc.)
Occupational Therapy, Physical Therapy, Speech Therapy
Medical services provided in the clinical setting or emergency room
Durable Medical Equipment (DME)
Orthotic and prosthetic devices (artifcal legs, breasts, etc.)
Surgical dressings that are used at home
Preventative medical services and immunizations
Immunosuppressive drugs
Psychiatric services
Infusion therapy and chemotherapy
Other assorted drugs and services described in the Medicare Hospital
Manual
Chapter 4 - Claim Form for the Doctors Ofce 169
SOAP Notes and the Patient-Oriented Medical Records (POMR)
The doctor and medical coder work with a number of protocols that are
used to organize patient medical records (aka-chart). The most common
format is known as the problem-oriented medical record (POMR).
The POMR has a section with data from the initial patient examination,
evaluation and assessment. When the patient makes additional visits,
the reasons for those encounters are listed separately and have their own
entries into the POMR. The process of the doctor performing evaluation and
management services (E/M) of the patient and creating the POMR requires
the use of the SOAP note format so that a comprehensive and sequential
collection of data is produced. This careful collection of the patients data
is important because it assists the doctor in keeping track of a patients
progress. More important, the medical record is a legal document and helps the
health care provider reduce mistakes and malpractice claims.
A problem-oriented medical record contains information known as SOAP
notes, which is a format that refects the doctors face-to-face encounter with
the patient, and has four parts: subjective, objective, assessment and plan.
S: The subjective information is what the patient discusses. It
documents the problems, complaints or trauma that brought the
patient to the doctors offce or hospital.
O: The objective information is what the physician fnds during the
examination of the patient and may include lab tests, x-rays and CAT
scans, reports from other providers and therapists, medical history,
other treatment, pharmaceuticals (drugs), etc.
A: The assessment, also called the evaluation, impression or conclusion, is
the doctors diagnosis and prognosis.
P: The plan, aka-advice or recommendations, is the course of treatment
and referrals the doctor recommends for the patient. This may
include surgery, medications, laboratory tests, referrals to other
providers and facilities, medical supplies, follow-up directions,
prognosis and disability evaluations concerning absence from work
or school.
Standard Code Sets
The ICD-9-CM, CPT-4, HCPCS, CDT and NDC are all examples of compatible
numbers and letters used to describe all health care diagnoses and conditions,
medical procedures and services, dental procedures and services, drugs, ambulance
services, and medical supplies and products, which are used by the medical coder
on the UB-04 and CMS-1500 claim forms. By using these standard collections
of numbers and letters, the hospital or doctor can consistently and reliably
communicate with the insurance carrier all health care activity the patient receives in
a concise and understandable manner anywhere in the country.
The Health Care Revenue Cycle 170
Defnitions: Types of Third Party Reimbursement and Categories
of Providers
1. Capitation: This is where the doctor is given a fxed amount of money
per patient per month (PMPM), regardless of how much medical service is
provided. Capitation is seen in HMOs with gatekeepers.
2. Straight Charges or Fee-for-Service (FFS): This is where the doctor charges
money for each service provided (a la carte) and is the most expensive
way to pay for health care treatment. It is an amount paid for each service by the
insurance company to the doctor.
3. Per Diem: This is where the hospital is paid by the insurance company a set
amount per day for each diagnosis regardless of how much the actual service
costs the hospital. The hospital may make a proft or suffer a loss if the
hospital does not properly anticipate the cost of providing the treatment.
4. Non-Participating Provider: This is a provider that has not contracted with
an insurance carrier, managed care plan or Medicare to provide health care
services to the carriers membership.
5. Participating Provider: This is a provider that has signed a contract with an
insurance carrier, MCO, or Medicare to provide health care services to the
carriers membership.
6. Any Willing Provider: Many states have any willing provider laws that
require a managed care organization to accept all qualifed physicians who
wish to participate in its plan (open panel). This regulation helps reduce the
number of patients who have to switch physicians if they change from one
MCO plan to another. Prior to this law, many MCOs used closed panels of
doctors, meaning they only accepted a certain number of providers in each
specialty in each geographic area, so that most of the providers, for example
in the Los Angeles metropolitan area, were shut out and could lose many of
their patients if the patients employers switched to an HMO in which the
provider was not participating.
Chapter 4 - Claim Form for the Doctors Ofce 171
Abbreviations and Acronyms
AARP American Association of Retired People
ABN Advanced Benefciary Notice
AKA Also Known As
APC Ambulatory Payment Classifcation
BBA Balanced Budget Act of 1997
ASC Ambulatory Surgical Center
BBRA Balanced Budget Refnement Act of 1999
CAH Critical Access Hospital
CERT Comprehensive Error Rate Testing
CPT-4 Current Procedural Terminology, 4th edition
DC Doctor of Chiropractic
DDS Doctor of Dental Surgery
DMD Doctor of Dental Medicine
DME Durable Medical Equipment
DPM Doctor of Podiatric Medicine (Foot Doctor)
DO Doctor of Osteopathy (Osteopathic Medicine)
EIN Employer Identifcation Number (used by the IRS)
EKG or ECG Electro-Cardiogram
E/M Evaluation and Management
ESRD End-Stage Renal Disease
FFS Fee-For-Service
FQHC Federally Qualifed Health Clinics
HICN or HIC Health Insurance Claim Number
HCPCS Healthcare Common Procedure Coding System
ICD-9-CM International Classifcation of Diseases, 9th Revision, Clinical
Modifcation
ICR Image Character Recognition
LMRPs Local Medical Review Policies
MCD Medicaid
MD Doctor of Medicine
MEC Mutually Exclusive Codes
MSN Medicare Summary Notice
The Health Care Revenue Cycle 172
MSP Medicare Secondary Payer
MUE Medically Unlikely Edits
NCCI National Correct Coding Initiative
NCD Medicares National Coverage Determinations
NPI National Provider Identifer Number
OBRA-86 Omnibus Reconciliation Act of 1986
OBRA-89 Omnibus Reconciliation Act of 1989
OD Doctor of Optometry (eye doctor)
OT Occupational Therapy
PHI Protected Health Information
PIN Provider Identifcation Number
PMPM Per Member Per Month
POMR Patient Oriented Medical Record
POS Place of Service
PPIN Performing Provider Identifcation Number used in a group practice
PRO Professional Review Organization or Peer Review Organization
PT Physical Therapy
RBRVS Resource Based Relative Value Scale
RHC (Hospital Based) Rural Health Clinics
RVU Relative Value Unit
SOAP Subjective, Objective, Assessment and Plan (notes)
ST Speech Therapy
UPIN Unique Provider Identifcation Number (for Medicare)
WHO World Health Organization
Chapter 4 - Claim Form for the Doctors Ofce 173
Sample Test Questions
These questions for the most part concentrate on details concerning the CMS-1500
claim form. The following 70 questions should be answered in 70 minutes or less.
1. The ICD-9-CM was developed and owned by the _____________.
A. CMS
B. Medicare
C. WHO
D. RBRVS
E. HIPAA
Answer: C
2. The ______________ establishes standards for medical billing, identifes codes
that are prone to fraud and abuse, and identifes codes that are susceptible to
unbundling or should not be billed together.
A. NCCI
B. Medicare
C. CERT
D. ABN
E, CPT-4
Answer: A
3. The RBRVS contains:
A. Fee schedule for paying doctors services.
B. MVPS.
C. Limiting Charge.
D. All of the above.
E. None of the above.
Answer: D
4. The _____________ is the basis of the Medicare fee schedule.
A. MVPS
B. RVU
C. ABN
D. E/M
E. RAC
Answer: B
5. The purpose of the ______________ is to reduce wrong payments by Medicare
to doctors and hospitals.
A. MVPS
B. RVU
C. ABN
D. E/M
E. RAC
Answer: E
The Health Care Revenue Cycle 174
6. The three most important key components of E/M services are __________. The
doctor uses E/M services to create the ________ which make up the _________.
A. History, Examination, Medical Decision Making by Doctor; SOAP notes,
POMR
B. Encounters, ABN, Medical Decision Making by Doctor; MVPS, RBRVS
C. Medical decision making by doctor, Highest Level of Specifcity, Evaluation
and Management; SOAP notes, POMR
D. ABN, HIPAA, NCCI; POMR, SOAP notes
E. A and B
F. B, C, and D
Answer: A
7. _______________ is legislation that states that HCPCS codes must be used on
the UB-04 claim forms for all Medicare inpatient and outpatient services used
in acute care hospitals.
A. OBRA-86
B. OBRA-89
C. HIPAA
D. LMRP
E. RBRVS
Answer: A
8. Examples of standard code sets include:
A. CPT-4
B. ICD-9-CM
C. HCPCS
D. CDT
E. NDC
F. All of the above
G. B, D, E
Answer: F
9. HCPCS Level I codes are the federal governments equivalent of
_________________ and are mandatory for billing procedures and services and
products for Medicare outpatiens.
A. CPT Category II codes
B. ICD-9-CM codes
C. CPT Category I codes
D. E/M codes
E. None of the above
Answer: C
Chapter 4 - Claim Form for the Doctors Ofce 175
10. HCPCS Level II codes begin with letters ______________ followed by
_____________ and are used to code ______.
A. M through Z; 4 numbers; DME, ambulance services, orthotics and prosthetics
B. A through V; 4 numbers; DME, ambulance services, orthotics and prosthetics
C. F through M; 5 numbers, DME, syringes, surgical dressings
D. A through V; 5 numbers; DME, ambulance services, syringes, comodes,
walkers
E. None of the above
Answer: B
11. _________ begin with the number 001 and go up through 999.9 and consist
of _________ chapters, which are further subdivided into sections, categories,
subcategories, and sub-classifcations.
A. E codes, 17
B. V codes, 17
C. ICD codes, 17
D. CPT codes, 6
E. HCPCS Level I codes, 2
F. HCPCS Level II codes, 2
Answer: C
12. V codes include the following medical services or health care situations except:
A. Vaccinations
B. Tissue Transplantation
C. Medical Screenings
D. Ambulance Services
E. Malignant Neoplasms
F. All of the above
G. D and E
Answer: G
13. The __________ is a uniform coding system that defnes and lists in numerical
order medical services and procedures such as surgery, CBC, x-rays, anesthesia,
etc.
A. CPT-4
B. ICD-9-CM
C. HCPCS Level I
D. HCPCS Level II
E. RBRVS
F. A and C
G. B and D
Answer: F
The Health Care Revenue Cycle 176
14. CPT Category I codes have __________ attached to them as a suffx, consist
of two numbers, that describe a medical situation that alters the main CPT
Category I code (such as 97039-50).
A. E codes
B. Modifers
C. E/M Services
D. Sub-classifcation codes
E. V codes
Answer: B
15. The CPT Category I codes are made up of _______ sections that include
__________________.
A. 5; E/M, Anesthesia, Surgery, Radiology, Pathology and Laboratory, Medicine.
B. 7; E/M, Anesthesia, Surgery, Radiology, Pathology and Laboratory, DME.
C. 6; E/M, Anesthesia, Surgery, Radiology, Pathology and Laboratory, Medicine.
D. None of the above.
Answer: C
17. The Table of Neoplasms are located in ____________.
A. Volume I, ICD
B. Category I, CPT
C. Category II, CPT
D. Volume II, ICD
E. HCPCS, Level I
Answer: D
18. The following ICD code represents the highest level of specifcity.
A. 123.4
B. 00889-P3
C. 345.67
D. 97039-50
E. D4567
Answer: C
19. In surgical cases, when the pre-operative diagnosis is different from the post-
operative diagnosis, the __________ is used in the UB-04 claim form.
A. Post-operative
B. Pre-operative
C. No diagnosis
D. None of the above
Answer: A
Chapter 4 - Claim Form for the Doctors Ofce 177
20. The three types of malignant neoplasms found in the Table of Neoplasms in
the Alphabetic Index of the ICD include:
A. Secondary Malignancy
B. Carcinoma in Situ
C. Primary Malignancy
D. Benign
E. Uncertain Behavior, Unspecifed Nature
F. C, D, E
G. A, B, C
Answer: G
21. _____________ is where CPT and HCPCS codes are reviewed due to anatomical
considerations to reduce linkage mistakes and incorrect coding errors.
A. CERT
B. MUE
C. RAC
D. MVPS
E. ABN
Answer: B
22. ___________ is a signed document that notifes the patient that a particular
service, product or procedure Medicare will probably not pay the doctor.
A. CERT
B. MUE
C. RAC
D. MVPS
E. ABN
Answer: E
23. Medicare Part A pays for:
A. Hospital inpatient services
B. Outpatient medical services administered in a hospital setting
C. Visits to the doctors offce
D. All of the above
E. B and C
F. A and B
Answer: F
24. ___________ defnes health care services that are safe and effective, reasonable
for the illness or injury, generally accepted medical services, consistent with
the diagnosis, not provided for the convenience for the patient or doctor, and
administered at an appropriate level of care.
A. ABN
B. Medical Necessity
C. APC
D. Waiver of Liability
E. CERT
Answer: B
The Health Care Revenue Cycle 178
25. All paid services that have clinical similarities are classifed into groups
known as ____________.
A. ABN or APCs
B. Medical Necessity
C. APCs or DRGs
D. Waiver of Liability or ABN
E. CERT or DME
F. SMI or CERT
Answer: C
27. The APC is a schedule of fees (OPPS) that Medicare has established to
reimburse for:
A. Outpatient medical services in a hospital setting.
B. Medicare Part B services for inpatients at hospitals that do not have Medicare
Part A coverage.
