Beruflich Dokumente
Kultur Dokumente
Critical Care
Hochgeladen von
avisenicOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Critical Care
Hochgeladen von
avisenicCopyright:
Verfügbare Formate
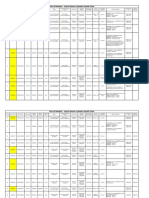
2002 Self-Assessment Exercise XXIX. Critical care [Return to Category List] Questions Question 6. Answer.
A 2-week-old infant presents with tachypnea, poor perfusion, gallop rhythm, diminished pulses, and hepatomegaly. Arterial blood gas shows metabolic acidosis. Echocardiography reveals critical aortic stenosis. Of the following, the intervention MOST likely to stabilize the infant's condition is: A. B. C. D. E. dobutamine epinephrine nitric oxide 100% oxygen prostaglandin E1 Answer.
Question 25.
A 4-year-old child is brought by ambulance to the emergency department. He is unconscious and has deep, regular, and rapid respirations. A clinical finding that BEST distinguishes this respiratory pattern as central hyperventilation rather than tachypnea is: A. B. C. D. E. arterial carbon dioxide pressure (Paco2) of 26 mm Hg decreased mental status nonreactive pupils oxygen saturation of 95% by pulse oximetry sternal retractions Answer.
Question 46.
The most likely finding in the initial stages of septic shock is: A. B. C. abnormally low blood pressure absent femoral pulses delayed capillary refill
D. E.
hyperpnea tachypnea Answer.
Question 66.
A 5-year-old boy is given general anesthesia with halothane for a tonsillectomy and adenoidectomy. Shortly after initiating the procedure, he develops tachycardia, a temperature of 103F (39.4C), and muscle rigidity. Of the following, the MOST appropriate definitive treatment includes discontinuation of anesthetic and treatment with: A. B. C. D. E. acetaminophen dantrolene dapsone hydrocortisone succinylcholine
Question 110. Answer. A 7-year-old child presents after a motor vehicle accident. He was not wearing a seatbelt, and he was sitting at the point of impact in the left rear passenger seat. There was intrusion into the vehicle. He complains of left upper quadrant abdominal pain and left shoulder pain. Physical examination shows diffuse abdominal tenderness, but no obvious tenderness or trauma to the shoulder. Blood pressure is 120/80 mm Hg and heart rate is 120 beats/ min. You have sent blood for a complete blood count. Of the following, the MOST appropriate next diagnostic study is: A. B. C. D. E. abdominal computed tomography abdominal ultrasonography barium contrast enema diagnostic peritoneal lavage upright plain abdominal film
Question 132. Answer. A 2-day-old boy has biphasic stridor that worsens with agitation. He has intermittent desaturations with bradycardia and a weak cry. Blood pressure is 80/60 mm Hg, and pulse rate is 112 beats/min. Of the following, the MOST likely etiology of this child's condition is:
A. B. C. D. E.
congenital subglottic stenosis cystic fibrosis hypoplastic left heart innominate artery compression tracheoesophageal fistula
Question 154. Answer. An adolescent who has systemic lupus erythematosus develops pericardial tamponade. In addition to muffled heart tones, the MOST likely finding would be decreased: A. B. C. D. E. heart rate during expiration heart rate during inspiration jugular venous pulsation during expiration systolic blood pressure during expiration systolic blood pressure during inspiration
Question 177. Answer. A 6-year-old boy presents with a 24-hour history of fever, malaise, and bruising. Physical examination reveals an ill-appearing child whose temperature is 103.1F (39.5C). He has widespread petechiae and areas of palpable purpura, especially on the buttocks and lower extremities. The hemoglobin is 10.5 g/dL (105 g/L), white blood cell count is 18,500/cu mm (18.5 x 109/L), and platelet count is 25,000/cu mm (25 x 109/L). Of the following, the MOST likely diagnosis is: A. B. C. D. E. Henoch-Schnlein purpura idiopathic thrombocytopenic purpura Lyme disease meningococcemia Rocky Mountain spotted fever
Question 200. Answer. A 16-year-old driver who was not wearing a seatbelt was involved in a high-speed head-on collision. He has suffered extensive trauma to the chest. In the emergency department, he is alert but tachypneic, with markedly diminished breath sounds on the right. Chest radiography reveals several anterior rib fractures on the right and fluid in the right pleural space.
Of the following, the MOST appropriate next step in the management of this boy is: A. B. C. D. E. administration of intravenous furosemide chest tube placement elevation of the head of the bed emergent thoracotomy endotracheal intubation
Question 221. Answer. A 6-month-old previously healthy child presents in January with fever of 3 days' duration and wheezing that has increased in severity for 2 days. On physical examination, the child is awake and interactive. Respiratory rate is 60 breaths/min, and there are marked wheezes bilaterally and intercostal retractions. Because there is no improvement after two treatments with nebulized albuterol, you admit the child to the hospital. Upon re-evaluation 4 hours later, the child is agitated and has a respiratory rate of 80 breaths/min. Arterial blood gas while receiving 35% oxygen reveals pH of 7.24, Po2 of 65 mm Hg, and Pco2 of 60 mm Hg. Of the following, the MOST appropriate next step in management is: A. B. C. D. E. administration of intramuscular dexamethasone administration of racemic epinephrine continuous albuterol nebulization immediate endotracheal intubation increase of inspired oxygen to 50%
Question 243. Answer. The mother of a 3-year-old girl finds the girl submerged in a backyard pool. Of the following, the finding that is MOST compatible with a favorable neurologic prognosis for this child is: A. B. C. D. E. apnea at the time of admission to the emergency department coma at the time of admission to the emergency department first spontaneous respirations within 10 minutes of resuscitation initial arterial pH <7.0 submersion of more than 25 minutes
Question 263. Answer.
A 14-year-old girl presents with sustained palpitations and a heart rate of 210 beats/min. Electrocardiography shows narrow complex supraventricular tachycardia (SVT). Administration of an intravenous bolus of adenosine results in normal sinus rhythm for 30 seconds, followed by a return of sustained SVT. Of the following, the MOST appropriate intervention for this girl is: A. B. C. D. E. intravenous amiodarone intravenous digoxin intravenous diltiazem intravenous quinidine synchronized electrical cardioversion
Answers Critique 6. Preferred Response: E
[View Question] The infant in the vignette presents with severe congestive heart failure and cardiogenic shock at a typical age for critically obstructive left heart lesions, such as hypoplastic left heart syndrome, critical neonatal coarctation of aorta, and critical congenital aortic stenosis (Figure 6A). As the ductus arteriosus closes, the early compensatory right ventricular contribution to systemic blood flow and vital perfusion to the kidneys and other organs are lost. The result is rapidly developing severe metabolic acidosis that contributes to myocardial and other organ dysfunction. The presentation of affected infants often resembles that of septic shock. A high index of suspicion for congenital left heart obstructive lesions must be maintained for infants who have signs of shock in the first two months of life. These signs include gray color and poor capillary refill, thready or absent peripheral or central pulses, tachypnea and hyperpnea, hypotension, and obtundation. In the infant who has presumed septic shock, severe metabolic acidosis, and cardiomegaly on chest radiography, echocardiographic evaluation should be undertaken to exclude left heart obstructive lesions. Base deficit pH values greater than 25 on arterial blood gas measurement are common after ductal closure in these infants. Good clinical outcomes have been described even in infants who present with pH values less than 7.0. Essential to good resuscitation of the infant who has shock from obstructive left heart lesions is reopening of the ductus arteriosus. Presumably, once the ductus closes, the spiral of fatal deterioration develops rapidly. Accordingly, a trial of prostaglandin E1 (alprostadil) infusion should be administered even to an infant as old as 1 to 2 months of age to open the recently closed ductus arteriosus. The open ductus allows the right ventricle to provide systemic blood flow when the left ventricle cannot.
Inotropic agents such as dobutamine or epinephrine may provide adjunctive and supportive therapy, but they will not be lifesaving if prostaglandin E1 is not employed to open the ductus. Serious hypoxia is not a problem for infants who have obstructive left heart lesions. In fact, the arterial Po2 may be normal on initial blood gas measurement, even in the presence of alarming metabolic acidosis and clinical shock. As the ductus opens with prostaglandin treatment, the arterial Po2 may decrease, with improving right ventricular flow to the body. Attempts to keep the arterial Po2 high are detrimental because a high inspired oxygen level is a powerful vasodilator of the pulmonary arteries. Some degree of pulmonary hypertension is essential to promote flow to the systemic circulation via the ductus. Pulmonary artery vasodilatation from supplemental oxygen steals the right ventricular output to the pulmonary arteries and away from the body. This steal phenomenon, not oxygen-induced ductal closure, is the primary risk associated with use of supplemental oxygen when prostaglandin E1 is being used to keep the ductus open. Nitric oxide also is a powerful pulmonary arterial vasodilator. Although it may be a lifesaving treatment for newborns who have severe pulmonary hypertension and inadequate pulmonary blood flow, it is contraindicated in the presence of obstructive left heart lesions. References: Fedderly RT. Left ventricular outflow obstruction. Pediatr Clin North Am. 1999;46:369-384 Rothman A. Coarctation of the aorta: an update. Curr Probl Pediatr. 1998;28:33-60 Critique 25. Preferred Response: C
[View Question] Central hyperventilation, characterized by sustained, rapid, and fairly deep hyperpnea, differs from the rapid, shallow respirations of simple tachypnea. Central hyperventilation typically represents one sign in the stages of coma that result from markedly elevated intracranial pressure and progression toward transtentorial or uncal herniation (Figure 25A). The earliest signs are decreased level of consciousness and alterations in the respiratory pattern. Patients who have central hyperventilation may have hypertension and bradycardia (Cushing triad). During the systematic stages of coma, specific signs develop as injury progresses inferiorly along the brainstem. Initially, in the low diencephalic stage, the child is comatose, has Cheyne-Stokes respirations (crescendo-decrescendo hyperventilation to apnea), small and sluggishly reactive pupils, dolls eyes (oculocephalic) and caloric (oculovestibular) reflexes, and decorticate (flexion of the upper extremities and extension of the lower extremities) response to pain. Later, at the midbrain stage, the respiratory pattern changes to sustained central hyperventilation, the pupils become midposition and fixed, and there is a stereotyped decerebrate (extensor with all extremities) posturing to noxious stimuli. At the pontine stage, hyperventilation gives way to apneustic breathing (deep respirations with
prolonged pauses), the pupils are small-to-pinpoint and nonreactive, and caloric and dolls eyes reflexes may be absent. Finally, the extremities become flaccid with absent motor response, breathing becomes ataxic, and death ensues. Decreased oxygen saturation and diminished mental status are nonspecific findings that can characterize many processes other than central hyperventilation, such as hypoxia secondary to pulmonary disease. A decreased arterial carbon dioxide pressure can be seen in hyperventilation attacks or psychogenic hyperventilation as well as central hyperventilation. Sternal retractions are typical of hypoxia in patients who have lower airway disease and are not a feature of central hyperventilation. Loss of pupillary response is typical for a midbrain or pontine brainstem process and, combined with loss of consciousness, should alert the clinician to the possibility of impending uncal herniation. Other causes for bilateral loss of pupillary reflex (eg, pilocarpine drops, opiates, atropine drops, cocaine, and jimson weed) should be considered only after the possibility of increased intracranial pressure has been excluded. References: Bergman I. Increased intracranial pressure. Pediatr Rev. 1994;15:241-244 Rubenstein JS. Initial management of coma and altered consciousness in the pediatric patient. Pediatr Rev. 1994;15:204-207 Stokes DC. Respiratory failure. Pediatr Rev. 1997;18:361-366 Critique 46. Preferred Response: C
[View Question] Shock is a state of inadequate delivery of oxygenated blood flow to the bodys organs relative to the demands of those organs. Ischemia is lack of normal blood flow. Hypoxemia is abnormally low oxygen tension in the blood. The combination of hypoxemia and ischemia is most detrimental, resulting in irreversible damage to organs and if not corrected, resulting in death. Pure hypoxemia without ischemia can be tolerated well, especially if it develops chronically. An example of this principle is the sometimes surprisingly healthy status and normal mental development of children who have partially repaired cyanotic heart disease. Children who have single ventricle physiology, such as hypoplastic left heart syndrome, may await completion of the Fontan repair for several years. During that time, the systemic oxygen saturation may be less than 80%, but there is normal blood flow to the bodys organs and no untoward symptoms other than lower-than-normal exercise tolerance. Conversely, a myocardial infarction or stroke causes damage to the heart or brain from the sudden lack of blood flow to the tissues. Appreciated but not completely understood is the importance of the role of blood flow in washing out toxic metabolites from cells, a function independent from oxygen delivery.
