Beruflich Dokumente
Kultur Dokumente
Amputation: Impaired Physical Mobility
Hochgeladen von
Ahmad EfendiOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
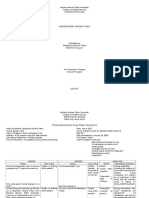
Amputation: Impaired Physical Mobility
Hochgeladen von
Ahmad EfendiCopyright:
Verfügbare Formate
Amputation
In general, amputation of limbs is the result of trauma, peripheral vascular disease, tumors, and congenital disorders. For the purpose of this plan of care, amputation refers to the surgical/traumatic removal of a limb. Upper-extremity amputations are generally due to trauma from industrial accidents. Reattachment surgery may be possible for fingers, hands, and arms. Lower-extremity amputations are performed much more frequently than upper-extremity amputations. Five levels are currently used in lowerextremity amputation: foot and ankle, below knee (BKA), knee disarticulation and above (thigh), knee-hip disarticulation; and hemipelvectomy and translumbar amputation. There are two types of amputations: (1) open (provisional), which requires strict aseptic techniques and later revisions, and (2) closed, or flap. Diagnostiq study assesment
X-rays: Identify skeletal abnormalities. CT scan: Identifies soft-tissue and bone destruction, neoplastic lesions, osteomyelitis, hematoma formation. Angiography and blood flow studies: Evaluate circulation/tissue perfusion problems and help predict potential for tissue healing after amputation. Doppler ultrasound, laser Doppler flowmetry: Performed to assess and measure blood flow. Transcutaneous oxygen pressure: Maps out areas of greater and lesser perfusion in the involved extremity. Thermography: Measures temperature differences in an ischemic limb at two sites: at the skin and center of the bone. The lower the difference between the two readings, the greater the chance for healing. Plethysmography: Segmental systolic BP measurements evaluate arterial blood flow. ESR: Elevation indicates inflammatory response. Wound cultures: Identify presence of infection and causative organism. WBC count/differential: Elevation and shift to left suggest infectious process. Biopsy: Confirms diagnosis of benign/malignant mass
NURSING CARE PLAN
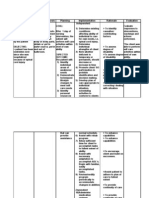
Impaired Physical Mobility
Related to: Loss of a limb (particularly a lower extremity); pain/discomfort; perceptual impairment (altered sense of
balance)
Possibly evidenced by Reluctance to attempt movement
Impaired coordination; decreased muscle strength, control, and mass
Desired Outcomes: Verbalize understanding of individual situation, treatment regimen, and safety measures.
Maintain position of function as evidenced by absence of contractures. Demonstrate techniques/behaviors that enable resumption of activities. Display willingness to participate in activities.
Nursing Interventions Provide stump care on a routine basis, e.g., inspect area, cleanse and dry thoroughly, and rewrap stump with elastic bandage or air splint, or apply a stump shrinker (heavy stockinette sock), for delayed prosthesis. Measure circumference periodically Rewrap stump immediately with an elastic bandage, elevate if immediate/early cast is accidentally dislodged. Prepare for reapplication of cast. Assist with specified ROM exercises for both the affected and unaffected limbs beginning early in postoperative stage.
Rationale Provides opportunity to evaluate healing and note complications (unless covered by immediate prosthesis). Wrapping stump controls edema and helps form stump into conical shape to facilitate fitting of prosthesis. Note: Air splint may be preferred, because it permits visual inspection of the wound Measurement is done to estimate shrinkage to ensure proper fit of sock and prosthesis. Edema will occur rapidly, and rehabilitation can be delayed
Prevents contracture deformities, which can develop rapidly and could delay prosthesis usage. Increases muscle strength to Encourage active/isometric exercises for upper facilitate transfers/ambulation and promote torso and unaffected limbs. mobility and more normal lifestyle. Provide trochanter rolls as indicated. Prevents external rotation of lower-limb stump Strengthens extensor muscles and prevents Instruct patient to lie in prone position as flexion contracture of the hip, which can begin tolerated at least twice a day with pillow under to develop within 24 hr of sustained abdomen and lower-extremity stump. malpositioning. Use of pillows can cause permanent flexion Caution against keeping pillow under lowercontracture of hip; a dependent position of extremity stump or allowing BKA limb to hang stump impairs venous return and may increase dependently over side of bed or chair. edema formation. Facilitates self-care and patients Demonstrate/assist with transfer techniques and independence. Proper transfer techniques use of mobility aids, e.g., trapeze, crutches, or prevent shearing abrasions/dermal injury walker. related to scooting. Reduces potential for injury. Ambulation after Assist with ambulation. lower-limb amputation depends on timing of
Instruct patient in stump-conditioning exercises
Refer to rehabilitation team
Provide foam/flotation mattress.