C. Hospitalization services for community mental health centers.
D. DME
E. A, B, C
F. C and D
Answer: E
28. Medicare Timely Filing regulations stipulate that health care services provided
on June 1, 2009 can be billed to Medicare no later than _______________.
A. December 31, 2009
B. December 31, 2010
C. December 31, 2008
D. December 31, 2011
E. None of the above
Answer: B
29. Medicare Timely Filing regulations stipulate that health care services provided
on November 1, 2009 can be billed to Medicare no later than _____________.
A. December 31, 2009
B. December 31, 2010
C. December 31, 2008
D. December 31, 2011
E. None of the above
Answer: D
30. Ancillary services include all of the following except:
A. Operating room
B. Anesthesia
C. Pharmacy
D. Ambulance
E. PT, OT, ST
F. Radiology
Answer: D
Chapter 4 - Claim Form for the Doctors Ofce 179
31. Hospitals and health care facilities that are exempt from APCs include:
A. CAH
B. Certain Hospitals in Maryland
C. Cancer Hospitals
D. IHS facilities
E. All of the above
F. None of the above
Answer: E
32. Sequencing means that the ICD codes should be placed in order of
________________ on the UB-04 or CMS-1500 claim forms.
A. Severity
B. Cost
C. The Alphabet
D. None of the above
Answer: A
33. _____________ is a regulation that is used when a Medicare patient did not
know, or was reasonably not expected to know, that certain medical services
would not be covered by Medicare and therefore the patient is not liable
to pay for those Medicare denied services when found to be not medically
necessary or reasonable.
A. Advanced Benefciary Notice
B. Medical Unlikely Edits
C. Waiver of Liability
D. Medicare Timely Filing Regulations
E. FQHC
Answer: C
34. ______________ describes reimbursement to the doctor where he is paid a fxed
amount (of money) per member (patient) per month; ______________ describes
reimbursement to the doctor where he is paid for each service provided, the
most expensive way to pay for health care services; _____________ describes
reimbursement to the hospital on a daily basis a fxed amount no matter what
the service actually costs the hospital.
A. Per Diem; Capitation (PMPM); FFS
B. FFS; Per Diem; Capitation (PMPM)
C. Capitation (PMPM); FFS; Per Diem
D. SMI; Capitation; Cash
E. None of the above
Answer: C
The Health Care Revenue Cycle 180
35. All laboratory services a Medicare patient receives must be provided by a
laboratory certifed by ____________.
A. PMPM
B. CLIA
C. DME
D. BBRA
E. Medigap
F. SMI
Answer: B
36. A ___________ policy pays for deductibles, co-payments, and co-insurances
that the patient would normally be responsible for under Medicare.
A. MCD
B. CLIA
C. DME
D. BBRA
E. Medigap
Answer: E
37. ___________ is a joint state-federal program that provides monetary assistance,
food stamps, health care, and other benefts to those who are low income.
A. Medigap
B. Medicare
C. Medicaid
D. SMI
E. MCD
F. CLIA
Answer: C
38. Dual Eligibility means the benefciary has both _____________ and
_____________ coverage. ___________ is the program that is known as the
payer of last resort.
A. Medicare, Blue Cross/Blue Shield; Medicaid
B. Medigap, Medicare; MCD
C. CLIA, Medicare; Medicaid
D. Medicare, Medicaid; MCD
E. None of the above.
Answer: D
39. The CMS-1500 claim form:
A. Is printed in red drop out ink
B. Can be scanned optically
C. Photocopies will not be accepted by Medicare
D. Must be complete and valid in order to be paid
E. All of the above
F. None of the above
Answer: E
Chapter 4 - Claim Form for the Doctors Ofce 181
40. The ICD diagnosis codes are placed in block _____________ in the CMS-1500
claim form.
A. 24J
B. 21
C. 24B
D. 10A
E. 1
Answer: B
41. The Rendering Provider ID number is placed in block ___________ in the
CMS-1500.
A. 24J
B. 21
C. 24B
D. 10A
E. 1
Answer: A
42. The type of health care insurance carrier is placed in block __________ in the
CMS-1500.
A. 24J
B. 21
C. 24B
D. 10A
E. 1
Answer: E
43. The actual location where medical services are billed is placed in block
_________ in the CMS-1500.
A. 31
B. 32
C. 33
D. 12
E. 13
Answer: C
44. The actual location where medical services are rendered to the patient (POS) is
placed in block _______ in the CMS-1500.
A. 31
B. 32
C. 33
D. 12
E. 13
Answer: B
The Health Care Revenue Cycle 182
45. The HCPCS/CPT codes for medical services and procedures provided to the
patient are placed in block_________.
A. 24A
B. 24B
C. 24C
D. 24D
E. 24E
Answer: D
46. The charges for medical services rendered to the patient are placed in block
__________.
A. 24A
B. 24C
C. 24E
D. 24F
E. 24G
Answer: D
47. The correct way to enter the date on the CMS-1500 form is:
A. MM/DD/YY
B. DD/MM/YY
C. MM/DD/YYYY
D. YYYY/MM/DD
Answer: A
48. The CLIA number is placed in block _________ in the CMS-1500 claim form.
A. 21
B. 22
C. 23
D. 24
E. 25
Answer: C
49. Patients address and phone number are placed in block ____________.
A. 1
B. 2
C. 3
D. 4
E. 5
Answer: E
50. The name of the person whose insurance is paying for the medical services
(guarantor) is placed in block ___________.
A. 1
B. 2
C. 3
D. 4
E. 5
Answer: D
Chapter 4 - Claim Form for the Doctors Ofce 183
51. The purpose of the ____________ is to reduce wrong payments by Medicare to
doctors and hospitals. It does this by detecting and correcting overpayments
and underpayments made by Medicare.
A. RAC
B. ABN
C. PRO
D. ICR
E. CERT
Answer: A
52. Date of current illness, injury or pregnancy (MM/DD/YY) is put in this block
in the CMS-1500.
A. 12
B. 13
C. 14
D. 15
E. 16
Answer: C
53. Federal Tax Identifcation Number, Employer Identifcation Number (EIN), or
Social Security Number (SSN) of the doctor or supplier of health care services
or products is placed in this block in the CMS-1500.
A. 24A
B. 24B
C. 26
D. 25
E. 33
Answer: D
54. The ____________________________ means that ICD codes have been
established to the greatest degree of defnition and accuracy.
A. Advanced Benefciary Notice
B. Highest Level of Specifcity
C. Assignment of Benefts
D. Surgical Package
E. Per Member Per Month
Answer: B
55. ___________ include medical services or health care situations other than
disease or pathologies such as immunizations, medical history, and tissue
transplantation.
A. E codes
B. ICD codes
C. HCPCS Level I codes
D. CPT Category II codes
E. V codes
Answer: E
The Health Care Revenue Cycle 184
56. __________document EXTERNAL causes of disease, injury or trauma such as
mvas, sports accidents, terrorism, and poisoning.:
A. E codes
B. ICD codes
C. HCPCS Level I codes
D. HCPCS Level II codes
E. V codes
Answer: A
57. ___________ codes refect all the cognitive (thinking) activities, such as analysis
of examination fndings, diagnostic imaging studies, laboratory tests, medical
history, previous treatment, and referrals, the doctor goes through at arriving
at a determination of what the diagnoses are and what treatment to give the
patient. The most common format for medical records is the ___________
which contains ___________ and has 4 parts.
A. E codes; ABN; SOAP notes
B. V codes; CLIA; HCIN
C. ICD codes; SOAP notes; POMR
D. E/M codes; POMR; SOAP notes
E. None of the above
Answer: D
58. _____________ describes where multiple medical services are coded with one
CPT code, and billed and paid with one fee, AKA- Global Surgical Fee or
Surgical Package.
A. Unbundling
B. Bundling
C. Capitation
D. Medical Necessity
E. ABN
Answer: B
59. Block __________ in the CMS-1500 claim form is for Accepts Assignment.
Check this block YES or NO to indicate whether the doctor accepts
assignment of Medicare benefts (takes what Medicare will pay according to
the fee schedule), will bill Medicare directly, and will wait for payment from
Medicare.
A. 25
B. 26
C. 27
D. 28
E. 29
Answer: C
Chapter 4 - Claim Form for the Doctors Ofce 185
60. Block ___________ is for the Diagnosis Pointer. This is where the ICD
diagnoses are matched (linked) to the HCPCS/CPT procedural codes.
A. 24C
B. 24D
C. 24E
D. 24F
E. 24G
Answer: C
61. Medicare Part B insurance is also known as ___________.
A. ABN
B. SMI
C. CLIA
D. HCIN
E. MUE
Answer: B
62. Medigap insurance is meant for consumers with:
A. Medicare Parts A and B
B. Original Medicare Plan
C. Medicare Parts C and D
D. Medicaid
E. A and B
F. A, B, C and D
Answer: E
63. _______ is a schedule of fees (OPPS) that Medicare pays for certain medical
services provided for patients who are outpatients.
A. DRG
B. APC
C. MCO
D. HCIN
E. SSN
Answer: B
64. 123-45-6789D is the ______________ for the _____________.
A. HCIN, Child
B. SSN, Spouse
C. HCIN, Widow
D. DRG, Wage Earner
E. HCIN, Adopting Father
Answer: C
The Health Care Revenue Cycle 186
65. The suffx ___________ in the HCIN is for the Disabled Adult, and the suffx
__________ in the HCIN is for the Adopting Father.
A. A, B
B. B, HAD
C. D, F5
D. HAD, F5
E. HAD, A
F. F5, C
Answer: D
66. Many states have _____________ laws that require a managed care organization
to accept all qualifed physicians who wish to participate in its plan (open
panel).
A. Participating Provider
B. Any Willing Provider
C. Non-participating Provider
D. Closed Panel
E. FQHC
Answer: B
67. If the court issues a __________, this is a court order demanding the doctor or a
member of the medical staff to appear in person and testify.
A. HIPAA Security Rule
B. Encryption
C. POMR
D. Subpoena
E. Malpractice
Answer: D
68. If the court requires the witness to bring specifc evidence, such as a patients
medical record, it issues a ___________, which demands the doctor or member
of the staff to appear, testify, and to bring the requested documentation.
A. Subpoena
B. SOAP notes
C. Subpoena duces tecum
D. ABN
E. HIPAA Security Rule
Answer: C
69. When the doctor documents several working diagnoses in the course of
the patients hospitalization until further testing and examination fnally
establishes the fnal clinically correct diagnosis, this process is called creating a
______________.
A. Differential Diagnosis
B. Prognosis
C. Against Medical Advice
D. Pre-operative Diagnosis
E. None of the above
Answer: A
Chapter 4 - Claim Form for the Doctors Ofce 187
70. The _________________ requires covered entities (doctors, hospitals, SNFs,
governmental bodies, public health clinics, etc.) to establish and enforce
safeguards to protect the patients Protected Health Information (PHI).
A. NPI
B. Waiver of Liability
C. HIPAA Security Rule
D. Subpoena
E. Subpoena duces tecum
Answer: C
End of Chapter 4
Chapter 5 - Doctor/Hospital Financial Matters 189
Chapter 5 Doctor/Hospital Financial Matters
Chapter Topics
Medical Identity Theft
Third Party Collection Activity
Bankruptcy
Collection Regulations of the Federal Government
Calculations: Average Daily Revenues and Average Days of Revenue in
Accounts Receivable (ADRR)
Abbreviations and Acronyms
Sample Test Questions
After studying this chapter you will understand:
Medical Identity Theft
Third Party Collections; Bad Debt Requirements
Bankruptcy: Chapters 7, 11, 12 and 13
Involuntary Bankruptcy
The Bankruptcy Abuse Prevention and Consumer Protection Act of 2005
Discharge of Debtor
Dismissal of Bankruptcy
The Truth in Lending Act
Fair Debt Collection Practices Act (FDCPA)
Fair Credit Billing Act
Fair Credit Reporting Act (FCRA)
Fair and Accurate Credit Transaction Act
Equal Credit Opportunity Act (ECOA)
Deceased Patient Notifcation
SKIP
Statute of Limitations
Judgement, Lien, Tort Liability
Charity, Indigent and Bad Debt
Courtesy Discharge
Average Daily Revenues
Average Days of Revenue in Accounts Receivable (ADRR)
The Health Care Revenue Cycle 190
Medical Identity Theft
Medical Identity Theft occurs when someone uses the patients protected health information
(PHI) without the consumers knowledge or permission in order to obtain or receive payment
for medical treatment or services or products. Medical Identify Theft is a crime that
has increased exponentially in the last several decades, and is particularly harmful
because it can result in erroneous entries into the patients medical records creating
fctitious medical records in the victims name. Wrong data in the medical record can
adversely affect future treatment the patient will receivefor example, an incorrect
medical history of diabetes or cancer. If such mistaken information is found in the
medical record, and the patient appears for treatment, this may lead the doctor
to make treatment decisions that could adversely affect the patients diagnosis,
prognosis, health care, or even their life.
A wrong medical history of diabetes or cancer could also negatively affect the
patients future ability to get employment or purchase life or health or disability
insurance. In addition, an erroneous medical history of diabetes or cancer could
result in needlessly higher costs due to medical care the patient does not need such
as excessive testing, incorrect treatment, misuse of medical providers and hospital
resources, and a longer stay in the hospital.