In pediatric practice, the most common causes of shock are severe dehydration and overwhelming sepsis. Hypotension and increased metabolic demand combine to produce inadequate tissue blood flow, with the development of metabolic acidosis that can end in death. Therefore, early clinical recognition of shock is vitally important. Studies show that cardiac output may be compromised significantly before any clinically significant fall in blood pressure becomes apparent. Accordingly, hypotension and absent femoral pulses are late findings of shock. Hyperpnea (deep respirations) and tachypnea (rapid respirations) occur in shock, especially as metabolic acidosis develops when perfusion of the kidneys and other organs falls to critically low levels. However, these findings usually are not the earliest clinical signs of inadequate tissue perfusion. The flush of pink color into the finger tips or toes following release of gentle pressure on the digit (capillary refill) provides a direct view of the arterial filling of the distal extremities. The speed and vigor with which capillary refill occurs is a good early warning system in the child or infant in whom shock may develop. Delayed capillary refill (>3 sec) is an early sign of shock. Serial assessments of this physical sign should be as routine and frequent as vital signs in all seriously ill hospitalized infants and children. References: Abelow B. Respiratory acidosis. In: Understanding Acid-Base. Baltimore, Md: Williams & Wilkins; 1998:171-181 Schexnayder SM. Pediatric septic shock. Pediatr Rev. 1999;20:303-307 Critique 66. Preferred Response: B
[View Question] Malignant hyperthermia (MH) is a rare, life-threatening complication of general anesthesia. It is characterized by tachypnea, tachycardia, hypermetabolism, muscle rigidity, hypercarbia, acidosis, and fever that can occur following exposure to inhalational anesthetics such as halothane, isoflurane, or a depolarizing muscle relaxer such as succinylcholine. The potential to develop MH is inherited in an autosomal dominant pattern with variable penetrance. Because of this, a family history of anesthesia-associated complications should be sought prior to surgery. It is more common among patients who have a variety of myopathic disorders, including Duchenne muscular dystrophy. Initial indications of MH during general anesthesia may be tachycardia, tachypnea, fever, or any of the other symptoms mentioned previously. Monitoring temperature and cardiovascular stability during general anesthesia is essential to identify and allow for early treatment of this complication. Treatment includes cessation of triggering anesthetic agents, hyperventilation with oxygen, and administration of dantrolene 3 mg/kg intravenously to a total loading dose of 10 mg/kg, if necessary. Dantrolene works directly on skeletal muscle, causing excitationcontraction coupling dissociation by interfering with the release of calcium from the
sarcoplasmic reticulum. Circulatory support, treatment of hyperkalemia and acidosis, active cooling measures, and urinary alkalinization to prevent tubular injury from severe rhabdomyolysis also are appropriate. If subsequent procedures must be performed under general anesthetic, nontriggering anesthetics that may be used safely include barbiturates, opioids, propofol, nitrous oxide, benzodiazepines, and nondepolarizing muscle relaxers. Local anesthetics also represent safe alternatives. Administration of acetaminophen for fever is an appropriate adjunctive measure when MH is diagnosed, but treating only the fever will not prevent the life-threatening consequences. Dapsone may be used in the treatment of a variety of disorders, including dermatitis herpetiformis and leprosy, and for malaria prophylaxis. Hydrocortisone should be considered for the treatment of a suspected allergic reaction, but such a reaction should not manifest with fever or muscle rigidity. Because it is a likely triggering agent for MH, succinylcholine is contraindicated. References: Abraham RB, Adnet P, Glauber V, Perel A. Malignant hyperthermia. Postgrad Med J. 1998;74:11-17 Ben Abraham R, Cahana A, Krivosic-Horber RM, Perel A. Malignant hyperthermia susceptibility: anaesthetic implications and risk stratification. QJM. 1997;90:13-18 Berde CB, Schechter WS. Anesthesia and perioperative care. In: Behrman RE, Kliegman RM, Jenson HB, eds. Nelson Textbook of Pediatrics. 16th ed. Philadelphia, Pa: WB Saunders Co; 2000:297-305 Denborough M. Malignant hyperthermia. Lancet. 1998;352:1131-1136 Kaus SJ, Rockoff MA. Malignant hyperthermia. Pediatr Clin North Am. 1994;41:221-237 Critique 110. Preferred Response: A
[View Question] The initial management of this trauma victim should include a rapid assessment of the ABCs: Airway, Breathing, and Circulation. All clothing should be removed and a rapid neurologic examination undertaken simultaneously. Once immediate, life-threatening conditions have been identified and management initiated, a secondary complete body survey should be performed to identify any other injuries. If abdominal trauma is suspected, as suggested for the child described in the vignette, the imaging modality of choice in a pediatric patient is computed tomography, usually with at least double contrast (oral and intravenous). Laboratory tests may include a complete blood count, type and crossmatch, blood gas determination, urinalysis, and chemistries that include serum amylase. The role of abdominal ultrasonography in the pediatric patient has not yet been established, although its use has become common in
adults. Although a film of the pelvis often is warranted to assess for pelvic fractures, an upright abdominal film generally is neither helpful nor practical. Diagnostic peritoneal lavage has little role in pediatric trauma unless the patient is hemodynamically unstable. Easy access to rapid computed tomography has made this a rare procedure. A barium contrast enema is rarely, if ever, indicated. Most pediatric abdominal injuries result from trauma, typically after a fall or a motor vehicle crash. Some abdominal injuries are more common in children than in adults, including duodenal hematomas (Figure 110A), blunt pancreatic injuries, small bowel perforations at or near the ligament of Treitz, and bladder injuries. It is imperative that children who are suspected of having major abdominal trauma be evaluated in a trauma center. The spleen is the most commonly injured abdominal organ in a child. Due to its highly vascular nature, significant bleeding into the peritoneal cavity often results. Abdominal tenderness is not invariably present with mild splenic trauma, but if it localizes, it does so to the left upper quadrant. Massive hemorrhage may lead to hemodynamic instability, although up to 80% of splenic trauma can be managed nonoperatively with observation in an intensive care unit. References: Andrews JS, DeAngelis C. Index of suspicion. Case 2. Splenic injury. Pediatr Rev. 1994;15:391393 American College of Surgeons Committee on Trauma. Pediatric trauma. In: Advanced Trauma Life Support for Doctors: Student Course Manual. 6th ed. Chicago, Ill: American College of Surgeons; 1997:289-311 Critique 132. Preferred Response: A
[View Question] Stridor is produced by rapid, turbulent flow of air through a narrow segment of the airway. Biphasic stridor suggests an anatomic location at the glottic or subglottic level. Inspiratory stridor typically is produced by an obstruction above the vocal cords; expiratory stridor is produced by an intrathoracic site of obstruction. The most common cause of congenital stridor is laryngomalacia, which typically presents as relatively benign inspiratory stridor without significant airway distress. Vocal cord paralysis is the second most common cause of congenital stridor and usually presents as predominately inspiratory obstruction. Infants who have vocal cord paralysis may present with respiratory distress, failure to thrive, and blue spells. The third most common cause of congenital stridor is congenital subglottic stenosis (Figure 132A) or glottic and subglottic web. Congenital subglottic stenosis is characterized by biphasic stridor that typically worsens with agitation, as described for the infant in the vignette. In severe cases that involve a very narrow airway, respiratory distress with retractions, desaturations, and bradycardia can
occur. The presence of a weak cry suggests involvement of the stenosis up to the vocal cord level. Normal cardiovascular stability typically is maintained until end-stage airway crisis. Flexible airway endoscopy is the best initial diagnostic procedure for evaluation of congenital stridor. Laryngomalacia and vocal cord paralysis are usually visible, subglottic narrowing can be evaluated, and tracheomalacia can be assessed easily. Endoscopy often reveals anterior pulsatile tracheal compression in innominate artery compression, demonstrates narrowing consistent with double aortic arch, and shows tracheoesophageal fistula or laryngeal cleft. Chest radiography may reveal subglottic narrowing or tracheal narrowing that possibly are consistent with tracheal stenosis or tracheomalacia. Severe distal tracheal obstruction from a high-grade stenosis or foreign body frequently is suggested by air trapping and hyperexpansion on the affected side. Cystic fibrosis often presents with meconium ileus at birth and the development of chronic cough, respiratory distress, and failure to thrive later in life. Stridor is uncommon. Patients who have hypoplastic left heart syndrome do not have obvious stridor; rather, they present with signs of cyanosis and hypoperfusion. Signs of congestive failure usually appear within the first few days or weeks of life. Tracheoesophageal fistula presents with excessive oral secretions, choking, coughing, and cyanosis when feeding is attempted. Tracheomalacia may cause expiratory stridor, but biphasic stridor is uncommon. Innominate artery compression, although usually mild and asymptomatic, may cause expiratory stridor, cough, and recurrent pneumonias. Respiratory distress is uncommon. References: Brodsky L. Congenital stridor. Pediatr Rev. 1996;17:408-411 Cotton, RT, Reilly JS. Stridor and airway obstruction. In: Bluestone CD, Stool SE, Kenna MA, eds. Pediatric Otolaryngology. 3rd ed. Philadelphia, Pa: WB Saunders Co; 1996:1275-1287 Holinger LD. Etiology of stridor in the neonate, infant and child. Ann Otol Rhinol Laryngol. 1980;89:397-400 Critique 154. Preferred Response: E
[View Question] Abnormally decreased systolic blood pressure during inspiration is termed pulsus paradoxus. In fact, this is not a paradoxic response to respiratory changes in intrathoracic pressure. Normally, inspiration creates a more negative intrathoracic pressure, which results in enhanced right atrial and right ventricular filling at the minor expense of decreased left ventricular filling. A phasic increase in heart rate that is modulated by withdrawal of vagal tone compensates for the decrease in left ventricular preload during inspiration as the aortic baroreceptors signal the brainstem that left ventricular stoke volume has decreased by end inspiration. During exhalation, opposite changes occur. Left ventricular filling is increased modestly, resulting in a heart rate that slows slightly by end expiration. Normal sinus
arrhythmia results from this phasic respiratory change in ventricular filling. These respiratory changes also are primarily responsible for the normal variation in the splitting of the second heart sound that occurs during the respiratory cycle. When there is cardiac tamponade from a large pericardial effusion, the normal decrease in left ventricular preload during inspiration is accentuated, and blood pressure falls. In severe tamponade, this inspiratory fall can be detected easily by the absence of a palpable pulse during inspiration and a return of the pulse during exhalation. More subtle degrees of abnormal pulsus paradoxus may be detected by careful auscultation of the blood pressure as the cuff is deflated slowly. The first Korotkoff sound (K1) is heard, but only intermittently at first. The difference between this systolic blood pressure and the pressure at which a constant audible Korotkoff sound appears is the measured pulsus paradoxus. Values greater than 10 torr are abnormal. A measurement greater than 20 torr is considered severe and indicates that cardiac filling is seriously impaired by the effusion around the heart. An abnormally large variation in intrathoracic pressure also can produce a pulsus paradoxus, as during a severe asthma exacerbation. Normal heart rate changes during the respiratory cycle generally are diminished because normal vagal tone is removed during expiration. Sympathetic tone predominates during all respiratory phases in the presence of tamponade. Accordingly, sinus tachycardia is one of the signs of cardiac tamponade. Jugular venous pulsations may increase inappropriately during inspiration when filling of the right heart is impeded by the large effusion in the pericardial space. This sign is subtle. Increased jugular venous distention is seen in cardiac tamponade without significant change during respiration. The systolic blood pressure does fall during both inspiration and expiration once full tamponade results in systemic hypotension. It suggests the imminence of death. References: Roberts WC, Spray TL. Pericardial heart disease. Curr Probl Cardiol. 1977;2:1-71 Sagrista-Sauleda J, Merce J, Permanyer-Miralda G, Soler-Soler J. Clinical clues to the causes of large pericardial effusions. Am J Med. 2000;109:95-101 Critique 177. Preferred Response: D
[View Question] Extravasation of red blood cells into the skin produces erythematous or violaceous lesions that do not blanch. Small lesions (<2 mm) are termed petechiae, those of intermediate size (2 mm to 1 cm) are called purpura (Figure 177A), and larger lesions are referred to as ecchymoses. In general, platelet disorders produce petechiae, vasculitis causes purpura that is elevated (palpable purpura), and coagulation disorders result in ecchymoses that may be palpable. The presence of palpable purpura, particularly when accompanied by fever, should raise concern about the possibility of septicemia. The child described in the vignette has
