Beruflich Dokumente
Kultur Dokumente
Nursing Care Plan HOPE THIS HELPS ALONG THE WAY
Hochgeladen von
Rye AnchCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nursing Care Plan HOPE THIS HELPS ALONG THE WAY
Hochgeladen von
Rye AnchCopyright:
Verfügbare Formate
NURSING CARE PLAN
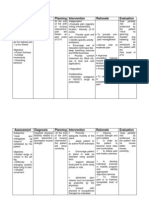
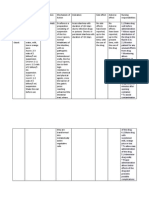
Assessment Subjective: Masakit ang banding gitna ng likod ko as verbalized by the patient. -Aching -Onset is indefinite -Localized in the middle area of the back -Pain goes away for up to 30 minutes at times but recurs again -Pain scale of 6/10, when not moved -With pulsation
Diagnosis Chronic pain related to thoracic compression as manifested by facial grimace and guarding behavior
Inference Precipitating factors: -Obesity -Work: (junkerheavy lifter) and Predisposing factors: -T8 spinal abscess -Kyphosis T9 spinal compression Alteration of peripheral nervous system impulses (T8T9) Nociception Transmission
Planning Short term:
Intervention Independent:
Rationale
Evaluation Short term: After an hour of nursing interventions, the patient was able to verbalize that pain is relieved/ controlled as evidenced by pain scale of 3/10 or lower Long term: After 3days of nursing interventions, the patient was able to verbalize nonpharmacologic methods that provide relief and follow prescribed pharmacological regimen
After an hour of nursing -Assess for pain interventions, the tolerance patient will be able to verbalize that pain is relieved/ controlled as evidenced by pain scale of 3/10 or lower -Note cultural Long term: and developmental After 3days of influences nursing affecting pain interventions, the patient will be able to verbalize non-Provide comfort pharmacologic measures, quiet methods that environment, provide relief and calm and follow activities prescribed
-To help determine possibility of underlying condition or organ dysfunction requiring treatment -Verbal or behavioral cues may have no direct relationship to the degree of pain perceived -To promote nonpharmacological pain management
-Pain worsens when repositioning (9/10) Objectives: -Body temperature of 36.8C rose to 37.3C in 4 hours -Facial grimace noted -Observed evidence of pain during repositioning -restlessness -sleep disturbance -Spinal cord (T8) abscess -T9 compression
and pharmacological interpretation of regimen pain signal to the brain Localized midposterior pain Guarding behavior; restlessness; irritability The gate control theory of pain is the idea that physical pain is not a direct result of activation of pain receptor neurons, but rather its perception is modulated by interaction between different neurons.
-Note when pain occurs -Investigate report of pain, noting characteristics, location, intensity (0-10 scale) -Provide firm mattress and small pillows
-To medicate prophylactically, as appropriate -Helpful in determining pain management needs and effectiveness of the program -Soft or sagging mattresses and large pillows inhibit the proper body alignment -In acute phase, total bed rest maybe necessary to limit pain
-Suggest patient to assume position of proper comfort while in bed. Promote bed rest as indicated -Encourage frequent changes of position -Encourage use of stress
-Prevent general fatigue and joint stiffness -Promotes relaxation,
via CT Scan -Guarding behavior
management techniques
provides sense of control and may enhance coping activities -Increasing/ decreasing dosage, stepped program helps in self-management of pain
-Evaluate/ document patients response to analgesia, and assist in transitioning/ altering drug regimen, based on individual needs Dependent: -Administer/ monitor medication such as analgesics/, as indicated, to maximum dosage, as needed -Administer antibiotic as prescribed
