Beruflich Dokumente
Kultur Dokumente
Acquired Oculomotor Nerve Palsy
Hochgeladen von
Anggraeni ParwatiCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Acquired Oculomotor Nerve Palsy
Hochgeladen von
Anggraeni ParwatiCopyright:
Verfügbare Formate
12/6/13
Acquired Oculomotor Nerve Palsy - EyeWiki
Acquired Oculomotor Nerve Palsy
From EyeWiki
Acquired oculomotor nerve palsy(OMP) is an ocular pathology resulting from damage to third cranial nerve. It can presents in different ways causing somatic extraocular muscle dysfunction (superior, inferior, and medial recti; inferior oblique; and levator palpebrae superioris) and autonomic (pupillary sphincter and ciliary) muscles. (1)
Contents
1 Disease Entity 1.1 1.2 1.3 1.4 1.5 1.6 Disease Etiology Risk Factors General Pathology Pathophysiology A.Lesions at Oculomotor Nucleus (Midbain)
1.7 B.Lesions at Oculomotor Nerve Fascicles (Leaving the 3rd nerve nucleus) 1.8 C.Lesions in the Subarachnoid space 1.9 D.Lesions within the Cavernous Sinus and Superior Orbital Fissure 1.10 E.Lesions within the Orbit 1.11 Primary prevention 2 Diagnosis 2.1 History 2.2 2.3 2.4 2.5 2.6 2.7 Physical examination Signs Symptoms Clinical diagnos Diagnostic procedures
2.8 Laboratory test 2.9 Differential diagnosis 3 Management 4 References
Disease Entity
3rd nerve palsy, partial: 378.51, 3rd nerve palsy, total: 378.52
Disease
Clinical findings of acquired third nerve palsy depend on the affected area of the oculomotor nerve track. It can be divided into partial or complete palsy. Complete 3rd nerve palsy presents with complete ptosis, with the eye positioned downward and outward and unable to adduct, infraduct, or supraduct, and dilated pupil with sluggish reaction. (1) Partial 3rd nerve palsy are more common, and presents with a variable duction limitation of the affected extraocular muscles and with variable degree of ptosis and/or pupil dysfunction. (1)
Etiology
There are many etiologies for oculomotor palsy: vasculopathic process, trauma, compression (e.g. aneurysm) and/or infiltrative (e.g. leukemia), toxic (e.g. chemotherapy).
Risk Factors
Diabetes mellitus, Hypertension, Vasculitis, Trauma, Infections, Tumors
General Pathology
The manifestations depend on the affected area of 3rd nerve track. In some cases, the precise site of the lesion is clear, whereas in others, the location of the lesion is speculative. (2
Pathophysiology
To understand the pathophysiology of the oculomotor nerve palsy it is essential to know its track. The following flowchart presents CN 3 trail with designated description of clinical manifestations
eyewiki.aao.org/Acquired_Oculomotor_Nerve_Palsy#Management
1/4
12/6/13
Acquired Oculomotor Nerve Palsy - EyeWiki
A.Lesions at Oculomotor Nucleus (Midbain)
Usually produce bilateral defects. This is explained by the anatomy of the nucleus. It is divided in subnuclei according to the enervated area. Each superior recti (SR) are enervated by contralateral CN III subnucleus for this reason a nuclear CN III palsy would produce paralysis of the contralateral SR. Both levator palpebrae superioris are innervated by the one subnuclei (central caudal nucleaus) for this reason a nuclear affectation would produce bilateral ptosis. Patients with damage to the oculomotor nuclear complex need not have ipsilateral pupillary dilation, but when involved, it indicates dorsal rostral damage. (2) Mostly caused by ischemia, usually from embolic or thrombotic occlusion of small, dorsal perforating branches of the mesencephalic portion of the basilar artery. (2)
B.Lesions at Oculomotor Nerve Fascicles (Leaving the 3rd nerve nucleus)
Lesions at this level can produce complete or incomplete palsies. The majority of the time it cannot be differentiated from lesion outside of the midbrain. When the lesion is adjacent to CN III nucleus (midbrain) it can produce several manifestations that have been described according to other neurological manifestations. Lesion at the superior cerebellar
eyewiki.aao.org/Acquired_Oculomotor_Nerve_Palsy#Management
2/4
12/6/13
Acquired Oculomotor Nerve Palsy - EyeWiki
peduncle(Nothnagels Syndrome) presents ipsilateral 3rd nerve palsy and cerebellar ataxia. Lesions at the Red Nucleus (Benedikt's Syndrome) are characterized by ipsilateral 3rd nerve palsy and contralateral involuntary movement. Lesion at the crebellar peduncle (Webers Syndrome) produces ipsilateral 3rd nerve palsy and contralateral hemiplegia. It is important to remember that lesions can present combination of these findings depending on the degree of the insult. In addition, although it is classic that CN III separates in superior and inferior ramii at the superior orbital fissure, sometimes lesions at the fascicles can produce isolated dysfunction of either the superior and inferior division. (2) The most common causes are ischemic, hemorrhagic, compressive, infiltrative, traumatic, and rarely, infiltrative and demyelinizating process.