features of acute, fulminant meningococcemia, including the abrupt onset of fever, palpable purpura concentrated on the buttocks and lower extremities, and an elevated white blood cell count. In this clinical setting, thrombocytopenia suggests the possibility of associated disseminated intravascular coagulation. Because this disease constitutes a medical emergency, prompt institution of antibiotic therapy is indicated. Pending confirmation of the responsible organism, a child suspected of having sepsis-induced purpura may be treated intravenously with vancomycin and ceftriaxone. If the presence of Neisseria meningitidis is confirmed, intravenous aqueous penicillin G may be substituted. Henoch-Schnlein purpura (HSP) is an immunoglobulin A-mediated systemic vasculitis of small vessels that affects the skin, gastrointestinal tract, joints, and kidneys. The cutaneous lesions of HSP (Figure 177B) may begin as erythematous macules or papules, but palpable purpura develops within several days. Lesions are concentrated in dependent areas; thus, in an ambulatory patient, the buttocks and lower extremities are most affected. Although lesions may mimic those of meningococcemia, children who have HSP do not appear systemically ill, are afebrile or have only a low-grade fever, often have associated abdominal or joint pain, and do not have thrombocytopenia. Although petechiae, purpura, and thrombocytopenia are characteristic of idiopathic thrombocytopenic purpura, affected children appear well, are afebrile, and lack leukocytosis. The earliest clinical manifestation and the hallmark of Lyme disease is erythema migrans, not purpura. This lesion begins as a solitary, erythematous macule or papule that enlarges to form a patch or annule. Children who have early Lyme disease generally do not appear ill, although fever, malaise, and headache may be present. Rocky Mountain Spotted Fever (RMSF) must be considered in a child who has fever and purpura and resides in or has traveled to an endemic area (eg, Oklahoma, North and South Carolina, Tennessee). Although the onset of RMSF may be abrupt, generally it is gradual and characterized by fever, headache, and myalgias. The rash begins on the second or third day of illness as erythematous blanching macules that involve the wrists, ankles, palms (Figure 177C), or soles. It then becomes petechial or purpuric and spreads centrally. Although thrombocytopenia is observed commonly in patients who have RMSF, the white blood cell count is normal or depressed during the first 4 to 5 days of illness. References: Baselga E, Drolet BA, Esterly NB. Purpura in infants and children. J Am Acad Dermatol. 1997;37:673-705 Edwards MS, Baker CJ. Meningococcal infections. In: McMillan JA, DeAngelis CD, Feigin RD, Warshaw JB, eds. Oskis Pediatrics: Principles and Practice. 3rd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 1999:980-984 Feigin RD, Boom ML. Rickettsial diseases. In: McMillan JA, DeAngelis CD, Feigin RD, Warshaw JB, eds. Oskis Pediatrics: Principles and Practice. 3rd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 1999:898-908
Weston WL, Lane AT, Morelli JG. Color Textbook of Pediatric Dermatology. 2nd ed. St Louis, Mo: Mosby, Inc; 1996:232-235 Critique 200. Preferred Response: B
[View Question] The patient described in the vignette has a right hemothorax, a collection of blood in the pleural space due to trauma. Physical findings of an acute hemothorax include respiratory distress, shock due to blood loss, and diminished breath sounds with dullness to percussion on the affected side. A thoracostomy tube should be inserted to evacuate the hematoma in any patient who has a radiologically significant hemothorax. Evacuation of the blood both reduces the risk for a clotted hemothorax and eventual restrictive lung disease and provides a method for evaluation of continuing blood loss. If the patient is in respiratory or circulatory distress and other physical findings suggest a hemothorax, tube thoracostomy should be performed before a chest radiograph is obtained. Continued bleeding at greater than 1 to 2 mL/kg per hour after chest tube placement is an indication for emergent operative thoracotomy, as is retained blood within the pleural cavity or an inability to re-expand the lung. There is no indication in the patient in the vignette for a diuretic such as furosemide. Endotracheal intubation should be considered for those in severe respiratory distress despite chest decompression with a chest tube. Elevation of the head of the bed is not advisable in a patient who has suffered significant acute blood loss. Tube thoracostomy in a child is performed as in an adult at the 5th intercostal space anterior to the midaxillary line. The tube is tunneled into the thoracic cavity over the rib above the skin insertion site to avoid damage to the intercostal vessels. Blood within the pleural space may tamponade a bleeding source, so a hemothorax should be evacuated slowly to accommodate potential new bleeding. O-negative blood should be available for emergency transfusion if type-specific blood is not available. Blood from the hemothorax may be collected in a system that allows for autotransfusion. The primary cause of hemothorax in children is laceration of the lung or of an intercostal artery following blunt trauma. Penetrating trauma is a less common cause, particularly among children. The pliability of a childs chest wall causes much of the force in blunt trauma to be transmitted to the lung, often resulting in damage to the pulmonary parenchyma, even in the absence of rib fractures. The force required to fracture a childs rib is significantly higher than that required for an adult. If rib fractures are present in a child, injury to underlying organs, such as liver, spleen, and lungs, should be suspected. Flail chest refers to a discontinuity in a section of the thoracic cage following fractures in two or more ribs on the same side. This condition is uncommon in children because rib fractures are rare. The chest wall instability leads to paradoxic motion of the involved section during inspiration and expiration. Most patients who have a flail chest require positive-pressure ventilation via an endotracheal tube to re-expand the lung and splint the injured section.
References: American College of Surgeons Committee on Trauma. Pediatric trauma. In: Advanced Trauma Life Support for Doctors: Student Course Manual. 6th ed. Chicago, Ill: American College of Surgeons; 1997:289-311 American Heart Association, American Academy of Pediatrics. Trauma resuscitation. In: Chameides L, Hazinski MF, eds. Pediatric Advanced Life Support. Dallas, Tex: American Heart Association; 1997:8-18-9 Kadish H. Thoracic trauma. In: Fleisher GR, Ludwig S, eds. Textbook of Pediatric Emergency Medicine. 4th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2000:1351-1352 Critique 221. Preferred Response: D
[View Question] The agitation, significantly increased respiratory rate, and acute carbon dioxide retention described for the girl in the vignette indicate impending respiratory failure. The most appropriate management is immediate endotracheal intubation. Agitation is common in hypoxia; somnolence or tachycardia may be due to either carbon dioxide retention or severe hypoxemia. Bradycardia is an ominous development, usually indicating severe respiratory failure, hypoxemia, and impending cardiac arrest. Acute carbon dioxide retention (hypercapnia) often results in flushing, agitation, confusion, tachycardia, and headache. The child described in the vignette has symptoms of bronchiolitis. The wheezing results from necrosis and sloughing of the respiratory epithelium caused by the toxic effect of the virus on the cells. Partial airway obstruction ensues. Although bronchodilators may be of some benefit in affected children who have underlying reactive airways, they are of little to no benefit for most children. Steroids have no proven benefit in the management of bronchiolitis, although they may be beneficial in the respiratory distress caused by croup. Similarly, racemic epinephrine is of limited value in bronchiolitis. The initial management of hypoxemia is administration of oxygen at the highest concentration available, but increasing the inspired concentration of administered oxygen is not appropriate treatment of carbon dioxide retention. References: American Academy of Pediatrics, American Heart Association. Airway and ventilation. In: Chameides L, Hazinski MF, eds. Pediatric Advanced Life Support. Dallas, Tex: American Heart Association; 1997:4-14-22 Stokes DC. Respiratory failure. Pediatr Rev. 1997;18:361-366 Critique 243. Preferred Response: C
[View Question]
Although reporting data are incomplete, at least 6,500 drowning deaths occur each year in the United States. The rates are highest for children younger than age 5 and between the ages of 15 and 24 years. Males drown four times more frequently than females. Drownings peak during the summer months and are most common in the southern and western United States. Most of the pathology in drowning victims is related to the duration of asphyxia from the time of submersion until adequate respiration is restored. The brain and heart are most vulnerable to anoxic and ischemic injury. Other organs, such as the liver and kidneys, are relatively resistant to anoxia, but are sensitive to ischemic injury. The prognosis for near-drowning victims depends primarily on the degree of brain anoxia sustained. For most, the outcome is determined by the duration of submersion. Prolonged submersion (>25 min) is an unfavorable prognostic indicator. Other unfavorable prognostic indicators are apnea or coma at the time of admission to the emergency department and initial arterial pH of less than 7.0. Children who resume spontaneous respiration after initial resuscitation may survive with little or no cerebral insult. Ninety-five percent of victims who require fewer than 10 minutes of cardiopulmonary resuscitation survive with no or only mild neurologic impairment. References: DeNicola LK, Falk JL, Swanson ME, Gayle MO, Kissoon N. Submersion injuries in children and adults. Crit Care Clin. 1997;13:477-502 Fiser DH. Near-drowning. Pediatr Rev. 1993;14:148-151 Shaw KN, Briede CA. Submersion injuries: drowning and near-drowning. Emerg Med Clin North Am. 1989;7:355-370 Critique 263. Preferred Response: C
[View Question] The most common types of supraventricular tachycardia (SVT) in childhood are ones in which the electrical wavefront reciprocates from the atria to the ventricles and back up to the atria (re-entry type tachycardias). In young infants, the most common form is re-entry in which the electrical wavefront travels from atria to ventricles over the normal atrioventricular (AV) node and specialized conduction tissues (bundle branches) and returns to the atria over a retrograde conducting accessory pathway. This type of SVT is termed atrioventricular re-entry tachycardia (AVRT). AVRT is also common among adolescents, although at that age, re-entry within the tissues of the AV node also is a common SVT mechanism. In this situation, the atrial-to-ventricular conduction is antegrade over a slow AV node pathway, and re-entry to the atrium occurs within the AV node over fast-conducting tissue. The retrograde P waves are, therefore, nearly simultaneous with the QRS complex
that marks ventricular activation. In AVRT, the retrograde P waves usually are discernible as small deflections in the ST segment following the QRS complexes. Because both common forms of SVT require atrial-to-ventricular conduction over the AV node to sustain the re-entry circuit, it is possible to convert these arrhythmias to normal sinus rhythm by temporary conduction block of the AV node. Vagal maneuvers, such as application of an ice bag to the face of young infants or carotid sinus massage in older children, may block AV node conduction sufficiently to terminate SVT. When these maneuvers are not effective, drugs that block conduction in the AV node may be administered. Adenosine is a very effective AV node-blocking drug. It has a very short half-life (measured in seconds), which affords a higher margin of safety than other acute-acting antiarrhythmic drugs. Nevertheless, direct current electrical cardioversion always should be immediately available when using adenosine because the drug rarely can cause atrial fibrillation. Some patients who have SVT may have Wolff-Parkinson-White (WPW) (Figure 263A) syndrome that is not apparent until conversion out of SVT. Atrial fibrillation can be life-threatening in such patients due to extremely rapid conduction of atrial fibrillation over the accessory pathway. This warrants the requirement for electrical cardioversion availability. A repeat dose of adenosine is an option when short-lived AV node block from adenosine is not sufficient to prevent a rapid recurrence of sustained re-entry SVT, as reported in the vignette. However, another method to treat the SVT might be preferable to avoid recurrence of the SVT. Diltiazem is a calcium channel-blocking drug (Vaughn Williams class IV) that can be titrated as an intravenous drip to allow controlled blocking of AV node conduction. As such, it is a useful drug for SVT control in adolescents and older children. It has replaced intravenous verapamil in most emergency departments because of its shorter half-life and superior titratability. Similar to verapamil, another calcium channel blocker, diltiazem never is used in young infants who have SVT in whom excessive bradycardia, hypotension, and even cardiac arrest are possible. Amiodarone is a powerful antiarrhythmic drug of the Vaughn Williams class III type (prolongs repolarization), although its pharmacologic effects are not limited to repolarization of cardiac tissues. Intravenous amiodarone is indicated for life-threatening ventricular tachycardia and ventricular fibrillation. It has replaced intravenous lidocaine in the 2001 Advanced Cardiac Life Support guidelines for treatment of unstable ventricular tachycardia. Intravenous amiodarone also has been used in pediatric patients who have refractory serious forms of SVT, most notably for junctional ectopic tachycardia after open heart surgery. However, it is not indicated as a first-line drug for simple re-entry type SVT in children. Intravenous digoxin often is used in infants who have relapsing SVT after initial conversion to sinus rhythm. Its efficacy and safety in infants are well-established. Typically, spontaneous conversions from SVT to sinus rhythm will be noted hours after administration
of the first dose of intravenous digoxin (usually one half of the total digitalizing dose) and become gradually more sustained until SVT is controlled. This approach is acceptable in an infant in whom SVT often is tolerated well and in whom other medications may be potentially dangerous or difficult to use. However, waiting for hours to control tachycardia in an adolescent is inappropriate when there are alternatives for more rapid arrhythmia control. Moreover, digoxin may pose a hazard in the adolescent who has SVT and WPW syndrome. If SVT degenerates into atrial fibrillation, dangerously rapid conduction of the atrial fibrillatory impulses to the ventricle can occur, and digoxin may enhance this conduction. Intravenous quinidine, a class Ia drug, rarely is used in pediatric practice. QT prolongation and a small but real risk of torsades de pointes, a malignant polymorphic ventricular tachycardia, are associated with quinidine use. Further, the intravenous form is significantly associated with serious hypotension. Synchronized direct current electrical cardioversion can be used to treat re-entry SVT, but it is likely to have the same result as adenosine for the patient in the vignette, that is, only temporary conversion to normal sinus rhythm. References: Case CL. Diagnosis and treatment of pediatric arrhythmias. Pediatr Clin North Am. 1999;46:347-354 Jaeggi E, Chiu C, Hamilton R, Gilljam T, Gow R. Adenosine-induced atrial pro-arrhythmia in children. Can J Cardiol. 1999;15:169-172 Kugler JD, Danford DA. Management of infants, children, and adolescents with paroxysmal supraventricular tachycardia. J Pediatr. 1996;129:324-328 2001 Self-Assessment Exercise XXIX. Critical care [Return to Category List] Questions [Print Directions] Question 21. Answer.