-To maintain acceptable level of pain. Notify the physician if regimen is inadequate to meet pain control goal -To prevent further infection
Collaborative: -Coordinate with medical technologists, radiation technologists, nuclear medicine department -Coordinate with dietician, nutritionist -Coordinate with charitable institution and HMO -Coordinate with spiritual counselor Source: Gate Control Theory of Pain. (n.d.). Science Daily. Retrieved September 30, 2011, from www.sciencedaily.com/articles/g/gate_control_theory_of_pain.htm Doenges, M.E. et.al (2006). Nurses Pocket Guide: Diagnoses, Prioritized Interventions, and Rationale. ed. 10. 392-396 -For further diagnostic or laboratory evaluation
-To promote wellness -To provide financial support
-To support patient and family spiritually
Das könnte Ihnen auch gefallen
- Renr Study GuideDokument57 SeitenRenr Study GuideJerilee SoCute Watts92% (12)
- COE WorksheetDokument16 SeitenCOE WorksheetiloveraynaNoch keine Bewertungen
- NCP - Acute PainDokument3 SeitenNCP - Acute PainRene John Francisco0% (1)
- Acute Pain - Nursing Intervention - RationaleDokument2 SeitenAcute Pain - Nursing Intervention - Rationaledonnaluna203315100% (4)
- AssessmentDokument2 SeitenAssessmentKevin KroytNoch keine Bewertungen
- NCP - PainDokument3 SeitenNCP - PainAdrian Mallar100% (2)
- Reflexology: The Definitive Practitioner's Manual: Recommended by the International Therapy Examination Council for Students and PractitonersVon EverandReflexology: The Definitive Practitioner's Manual: Recommended by the International Therapy Examination Council for Students and PractitonersBewertung: 5 von 5 Sternen5/5 (5)
- Calcium Carbonate (Caltrate Plus 600 mg) Uses, Side Effects & Nursing CareDokument1 SeiteCalcium Carbonate (Caltrate Plus 600 mg) Uses, Side Effects & Nursing CareRye AnchNoch keine Bewertungen
- VancomycinDokument2 SeitenVancomycinRye AnchNoch keine Bewertungen
- JulieKJohnsonHe 2016 9ACascadeOfSmallEvent CaseStudiesInPatientSDokument5 SeitenJulieKJohnsonHe 2016 9ACascadeOfSmallEvent CaseStudiesInPatientSMarylanNoch keine Bewertungen
- 13 Implant Supported Fixed ProsthesesDokument52 Seiten13 Implant Supported Fixed ProsthesesJúliaJulieNoch keine Bewertungen
- Acute Pain Due To Gastritis Care Plan-G.a.Dokument1 SeiteAcute Pain Due To Gastritis Care Plan-G.a.Kristin Bienvenu85% (13)
- Acute Pain NCPDokument6 SeitenAcute Pain NCPPesky Pescante-MonterolaNoch keine Bewertungen
- PainDokument90 SeitenPainmikErlh100% (4)
- NCPDokument14 SeitenNCPRaidis Pangilinan0% (1)
- Acute Chest Pain ManagementDokument2 SeitenAcute Chest Pain ManagementErickson Caisido GarciaNoch keine Bewertungen
- Case NCPDokument2 SeitenCase NCPKyleDominicKohGoNoch keine Bewertungen
- Nursing Care Plan - Acute PainDokument6 SeitenNursing Care Plan - Acute PainAJ Tuban Compelio100% (1)
- PNS Pain Management Guideline For Nursing CompetencyDokument10 SeitenPNS Pain Management Guideline For Nursing Competencyvhon100% (1)
- NCP RheumatoidDokument5 SeitenNCP RheumatoidJane Elizabeth Gonzales MacahiaNoch keine Bewertungen
- Acute Pain Nursing DiagnosisDokument5 SeitenAcute Pain Nursing DiagnosisAngelo Cuaresma0% (1)
- Silvanus Chakra Puspita: Medical Staff of Mayapada Hospital Jakarta SelatanDokument44 SeitenSilvanus Chakra Puspita: Medical Staff of Mayapada Hospital Jakarta Selatanroby yuliandaNoch keine Bewertungen
- NCP Nursing Diagnosis: Acute PainDokument4 SeitenNCP Nursing Diagnosis: Acute Painphvega06Noch keine Bewertungen
- Control Post-Surgical Pain and Improve BreathingDokument12 SeitenControl Post-Surgical Pain and Improve BreathingMayraPagan-Carmenatty100% (1)
- Supplementary Material 7a Analgesia, Sedation and Neuromuscular BlockadeDokument10 SeitenSupplementary Material 7a Analgesia, Sedation and Neuromuscular BlockadeJeremiah Andre Poissonier AyupanNoch keine Bewertungen
