Beruflich Dokumente
Kultur Dokumente
Drugs Affecting Different Systems
Hochgeladen von
Dr-Usman KhanCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Drugs Affecting Different Systems
Hochgeladen von
Dr-Usman KhanCopyright:
Verfügbare Formate
Drugs Affecting ANS Cholinergic Drugs 1.
. Cholinergic Agonist: Direct Acting: Cholinergic agonists (also known as parasympathomimetics) mimic the effects of acetylcholine by binding directly to cholinoceptors. Acetylcholine, Pilocarpine, Bethanecol, Carbachol. Indirect Acting: Acetylcholinesterase is an enzyme that specifically cleaves acetylcholine to acetate and choline and, thus, terminates its actions. Inhibitors of acetylcholinesterase indirectly provide a cholinergic action by prolonging the lifetime of acetylcholine. Physostigmine, Neostigmine, Ecothiophate, Rivastigmine, Tacrine. Reactivation of Actylcholine-esterase: Pralidoxime. 2. Cholinergic Antagonist: Antimuscarinic: Commonly known as antimuscarinics, these agents block muscarinic receptors, causing inhibition of all muscarinic functions. Atropine, Scopolamine, Ipratropium. Ganglionic Bolckers: Ganglionic blockers specifically act on the nicotinic receptors of both parasympathetic and sympathetic autonomic ganglia. Except for nicotine, the other drugs mentioned in this category are nondepolarizing, competitive antagonists. Mecylamine, Nicotine. Neuromuscular Bolckers: These neuromuscular blockers are structural analogs of acetylcholine, and they act either as antagonists (nondepolarizing type) or agonists (depolarizing type) at the receptors on the end plate of the neuromuscular junction. Neuromuscular blockers are clinically useful during surgery for producing complete muscle relaxation Atracurium, Doxacurium, Succinylcholine, Tubocurarine. Adrenergic Drugs 1. Agrenergic Agonist: Direct Acting:
These drugs act directly on or receptors, producing effects similar to those that occur following stimulation of sympathetic nerves or release of the hormone epinephrine from the adrenal medulla. Dopamine, Epinephrine, Norepinephrine, Phenylephrine, Sameterol, Terbutaline. Indirect Acting: These agents, which include amphetamine, cocaine and tyramine, may block the uptake of norepinephrine (uptake blockers) or are taken up into the presynaptic neuron and cause the release of norepinephrine from the cytoplasmic pools or vesicles of the adrenergic neuron. As with neuronal stimulation, the norepinephrine then traverses the synapse and binds to the or receptors. Amphetamine, Cocaine, Tyramine. Mixed: Capacity both to stimulate adrenoceptors directly and to release norepinephrine from the adrenergic neuron. Ephedrine, Pseudoephedrine. 2. Adrenergic Antagonist: -Blockers: Drugs that block -adrenoceptors profoundly affect blood pressure. Doxazocin, Prazocin, Terazocin, Tamsulosin. - Blockers: All the clinically available B-blockers are competitive antagonists. Nonselective B-blockers act at both B1 and B2 receptors, whereas cardioselective B antagonists primarily block B1 receptors. Atenolol, Esmolol, Labetalol, Pindolol. NT Uptake or Release: Guanethidine, Reserpine.
CNS Drugs Anti-Parkinsonism Drugs: The disease is correlated with destruction of dopaminergic neurons in the substantia nigra. Levodopa, Carbidopa, Amantidine, Apomorphine, Benzotropine. Alzheimer Drugs: Major cause is loss of Cholinergic neurons.
Memantine, Rivastigmine, Tacrine. Anxiolytic Drugs: a. Benzodiazepenes: Alprazolam, Temazepam, Flurazepam, Lorazepam, Oxazepam. b. Barbiturates: Amobarbital, Phenobarbital, Pentobarbital, Thiopental. c. Other Anxiolytic: Buspirone(mediated by serotonin (5-HT1A) receptors), Hydroxyzine, Anti-depressants. CNS Stimulants: a. Psychomotor Stimulants: Psychomotor stimulants, cause excitement and euphoria, decrease feelings of fatigue, and increase motor activity. Amphetamine, Cocaine, Caffeine, Theobromine. b. Hallucinogens: The hallucinogens, or psychotomimetic drugs, produce profound changes in thought patterns and mood, with little effect on the brainstem and spinal cord. Lysergic Acid Diethylamide, Tetrahydro Cannabinol. CNS Drugs Anti-Depressants: a. SSRIs: Cetalopram, Fluoxetine, Fluvoxamine. b. SNRIs: Duloxetine, Venlafaxine. c. Atypical Ads: Bupropion, Trazodone. d. TCAs (Older SNRIs): Amitryptiline, Imipramine, Trimipramine. e. MAO Inhibitors: The MAO inhibitors may irreversibly or reversibly inactivate the mitochondrial enzyme (gut and liver), permitting neurotransmitter molecules to escape degradation and, therefore, to both accumulate within the presynaptic neuron and leak into the synaptic space.