Medical Identity Theft not only results in poor medical care, but increases the
chances of malpractice exposure for the health care provider and hospital. As
Medical Identity Theft can result in thousands of dollars of unnecessary medical
treatment, it could potentially drive the consumer into bankruptcy in an attempt to
pay health care bills that are insurmountable. Medical Identity Theft can plague the
consumer for years, destroy the consumers credit rating, take years to correct, and
require the use of expensive legal intervention.
Tips for preventing and detecting Medical Identity Theft by the
consumer include:
1. Monitoring health care records closely and address any errors quickly.
2. Share PHI, fnancial and insurance information only with trusted health care
providers and carriers and those the patient knows and trusts.
3. Monitor all EOB and fnancial records (itemized statements, data mailers,
receipts, etc.) received from insurance carriers, doctors and hospitals
for accuracy. Get an annual summary of all health care benefts paid by
insurance carriers to all doctors, suppliers and hospitals utilized by the
consumer. Contact and correct immediately all health care providers if fraud
or abuse is suspected or documented in the paperwork.
4. Maintain copies of all paperwork related to health care services and products
received by the patient.
5. Avoid the use of FREE medical services or products, as these are frequently
used to obtain information so criminals can submit fraudulent insurance
claims for money.
Chapter 5 - Doctor/Hospital Financial Matters 191
6. Protect all health insurance information such as insurance cards and
identifying numbers, EOBs, fnancial statements from doctors and hospitals,
or any other health care correspondence.
7. Review credit reports with nationwide credit reporting companies such
as Equifax, Experian, or TransUnion. Carefully review any medical debts
incurred and make sure they are accurate. Report immediately any suspected
fraudulent or abusive medical charges.
Responding to Medical Identity Theft incidents by the consumer
include:
1. Contacting the health information manager, HIPAA privacy offcer, or anti-
fraud hotline at the insurance company or Medicare.
2. Writing down dates, names, contact information (phone numbers, email
addresses, mailing addresses) of everyone contacted including what was
discussed, all paperwork involved, and any other relevant information.
Make hard copies of all letters, emails, legal correspondence, and any other
relevant information and keep in a fle safe from loss.
3. Filing complaints with the state Attorney General, state insurance
department and the insurance commissioner, the Identity Theft
Clearinghouse, and the federal Department of Health and Human Services in
Washington, DC.
4. Regularly changing all personal information numbers (PIN), usernames and
passwords for all PHI, internet access sites, etc.
5. Important Contact Numbers for detecting and correcting errors, and fling
complaints for Medical Identity Theft and related issues, include:
For suspected misuse of the patient's Social Security Number (SSN): 800-
269-0721. The SSN can be misused to get Medicare benefts, for example.
Explore "Tools for Victims" provided by the Federal Trade Commission
(FTC) at: www.ftc.gov/bcp/edu/microsites/idtheft/tools.html. This is
an excellent resource for the consumer to help correct and fle affdavits
for suspected cases of health care and fnancial fraud and abuse.
If the health care provider, hospital or insurance carrier refuses the
patient access to their medical records contact: Offce for Civil Rights at
Health and Human Services (HHS) at 866-627-7748 or www.hhs.gov/
ocr/privacyhowtofle.htm.
To fle a complaint with the Attorney General in the state where the
Medical Identity Theft or insurance problems have occurred, contact:
www.naag.org/attorneys_general.php.
To contact the insurance commissioner of each state to fle complaints
about an insurance carrier, visit the National Association of Insurance
Commissioners at www.naic.org.
The Health Care Revenue Cycle 192
To fle a complaint with the Identity Theft Data Clearinghouse, operated
by the FTC and the Internet Crime Complaint Center, contact: https://
rn.ftc.gov/pls/dod/widtpub$.starup?Z_ORG_CODE=PU03.
Third Party Collection Activity
1. Anytime the patient owes money for health care services to the hospital,
physician or medical supplier, outstanding balances can be forwarded to
a third party at anytime so the money can be collected. Obviously, for the
purposes of good public relations, it makes good sense to notify the patient
in advance of any collection activity to see if the outstanding balance can
be satisfed in an amicable fashion. This helps in reducing the accounts
receivable for the hospital or doctor and maintaining the patients good will.
If the hospital sends the patients outstanding balance to a collection agency,
it is recommended that they are always sent by certifed mail. Remember,
HIPAA does not allow disclosure of the patients PHI including medical,
therapeutic, diagnostic, or any other protected health care records to the
collection agency.
2. Before any collection activity is initiated, it is imperative that the
outstanding balance is legitimate, valid, and properly documented. Before
any third party collection activity begins, it behooves the hospital or doctors
offce to attempt all reasonable means of collecting the balance with data
mailers, phone calls, and other communication sent by regular mail, as well
as by certifed mail, so there is no doubt in the patients mind that they have
been notifed before collection activities commence.
3. Medicares Bad Debt Requirements recommend that an appropriate
sequence of collection attempts are tried by mail and phone, prior to a third
party collection agency becoming involved. Repeated phone contacts are the
most effective way to contact the patient or guarantor to attempt to collect
the debt.
4. Further information can be accessed on bankruptcy laws at the following
website: http://www.frstgov/Topics/Reference_Shelf.shtml.
5. Once an offcial written notice is received by the physicians offce or
hospital from the United States Bankruptcy Courts, particularly for Chapter
7 Bankruptcy, that the patient or guarantor or responsible party has fled for
relief under the United States Bankruptcy laws, all collection efforts must
stop.
6. It is very important the physicians offce or hospital document in the
patients account the legal chapter (7, 11, 12, or 13) and the court of the
bankruptcy notice, as well as the lawyer (name, address, and phone number)
who represents the patient with the bad debt. The physicians offce or
hospital must have a copy of the bankruptcy notice in the patients fle. It is
important the patient includes the debt owed to the doctor or hospital in the
bankruptcy legal petition so that the provider has a chance to collect monies
owed. Otherwise, the provider can proceed with normal collection activities
against the patient because their health care debts are not covered if not
Chapter 5 - Doctor/Hospital Financial Matters 193
included in the bankruptcy petition. Bad debts that are not included in the
bankruptcy notice are not protected from collection activities.
7. Debtor = The individual, patient or business that owes the doctor or hospital
money
Creditor = The individual or business (doctor or hospital) that is owed the
money by the patient or guarantor.
Money = Actual amount of cash the debtor possess
Assets = Stocks, bonds, property, cars, real estate (home), furniture, material
and machinery related to the patients business, etc. of the debtor. Assets
include all liquid (can be sold for money or liquidated) and non-liquid (hard
to sell for money) valuables.
Auction = A public selling of the assets of the debtor to raise money to pay
the bad debt owed by the debtor. Seen with Chapter 7 bankruptcy.
8. Patient Refunds. Money occasionally needs to be refunded to patients when
the practice has overcharged a patient for a service. The balance due the
patient must be refunded promptly if the patient has completed care and
has been discharged. However, if the patient is still active and in treatment,
the balance is listed as a credit on the patients account ledger. This
overpayment on the patients account ledger is applied to any charges the
patient may incur as a result of future treatment.
Bankruptcy
Figure 10: Bankruptcy
The Health Care Revenue Cycle 194
The most common bankruptcy chapters are the following:
1. Chapter 7: Applies to individuals and businesses that cannot pay their
debts based on their income. Some property and assets are exempt from
the bankruptcy laws which are determined according to each states laws.
Approximately seventy percent (70%) of all bankruptcy claims are fled
under Chapter 7. The debtors assets are auctioned (liquidated) to satisfy the
creditors Chapter 7 bankruptcy claims. This is also known as liquidation
bankruptcy.
2. Chapter 11, is also known as reorganization bankruptcy. Chapter 11
bankruptcy gives the business or corporation who is in fnancial trouble
relief, while it continues to function, so it can work out a repayment plan with
the bankruptcy judge overseeing all the companys important decisions. The
business has three months to draft a plan to pay its debts initially, then any
party (creditor) can submit a bankruptcy plan to the judge to have the bad
debts paid by the business who is in fnancial trouble. Most Chapter 11 cases
end up as Chapter 7 liquidation cases.
3. Chapter 12: This is bankruptcy for a farmer who has a regular annual
income, meaning that this individual makes a living primarily as a farmer.
Having a regular annual income for the farmer is to insure that there is a
suffcient stable amount of money being made every year on a regular basis,
even seasonally, so the debtor (farmer) can make payments and pay back the
bad debt to the creditor. Chapter 12 is known as voluntary meaning only
the debtor farmer can apply for this type of bankruptcy.
4. Chapter 13: This is bankruptcy for individuals who make a regular income
but who cannot currently pay their debts. The purpose of this type of
bankruptcy is to allow people who have fnancial problems, under court
supervision and protection, to repay their debts to their creditors over an
extended period of time. Chapter 13 bankruptcy permits the debtor to pay
their creditors, in installments, over a three year period of time. During this
three year period creditors cannot carry out continuing collection activities.
If the repayment period is for more than three years, it must be approved by
the court for suffcient reasons and cannot be longer than fve years.
Involuntary Bankruptcy
This is where the creditors force the debtor into bankruptcy under Chapter 7 or 11. If
the debtor has 12 or more creditors, three of which are for claims in excess of $5,000
each, then any of the three can force the debtor into Chapter 7 or 11 Bankruptcy. If there
are less than 12 creditors, then only one (1) creditor has to be owed at least $10, 775 to
force the debtor into Chapter 7 or 11 bankruptcy.
Chapter 5 - Doctor/Hospital Financial Matters 195
The Bankruptcy Abuse Prevention and Consumer Protection Act
of 2005
This is legislation making fling for bankruptcy more diffcult for individuals, and
insuring those debtors who are fnancially capable to pay what they can afford to
satisfy their debts.
1. Debtors will have to get credit counseling, including budgeting and debt
management advise, before they can fle a bankruptcy case and have their
debts eliminated. Before the bankruptcy case is fled with the court and
fnalized, the debtor will have to attend additional counseling to learn
personal fnancial management, then a bankruptcy discharge will be issued
by the court fnally wiping out their debts. The purpose of bankruptcy
counseling is to help the debtor determine whether they really need to
legally fle for bankruptcy, or if they could enter in an informal repayment
plan with their creditors.
2. Those with higher incomes may not be able to eliminate all their debts
under Chapter 7, but instead will have to pay back some of their debt under
Chapter 13.
3. New requirements will be placed on lawyers in bankruptcy cases,
therefore the consumer may experience more diffculty to fnd a lawyer for
representation.
Confrming Bankruptcy by the Doctor or Hospital
1. Contact the Federal United States Bankruptcy Court for the district where the
patient or guarantor (who owes the hospital or doctors bill) lives.
2. Use Voice Case Information System (VCIS), which is a telephone check
at the bankruptcy clerks offce (at the court), to confrm the bankruptcy.
Confrming the bankruptcy can also be done by using the national computer
system known as PACER, or by calling the District Clerks offce, or by
contacting the attorney handling the patients bankruptcy, or by confrming
the bankruptcy in the newspaper.
Notifcation of Bankruptcy
Once the doctor or hospital gets receipt of Chapter 7 Notifcation of Bankruptcy of
the patient or guarantor, the following must be done:
1. Clearly mark the patients account or fle indicating a Chapter 7 bankruptcy
has occurred.
2. End all collection activity and cease all contact with the patient for
payment, until receipt of fnal disposition of the patients bankruptcy has
been received from the Bankruptcy Court.
3. Make sure any third party collection agencies the doctor or hospital are
using are notifed to stop all collection activities with the patient due to the
patients Bankruptcy Notice. Send third party collection agencies a copy of
the Bankruptcy Notice.
The Health Care Revenue Cycle 196
4. If any payments are received on the patients account while under
bankruptcy, the doctor or hospital should NOTIFY all parties involved:
patient, third party collection agency, court, attorney, etc.
Discharge of Debtor
1. This is a legal notice concerning the patients bankruptcy, called the
Discharge of Debtor, which releases the patient or guarantor from
having to pay any of the money owed to the debtors creditors listed in the
Bankruptcy Petition. The patients debt is wiped out and the creditor cannot
legally collect what is owed to them by the debtor.
2. Any debts not listed in the Bankruptcy Petition will not be eliminated, and
the patient will still owe them and the doctor or hospital can continue with
collection activities.
3. It is important the doctor or hospital make certain that the patients debts
are legally listed in the bankruptcy petition. This is important because under
Chapter 7 bankruptcy the patients assets will be auctioned, and under
Chapter 13 bankruptcy the patient is put into a repayment plan, so there may
be a chance that the doctor or hospital can recover at least some of what is
owed. Otherwise, the doctor or hospital should write off the patients bad
debt (account balance) from their books. Smaller medical practices rarely sue
their patients to collect money they are owed. Hospitals and doctors owed
large amounts of money have a fnancial incentive to sue for collections;
however, this may generate an unfounded malpractice suit and will produce
bad public relations. Usually small unpaid balances are deemed uncollectible
to avoid going through the expense of a court case with uncertain results.
4. Both Medicare and Medicaid require a medical practice, hospital or supplier
to follow a specifc series of steps before an account can be written-off.
Writing-off some accounts and not others could be considered fraud if there
are discrepancies between charges for the same services, procedures or
products. Remember, the health care provider must charge the same fees
regardless of whether the patient is a Medicare, private insurance, workers
compensation, accident, or cash payer.