- Nursing Care PlanDokument3 SeitenNursing Care PlanMae Therese AlabotNoch keine Bewertungen
- Assessment Diagnosis Planning Intervention Rationale EvaluationDokument2 SeitenAssessment Diagnosis Planning Intervention Rationale EvaluationPaulo de JesusNoch keine Bewertungen
- Treating Dysmenorrhea Through Education and Pain ManagementDokument3 SeitenTreating Dysmenorrhea Through Education and Pain ManagementNadilaNoch keine Bewertungen
- Acute Pain..Dokument2 SeitenAcute Pain..Melody Kaye MonsantoNoch keine Bewertungen
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDokument3 SeitenAssessment Nursing Diagnosis Planning Intervention Rationale Evaluationdee_day_8Noch keine Bewertungen
- Grieve and LossDokument6 SeitenGrieve and LossRuffy AbdulazisNoch keine Bewertungen
- NCP Nursing DiagnosisDokument24 SeitenNCP Nursing Diagnosisphvega06Noch keine Bewertungen
- PainDokument90 SeitenPainTobiDaNoch keine Bewertungen
- Pain Management For Medical StudentsDokument37 SeitenPain Management For Medical Studentsamq aloqiliNoch keine Bewertungen
- PainDokument116 SeitenPainJan SurigaNoch keine Bewertungen
- Management of PainDokument6 SeitenManagement of PainSinging MedicNoch keine Bewertungen
- Independent:: Surgical Nursing, 7 TH Ed. by Black, Joyce M.Andjane Hokan Son Hawkspg.443)Dokument4 SeitenIndependent:: Surgical Nursing, 7 TH Ed. by Black, Joyce M.Andjane Hokan Son Hawkspg.443)KenPedreso100% (1)
- NCPDokument1 SeiteNCPMa R DyNoch keine Bewertungen
- NCP Acute PainDokument2 SeitenNCP Acute PainLyka Mae DominguezNoch keine Bewertungen
- Nursing Care PlanDokument3 SeitenNursing Care Plansarah hanaNoch keine Bewertungen
- NCP Inc.Dokument2 SeitenNCP Inc.Franklin A. Salaum III100% (1)
- Nursing care plan for pain managementDokument4 SeitenNursing care plan for pain managementSugar Capule - ManuelNoch keine Bewertungen
- Pain Management - 03-07 VersionDokument51 SeitenPain Management - 03-07 VersionanreilegardeNoch keine Bewertungen
- 2 Acute Pain Chronic Renal Failure Nursing Care PlansDokument5 Seiten2 Acute Pain Chronic Renal Failure Nursing Care Plansjustin_saneNoch keine Bewertungen
- NCPDokument5 SeitenNCPchristineleesNoch keine Bewertungen
- Nursing Care Plan Assessment Diagnosis Planning Intervention Rationale EvaluationDokument2 SeitenNursing Care Plan Assessment Diagnosis Planning Intervention Rationale EvaluationFrances Anne Nollido SorianoNoch keine Bewertungen
- NCPDokument18 SeitenNCPChristian Karl B. LlanesNoch keine Bewertungen
- Nursing Care Plan for Pain ReliefDokument3 SeitenNursing Care Plan for Pain ReliefRezhaNoch keine Bewertungen
- NCP1Dokument2 SeitenNCP1Anonymous 75TDy2yNoch keine Bewertungen
- NCP AppendicitisDokument2 SeitenNCP AppendicitisSHAMUS DANINoch keine Bewertungen
- Nursing Care Plan Rheumatoid ArthritisDokument4 SeitenNursing Care Plan Rheumatoid ArthritisLighto RyusakiNoch keine Bewertungen
- Assessment Diagnosis Inference Planning Nursing Intervention Rationale Subjective: "Palaging Sumasakit Ang IndependentDokument2 SeitenAssessment Diagnosis Inference Planning Nursing Intervention Rationale Subjective: "Palaging Sumasakit Ang IndependentAnna CaronanNoch keine Bewertungen
- Pemantauan Dan Penanganan Nyeri Pasca BedahDokument42 SeitenPemantauan Dan Penanganan Nyeri Pasca BedahAkbar Muitan LantauNoch keine Bewertungen
- Pain Wida FridayDokument24 SeitenPain Wida FridayWahida ZulkifliNoch keine Bewertungen
- R.O. Appendicitis.: Nursing Care Plan (NCP)Dokument2 SeitenR.O. Appendicitis.: Nursing Care Plan (NCP)Karen Joy ItoNoch keine Bewertungen
- Chronic Pain Management: Non-Drug Methods for ReliefDokument23 SeitenChronic Pain Management: Non-Drug Methods for Reliefmohs2007Noch keine Bewertungen
- Assessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationDokument3 SeitenAssessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationCrissa AngelNoch keine Bewertungen