A 10-year-old boy is brought to the emergency department after being struck by a car while riding his bicycle. He was not wearing a helmet. Physical examination immediately upon arrival reveals that he is responsive to painful stimuli only by moaning. His pupils are equal, small, and reactive. Of the following, the sign MOST LIKELY to be associated with increasing intracranial pressure in this patient is A. hyperventilation
B. C. D. E.
hypotension hypothermia nystagmus tachycardia
Question 102. Answer. You are evaluating a 15-year-old girl for muscular weakness, weight loss, and dizziness of 3 months' duration. She has no history of recent infection. Findings on physical examination include: blood pressure, 85/40 mm Hg; pulse, 120 beats/min; respiratory rate, 30 breaths/min; and oral thrush. Laboratory evaluation reveals: creatinine, 106 mcmol/L (1.2 mg/dL); blood urea nitrogen, 15 mmol/L of urea (42 mg/dL); sodium, 125 mmol/L (125 mEq/L); potassium, 6.5 mmol/L (6.5 mEq/L); chloride, 98 mmol/L (98 mEq/L); bicarbonate, 16 mmol/L (16 mEq/L); glucose 3.33 mmol/L (60 mg/dL); urine sodium, 80 mmol/L (80 mEq/L); urine potassium, 2 mmol/L (2 mEq/L); and urine specific gravity, 1.035. Of the following, the MOST likely diagnosis is A. B. C. D. E. acute tubular necrosis adrenal insufficiency diuretic abuse ipecac abuse syndrome of inappropriate secretion of antidiuretic hormone
Question 149. Answer. The mother of a 3-year-old reports that her son has begun to cough and have difficulty breathing. She was keeping him home from preschool today because he had a cough and upper respiratory tract infection without fever. The MOST likely cause of this child's symptoms is A. B. C. D. E. aspiration pneumonia bacterial pneumonia foreign body aspiration reactive airway disease vascular ring
Question 236. Answer.
You are examining a 10-year-old girl who sank to the bottom of the pool after a dive. Rescuers could detect no pulse, but she awakened before they initiated cardiopulmonary resuscitation. The girl's mother had been treated for epilepsy for 15 years and died at age 28 during a seizure. Of the following, the parameter MOST likely to be abnormal in this girl is A. B. C. D. E. coronary artery anatomy on angiography epileptiform activity on electroencephalography ionized calcium level on serum chemistry profile QT measurement on electrocardiography septal thickness on echocardiography
Answers Critique 21. Preferred Response: A
[View Question] Trauma is the leading cause of death in children older than 1 year of age, and head trauma with central nervous system injury accounts for most of these deaths. Common mechanisms for injury include falls, motor vehicle crashes, and bicycle accidents. Children who have head injuries must be evaluated systematically. The evaluation must include careful attention to the airway, breathing, and circulation, as well as neurologic status and any other accompanying injuries. The initial neurologic examination should include assessment of the level of consciousness, pupillary response, and signs of lateralized extremity weakness. Careful, repeated examinations are essential. The skull, or cranium, contains the brain, cerebrospinal fluid (CSF), and blood. Intracranial volume may increase following trauma due to hemorrhage, brain swelling, obstruction of CSF flow, or increased cerebral blood flow, all of which may lead to increased intracranial pressure (ICP) and, if untreated, subsequent cerebral herniation. Recognition of the signs and symptoms of increased ICP and appropriate management if increased ICP occurs are essential to the optimal outcome of the child who suffers a head injury. The most common signs of critically increased ICP after head trauma are unilateral or bilateral dilated pupils, poorly reactive pupils, and a decreased level of consciousness. Papilledema is a late finding that usually reflects the presence of elevated ICP that has developed slowly over weeks to months. Herniation of brain tissue may occur at several locations, depending on the site of the lesion. Uncal herniation (as seen with epidural hematoma) is associated with unilateral compression of cranial nerve III and compression of the brainstem. Clinical signs include an ipsilateral dilated and unresponsive pupil, central hyperventilation or Cheyne-Stokes respirations (hyperpnea followed by apnea), and contralateral hemiparesis. Central
herniation, due to diffuse brain swelling, is associated with small pupils that are initially reactive, Cheyne-Stokes respirations or central hyperventilation, and decorticate progressing to decerebrate posturing. Accordingly, hyperventilation is an important sign of increasing ICP. As ICP increases further, Cushing triad may be seen, characterized by bradycardia, hypertension, and irregular respirations. Tachycardia is not a common response to increased ICP. Hypotension and hypothermia are unusual and may occur as preterminal events. Dysconjugate gaze, not nystagmus, may be seen. References: Larsen GY, Goldstein B. Consultation with the specialist: increased intracranial pressure. Pediatr Rev. 1999;20:234-239 Nelson DS. Coma and altered level of consciousness. In: Fleisher GR, Ludwig S, eds. Textbook of Pediatric Emergency Medicine. 4th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2000:165-175 Zuckerman GB, Conway EE Jr. Accidental head injury. Pediatr Ann. 1997;26:621-632 Critique 102. Preferred Response: B
[View Question] Signs of intravascular volume depletion, oral thrush, prerenal failure, hyponatremia, hyperkalemia, and metabolic acidosis are consistent with the diagnosis of adrenal insufficiency. The manifestations of adrenal insufficiency include fasting hypoglycemia, decreased gastric acidity, nausea, vomiting, fatigue, headaches, muscle weakness, weight loss, salt craving, and hypotension. Classically, these patients have metabolic acidosis, hyponatremia (due to sodium losses in the urine and vomiting), and hyperkalemia (due to inability to excrete potassium). Some may sustain normal electrolyte homeostasis, except during stress, when an acute adrenal crisis may develop. The crisis is a medical emergency and presents with symptoms similar to those described in the vignette. Treatment includes administration of hydrocortisone intravenously and volume expansion. The syndrome of inappropriate secretion of antidiuretic hormone causes mild intravascular volume expansion and eventually is responsible for natriuresis. Although antidiuretic hormone levels are elevated in the patient described in the vignette, who has a high urine specific gravity of 1.035, the levels are appropriate for her hypovolemic status. Abuse of diuretics and ipecac, which is common among patients who have eating disorders, can be characterized by electrolyte disturbances and weight loss. However, hypokalemia and metabolic alkalosis would be expected. The blood urea nitrogen-to-creatinine ratio of greater than 35:1 and the elevated urine specific gravity in the child in the vignette suggest the presence of prerenal failure rather than acute tubular necrosis. Primary adrenal insufficiency or failure is rare in childhood and is caused by Addison disease (autoimmune adrenocortical insufficiency). The most common cause of Addison
disease is autoimmune destruction of the adrenal cortex with sparing of the adrenal medulla. Most patients have antiadrenal cytoplasmic antibodies and may have immunoglobulins that block the growth and steroidogenic effects of adrenocorticotropic hormone (ACTH). Although it may be idiopathic, Addison disease often is a component of two distinct autoimmune polyendocrinopathies. In type I, also known as autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy, mucocutaneous candidiasis frequently is the first manifestation, followed by hypoparathyroidism and Addison disease. Other associated disorders include gonadal failure, alopecia, vitiligo, keratopathy, enamel hypoplasia, nail dystrophy, intestinal malabsorption, and chronic active hepatitis. Approximately 10% of patients who have type I polyendocrinopathy develop hypothyroidism and type 1 diabetes mellitus. The disorder is autosomal recessive, and the gene has been encoded to the long arm of chromosome 21 (21q22.3). In type II autoimmune polyendocrinopathy, Addison disease is associated with autoimmune thyroid disease or type 1 diabetes mellitus. Gonadal failure, vitiligo, alopecia, and chronic atrophic gastritis with or without pernicious anemia may occur. Human leukocyte antigen (HLA)-D3 and HLA-D4 predominate in these patients. Other causes of primary adrenal insufficiency or failure include congenital adrenal hyperplasia, bilateral adrenal hemorrhage (Waterhouse-Friderichsen syndrome), trauma, infection (eg, tuberculosis), thrombosis, tumor metastasis, and degeneration (eg, adrenoleukodystrophy). The diagnosis of adrenal insufficiency is confirmed by demonstrating low or absent plasma cortisol and aldosterone levels. Plasma renin activity always is elevated, and ACTH levels are high. A fasting 8 am cortisol level is low and is not stimulated with ACTH. Antiadrenal cytoplasmic antibodies should be measured. Other endocrine gland function and antibodies to the other glands should be assessed. Maintenance treatment includes replacement with glucocorticoid and mineralocorticoid. References: August GP. Treatment of adrenocortical insufficiency. Pediatr Rev. 1997;18:59-62 Donohoue PA. Adrenal cortex. In: McMillan JA, DeAngelis CD, Feigin RD, Warshaw JB, eds. Oski's Pediatrics: Principles and Practice. 3rd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 1999:1812-1819 Levine LS, DiGeorge AM. Adrenocortical insufficiency. In: Behrman RE, Kliegman RM, Jenson HB, eds. Nelson Textbook of Pediatrics. 16th ed. Philadelphia, Pa: WB Saunders Co; 2000:1725-1729 Werbel SS, Ober KP. Acute adrenal insufficiency. Endocrinol Metab Clin North Am. 1993;22:303-328 Critique 149. Preferred Response: D
[View Question] Approximately 85% of children who have asthma experience an episode of wheezing when they develop an upper respiratory tract infection. The child described in the vignette is experiencing an initial episode of wheezing or reactive airway disease (RAD). As the initial event, it does not meet the criteria for the diagnosis of asthma, but it probably represents an exacerbation of RAD triggered by an upper respiratory tract infection. Aspiration pneumonia is not a likely possibility in a child who has had no emesis and is neurologically normal. Bacterial pneumonia is not likely in an afebrile child who has an upper respiratory tract infection. A vascular ring or foreign body aspiration is unlikely without a previous history of respiratory symptoms. Appropriate evaluation for the child described in the vignette includes chest radiography to help distinguish between foreign body aspiration, pneumonia, and a vascular ring. Vascular rings occasionally are diagnosed on routine chest radiography by the position of the aorta. References: Holroyd HJ. Foreign body aspiration: potential cause of coughing and wheezing. Pediatr Rev. 1998;10:59-63 Lemanske RF Jr, Green CG. Asthma in infancy and childhood. In: Middleton E Jr, Ellis EF, Yunginger JW, et al, eds. Allergy Principles & Practice. 5th ed. St Louis, Mo: Mosby-Year Book, Inc; 1998:877-900 National Asthma Education Program, Expert Panel Report II. Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: US Department of Health and Human Services, Public Health Service, National Institutes of Health; 1997:No. 97-4051 Critique 236. Preferred Response: D
[View Question] Congenital long QT syndrome (LQTS) (Figure 236A) is associated with episodic syncope, brief generalized seizures, episodes of near-sudden death, and sudden death. These are caused by a malignant form of ventricular tachycardia (Figure 236B) called torsade de pointes. This polymorphic rapid ventricular tachycardia results in loss of effective cardiac output and pulse. A brief episode that lasts seconds results in syncope. Torsade of intermediate duration, usually 30 seconds to 1 minute, may cause a generalized tonic-clonic seizure due to cerebral hypoperfusion. Longer duration of torsade results in sudden death. In one series, 9% of pediatric cases of LQTS presented with cardiac arrest, 26% with syncope, 10% with seizures, and 6% with palpitations. When in normal sinus rhythm, electrocardiography shows repolarization abnormality with abnormally prolonged QT interval (duration from onset of QRS complex to end of T wave). Torsade de pointes may occur at any time in a patient who has LQTS, but a sudden catecholamine surge often is the trigger for malignant ventricular tachycardia. Near-sudden