Phenelzine, Selegiline. f. Anti-Mania & Bipolar Disorders: Valproic Acid, Lithium Salts. Anti-Epileptics: By a variety of mechanisms, including blockade of voltage-gated channels (Na+ or Ca2+), enhancement of inhibitory GABAergic impulses, or interference with excitatory glutamate transmission. Barbiturates, BZDs, Carbamezepine, Gabapentin, Ethosuximide, Levetiracetam, Felbamate, Phenytoin, Zonisamide. CNS Drugs Neuroleptic Drugs (Anti-Psychotic or Major Tranquilizers): They inactivate Dopamine receptors. a. Typical but low potency: Chlorpromazine, Prochlorperazine. b. Typical but high potency: Haloperidol, Thiothixene. c. Atypical: Clozapine, Olanzapine, Risperidone. Opoids: Activation of the opoid receptor decreases the Ca2+ influx and increases the K+ efflux. Decrease Ca+ influx decreases the release of excitatory NT and increased K+ efflux decreases the response of post-synaptic neuron to excitatory NT (Glutamate). a. Strong Agonists: Meperadine, Methadone, Heroine, Fentanyl. b. Moderate/Low Agonists: Codeine, Propoxyphene. c. Partial Agonists: Buprenorphine, Pentazocine. d. Antagonists: Naloxone, Naltrexone. e. Others:
Tramadol.
CVS Drugs Congestive Heart Failure(CHF): a. Renin Angiotensin System Blockers: These drugs block the enzyme that cleaves angiotensin I to form the potent vasoconstrictor angiotensin II. Also diminish the rate of bradykinin inactivation. [Note: Vasodilation occurs as a result of the combined effects of lower vasoconstriction caused by diminished levels of angiotensin II and the potent vasodilating effect of increased bradykinin.] By reducing circulating angiotensin II levels, ACE inhibitors also decrease the secretion of aldosterone, resulting in decreased sodium and water retention. Captopril, Lisinopril, Quinapril, Ramipril, Enalapril (ACE Inhibitors) ARBs are nonpeptide, orally active compounds that are extremely potent competitive antagonists of the angiotensin type 1 receptor. Losartan, Valsartan, Telmisartan (ARBs) b. -Blockers: Atenolol, Metoprolol, Carvedilol. c. Diuretics: Diuretics decrease plasma volume and, subsequently, decrease venous return to the heart (preload). This decreases the cardiac workload and the oxygen demand. Bumetanide, Furesamide, Metolazone, Hydrochlorthiazide. d. Direct Vasodilators: Hydralazine, Isosorbide dinitrate, Sod nitroprusside. e. Inotropic Agents: Enhance cardiac muscle contractility and, thus, increase cardiac output. Digitoxin, Digoxin, Dobutamine, Amrinone. f. Aldosterone Antagonist: Spironolactone. *Dec. Angiotensin II cause dec. Aldosterone which cause decreased water & sod retention. Plasma vol is decreased and hence preload also decreased & BP lowered.
Anti-Arrythmic Drugs: Arrhythmias arise either from aberrations in impulse generation (abnormal automaticity) or from a defect in impulse conduction. a. Na+ Channel Blockers: Quinidine, Procanamide, Propafenone. b. -Blockers: Inhibits Phase 4 depolarization in SA & AV nodes. Esmolol, Propranolol, Metoprolol. c. K+ Channel Blockers: Prolongs Phase 3 repolarization in ventricular muscle fibres. Amiodarone, Sotalol, Dofetilide. d. Ca2+ Channel Blockers: Inhibits action potential in SA & AV nodes. Diltiazem, Verapamil. e. Others: Adenosine, Digoxin.
Anti-Anginal Drugs: a. Organic Nitrates: Nitrates decrease coronary vasoconstriction or spasm and increase perfusion of the myocardium by relaxing coronary arteries. In addition, they relax veins, decreasing preload and myocardial oxygen consumption. Isosorbide dinitrate & mononitrate, Nitroglycerin. b. -Blockers: They decrease the oxygen demands of the myocardium by lowering both the rate and the force of contraction of the heart. Acebutolol, Atenolol, Metoprolol, Propranolol.
c. Ca Channel Blockers: The calcium-channel blockers protect the tissue by inhibiting the entrance of calcium into cardiac and smooth muscle cells of the coronary and systemic arterial beds. Amlodipine, Diltiazem, Verapamil, Nicardipine, Nifedipine.
Anti-Hyperlipidemics: a. HMG CoA Reductase Inhibitors: Analogs of HMG(precursor of Cholesterol). Because of their strong affinity for the enzyme, all compete effectively to inhibit HMG CoA reductase, the rate-limiting step in cholesterol synthesis (de novo synthesis). Atorvastatin, Lovastatin, Provastatin, Simvastatin. b. Fibrates: Gemfibrozil, Fenofibrate. c. Niacin: Niacin strongly inhibits lipolysis in adipose tissue, the primary producer of circulating free fatty acids. d. Bile Acid Sequestrants: Colestipol, Colestyramine, Colesevelam.
e. Cholesterol Absorption Inhibitors: It inhibits intestinal absorption of dietary and biliary cholesterol in the small intestine, leading to a decrease in the delivery of intestinal cholesterol to the liver. This causes a reduction of hepatic cholesterol stores and an increase in clearance of cholesterol from the blood. Ezetimibe.
Anti-Hypertensives: a. Diuretics: They cause increased water and sodium excretion leading to decreased extracellular volume & decreased cardiac output. Bumetanide, Furosamide, Spironolactone, Hydrochlorthiazide. b. -Blockers: Decrease Cardiac Output. Atenolol, Carvedilol, Labetalol, Metoprolol. c. ACE-Inhibitors: ACE inhibitors decrease conversion into angiotensin II and increase bradykinin levels. Vasodilation occurs as a result of the combined effects of lower vasoconstriction caused by diminished levels of angiotensin II and the potent vasodilating effect of increased bradykinin. Captopril, Enalapril,Fosinopril, Lisinopril, Ramipril. d. ARBs: Same As ACEIs but no Cough or Angiodema. Candesartan, Losartan, Telmisartan, Valsartan. e. Ca Channel Blockers: Verapamil, Nifedipine, Nicardipine, Diltiazem, Amlodipine. f. -Blockers: They decrease peripheral vascular resistance and lower arterial blood pressure by causing relaxation of both arterial and venous smooth muscle. Doxazocin, Prazocin, Terazocin. g. Others: Clonidine, Hydralazine, Sod. nitroprusside, Minoxidil, -Methyldopa.