prosthesis placement. Hardens the stump by toughening the skin and altering feedback of resected nerves to facilitate use of prosthesis. Provides for creation of exercise/activity program to meet individual needs and strengths, and identifies mobility functional aids to promote independence. Early use of a temporary prosthesis promotes activity and enhances general well-being/positive outlook. Note: Vocational counseling/retraining also may be indicated. Reduces pressure on skin/tissues that can impair circulation, potentiating risk of tissue ischemia/breakdown
Risk for Infection
Risk factors may include Inadequate primary defenses (broken skin, traumatized tissue)
Invasive procedures; environmental exposure Chronic disease, altered nutritional status
Desired Outcomes Achieve timely wound healing; be free of purulent drainage or erythema; and be afebrile.
Nursing Interventions Maintain aseptic technique when changing dressings/caring for wound. Inspect dressings and wound; note characteristics of drainage. Rationale Minimizes opportunity for introduction of bacteria. Early detection of developing infection provides opportunity for timely intervention and prevention of more serious complications. Hemovac, Jackson-Pratt drains facilitate removal of drainage, promoting wound healing and reducing risk of infection. Prevents contamination in lower-limb amputation. Maintains cleanliness, minimizes skin contaminants, and promotes healing of tender/fragile skin. Temperature elevation/tachycardia may reflect developing sepsis. Identifies presence of infection/specific organisms and
Maintain patency and routinely empty drainage device. Cover dressing with plastic when using the bedpan or if incontinent. Expose stump to air; wash with mild soap and water after dressings are discontinued. Monitor vital signs. Obtain wound/drainage cultures and sensitivities as
appropriate.
Administer antibiotics as indicated.
appropriate therapy. Wide-spectrum antibiotics may be used prophylactically, or antibiotic therapy may be geared toward specific organisms.
Situational Low Self-Esteem
May be related to Loss of body part/change in functional abilities Possibly evidenced by Anticipated changes in lifestyle; fear of rejection/reaction by others
Negative feelings about body, focus on past strength, function, or appearance Feelings of helplessness, powerlessness Preoccupation with missing body part, not looking at or touching stump Perceived change in usual patterns of responsibility/physical capacity to resume role
Desired Outcomes Begin to show adaptation and verbalize acceptance of self in situation (amputee).
Recognize and incorporate changes into self-concept in accurate manner without negating self-esteem. Develop realistic plans for adapting to new role/role modifications.
Nursing Interventions
Assess/consider patients preparation for and view of amputation.
Encourage expression of fears, negative feelings, and grief over loss of body part. Reinforce preoperative information including type/location of amputation, type of prosthetic fitting if appropriate (i.e., immediate, delayed), expected postoperative course, including pain control and rehabilitation. Assess degree of support available to patient. Ascertain individual strengths and identify
Rationale Research shows that amputation poses serious threats to patients psychological and psychosocial adjustment.Patient who views amputation as life-saving or reconstructive may be able to accept the new self more quickly.Patient with sudden traumatic amputation or who considers amputation to be the result of failure in other treatments is at greater risk for self-concept disturbances. Venting emotions helps patient begin to deal with the fact and reality of life without a limb. Provides opportunity for patient to question and assimilate information and begin to deal with changes in body image and function, which can facilitate postoperative recovery. Sufficient support by SO and friends can facilitate rehabilitation process. Helpful to build on strengths that are already
previous positive coping behaviors.
Encourage participation in ADLs. Provide opportunities to view/care for stump, using the moment to point out positive signs of healing.
Encourage/provide for visit by another amputee, especially one who is successfully rehabilitating. Note withdrawn behavior, negative self-talk, use of denial, or over concern with actual/perceived changes. Provide open environment for patient to discuss concerns about sexuality. Discuss availability of various resources, e.g., psychiatric/ sexual counseling, occupational therapist.
available for patient to use in coping with current situation. Promotes independence and enhances feelings of self worth. Although integration of stump into body image can take months or even years, looking at the stump and hearing positive comments (made in a normal, matterof-fact manner) can help patient with this acceptance. A peer who has been through a similar experience serves as a role model and can provide validity to comments and hope for recovery and a normal future. Identifies stage of grief/need for interventions. Promotes sharing of beliefs/values about sensitive subject, and identifies misconceptions/myths that may interfere with adjustment to situation. May need assistance for these concerns to facilitate optimal adaptation and rehabilitation.