deaths occurring when a loud alarm sounds or at the time of hitting the water after a dive have been reported in several cases of LQTS. For this reason, provocative testing with epinephrine infusion sometimes has been used to diagnose a predilection for malignant arrhythmia. Many cases of LQTS are familial, most often with a dominant pattern of inheritance. Clinical expression of the LQTS gene may vary significantly within a family. Romano-Ward syndrome has been used to refer to dominantly inherited LQTS. It now is appreciated that three or more distinct gene defects may be found in families who have inherited LQTS. Most involve mutations in potassium ion channels in the sarcolemmal membrane, but one form of LQTS apparently is caused by a mutation in the sodium channel. One clinical form of LQTS, the Jervell and Lange-Nielsen syndrome, appears to be inherited as an autosomal recessive condition, sometimes associated with deafness. Measurement of the QT interval on electrocardiography should be corrected for heart rate as the QT interval shortens in response to increased heart rates, as with exercise. Most commonly, Bazetts formula is used: QT corrected (QTc) = measured QT/square root of measured RR interval (in seconds). Values in excess of 0.45 seconds are possibly abnormal. In the long QT syndrome, corrected QT intervals may exceed 0.50 seconds, and sometimes there are bizarre giant or alternating morphology T waves. Because variations in the QTc may occur in patients who have LQTS, this interval must be measured carefully on screening electrocardiography performed on individuals who have any of the symptoms that may be caused by LQTS, such as the girl described in the vignette. Screening electrocardiography to exclude LQTS is indicated for any patient who has a syncopal episode, a brief generalized seizure, or near-sudden death. Anomalous or aberrant coronary arterial patterns (Figure 236C) may cause sudden death due to episodes of cardiac ischemia, especially during exercise. The most common potentially dangerous form of this anomaly is origin of the left coronary artery from the right aortic sinus rather than the normal left aortic sinus. The abnormally shaped left coronary arterial ostium is believed to create the equivalent of coronary arterial stenosis. Evaluation of the coursing pattern of the coronary arteries is indicated for young individuals who experience near-sudden death precipitated by exercise. The family history of sudden death in a patient who has recurrent seizures, as for the girl in the vignette, is not typical for congenital coronary anomaly. Epilepsy can be familial, but death during a seizure, as reported for the mother of the girl in the vignette, immediately raises the suspicion of LQTS rather than epilepsy. Tetany and seizures can result from hypocalcemia (eg, hypoparathyroidism). However, tetany is not suggested in the vignette. Although hypocalcemia does cause prolongation of the QT interval on electrocardiography, serum calcium measurements are normal in patients who have LQTS. Hypertrophic cardiomyopathy, a condition sometimes referred to as idiopathic hypertrophic subaortic stenosis, can be associated with sudden death and syncope and can be inherited dominantly. It is caused by multiple mutations in several of the cardiac muscle
proteins, most commonly myosin heavy chain mutations. However, the family history of seizures followed by a sudden death is more suggestive of LQTS. References: Ackerman MJ. The long QT syndrome. Pediatr Rev. 1998;19:232-238 Carboni MR, Garson A Jr. Ventricular arrhythmias. In: Garson A Jr, Bricker JT, Fisher DJ, Neish SR, eds. The Science and Practice of Pediatric Cardiology. 2nd ed. Baltimore, Md: Williams & Wilkins; 1998:2121-2168 Emmanouilides GC, Allen HD, Riemenschneider TA, Gutgesell HP. Arrhythmias, syncope, sudden death, and cardiopulmonary arrest. In: Clinical Synopsis of Moss and Adams' Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adult. Baltimore, Md: Williams & Wilkins; 1998:728-729 2000 Self-Assessment Exercise XXIX. Critical care [Return to Category List] Questions [Print Directions] Question 21. Answer.
A 4-month-old girl has failed to thrive, feeds poorly, and is tachypneic. Findings on physical examination include a third heart sound, faint expiratory rales, and hepatomegaly. Of the following, the MOST likely explanation for these findings is A. B. vein C. D. E. anomalous origin of the left coronary artery from the pulmonary artery atrial septal defect with partial anomalous drainage of the right upper pulmonary
tetralogy of Fallot with severe pulmonic stenosis transposition of the great arteries with intact ventricular septum truncus arteriosus with severe truncal valve incompetence Answer.
Question 59.
A healthy-appearing 6-month-old infant has a resting heart rate of 55 beats/min that increases to 70 beats/min while crying. When quiet, he has a soft, vibratory ejection murmur. Careful inspection of the extended neck reveals an intermittent brisk jugular venous pulse wave. Of the following, the MOST likely explanation for these findings is A. carditis due to Lyme disease
B. C. D. E.
congenital complete heart block congenital long QT syndrome familial dysautonomia sick sinus syndrome
Question 115. Answer. A 4-year-old child is struck by a car when crossing the street. At the emergency department, examination of the child's abdomen reveals distention, diffuse tenderness, and absent bowel sounds. Of the following, the best INITIAL radiologic study to evaluate this abdominal injury is A. B. C. D. E. computed tomography intravenous pyelography magnetic resonance imaging plain radiography ultrasonography
Question 164. Answer. An 11-month-old girl is brought to the emergency department because she is having a generalized seizure. She had been playing all day in an above-ground pool when she began to jerk. There is no history of recent fever or trauma, and her development has been normal. Intravenous administration of appropriate doses of anticonvulsants results in partial cessation of the seizure activity. Of the following, the test that is MOST likely to explain these findings is A. B. C. D. E. a culture of the cerebrospinal fluid magnetic resonance imaging of the brain measurement of the tympanic membrane temperature serum electrolyte concentrations skull radiography
Question 217. Answer. A 4-year-old girl presented 18 hours ago to the emergency department in severe respiratory distress and septic shock. A diagnosis of severe viral pneumonia was made, and she now is in the pediatric intensive care unit, intubated and on assisted ventilation. Over the past few hours, she has become more hypoxemic on current ventilator settings.
Of the following, the BEST way to increase her oxygenation is to A. B. C. D. E. decrease the inspiratory time decrease the peak inspiratory pressure increase the expiratory time increase the positive end-expiratory pressure increase the rate (breaths/min)
Answers Critique 21 Preferred Response: A
[View Question] Symptoms of congestive heart failure in an infant can be subtle. Failure to thrive is common and probably is due to increased caloric expenditure from tachypnea, mild persistent tachycardia, and an underlying increased metabolic rate related to an elevation of circulating endogenous catecholamines. In addition, when symptoms of cardiac failure are due to a large left-to-right shunt at the ventricular level, some degree of increased metabolic rate also may be attributed to the demands of increased cardiac output of the left ventricle, which receives two or even three times the usual pulmonary venous return during each diastolic filling period. In infants who have congestive heart failure, tachypnea is related to pulmonary venous congestion. Rales or occasionally wheezing may be present. Difficulty with feeding usually occurs in the setting of mild chronic respiratory distress and also may be due in part to vascular congestion of the gut. The infant's caloric intake is unable to meet these increased demands. Vascular congestion may be appreciated on physical examination as hepatomegaly, as noted in the vignette, which is more common in infants who have heart failure than noticeable edema. Activation of the renin-angiotensin axis partially explains the increases in circulating and extravascular fluid volumes in these patients. Left ventricular enlargement causes a gallop or prominent third heart sound during filling, which is audible after the second heart sound. Poor left ventricular function is less common than large ventricular left-to-right shunting as a cause of the symptoms of congestive failure in infants. However, dilated cardiomyopathies, myocarditis, and ischemic cardiomyopathy from congenital coronary arterial anomalies all can occur in infants. Of the options listed, the most likely explanation for the findings of congestive heart failure described in the vignette is an anomalous origin of the left coronary artery from the pulmonary artery. As a result of myocardial ischemia, affected infants often display all of the signs of congestive heart failure without any significant heart murmur from turbulent flow across a stenotic cardiac valve or across a ventricular septal defect.
Truncus arteriosus with severe truncal valve incompetence can cause congestive heart failure in infants, but it is accompanied by a loud murmur of truncal valve incompetence. Tetralogy of Fallot can be associated with signs of heart failure in infants when there is a large left-to-right shunt (pink tetralogy). However, as the degree of pulmonic stenosis becomes more severe, signs of congestive failure usually resolve and the infant becomes cyanotic. An atrial septal defect (ASD) can cause a significant left-to-right shunt, but the excess pulmonary blood flow does not return to the left ventricle, and the shunt is well tolerated without any evidence of heart failure. An ASD that is associated with partial drainage of a pulmonary vein to the superior vena cava or right atrium also is not characterized by congestive heart failure. In contrast, patients who have total anomalous pulmonary venous return will develop a torrential left-to-right shunt and signs of heart failure. Transposition of the great arteries is associated with increased pulmonary blood flow, but affected infants should present with severe cyanosis within the first month of life. Congestive heart failure would be the predominant symptom in an infant who has transposition of the great arteries only when there is both a large ventricular septal defect and a large ASD. References: Gessner IH. Heart failure in the infant. In: Gessner IH, Victoria BE, eds. Pediatric Cardiology: A Problem Oriented Approach. Philadelphia, Pa: WB Saunders Co; 1993: 122-125 Hoffman JIE. Congenital anomalies of the coronary vessels and the aortic root. In: Emmanouilides GC, Riemenschneider TA, Allen HD, Gutgesell HP, eds. Moss and Adams Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adult. 5th ed. Baltimore, Md: Williams & Wilkins; 1995:769-790 Critique 59 Preferred Response: B
[View Question] The 6-month-old infant described in the vignette has a resting heart rate of 55 beats/min that increases to 70 beats/min while crying. Physical examination reveals a soft, vibratory ejection murmur and an intermittent visible brisk jugular venous pulse wave. These findings are most consistent with the diagnosis of congenital complete atrioventricular (AV) block. In some affected newborns, the heart rate can be fast enough while crying that the diagnosis is missed until bradycardia is discovered on a subsequent examination performed months or even years later. In addition, some cases of congenital AV block progress from second- or even first-degree AV block at birth to complete AV block months later. In complete heart block, AV dissociation develops and there is no relationship between the atrial rate, which is normal, and the ventricular rate, which is slower. Occasionally a random atrial contraction will occur simultaneously with ventricular contraction. On physical examination this is appreciated as cannon A waves that are seen easily as jugular venous pulsations occurring at the time of atrial contraction while the mitral and tricuspid valves are closed. Functional flow murmurs are common among infants and children who have heart block because the slow heart rate results in a compensatory enlargement of the ventricular chambers. Cardiac output is preserved by delivering a larger stroke volume with each beat.