C.Lesions in the Subarachnoid space
This space is defined as the area traveled by the oculomotor nerve between the ventral surfaces of the midbrain to the entrance of the cavernous sinus, also known as the interpeduncular fossa. Oculomotor nerve damage in this area can produce varied presentations. CN III palsy w ith fixed dilated pupil, it is important to recall that pupillary fibers occupy a peripheral location and receive more collateral blood supply that the main trunk of the nerve. (2) This is why they are susceptible to compression (e.g. aneurysm). The most common known etiology is a posterior communicating artery aneurysm. This is a medical emergency. CN III palsy w ithout pupil inv olv ement, as mentioned above pupillary fibers occupy a peripheral location and receive more collateral blood supply that the main trunk of the nerve. (2) For this reason are less susceptible to ischemia.. This is why in most of the cases patients have diabetes mellitus, systemic hypertension, atherosclerosis and in some cases migraine. Nevertheless, compressive masses or aneurysm can also cause it. On the course to the cavernous sinus the CN III rest on the edge of the tentorium cerebelli. The edge of the uncal portion overlies the tentorium for this reason in the setting of increased intracranial pressure this brain section can herniate producing displacement of the midbrain compressing the ipsilateral oculomotor nerve. This causes ipsilateral ophthalmoplegia and mydriasis. The most common cause of uncal herniation is intracranial hemorrhages.
D.Lesions within the Cavernous Sinus and Superior Orbital Fissure
Lesion at these zones can produce isolated CN III palsy, but it is most commonly associated with other cranial nerves dysfunctions. Differentiating between lesions at the cavernous sinus versus the superior orbital fissure can be challenging and sometimes the literatures describe it as sphenocavernous syndrome. It presents as paresis of oculomotor, trochlear and abducens nerves with associated maxillary division of trigeminal nerve, producing pain. This can be caused by primary (direct invasion) or secondary (intracranial/intraorbital lesion compressing these areas) lesions. Most common causes are tumor (e.g. meningiomas) There is another described pathology within the cavernous sinus and superior orbital fissure that presents with painful ophthalmoplegia known as Tolosa Hunt Syndrome. It is described as an idiopathic granulomatous inflammation. This is a diagnosis of exclusion, therefore tumors, metastasis or aneurysm must be ruled out with neuroimaging. Although tumor are the most common causes of lesions at this zone, vascular processes can also produce damages to the structures present in it. Cavernous sinus thrombosis, carotid cavernous fistulas, syphilis, vasculitis, and/or autoimmune connective tissue diseases (e.g. systemic lupus erythematosus) can produce painful ophthalmolegias typical of cavernous sinus syndrome.(2)
E.Lesions within the Orbit
Lesions within the orbit are associated with visual loss, ophthalmopleagia and proptosis. 3rd nerve ophthalmoplegia can be associated with trochlear and abducence nerves palsies. It is important to remember that at the orbit the oculomotor nerve divides into superior and inferior division. This can cause partial oculomotor nerve palsies. Most common etiologies: trauma, masses, inflammation, and/or infiltrative processes.
Primary prevention
Although there are many risk factors, some of them can be controlled to minimized the risk of acquiring oculomotor nerve palsy. It is encouraged to maintaing blood pressure and glycemic control which are the most common causes of vasculopathic third nerve palsy.
Diagnosis
Acquired oculomotor nerve palsy is a clinical diagnosis.
History
The most common ocular manifestations are diplopia and ptosis. In addition, depending on affected section of the third craneal nerve track it can also produce other neurologic manifestations as involuntrary movements, hemiplegia, and altered mental status.
Physical examination
Consist on complete ophthalmic exam including visual acuity, ductions and versions, levator function, pupils reaction to light and to accommodation. In addition, general physical and/or neurological evaluation should be consider.
Signs
The presenting signs depend on the affected area of 3rd nerve track. In some cases, the precise site of the lesion is clear, whereas in others, the location of the lesion is speculative. It can present in different ways causing somatic extraocular muscle dysfunction (superior, inferior, and medial recti; inferior oblique; and levator palpebrae superioris) and autonomic (pupillary sphincter and ciliary) muscles. (1)
Symptoms
Symptoms depends on the location of the lesion. The most common ocular complaint is diplopia secondary to somatic extraocular muscle dysfunction, but pain and ptosis can also me present.
Clinical diagnos
DIagnosis is made by physical examination.