Das könnte Ihnen auch gefallen
- 25 FREE Coaching Tools and TechniquesDokument69 Seiten25 FREE Coaching Tools and TechniquesLuiza Sava97% (29)
- Self EsteemDokument7 SeitenSelf Esteembalachmalik100% (1)
- B00H83LE66 SoftArchive - Net WomenDokument102 SeitenB00H83LE66 SoftArchive - Net WomensuzukishareNoch keine Bewertungen
- Limbatic BrainDokument6 SeitenLimbatic BrainKarthick KaruppusamyNoch keine Bewertungen
- Nursing Diagnosis Related ToDokument9 SeitenNursing Diagnosis Related ToGrape JuiceNoch keine Bewertungen
- Exposure TherapyDokument8 SeitenExposure TherapyFatima MalikNoch keine Bewertungen
- Stevens-Johnson Syndrome CASEDokument38 SeitenStevens-Johnson Syndrome CASEChristy Rose AgrisNoch keine Bewertungen
- Log Rolling A PatientDokument27 SeitenLog Rolling A PatientIrish Jane Gallo100% (1)
- IMAGINERIA AFECTIVA GUIADA - Hanscarl Leuner Con Notas en EspañolDokument17 SeitenIMAGINERIA AFECTIVA GUIADA - Hanscarl Leuner Con Notas en EspañolmariafeveNoch keine Bewertungen
- Nursing Care Plan For "Hysterectomy"Dokument10 SeitenNursing Care Plan For "Hysterectomy"jhonroks94% (18)
- NCP OsteosarcomaDokument6 SeitenNCP OsteosarcomaNiksNoch keine Bewertungen
- DM NCPDokument8 SeitenDM NCPCaress Mae Gubaton CabudoyNoch keine Bewertungen
- Impaired Physical Mobility NCPDokument3 SeitenImpaired Physical Mobility NCPMeljonesDaan100% (1)
- Challenging Cognitive Distortions HealthyPsych - ComDokument1 SeiteChallenging Cognitive Distortions HealthyPsych - ComLeila MargaridaNoch keine Bewertungen
- NCP Potts DiseaseDokument2 SeitenNCP Potts Diseasearcitap0% (1)
- Robbins mgmt15 PPT 16Dokument43 SeitenRobbins mgmt15 PPT 1620211211018 DHANI AKSAN ARASYAD100% (1)
- 4 Amputation Nursing Care Plans - Nurseslabs-1 PDFDokument12 Seiten4 Amputation Nursing Care Plans - Nurseslabs-1 PDFsaidi MwanamongaNoch keine Bewertungen
- In General, Amputation of Limbs Is TheDokument11 SeitenIn General, Amputation of Limbs Is TheCay Sevilla100% (1)
- Hospital Attachment Report: Kenya Medical Training College, Thika CampusDokument3 SeitenHospital Attachment Report: Kenya Medical Training College, Thika CampusCollins Otieno100% (1)
- Communicable Diseases ReviewerDokument12 SeitenCommunicable Diseases ReviewerClarissa GuifayaNoch keine Bewertungen
- Pott Disease 1223292121651385 8Dokument54 SeitenPott Disease 1223292121651385 8Ismail SalimNoch keine Bewertungen
- Nursing Skills Output (Nso)Dokument4 SeitenNursing Skills Output (Nso)Julius ElciarioNoch keine Bewertungen
- Journal Diabetes MellitusDokument11 SeitenJournal Diabetes Mellitusnabila noorNoch keine Bewertungen
- Unit 1 5ADokument7 SeitenUnit 1 5AArvin O-CaféNoch keine Bewertungen
- E. Nursing DiagnosisDokument2 SeitenE. Nursing DiagnosisAle SandraNoch keine Bewertungen
- 10 Triage, Stabilization, Transport, CommunicationDokument24 Seiten10 Triage, Stabilization, Transport, CommunicationYui HirasawaNoch keine Bewertungen
- 2 - Prevention of Iatrogenic InjuriesDokument34 Seiten2 - Prevention of Iatrogenic InjuriesMariya DantisNoch keine Bewertungen
- NPI NCMH StephDokument12 SeitenNPI NCMH StephAnonymous 2fUBWme6wNoch keine Bewertungen
- Earthquake-Report in WordDokument3 SeitenEarthquake-Report in WordHazel Penix Dela CruzNoch keine Bewertungen
- Nursing Care Plan A Client With HemophiliaDokument1 SeiteNursing Care Plan A Client With Hemophilia08000046Noch keine Bewertungen
- Perioperative Nursing Version 2Dokument38 SeitenPerioperative Nursing Version 2Justine CagatanNoch keine Bewertungen