Congenital heart block characteristically is due to disease within the AV node. However, the His-Purkinje system below the AV node is normal. Therefore, an escape rhythm originates in the AV junction and is called a junctional rhythm. This rhythm is faster than an escape rhythm that originates from the ventricles and usually is not associated with the symptoms that occur when there is heart block from disease or damage lower in the HisPurkinje system, which may include syncope and sudden death. Surgical trauma usually causes the latter type of complete heart block, which requires treatment with a permanent pacemaker. Congenital complete heart block often can be managed without placement of a permanent pacemaker. Nevertheless, it has become evident in recent years that the prognosis is not uniformly benign. In utero hydrops and fetal demise have occurred in association with congenital heart block when the (presumed) junctional escape rhythm is inadequate. Sudden death also has been reported in affected infants. If the average heart rate is less than 50 beats/min, treatment with a permanent pacemaker should be recommended, even in asymptomatic infants. In many cases, the etiology of congenital complete heart block is the presence of maternal antibodies that cross-react with fetal cardiac tissue. These antibodies may develop in mothers who have systemic lupus erythematosus or similar autoimmune diseases. Typically there is no clinical maternal illness, but the maternal antibodies anti-Ro (SS-A) or anti-LA (SS-B) are present. The benefit of immune-modulating therapies in a fetus who has newly diagnosed heart block are under investigation. Lyme disease can cause AV block, but this is a less likely etiology than congenital AV block in a 6-month-old infant. Congenital long QT syndrome may result in life-threatening ventricular tachycardia (torsade de pointes). Some affected infants exhibit a resting sinus bradycardia, but the intermittent cannon A waves from AV dissociation are not characteristic. Very rarely, the QT prolongation in such infants is so severe that the ventricles remain refractory to depolarization when the sinus P wave occurs within the late T wave. These infants have a grave prognosis. In severe QT prolongation, the interval between two QRS complexes is long enough to allow electrical recovery, and the heart block is seconddegree, with 2-to-1 AV conduction rather than complete AV block. Thus, cannon A waves would not be intermittent, but would occur at regular intervals. Familial dysautonomia is a rare syndrome that involves such clinical abnormalities as feeding problems, excessive sweating, temperature instability, and ataxia. Hypertension and cyclic vomiting may occur in association with autonomic crises in children who are older than 3 years of age, but bradycardia and complete heart block do not occur. Sick sinus syndrome unrelated to previous surgery for congenital heart disease is extremely rare in infancy. References: Epstein ML. Disturbances of cardiac rhythm. In: Gessner IH, Victorica BE, eds. Pediatric Cardiology: A Problem Oriented Approach. Philadelphia, Pa: WB Saunders Co; 1993:167-181
Fish F, Benson DW Jr. Disorders of cardiac rhythm and conduction. In: Emmanouilides GC, Riemenschneider TA, Allen HD, Gutgesell HP, eds. Moss and Adams Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adult. 5th ed. Baltimore, Md: Williams & Wilkins; 1995:1555-1571 Critique 115 Preferred Response: A
[View Question] Abdominal trauma is the most common cause of unrecognized fatal injury in childhood, and blunt trauma from motor vehicle crashes causes more than 50% of the abdominal injuries seen in children. The initial approach to a child who has a suspected abdominal injury, as in any victim of trauma, is careful and systematic assessment and attention to the airway, breathing, and circulation. Circulatory compromise is common among children who have abdominal trauma, most often due to intra-abdominal hemorrhage. The spleen is injured most frequently, followed by injuries to the liver and kidneys. Computed tomography (CT) is the best initial radiologic study to assess the child who has suspected abdominal trauma, such as the one described in the vignette. It is highly sensitive and specific and has replaced diagnostic peritoneal lavage except when there is extreme hemodynamic instability or a need for immediate neurosurgical intervention. Abdominal injuries least likely to be identified by CT include small hollow viscous perforations and pancreatic injury. One limitation of CT is that the patient must be relatively stable before being sent to the radiology department. Intravenous pyelography will document renal injury, but it has little utility in evaluating multisystem trauma that could include the liver, spleen, and other intraabdominal organs. Magnetic resonance imaging is not useful in the setting of acute trauma, and plain radiography is too insensitive and nonspecific for intra-abdominal injuries to be beneficial. Ultrasonography has been used in the evaluation of abdominal trauma for several years in Europe and Japan and has been shown to be very sensitive and specific in identifying intraperitoneal hemorrhage in adults. Its usefulness in pediatric patients has yet to be evaluated satisfactorily. Ultrasonography also does not identify specific organ injury. References: Cantor RM, Leaming JM. Evaluation and management of pediatric major trauma. Emerg Med Clin North Am. 1998; 16:229-256 Haller JA Jr. Blunt trauma to the abdomen. Pediatr Rev. 1996;17:29-31 Saladino RA, Lund DP. Abdominal trauma. In: Fleisher GR, Ludwig S, eds. Textbook of Pediatric Emergency Medicine. 3rd ed. Baltimore, Md: Williams & Wilkins; 1993:1167-1174 Critique 164 Preferred Response: D
[View Question]
Infants and children playing in a swimming pool are much more likely than adults to swallow substantial amounts of water. An 11-month-old infant can swallow enough water to cause a precipitous decrease in his or her serum sodium concentration, which could result in seizures that are only partially responsive to anticonvulsants. The infant described in the vignette is developmentally normal. Her most recent activities consisted of playing with family members in an above-ground pool throughout an entire day. There is no mention of trauma or intercurrent illness. Accordingly, measurement of serum electrolyte concentrations is most likely to reveal the etiology of the seizure as hyponatremia resulting from water intoxication. A toxic ingestion also must be considered when seizure activity develops in a previously healthy child. The most common type of seizure in infants is a febrile seizure, which typically is a generalized tonic-clonic seizure. A rapid rise in the temperature appears to trigger the seizure, which may last several minutes. The prolonged duration of the seizure activity described in the vignette is not characteristic of a febrile seizure. Questioning the parents usually will reveal the presence of an acute illness and fever. Cerebrospinal fluid should be analyzed and cultured to exclude meningitis or encephalitis in a child who has seizures in conjunction with other findings suggestive of meningitis (eg, fever, bulging fontanelle, nuchal rigidity, cranial nerve palsies). However, a lumbar puncture would not be performed immediately in an afebrile child who had none of these findings. Magnetic resonance imaging of the brain is helpful in confirming a suspected intracranial mass, but this would be unlikely in a child who has no other neurologic findings. Skull radiography also is unlikely to be revealing in the absence of a history of trauma. Measurement of the tympanic membrane temperature can help to establish the presence of a fever, but an elevated temperature probably would have been noted by a parent following the onset of the seizure activity. References: Harmon W, Mandel J. Disorders of sodium balance. In: Avery ME, First LR, eds. Pediatric Medicine. 2nd ed. Baltimore, Md: Williams & Wilkins; 1994:675-676 Hellerstein S. Fluid and electrolytes: clinical aspects. Pediatr Rev. 1993;14:103-115 Keating JP, Schears GJ, Dodge PR. Oral water intoxication in infants. An American epidemic. Am J Dis Child. 1991;145:985-990 Critique 217 Preferred Response: D
[View Question] Acute respiratory distress syndrome (ARDS) is precipitated by a diffuse alveolar insult that may be caused by shock, trauma, pneumonia, near-drowning, aspiration, or burns. It is a syndrome of acute lung dysfunction characterized by tachypnea and hypoxemia, patchy infiltrates on chest radiography, and a decrease in lung compliance. Cardiogenic pulmonary
edema and chronic pulmonary disease must be excluded as causes of the dysfunction. The exact mechanism of injury is unclear. Pulmonary edema occurs because alveolar capillary membranes have increased permeability. ARDS is characterized histologically by diffuse alveolar epithelial and endothelial damage and the deposition of water, solutes, protein, and cellular elements in the interstitium and air spaces. Patients of any age may be affected. Signs and symptoms arise a few hours to several days after the precipitating event and include tachypnea, hypoxemia, and worsening infiltrates on chest radiography. Findings after intubation and mechanical ventilation include decreasing lung compliance and increasing need for oxygen, as described for the girl in the vignette. The use of positive end-expiratory pressure (PEEP) is a mainstay of treatment for pulmonary edema and ARDS in patients who are receiving mechanical ventilation. PEEP is the residual pressure maintained upon opening of the airway and at the end of expiration. PEEP improves oxygenation by increasing functional residual capacity due to recruitment of collapsed alveoli, redistributing of lung water from alveoli to the interstitium, optimizing the ventilation/perfusion ratio, and preventing collapse in small airways and alveoli. PEEP may have deleterious effects, such as a reduction in cardiac output by reducing venous return to the heart and decreasing compliance of the left ventricle. Careful fluid management of a patient who is receiving PEEP is essential. Decreasing the inspiratory time or the peak inspiratory pressure in a patient who has pulmonary edema will worsen oxygenation because lung compliance will be decreased. Increasing the breathing rate will affect primarily alveolar ventilation, which will translate into a decreased carbon dioxide level rather than improving the oxygenation. Increasing the expiratory time, thereby allowing increased passive expiration, also will affect primarily carbon dioxide levels and have minimal effect on oxygenation. References: Nichols DG, McCloskey JJ, Mayor A. Adult respiratory distress syndrome. In: Rogers MC, Helfaer MA, eds. Handbook of Pediatric Intensive Care. 2nd ed. Baltimore, Md: Williams & Wilkins; 1995:115-132 Toro-Figueroa LO, Barton RP, Luckett PM, Perkin RM. Mechanical ventilation and oxygen support systems. In: Levin DL, Morriss FC, eds. Essentials of Pediatric Intensive Care. 2nd ed. New York, NY: Churchill Livingstone, Inc; 1997:1416-1452 1999 Self-Assessment Exercise XXIX. Critical care [Return to Category List] Questions [Print Directions] Question 103. Answer.
You are treating a 12-year-old boy who has purpura. His blood pressure is 68/43 mm Hg. Arterial blood gas analysis on 100% FIO2 reveals: pH, 7.20; PO2, 160 torr; PCO2, 21 torr. Following intubation and the administration of intravenous antibiotics, saline (20 mL/kg), and dopamine (10.0 mcg/kg per minute), the blood pressure is 72/56 mm Hg and pulses are easily felt, but acidosis persists. The most appropriate NEXT step is to A. B. C. D. E. administer a bolus of 5% albumin (20 mL/kg) administer another bolus of saline (30 mL/kg) begin dobutamine infusion at 5.0 mcg/kg per minute begin norepinephrine infusion at 0.5 mcg/kg per minute increase dopamine infusion to 15.0 mcg/kg per minute
Answers Critique 103 Preferred Response: D
[View Question] The boy described in the vignette has evidence of septic shock due to meningococcemia and its characteristic nonthrombocytopenic petechiae and purpura. Following treatment with fluid resuscitation and inotropic drug support, it may be necessary to add vasopressor therapy in the form of a norepinephrine infusion. Sepsis may be accompanied by the release of vasoactive cytokines that reduce the vascular response to vasoconstrictors. The term "warm shock" may be used for patients who have inadequate tissue perfusion (as evidenced by persistent metabolic acidosis and persistent hypotension), but good peripheral pulses. Despite physiologic concerns that vasopressor drugs may increase the afterload and, therefore, increase the work of the heart during shock, administration of vasopressors, especially norepinephrine, has become more accepted in treating patients who are in septic shock. In pure cardiogenic shock, such as following pediatric cardiac surgery, inotropic drugs (eg, dobutamine) are the mainstay of treatment. Lower blood pressure levels may be acceptable and even desirable when the problem is primary cardiac pump dysfunction rather than sepsis. In patients who have hypotensive septic shock, administration of repeated fluid boluses or the addition of a second inotropic drug (eg, dobutamine) to a regimen of dopamine is unlikely to restore effective blood pressure. Administration of higher doses of dopamine may have a greater vasopressor effect than low-dose infusions, but they can be associated with undesirable tachycardia. Maintaining a low dose of dopamine (2 to 5 mcg/kg per minute) as well as norepinephrine infusion has been reported to promote renal blood flow in some studies; in other reports it has not appeared to augment the hemodynamic
state or renal function. Once blood pressure is increased to an acceptable level, a vasodilating agent (eg, nitroprusside) may be added to the regimen or the vasopressor dose may be weaned with the goal of returning to low-to-moderate dose inotropic drugs (eg, dobutamine or dopamine). References: Lucas CE. A new look at dopamine and norepinephrine for hyperdynamic septic shock. Chest. 1994;105:7-8 Martin C, Papazian L, Perrin G, Saux P, Gouin F. Norepinephrine or dopamine for the treatment of hyperdynamic septic shock? Chest. 1993;103:1826-1831 1998 Self-Assessment Exercise XXIX. Critical care [Return to Category List] Questions [Print Directions] Question 28. Answer.