Dismissal of Bankruptcy
This is where the court rules the debtors (patient) bankruptcy is ended (cancelled).
The bankruptcy is no longer in effect. This means the creditor (doctor or hospital)
can begin billing the patient directly, refer the account to a debt collection agency,
or begin legal action against the debtor to collect the debt. When the patients
bankruptcy is no longer valid, it is most commonly due to the following:
1. Debtor (patient) is not following through with the legal process of fling for
bankruptcy.
2. Patient is not paying their attorneys fees to execute their bankruptcy.
3. The debtor fails to provide requested legal documentation for their
bankruptcy.
Chapter 5 - Doctor/Hospital Financial Matters 197
Collection Regulations of the Federal
Government
It is important not to confuse the different Titles of the Consumer Credit Protection
Act. Know the differences between all the following pieces of legislation.
Remember:
1. Title I of the Consumer Credit Protection Act = The Truth in Lending Act or
Truth in Lending Consumer Credit Cost Disclosure Act (1969) or Regulation
Z or The Consumer Credit Protection Act
2. Title VI of the Consumer Credit Protection Act = Fair Credit Reporting Act
(FCRA) (1971)
3. Title VIII of the Consumer Credit Protection Act = Fair Debt Collection
Practices Act (FDCPA) (1978)
The Truth in Lending Act (TLA) or Truth in Lending Consumer
Credit Cost Disclosure Act (1969).
This is Title I of the Consumer Credit Protection Act.
1. Also known as Regulation Z or The Consumer Credit Protection Act.
2. This act deals with the disclosure of information to the consumer before
credit is given to the consumer. Disclosure means complete and full explanation of
all information.
3. The disclosure is made in writing by the company extending the credit and
the consumer receives a copy of this disclosure.
The annual percentage rate (APR) and fnance charge must be clearly
and obviously seen by the consumer.
If the APR and fnance charges are estimates, this fact must be clearly
stated to the consumer.
If more than one creditor is involved, all the creditors have to agree
amongst themselves who will comply with the credit regulations, APR,
and fnance charges.
Fair Debt Collection Practices Act (FDCPA) (1978)
This is Title VIII of the Consumer Credit Protection Act
Imposes strict limitations on:
1. How the debt collector acquires information on the location of the debtor
(consumer).
2. How the debt collector communicates with the debtor or others in the
collection of a debt.
The FDCPA prohibits:
The Health Care Revenue Cycle 198
1. Harassment or abuse of the debtor in the collection process. This includes
the debt collector using any profanity or threatening language.
2. Use of false or misleading information in the collection process. This
includes lying to the debtor.
3. Communication by the debt collector with the debtor at unusual times or
places.
4. At any unusual place includes locations that are inconvenient to the debtor
such as public humiliation of the debtor at their job, home, social functions,
movies or church.
5. Unusual times such as middle of the night or very early in the morning.
Debt collection activities can only occur between 8 AM to 9 PM (debtors
time zone), unless prior approval has been granted to the debt collector from
the consumer. Abusive debt collection activities include repeated harassing
telephone calls or emails, or personal face-to-face contact, at the consumers
home, place of employment, social functions, church, etc.
6. Communication by the debt collector with the consumer is strictly forbidden
if the debtor has legal representation, unless prior approval is received by
the debt collector from the attorney for communication with the consumer.
7. If communication at the place of the debtors employment is permitted, the
debt collector does not discuss the nature of the call except with the debtor
and in private.
Fair Credit Billing Act (1975)
The purpose of this act is to protect consumers from the following:
1. Inaccurate or unfair practices by those who issue open ended credit, for
example: a bank (Mastercard or VISA) or department store (Sears, Macys,
Lord and Taylor, Walmart, Target, etc.).
2. Requires creditors to inform debtors of their rights and responsibilities under
this act.
3. Main goal of this act is to provide prompt settlement (clear up inaccuracies)
of billing problems.
This act as related to hospital billing includes:
1. The patient must notify the hospital of any errors within 60 days after the
patient receives a bill or statement from the hospital. The hospital then has 30
days to respond to the patients inquiry.
2. The error must be corrected by the hospital, or the accuracy of the
statement or bill explained satisfactorily to the patient (customer), within
two billing cycles or a maximum of 90 days.
3. If the time frames in #1 or #2 above are not met, the patients rights are
violated and forfeiture (cancellation) of the hospitals account may occur. In
other words, the hospital may lose its right to collect the disputed amounts of
money if they do not respond to the patient correctly within 90 days.
Chapter 5 - Doctor/Hospital Financial Matters 199
Fair Credit Reporting Act (FCRA) (1971)
Title VI of the Consumer Credit Protection Act
1. This act defnes what information from a consumer credit report can be used
and by who. The FCRA provides maximum protection of the consumers
right to privacy and confdentiality concerning the consumers credit
report. The consumer report is a listing of the consumers credit, and all
the credit that has been extended to the consumer, such as credit cards,
mortgages, student loans, car loans, all business and personal loans (secured
and unsecured), etc.
2. FCRA is enforced by the Federal Trade Commission (FTC), is designed to
promote accuracy and privacy of the information used in consumer reports,
establish and police the activities of Credit Reporting Agencies (CRA) and
the businesses that supply data about debtors to CRAs, and those entities
that use the information found in CRAs.
3. CRAs are used:
To determine whether an applicant is eligible to be extended credit
for credit cards, to buy insurance policies, personal or business loans,
mortgages, car loans, etc.
For employment purposes.
For legal or court related matters.
For legitimate requirements connected with a business transaction
(buying a car or home).
Fair and Accurate Credit Transaction Act (includes SKIP)
Amends the FCRA which include:
1. Make the reporting of delinquent data (and dates of delinquency) more
consistent and clear.
2. Creating Safe Harbors (legal places where legal liability is reduced) for
debt collectors and those who provide information to debt collectors.
3. Guidance, clarifcation and limits to legal liability with reasonable policies
and procedures for the debt collector.
SKIP and SKIP Tracing Resources (Important)
1. A SKIP is a debtor who cannot be located by a creditor.
2. There are three types of SKIP:
Intentional SKIP are debtors who avoid paying bills by intentionally
changing where they live (residency), failing to leave a forwarding
address, intentionally changing their name or intentionally providing
wrong information to hinder collection activities.
Un-intentional SKIP: A debtor (patient) who moves or changes
their residency, but unintentially does not notify their creditors of a
forwarding address.
The Health Care Revenue Cycle 200
False SKIP: This type of SKIP is unintentional and caused by a clerical
error when the patients information is entered (registration), such as
numbers in the street address are mixed up or wrong, incorrect zip code,
or incomplete information.
3. SKIP Tracing resources gives the debt collector information to contact the
debtor and include:
Internet
Telephone Directories
Credit Bureaus such as TRW
U.S. Postal Service
Cross-reference directories known as bressers (matching names with
addresses and phone numbers, etc).
Department of Motor Vehicles
Tax Records
Landlord or Mortgage Holder
Employers (when asking the employer for help to locate the debtor,
ALWAYS SPEAK to Human Resources, and keep all communication
private)
Relatives, neighbors
Equal Credit Opportunity Act (ECOA)
This legislation does not allow creditors to discriminate against applicants on
the basis of sex, marital status, race, national origin, ethnicity, religion or age.
Furthermore, creditors cannot deny credit because the applicant receives public
assistance or has exercised their rights under the Consumer Credit Protection Act (for
example, Titles I, VI or VIII above).
Deceased Patient Notifcation: When the hospital or doctor is
notifed the patient is deceased (has died):
1. Check to see if a legitimate estate exists (check register of wills at the county
courthouse for estate information) and fle appropriate caveat (legal claim) to
the estate to retrieve money owed.
2. Change the mailing address of the patient to: To the Estate of. . . . so that it
will be properly delivered to the executor of the deceased patients estate in a
timely manner.
3. If no estate exists, and another party cannot be located that assumes the
patients debt, make sure all insurance has been collected, then write off
(cancel) any remaining balance the deceased patient is responsible for.
4. Estate is a legal term describing all of the deceased persons possessions
and assets. The executor is the individual who the debtor legally has
given permission to handle all their legal and fnancial affairs (carry out
the deceased persons will) after the debtor has died. The will is a legal
Chapter 5 - Doctor/Hospital Financial Matters 201
document indicating the distribution of a persons possessions and to carry
out their wishes after their death.
General Accounting Principles Applied to Cashier Functions for
the Hospital or Doctor.
1. Patients checks are to be endorsed with For Deposit Only, and a duplicate
numbered receipt log is maintained so both patient, doctor and hospital have
identical records of all fnancial transactions. The patient cannot later say
they paid by check or cash but there remains a balance on their account, there
is always a receipt.
2. Issue patient a receipt for all cash deposits and make all deposits in the bank
the same day.
3. Store undeposited payments, cash or check, and valuables in a fre-proof
safe.
4. The rules the cashier follows in all fnancial transactions is listed in the
Generally Accepted Accounting Procedures (GAAP)
Efective Collection Policies Include:
1. At admission, the hospital or doctor must have policies to collect minimally
acceptable payments from the patient. The optimal time to get the patient
to pay deductibles, co-payments, co-insurances, and deposits is at pre-
admission or admission, before any health care services are provided. Once
the patient is admitted and medical services are rendered, or at discharge, or
after discharge when the patient is at home, the sense of urgency is gone and
it is much harder for the hospital or doctor to collect any outstanding debts.
The sense of urgency is greatest before any health care is delivered and is the
best time to collect monies owed by the patient.
2. Follow-up policies for the hospital or doctor to collect payments from the
patient must be established and the patient should be informed of these
policies. This improves the hospitals public relations.
3. Make sure public relations concerns are taken into account when getting
payments from the patient. Insure repeat business for the hospital and doctor
with a satisfed patient.
4. Policies for charity care and discounts for the patient are clearly known.
Again, these help improve the hospitals or doctors public relations image
with the patient and their families.
5. Policies for charging interest are clearly understood by the patient and/or
guarantor.
6. Policies to collect outstanding balances from the patient, whether they are
collectible or bad debt, and cancelling bad debt, should be clearly stated.
The Health Care Revenue Cycle 202
Statute of Limitations
1. Statute of Limitations is defned as the amount of time (which varies from
state to state) in which a claim against the patient, for outstanding monies
owed to the hospital or doctor, must be collected before it is considered paid
or uncollectible.
2. The Statute of Limitations is in effect when:
If the patient owes money, get the patient to sign a written "Promise to
Pay" document making it a legal obligation. At this point, the Statute
of Limitations is in effect as there will be a legally established period
of time the patient has to pay the debt, before it goes to a debt collector
for non-payment. The "Promise to Pay" helps with the doctor's or
hospital's efforts at good public relations. For example, the patient signs
the "Promise to Pay" and agrees to pay $100 every month for the next 6
months until their balance of $600 is satisfed.
Get the patient to pay a partial payment on the amount owed, which
legally binds the patient to the whole debt owed, and the patient is
now obligated to pay the entire debt. Once a partial payment has been
documented, the Statute of Limitations in legally in effect as the patient
has a certain period of time to pay the rest of the debt, otherwise the debt
goes to a collection agency.
Collection Calls to the Patient and Collection Policies
1. The primary purpose of placing a collection (telephone) call to the patient
or guarantor is to get payment in full of the outstanding balance. Make
sure all facts and questions are prepared in advance by the debt collector.
Repeated telephone contact is more effective than letter writing.
2. A written collection policy should include:
Standards to be used to pursue and follow-up on the patient's account.
Time limits when the account should be considered uncollectible.
Third Party Collection Agencies
Third Party Collection Agencies are involved in collecting outstanding debts owed
by the patient. By capturing as much money owed as is possible by debt collecting
agencies, which are hired by the hospital (the hospital is the frst party, the patient is
the second party, the collection agency is the third party), cash fow is improved and
accounts receivable (A/R) are reduced. It is important in the account aging process,
which is the amount of time a debt is owed by the patient to the doctor or hospital,
is kept to a minimum. The longer a debt is owed, the longer the aging process (30 to
60 to 90 days), the less chance the hospital or doctor have of being receiving payment
from the patient.
1. Common reasons the bill is not paid on time by the insurance company, or
patient does not pay their debt, are as follows:
Never received the hospital or doctor's bill
Chapter 5 - Doctor/Hospital Financial Matters 203
Coordination of Benefts (COB) problems by insurance companies and
Medicare
Medical chart review requested by the insurance company; Peer Review
Organixation (PRO) requirements
Insurance claim forms have invalid or incomplete information, coding
problems, wrong insurance numbers, etc.
Referral forms, authorization, and pre-certifcation requirements are
invalid or incomplete
Time requirements were not met to fle claims, legal adjudication
problems (the workers' compensation or motor vehicle accident [MVA]
case may take years to settle and health care bills paid)
Workers' compensation, Application for Benefts, and other forms not
received or invalid or incomplete
2. When attempting to collect a patients outstanding debt, work the accounts
from the highest amount owed to the lowest.
Charity Care, Indigent Patient, and Bad Debt
1. Charity Care is defned when hospital or doctors services are provided and
payment is never expected. Charity care is considered providing health care
services free of charge to those patients who meet certain fnancial criteria.
2. An Indigent Patient has no way of paying for health care services and is not
eligible for Medicaid or Public Assistance.