- The Art of Holistic Pain Management: A Practical HandbookVon EverandThe Art of Holistic Pain Management: A Practical HandbookNoch keine Bewertungen
- Holistic Pain Relief: How to ease muscles, joints and other painful conditionsVon EverandHolistic Pain Relief: How to ease muscles, joints and other painful conditionsNoch keine Bewertungen
- Assessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsVon EverandAssessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsNoch keine Bewertungen
- Holistic Home Remedies for Acute Low Back Pain: Incorporating Stretching and the McKenzie MethodVon EverandHolistic Home Remedies for Acute Low Back Pain: Incorporating Stretching and the McKenzie MethodNoch keine Bewertungen
- The Breakthrough Back Pain Healing and Relief Plan: The book that unlocked the secrets of back pain care, sciatica pain relief naturally via diet, exercises & understanding the mind-body connectionVon EverandThe Breakthrough Back Pain Healing and Relief Plan: The book that unlocked the secrets of back pain care, sciatica pain relief naturally via diet, exercises & understanding the mind-body connectionNoch keine Bewertungen
- Holistic Approach to Relieve Neck Pain, Back, and Shoulder Pain: An Effective Method for Pain ReductionVon EverandHolistic Approach to Relieve Neck Pain, Back, and Shoulder Pain: An Effective Method for Pain ReductionBewertung: 3 von 5 Sternen3/5 (1)
- ImproNES Dadfsdfsdfsdfsd DFSDFSD Fasdfa SDFDokument1 SeiteImproNES Dadfsdfsdfsdfsd DFSDFSD Fasdfa SDFRye AnchNoch keine Bewertungen
- Some Useful QuotesDokument1 SeiteSome Useful QuotesRye AnchNoch keine Bewertungen
- Aditional Client PresDokument2 SeitenAditional Client PresRye AnchNoch keine Bewertungen
- Drug StudyDokument8 SeitenDrug StudyRye AnchNoch keine Bewertungen
- Anatomy of The FaceDokument21 SeitenAnatomy of The FaceRye AnchNoch keine Bewertungen
- VS Easy VS PaperDokument1 SeiteVS Easy VS PaperRye AnchNoch keine Bewertungen
- Attention Deficit Hyperactivity DisorderDokument9 SeitenAttention Deficit Hyperactivity DisorderRye AnchNoch keine Bewertungen
- Alternative Treatment For Parkinson's DiseaseDokument3 SeitenAlternative Treatment For Parkinson's DiseaseRye AnchNoch keine Bewertungen
- Abstract Pathophysiology of Gun Shot Wound On The BrainDokument1 SeiteAbstract Pathophysiology of Gun Shot Wound On The BrainRye AnchNoch keine Bewertungen
- Alcohol Related DisordersDokument14 SeitenAlcohol Related DisordersRye AnchNoch keine Bewertungen
- Omeprazole Drug StudyDokument2 SeitenOmeprazole Drug StudyRye Anch75% (8)
- Drug ListDokument1 SeiteDrug ListRye AnchNoch keine Bewertungen
- Pathophysiology PTBDokument4 SeitenPathophysiology PTBRye AnchNoch keine Bewertungen
- Erce FloraDokument2 SeitenErce FloraRye Anch0% (1)
- Taking Action To Close The Nursing-Finance Gap: Learning From SuccessDokument3 SeitenTaking Action To Close The Nursing-Finance Gap: Learning From SuccessRye Anch100% (1)
- Ok Psychomotor SkillsDokument1 SeiteOk Psychomotor SkillsRye AnchNoch keine Bewertungen
- Client PressentationDokument2 SeitenClient PressentationRye AnchNoch keine Bewertungen
- DrugsDokument7 SeitenDrugsRye AnchNoch keine Bewertungen
- Atorvastatin Drug StudyDokument2 SeitenAtorvastatin Drug StudyRye Anch88% (17)
- Bailen - FNCPDokument2 SeitenBailen - FNCPRye AnchNoch keine Bewertungen
- VideoasdfasdfasdfasdfaDokument1 SeiteVideoasdfasdfasdfasdfaRye AnchNoch keine Bewertungen
- Omeprazole Drug StudyDokument2 SeitenOmeprazole Drug StudyRye Anch75% (8)
- Conditions That Can Beconsidered ABCDokument4 SeitenConditions That Can Beconsidered ABCRye AnchNoch keine Bewertungen
- HYDROXYZINE DIHCL (Iterax)Dokument1 SeiteHYDROXYZINE DIHCL (Iterax)Rye Anch100% (1)
- Tramadol Hydrochloride (Ultran, Ultracet)Dokument1 SeiteTramadol Hydrochloride (Ultran, Ultracet)Rye AnchNoch keine Bewertungen