Diuretics: a. Thiazides: These drugs increase the concentration of Na+ and Cl- in the tubular fluid by decreasing the reabsorption of Na in the distal convulated tubule. Chlorothiazide, Chlorthalidone, Indapamide, Hydrochlorthiazide. b. Loop Diuretics: Loop diuretics inhibit the cotransport of Na+/K+/2Cl- in the luminal membrane in the ascending limb of the loop of Henle. Therefore, reabsorption of these ions is decreased. Most efficacious. Bumetanide, Furosamide, Torsemide. c. Potassium Sparing Diuretics: Amiloride, Spironolactone, Triamterene. d. Carbonic Anhydrase Inhibitors: Acetazolamide. e. Osmotic Diuretics: Mannitol, Urea.
Antibiotics (Antimicrobials) Cell Wall Inhibitors: These drugs interfere with the last step of bacterial cell wall synthesis (transpeptidation or cross-linkage), resulting in exposure of the osmotically less stable membrane. Cell lysis can then occur, either through osmotic pressure or through the activation of autolysins. These drugs are thus bactericidal. a. B-lactams: i- Penicillins: Amoxicillin, Ampicillin, Piperacillin, Oxacillin, Methicillin, Nafcillin. ii- Cephalosporins: 1st Generation (Cefadroxil, Cefalexin) 2nd Generation (Cefaclor, Cefoxitin, Cefprozil) 3rd Generation (Cefixime, Cefotaxime, Cefibuten, Ceftriaxone) 4th Generation (Cefepime) iii- Carbapenems: Meropenem, Imipenem. Iv- Monobactam: Aztreonam. b. Other Antibiotics: Bacitracin, Vancomycin, Daptomycin.
Protein Synthesis Inhibitors: a. Tetracyclines: The drug binds reversibly to the 30S subunit of the bacterial ribosome, thereby blocking access of the amino acyl-tRNA to the mRNA-ribosome complex at the acceptor site. By this mechanism, bacterial protein synthesis is inhibited. Doxycycline, Minocycline, Tetracycline. b. Glycylcyclines: Also binds reversibly to the 30S of the ribosomal unit. Tigecycline. c. Aminoglycosides (derived from Streptomyces have -mycin suffixes, whereas those derived from Micromonospora end in micin): Also binds reversibly to the 30S ribosomal subunit & inhibiting protein translation. All aminoglycosides should be given parenterally except neomycin. Amikacin, Gentamicin, Neomycin, Tobramycin, Streptomycin. d. Macrolides/Ketolides: The macrolides bind irreversibly to a site on the 50S subunit of the bacterial ribosome, thus inhibiting the translocation steps of protein synthesis. Azithromycin, Clarithromycin, Erythromycin, Telithromycin. e. Chloramphenicol (50S subunit) f. Clindamycin g. Dalfopristin/Quinupristin (50S subunit) h. Linezolid (binds to a site on the 50S subunit near the interface with the 30S subunit)
Fluoroquinolones: These drugs enter the bacterium by passive diffusion through water-filled protein channels (porins) in the outer membrane and then inhibit the replication of bacterial DNA by interfering with the action of DNA gyrase (topoisomerase II) and topoisomerase IV during bacterial growth and reproduction. Nalidixic Acid, (Ciprofloxacin, Ofloxacin, Norfloxacin), Levofloxacin, Moxifloxacin.
Folate Synthesis Inhibitors: Silver Sulfadiazene, Sulfamethoxazole, Sulfasalazine, Sulfisoxazole.
Folate Reduction Inhibitors: Pyrimethamine, Trimethoprim.
Combination of Above two: Co-trimoxazole.
UTI Antiseptics: Methenamine, Nitrofurantoin(urine discoloration). Where Sulfonamides and Trimethoprim act ?? Pteridine + p-ABA + Glutamate Dihydrofolic Acid Tetrahydrofolic Acid Thymidine Synthesis Dihydrofolic Acid (Sulfonamide) (microbes) Tetra hydro folic Acid (Trimethoprim) (humans) Amino Acid Synthesis + Purine Synthesis +
Antimycobacterials And Antifungals Anti-TB drugs: Isoniazid(altering cell membrane function), Ethambutol(inhibit normal arabinogalactin cell wall), Rifampicin(inhibits synthesis of mRNA), Pyrazinamide(unknown). (1st line drugs) Aminoglycosides, Macrolides, Cycloserine, Ethionamide,. (2nd line drugs)
Anti-Leprosy Drugs: Clofazimine, Dapsone, Rifampin.
Subcutaneous and Systemic Mycoses: Amphitericin B, Fluconazole, Ketoconazole, Micafungin, Capsofungin.
Cutaneous Mycoses: Butoconazole, Griseofulvin, Nystatin, Terbinafine.
Antiprotozoals & Antihelminthics Amebiasis: Chloroquine, Emetine, Dehydroemetine, Metronidazole, Paramomycin.
Malaria: Artemisinin, Primaquine, Pyrimethamine, Mefloquine, Quinine/Quinidine.
Trypanosomiasis: Benznidazole,Suramin, Nifurtimox, Melarsoprol.
Leishmaniasis: Sodium stibogluconate.
Toxoplasmosis: Pyrimethamine.
Giardiasis: Metronidazole, Nitazoxanide, Tinidazole.