3. Bad Debt is money that cannot be collected from the patient or guarantor
resulting from giving the patient or guarantor credit. Bad debt includes a
patient who defaults (simply does not or refuses to pay) their medical bill,
patient that SKIPS, patient that fles bankruptcy without assets, or a patient
that has insolvent assets (the patient dies and whose estate has no money).
Judgment, Lien and Tort Liability
1. A Judgment is a legally binding claim against a debtor (patient) issued by a
court.
2. A Lien is a recorded claim (written and legally binding) against the patients
real and personal property as a result of a debt (money owed the hospital by
the patient). A lien occurs after a judgment has been issued.
3. Tort Liability is a legal obligation as a result of an injury or other damage
done by one person to another (as a result of a breach, or breaking, of legal
duty). This could include a car accident, falling on someones property, one
person injuring another, not fulflling the terms of a contract, etc.)
Courtesy Discharge
1. When the patient or guarantor has met all their fnancial obligations (and a
payment schedule has been worked out) to the hospital, a courtesy discharge
occurs where the patient is permitted to leave the hospital without going
through the usual discharge formalities.
The Health Care Revenue Cycle 204
2. Advantages: Improves pubic relations for the hospital; patient can leave the
hospital in a more controlled fashion at their convenience when the hospital
is not busy.
Improves patient fow through the hospital, opens up more hospital beds
and facilities.
By providing courtesy discharge at non-peak times, the need for
additional staff is reduced. This avoids "rush hour" type of patient
discharge.
Allows for greater accuracy in billing because patient's fnancial
considerations are determined in advance of discharge.
Calculations
Average Daily Revenues and Average Days of Revenue in Ac-
counts Receivable (ADRR)
Average Daily Revenues = Average Amount of Revenue (money or charges)
generated by the hospital for a specifc period of time.
Formula =
Total Amount of Money and Charges ($) Generated For a specifc number of days
Total number of days (for example, number of days in January 2010)
For Example:
January 2009 Revenue / Charges = $3,000,000
(January has 31 days)
February 2009 Revenue / Charges = $2,600,000
(February has 28 days)
March 2009 Revenue / Charges = $2,000,000
(March has 31 days)
Total for Jan., Fe b., Mar. 2009 = $5,600,000
(Jan., Feb., Mar. have a total of 90 days)
Total Money/Charges
Total Number of Days
$5,600,000
90 Days
= = $62,222
Therefore, $62,222 is generated for each day the hospital was in business. This is
equal to the Average Daily Revenues.
$62,222 represents the average amount of money the hospital generates per
day for 90 days for January 2009, February 2009 and March 2009.
Average Days of Revenue in Accounts Receivable also known as AR Days
Outstanding or ADRR. This number is an estimate, using average current revenues
Chapter 5 - Doctor/Hospital Financial Matters 205
(amount of money made), of the days required to turn over the accounts receivable
(earn enough money to equal the A/R), under the hospitals normal operating
conditions (the hospital is providing the usual treatment and services to patients).
The Accounts Receivable or A/R is the amount of money the hospital is owed
(balance) from providing services to patients.
Warning. This is a diffcult fnancial concept telling the accountants in the
hospital how long it will take the hospital to earn the money that the hospital
is owed by patients and insurance carriers and Medicare, who have yet to
pay their bills for the medical treatment and products it has provided to
them. In this case, it will take the hospital working for 144.6 days to earn
$9,000,000, which is the accounts receivable, or the amount of money it is
owed as of 3/31/09.
Accounts Receivable at a Specifc Time
Average Daily Revenue
= ADRR =
Required to turnover
(collect or earn) the A/R
under the hospitals normal
operating conditions
For example: The Accounts Receivable (A/R) is $9,000,000 as of March 31,
2009; this is the amount of money that is OWED to the hospital as of 3/31/09 from
providing health care services to patients.
The average daily revenue from Jan., 2009, Feb., 2009 and March, 2009 =
$62,222 (see Average Daily Revenues above)
Therefore,
$9,000,000
$62,222
A/R =
Average Daily Revenue =
= 144.6 Days Outstanding
the average number of days (144.6) necessary for the hospital to generate the
$9,000,000 (A/R) from providing health care service to patients.
The Health Care Revenue Cycle 206
Abbreviations and Acronyms
ADRR Average Days of Revenue in Accounts Receivable or AR Days
Outstanding
APR Annual Percentage Rate
A/R Accounts Receivable
COB Coordination of Benefts
CRA Credit Reporting Act
ECOA Equal Credit Opportunity Act
FCRA Fair Credit Reporting Act (Title VI of the Consumer Credit Protection
Act)
FDCPA Fair Debt Collection Practices Act (Title VIII of the Consumer Credit
Protection Act)
FTC Federal Trade Commission
HHS Health and Human Services
MVA Motor Vehicle Accident
PACER Is a national computer system used to verify bankruptcy
PHI Protected Health Information
PIN Personal Information Number
Regulation Z The Truth in Lending Act (TLA) (Title I of the Consumer Credit
Protection Act)
SKIP When a debtor cannot be located by the creditor
SSN Social Security Number
VCIS Voice Case Information System
Chapter 5 - Doctor/Hospital Financial Matters 207
Sample Test Questions
These questions emphasize the various pieces of legislation covered in this chapter,
including their various names and acronyms and what they represent, plus the four
types of bankruptcy. These 65 questions should be answered in 65 minutes or less.
1. _______________bankruptcy is for farmers.
A. Chapter 7
B. Chapter 11
C. Chapter 12
D. Chapter 13
E. Involuntary Bankruptcy
Answer: C
2. ______________ bankruptcies are for individuals, excluding farmers.
A. Chapter 7
B. Chapter 11
C. Chapter 12
D. Chapter 13
E. A and D
F. B and C
Answer: E
3. Once the doctor or hospital receives notice from the court of a patients
bankruptcy, all collection efforts must:
A. Stop
B. Continue
C. May continue if the doctor or hospital desire to do so.
D. Stop, then continue, then stop again at the decision of the doctor or hospital.
Answer: A
4. The ___________ is the one who is owed money by the patient for health care
services rendered.
A. Creditor
B. Debtor
C. Hospital or Doctor
D. A and C
E. B and C
Answer :D
5. Concerning involuntary bankruptcy:
A. The debtor can only be forced into Chapter 7 or 11 bankruptcy by the
creditor.
B. If more than 12 creditors, at least three creditors must be owed more than
$5,000 each to force involuntary bankruptcy.
C. If less than 12 creditors, then only one creditor must be owed at least $10,775
to force involuntary bankruptcy.
D. All of the above.
E. None of the above.
Answer: D
The Health Care Revenue Cycle 208
6._____________ bankruptcy is for individuals with a regular income who cannot
currently pay their debts but want to.
A. Chapter 7
B. Chapter 11
C. Chapter 12
D. Chapter 13
Answer: D
7. Chapter 13 bankruptcy allows the debtor to pay creditors, in installments, over
a ___________ period of time but can be extended to a _____________ period
of time if approved by the bankruptcy judge. Creditors __________ continue
to pursue collection activities during the Chapter 13 bankruptcy repayment
period.
A. 5 year, 3 year, can
B. 3 year, 5 year, cannot
C. 1 year, 3 year, can
D. 3 year, 7 year, cannot
Answer: B
8. _________________ is also known as reorganization bankruptcy and
is designed for _________________ who continue to function, work out a
repayment plan, and pay back their creditors.
A. Chapter 7, individuals
B. Chapter 11, businesses
C. Chapter 12, farmers
D. Chapter 13, individuals
Answer: B
9. The Truth in Lending Act:
A. is also known as Title I of the Consumer Credit Protection Act
B. is also known as Regulation Z
C. is also known as the Truth in Lending Consumer Credit Cost Disclosure Act
D. means the APR and fnance charges must be clearly identifed to the
consumer
E. means the disclosure of credit is made in writing and the consumer receives
a copy
F. All of the above
G. A, C, E
Answer: F
10. _______________ is where the court rules that the debtors (patient) bankruptcy
is ended or cancelled.
A. Discharge of Debtor
B Regulation Z
C. Dismissal of Bankruptcy
D. VCIS
E. Chapter 7
Answer: C
Chapter 5 - Doctor/Hospital Financial Matters 209
11. _____________ is where the patient or guarantor is legally no longer
responsible for paying the debts owed to the listed creditors in the bankruptcy
petition.
A. Discharge of Debtor
B. Regulation Z
C. Dismissal of Bankruptcy
D. Fair Credit Billing Act
E. FDCPA
Answer: A
12. The FDCPA:
A. Is Title VIII of the Consumer Credit Protection Act
B. Prohibits harassment or abuse in the collection process
C. Prohibits the use of false or misleading information in the collection process
D. Prohibits communication with the debtor before 8AM or after 9PM
E. Prohibits communication with debtor if there is an attorney or at the debtors
place of employment, unless prior approval has been given
F. All of the above
G. B, D, E
Answer: F
13. According to the Fair Credit Billing Act, the patient must notify the hospital
of any errors within __________ after the statement has been mailed to the
patient, and the hospital has _______________ to correct the error or prove the
accuracy of the bill to the patient.
A. 90 days, 60 days
B. 60 days, 90 days
C. 30 days, 60 days,
D. 3 months, 2 months
E. None of the above
Answer: B
14. The FCRA:
A. Is known as Title VI of the Consumer Credit Protection Act
B. Is enforced by the FTC
C. Promotes accuracy and insures privacy of information used in consumer
reports
D. Oversees the activities of CRAs
E. All of the above
F. B, C, D
Answer: E
15. A ___________ SKIP is a patient who moves or changes their address, but fails
to notify creditors, but a forwarding address is normally on fle.
A. False
B. Un-intentional
C. Intentional
D. Deceased
Answer: B
The Health Care Revenue Cycle 210
16. A __________ SKIP is caused by a clerical error such as mixed up numbers on
the street address, incorrect zip code, or missing information.
A. False
B. Un-intentional
C. Intentional
D. Deceased
Answer: A
17. SKIP tracing resources include:
A. Internet
B. Landlord or Mortgage holder
C. Employers, Relatives, Neighbors
D. Telephone Directories
E. All of the above
F. B and C
Answer: E
18. ____________ makes the reporting of delinquent data more consistent and
clear, creates safe harbors for debt collectors and those businesses who provide
information to debt collectors.
A. FCRA
B. FDCPA
C. Fair and Accurate Credit Transaction Act
D. Regulation Z
E. Chapter 11
Answer: C
19. ____________ represents the average amount of money the hospital generates
from providing health care services to patients over a specifc period of time,
for example, 90 days.
A. ADRR
B. Average Daily Revenue
C. FDCPA
D. Intentional SKIP
E. A/R
Answer: B
20. ___________ represents an estimate, using average current revenues (money
generated) of the days required to turn over the accounts receivable under the
hospitals normal operating conditions.
A. ADRR
B. Average Daily Revenues
C. FDCPA
D. Intentional SKIP
E. A/R
Answer: A
Chapter 5 - Doctor/Hospital Financial Matters 211
21. ___________ is a legally binding claim against a debtor issued by a court.
A. Lien
B. Tort Liability
C. Judgment
D. A/R
E. SKIP
Answer: C
22. ___________ is a recorded claim (written and legally binding) against the
patients property as a result of a debt.
A. Lien
B. Tort Liability
C. Judgment
D. A/R
E. SKIP
Answer: A
23. _____________ is a legal obligation as a result of an injury or other damage
done by one person to another person.
A. Lien
B. Tort Liability
C. Judgment
D. A/R
E. SKIP
Answer: B
24. A ____________ is a debtor who cannot be located by a creditor.
VCIS is the acronym for:
A. Courtesy Discharge; Voice Case Information System
B. Tort Liability; Vicarious Caseload Information System
C. Judgment; Voice Case Informed System
D. A/R; Vacated Case Information System
E. SKIP; Voice Case Information System
Answer: E
25. A ____________ is when a patient or guarantor has met all their fnancial
obligations to the hospital and is permitted to leave the hospital without going
through the normal discharge formalities.
A. Courtesy Discharge
B. Indigent
C. Judgment
D. A/R
E. SKIP
Answer: A
The Health Care Revenue Cycle 212
26. ______________ has no way of paying for health care services and is not
eligible for Medicaid or Public Assistance.
A. Courtesy Discharge
B. Indigent Patient
C. Bad Debt
D. A/R
E. Aging Account
Answer: B
27. ____________ is money that cannot be collected from the patient or guarantor
from giving credit to the patient or guarantor.
A. Charity Care
B. Indigent Patient
C. Bad Debt
D. A/R
E. Judgment
Answer: C
28.______________ is when a hospitals or doctors services are provided and
payment is never expected.
A. Charity Care
B. Indigent Care
C. Bad Debt
D. A/R
E. Lien
Answer: A
29. An ______________ is the amount of time an outstanding debt is owed by the
patient to the hospital, for example, 30 or 60 or 90 days.
A. Lien
B. Bad Debt
C. Aging Account
D. Involuntary Bankruptcy
E. Average Daily Revenues
Answer: C
30. _____________ is Title VI of the Consumer Credit Protection Act.
A. FCRA
B. FDCPA
C. A/R
D. Regulation Z
E. ADRR
Answer: A
Chapter 5 - Doctor/Hospital Financial Matters 213
31. ____________ is Title VIII of the Consumer Credit Protection Act.
A. FCRA
B. FDCPA
C. A/R
D. Truth in Lending Act
E. Regulation Z
Answer: B
32. ____________ is Title I of the Consumer Credit Protection Act.