- Physical Assessment Compilation FinalDokument13 SeitenPhysical Assessment Compilation FinalRye AnchNoch keine Bewertungen
- DfasdfasdfasdfasdfaDokument2 SeitenDfasdfasdfasdfasdfaRye AnchNoch keine Bewertungen
- Tramadol Hydrochloride (Ultran, Ultracet)Dokument1 SeiteTramadol Hydrochloride (Ultran, Ultracet)Rye AnchNoch keine Bewertungen
- NSTP ProjDokument11 SeitenNSTP ProjLeeroi Christian Q Rubio100% (2)
- Valium drug guide for nursesDokument2 SeitenValium drug guide for nursesRhea Liza Comendador-TjernmoenNoch keine Bewertungen
- Sepsis: Signs and SymptomsDokument5 SeitenSepsis: Signs and SymptomssujithasNoch keine Bewertungen
- Bmet 262 Outline 2022 2023Dokument12 SeitenBmet 262 Outline 2022 2023Emmanuel PrahNoch keine Bewertungen
- Quiz Process RecordingDokument7 SeitenQuiz Process RecordingDewley Guevarra MontenegroNoch keine Bewertungen
- High Yield Step 2ckDokument4 SeitenHigh Yield Step 2ckCesar_Palana_3832Noch keine Bewertungen
- Psychotherapy Assessment FormatDokument10 SeitenPsychotherapy Assessment Formatshivani singh100% (1)
- The Reliability and Validity of The Vancouver Classification of Femoral Fractures After Hip ReplacementDokument4 SeitenThe Reliability and Validity of The Vancouver Classification of Femoral Fractures After Hip ReplacementDavidBeatonComuladaNoch keine Bewertungen
- CBT For CandA With OCD PDFDokument16 SeitenCBT For CandA With OCD PDFRoxana AlexandruNoch keine Bewertungen
- LeprosyDokument7 SeitenLeprosytankmpNoch keine Bewertungen
- New Law Regarding Mental Health Part 2 1 UpDokument43 SeitenNew Law Regarding Mental Health Part 2 1 UpHollister TidwellNoch keine Bewertungen
- Protection of Human Rights of Women PrisonersDokument5 SeitenProtection of Human Rights of Women PrisonersBrajakanta NameirakpamNoch keine Bewertungen
- Euro J of Neurology - 2021 - Van Den Bergh - European Academy of Neurology Peripheral Nerve Society Guideline On DiagnosisDokument28 SeitenEuro J of Neurology - 2021 - Van Den Bergh - European Academy of Neurology Peripheral Nerve Society Guideline On DiagnosisSusana RocheNoch keine Bewertungen
- Speech & Language Therapy in Practice, Summer 2008Dokument32 SeitenSpeech & Language Therapy in Practice, Summer 2008Speech & Language Therapy in PracticeNoch keine Bewertungen
- Congenital Syphilis Causes and TreatmentDokument4 SeitenCongenital Syphilis Causes and TreatmentAlya Putri Khairani100% (1)
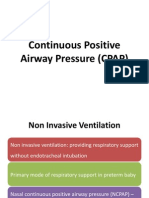
- Continuous Positive Airway Pressure (CPAP)Dokument53 SeitenContinuous Positive Airway Pressure (CPAP)indiamahesh100% (1)
- IssuancesDokument347 SeitenIssuancesReia RuecoNoch keine Bewertungen
- Congenital AnomaliesDokument94 SeitenCongenital AnomaliesDeepti Kukreti100% (1)
- Current Status of NTD PhilippinesDokument28 SeitenCurrent Status of NTD PhilippinesMelody PardilloNoch keine Bewertungen
- E Stim PDFDokument6 SeitenE Stim PDFAlvaro Toledo100% (1)
- What Are The Parameters of An Extended Aeration Activated Sludge System - Water Tech Online PDFDokument9 SeitenWhat Are The Parameters of An Extended Aeration Activated Sludge System - Water Tech Online PDFZoran KostićNoch keine Bewertungen
- Pharmaceutical ExipientDokument14 SeitenPharmaceutical ExipientShekhar SinghNoch keine Bewertungen
- Pil 2425Dokument6 SeitenPil 2425Gabriela ChiritoiuNoch keine Bewertungen
- Konversi Kode Prosedure INACBGs Ke Kode ICD 9-CMDokument349 SeitenKonversi Kode Prosedure INACBGs Ke Kode ICD 9-CMTri Muhammad HaniNoch keine Bewertungen
- ME Pharma Form July 2010Dokument3 SeitenME Pharma Form July 2010darningNoch keine Bewertungen
- Updated February 10, 2012: Preview of The Medifocus Guidebook On: Alzheimer's DiseaseDokument30 SeitenUpdated February 10, 2012: Preview of The Medifocus Guidebook On: Alzheimer's Diseaseexpedito andres prada suarezNoch keine Bewertungen