Anti-Nematodes (Ascaris, Hookworms, Filarias. Enterobius, Trichinella): Ivermectin, Pyrantel pamoate, Diethylcarbamazine.
Anti-Trematodes (Schistosomes): Praziquantel.
Anti-Cestodes (Tapeworms): Niclosamide, Albendazole.
Anti-Virals Respiratory Virus Infections: Amantadine, Rimantadine, Ribavirin, Zanamivir.
Hepatic Viral Infections: Interferon, Adefovir, Entecavir.
HIV Infections: Abacavir, Didanosine, Etravirine, Fosamprenavir, Tenofovir.
Anti-Cancers Antimetabolites: Methotrexate, Gemcitabine, 6-Mercaptopurine, Cytarabine. Antibiotics: Bleomycin, Doxorubicin, Daunorubicin. Alkylating Agents: Cyclophosphamide, Busulfan, Ifosfamide, Mechlorethamine, Streptozocin.
Microtubule Inhibitors: Docetaxel, Vincristine, Vinblastine, Vinorelbine.
Steroids, Hormones and their Antagonists: Prednisone, Tamoxifen, Estrogens, Goserelin, Letrozole.
Monoclonal Antibodies: Cetuximab, Rituximab. Others: Asparaginase, Interferons, Cisplatin, Etoposide, Imanitib, Topotecan, Oxaliplatin.
Anti-Inflammatory NSAIDs: Aspirin, Diclofenac, Indomethacin, Fenamates, Ibuprofen, Piroxicam, Sulindac. CoX-2 Inhibitors: Celecoxib. Other Analgesics: Acetaminophen. Anti-Arthritis: Adalimumab, Anakinra, Infliximab, Gold salts, D-Penicillamine. Drugs for Gout: Allopurinol, Colchicine, Probenecid, Sufinpyrazone.
Autocoids & Their Antagonists Prostaglandins: Misoprostol.
H1-Antihistamines: H1 receptors present in exocrine excretion, bronchial smooth muscles, intestinal smooth muscles and sensory nerve endings. H1 & H2 receptors present in CVS & Skin. H2 receptors found only in stomach. First Generation (Chlorpheniramine, Diphenhydramine, Dimenhydrinate) Second Generation (Cetrizine, Fexofenadine, Loratadine)
Migraine Headache: Almotriptan, Naratriptan, Riztriptan, Sumatriptan, Zolmitriptan.
Facts to Remember Substance P Blocker: APREPITANT Isoniazid written as INH represents IsoNicotinic acid Hydrazide. Uterus Parts: Fundus; Body; Corporis; Cervix. Fallopian tube connects ovary with uterus. Female Reproductive System: Ovary; Fallopian Tube; Uterus; Vagina. Embryo life cycle: 1-8weeks Fetus: After 8weeks Uterus walls: Endometrium Myometrium; Parametrium. Endo & Myometrial walls involved in the production of Prostaglandins. F2: Vasoconstrictor(dysmenorrhia) E2: Vasodilator (menorraghia) I2: Myometrial relaxation; vasodialtion; anti-platelets. Menarchie: First Periods of a woman (8-16yrs) Avg: 13yrs. Most regularized periods:20-40yrs. Average cycle: 28days (24-36days) Average Flow: 3-7days; Typical Flow: 5days Starts light then heavy then again light. ACEIs contraindicated in bilateral renal artery stenosi. Desmopressine used in nocturnal enuresis. Ovulation: Release of ova from the ovary. Range: Day 8th-20th (14th day). A woman has almost 2000days of periods in her life (400cycles) except pregnancy and illness. Menstrual cycle: Menstruation; Proliferation; Ovulation; Secretory. Menstruation: Day 1-5. Proliferation: Day 6-13. Ovulation: Day 14th. Secretory: Day 15-28.
Graffian Follicle before ovulation secrete estrogen and after ovulation is is known as Corpeus Luteum and secretes Progesterone which develops thick wall of uterus (endometrium). Cervix: Neck of uterus. Basal Body Temperature (BBT):Temp at relaxed body state. Nociceptives: Nerve Endings that sense pain. Anhedonia: An unprovoked stimuli could result in painful sensation normally not painful. Gestational Diabetes: Diabetes that occurs during pregnancy and soon disappears after child birth. Major Adverse effect of Adenosine is Dyspnea. Verapamil is contraindicated with CNS Depressants. Daily dose of Folic Acid is 400-500g. Types of Pain: a. Nociceptive: Pain due to sensitization of nociceptive nerve endings due to certain tissue damage. b. Neuropathic: Any lesion or damage to the nerve fibres, resulting in pain. E.g. Diabetic Peripheral Neuropathy (DPN) c. Mixed: Low back pain; Ankolysing Spondylitis. Mechanism of Feeling pain: a. Reception: Stimulation of nociceptives by PGs. b. Conduction: From Nerve ending to brain. c. Perception: Cortex & Thallamus receive impulse. d. Suffering: Reaction. Pain & Inflammation Mediators: Histamine; Bradykinins; Kinins; Substace P; PGs. PGs increase blood flow to the injury site and accelerate the transfer of WBCs and Platelets. Inflammation: Natural response to the injury to inactivate causative agent. PGs increase vascular permeability and WBCs migration and sensitization of Nociceptives. PAE: The postantibiotic effect (PAE) is a persistent suppression of microbial growth that occurs after levels of antibiotic have fallen below the MIC.