A. FCRA
B. FDCPA
C. A/R
D. Truth in Lending Act
E. Regulation Z
F. D and E
G. B and C
Answer: F
33. Advantages of a courtesy discharge include:
A. Better PR for the hospital and doctor
B. Patient can leave the hospital in a more controlled fashion
C. Improves patient fow through the hospital
D. Reduces the amount of hospital staff required to discharge the patient
E. A and B
F. All of the above
Answer: F
34. The best time for the hospital to collect deposits, deductibles, co-payments, and
co-insurances from the patient or guarantor is:
A. At discharge
B. When the patient is already admitted to the hospital
C. At Admission
D. At Pre-admission
E. Does not matter
Answer: D
35. Debts that are not included in the bankruptcy petition ____________be
eliminated when the bankruptcy is granted.
A. Will
B. Will Not
C. May not
D. Cannot be
Answer: B
The Health Care Revenue Cycle 214
36. _____________ is where the debtors assets are liquidated to pay the creditors.
A. Chapter 13
B. Chapter 12
C. Chapter 11
D. Chapter 7
E. Involuntary Bankruptcy
Answer: D
37. Most ____________ bankruptcies cases wind up as Chapter 7 bankruptcies.
A. Chapter 13
B. Chapter 12
C. Chapter 11
D. Chapter 7
E. Involuntary Bankruptcy
Answer: C
38. When the debt collector is working outstanding debts owed by patients to the
hospital, try to collect debts with the _____________ balances frst.
A. Lowest
B. No
C. Highest
D. Minimal
Answer: C
39. The FTC enforces the ___________ and regulates the activities of CRAs.
A. FCRA
B. Fair and Accurate Credit Transaction Act
C. FDCPA
D. ADRR
E. Regulation Z
Answer: A
40. ___________ are used to determine whether credit should be extended to an
applicant, for credit checks for employment, for legal matters, or connected
with business transactions such as buying a car or a house.
A. FCRA
B. FDCPA
C. CRAs
D. Judgment
E. Fair Credit Billing Act
Answer: C
41. The Truth in Lending Act:
A. Is AKA Regulation Z
B. Is AKA Consumer Credit Protection Act
C. Is AKA Truth in Lending Consumer Credit Cost Disclosure Act
D. Is AKA FDCPA
E. A, B, C
F. B, C, D
Answer: E
Chapter 5 - Doctor/Hospital Financial Matters 215
42. The FDCPA prohibits the debt collector from contacting the debtor:
A. Between 8AM and 9PM, in the debtors time zone
B. Before 8AM and after 9PM, in the debtors time zone
C. At the place of the debtors employment, unless the debt collector is given
permission
D. A and B
E. B and C
Answer: E
43. The ________________ is the amount of time, varying from state to state, in
which a claim against a patient (debtor) for outstanding monies owed to the
hospital for services rendered, must be paid before it is considered paid or
uncollectible.
A. Fair Credit Billing Act
B. Statute of Limitations
C. Average Daily Revenues
D. ADRR
E. Judgment
Answer: B
44. SKIP tracing resources include:
A. Internet
B. Telephone Directories
C. Employer, Neighbors, Family
D. Mortgage Holder or Landlord
E. All of the above
F. A, B, and D
Answer: E
45. Regulation Z includes:
A. Disclosure of information to the consumer, in writing, before credit is given
to the consumer
B. APR and fnance charge must be clearly written and obvious to the consumer
C. Prohibits harassment and abuse of the debtor by the debt collector
D. If more than one creditor is involved in getting credit, all the creditors must
agree on one creditor who will comply with the APR, fnance charge, and
other terms of the credit
E. A, B, C
F. A, B, and D
Answer: F
The Health Care Revenue Cycle 216
46. When the doctor or hospital has to confrm a patients bankruptcy, the
following are employed:
A. VCIS
B. SKIP
C. Pacer
D. Contacting District Clerks offce or confrming the bankruptcy in the
newspaper
E. Contacting the patients attorney handling the bankruptcy
F. A, C, D and E
G. A, B, C
Answer: F
47. A ____________ is a patient who owes money to the hospital which is called
the ___________.
A. Debtor, Creditor
B. Creditor, Debtor
C. SKIP, Judgment
D. Auction, Creditor
E. Lien, Debtor
Answer: A
48. Average amount of revenues generated by the hospital over a specifc period of
time is called:
A. ADRR
B. Average Daily Revenues
C. Average Days of Revenue in Accounts Receivable
D. VCIS
E. FCRA
F. AR Days Outstanding
Answer: B
49. An estimate, using average current revenues (of the hospital), of the days
required to turn over the accounts receivable under normal operating
conditions, is called:
A. ADRR
B. Average Daily Revenues
C. Average Days of Revenue in Accounts Receivable
D. VCIS
E. FCRA
F. AR Days Outstanding
G. A,C,F
H. A,D,E
Answer: G
Chapter 5 - Doctor/Hospital Financial Matters 217
50. ____________ occurs when someone uses the patients protected health
information without the patients knowledge or consent to obtain treatment or
receive payment for medical services.
A. ADRR
B. Average Daily Revenues
C. Medical Identity Theft
D. SKIP
E. Coordination of Benefts
Answer: C
51. Medical Identity Theft can result in:
A. Erroneous entries made into the patients medical records
B. Production of fctitious medical information in the patients name
C. Take years to correct
D. Affect the treatment given to the patient and risk the patients health
E. Adversely effect the consumer getting life, health and disability insurance
F. All of the above
G. A, C, D
Answer: F
52. ______________ of the Consumer Credit Protection Act is AKA The Truth in
Lending Act or _______________.
A. Title VI, Regulation A
B. Title VIII, Regulation Z
C. Title I, Regulation Z
D. Title V, Regulation Y
Answer: C
53. ___________ of the Consumer Credit Protection Act is known as The Fair Debt
Collection Practices Act. ___________ does not allow creditors to discriminate
against applicants on the basis of sex, marital status, race, or religion or
because they receive public assistance or have exercised their rights under the
Consumer Credit Protection Act.
A. Title VIII, ECOA
B. Title VII, FDCPA
C. Title I, ECOA
D. Title VI, FCRA
E. Title V, TLA
Answer: A
54. __________ of the Consumer Credit Protection Act is AKA Fair Credit
Reporting Act, and expands rights and places additional requirements on
_______.
A. Title VIII, FDCPA
B. Title I, FDCPA
C. Title VI, SKIP
D. Title VI, CRA
E. Title I, CRA
Answer: D
The Health Care Revenue Cycle 218
55. The primary objective of the debt collector making a collection telephone call
is to request payment of the patients outstanding balance ____________.
A. in time.
B. in part.
C. in full
D. according to a new repayment schedule
E. to determine if this is a charity case
Answer: C
56. Collection calls are regulated by the guidelines established by:
A. HIPAA
B. FCRA
C. ADRR
D. FDCPA
E. Regulation Z
Answer: D
57. Financially distressed companies can use which bankruptcy code to establish a
repayment schedule with their creditors?
A. Chapter 7
B. Chapter 11
C. Chapter 12
D. Chapter 13
E. Regulation Z
Answer: B
58. Before a patients account is sent to a debt collection agency, you must have:
A. Proof the patient received a valid and verifed medical service
B. Multiple attempts to contact the patient by phone and mail
C. The diagnosis, prognosis and coding are confrmed
D. The patients medical records are properly stored
E. None of the above
Answer: A
59. The following piece of legislation defnes SKIP and SKIP tracing resources:
A. FDCPA
B. The Truth in Lending Act
C. Regulation Z
D. Fair and Accurate Credit Transaction Act
E. FCRA
Answer: D
60. A clerical error in the debtors address or phone number is known as a
______________.
A. Intentional SKIP
B. Unintentional SKIP
C. False SKIP
D. Late SKIP
Answer: C
Chapter 5 - Doctor/Hospital Financial Matters 219
61 A patient who is medically indigent is:
A. Has the ability to pay for medical services
B. Does not have the ability to pay for treatment
C. Does not have the ability to pay and is not eligible for Medicaid or Public
Assistance
D. Doctors services are provided and payment is not expected
E. None of the above.
Answer: C
62. When the patients account has a balance for medical treatment rendered,
but has passed timely fling limits, the Statute of Limitations has passed, the
doctor or hospital:
A. Rebills the insurance carrier or Medicare for what the patient owes
B. Bills the patient again
C. Asks the debt collection agency to begin collection activities
D. Do not bill the patient, and write-off the debt as uncollectible
E. All of the above
Answer: D
63. The defnition of bad debt versus charity care is:
A. The patient wont pay compared to the patient cant pay
B. The patient cant pay versus the patient refuses to pay
C. Intentional SKIP versus False SKIP
D. FCRA compared to the FDCPA
Answer: A
64. Money occasionally needs to be ___________ to patients when the practice has
overcharged a patient for a medical service.
A. Discharged
B. SKIP
C. Refunded
D. Kept
E. Not Refunded
Answer: C
65. A bankruptcy dismissal allows for all of the following except:
A. Legal activity to collect the patients account can be pursued by the doctor or
hospital
B. Billing the patient directly for the outstanding balance due can occur
C. Referral of the account to a debt collection agency
D. The patients bankruptcy has been cancelled and is not longer legally in
effect
E. The doctor or hospital can write-off the account as uncollectible as a result of
bankruptcy
Answer: E
End of Chapter 5
Appendix 221
Appendix A: CMS-1500 Form
The Health Care Revenue Cycle 222
Appendix B: UB-04 Form
Appendix 223
Appendix C: Superbill
The Health Care Revenue Cycle 224
Appendix D: Medicare Card
Bio 225
Robert A. Kaplan BA, DC, MBA, CPAT
For the past twenty years, Dr. Kaplan has built and operated three chiropractic offces.
He is NHA certifed as a medical billing and coding specialist. He has lectured students
in anatomy, physiology, dissection, pathology and medical terminology. In addition,
he has taught medical billing and coding and front offce procedures. Because of his
extensive knowledge of the health care industry, hes been interviewed on CBS and
Fox News as well as many well-known radio talk shows. He is a Doctor of Chiropractic
Medicine. He earned his BA in Biology at LaSalle College in Philadelphia and his MBA
in Health Care Administration from Eastern College in St. Davids, PA. Dr. Kaplan is
also dedicated to his volunteer work with senior citizens in the Ever Young Club and
Interac.
Index 227
Index
Symbols
72-Hour Rule .............................................................................. 115
A
Admission, Patient ........................................................................ 50
Admitting Categories, Hospital .................................................... 62
Admitting Protocols, Hospital ...................................................... 71
Advanced Benefciary Notice (ABN) ................................... 70, 142
Ambulatory Payment Classifcation (APC) ................................ 143
Anti-Kickback Statute ................................................................... 20
Average Daily Revenues and Average Days of Revenue in Accounts
Receivable (ADRR) ................................................................ 204
Average Length of Stay (ALOS) .................................................. 52
B
Balanced Budget Act of 1997 (BBA) ........................................... 12
Bankruptcy .................................................................................. 193
Bankruptcy Abuse Prevention and Consumer Protection Act
of 2005 ...................................................................... 195
Chapter 7 ........................................................................ 194
Chapter 11 ....................................................................... 194
Chapter 12 ...................................................................... 194
Chapter 13 ...................................................................... 194
Confrming Bankruptcy by the Doctor or Hospital ........ 195
Discharge of Debtor........................................................ 196
Involuntary Bankruptcy .................................................. 194
Notifcation of Bankruptcy ............................................. 195
BBA
see Balanced Budget Act of 1997 ..................................... 12
Birthday Rule .............................................................................. 112
Bundled Services ........................................................................ 159
C
Census
Average Daily Census ...................................................... 77
defned .............................................................................. 76
Percentage of Occupancy ................................................. 77
Centers for Medicare and Medicaid Services (CMS) ................. 7, 9
CHAMPVA................................................................................... 66
Chargemaster .............................................................................. 116
Civil Monetary Penalties (CMP) .................................................. 19
Civil Monetary Penalties Law (CMP or CMPL) .......................... 12
Claim Form Processing Terminology ......................................... 110
Clean Claim ............................................................................ 53, 54
and the Hospial Registration Staff .................................... 53
Clearinghouse
defned ................................................................................ 6
Clinical Laboratory Improvement Amendment (CLIA) ............. 148
CMS
see Centers for Medicare and Medicaid Services ............... 7
CMS-1500 Claim Form .............................................................. 151
How to Complete the CMS-1500 Claim Form ............... 152
CMS-1500 Form ......................................................................... 221
COBRA
see Consolidated Omnibus Budget Reconciliation Act of
1985 ............................................................................ 13
Coding
defned ................................................................................ 5
Co-insurance ................................................................................... 3
Collection Calls to the Patient and Collection Policies .............. 202
Collection Regulations of the Federal Government .................... 197
Common Working File (CWF) ................................................... 107
Comprehensive Error Rate Testing (CERT) ............................... 143
Consent
defned .............................................................................. 60
Six types ........................................................................... 61
Consolidated Omnibus Budget Reconciliation Act of 1985 (CO-
BRA) ......................................................................................... 13
Continued Health Care Beneft Program (CHCBP) ...................... 68
Coordination of Benefts (COB) ................................................. 140
Courtesy Discharge ..................................................................... 203
CPT-4
see Current Procedural Terminology, 4th edition ............. 16
Current Dental Terminology manual (CDT) ................................ 17
Current Procedural Terminology, 4th edition (CPT-4) ......... 16, 165
Custodial Care ............................................................................... 65
D
Data Mailer ................................................................................. 120
Deceased Patient Notifcation ..................................................... 200
Defense Enrollment Eligibility Reporting System (DEERS) ....... 68
Defcit Reduction Act of 1984 (DEFRA) ..................................... 12
DEFRA
see Defcit Reduction Act of 1984 .................................... 12
Department of Health and Human Services (DHHS) ................. 7, 9
Department of Justice (DOJ) ........................................................ 16
DHHS
see Department of Health and Human Services ................. 7
DRG
see Medicare ................................................................... 115
E
EDI
see National Electronic Data Interchange ........................ 16
Effective Collection Policies ....................................................... 201
Electronix Billing
Electronic Data Interchange: EDI .................................. 119
Emancipated Minor ....................................................................... 61
Emergency Medical Treatment and Active Labor Act
(EMTALA) ................................................................................... 21
Employer Identifcation Number (EIN) .......................................... 7
EMTALA ...................................................................................... 71
Admitting process ............................................................. 71
see Emergency Medical Treatment and Active Labor Act 21
End stage renal disease (ESRD) ................................................. 113
Equal Credit Opportunity Act (ECOA) ...................................... 200
Established Patient
The Health Care Revenue Cycle 228
defned ................................................................................ 5
Evaluation and Management Services (E/M) ............................. 167
F
Fair and Accurate Credit Transaction Act (includes SKIP) ........ 199
Fair Credit Billing Act (1975) ..................................................... 198
Fair Credit Reporting Act (FCRA) (1971) .................................. 199
False Claims Act (FCA) ................................................................ 20
FCA
see False Claims Act ......................................................... 20
Fee-for-service (FFS) ...................................................................... 3
Field Locators ............................................................................. 101