- Group 5 - Experiment No.10 - Culture and SensitivityDokument11 SeitenGroup 5 - Experiment No.10 - Culture and SensitivityPMG BrightNoch keine Bewertungen
- Journal - A Review of Diabetes MellitusDokument6 SeitenJournal - A Review of Diabetes Mellitusifaans16Noch keine Bewertungen
- Case Presentation For Blount's Disease B Proximal TibiaDokument43 SeitenCase Presentation For Blount's Disease B Proximal TibiaCzarinah Joyce Novencido0% (1)
- NCP Acute PainDokument2 SeitenNCP Acute PainLyka Mae DominguezNoch keine Bewertungen
- COVID-19: Brian, Fernando, Jason, FelitaDokument8 SeitenCOVID-19: Brian, Fernando, Jason, FelitaCharson ChenNoch keine Bewertungen
- Oks Na To Thank U Aubs!!: Okiii!!! Wuv U All!Dokument10 SeitenOks Na To Thank U Aubs!!: Okiii!!! Wuv U All!CiaraNoch keine Bewertungen
- Dos and Dont in OtDokument3 SeitenDos and Dont in OttanishaNoch keine Bewertungen
- NCM 118 Medsurg EndtermDokument25 SeitenNCM 118 Medsurg EndtermJmarie Brillantes PopiocoNoch keine Bewertungen
- Orientation On Community Health - Doh Programs & ServicesDokument11 SeitenOrientation On Community Health - Doh Programs & ServicesAudrey Beatrice ReyesNoch keine Bewertungen
- Ch42 NCP IneffectiveCoping 1075-1076Dokument2 SeitenCh42 NCP IneffectiveCoping 1075-1076Dizerine Mirafuentes RolidaNoch keine Bewertungen
- Thoracentesis Reflective EssayDokument2 SeitenThoracentesis Reflective EssayAnjae GariandoNoch keine Bewertungen
- Pathophysiology Hypokalemia Periodic ParalysisDokument4 SeitenPathophysiology Hypokalemia Periodic Paralysisloyea0% (2)
- NCPDokument5 SeitenNCPf_jm06_gNoch keine Bewertungen
- Case StudyDokument5 SeitenCase StudyMoath MahmoudNoch keine Bewertungen
- Or RRLDokument4 SeitenOr RRLAlponce Edal AdagNoch keine Bewertungen
- Epidemiology and Pathophysiology of Colonic Diverticular DiseaseDokument8 SeitenEpidemiology and Pathophysiology of Colonic Diverticular DiseaseAnonymous Hz5w55Noch keine Bewertungen
- NCP Hip FractureDokument5 SeitenNCP Hip FractureCherry Ann BalagotNoch keine Bewertungen
- Brain Surgery Post Op NCPDokument6 SeitenBrain Surgery Post Op NCPunnamed personNoch keine Bewertungen
- Nur 111 Session 1 Sas 1Dokument8 SeitenNur 111 Session 1 Sas 1Zzimply Tri Sha UmaliNoch keine Bewertungen
- Annotated Group 2 Impetigo Concept Mapping 1Dokument30 SeitenAnnotated Group 2 Impetigo Concept Mapping 1DHANE ANN CAMPOSANONoch keine Bewertungen
- Hepatitis B VaccineDokument3 SeitenHepatitis B VaccineChoox PriiNoch keine Bewertungen
- CHN Notes PrelimDokument30 SeitenCHN Notes PrelimCHINGCHONG SLAYERNoch keine Bewertungen
- Final ResearchDokument65 SeitenFinal ResearchHarbrinder GurmNoch keine Bewertungen
- Ameloblastoma PathophysiologyDokument2 SeitenAmeloblastoma PathophysiologyKongzter 康明美100% (2)
- Cholera & DysenteryDokument28 SeitenCholera & DysenterySherbaz Sheikh100% (1)
- Nur 111 Session 18 Sas 1Dokument11 SeitenNur 111 Session 18 Sas 1Zzimply Tri Sha UmaliNoch keine Bewertungen
- Philippine Nursing Act of 2002 (R.A. No. 9173)Dokument85 SeitenPhilippine Nursing Act of 2002 (R.A. No. 9173)Lorraine Nicolne B. CortejoNoch keine Bewertungen
- Evidence-Based Nursing: I. Clinical QuestionDokument4 SeitenEvidence-Based Nursing: I. Clinical QuestionRay Jorge MarmetoNoch keine Bewertungen
- Nurse Patient Interaction (NPI)Dokument15 SeitenNurse Patient Interaction (NPI)ever existenceNoch keine Bewertungen
- Philippine Nursing Organizations Org Name DescriptionDokument8 SeitenPhilippine Nursing Organizations Org Name DescriptionShehada Marcos BondadNoch keine Bewertungen