Myasthenia gravis: (Muscle weakness)Autoimmune disorder due to blockade of cholinoceptors by circulating antibodies. Treatment by Neostigmine, physostigmine. Diabetes Type-I: Insulin Dependant; when the body stops making insulin. Also called brittle or labile diabetes. Diabetes Type-II: Non Insulin Dependant; body is making insulin either in insufficient amount or the cells do not respond to body made insulin. Menorrhagia: Excess Blood flow in frequency, duration or amount; upto 80ml. (2030ml) PGE2: Inc. vasodilation; Dec. platelet adhesion & aggregation Inc. Blood Flow. PGF2: Inc. vasospasm; Inc. uterine contractions Painful Menses. Hyperalgesia: Intensed Pain. Articular: Bones & Joints. Non-Articular: Tendons; Ligaments; Bursa.
Epicondyl: Bony projections at the end of long bones. Sprains: Injury to the ligament. Stills Disease: Juvenile Idiopathic Arthritis. In enteral route duodenum is the major site for drug absorption. Bioavailability: Fraction of the drug that reaches the blood stream. Total body water in 70kg human=42litres. Intracellular( 28ltrs) + Interstitial(10ltrs) + Plasma(4ltrs)= 42 litres. Volume of Distribution: Hypothetical volume of fluids into which drug is dispersed. Albumin has the strongest affinity with anionic and hydrophobic drugs. Each cell may have 10,000 receptors e.g. heart has B-receptor for norepinephrine and muscarinic receptor for acetylcholine. Potassium is administered as Slow IV infusions. Receptor: Biological molecule to which drug binding produce measurable response. Receptor Types: a. Ligand gated Ion Channels: GABA (Fastest reception) b. G-protein Coupled: Sildenafil c. Enzyme Linked: Insulin d. Intracellular Receptors: Steroids (Slowest reception) Competitive Antagonism: Same site on same receptor e.g. Prazocin & Norepinephrine.
Non-competitive Antagonism/Allosteric: Different sites on same receptor e.g. Protamine & Heparin. Functional/Physiologic Antagonism: Different receptors involved e.g. Epinephrine & Histamine. Quantal-Dose Response: Study of dose-response on a population that responds. Therapeutic Index: Ratio of toxic dose to effective dose. Drugs with High Therapeutic Index is SAFER to use. Catecholamines have brief duration & rapid onset of action and do not cross BBB. Non-catecholamines have longer duration of action and can be administered orally. Narcolepsy: Narcolepsy is a relatively rare sleep disorder that is characterized by uncontrollable bouts of sleepiness during the day. It is sometimes accompanied by catalepsy, a loss in muscle control, or even paralysis brought on by strong emotions, such as laughter. P450 enzyme INDUCERS: Smoking, Omeprazole, Rifampicin, Carbamazepine, Phenytoin, Phenobarbital. P450 enzyme INHIBITORS: Cimetidine, Fluvoxamine, Isoniazid Quinidine, Macrolides, Chloramphenicol. INR: A laboratory test to called INTERNATIONAL NORMALISED RATIO measures the time it takes for a blood sample to clot and compares it with average clotting time (511min). Average CT measured by Dales method (taking a blood sample in a thin capillary and the end of tube is broken every 30sec until clot formed). Bleeding Time: It is the time until which the blood continues oozing from the injured site(1-5min). Measured by Dukes method (pricking a finger and taking the blood sample every 30sec. on a filter paper until blood stops coming).
Norepinephrine is ineffective orally. Alpha Methyldopa is the only ani-hypertensive used in pregnancy. Major side effect of Doxorubicin is tissue necrosis. Oxidation is Phase-I reaction. In overdosage of Digoxin we use Antidote FAB fragment. Digitoxin toxicity reflects in ECG as to prolong PR interval. Myxodema (Hypothyroidism) treated by Thyroid sodium. Vit A daily dose is 30,000-50,000 IU. Vit C daily dose is 400mg for both men and women. Floxapen (flucloxacillin) is resistant to penicilinnase.
Chelators are drugs that form covalent bonds with cationic metals. Antibiotics showing Conc. dependant flouroquinolones, carbapenems. killing involve aminoglycosides,
While those showing time dependant killing involve -lactams, macrolides, clindamycin. Narrow Spectrum: Covering single or limited group of microbes. e.g Isoniazid. Extended Spectrum: Covering gram +ve and also significant gram ve bacteria. e.g Ampicillin Broad Spectrum: Covering a wie variety of microbes; also the beneficial microbes causing Candida albicans. e.g Tetracyclines, Chloramphenicol. Angina Pectoris: It is a characteristic sudden, severe, pressing chest pain radiating to the neck, jaw, back, and arms. It is caused by coronary blood flow that is insufficient to meet the oxygen demands of the myocardium, leading to ischemia. Stable Angina(Typical): It is characterized by a burning, heavy, or squeezing feeling in the chest. It is caused by the reduction of coronary perfusion due to a fixed obstruction produced by coronary atherosclerosis. Unstable Angina: In unstable angina, chest pains occur with increased frequency and are precipitated by progressively less effort.(lies b/w Angina and MI) Prinzmetal/Variant/Vasopastic Angina: It is an uncommon pattern of episodic angina that occurs at rest and is due to coronary artery spasm. Symptoms are caused by decreased blood flow to the heart muscle due to spasm of the coronary artery. Mixed Angina: Patients with advanced coronary artery disease may present with angina episodes during effort as well as at rest, suggesting the presence of a fixed obstruction associated with endothelial dysfunction. Angiodema: Angioedema or Quincke's edema is the rapid swelling (edema) of the dermis, subcutaneous tissue, mucosa and submucosal tissues. Also known as angioneurotic oedema. Due to increased bradykinin(vasodilator) levels which occurs in ACEIs treatment. Hydralazine causes Lupus Like Syndrome. Hypothyroidism & Antidepressants causes Weight Gain. Low Density Lipoproteins LPLs act as Carriers of cholesterol in Plasma. HDLs cause atherosclerosis. Sites of Antibiotics: Cell wall synthesis(B-lactams); metabolism(sulfonamides); protein synthesis(macrolides); nucleic acid function or synthesis(cipro); cell membrane function(isoniazid).