Diagnostic procedures
Acquired oculomotor nerve palsy can be secondary to many etiologies. Nevertheless, neuroimaging is usually done specially if intracraneal pathology is suspected. In a conscious patient presenting with ophthalmoplegia, ptosis and mydriasis a compressive etiology, as an intracraneal aneurysm, must be ruled out. If an intracraneal aneurysm is suspected a computed tomography angiography (CTA) and/or magnetic resonance imaging (MRI) must be done, with a 90% sensitivity in aneurysms of 3mm or greater in diameter, although the gold standard is the digital substraction angiography (DSA).
Laboratory test
If a patient presents with complete oculomotor nerve palsy without pupil involvement it is most likely to be related to ischemic process, but compression and inflammation must be considered. Evaluation and management will vary according to patients systemic illnesses, age, and associated symptoms. Nevertheless, basic workup must be done. This includes the following: vital signs (e.g. blood pressure), complete blood count (CBC), sedimentation rate (ESR), comprehensive metabolic panel (CMP), central nervous system imaging (MRI or CT) can also be used to ruled out acute intracranial pathology, especially if ophthalmoplegia is associated with pain. (2)
eyewiki.aao.org/Acquired_Oculomotor_Nerve_Palsy#Management
3/4
12/6/13
Acquired Oculomotor Nerve Palsy - EyeWiki
Differential diagnosis
Myasthenia Gravis, Thyroid associated orbitopathy, Internuclear ophthalmoplegia, Chronic progressive external ophthalmoplegia, Orbital pseudotumor, Giant cell arteritis
Management
Acquired oculomotor nerve palsy evaluation depends on signs and symptoms, patients age and systemic diseases. Management depends on the presented scenarios. In a conscious patient presenting with ophthalmoplegia, ptosis and mydriasis a compressive etiology, as an intracraneal anurysm, must be ruled out. In the other hand if a patient presents with complete oculomotor nerve palsy without pupil involvement it is most likely to be related to ischemic process, but compression and inflammation must be considered. The majority of complete or incomplete CN III palsy without pupil involvement are secondary ischemic process. These patients observe an improvement after the first 4 weeks with full resolution in 12 weeks of the insult. (9) Those patients presenting with that are left with a residual deficit can submitted to strabismus surgery after 6 of stability to maximize the possibility of spontaneous resolution and surgical outcome. In these cases the main goal of strabismus surgery is to provide alignment in primary and reading position.
References
(1) BCSC Neurophthalmology : Chapter 8 The patient with diplopia. P.228-229 2010-2011. (2) Miller, N and Newman, N. Clinical neuro-ophthalmology 5th edition. P. 1194-1223 (3) Kline, Lanning B. Neuro-Opthalmology. 6th edition. P. 95-105 (4) Kaiser, Peter. MD., Friedman, Neil. MD., Pineda, Roberto. MD. Third cranial nerve palsy. The Massachusetts eye and ear infirmary Illustrated manual of Ophthalmology. 2nd edition. P. 39-41 (5) Bhatt, VR. Naqi, M. Bartaula R., Murukutla S., Misra, S. Popalzai, M., Paramanathan, K. Dai, Q. T cell acute lymphoblastic leukaemia presemting with sudden onset right oculomotor nerve palsy with normal neuroradiography and cerebrospinal fluid. BMJ Case Rep. 2012 Mar 27;2012. (6) Appenzeller S, Veilleux, M. Clarke, A. Lupus. Third cranial nerve palsy or pseudo 3rd nerve palsy of myasthenia gravis? A challenging diagnosis in systemic lupus erythematosus. 2009 Lupus. Aug;18(9):836-40. (7) Chaudhary,N. et al Imaging of Intracranial Aneurysms Causing Isolated Third Nerve Palsy. J. Neuro-Ophthalmol 2009;29:238-244 (8) Trobe,J. Searching for Brain Aneurism in Third Cranial Nerve Palsy. J Neuro-Ophthalmol vol. 29,No.3,2009 pg.171-3 (9) Capo, H., M.D., Warren, F., M.D., Kupersmith, M. , M.D. Evolution of Oculomotor Nerve Palsies. Journal of Clincal Neuro-ophathalmology (12)1:21-25, 1992.