18 Date of Patient or Benefciary Retirement.
Value Codes .................................................................... 102
Completion of the #4 Form Locator in the UB-04 ......... 104
Condition Codes ............................................................. 102
Data Elements ................................................................. 101
ICD-9-CM Codes ........................................................... 103
Important UB-04 Code/FL Defnitions ........................... 101
Occurrence Codes ........................................................... 102
Revenue Codes ............................................................... 103
Financial Concerns, Patient .......................................................... 50
Financial Counselor ...................................................................... 55
Financial Statements ................................................................... 120
Data Mailer ..................................................................... 120
Itemized Statement ......................................................... 120
Superbill ......................................................................... 120
Five Control Points, Registration .................................................. 59
Fraud and Abuse ........................................................................... 18
defned .............................................................................. 18
Department of Justice (DOJ) ............................................ 16
Offce of Inspector General (OIG) ................................... 16
reporting ........................................................................... 19
G
Gatekeeper ................................................................................ 4, 65
General Accounting Principles Applied to Cashier Functions for the
Hospital or Doctor ................................................................... 201
Generally Accepted Accounting Principles (GAAP) ................... 78
Good Samaritan Act ........................................................................ 5
defned ................................................................................ 5
H
Health Care Charges, Categories .................................................. 63
Health Care Common Procedure Coding System (HCPCS) ...... 167
Health Care Coverage in the Military ........................................... 65
Health Care Delivered to the Consumer
Categories ......................................................................... 64
Health Care Practitioner
defned ................................................................................ 5
Health Coverage Protocols ........................................................... 53
Health Insurance Claim Number (HICN or HIC) ....................... 148
Examples of Suffxes used in the HCIN ......................... 148
Health Insurance Portability and Accountability Act of 1996
(HIPAA) .................................................................................... 15
Health Maintenance Organizations (HMOs)
see Managed Care Coverage
60
Health Savings Accounts (HSAs) ................................................. 15
HIPAA
see Health Insurance Portability and Accountability Act of
1996 ............................................................................ 15
HIPAA Security Rule ................................................................. 160
Home Health Care ......................................................................... 65
Hospital Admitting Protocols ....................................................... 71
Hospital Inpatient Beneft Days Coverage .................................... 69
I
ICD-9-CM ..................................................................................... 16
see International Classifcation of Diseases, 9th Revision,
Clinical Modifcations .............................................. 160
ICD-10-PCS .................................................................................. 16
Indemnity ........................................................................................ 3
Inpatient ........................................................................................ 62
defned ................................................................................ 5
International Classifcation of Diseases, 9th Revision, Clinical ........
Modifcation (ICD-9-CM) ................................................. 16, 160
J
JCAHO
see Joint Commission on Accreditation of Health Care Or-
ganizations .................................................................. 74
Joint Commission on Accreditation of Health Care Organizations
(JCAHO) ................................................................................... 74
Judgment, Lien and Tort Liability .............................................. 203
L
Lincoln Act ................................................................................... 20
Long-term Care (LTC) .................................................................. 64
M
Managed Care Coverage
Criteria for Registering Patients ....................................... 60
Managed Care Organization (MCO)
goal ..................................................................................... 3
Health Maintenance Organizations (HMO) ....................... 3
participating providers ........................................................ 3
Point-of-Service Plans ........................................................ 4
Preferred Provider Organizations (PPO) ............................ 3
Medicaid (MCD) ................................................................... 11, 149
Medical Case Management/Utilization Review ........................... 60
Medical Ethics .............................................................................. 18
Medical Identify Theft
Responding to Medical Identity Theft ............................ 191
Medical Identity Theft ................................................................ 190
Preventing and detecting ................................................ 190
Medical Malpractice ................................................................... 146
Medical Necessity
defned ............................................................................ 145
Medical Standards of Care and Malpractice ............................... 146
Index 229
Medical Unlikely Edits (MUE) ................................................... 140
Medicare ............................................................................... 10, 138
Ancillary Services .......................................................... 138
Coordination of Benefts (COB) ..................................... 140
End-stage renal disease (ESRD) ............................... 11, 113
Medical Spell of Illness .................................................... 69
Medicare Secondary Payer (MSP) ................... 70, 112, 159
Medicare Claim Editor (MCE) ....................................... 109
Medicare Deductibles, Co-Payments and Co-Insurances for
2009 .......................................................................... 118
Medicare Determination of Patient Eligibility ................. 69
Medicare DRG Window (The 72-Hour Rule) ................ 115
Medicare Processing of the UB-04 Claim Form ............ 108
Part A ........................................................................ 10, 139
Part B ........................................................................ 10, 139
Part C ........................................................................ 11, 140
Part D ........................................................................ 11, 140
Timely Filing of Claims (UB-04/CMS-1500) Requirements
for Medicare Parts A and B ....................................... 138
Medicare Secondary Payer (MSP) ................................ 70, 112, 159
Medicare Card ............................................................................. 224
Medicare Volume Performance Standard (MVPS) ...................... 14
Medigap ...................................................................................... 140
Military, Health Care Coverage .................................................... 65
CHAMPVA ....................................................................... 66
Continued Health Care Beneft Program (CHCBP) ......... 68
TRICARE ......................................................................... 66
MS-DRGs, Medicare Severity-Diagnosis Related Groups ....... 114
N
NAS
see Non-Availability Statement ....................................... 67
National Correct Coding Initiative (NCCI or CCI) .................... 141
National Drug Code manual (NDC) ............................................. 17
National Electronic Data Interchange (EDI) ................................. 16
National Provider Identifer (NPI) .................................................. 7
National Uniform Billing Committee (NUBC) .......................... 101
New Patient
defned ................................................................................ 5
Non-Availability Statement (NAS) ............................................... 67
Non-participating provider .............................................................. 3
O
OBRA of 1986
see Omnibus Budget Reconciliation Act of 1986 ............. 13
OBRA of 1989
see Omnibus Budget Reconciliation Act of 1989 ............. 13
OBRA of 1990
see Omnibus Budget Reconciliation Act of 1990 ...... 14, 74
Offce for Civil Rights (OCR) ....................................................... 16
Offce of Inspector General (OIG) ................................................ 16
Omnibus Budget Reconciliation Act of 1986 ............................... 13
Omnibus Budget Reconciliation Act of 1989 ............................... 13
Omnibus Budget Reconciliation Act of 1990 ......................... 14, 74
Operation Restore Trust of 1995 (ORT) ....................................... 14
ORT
see Operation Restore Trust of 1995 ................................ 14
Outpatient ...................................................................................... 62
defned ................................................................................ 5
Outpatient Care ............................................................................. 64
P
Participating provider ...................................................................... 3
Patient Bill of Rights ..................................................................... 22
Patient Confdentiality .................................................................. 72
Patient Registration, Admission, and Financial Concerns ............ 50
Patient Self-Determination Act (PSDA) ....................................... 73
Patients Medical Record and Telephone/Verbal Communication in
the Hospital ................................................................................ 72
Performing Provider Identifcation Number (PPIN) ................... 159
Per Member Per Month or PMPM) ............................................... 4
Physician
defned ................................................................................ 5
Physician Direct Services ............................................................. 53
Point-of-Service Plans .................................................................... 4
Point of Service plans (POS)
see Managed Care Coverage
60
Pre-Admitting Patients .................................................................. 57
Pre-Admitting Patients, Disadvantages ........................................ 58
Pre-certifcation
defned ................................................................................ 6
Pre-Certifcation ............................................................................ 59
Preferred Provider Organizations (PPO) ........................................ 4
Preferred Provider Organizations (PPOs)
see Managed Care Coverage
60
Primary Care Provider (PCP) ........................................................ 65
Privacy Act of 1974 ...................................................................... 72
Professional Liability .................................................................... 18
Program for Persons with Disabilities. ......................................... 67
Provider Identifcation Number (PIN) .................................... 6, 159
PSDA
see Patient Self-Determination Act .................................. 73
Q
Quality Improvement Organizations (QIO) .................................. 22
Qui Tam Statute ............................................................................ 20
R
Recovery Audit Contractors (RAC) ............................................ 143
Registering Patients with Managed Care Coverage ...................... 60
Registrar
Five Control Points ........................................................... 59
Registration, Patient ...................................................................... 50
Registration Staff, Responsibilities ............................................... 52
Relative Value Scale (RBRVS) .................................................... 13
Relative Value Unit (RVU) .......................................................... 13
Resource Based Relative Value Scale (RBRVS) ........................ 149
Respite Care .................................................................................. 64
The Health Care Revenue Cycle 230
S
Sarbanes-Oxley Act of 2002 ......................................................... 21
Scheduling, Effective Patient ........................................................ 57
SCHIP
see State Childrens Health Insurance Program ............... 12
Fair Debt Collection Practices Act (FDCPA) (1978) ................. 197
Skilled Nursing Facility Coverage (SNF) ..................................... 69
SKIP and SKIP Tracing Resources ......................................... 199
SOAP Notes and the Patient-Oriented Medical Records ............ 169
Standard Code Sets ..................................................................... 169
Stark Laws .................................................................................... 20