Drugs Affecting Other Organs Respiratory System: a. Asthma: 2-Adrenergic Agonists, Corticosteroids, Montelukast(Cysteinyl leukotriene antagonist), Theophylline, Omalizumab. b. Allergic Rhinitis: -Adrenergic Agonists, Antihistamines, Corticosteroids, Cromolyn. c. COPD: -Adrenergic Agonists, Corticosteroids, Ipratropium. d. Cough: Dextromethorphan, Opiates.
GIT Drugs: Parietal cell is acted upon by Acetylcholine, Gastrin, Histamine & Prostaglandin. PG has inhibitory effect while others increase acid release. a. Anti-Microbials: Amoxycillin, Clarithromycin, Tetracycline, Metronidazole. b. H2-Receptor Antagonist: They are competitive antagonists of histamine and are fully reversible. These agents completely inhibit gastric acid secretion induced by histamine or gastrin. Cimetidine, Ranitidine, Famotidine. c. PPIs: They bind to the H+/K+-ATPase enzyme system (proton pump) of the parietal cell, thereby suppressing secretion of hydrogen ions into the gastric lumen. The membrane-bound proton pump is the final step in the secretion of gastric acid Esomeprazole, Omeprazole, Lansoprazole. d. Prostaglandins: Prostaglandin E2, produced by the gastric mucosa, inhibits secretion of HCl and stimulates secretion of mucus and bicarbonate. Misoprostol (Prostaglandin E2 analog). e. Antacids: Aluminium Hydroxide, Magnesium Hydroxide. f. Mucosal Protective Agents: Sucralfate.
Anti-Emetics: a. Phenothiazines: Prochlorperazine (Block dopamine receptors) b. 5-HT3 receptor blocker: They selectively block 5-HT3 receptors in the periphery (visceral vagal afferent fibers) and in the brain. Ondansetron, Granisetron, Dolasetron. c. Butyrophenones: Droperidol, Haloperidol (Block Dopamine receptors). d, Substance P/Neurokinin-I Blocker: Aprepitant (It targets the neurokinin receptor in the brain and blocks the actions of the natural substance)
Anti-diarrheals: a. Anti-motility agents: Both are analogs of meperidine and have opioid-like actions on the gut, activating presynaptic opioid receptors in the enteric nervous system to inhibit acetylcholine release and decrease peristalsis. At the usual doses, they lack analgesic effects. Diphenoxylate, Loperamide. b. Adsorbents: Bismuth subsalicylate, Methylcellulose, Aluminum hydroxide. c. Agents that modify fluid and electrolyte transport: Bismuth subsalicylate. (Travellers diarrhea)
Laxatives: a. Irritants & Stimulants: Senna, Bisacodyl. b. Bulk Laxatives: They form gels in the large intestine, causing water retention and intestinal distension, thereby increasing peristaltic activity. Methylcellulose, Psyllium seeds, Bran. c. Stool softeners: (Emollient laxatives/Surfactants) Docusate sodium, Docusate calcium, Docusate potassium. d. Lubricant Laxatives: Mineral oil & Glycerin suppositories. (Facilitate the passage of hard stools)
Other Therapies Erectile Dysfunction (PDE-5 Inhibitors): Sildenafil, Vardenafil. Osteoporosis: Alendronate, Ibandronate, Calcitonin, Zoledronic Acid. Obesity: Orlistat (lipase inhibitor), Sibutramine (anorexiant), Phentermine (anorexiant).
Adrenal Hormones Structure: Inner part Medulla secreting Epinehprine. Outer part cortex. Cortex is further divided into three parts. Inner most of cortex is Reticularis which secretes Adrenal androgens; Middle part called Fasciculata secreting Glucocorticoids and outer most is the Glomerulosa which secretes Mineralocorticoids. Physiology: Hypothalamus A Pituitary Adrenal Gland
Glucocorticoids & Mineralocorticoids are collectively known as Corticosteroids. Cortisol also acts as a feedback mechanism and inhibits both processes from hypothalamus to anterior pituitary and pituitary to adrenal glands. Glucocorticoids: a. Short Acting (1-12 hrs): Hydrocortisone, Cortisone. b. Intermediate Acting (12-36hrs): Prednisone, Prednisolone, Methylprednisolone. c. Long Acting (36-55hrs): Betamethasone, Dexamethasone. Mineralocorticoids: Deoxycorticosterone, Fludrocortisone. Glucocorticoids act as anti inflammatory by inhibiting PGs and Leukotrienes & also redistribute WBCs to other body sites; also reduce histamine release from mast cells and basophils; decrease ability of macrophages and leukocytes to antigens and mitogens. Also used in Treatment of Allergies and Diagnosis of Cushings disease (Overproduction of glucocoricoids)
Biopharm Concepts Metabolism can happen in two phases. Phase I reactions involve hydrolysis, oxidation and reduction (results in low hydrophilicity). Phase II reactions involve glucoronidation, sulfonation, acetylation, methylation, conjugation with glutathione or amino acids(cause high hydrophilicity). Phase I may or may not precede Phase II. Clearance is the volume of plasma cleared off drug per unit time. Its unit is ml/min. Pharmacokinetics involves the movement of drug or its metabolites into or out of the body and also evaluates its metabolism rates. Zero order kinetics is independent of drug concentrations; usually seen when reaction system is saturated.e.g Metabolism of Phenytoin, Constant rate IV Infusion. In First order kinetics rate of drug elimination at particular time is directly proportional to the amount of drug in the body at that time; Semi Logarithmic plot of Plasma Drug Conc vs time is a straight line. Elimination rate constant, Vd, clearance and half life are independent of the dose of the drug. First order kinetics is also known as monoexponential kinetics; in which rate of reaction is directly proportional to the drug concentration in the reaction. Mixed Order Kinetics depends on the dose of the drug and are thus known as Dose Dependant or Non-Linear Kinetics. Generally described by Michelis Menten Equation.