- Esophagus, TearDokument36 SeitenEsophagus, Tearapi-19641337Noch keine Bewertungen
- Community Health Nursing-1 Unit 2Dokument52 SeitenCommunity Health Nursing-1 Unit 2Asif Ali LashariNoch keine Bewertungen
- Psych - Chapter 23 Into To Milieu ManagementDokument4 SeitenPsych - Chapter 23 Into To Milieu ManagementKaren かれんNoch keine Bewertungen
- Nursing Diagnosis May Be Related To Possibly Evidenced byDokument37 SeitenNursing Diagnosis May Be Related To Possibly Evidenced byLea TanNoch keine Bewertungen
- Nursing Care PlansDokument22 SeitenNursing Care PlansAnonymous 0C4OZmR0% (1)
- Nursing Care Plans CVADokument6 SeitenNursing Care Plans CVAJeffrey Dela CruzNoch keine Bewertungen
- HysterectomyDokument10 SeitenHysterectomyJORINA PUMIHICNoch keine Bewertungen
- Medical Prognosis: Justification Onset of The IllnessDokument3 SeitenMedical Prognosis: Justification Onset of The IllnessJairah CandaoNoch keine Bewertungen
- Essay WorkDokument6 SeitenEssay Workgabrielle raichleNoch keine Bewertungen
- Finlay JonesDokument247 SeitenFinlay JonescovasaNoch keine Bewertungen
- Christian TransformationDokument21 SeitenChristian Transformationapi-128065301Noch keine Bewertungen
- SychologyDokument4 SeitenSychologyNiranjan DiwakarNoch keine Bewertungen
- Lesson PlanDokument5 SeitenLesson Planapi-242642664Noch keine Bewertungen
- Drug Addiction Treatment CenterDokument6 SeitenDrug Addiction Treatment CenterAndrew TanNoch keine Bewertungen
- Developmental SupervisionDokument63 SeitenDevelopmental SupervisionRitu Bansal100% (1)
- Worksheet - Collocations EmotionsDokument3 SeitenWorksheet - Collocations EmotionsTanitaNoch keine Bewertungen
- Chapter 3 Values, Attitudes and Job Satisfaction - 2Dokument32 SeitenChapter 3 Values, Attitudes and Job Satisfaction - 2مولنارزقىNoch keine Bewertungen
- Student Pre SurveyDokument7 SeitenStudent Pre Surveyapi-490976036Noch keine Bewertungen
- Unit 14 Psychological DisordersDokument15 SeitenUnit 14 Psychological DisordersDorsa RadNoch keine Bewertungen
- Trauma in Early Childhood: A Neglected PopulationDokument20 SeitenTrauma in Early Childhood: A Neglected PopulationFrancisca AldunateNoch keine Bewertungen
- Experience of Mental Health in Women With Polycystic Ovary Syndrome A Descriptive Phenomenological StudyDokument11 SeitenExperience of Mental Health in Women With Polycystic Ovary Syndrome A Descriptive Phenomenological StudyMelany AntounNoch keine Bewertungen
- 33 Diagnosis Keperawatan Jiwa NANDADokument1 Seite33 Diagnosis Keperawatan Jiwa NANDAAnonymous W09Ufp8VJNoch keine Bewertungen
- Boat Designer Interview QuestionsDokument6 SeitenBoat Designer Interview QuestionsVirgil SorcaruNoch keine Bewertungen
- 20 - Appendix 6 PDFDokument36 Seiten20 - Appendix 6 PDFKumud SharmaNoch keine Bewertungen
- George R. Taylor - Improving Human Learning in The Classroom - Theories and Teaching Practices-Rowman & Littlefield Education (2008) PDFDokument327 SeitenGeorge R. Taylor - Improving Human Learning in The Classroom - Theories and Teaching Practices-Rowman & Littlefield Education (2008) PDFsiddharth100% (1)
- Grade 2 Home LinksDokument11 SeitenGrade 2 Home Linksapi-360345401Noch keine Bewertungen
- Rorscach Ink Blot DescriptionDokument10 SeitenRorscach Ink Blot DescriptionDandy VictaNoch keine Bewertungen
- Resilience ResearchDokument5 SeitenResilience Researchvidhi yadavNoch keine Bewertungen
- Technology and Psychology - (Yair - Amichai-Hamburger) PDFDokument303 SeitenTechnology and Psychology - (Yair - Amichai-Hamburger) PDFAyu Puji LestariNoch keine Bewertungen