A 2-week-old infant has tachycardia, tachypnea, and poor weight gain. Findings include: chest radiography, cardiomegaly; echocardiography, a structurally normal heart, left ventricular dilatation, ejection fraction of 20% (normal, >55%), a small pericardial effusion, and mild mitral and tricuspid regurgitation. Arterial blood gases: pH, 7.30; PO2, 72 torr; PCO2, 41 torr. The most appropriate INITIAL step in management is intravenous administration of A. B. C. D. E. angiotensin-converting enzyme inhibitor corticosteroid digoxin epinephrine furosemide
Question 131. Answer. Of the following, the MOST likely finding in a child who has impending liver failure is A. B. C. D. acute onset of ascites hyperammonemia and mental status changes polyuria severe epistaxis
E.
significant hepatomegaly
Answers Critique 28 Preferred Response: E
[View Question] The infant in the vignette has severe myocardial dysfunction with an ejection fraction less than one third of normal. The mitral and tricuspid valve regurgitations are due to the myocardial dysfunction. In view of the normal intracardiac anatomy in this infant, differential diagnosis includes coarctation, myocarditis, anomalous origin of the left coronary artery from the pulmonary artery, coronary calcinosis, and idiopathic cardiomyopathy. Treatment should begin immediately; digoxin, an angiotensin-converting enzyme (ACE) inhibitor, and furosemide all are potential choices. However, furosemide is the drug of immediate choice because its onset of action is within minutes, it usually affords rapid symptomatic improvement, and it can prevent the progression of respiratory distress and obviates the need for endotracheal intubation. Digoxin requires a longer time to take effect than furosemide and will have only a modest influence on ventricular function in this patient. In a patient who may have myocarditis, the dose of digoxin must be reduced because of possible arrhythmogenic effects. ACE inhibitors are drugs of choice for long-term treatment of congestive heart failure. In adults who have ventricular dysfunction, these drugs have offered symptomatic relief, decreased hospitalization time, and reduced mortality. Results of similar controlled studies are not available in children, but improved hemodynamic function has been reported after use of these agents. There is only one intravenous ACE inhibitor available, and no studies of its effectiveness in pediatric patients have been published. Corticosteroids have been used in patients who have myocarditis, and there are reports suggesting they may be effective, but there are no controlled studies proving efficacy, and these agents might be harmful in the early infectious stage of myocarditis.
Epinephrine is not used as a first-line drug in the emergency setting because of its alpha-adrenergic effects, which can increase systemic peripheral resistance and decrease cardiac output. However, intravenous dobutamine would be a reasonable first-line inotropic agent. References: Bernstein D. Congestive heart failure. In: Nelson WE, Behrman RE, Kliegman RM, Arvin AM, eds. Nelson Textbook of Pediatrics. 15th ed. Philadelphia, Pa: WB Saunders Co; 1996:13591363
Park MK. Congestive heart failure. In: Pediatric Cardiology for Practitioners. 3rd ed. St Louis, Mo: Mosby-Year Book, Inc; 1996:401-411 Steeg CN. Congestive heart failure.01220 Pediatrics in Review. 1992;13:118 Critique 131 Preferred Response: B
[View Question] Fulminant hepatic failure (FHF) is characterized by the development of encephalopathy within several weeks of the onset of illness. FHF results from deterioration of liver function in a patient who has known liver disease or may be the presenting feature of acute liver disease. The differential diagnosis of hepatitis includes: infection (eg, hepatitis A, hepatitis B, hepatitis D, herpesvirus, echovirus), exposure to toxins (eg, carbon tetrachloride, acetaminophin, valproic acid), metabolic disorders (eg, urea cycle disorders, Wilson disease, fatty liver of pregnancy, heredity fructose intolerance, galactosemia, tyrosinemia), sepsis and shock, autoimmune hepatitis, and malignancy (eg, leukemic infiltrates of the liver). Progressive hyperbilirubinemia, anorexia, vomiting, and abdominal pain often are present in patients who have FHF. An atypical course of acute viral hepatitis should suggest progression to hepatic failure. Epistaxis, bruising, and gastrointestinal hemorrhage are common, and ascites may develop. However, the most likely findings in a child who has impending liver failure are hyperammonemia and altered sensorium (encephalopathy) characterized by confusion, somnolence, and combativeness that may progress to unresponsiveness and coma. A rapid decrease in liver size, rather than hepatomegaly, is an ominous sign that is associated with liver failure. The prognosis in children who have hepatic failure varies, depending upon the etiology of the liver disease and the stage of encephalopathy. Encephalopathy is the hallmark of hepatic failure and, in a patient who has hepatitis, is one of the earliest indicators of the potential for hepatic failure. Encephalopathy progresses from stage I (periods of lethargy and euphoria, difficulty in performing mental tasks, sleep disorders, slurred speech, and a normal electroencephalogram [EEG]), to Stage II (drowsiness, agitation and disorientation, asterixis, and generalized slowing on EEG), to Stage III (stuporous but arousable, confusion, hyperreflexia and rigidity, markedly abnormal EEG), to Stage IV (coma, areflexia, flaccidity, varied response to pain with electrocortical silence upon EEG). The stage of encephalopathy is of prognostic significance; the survival rate in stage I to II encephalopathy is approximately 66% compared with only 15% in stage IV. Of note, the results of biochemical tests do not parallel the clinical course of hepatic encephalopathy. The pathophysiology of hepatic encephalopathy is unclear. Common theories used to explain this phenomenon include: 1) ammonia accumulation in the central nervous system (CNS), 2) accumulation of neurotoxins in the CNS, 3) production of inhibitory neutotransmitters (eg, serotonin, gamma-aminobutyric acid [GABA], and 4) production of false neurotransmitters (ie, octopamine). Hepatic encephalopathy is treated with nutritional support that includes carbohydrate (to prevent hypoglycemia and reverse catabolism), protein (to permit hepatic
regeneration), and lactulose (to reduce gastrointestinal absorption of ammonia). Oral antibiotics are used to sterilize the gastrointestinal tract, thereby reducing ammonia production by gut bacteria. Endotracheal intubation and hyperventilation can prevent aspiration and control increased intracranial pressure. Coagulopathy is treated with the administration of vitamin K and fresh frozen plasma. Corticosteroids should be avoided. Coagulopathy associated with hepatic failure is the result of decreased vitamin Kdependent factors (factors II, V, VII, IX, and X), which are reduced as the liver's synthesizing capability is compromised. Increased prothrombin time that does not improve after the administration of vitamin K indicates severe hepatocellular disease and a poor prognosis. Factor VIII, produced in the liver and nonhepatic endothelial tissue, often is increased in patients who have hepatic failure but is depressed in those who have diffuse intravascular coagulopathy. Platelet dysfunction may contribute to the bleeding diathesis and may be associated with disseminated intravascular coagulopathy. Significant abnormalities in coagulation can occur without clinical hemorrhage, and hemorrhage can occur in patients who have mild coagulopathy. Gastrointestinal hemorrhage occurs in 70% of children who have FHF and accounts for one fifth of all deaths. The hemorrhage typically results from gastric or esophageal erosions. Thus, severe epistaxis is not predictive of impending liver failure. Hepatorenal syndrome is the most common cause of renal impairment in patients who have hepatic failure. It is characterized by oliguria (rather than polyuria) that is unresponsive to volume expansion, sodium retention, and a benign urinary sediment. The current theory regarding the pathogenesis of hepatorenal syndrome is an imbalance between the vasoconstrictive effects of thromboxine A2 and the vasodilating effects of prostaglandins I2 and E2. Renal vasoconstriction in patients who have hepatic failure results in sodium and water retention. When increased portal pressure is associated with hypoalbuminemia (decreased colloid oncotic pressure), intravascular volume expansion leads to ascites. Although ascites and coagulopathy are ominous signs in children who have FHF, they are nonspecific and can be seen in other forms of liver disease. Despite advances in intensive care, the mortality of FHF remains very high. Conservative management focuses on careful monitoring and the prevention and treatment of complications. Orthotopic liver transplantation has reduced the mortality in patients who have FHF from 80% to between 30% and 50%. References: Kirsh BM, Lam N, Layden TJ, Wiley TE. Diagnosis and management of fulminant hepatic failure. Compr Ther. 1995;21:166-171 Lee WM. Acute liver failure. N Engl J Med. 1993;329:1862-1872 Mammen EF. Coagulation defects in liver disease. Med Clin North Am. 1994;78:545-554
Macdougall BR, Bailey RJ, Williams R. H2-receptor antagonists and antacids in the prevention of acute gastrointestinal haemorrhage in fulminant hepatic failure. Two controlled trials. Lancet. 1977;1:617-619 Plum F, Hindfelt B. The neurological complications of liver disease. In: Vinken PJ, Bruyn GW, eds. Handbook of Clinical Neurology: Metabolic and Deficiency Diseases of the Nervous System. New York, NY: American Elsevier Publishing Company, Inc; 1976:349-377 Saunders SJ, Hickman R, Macdonald R, Terblanche J. The treatment of acute liver failure. Prog Liver Dis. 1972;4:333-344 Trey C, Lipworth L, Davidson CS. Parameters influencing survival in the first 318 patients reported to the fulminant hepatic failure surveillence study. Gastroenterology. 1970;58:306
Das könnte Ihnen auch gefallen
- PANCE Prep Pearls Cardio Questions PDFDokument9 SeitenPANCE Prep Pearls Cardio Questions PDFkat100% (3)
- ISO 9001:2015 Explained, Fourth Edition GuideDokument3 SeitenISO 9001:2015 Explained, Fourth Edition GuideiresendizNoch keine Bewertungen
- FRACP Written Exam Otago MCQ Book 2016Dokument470 SeitenFRACP Written Exam Otago MCQ Book 2016Qiliang Liu100% (2)
- Final Questions 2021Dokument8 SeitenFinal Questions 2021PatrycjaSkierkaNoch keine Bewertungen
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtVon EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtBewertung: 5 von 5 Sternen5/5 (1)
- Basic Course of Radionics and RadiesthesiaDokument33 SeitenBasic Course of Radionics and RadiesthesiaSolomanTrismosinNoch keine Bewertungen
- CVS MCQsDokument14 SeitenCVS MCQsThana AlAnsari100% (2)
- Shocks MCQDokument6 SeitenShocks MCQJaya Krishna Naidu100% (1)
- Aortic dissection CT findings pathophysiologyDokument44 SeitenAortic dissection CT findings pathophysiologyRoni ArmandaNoch keine Bewertungen
- PracticeExam 3 AnsDokument52 SeitenPracticeExam 3 AnsBehrouz YariNoch keine Bewertungen
- Advanced Knowledge Assessment in Adult Critical CareDokument570 SeitenAdvanced Knowledge Assessment in Adult Critical CareMajor EmadNoch keine Bewertungen
- Critical CareDokument9 SeitenCritical CareGalaleldin AliNoch keine Bewertungen
- Jolo PartDokument3 SeitenJolo PartsatruetalagaNoch keine Bewertungen
- RENALDokument10 SeitenRENALbhagavan prasadNoch keine Bewertungen