Biopharm Concepts Pharmacokinetic Models are imaginary compartments. Central Compartment represents plasma and tissues which rapidly equilibrate with drugs. Peripheral Compartments represents tissues or organs which equilibrate slowly. Number and site of compartments is determined by the blood perfusion capacity and drug physicochemical properties. Michelis Menten Equation: -dc = Vmax x C dt Km + C
Plasma albumin has 4 binding sites .i.e Warfarin, Diazepam, Tamoxifen, Digoxin. Total body tissue comprises 40% of the total body.
Pharmaceutical Equivalents: If two drugs contain same amount of active ingredient in same dosage form. They may contain different excipients. Pharmaceutical Alternatives: If two drugs contain same drug molecule but in different chemical form e.g different salt or strength. Bioavailability: Rate and extent to which a drug is absorbed from the site of administration and become available at the site of action. Bioeuivalence: Drugs showing same bioavailability are said to be bioequivalent. Essentially Similar Product: A copy of the research or Innovator Product. (ME 2) Biopharm Concepts Therapeutic Equivalents: If two drugs provide the same desired therapeutic effect with same safety and efficacy. Cmax: Maximum Drug Plasma concentration partly depends on the rate of release of drug from the formulation. Tmax: Time required to reach maximum Plasma drug concentration; also dependant on rate of drug release. T1/2: Elimination half life. Mean Residence Time (MRT): Time a drug molecule spends in the body before it gets excreted out. Metabolism reactions are also said to be Bioactivation reactions. Metabolism is basically involved in converting a drug more hydrophilic to facilitate its excretion from the body.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- STUDENT LINKING WORDS AND PHRASESDokument6 SeitenSTUDENT LINKING WORDS AND PHRASESEdward YooNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- IELTS Writing Answer SheetDokument4 SeitenIELTS Writing Answer SheetHighPoint IELTS Preparation Services, Inc.Noch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Essay Question 1 - Outsourcing Labour Related Work To Poorer Nations - Corrected by RyanDokument5 SeitenEssay Question 1 - Outsourcing Labour Related Work To Poorer Nations - Corrected by RyanDr-Usman Khan0% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- TransitionsDokument3 SeitenTransitionsDr-Usman KhanNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- IELTS Speaking Part 1 VocabularyDokument24 SeitenIELTS Speaking Part 1 VocabularyDr-Usman Khan100% (1)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Nol 7zone Eng PDFDokument1 SeiteNol 7zone Eng PDFneedzinNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- YES-IELTS - Decoding The IELTS Band Descriptors - Writing Task 2 - Task Response - Bands 6, 7, 8, 9Dokument6 SeitenYES-IELTS - Decoding The IELTS Band Descriptors - Writing Task 2 - Task Response - Bands 6, 7, 8, 9YES IELTS100% (2)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- IELTS True False Not GivenDokument5 SeitenIELTS True False Not GivenDr-Usman Khan100% (2)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Difference BTW False, No, NGDokument1 SeiteDifference BTW False, No, NGDr-Usman KhanNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- Speaking Tips by RyanDokument2 SeitenSpeaking Tips by RyanDr-Usman Khan100% (3)
- Connectors For IELTSDokument24 SeitenConnectors For IELTSDr-Usman KhanNoch keine Bewertungen
- Difference BTW False, No, NGDokument1 SeiteDifference BTW False, No, NGDr-Usman KhanNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
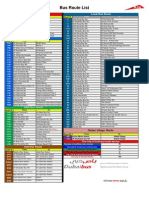
- Bus Route List EnglishDokument1 SeiteBus Route List EnglishDr-Usman KhanNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Bus Route List EnglishDokument1 SeiteBus Route List EnglishDr-Usman KhanNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Exam MaterialsDokument4 SeitenExam MaterialsDr-Usman KhanNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- PharmaciesDokument18 SeitenPharmaciesDr-Usman KhanNoch keine Bewertungen
- 32 Ielts Essay Samples Band 9Dokument34 Seiten32 Ielts Essay Samples Band 9mh73% (26)
- Delcaration Form by The Sponsoring FacilityDokument1 SeiteDelcaration Form by The Sponsoring FacilityDr-Usman Khan100% (1)
- 06 MarchDokument3 Seiten06 MarchDr-Usman Khan0% (1)
- 23 QsDokument8 Seiten23 QsDr-Usman Khan0% (1)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- 5 2 2014 - 2Dokument2 Seiten5 2 2014 - 2Dr-Usman Khan100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- 5 2 2014 - 2Dokument2 Seiten5 2 2014 - 2Dr-Usman Khan100% (1)
- 570 Academic Word List For IELTSDokument26 Seiten570 Academic Word List For IELTSXanh Lè100% (1)