Original article contributed by: Betsy Colon-Acevedo, MD
Retrieved from "http://eyewiki.aao.org/Acquired_Oculomotor_Nerve_Palsy" Categories: Articles | Neuro-ophthalmology/Orbit | Oculoplastics/Orbit This page was last modified on 19 January 2013, at 13:41.
eyewiki.aao.org/Acquired_Oculomotor_Nerve_Palsy#Management
4/4
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- FHHR 013 Red Tag Procedure PDFDokument5 SeitenFHHR 013 Red Tag Procedure PDFN3N5YNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- D. Das and S. Doniach - Existence of A Bose Metal at T 0Dokument15 SeitenD. Das and S. Doniach - Existence of A Bose Metal at T 0ImaxSWNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Strategic Capital Management: Group - 4 Jahnvi Jethanandini Shreyasi Halder Siddhartha Bayye Sweta SarojDokument5 SeitenStrategic Capital Management: Group - 4 Jahnvi Jethanandini Shreyasi Halder Siddhartha Bayye Sweta SarojSwetaSarojNoch keine Bewertungen
- Laudon - Mis16 - PPT - ch11 - KL - CE (Updated Content For 2021) - Managing Knowledge and Artificial IntelligenceDokument45 SeitenLaudon - Mis16 - PPT - ch11 - KL - CE (Updated Content For 2021) - Managing Knowledge and Artificial IntelligenceSandaru RathnayakeNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- VerificationManual en PDFDokument621 SeitenVerificationManual en PDFurdanetanpNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- New Microsoft Office Word DocumentDokument5 SeitenNew Microsoft Office Word DocumentSukanya SinghNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- India Biotech Handbook 2023Dokument52 SeitenIndia Biotech Handbook 2023yaduraj TambeNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- What Are Some of The Best Books On Computer ScienceDokument9 SeitenWhat Are Some of The Best Books On Computer ScienceSarthak ShahNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- A2 UNIT 5 Culture Teacher's NotesDokument1 SeiteA2 UNIT 5 Culture Teacher's NotesCarolinaNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- SXV RXV ChassisDokument239 SeitenSXV RXV Chassischili_s16Noch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Serious Student of HistoryDokument5 SeitenThe Serious Student of HistoryCrisanto King CortezNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Jurnal 1 Ieevee LPF PDFDokument4 SeitenJurnal 1 Ieevee LPF PDFNanda SalsabilaNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Managemant PrincipleDokument11 SeitenManagemant PrincipleEthan ChorNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Digestive System Worksheet 2013 2Dokument3 SeitenDigestive System Worksheet 2013 2contessa padonNoch keine Bewertungen
- BA 4722 Marketing Strategy SyllabusDokument6 SeitenBA 4722 Marketing Strategy SyllabusSri GunawanNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Vishal: Advanced Semiconductor Lab King Abdullah University of Science and Technology (KAUST) Thuwal, Saudi Arabia 23955Dokument6 SeitenVishal: Advanced Semiconductor Lab King Abdullah University of Science and Technology (KAUST) Thuwal, Saudi Arabia 23955jose taboadaNoch keine Bewertungen
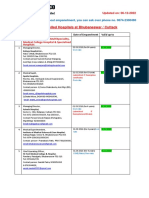
- Empanelled Hospitals List Updated - 06-12-2022 - 1670482933145Dokument19 SeitenEmpanelled Hospitals List Updated - 06-12-2022 - 1670482933145mechmaster4uNoch keine Bewertungen
- San Mateo Daily Journal 01-28-19 EditionDokument28 SeitenSan Mateo Daily Journal 01-28-19 EditionSan Mateo Daily JournalNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- List of Olympic MascotsDokument10 SeitenList of Olympic MascotsmukmukkumNoch keine Bewertungen
- UBMM1011 Unit Plan 201501Dokument12 SeitenUBMM1011 Unit Plan 201501摩羯座Noch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- EDB Postgres Failover Manager Guide v2.1Dokument86 SeitenEDB Postgres Failover Manager Guide v2.1Anggia MauritianaNoch keine Bewertungen
- R15 Understanding Business CyclesDokument33 SeitenR15 Understanding Business CyclesUmar FarooqNoch keine Bewertungen
- 2 - Sample Kids Can Read and Write 2 and 3 Letter Words - Step 2 Final Downloadable Version For Website PDFDokument18 Seiten2 - Sample Kids Can Read and Write 2 and 3 Letter Words - Step 2 Final Downloadable Version For Website PDFsantoshiNoch keine Bewertungen
- Flip The Coin - EbookDokument306 SeitenFlip The Coin - EbookAjesh Shah100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- MSC ACFN2 RD4 ClassDokument25 SeitenMSC ACFN2 RD4 Classmengistu jiloNoch keine Bewertungen
- FKTDokument32 SeitenFKTNeeraj SharmaNoch keine Bewertungen
- JBF Winter2010-CPFR IssueDokument52 SeitenJBF Winter2010-CPFR IssueakashkrsnaNoch keine Bewertungen
- Chapter 13Dokument15 SeitenChapter 13anormal08Noch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- AMO Exercise 1Dokument2 SeitenAMO Exercise 1Jonell Chan Xin RuNoch keine Bewertungen
- Saif Powertec Limited Project "Standard Operating Process" As-Is DocumentDokument7 SeitenSaif Powertec Limited Project "Standard Operating Process" As-Is DocumentAbhishekChowdhuryNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)