- 12 Week Old With A Uti: Radiological Investigation 1Dokument8 Seiten12 Week Old With A Uti: Radiological Investigation 1yeezeeNoch keine Bewertungen
- MCQ Cardio 3Dokument50 SeitenMCQ Cardio 3Dian ParamitaNoch keine Bewertungen
- Try Out NewDokument19 SeitenTry Out NewIke AdrianaNoch keine Bewertungen
- Abb IonsDokument26 SeitenAbb Ionssaxebe7427Noch keine Bewertungen
- Materi To Kardio 03 JanuariDokument50 SeitenMateri To Kardio 03 JanuariMamanNoch keine Bewertungen
- Sudden Worsening Shortness of BreathDokument6 SeitenSudden Worsening Shortness of BreathAndi HidayatNoch keine Bewertungen
- Masterclass Book Part 2Dokument367 SeitenMasterclass Book Part 2Eng Kian Ng100% (5)
- MCQs and Cases in MedicineDokument14 SeitenMCQs and Cases in Medicineyoune6Noch keine Bewertungen
- Right Side Pleuritic Chest Pain For A Few Hours. On Examination Tachycardia, Respiratory Distress, O Breath Sounds On The Right SideDokument9 SeitenRight Side Pleuritic Chest Pain For A Few Hours. On Examination Tachycardia, Respiratory Distress, O Breath Sounds On The Right SideRabia RabiaNoch keine Bewertungen
- ER Pediatric EmergenciesDokument7 SeitenER Pediatric EmergenciesSylphana Astharica LawalataNoch keine Bewertungen
- 2021 Oct Dwe Adult Medicine Practice Exam Questions and AnswersDokument18 Seiten2021 Oct Dwe Adult Medicine Practice Exam Questions and AnswersMohammed HamedNoch keine Bewertungen
- 19-Year-Old Female With Hypokalemia EvaluatedDokument5 Seiten19-Year-Old Female With Hypokalemia EvaluatedMohammed AhmedNoch keine Bewertungen
- Cyanosis in A Newborn Immediately After BirthDokument8 SeitenCyanosis in A Newborn Immediately After BirthLộc Nguyễn ĐìnhNoch keine Bewertungen
- Paper C KMU 2019 cardiac mcqsDokument28 SeitenPaper C KMU 2019 cardiac mcqsaizaz100% (1)
- Neuropathology Case Studies GuideDokument10 SeitenNeuropathology Case Studies GuideMicole NatividadNoch keine Bewertungen
- Soal Kardio 08Dokument22 SeitenSoal Kardio 08Defina BudiNoch keine Bewertungen
- Echocardiogram findings in restrictive cardiomyopathyDokument93 SeitenEchocardiogram findings in restrictive cardiomyopathyArash SamieiNoch keine Bewertungen
- 001 ICU Case CoyocaDokument9 Seiten001 ICU Case CoyocaMiguel Kelly CataneNoch keine Bewertungen
- CPC PowerpointDokument36 SeitenCPC Powerpointapi-277377339Noch keine Bewertungen
- Formative Assessment FinalDokument5 SeitenFormative Assessment FinalJonathan YeohNoch keine Bewertungen
- 3-Case Study_ 60-Year-Old Female Presenting With Shortness of Breath - StatPearls - NCBI BookshelfDokument9 Seiten3-Case Study_ 60-Year-Old Female Presenting With Shortness of Breath - StatPearls - NCBI Bookshelfabdeali hazariNoch keine Bewertungen
- IMCQ 10 - Pulmonary - KEYDokument13 SeitenIMCQ 10 - Pulmonary - KEYReggieNoch keine Bewertungen
- General Pathology Q2 Heart ConditionsDokument9 SeitenGeneral Pathology Q2 Heart ConditionsAdrian CaballesNoch keine Bewertungen
- Anaesthesia for Ventriculoperitoneal ShuntsDokument3 SeitenAnaesthesia for Ventriculoperitoneal Shuntsnaren_winv1350Noch keine Bewertungen
- Gerry B. Acosta, MD, FPPS, FPCC: Pediatric CardiologistDokument51 SeitenGerry B. Acosta, MD, FPPS, FPCC: Pediatric CardiologistChristian Clyde N. ApigoNoch keine Bewertungen
- HY Mixed USMLE Review Part IVDokument22 SeitenHY Mixed USMLE Review Part IVDr.Mohammed N. AbedNoch keine Bewertungen
- Soal Board IcuDokument402 SeitenSoal Board IcudoktersaktiNoch keine Bewertungen
- ALO Case Report PDFDokument5 SeitenALO Case Report PDFemma mojokertoNoch keine Bewertungen
- USMLE CompilationDokument101 SeitenUSMLE CompilationRendi RafsanjaniNoch keine Bewertungen
- Cardiology ExamDokument9 SeitenCardiology ExamKhadar mohamedNoch keine Bewertungen
- RLEFandECS Garlitos RoanneDokument4 SeitenRLEFandECS Garlitos RoannePaul JacksonNoch keine Bewertungen
- Cardiovascular Medicine Questions: Risk Assessment, Heart Failure, Chest Pain, PalpitationsDokument102 SeitenCardiovascular Medicine Questions: Risk Assessment, Heart Failure, Chest Pain, PalpitationsManisha DesaiNoch keine Bewertungen
- Waveform Questions /critical Care Board ReviewDokument14 SeitenWaveform Questions /critical Care Board ReviewAzmachamberAzmacareNoch keine Bewertungen
- 3 Chapter 29 Practice Questions CardioDokument17 Seiten3 Chapter 29 Practice Questions CardioNursyNurseNoch keine Bewertungen
- Test - Surgery Book MCQs - Final Exam - QuizletDokument158 SeitenTest - Surgery Book MCQs - Final Exam - Quizlety SNoch keine Bewertungen
- Cardiovascular Medicine:Question 1Dokument101 SeitenCardiovascular Medicine:Question 1abdullahmushlihNoch keine Bewertungen
- ABG Cases Rev 2.0Dokument10 SeitenABG Cases Rev 2.0Maram AbdullahNoch keine Bewertungen
- First Part Exam - October 2020Dokument16 SeitenFirst Part Exam - October 2020hassan mohamedNoch keine Bewertungen
- RevisionDokument9 SeitenRevisionF6imNoch keine Bewertungen
- Casi Clinici Medicine and Critical CareDokument85 SeitenCasi Clinici Medicine and Critical CarePaolo OnidaNoch keine Bewertungen
- Primary SurveyDokument13 SeitenPrimary SurveyNurul FadliNoch keine Bewertungen
- P Wave T Waves QRS ComplexDokument16 SeitenP Wave T Waves QRS ComplexYousef Al-AmeenNoch keine Bewertungen
- Case Report (Septaecemia) : SummaryDokument3 SeitenCase Report (Septaecemia) : Summaryikbal al-lamiNoch keine Bewertungen
- MCQ Exam 2018 - 2Dokument42 SeitenMCQ Exam 2018 - 2aditya rajputNoch keine Bewertungen
- Structure WaterDokument32 SeitenStructure WateravisenicNoch keine Bewertungen
- Adolescent Medicine and GynecologyDokument69 SeitenAdolescent Medicine and GynecologyavisenicNoch keine Bewertungen
- Korean FoodDokument11 SeitenKorean FoodavisenicNoch keine Bewertungen
- Water PapaerDokument15 SeitenWater PapaeravisenicNoch keine Bewertungen
- Paediatric and Child Health - Self Assessment - All - 2009Dokument32 SeitenPaediatric and Child Health - Self Assessment - All - 2009avisenicNoch keine Bewertungen
- XXVI. Substance AbuseDokument26 SeitenXXVI. Substance AbuseavisenicNoch keine Bewertungen
- Disorders of The EyeDokument25 SeitenDisorders of The EyeavisenicNoch keine Bewertungen
- Pulsator AirDokument6 SeitenPulsator AiravisenicNoch keine Bewertungen
- Pengaruh Medan Magnet THD AirDokument8 SeitenPengaruh Medan Magnet THD AiravisenicNoch keine Bewertungen
- Endocrine DisordersDokument51 SeitenEndocrine DisordersavisenicNoch keine Bewertungen
- Collagen Vascular and Other Multisystem DisordersDokument32 SeitenCollagen Vascular and Other Multisystem DisordersavisenicNoch keine Bewertungen
- Self AssessmentDokument3 SeitenSelf AssessmentavisenicNoch keine Bewertungen
- Tendon Shortening Risk in Hemophilia BoyDokument72 SeitenTendon Shortening Risk in Hemophilia BoyavisenicNoch keine Bewertungen
- Allergy Self-Assessment QuestionsDokument63 SeitenAllergy Self-Assessment QuestionsavisenicNoch keine Bewertungen
- Fluid and electrolyte metabolism questionsDokument41 SeitenFluid and electrolyte metabolism questionsavisenicNoch keine Bewertungen
- Fluid and electrolyte metabolism questionsDokument41 SeitenFluid and electrolyte metabolism questionsavisenicNoch keine Bewertungen
- Jurnal NeuroDokument7 SeitenJurnal NeuroavisenicNoch keine Bewertungen
- PediaClub CasesDokument80 SeitenPediaClub CasesavisenicNoch keine Bewertungen
- INDEX of SuspecionDokument6 SeitenINDEX of SuspecionavisenicNoch keine Bewertungen
- Motor DelayDokument14 SeitenMotor DelayavisenicNoch keine Bewertungen
- Paediatric and Child Health - Self Assessment - All - 2007Dokument53 SeitenPaediatric and Child Health - Self Assessment - All - 2007avisenicNoch keine Bewertungen
- Self-Assessment Questions, Group 6Dokument20 SeitenSelf-Assessment Questions, Group 6naveenkovalNoch keine Bewertungen
- Jurnal KardioDokument9 SeitenJurnal KardioavisenicNoch keine Bewertungen
- The Sag Nac EffectDokument19 SeitenThe Sag Nac EffectavisenicNoch keine Bewertungen
- Lintasan CurvaDokument25 SeitenLintasan CurvaavisenicNoch keine Bewertungen
- Feb 2002 Supplemental NotesDokument8 SeitenFeb 2002 Supplemental NotesavisenicNoch keine Bewertungen
- Phys Propt of Struct WaterDokument7 SeitenPhys Propt of Struct WateravisenicNoch keine Bewertungen
- Nature'S Geometry: Soumitro BanerjeeDokument9 SeitenNature'S Geometry: Soumitro BanerjeeavisenicNoch keine Bewertungen
- Propiedades Grado 50 A572Dokument2 SeitenPropiedades Grado 50 A572daniel moreno jassoNoch keine Bewertungen
- QuickTransit SSLI Release Notes 1.1Dokument12 SeitenQuickTransit SSLI Release Notes 1.1subhrajitm47Noch keine Bewertungen
- Oxford Digital Marketing Programme ProspectusDokument12 SeitenOxford Digital Marketing Programme ProspectusLeonard AbellaNoch keine Bewertungen
- ServiceDokument47 SeitenServiceMarko KoširNoch keine Bewertungen
- Estimation of Working CapitalDokument12 SeitenEstimation of Working CapitalsnehalgaikwadNoch keine Bewertungen
- Polytechnic University Management Services ExamDokument16 SeitenPolytechnic University Management Services ExamBeverlene BatiNoch keine Bewertungen
- 2023 Test Series-1Dokument2 Seiten2023 Test Series-1Touheed AhmadNoch keine Bewertungen
- Site Visit Risk Assessment FormDokument3 SeitenSite Visit Risk Assessment FormAmanuelGirmaNoch keine Bewertungen
- KPMG Inpection ReportDokument11 SeitenKPMG Inpection ReportMacharia NgunjiriNoch keine Bewertungen
- 621F Ap4405ccgbDokument8 Seiten621F Ap4405ccgbAlwinNoch keine Bewertungen
- 17BCE0552 Java DA1 PDFDokument10 Seiten17BCE0552 Java DA1 PDFABHIMAYU JENANoch keine Bewertungen
- Data Sheet: Experiment 5: Factors Affecting Reaction RateDokument4 SeitenData Sheet: Experiment 5: Factors Affecting Reaction Ratesmuyet lêNoch keine Bewertungen
- Android software download guideDokument60 SeitenAndroid software download guideRizky PradaniNoch keine Bewertungen
- Report Emerging TechnologiesDokument97 SeitenReport Emerging Technologiesa10b11Noch keine Bewertungen
- BPL Millipacs 2mm Hardmetrics RarDokument3 SeitenBPL Millipacs 2mm Hardmetrics RarGunter BragaNoch keine Bewertungen
- Service and Maintenance Manual: Models 600A 600AJDokument342 SeitenService and Maintenance Manual: Models 600A 600AJHari Hara SuthanNoch keine Bewertungen
- Nursing Care Management of a Client with Multiple Medical ConditionsDokument25 SeitenNursing Care Management of a Client with Multiple Medical ConditionsDeannNoch keine Bewertungen
- Zelev 1Dokument2 SeitenZelev 1evansparrowNoch keine Bewertungen
- CMC Ready ReckonerxlsxDokument3 SeitenCMC Ready ReckonerxlsxShalaniNoch keine Bewertungen
- Panel Data Econometrics: Manuel ArellanoDokument5 SeitenPanel Data Econometrics: Manuel Arellanoeliasem2014Noch keine Bewertungen
- KSEB Liable to Pay Compensation for Son's Electrocution: Kerala HC CaseDokument18 SeitenKSEB Liable to Pay Compensation for Son's Electrocution: Kerala HC CaseAkhila.ENoch keine Bewertungen
- 2nd Pornhub Awards - WikipediaaDokument13 Seiten2nd Pornhub Awards - WikipediaaParam SinghNoch keine Bewertungen
- Fernandez ArmestoDokument10 SeitenFernandez Armestosrodriguezlorenzo3288Noch keine Bewertungen
- AsiaSat 7 at 105Dokument14 SeitenAsiaSat 7 at 105rahman200387Noch keine Bewertungen
- Evaluating MYP Rubrics in WORDDokument11 SeitenEvaluating MYP Rubrics in WORDJoseph VEGANoch keine Bewertungen
- MODULE+4+ +Continuous+Probability+Distributions+2022+Dokument41 SeitenMODULE+4+ +Continuous+Probability+Distributions+2022+Hemis ResdNoch keine Bewertungen
- Reflection Homophone 2Dokument3 SeitenReflection Homophone 2api-356065858Noch keine Bewertungen
- Biagioli Did Galileo Copy The TelescopeDokument28 SeitenBiagioli Did Galileo Copy The TelescopeGregory HooNoch keine Bewertungen
- Algorithms For Image Processing and Computer Vision: J.R. ParkerDokument8 SeitenAlgorithms For Image Processing and Computer Vision: J.R. ParkerJiaqian NingNoch keine Bewertungen