- 30-01-2014 Test Malik Asif Javaid AwanDokument4 Seiten30-01-2014 Test Malik Asif Javaid AwanDr-Usman Khan67% (3)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Dha Prometric Feb-3 ShabeerDokument2 SeitenDha Prometric Feb-3 ShabeerDr-Usman KhanNoch keine Bewertungen
- Writing Task 1 1-8Dokument28 SeitenWriting Task 1 1-8Dr-Usman KhanNoch keine Bewertungen
- Dha Prometric Feb-3 ShabeerDokument2 SeitenDha Prometric Feb-3 ShabeerDr-Usman KhanNoch keine Bewertungen
- DHA Prometric Exam 02-01-2014 Role of Carbidopa in ParkinsonismDokument4 SeitenDHA Prometric Exam 02-01-2014 Role of Carbidopa in ParkinsonismDr-Usman Khan79% (14)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Good CommunicationDokument6 SeitenGood CommunicationKranthi KumarNoch keine Bewertungen
- The Drugs Act, 1976Dokument32 SeitenThe Drugs Act, 1976Dr-Usman KhanNoch keine Bewertungen
- Chemotheraphy and Its Side EffectsDokument2 SeitenChemotheraphy and Its Side EffectsALYSSA MAE RAPERNoch keine Bewertungen
- Pyrantel Dosage Guide With PrecautionsDokument1 SeitePyrantel Dosage Guide With PrecautionsMey KhNoch keine Bewertungen
- BCS Class PDFDokument14 SeitenBCS Class PDFdhimas11100% (1)
- Antiepilepsy Drugs: Pharmacodynamics and Principles of Drug SelectionDokument22 SeitenAntiepilepsy Drugs: Pharmacodynamics and Principles of Drug SelectionNaela RizqiNoch keine Bewertungen
- ChemotherapyDokument7 SeitenChemotherapyraecmyNoch keine Bewertungen
- RANITIDINE - Ranitidine Hydrochloride Injection, Solution: Page 1 of 9Dokument9 SeitenRANITIDINE - Ranitidine Hydrochloride Injection, Solution: Page 1 of 9Nur Syamsiah LaisaNoch keine Bewertungen
- Medicine Price List MPL Acute and Chronic November 2020Dokument123 SeitenMedicine Price List MPL Acute and Chronic November 2020karar hussainNoch keine Bewertungen
- 07.04.05 Venturi Face Mask PDFDokument2 Seiten07.04.05 Venturi Face Mask PDFRosintchi MirsalNoch keine Bewertungen
- Muscle Energy Techniquesto Correct Postural DysfunctionsDokument3 SeitenMuscle Energy Techniquesto Correct Postural DysfunctionsdasaNoch keine Bewertungen
- Maxolon Injection 5 MG / MLDokument1 SeiteMaxolon Injection 5 MG / MLJunaid IjazNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Moh Exam Prep MaterialDokument159 SeitenMoh Exam Prep MaterialAbid Ali Khan100% (1)
- Danger, Medicine, Fitness and Health VocabularyDokument4 SeitenDanger, Medicine, Fitness and Health VocabularyPhương ThảoNoch keine Bewertungen
- Pharmacy Board - Guidelines - Guidelines For Dispensing of MedicinesDokument19 SeitenPharmacy Board - Guidelines - Guidelines For Dispensing of MedicinesAnna WangNoch keine Bewertungen
- Bevacizumab Carboplatin Paclitaxel For Cervical Cancers CRP14GY017 v1.0Dokument6 SeitenBevacizumab Carboplatin Paclitaxel For Cervical Cancers CRP14GY017 v1.0andibarosNoch keine Bewertungen
- Classification Des MédicamentsDokument28 SeitenClassification Des MédicamentsGustyl KolinsNoch keine Bewertungen
- Walmart Drug ListDokument6 SeitenWalmart Drug ListShirley Pigott MDNoch keine Bewertungen
- Management of Severe Local Anaesthetic ToxicityDokument2 SeitenManagement of Severe Local Anaesthetic Toxicitymonir61Noch keine Bewertungen
- PharmacologyDokument236 SeitenPharmacologyyalahopa100% (2)
- Common Drugs - Med WardDokument1 SeiteCommon Drugs - Med WardRohannah D. MalawadNoch keine Bewertungen
- Nama Item AlkesDokument17 SeitenNama Item Alkesrian agustianNoch keine Bewertungen
- LM Database of Radiation OncologistsDokument17 SeitenLM Database of Radiation OncologistsNishant ChandraNoch keine Bewertungen
- Medication AdministrationDokument10 SeitenMedication AdministrationJemma NocalanNoch keine Bewertungen
- Studi Bioekivalensi Amoksisilin Generik Dan Dagang Menggunakan Matriks UrinDokument7 SeitenStudi Bioekivalensi Amoksisilin Generik Dan Dagang Menggunakan Matriks UrinEA12345aeNoch keine Bewertungen
- 1.application To Market A New DrugDokument4 Seiten1.application To Market A New DrugcardiacanesthesiaNoch keine Bewertungen
- (9781585286584 - ASHP® Injectable Drug Information™) Preliminary MaterialDokument24 Seiten(9781585286584 - ASHP® Injectable Drug Information™) Preliminary MaterialSathundorn NuntaNoch keine Bewertungen
- Stock 27072023 - ShareDokument80 SeitenStock 27072023 - ShareDanang WahyuNoch keine Bewertungen
- Anesthesia For Day-Care SurgeryDokument13 SeitenAnesthesia For Day-Care SurgeryMadhur AcharyaNoch keine Bewertungen
- Students Practical Training Report Project As Per PCI NormsDokument82 SeitenStudents Practical Training Report Project As Per PCI NormsAakif Anjum100% (1)
- Salinan Dari Jadwal KF Kedung CowekDokument47 SeitenSalinan Dari Jadwal KF Kedung Cowekdwikamaliyatissholehah94Noch keine Bewertungen
- TabletsDokument2 SeitenTabletsHector De VeraNoch keine Bewertungen
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisVon EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (13)