State Childrens Health Insurance Program (SCHIP) ................... 12
Statute of Limitations .................................................................. 202
Superbill .............................................................................. 120, 223
T
Tax Equity and Fiscal Responsibility Act of 1982 (TEFRA) ....... 12
TEFRA
see Tax Equity and Fiscal Responsibility Act of 1982 ..... 12
Test Taking and Study Strategies ................................................. 27
Physicians Identifcation Numbers ................................................ 6
The Truth in Lending Act (TLA) or Truth in Lending Consumer
Credit Cost Disclosure Act (1969) .......................................... 197
Third Party Collection Activity .................................................. 192
Third Party Collection Agencies ................................................. 202
Third Party Reimbursement, Doctors and Hospitals, Types of
Any Willing Provider ..................................................... 170
Capitation ....................................................................... 170
Non-Participating Provider ............................................. 170
Participating Provider ..................................................... 170
Per Diem ......................................................................... 170
Straight Charges or Fee-for-Service (FFS) ..................... 170
TRICARE ..................................................................................... 66
Defense Enrollment Eligibility Reporting System ........... 68
Exclusions to NAS requirements ...................................... 67
TRICARE Extra ............................................................... 66
TRICARE for Life ............................................................ 67
TRICARE Prime .............................................................. 66
TRICARE Standard .......................................................... 66
U
UB-04 Claim Form ............................................................. 100, 222
Electronic version, X12N837 ......................................... 101
Field Locators ................................................................. 101
Important UB-04 Code/FL Defnitions ........................... 101
Medicare Processing of the UB-04 Claim Form ............ 108
Unbundled Services .................................................................... 159
Unique Provider Identifcation Number (UPIN) ..................... 6, 159
W
Waiver of Liability ...................................................................... 146
X
X12N837 Institutional Health Care Claim Transaction .............. 101
Das könnte Ihnen auch gefallen
- Healthcare Coding Billing Reimbursement OverviewDokument130 SeitenHealthcare Coding Billing Reimbursement Overviewsvuhari100% (3)
- Basics of Medical Billing & CodingDokument86 SeitenBasics of Medical Billing & CodingRic Sánchez100% (3)
- Introduction To The Medical Billing ProcessDokument34 SeitenIntroduction To The Medical Billing ProcessSohailRaja100% (5)
- Plugin-Introduction To CPT Medical Billing 101Dokument47 SeitenPlugin-Introduction To CPT Medical Billing 101fiesty7983% (6)
- Newman's Billing and Coding Technicians Study GuideVon EverandNewman's Billing and Coding Technicians Study GuideBewertung: 4.5 von 5 Sternen4.5/5 (2)
- Training Manual (New)Dokument16 SeitenTraining Manual (New)fahhad lashari100% (3)
- Coding and Billing BasicsDokument33 SeitenCoding and Billing BasicsGinwong100% (3)
- Medical Billing ProcessDokument24 SeitenMedical Billing ProcessNajamHass100% (5)
- How to Open & Operate a Financially Successful Medical Billing Service With Companion CD-ROMVon EverandHow to Open & Operate a Financially Successful Medical Billing Service With Companion CD-ROMNoch keine Bewertungen
- Medical Practice ManagementDokument44 SeitenMedical Practice Managementturki kamal100% (2)
- Coding Denial Tip Sheet - August 3 2021Dokument17 SeitenCoding Denial Tip Sheet - August 3 2021dinesh ram100% (2)
- The Art of Blues SolosDokument51 SeitenThe Art of Blues SolosEnrique Maldonado100% (8)
- Hospital Billing and Coding Process PDFDokument44 SeitenHospital Billing and Coding Process PDFrahul_didoNoch keine Bewertungen
- Medical Billing & Coding Demystified, 2nd EditionVon EverandMedical Billing & Coding Demystified, 2nd EditionBewertung: 4 von 5 Sternen4/5 (1)
- Revenue CycleDokument240 SeitenRevenue CyclePercentage International School100% (2)
- Denial Management HandbookDokument5 SeitenDenial Management HandbooknandyboyNoch keine Bewertungen
- Medical Auditing Training: CPMA®: Practical Application WorkbookDokument27 SeitenMedical Auditing Training: CPMA®: Practical Application WorkbookAnthony El Hage100% (1)
- Basic Revenue Cycle Management Handout 20190522Dokument2 SeitenBasic Revenue Cycle Management Handout 20190522Hannah Pascua100% (1)
- Lectura - Healthcare ReimbursementDokument28 SeitenLectura - Healthcare ReimbursementKatherine Silva100% (2)
- AB202011 Ch09 StudentWorkbookDokument7 SeitenAB202011 Ch09 StudentWorkbookcasti13425% (4)
- AB202011 Ch09 StudentWorkbookDokument7 SeitenAB202011 Ch09 StudentWorkbookcasti13425% (4)
- Medical Billing Best Practices Ebook GreenwayDokument26 SeitenMedical Billing Best Practices Ebook GreenwayKiran KambleNoch keine Bewertungen
- AR AnalysisDokument143 SeitenAR AnalysisSai Teja100% (2)
- Claims Training Powerpoint1 PDFDokument54 SeitenClaims Training Powerpoint1 PDFshashi madishetty100% (1)
- MedicalRecordsManual PDFDokument126 SeitenMedicalRecordsManual PDFnurhaidahNoch keine Bewertungen
- ICD-10-CM/PCS Documentation TipsDokument78 SeitenICD-10-CM/PCS Documentation Tipschristofel100% (2)
- Health Insurance Domain Basics PDFDokument47 SeitenHealth Insurance Domain Basics PDFGautam Kumar DwivedyNoch keine Bewertungen
- Medical Billing TrainingDokument11 SeitenMedical Billing TrainingHarry Canaba100% (1)
- Billing Process ChecklistDokument2 SeitenBilling Process ChecklistSandeep SharmaNoch keine Bewertungen
- Revenue Cycle Management (RCM)Dokument15 SeitenRevenue Cycle Management (RCM)senthil kumar100% (5)
- Icd Jan1Dokument325 SeitenIcd Jan1Riyan NugrahaNoch keine Bewertungen
- Us Healthcare OverviewDokument17 SeitenUs Healthcare OverviewVijju Yadav100% (3)
- Denial Management StepsDokument42 SeitenDenial Management StepsDeepak DpkNoch keine Bewertungen
- Flow ChartDokument8 SeitenFlow ChartiEuvilleNoch keine Bewertungen
- Medical Billing Process: Naveen MajetyDokument21 SeitenMedical Billing Process: Naveen MajetyNaveen KumarNoch keine Bewertungen
- Healthcare Revenue Cycle ManagementDokument6 SeitenHealthcare Revenue Cycle ManagementE-Rad Imaging and Reporting services Pvt LtdNoch keine Bewertungen
- Denials Claims ExplainationDokument3 SeitenDenials Claims ExplainationNaga RajNoch keine Bewertungen
- Training MateriaL RCM (Healthcare)Dokument66 SeitenTraining MateriaL RCM (Healthcare)Naveen Babu100% (1)
- Healthcare AnalyticsDokument43 SeitenHealthcare AnalyticsVaibhav Kalyansingh ChauhanNoch keine Bewertungen
- ACDIS White Paper - How To Review A Medical RecordDokument19 SeitenACDIS White Paper - How To Review A Medical RecordCamille05100% (1)
- EZplayer Operation ManualDokument40 SeitenEZplayer Operation Manualcasti134Noch keine Bewertungen
- Revenue Cycle MGMT in Healthcare 414 v1Dokument426 SeitenRevenue Cycle MGMT in Healthcare 414 v1Pravin DixitNoch keine Bewertungen
- Healthcare Revenue Cycle Management RCM Important Approach That Hospitals Should FollowDokument10 SeitenHealthcare Revenue Cycle Management RCM Important Approach That Hospitals Should FollowMohab FawzyNoch keine Bewertungen
- Health Information Technology Evaluation Handbook From Meaningful Use To Meaningful OutcomeDokument237 SeitenHealth Information Technology Evaluation Handbook From Meaningful Use To Meaningful OutcomeAdrianus Yoga50% (2)
- BA Domain Day-3Dokument53 SeitenBA Domain Day-3Nikhil Satav0% (1)
- Medical Coding OrientationDokument16 SeitenMedical Coding Orientationdrrskhan100% (1)
- ModifiersDokument8 SeitenModifiersKarna Palanivelu100% (6)
- Accenture EMR Markets Whitepaper VfinalDokument16 SeitenAccenture EMR Markets Whitepaper VfinalcapaxtremeNoch keine Bewertungen
- Revenue Cycle ManagementDokument12 SeitenRevenue Cycle ManagementJarjitha ANoch keine Bewertungen
- Revenue Cycle Management A Complete Guide - 2019 EditionVon EverandRevenue Cycle Management A Complete Guide - 2019 EditionNoch keine Bewertungen
- Lending OperationsDokument54 SeitenLending OperationsFaraz Ahmed FarooqiNoch keine Bewertungen
- Healthcare AnalyticsDokument4 SeitenHealthcare Analyticsmakvar7465Noch keine Bewertungen
- Catalogo AWSDokument46 SeitenCatalogo AWScesarNoch keine Bewertungen
- HSBC in A Nut ShellDokument190 SeitenHSBC in A Nut Shelllanpham19842003Noch keine Bewertungen
- Medical Billing Service Marketing PlanDokument20 SeitenMedical Billing Service Marketing PlanPalo Alto Software100% (7)
- Analytics Landscape in Healthcare-1Dokument24 SeitenAnalytics Landscape in Healthcare-1positiveworker88Noch keine Bewertungen
- Revenue Cycle ManagementDokument12 SeitenRevenue Cycle ManagementJarjitha ANoch keine Bewertungen
- Reducing DelaysDokument205 SeitenReducing Delayscasti134Noch keine Bewertungen
- Sourcing Decisions in A Supply Chain: Powerpoint Presentation To Accompany Powerpoint Presentation To AccompanyDokument58 SeitenSourcing Decisions in A Supply Chain: Powerpoint Presentation To Accompany Powerpoint Presentation To AccompanyAlaa Al HarbiNoch keine Bewertungen
- HFMA's Introduction to Hospital Accounting, Fifth EditionVon EverandHFMA's Introduction to Hospital Accounting, Fifth EditionNoch keine Bewertungen
- Information Security Chapter 1Dokument44 SeitenInformation Security Chapter 1bscitsemvNoch keine Bewertungen
- D - MMDA vs. Concerned Residents of Manila BayDokument13 SeitenD - MMDA vs. Concerned Residents of Manila BayMia VinuyaNoch keine Bewertungen
- Wind Energy in MalaysiaDokument17 SeitenWind Energy in MalaysiaJia Le ChowNoch keine Bewertungen
- Understanding the U.S. Health Services System, Fourth EditionVon EverandUnderstanding the U.S. Health Services System, Fourth EditionBewertung: 4 von 5 Sternen4/5 (1)
- Utilization Review Coordinator: Passbooks Study GuideVon EverandUtilization Review Coordinator: Passbooks Study GuideNoch keine Bewertungen
- EPIC InfoDokument8 SeitenEPIC InfoVijay TupakulaNoch keine Bewertungen
- Hcr201 v6 Wk1 Medical Billing Terminology WorksheetDokument2 SeitenHcr201 v6 Wk1 Medical Billing Terminology WorksheetMarissa Marie100% (1)
- Medical Billing Final ProjectDokument293 SeitenMedical Billing Final ProjectNadeem ShahzadNoch keine Bewertungen
- 230 S HelicopterDokument21 Seiten230 S Helicoptercasti134Noch keine Bewertungen
- Ix12 TX Manual EN PDFDokument309 SeitenIx12 TX Manual EN PDFcasti134Noch keine Bewertungen
- 2-1 IP Addresses - Composition, Types and Classes - Free CCNA Study Guide Free CCNA Study GuideDokument5 Seiten2-1 IP Addresses - Composition, Types and Classes - Free CCNA Study Guide Free CCNA Study Guidecasti134Noch keine Bewertungen
- Stage 1 vs. Stage 2 Comparison Table For Eligible Hospitals and Cahs Core Objectives (16 Total)Dokument12 SeitenStage 1 vs. Stage 2 Comparison Table For Eligible Hospitals and Cahs Core Objectives (16 Total)casti134Noch keine Bewertungen
- 1-2 Networking TypesDokument2 Seiten1-2 Networking Typescasti134Noch keine Bewertungen
- Sample Implementation TimelineDokument1 SeiteSample Implementation Timelinecasti134Noch keine Bewertungen
- MOTOR INSURANCE - Two Wheeler Liability Only SCHEDULEDokument1 SeiteMOTOR INSURANCE - Two Wheeler Liability Only SCHEDULESuhail V VNoch keine Bewertungen
- SM Land Vs BCDADokument68 SeitenSM Land Vs BCDAelobeniaNoch keine Bewertungen
- 3412C EMCP II For PEEC Engines Electrical System: Ac Panel DC PanelDokument4 Seiten3412C EMCP II For PEEC Engines Electrical System: Ac Panel DC PanelFrancisco Wilson Bezerra FranciscoNoch keine Bewertungen
- Basic DfwmacDokument6 SeitenBasic DfwmacDinesh Kumar PNoch keine Bewertungen
- A. The Machine's Final Recorded Value Was P1,558,000Dokument7 SeitenA. The Machine's Final Recorded Value Was P1,558,000Tawan VihokratanaNoch keine Bewertungen
- Interruptions - 02.03.2023Dokument2 SeitenInterruptions - 02.03.2023Jeff JeffNoch keine Bewertungen
- Dissertation On Indian Constitutional LawDokument6 SeitenDissertation On Indian Constitutional LawCustomPaperWritingAnnArbor100% (1)
- Sky ChemicalsDokument1 SeiteSky ChemicalsfishNoch keine Bewertungen
- IEC Blank ProformaDokument10 SeitenIEC Blank ProformaVanshika JainNoch keine Bewertungen
- Google App EngineDokument5 SeitenGoogle App EngineDinesh MudirajNoch keine Bewertungen
- Ucm6510 Usermanual PDFDokument393 SeitenUcm6510 Usermanual PDFCristhian ArecoNoch keine Bewertungen
- MMC Pipe Inspection RobotDokument2 SeitenMMC Pipe Inspection RobotSharad Agrawal0% (1)
- HealthInsuranceCertificate-Group CPGDHAB303500662021Dokument2 SeitenHealthInsuranceCertificate-Group CPGDHAB303500662021Ruban JebaduraiNoch keine Bewertungen
- Recommended Practices For Developing An Industrial Control Systems Cybersecurity Incident Response CapabilityDokument49 SeitenRecommended Practices For Developing An Industrial Control Systems Cybersecurity Incident Response CapabilityJohn DavisonNoch keine Bewertungen
- Vangood Quotation - Refrigerator Part - 2023.3.2Dokument5 SeitenVangood Quotation - Refrigerator Part - 2023.3.2Enmanuel Jossue Artigas VillaNoch keine Bewertungen
- SCDT0315 PDFDokument80 SeitenSCDT0315 PDFGCMediaNoch keine Bewertungen
- Ajp Project (1) MergedDokument22 SeitenAjp Project (1) MergedRohit GhoshtekarNoch keine Bewertungen
- TEVTA Fin Pay 1 107Dokument3 SeitenTEVTA Fin Pay 1 107Abdul BasitNoch keine Bewertungen
- CNC USB English ManualDokument31 SeitenCNC USB English ManualHarold Hernan MuñozNoch keine Bewertungen
- Fidp ResearchDokument3 SeitenFidp ResearchIn SanityNoch keine Bewertungen
- A Novel Adoption of LSTM in Customer Touchpoint Prediction Problems Presentation 1Dokument73 SeitenA Novel Adoption of LSTM in Customer Touchpoint Prediction Problems Presentation 1Os MNoch keine Bewertungen
- BYJU's July PayslipDokument2 SeitenBYJU's July PayslipGopi ReddyNoch keine Bewertungen